Table of Contents
Definition / general | Essential features | Pathophysiology | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Cytology images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Molecular / cytogenetics images | Board review style question #1 | Board review style answer #1Cite this page: Ly TY, Walsh NM. MCPyV (CM2B4). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsMCPyV.html. Accessed April 3rd, 2025.
Definition / general
- CM2B4 is a monoclonal antibody that detects Merkel cell polyomavirus (MCPyV) large T antigen expression in Merkel cell carcinoma (MCC)
Essential features
- Merkel cell polyomavirus (MCPyV) is causally linked to the majority of Merkel cell carcinomas (MCC) (up to ~80%) (Eur J Cancer 2017;71:53, J Invest Dermatol 2017;137:819)
- CM2B4 is a monoclonal antibody that detects Merkel cell polyomavirus (MCPyV) large T antigen expression in MCC
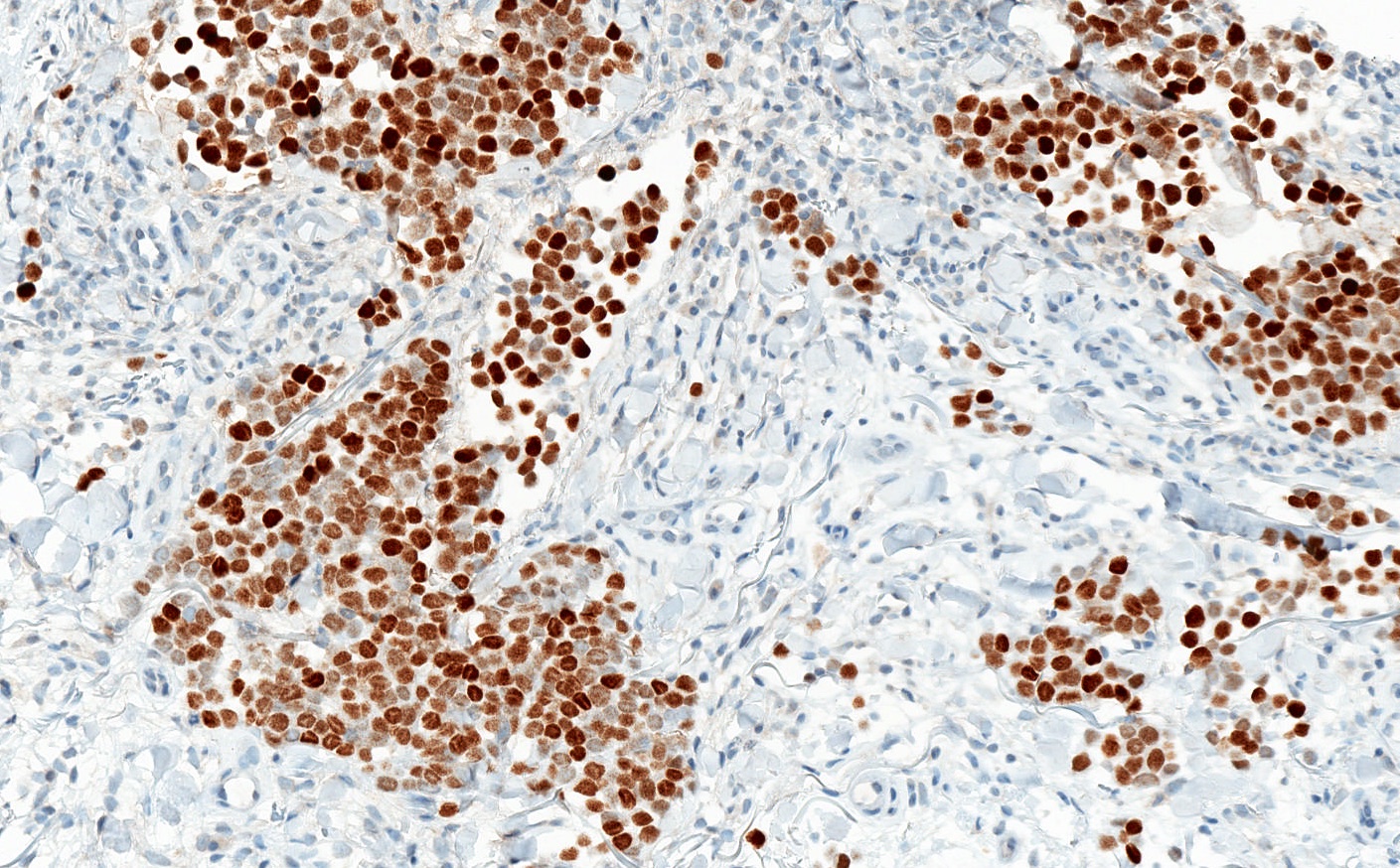
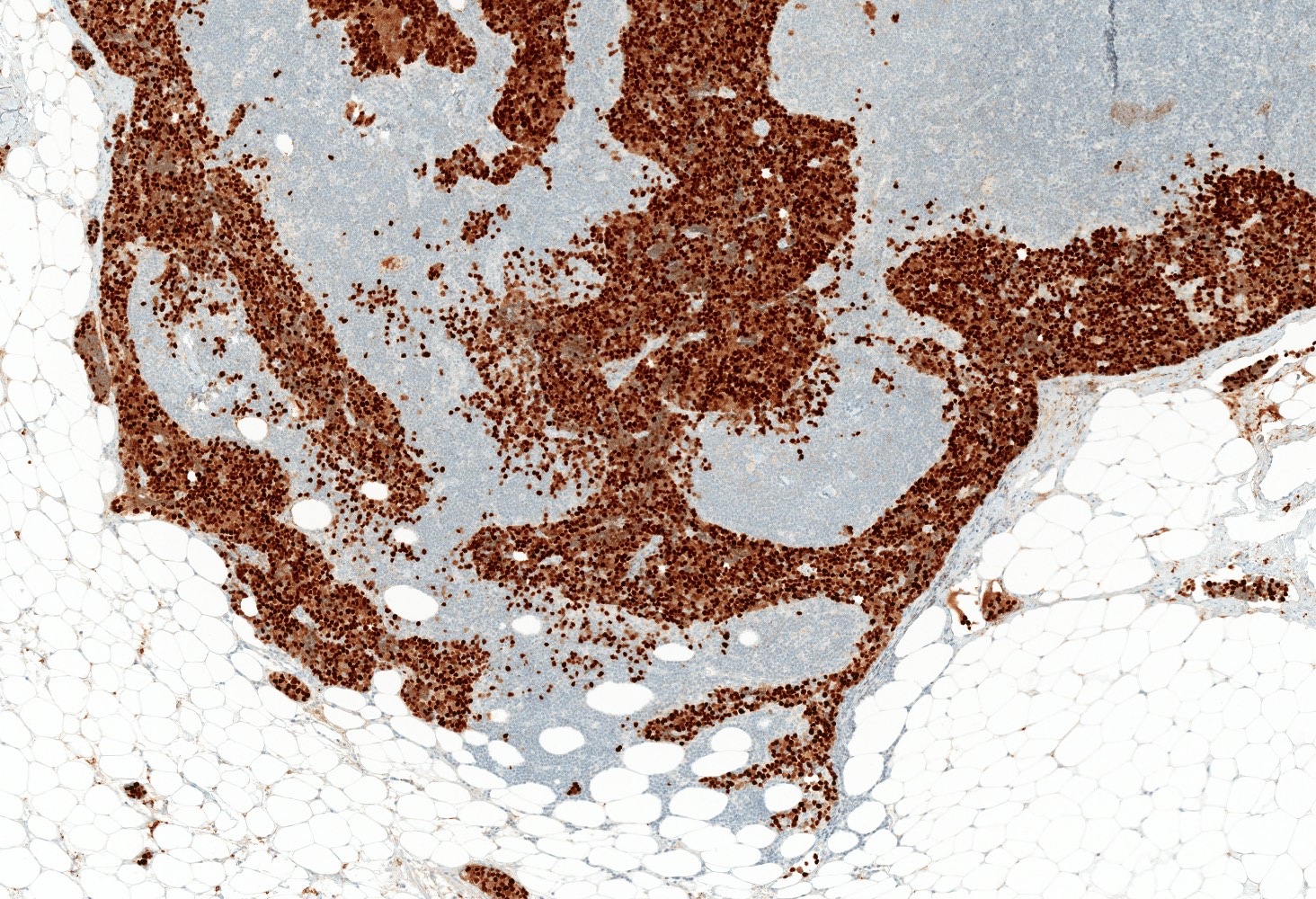
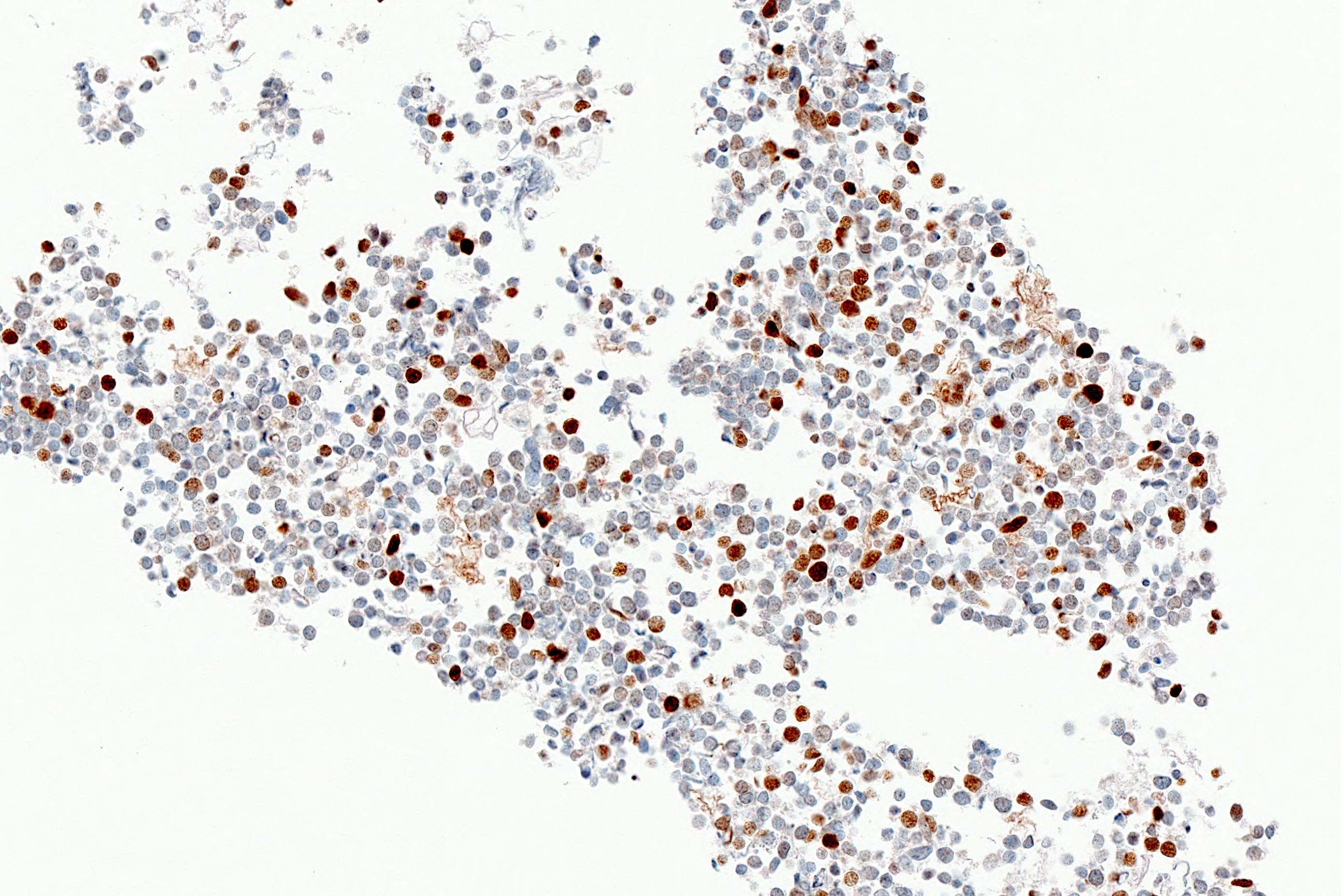
- Nuclear pattern of CM2B4 immunoreactivity in MCC indicates MCPyV large T antigen expression (virus positivity)
- Immunohistochemical identification of MCPyV is practical, sensitive and specific compared to PCR (J Clin Invest 2012;122:4645, Hum Pathol 2012;43:557, J Med Virol 2014;86:1813, Diagn Pathol 2014;9:65)
- Emerging evidence suggests MCPyV status is prognostically significant as MCPyV positive MCC is associated with better prognosis (J Invest Dermatol 2017;137:819, Mod Pathol 2019;32:1605)
Pathophysiology
- Merkel cell polyomavirus (MCPyV) is a small (~5400 bp) double stranded DNA virus
- Causally linked to up to 80% of Merkel cell carcinomas (MCC) (Eur J Cancer 2017;71:53, J Invest Dermatol 2017;137:819)
