Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Diagrams / tables | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining - normal | Negative staining - disease | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Cite this page: McDonald W. SF1. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainssf1.html. Accessed March 31st, 2025.
Definition / general
- Steroidogenic factor 1 (SF1) is a member of the steroid receptor superfamily; a transcription factor that regulates genes involved in gonadal and adrenal steroidogenesis
- Present in pituitary and steroidogenic tissues:
- Anterior pituitary gonadotrophs, which produce luteinizing hormone (LH) or follicle stimulating hormone (FSH); not found in other adenohypophyseal cell types
- Adrenal cortex
- Granulosa and theca cells of the ovary
- Sertoli and Leydig cells of the testis
- Pituitary adenoma / pituitary neuroendocrine tumor has traditionally been classified using a combination of immunohistochemical stains for anterior pituitary hormones, including stains for prolactin, growth hormone, thyrotroph (TSH), luteinizing hormone (LH), follicle stimulating hormone (FSH), adrenocorticotropic hormone (ACTH) and the alpha subunit (ASU) of the glycoprotein hormones
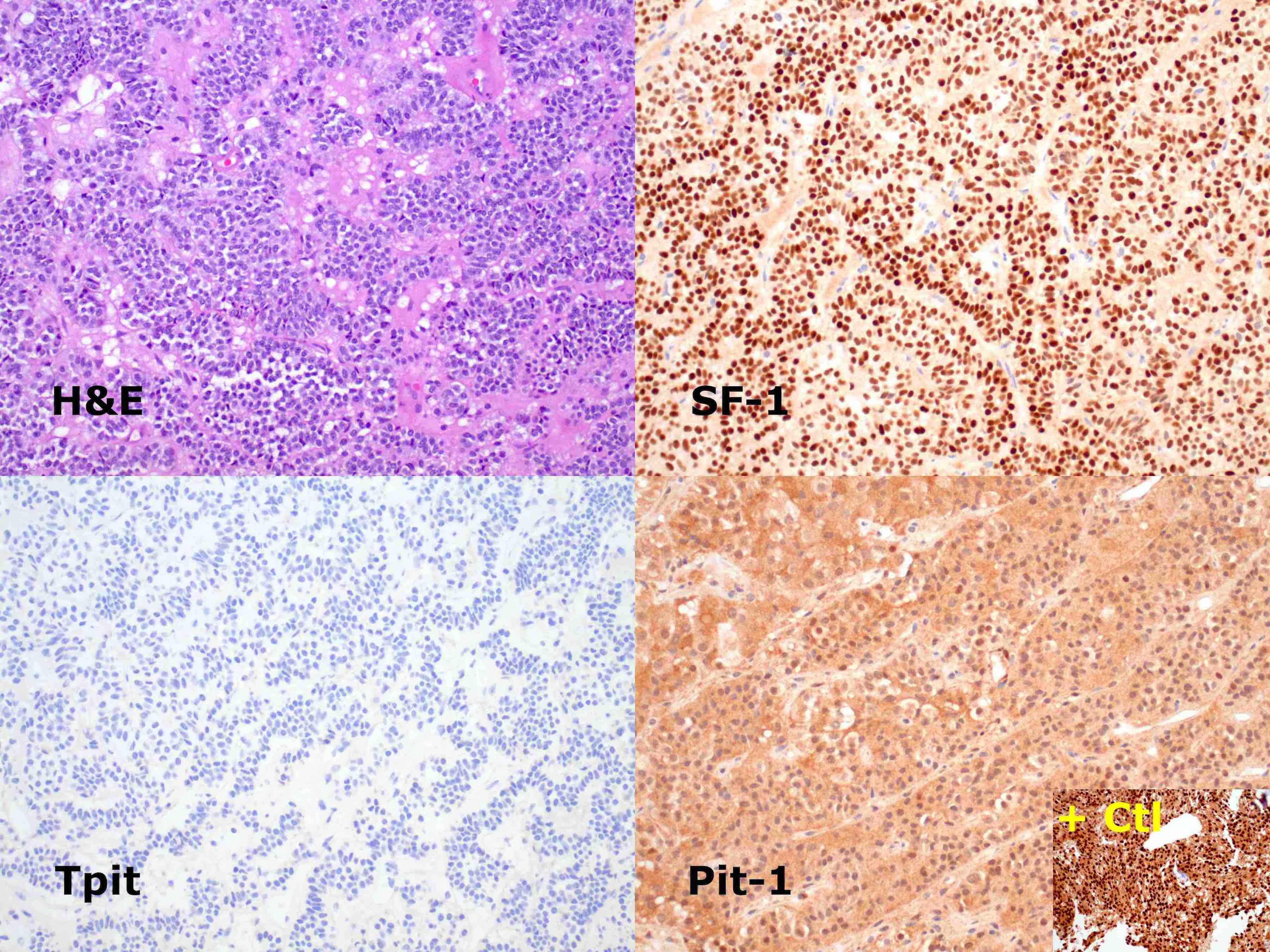
- Immunostains for anterior pituitary transcription factors steroidogenic factor 1 (SF1), Pit1 and T box transcription factor (Tpit) have been shown to have higher sensitivity and specificity than hormone IHC stains and are often used in conjunction with them to classify pituitary adenomas
Essential features
- Strong nuclear staining
- Is expressed within the anterior pituitary gland and steroidogenic tissues of the gonads and adrenal glands
- Within the pituitary, SF1 is the stain of choice for gonadotrophic pituitary adenomas
- SF1 is also useful in resolving difficult differential diagnoses for tumors involving the adrenal gland and gonads
Terminology
- Steroidogenic factor 1 (SF1)
Pathophysiology
- SF1 has roles within the pituitary and periphery; it is necessary for the development of primary steroidogenic tissue (knockout mice lack adrenal and gonadal glands)
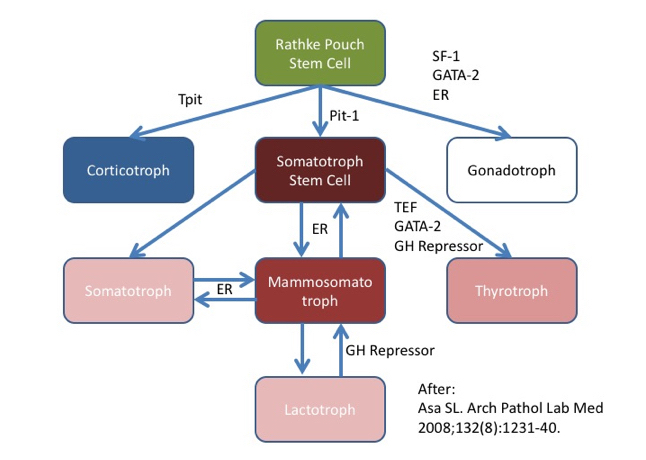
- In the pituitary, SF1 drives gonadotroph differentiation (J Clin Endocrinol Metab 1996;81:2165, see diagram below)
