Table of Contents
Definition / general | Essential features | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Board review style question #1 | Board review style answer #1Cite this page: Chen-Yost HI, Antic T. Prostate specific antigen (PSA). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsPSA.html. Accessed March 31st, 2025.
Definition / general
- Androgen regulated serine protease
- Encoded by kallikrein gene (KLK3, kallikrein related peptidase 3) located on chromosome 19 (Endocr Rev 2010;31:407)
Essential features
- A cytoplasmic marker that is sensitive and specific for prostatic tissue and adenocarcinoma of prostatic origin
- Loss of PSA in prostatic adenocarcinoma correlates to poor differentiation and poor prognosis
- Negative in some prostate cancers, such as basal cell, squamous cell carcinoma and sarcomatous elements of carcinosarcoma
Pathophysiology
- Produced by the secretory cells of prostatic ducts and acini in males and Skene glands in females
- Regulated by androgen receptor
- Secreted into the lumen of the glands where it cleaves semenogelin I and II (PLoS One 2014;9:e107819)
- Semengolein I and II make coagulum, which mediates gel formation in semen
- Liquefied coagulum leads to release of sperm
Clinical features
- PSA level in blood has been used as a marker to detect prostate cancer (Clin Chem Lab Med 2020;58:326)
- Total PSA: both free and bound PSA
- Free PSA: amount of protein that has been inactivated by internal proteolytic cleavage
- Other ways to stratify prostate cancer risk with PSA
- Free PSA to total PSA ratio (f/t PSA) can be calculated (Med Clin North Am 2018;102:199)
- f/t PSA ratio of < 10 - 15% is highly suspicious for prostate cancer
- f/t PSA ratio of > 25% is more likely to be benign
- By itself has low sensitivity and specificity (Medicine 2018;67:e0249)
- MRI with elevated PSA can detect occult prostate cancers, even with negative biopsy (Eur Urol 2014;65:809)
- Free PSA to total PSA ratio (f/t PSA) can be calculated (Med Clin North Am 2018;102:199)
- Risks and benefits of PSA based screening
- Pros
