Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - tumors | Negative staining - normal | Negative staining - tumors | Board review style question #1 | Board review style answer #1Cite this page: Wang S, Hu Z. T cell leukemia / lymphoma protein 1 (TCL1). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsTCL1.html. Accessed April 2nd, 2025.
Definition / general
- Locus: 14q32.13
- Protein expression in immature T and B lymphoid cells
- Overexpression of TCL1 is considered critical in the oncogenetic transformation (Nat Rev Cancer 2005;5:640)
Essential features
- Normally found in early embryonic tissue, the ovary, and lymphoid lineage cells (Blood 2005;105:1288)
- Expressed in B cells, under both reactive and neoplastic conditions, from antigen committed B cells to germinal center B cells (Cancer Res 2000;60:2095)
- Down regulated in the latest stage of B cell differentiation
- Positive in precursor B cells (hematogones) (Hum Pathol 2017;65:175)
- Homogenously highly expressed in Burkitt lymphoma (N Engl J Med 2006;354:2495, Am J Surg Pathol 2008;32:113)
- Overexpression in 80 - 90% of T cell prolymphocytic leukemia (Am J Hematol 2017;92:441)
- Often shows cytoplasmic and nuclear staining pattern
Terminology
- Other alias: T cell leukemia / lymphoma 1
Clinical features
- T cell prolymphocytic leukemia is usually associated with inv(14)(q11;q32) or t(14;14)(q11;q32), which juxtaposes T cell leukemia 1 (TCL1) coding region with T cell receptor (TCR) locus at 14q11, resulting in overexpression of TCL1 oncoprotein (J Clin Pathol 2018;71:309)