- Remaining MCCs develop via UV induced oncogenesis (Eur J Cancer 2017;71:53)
- Ubiquitous virus and is the only known oncogenic human polyomavirus (Nat Rev Clin Oncol 2018;15:763)
- Asymptomatic infection, typically in early life
- ~40 - 80% seropositivity in adults (J Clin Oncol 2011;29:1612, Int J Cancer 2009;125:1250)
- High seroprevalence and high antibody titers in elderly individuals suggest virus reactivation in late adulthood (Clin Vaccine Immunol 2013;20:363, Int J Cancer 2009;125:1250)
- Skin is a major site for infection (Nat Rev Clin Oncol 2018;15:763)
- MCPyV mediated oncogenic transformation requires viral integration into host genome and a truncating mutation of large T antigen (LT)
- Truncated LT binds Rb, promoting cell cycle progression (Science 2008;319:1096, Proc Natl Acad Sci U S A 2008;105:16272, Nat Rev Clin Oncol 2018;15:763)
- Other viral oncoproteins (e.g. small T antigen) and host factors (e.g. immune suppression) and somatic mutations also play a role in tumor development (J Clin Invest 2011;121:3623, Eur J Cancer 2017;71:53)
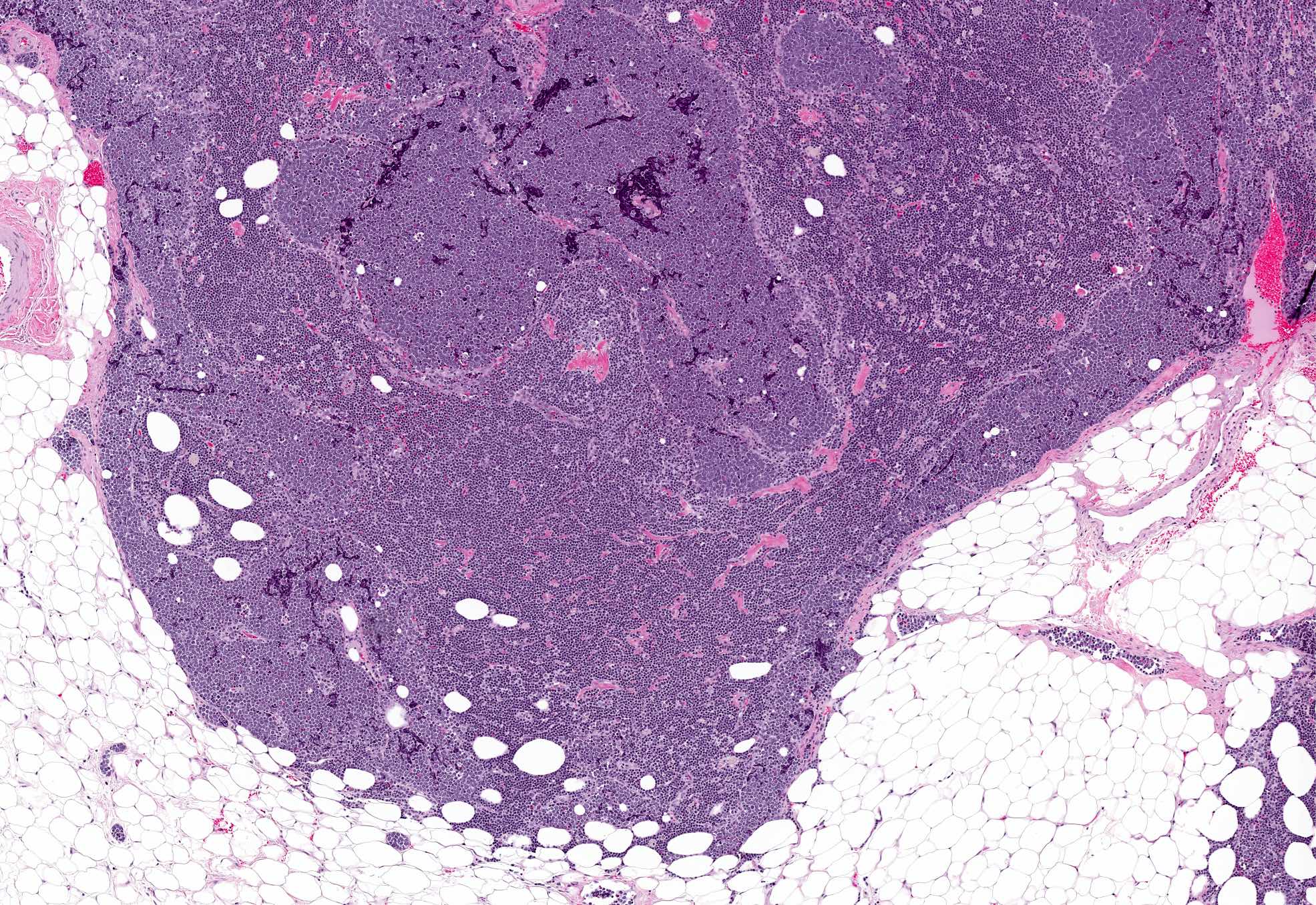
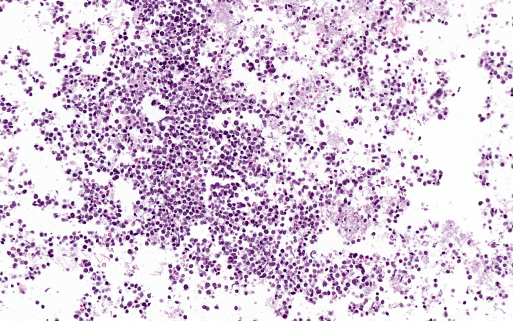
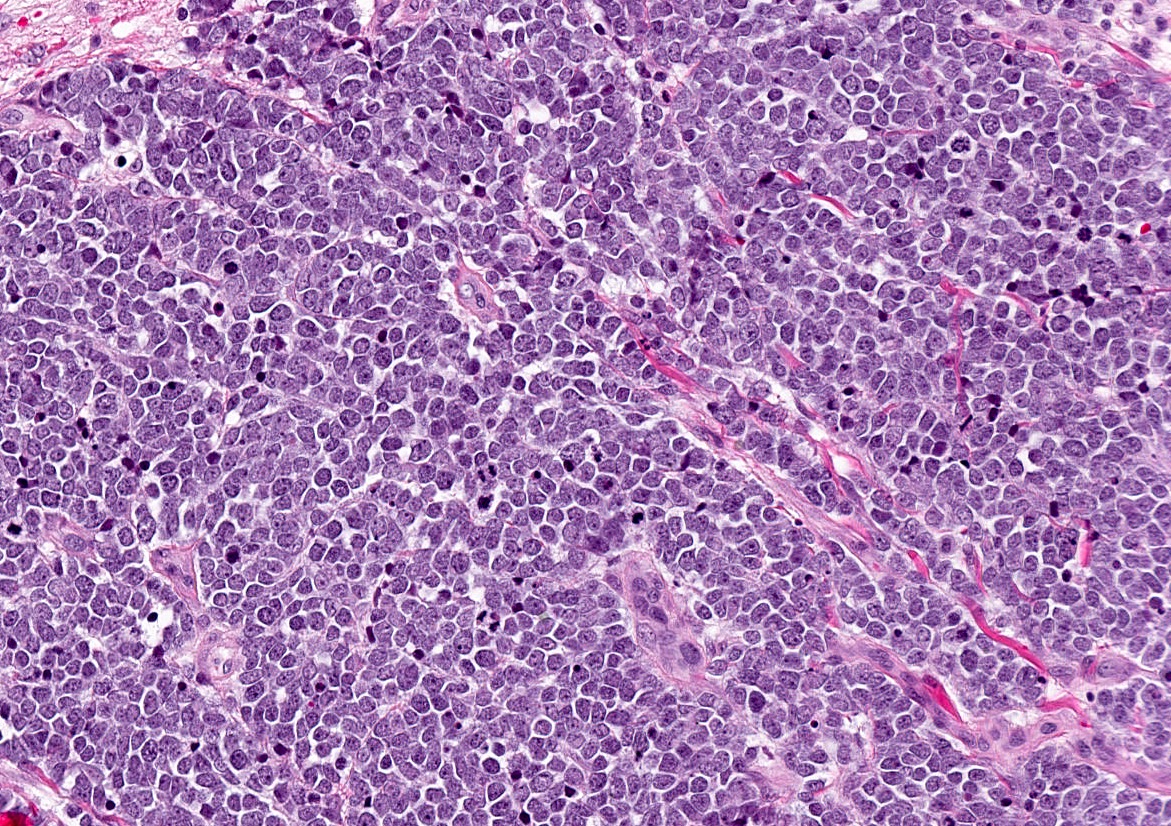
- Majority of MCC display pure neuroendocrine morphology (termed pure MCC) with MCPyV positive and MCPyV negative subtypes (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378, Hum Pathol 2001;32:680)
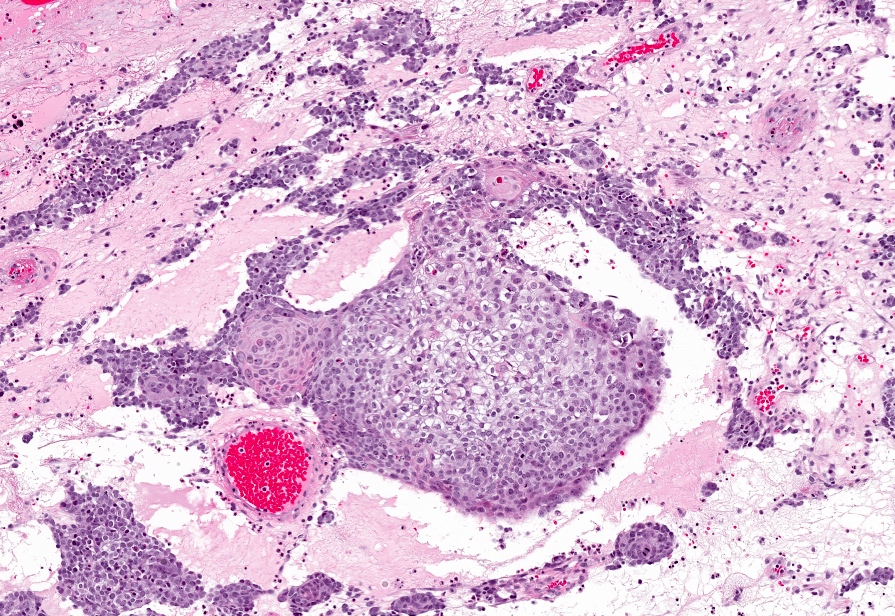
- A smaller proportion of MCC are morphologically heterogeneous (termed combined MCC) and feature typical neuroendocrine elements intimately associated with other cutaneous neoplasms (most commonly in situ or invasive squamous cell carcinoma) or exhibit