- Screening increases the detection of prostate cancer versus having no screening (Cochrane Database Syst Rev 2013;1:CD004720)
- Cons
- Uncertain if screening decreases mortality (N Engl J Med 2020;382:1557)
- Can lead to overdiagnosis of indolent prostate cancer and lead to anxiety; exposes risk of prostate cancer therapy to patients with indolent cancer (including erectile and bladder dysfunction)
- Pros
- PSA caveats
- Can be falsely elevated in settings and conditions unrelated to carcinoma
- Postsurgical (i.e. cystoscopy)
- Age
- Nodular hyperplasia
- Prostatitis
- Infarction
- Post-ejaculation
- Can be falsely low with medications
- 5-alpha reductase inhibitors (used to treat benign prostatic hyperplasia) (Am Fam Physician 2010;81:76)
- Herbal mixtures
- Can be falsely elevated in settings and conditions unrelated to carcinoma
- The United States Preventive Service Task Force (USPSTF) states screening for prostate cancer for people of average risk should only occur if men express a preference for screening after being informed of and understanding the benefits and risks (JAMA 2018;319:1901)
- PSA based screening for men aged 55 - 69: C recommendation (no recommendation for or against)
- PSA based screening for men over 70 years old with < 15 year life span: D recommendation (recommend against)
- Men at higher risk of developing prostate cancer can start at 40 years
- BRCA carriers
- Black men
- Men with a family history, especially first degree relative who was diagnosed < 65 years old
- If a patient decides to be screened
- Perform PSA alone
- Digital rectal exam no longer recommended
- Frequency of PSA test: annually to every 2 years until at age where life expectancy is < 10 years
- Recommended PSA level for further evaluation: > 4.0 ng/mL
- Perform PSA alone
Interpretation
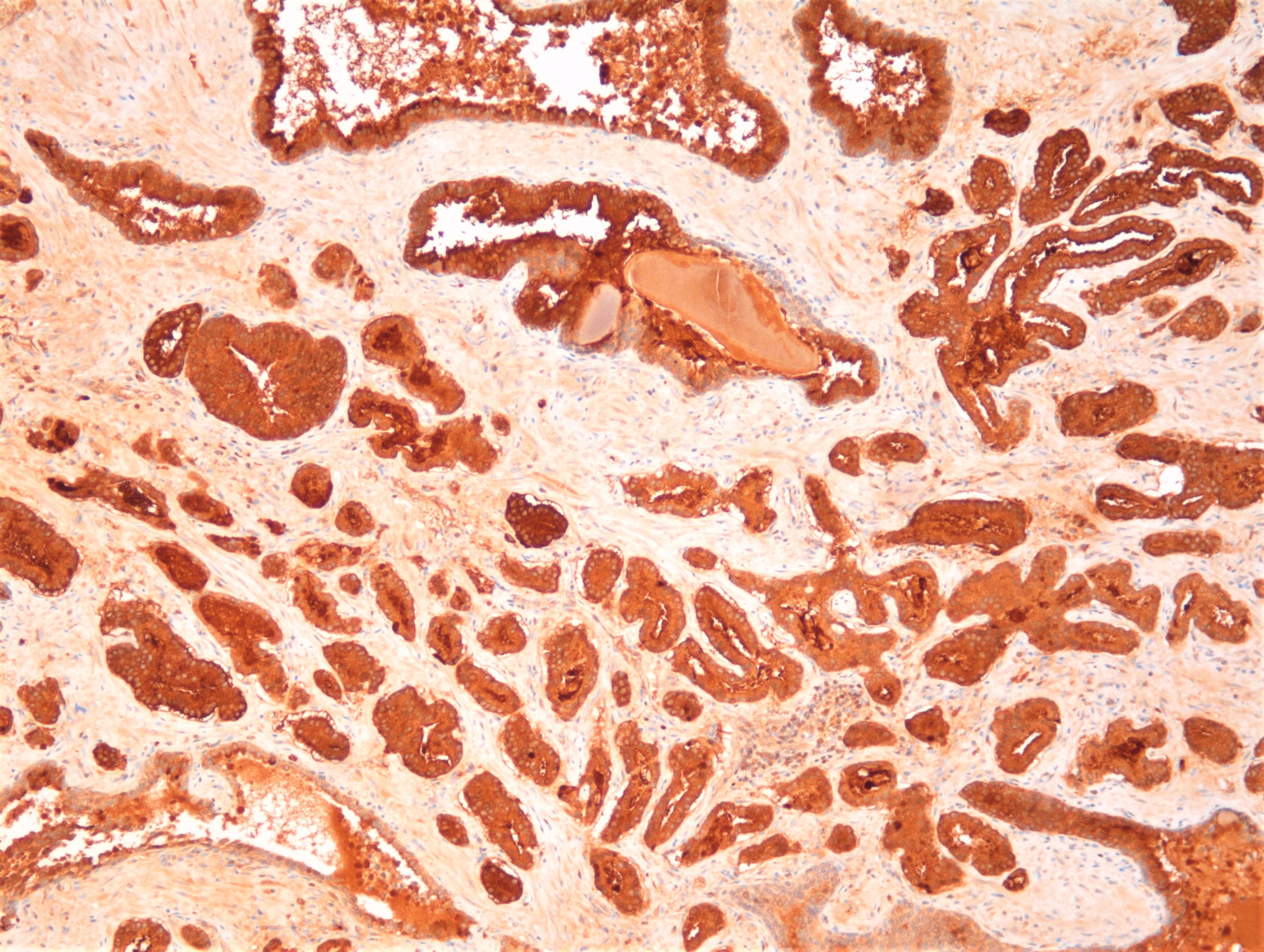
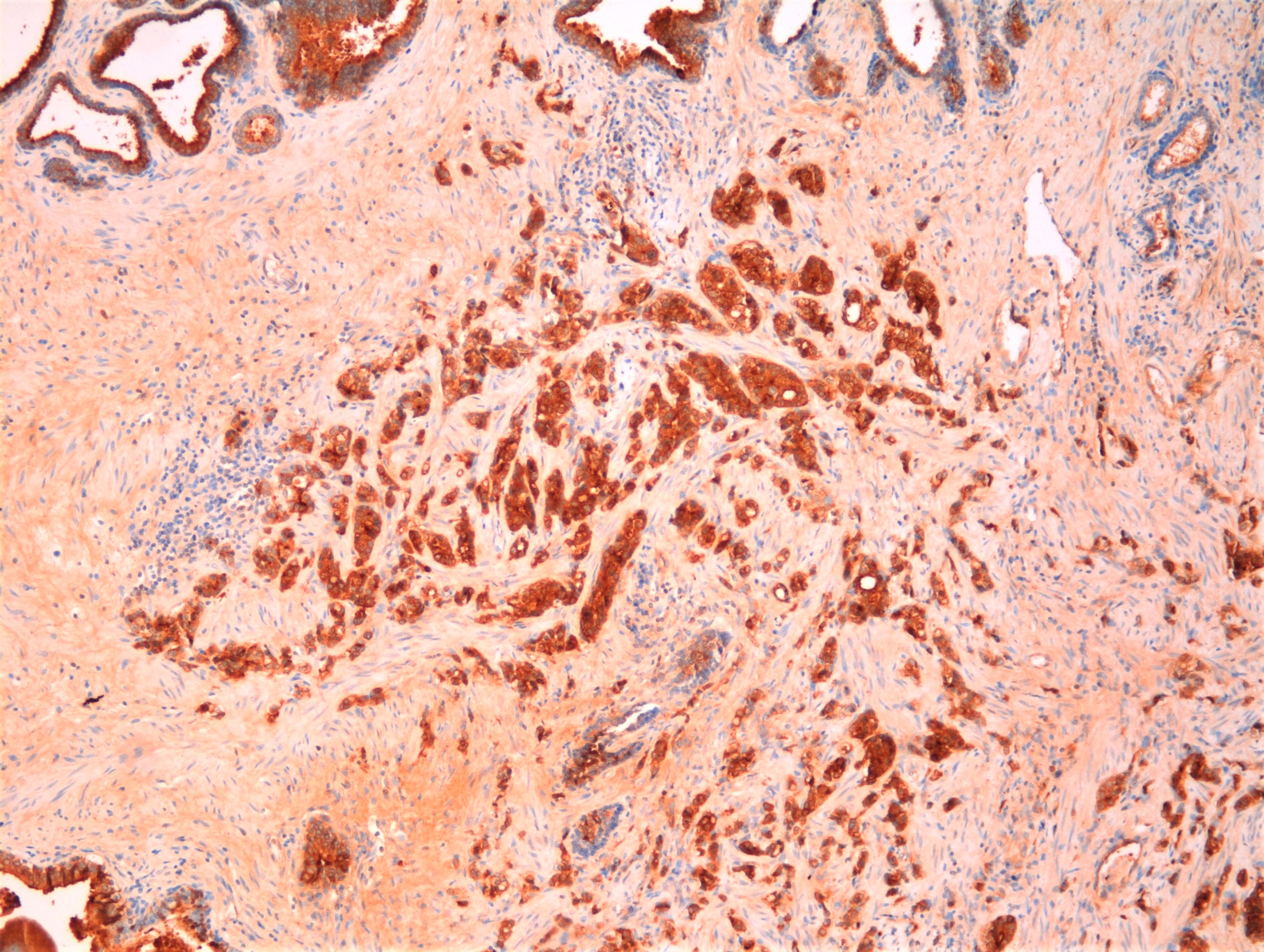
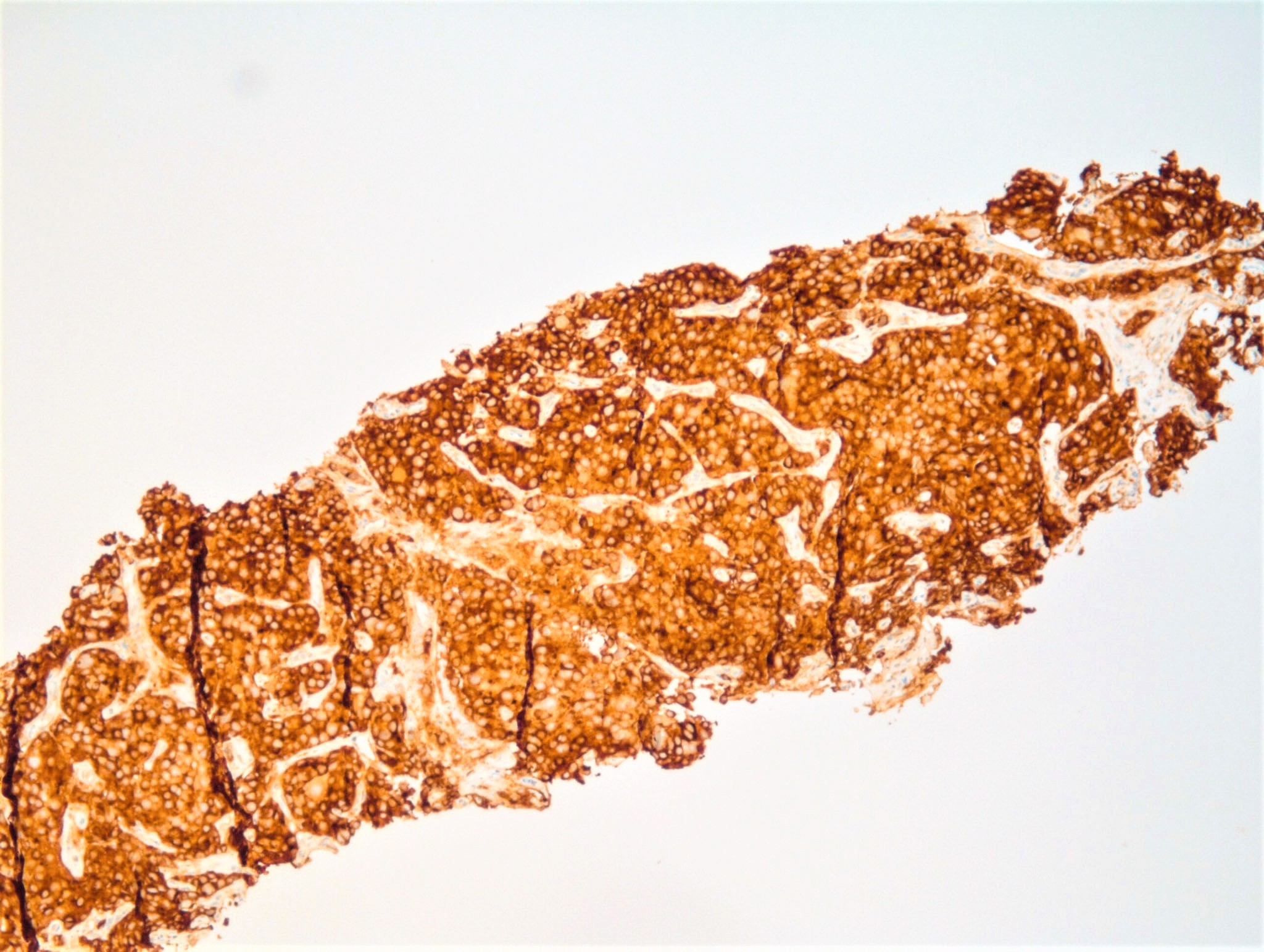
- Cytoplasmic staining (positive expression is strong, granular, diffuse)
Uses by pathologists
- Detected in benign and malignant prostate tissue