Uses by pathologists
- Differentiates T prolymphocytic leukemia (TCL1+) from other mature T cell lymphomas / leukemia (TCL1-) (J Clin Pathol 2018;71:309)
- Differentiates blastic plasmacytoid dendritic cell neoplasm (TCL1+) from myeloid / monocytic sarcoma or NK cell lymphoma (TCL1-) (Blood 2003;101:5007, Mod Pathol 2014;27:1137)
- May have prognostic significance in B cell lymphomas
Prognostic factors
- Overexpression may be a poor prognostic factor for chronic lymphocytic leukemia and mantle cell lymphoma (Mod Pathol 2009;22:206)
- Expression correlates with an adverse clinical outcome in diffuse large B cell lymphoma (Int J Oncol 2005;26:151)
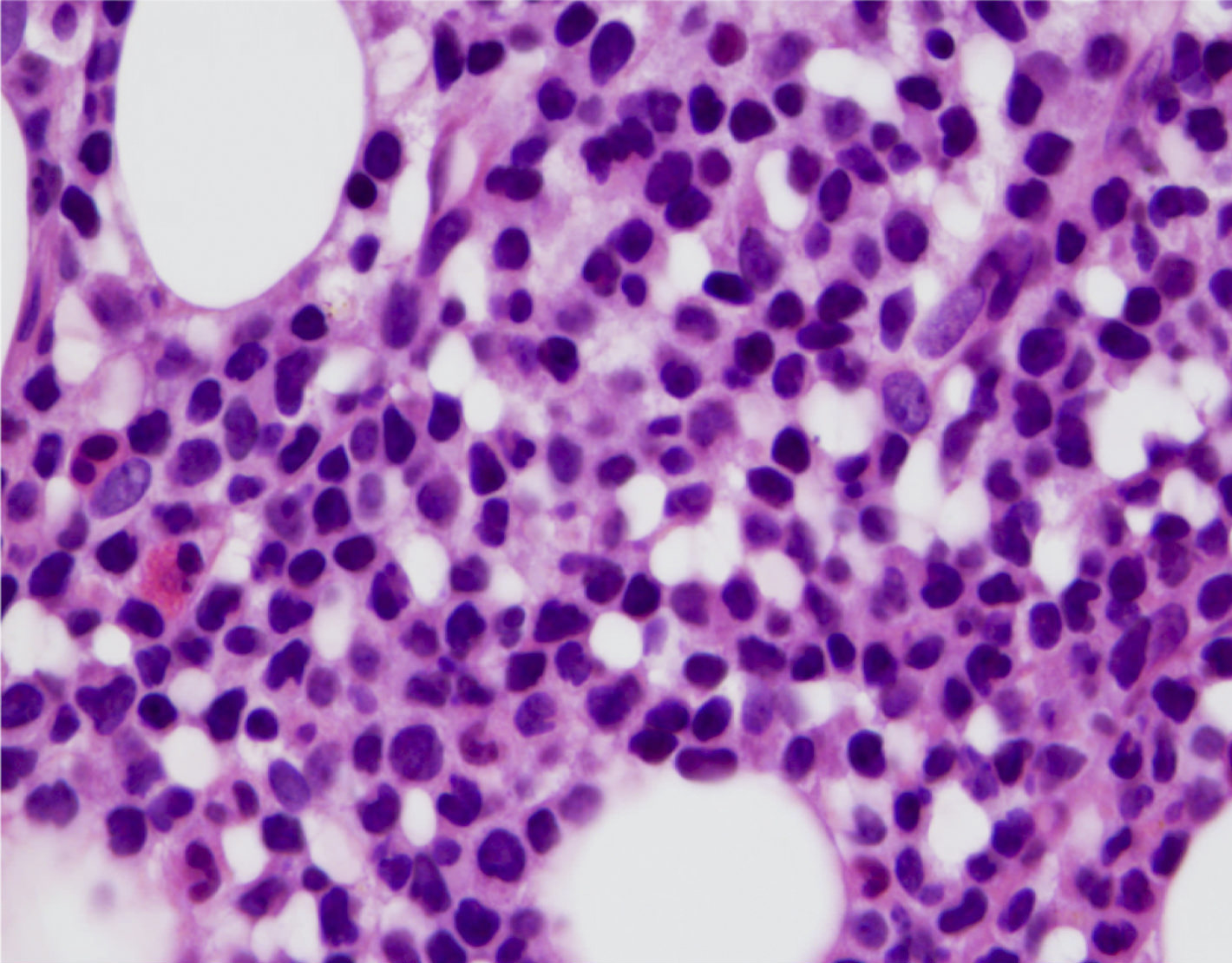
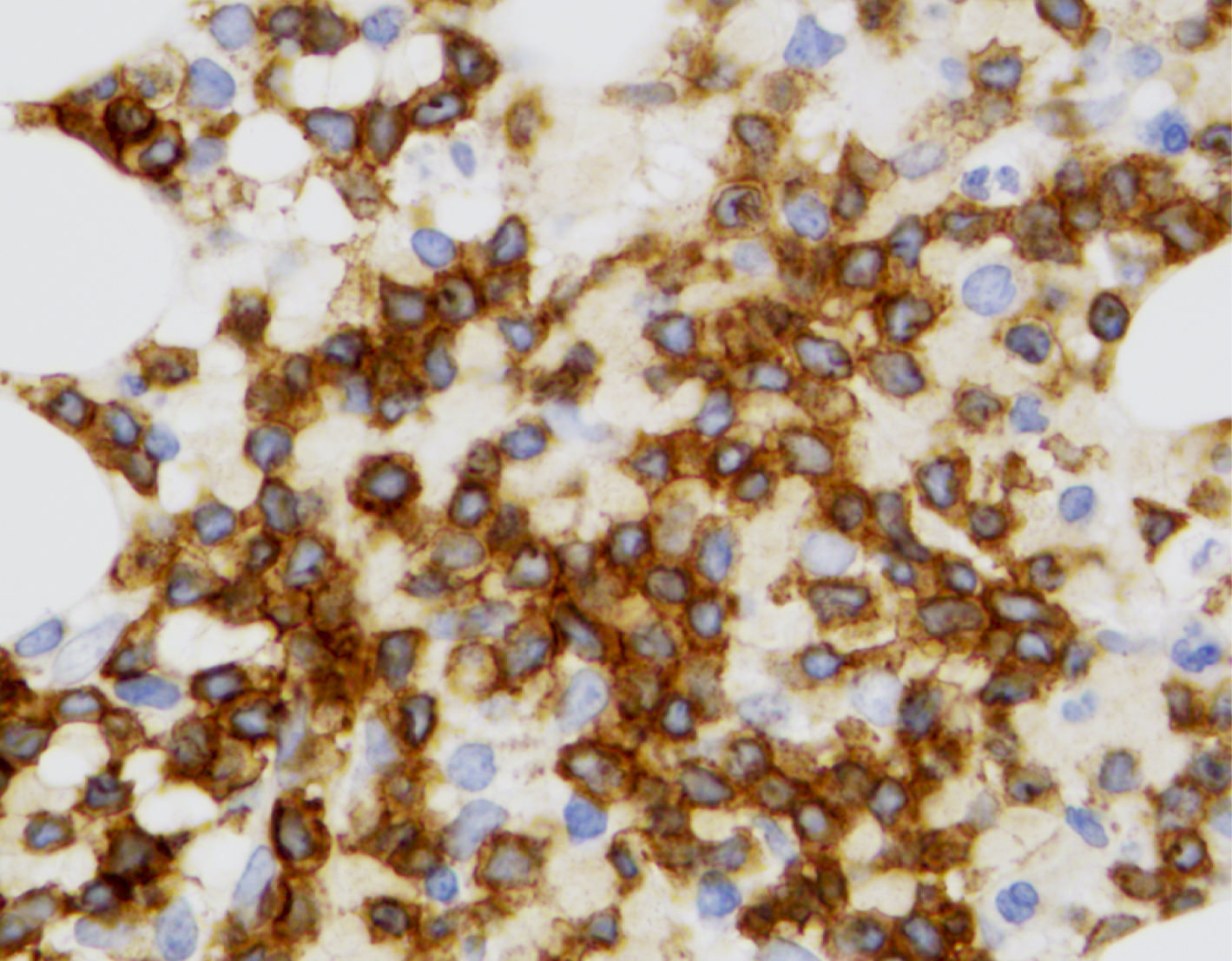
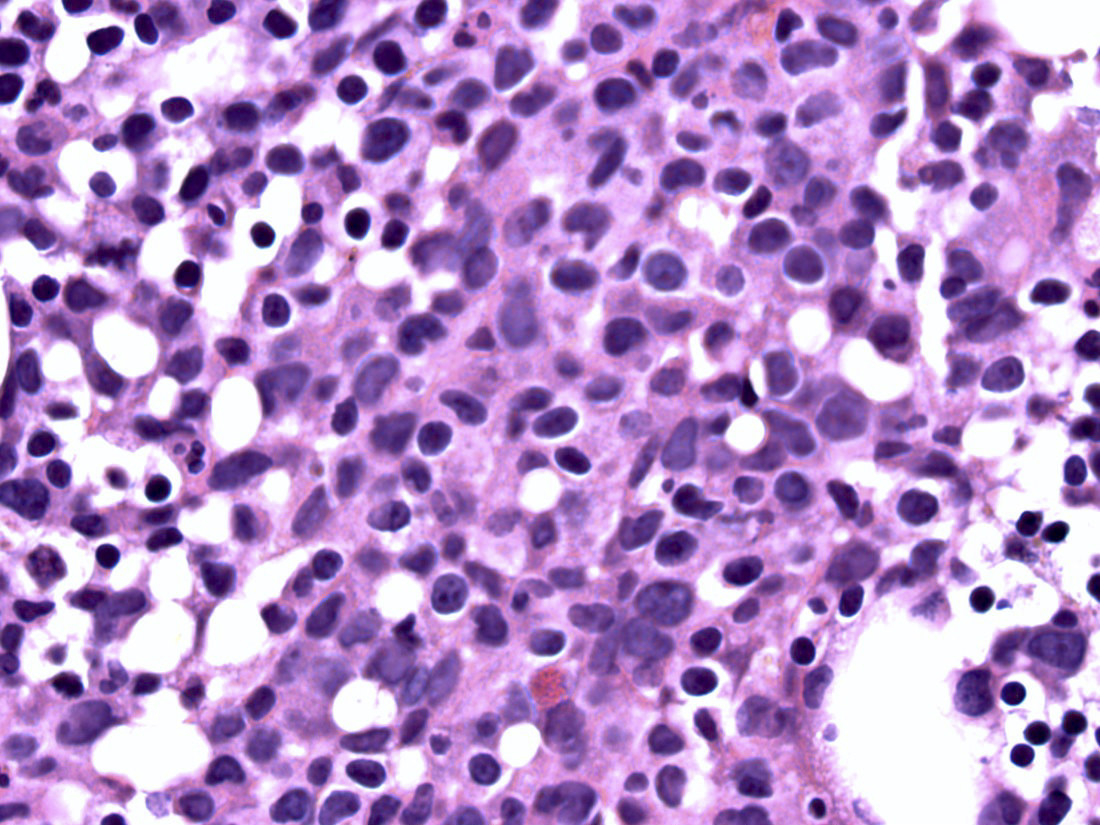
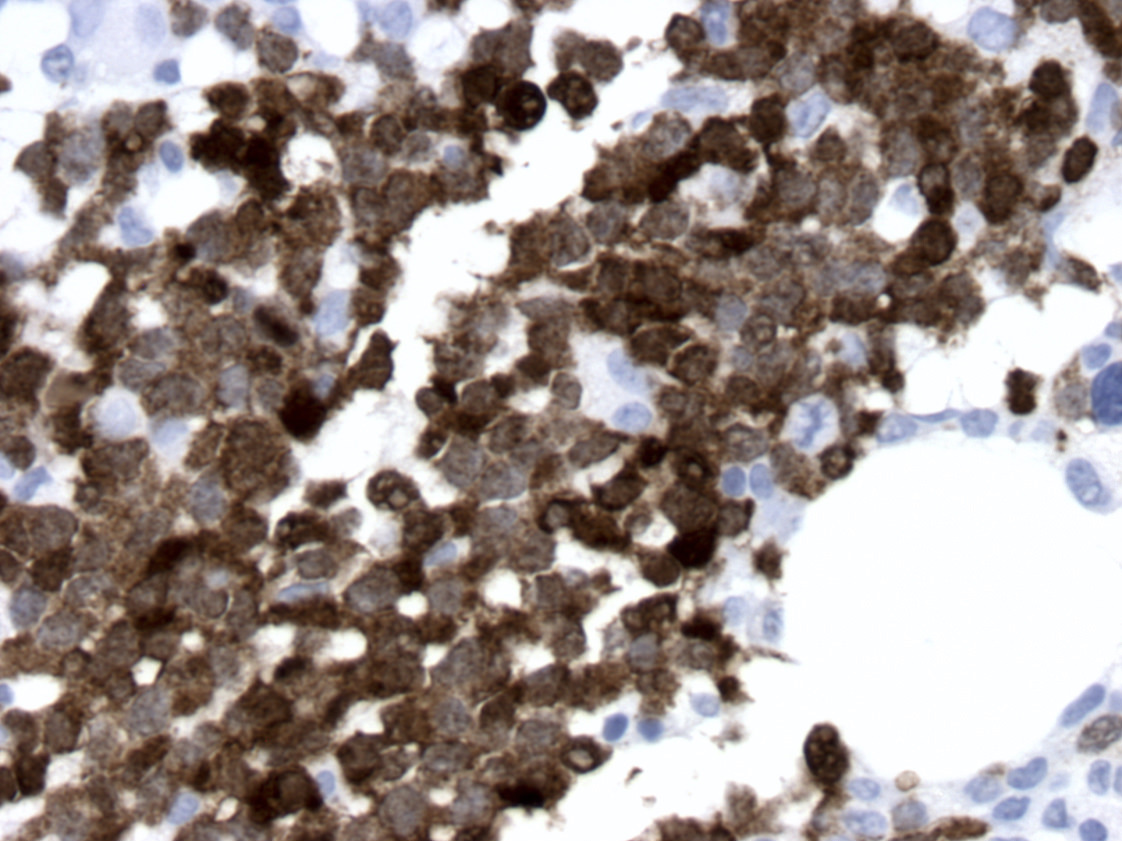
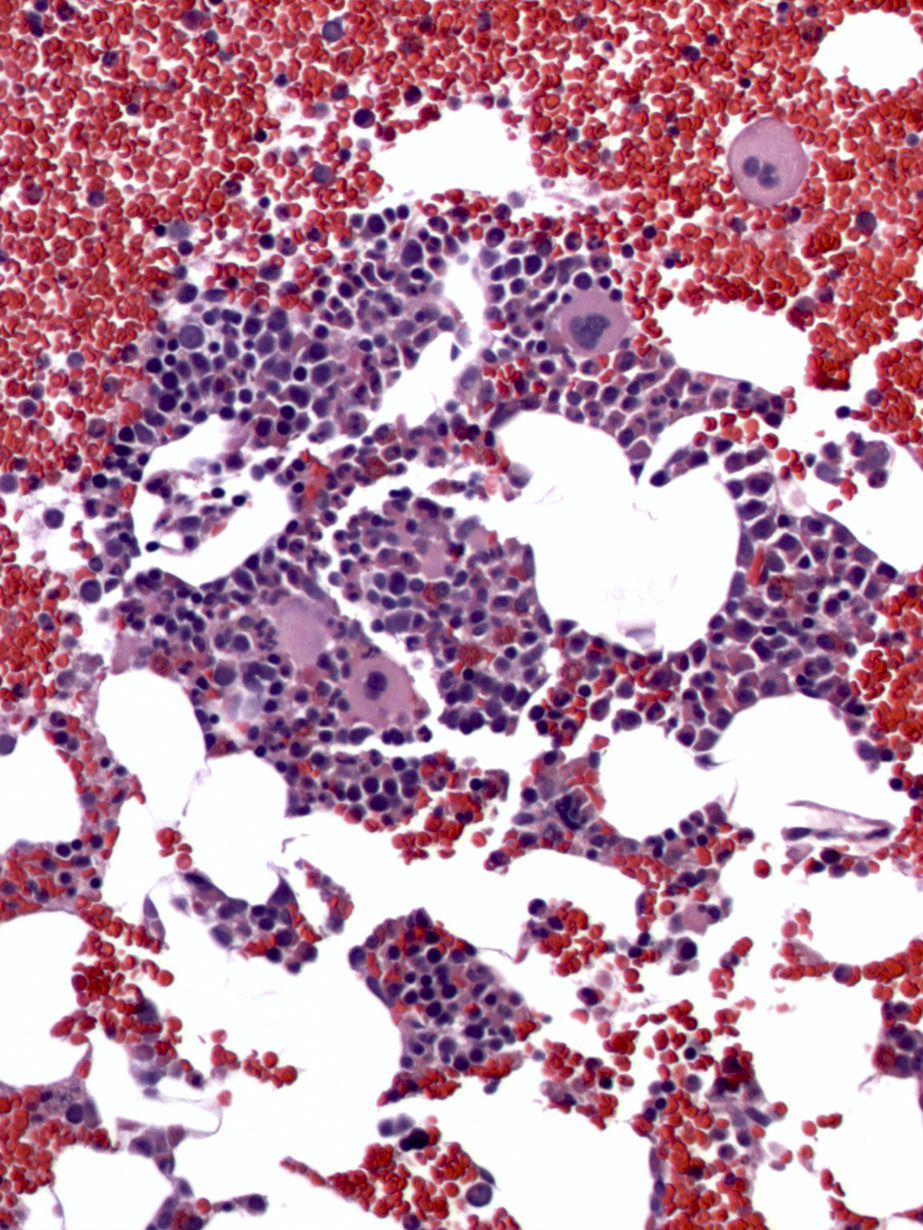
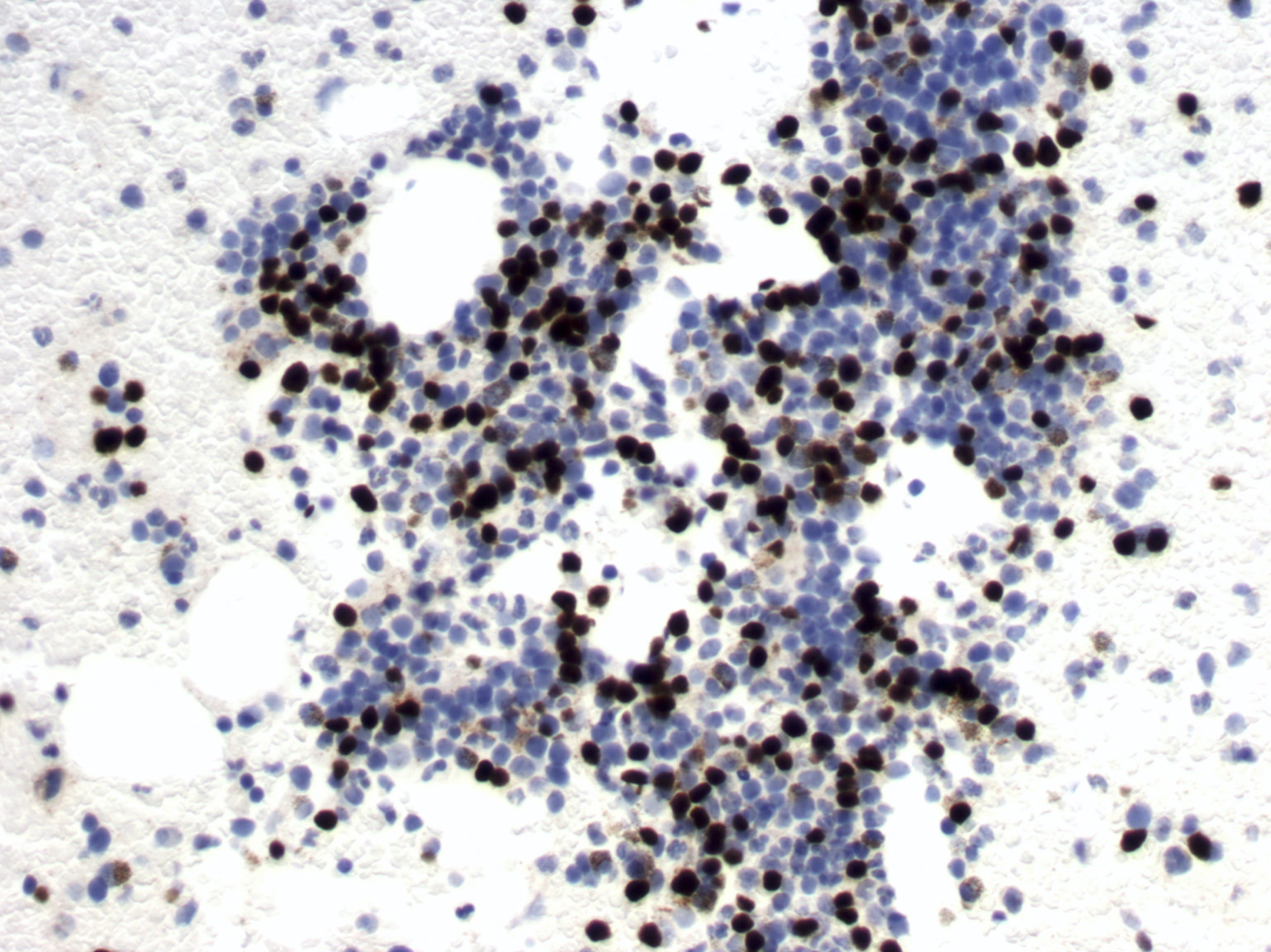
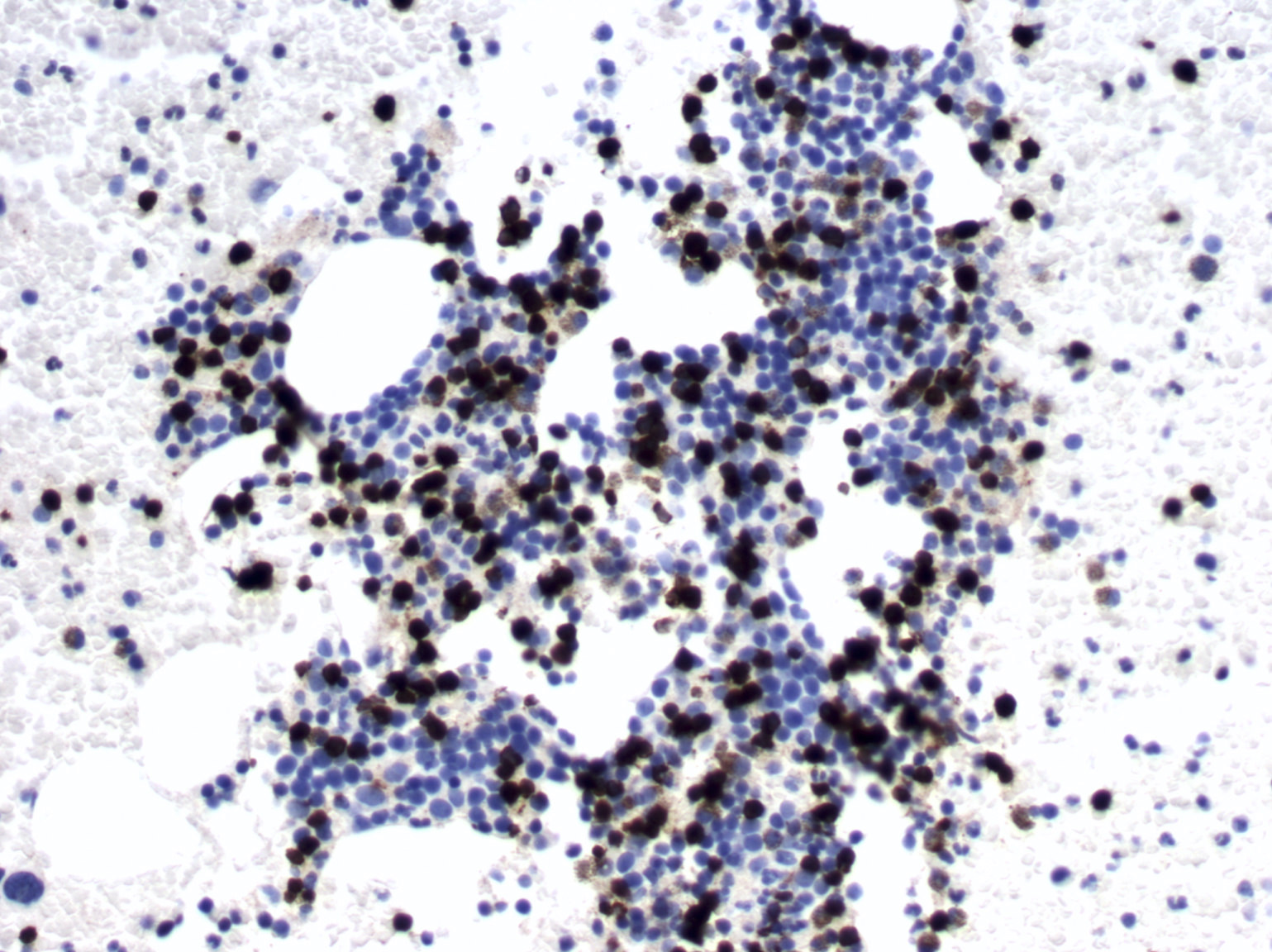
Microscopic (histologic) images
Positive staining - normal
- Precursor B cells (hematogones) (Hum Pathol 2017;65:175)
- Various subsets of normal B cells, from antigen committed B cells to germinal center B cells
- Surface CD3− CD4− CD8− thymocytes (Nat Rev Cancer 2005;5:640)
- Early embryogenesis in fetal lymphoid tissues, including liver, yolk sac, thymus, spleen, tonsil and bone marrow (Proc Natl Acad Sci U S A 2002;99:11712)