- Gonadotroph adenomas comprise the largest category of pituitary adenomas (Arch Pathol Lab Med 2017;141:104, Mod Pathol 2018;31:900)
- LH and FSH immunostains also mark gonadotroph adenomas but are much less sensitive (although quite specific) (Mod Pathol 2018;31:900)
- Some labs use alpha subunit of glycoprotein hormones or estrogen receptors to supplement gonadotroph tumor workup but these lack both sensitivity and specificity (Mod Pathol 2018;31:900)
Clinical features
- Most gonadotroph adenomas are hormonally silent macroadenomas
- Tumors of the adrenal cortex, ovary and testis may be difficult to distinguish from other neoplasms
Interpretation
- Nuclear expression is evaluated (reactivity only in the cytoplasm is regarded as negative)
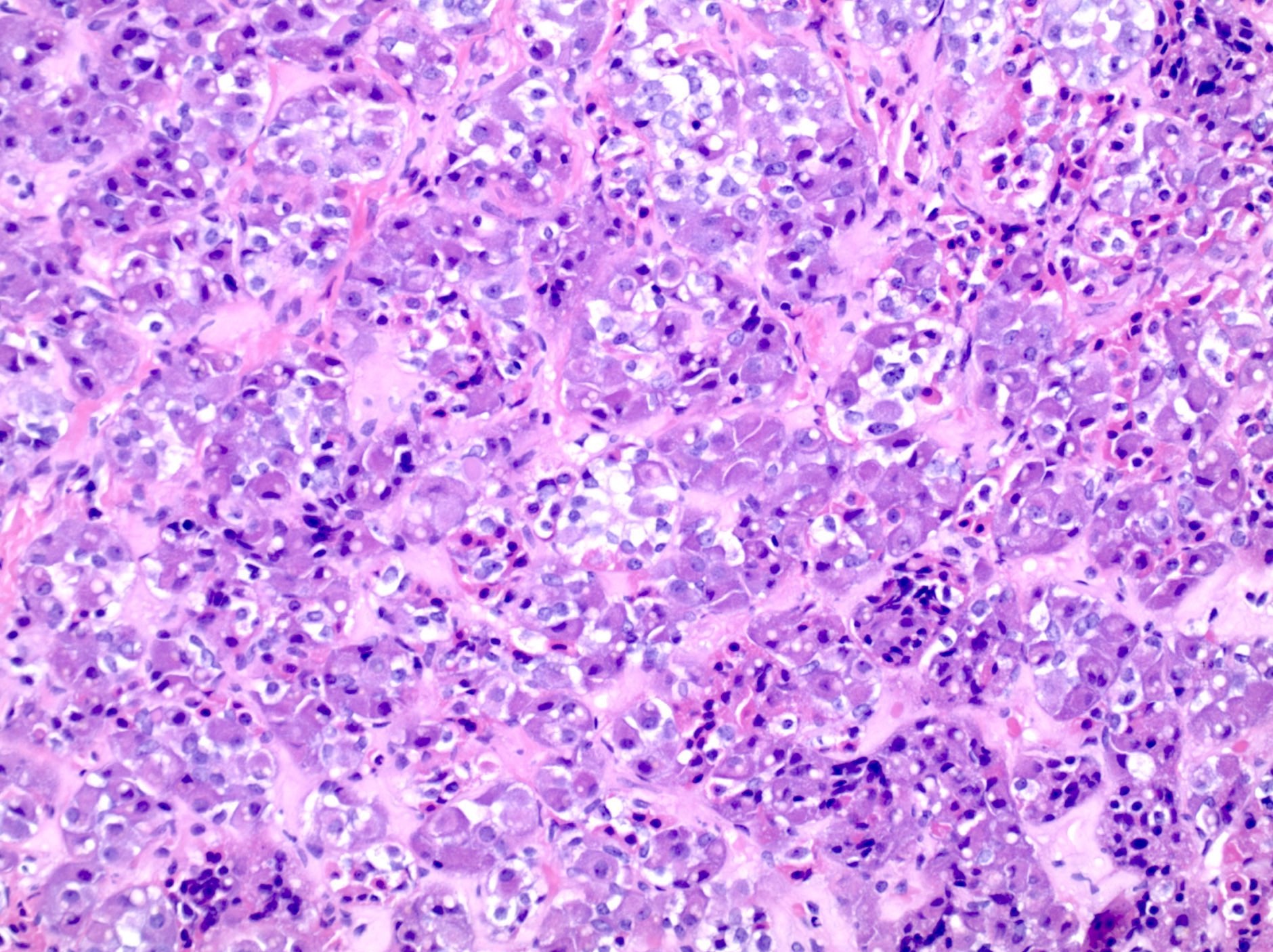
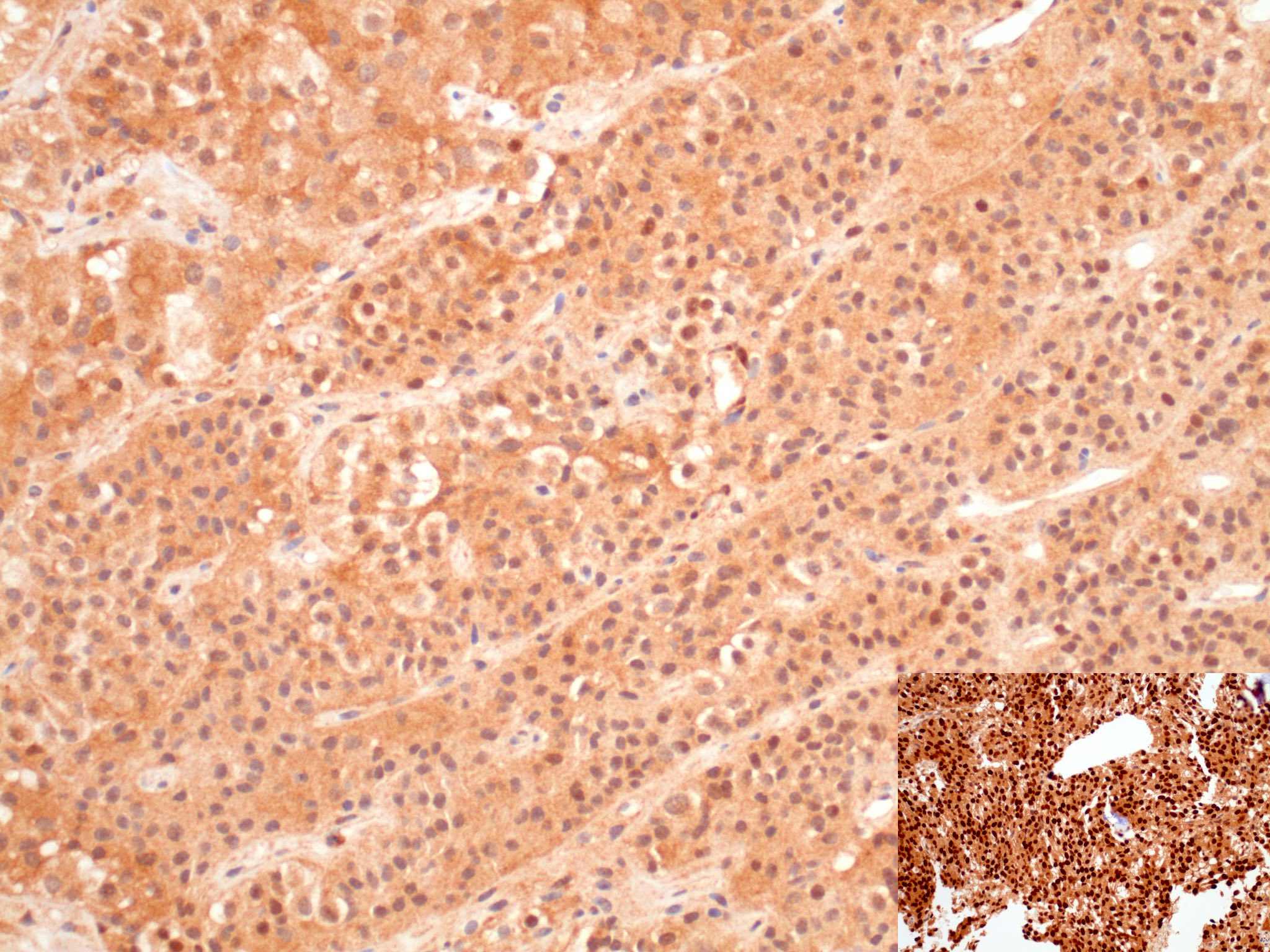
- SF1 immunoreactivity in gonadotroph adenoma is typically diffuse, strong and nuclear (score 7 or 8 in the Allred scale, Mod Pathol 1998;11:155; see photomicrograph below)
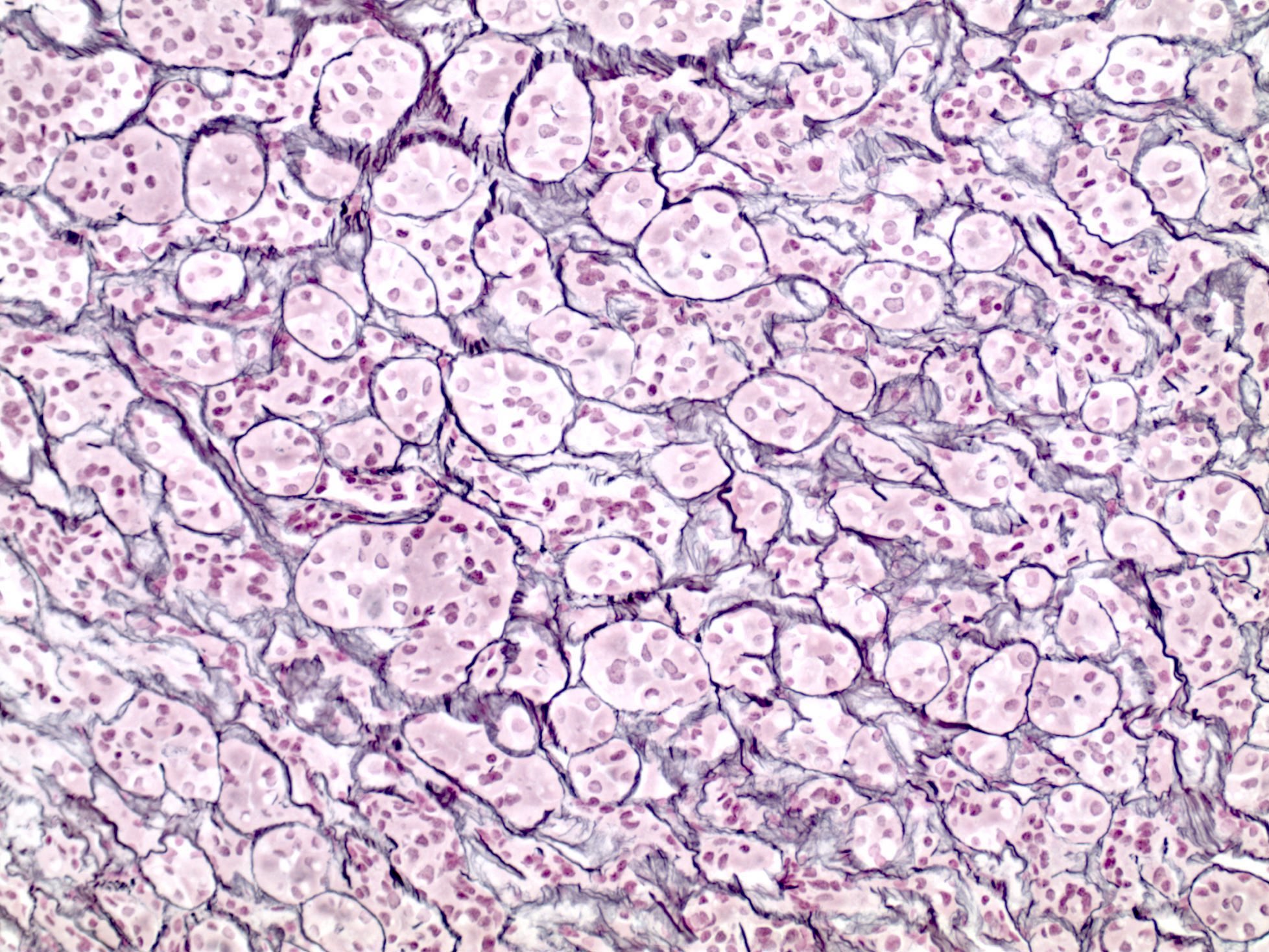
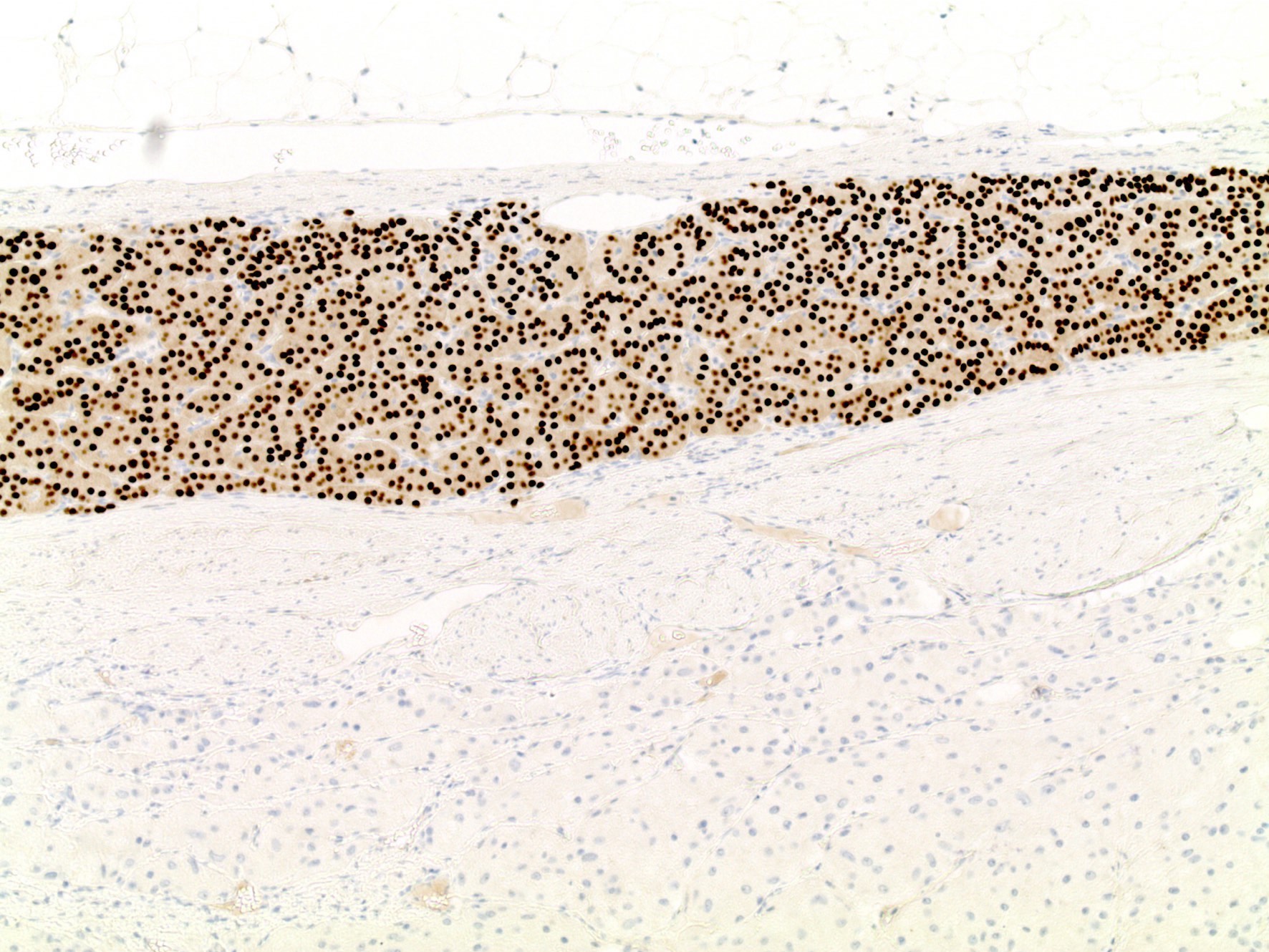