- Identifies prostatic origin of most metastatic tumors
- Differentiates between prostatic and urothelial carcinoma
- More sensitive and specific than PSAP
- Nonprostate tumors usually negative or weak for PSA
- Can be used in combination with NKX3.1 to increase sensitivity (Int J Mol Sci 2017;18:1151)
- Identifies prostatic origin of most metastatic tumors
- Other uses
- Distinguish mesonephric remnants (PAX8+, PSA-) (Mod Pathol 2003;16:630)
Prognostic factors
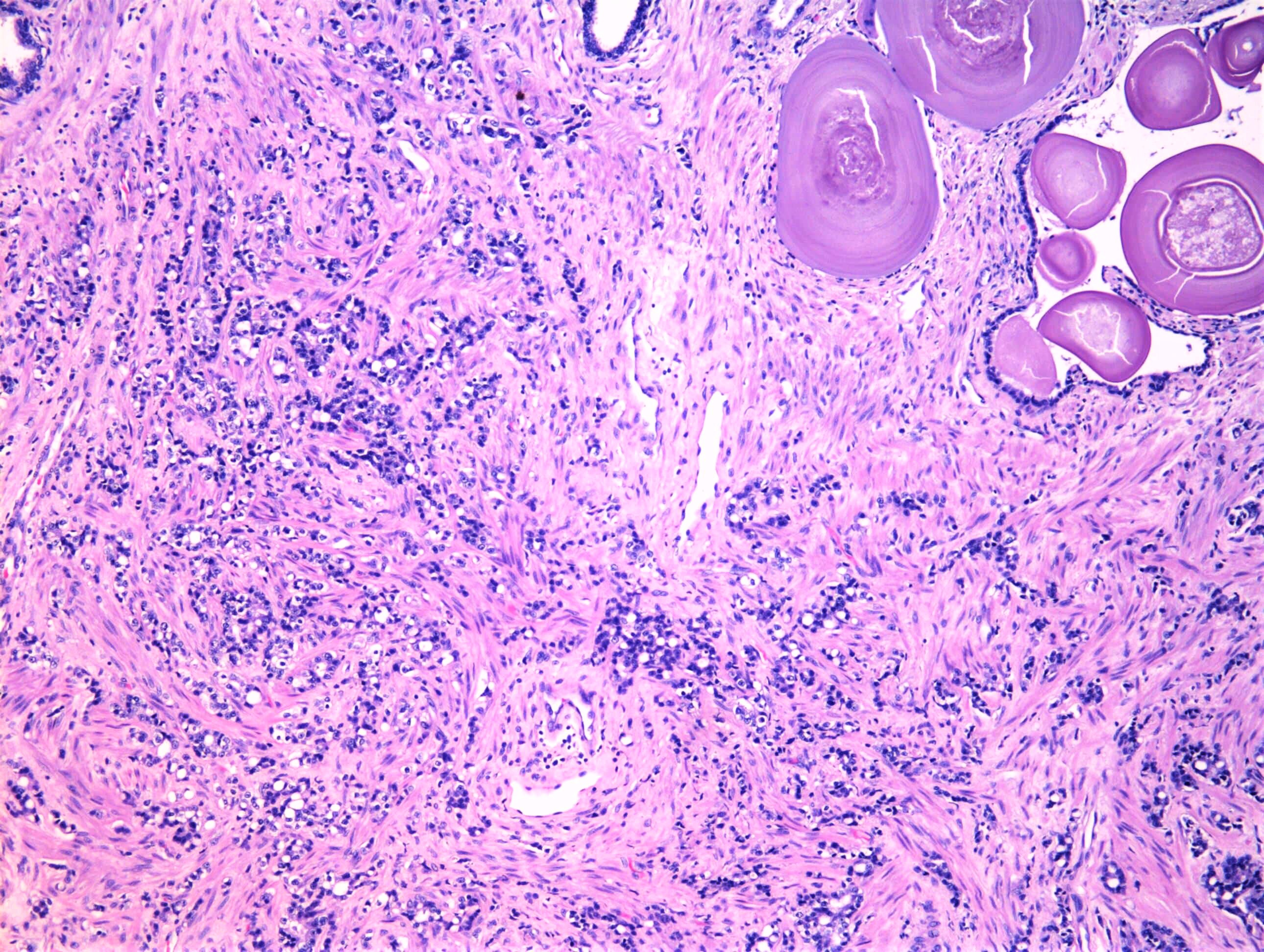
- Reduced or negative expression in poorly differentiated prostate cancers linked to unfavorable tumor phenotype and poor prognosis (Oncotarget 2019;52:5439)
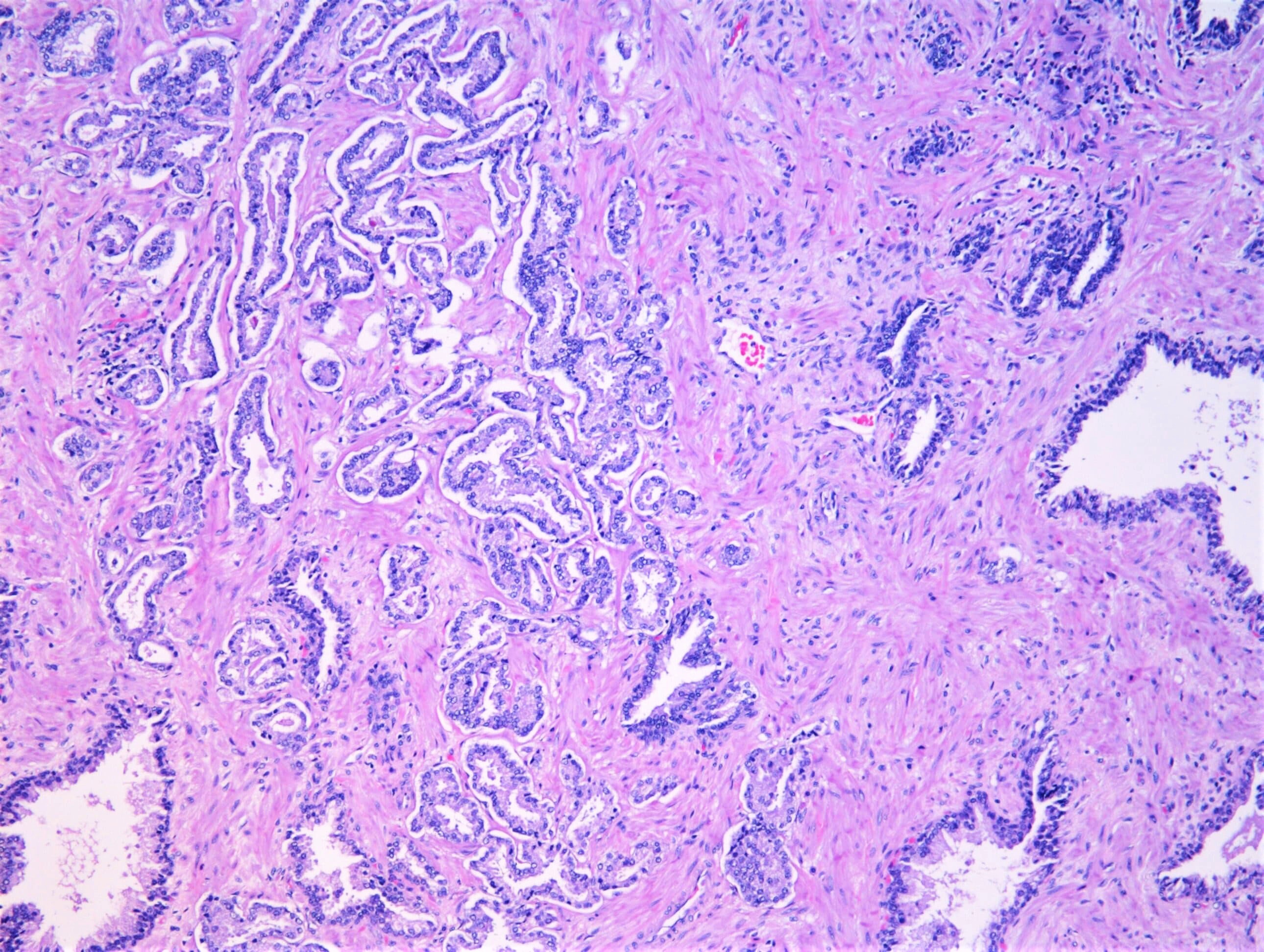
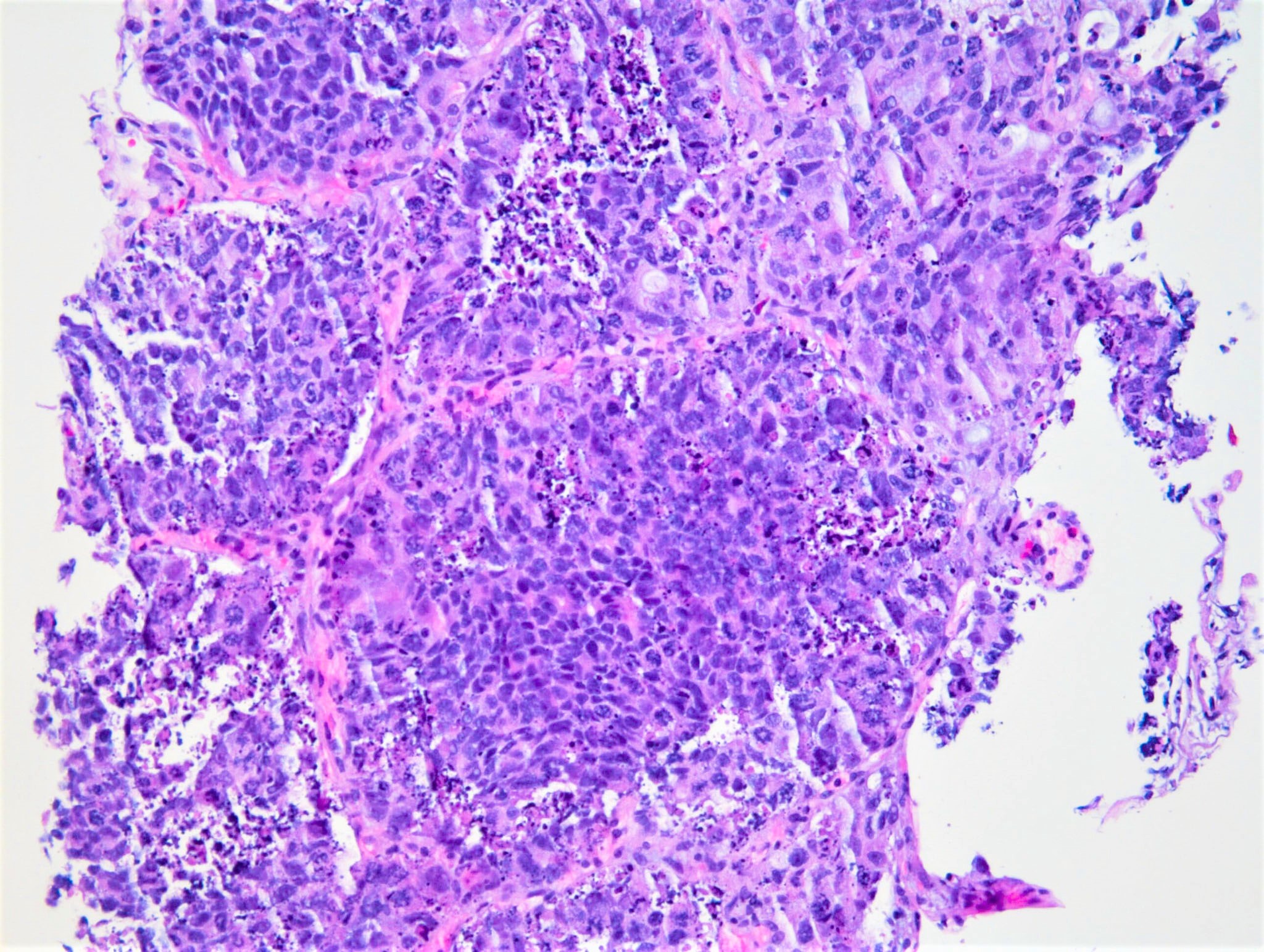
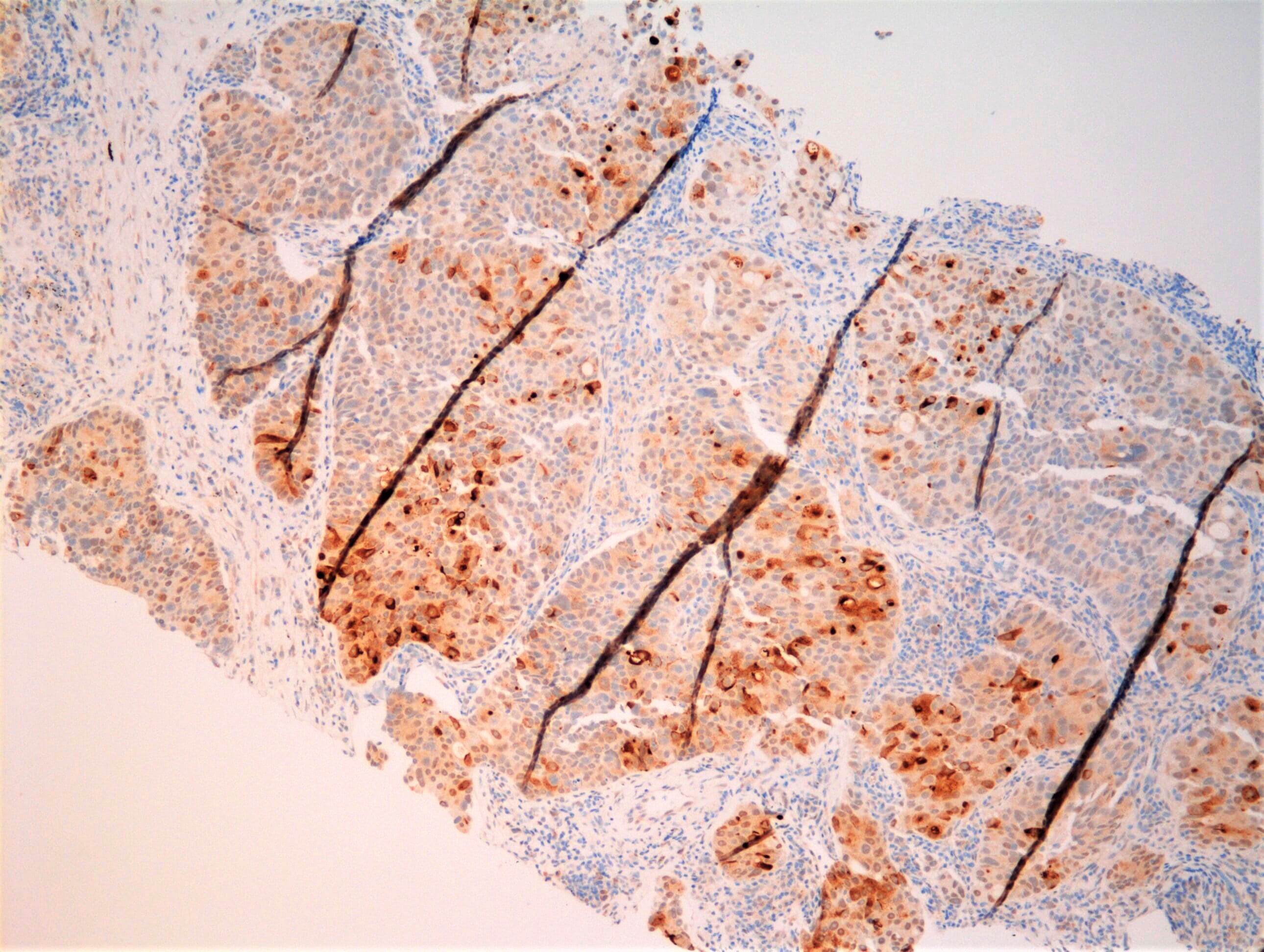
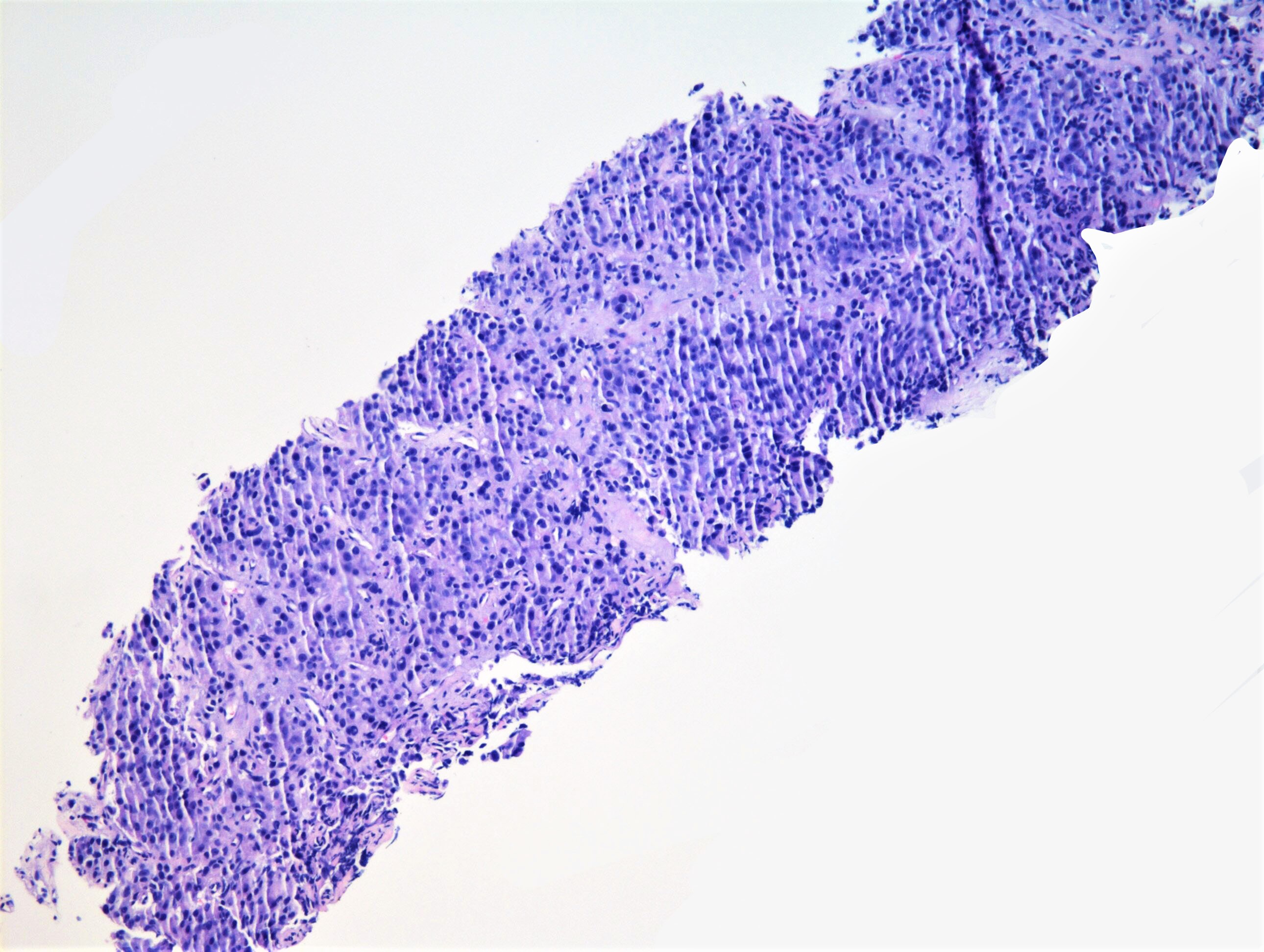
Microscopic (histologic) images
Positive staining - normal
- Prostatic secretory epithelium
- Weak positive staining in salivary ductal cells (Pathobiology 2020;87:30)
Positive staining - disease
- Prostatic adenocarcinoma