- Highly expressed in normal plasmacytoid dendritic cells in lymph nodes, tonsils, spleen and bone marrow (Blood 2003;101:5007)
Positive staining - tumors
- T cell prolymphocytic leukemia
- Blastic plasmacytoid dendritic cell neoplasm
- Burkitt lymphoma
- Hairy cell leukemia (Virchows Arch 2012;461:677)
- Diffuse large B cell lymphoma
- Follicular lymphoma
- Chronic lymphocytic leukemia
- Mantle cell lymphoma
- Testicular seminoma and intratubular neoplasia but infrequent in mediastinal seminoma (Am J Clin Pathol 2010;133:762, Histopathology 2010;57:152, Hum Pathol 2015;46:376)
- Adenocarcinoma, Barrett esophagus (Oncol Rep 2014;31:1745)
Negative staining - normal
- Post germinal center memory B cells and plasma cells (Proc Natl Acad Sci U S A 2002;99:10014)
- Normal mature T cells in the periphery (Nat Rev Cancer 2005;5:640)
- NK cells
- Bone marrow hematopoietic cells
Negative staining - tumors
- Other mature T cell lymphomas except T cell prolymphocytic leukemia (J Clin Pathol 2018;71:309, Blood 2003;101:5007)
- Classic Hodgkin lymphoma
- Multiple myeloma
- Splenic marginal zone lymphoma (Blood 2012;120:1613)
- Myeloid sarcoma, monocytic sarcoma and other dendritic and histiocytic tumors
- Nonseminomatous germ cell tumors
Board review style question #1
A 60 year old man presented with skin lesions and peripheral blood smear showing marked leukocytosis with lymphocytosis. The lymphocytes are small to medium with small nucleoli. Flow cytometry analysis is of peripheral blood sample shows an aberrant T cell population with the immunophenotype of