- SF1 immunoreactivity in anterior pituitary gland (nonneoplastic anterior pituitary) shows moderate to strong nuclear staining in scattered adenohypophysis cells; gonadotrophs are a minority population within the adenohypophysis
Uses by pathologists
- Useful for diagnosis of gonadotroph adenomas (Arch Pathol Lab Med 2017;141:104, Mod Pathol 2018;31:900)
- More sensitive than antibodies to LH and FSH (Mod Pathol 2018;31:900)
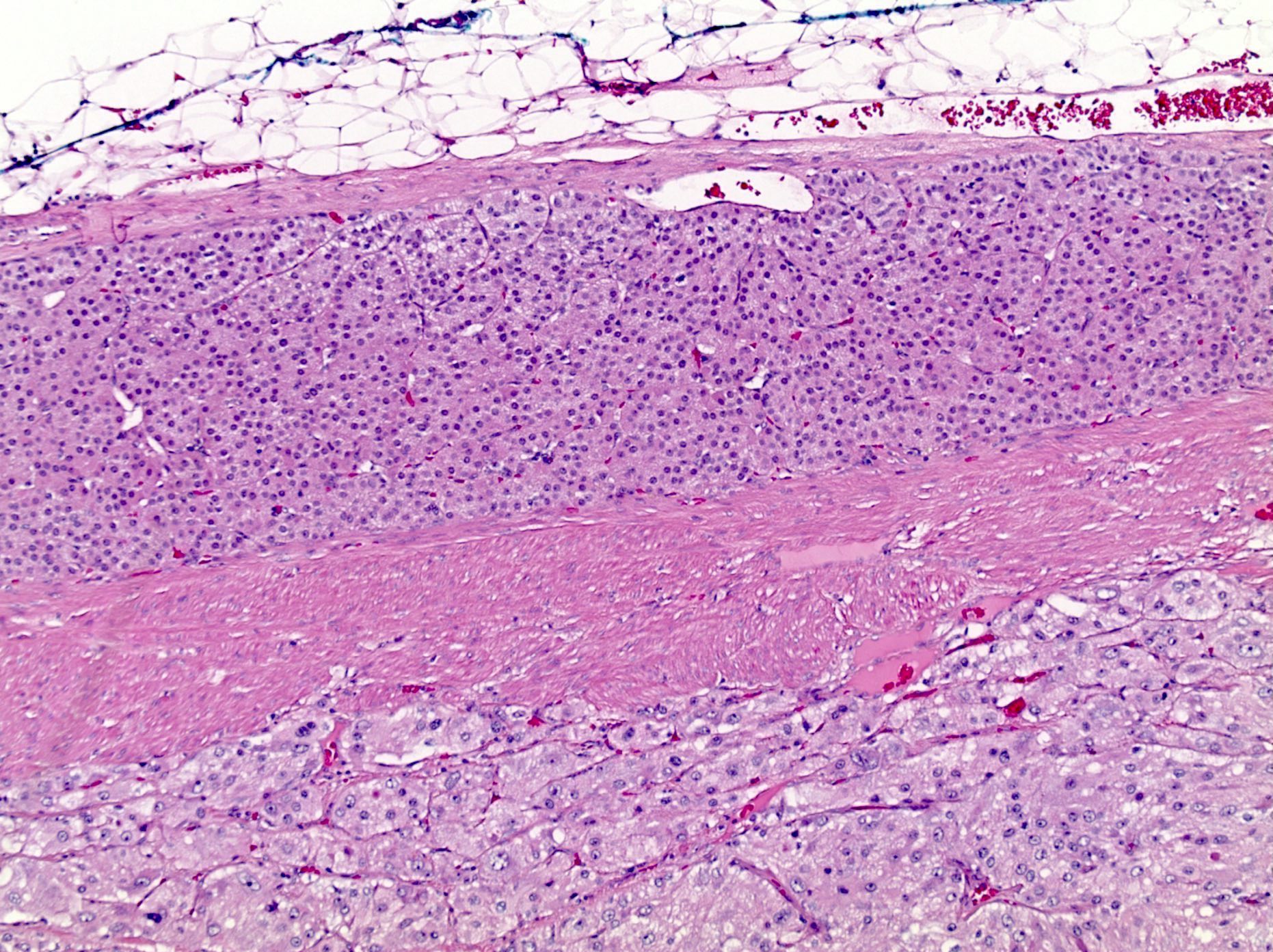
- Also present within normal anterior pituitary gland so the presence of pituitary adenoma must be confirmed on H&E stains (occasionally with the support of ancillary stains such as reticulin for normal adenohypophyseal architecture)
- Often used in conjunction with other pituitary transcription factor IHC; see Pit1 and Tpit (Arch Pathol Lab Med 2021;145:592)
- Sensitive and specific marker of sex cord stromal tumors of the ovary and can be used to distinguish these tumors from other types of ovarian tumors (Int J Gynecol Pathol 2008;27:507, Am J Surg Pathol 2009;33:354, Int J Gynecol Pathol 2016;35:167, Pathology 2016;48:434, Int J Gynecol Pathol 2008;27:507)