- Less sensitive in poorly differentiated tumors (Am J Surg Pathol 2007;31:1246, Histopathology 2005;47:1)
- In rare cases, can be negative after androgen deprivation treatment (castrate resistant tumors) (Pathology International 2008;58:687)
- Other cancers of prostate
- Can be either negative or positive in the carcinoma elements of prostatic carcinosarcoma (Am J Clin Pathol 1989;92:131)
- Focal in small cell carcinoma of the prostate (Nat Rev Urol 2014;11:213)
- Variable immunoreactivity in salivary gland tumors
- Salivary duct carcinomas (~ 57%) (Am J Surg Pathol 2000;24:579)
- Parotid neoplasms: oncocytomas, pleomorphic adenomas (including metastatic versions) (Diagn Cytopathol 1998;19:221, J Craniomaxillofac Surg. 2014;42:1562, Am J Surg Pathol 2000;24:579)
- Variable immunoreactivity in breast carcinomas (Pathol Res Pract 1996;192:233)
- Serum PSA may reflect androgen receptor activity in postmenopausal breast cancer (BMC Cancer 2019;19:1021)
Negative staining
- Normal prostate: basal cells, urothelium, stromal cells
- Prostate cancers
- Basal cell carcinoma (Human Pathol 2012;43:313)
- Sarcomatous elements of prostatic carcinosarcoma (Am J Clin Pathol 1989;92:131)
- Squamous cell carcinoma (Am J Clin Pathol 1988;90:597)
- Melanoma
- Hematopoietic malignancies
- Genitourinary cancers: carcinomas of urothelial origin, renal cell carcinoma, mesenchymal tumors of kidney, testicular tumors
- Recommended to first pair PSA with GATA3 (or HMWCK and p63) to differentiate between prostatic versus urothelial origin; prostate positive for PSA versus urothelial positive for GATA3 (Am J Surg Pathol 2014;38:1017)
Board review style question #1
A 67 year old man is found to have a mass involving the bladder and the prostate. Which stain combination would be most consistent with tumor originating from the prostate?
- PSA negative, CDX2 positive
- PSA negative, PAX8 positive, CAIX positive
- PSA negative, TTF1 positive, p40 negative
- PSA positive, GATA3 negative, p63 negative
- PSA positive, PAX8 negative, GATA3 positive
Board review style answer #1
D. PSA positive, GATA3 negative, p63 negative
A. PSA negative, CDX2 positive would be consistent with a colorectal adenocarcinoma or adenocarcinoma of the urinary bladder, intestinal type.
B. PSA negative, PAX8 positive, CAIX positive would be consistent with a clear cell renal cell carcinoma.
C. PSA negative, TTF1 positive, p40 negative would be consistent with an adenocarcinoma of lung origin.
E. PSA positive, PAX8 negative, GATA3 positive is seen in some salivary duct and breast carcinomas.
Comment Here
Reference: Prostate specific antigen (PSA)
A. PSA negative, CDX2 positive would be consistent with a colorectal adenocarcinoma or adenocarcinoma of the urinary bladder, intestinal type.
B. PSA negative, PAX8 positive, CAIX positive would be consistent with a clear cell renal cell carcinoma.
C. PSA negative, TTF1 positive, p40 negative would be consistent with an adenocarcinoma of lung origin.
E. PSA positive, PAX8 negative, GATA3 positive is seen in some salivary duct and breast carcinomas.
Comment Here
Reference: Prostate specific antigen (PSA)