CD2+ / CD3+ / CD4+ / CD7+ / CD8+ / CD26+ / TCRa / b. Which stain would be most helpful to make a diagnosis on this patient?
CD2+ / CD3+ / CD4+ / CD7+ / CD8+ / CD26+ / TCRa / b. Which stain would be most helpful to make a diagnosis on this patient?
- CD25
- CD30
- CD123
- TCL1
- TDT
Board review style answer #1
D. TCL1 stain. The major differential diagnoses include mycosis fungoides (MF) with blood involvement. Mycosis fungoides cells are more cerebriform and often show losses of CD7 and CD26 expression. Adult T cell leukemia / lymphoma often shows flower cells, with loss of CD26 and a bright expression of CD25. Peripheral T cell lymphoma with a leukemic presentation is uncommon; the immunophenotype is CD4 > CD8, with frequent CD7 loss. In the current case, the clinical presentation and immunophenotypic features of tumor cells are more in favor of T cell prolymphocytic leukemia. TCL1 protein is often overexpressed in 80 - 90% of T cell prolymphocytic leukemia, frequently due to TCL1 rearrangement as a result of inv(14)(q11;q32) or t(14;14)(q11;q32) but also can be overexpressed in the absence of the rearrangement. TCL1 is negative in mycosis fungoides, adult T cell lymphoma / leukemia and peripheral T cell lymphoma.
Comment Here
Reference: T cell leukemia / lymphoma protein 1 (TCL1)
Comment Here
Reference: T cell leukemia / lymphoma protein 1 (TCL1)