divergent differentiation (e.g. squamous or sarcomoid) (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378, Mod Pathol 2015;28:1023, Hum Pathol 2001;32:680)
- Reported incidence is variable, 5 - 41% of all MCC (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378, Hum Pathol 2001;32:680)
- Uniformly MCPyV negative (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378, Mod Pathol 2015;28:1023)
- CM2B4 is a monoclonal antibody developed against an epitope in exon 2 of the MCPyV T antigen (Int J Cancer 2009;125:1243)
- Highly specific for wildtype LT, truncated (tumor associated) LT and 57kT (an isoform translated from multiply spliced mRNA)
- Does not bind viral small T (ST) antigen
- Does not bind other common polyomaviruses (e.g. JC virus, BK virus)
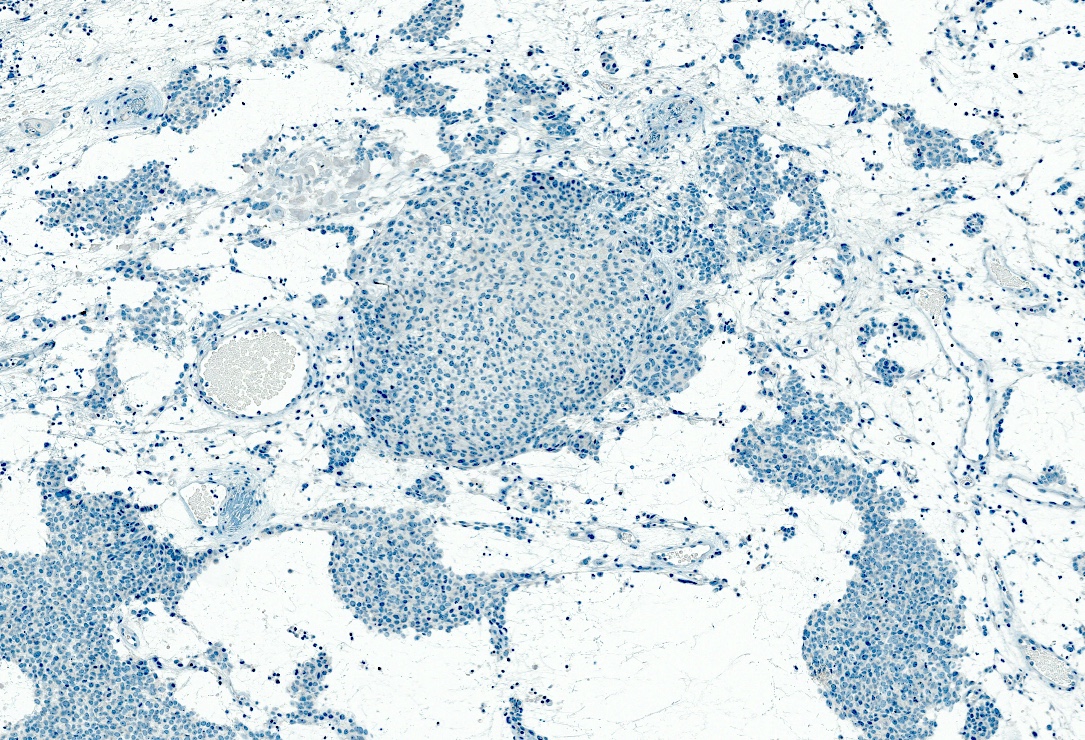
Interpretation
- Nuclear pattern of immunoreactivity