- Helpful in distinguishing adrenal cortical neoplasms from other tumor types (Hum Pathol 2013;44:822, Appl Immunohistochem Mol Morphol 2012;20:141, Am J Surg Pathol 2010;34:423, Am J Surg Pathol 2011;35:678, J Clin Endocrinol Metab 2010;95:E161)
- Useful in the setting of testicular tumors (Am J Surg Pathol 2015;39:1159, Appl Immunohistochem Mol Morphol 2013;21:318)
Prognostic factors
- Pituitary adenoma type is considered a prognostic factor
- Gonadotroph adenoma is felt to be more indolent than some other types of nonfunctioning adenoma (Expert Rev Endocrinol Metab 2016;11:149)
- Radiographic extent and adenoma classification are considered prognostic indicators
- High risk pituitary adenomas include sparsely granulated somatotroph adenoma, lactotroph adenoma in men, Crooke cell adenoma, silent corticotroph adenoma and plurihormonal Pit1+ adenoma
- Category of atypical adenoma was not reproducible so was removed from WHO classification (Endocrin Pathol 2017;28:228)
Microscopic (histologic) images
Positive staining - normal
- Scattered gonadotrophs in normal adenohypophysis (J Clin Endocrinol Metab 1996;81:2165)
- Adrenal cortex (Cell 1994;77:481)
- Atrophic testis, cryptorchidism, normal testis (Appl Immunohistochem Mol Morphol 2013;21:318)
Positive staining - disease
- Gonadotroph pituitary adenomas (Arch Pathol Lab Med 2017;141:104, Mod Pathol 2018;31:900)
- Rare plurihormonal pituitary adenomas
- Sex cord stromal tumors of ovary (Histopathology 2013;62:71, Int J Gynecol Pathol 2008;27:507, Am J Surg Pathol 2009;33:354, Int J Gynecol Pathol 2016;35:167, Pathology 2016;48:434)
- Sertoli and Leydig cell tumors of testis (Appl Immunohistochem Mol Morphol 2013;21:318)
- Adrenal cortical tumors (Hum Pathol 2013;44:822, Appl Immunohistochem Mol Morphol 2012;20:141, Am J Surg Pathol 2010;34:423, Am J Surg Pathol 2011;35:678, J Clin Endocrinol Metab 2010;95:E161)
Negative staining - normal
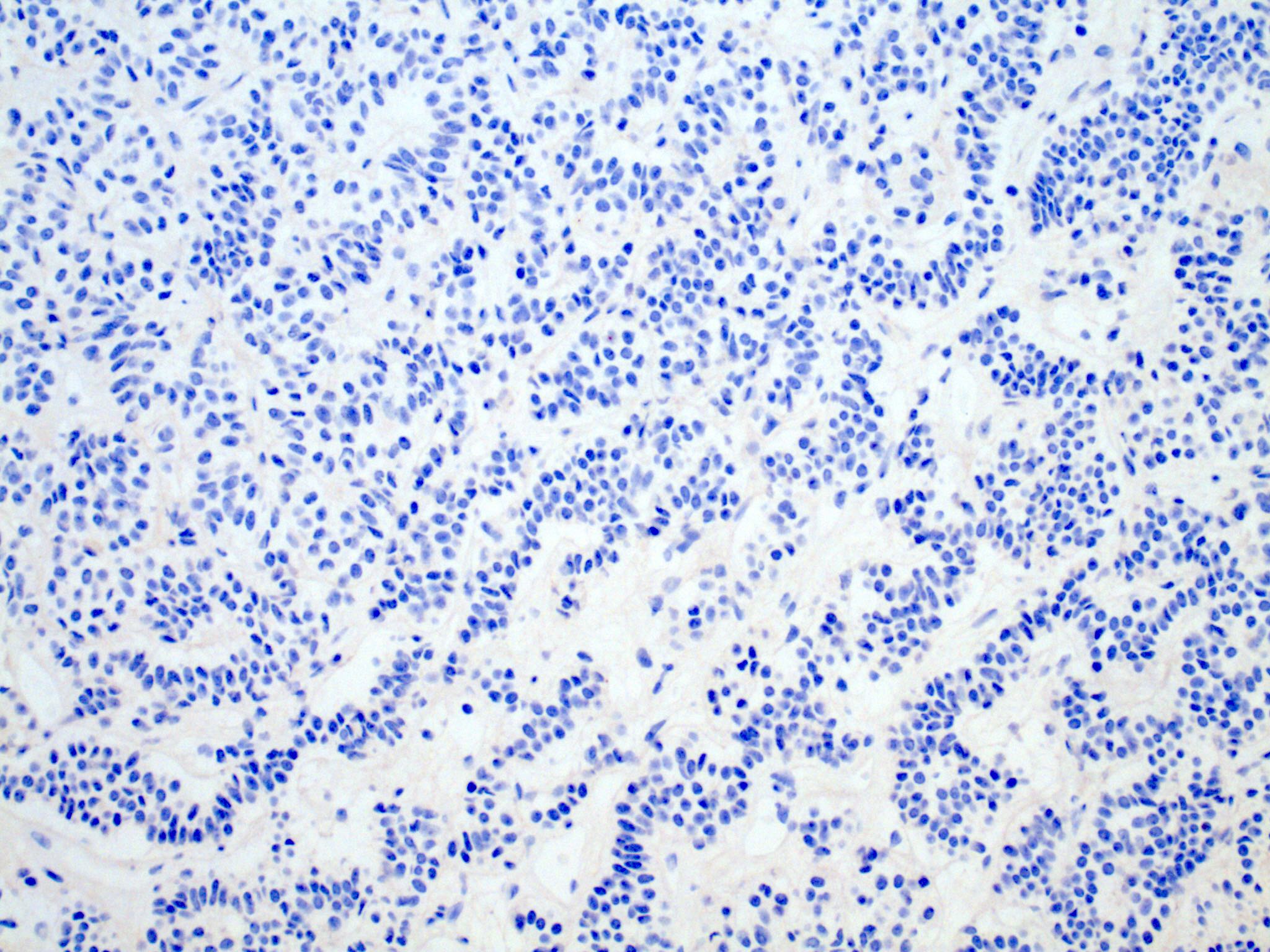
- Corticotrophs, Pit1 family adenohypophysial cells (producing prolactin, growth hormone or TSH)
Negative staining - disease
- Pituitary adenomas in the Pit1 family, corticotroph family (Arch Pathol Lab Med 2017;141:104, Mod Pathol 2018;31:900)
- Uterine tumor resembling ovarian sex cord stromal tumor (UTROSCT) (Pathology 2016;48:434)
- Nonsteroidogenic adrenal tumors, pheochromocytoma (J Clin Endocrinol Metab 2010;95:E161, Am J Surg Pathol 2010;34:423)
- Testicular germ cell tumors (Appl Immunohistochem Mol Morphol 2013;21:318)
- Endometrioid tumors and carcinoid (Int J Gynecol Pathol 2008;27:507)
Sample pathology report
- Sella turcica, resection:
- Pituitary adenoma (pituitary neuroendocrine tumor), gonadotroph type (see comment)
- Comment: This tumor shows diffuse nuclear immunoreactivity for SF1 and no immunoreactivity for Pit1 or Tpit. In the context of a macroadenoma without clinical or laboratory evidence of hormone excess, this is a gonadotroph adenoma.
- Clinical information: The patient presented with a 3 week history of visual blurring. Bitemporal hemianopsia was noted on ophthalmologic exam. Magnetic resonance imaging showed a 3.5 cm sellar and suprasellar mass extending into the suprasellar cistern and compressing the optic chiasm.
- Available preoperative endocrine testing:
- Prolactin 5.90 (2.74 - 19.64 ng/mL)
- IGF1 72 (57 - 202 ng/mL)
- TSH 0.64 (0.35 - 4.94 uIU/mL)
- Free T4 1.31 (0.70 - 1.80 ng/dL)
- Cortisol 10.4 (1330 draw, 5.0 - 15.0 ug/dL)
Additional references
Board review style question #1
A 57 year old man presents with bitemporal hemianopsia, mildly elevated serum prolactin and MRI showing a 2.5 cm mass within the sella turcica, which is noted to extend upward and push on the optic chiasm. Physical examination reveals no signs of hormone excess (no evidence of gynecomastia, galactorrhea, Cushing syndrome, acromegaly, etc.) and formal visual field testing confirms decreased vision in the outer half of the visual fields. Transsphenoidal resection confirms pituitary adenoma by routine stains. The adenoma shows immunohistochemical staining as illustrated above. How is this adenoma best classified?
- Corticotroph adenoma
- Gonadotroph adenoma
- Null cell adenoma
- Prolactinoma
Board review style answer #1
B. Gonadotroph adenoma. Absence of signs of hormone excess is the usual finding in gonadotroph adenoma. A small rise in prolactin can be seen in association with any lesion of the sella turcica that impinges on the stalk of the pituitary, interrupting dopaminergic inhibition of lactotrophs in the nonneoplastic anterior pituitary gland. SF1 immunohistochemistry is the most sensitive and specific means of classifying gonadotroph adenoma.
Comment Here
Reference: SF1
Comment Here
Reference: SF1