- Any degree of nuclear staining in tumor cells is considered positive
- Intratumoral staining may be heterogeneous (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378)
Uses by pathologists
- Identify MCPyV positive MCC (better prognosis) (Int J Cancer 2009;125:1243)
- Differentiate MCC from extracutaneous (e.g. lung, gastrointestinal) neuroendocrine carcinomas (Am J Surg Pathol 2009;33:1378, Hum Pathol 2012;43:557)
- Differentiate MCC from potential histologic mimics in the skin (Hum Pathol 2012;43:557, J Am Acad Dermatol 2010;63:400, Int J Cancer 2009;125:1243)
- E.g. basal cell carcinoma, squamous cell carcinoma, cutaneous adnexal tumor, metastatic extracutaneous neuroendocrine carcinoma, lymphoma / leukemia, melanoma, etc.
- Aid interpretation of immunohistochemical results
- MCPyV positive MCC frequently shows the classical MCC immunophenotype:
- CK20+, neurofilament+, TTF1-, CK7- (Hum Pathol 2018;82:232)
- MCPyV negative MCC, including combined MCC, can be diagnostically challenging due to potential aberrant immunophenotype:
- CK20-, neurofilament-, TTF1+, CK7+ (Hum Pathol 2018;82:232)
- Important to recognize this scenario does not exclude MCC and can be expected for a subset of MCPyV negative MCC
- MCPyV positive MCC frequently shows the classical MCC immunophenotype:
Prognostic factors
- MCC mortality rate is 33 - 46% (Eur J Cancer 2017;71:53)
- MCPyV positive MCC appears to have a better prognosis than MCPyV negative MCC (J Invest Dermatol 2017;137:819, Mod Pathol 2019;32:1605)
- MCPyV status does not influence response to immune checkpoint blockade therapy targeting the PDL1 / PD1 pathway in advanced MCC (Lancet Oncol 2016;17:1374, N Engl J Med 2016;374:2542)
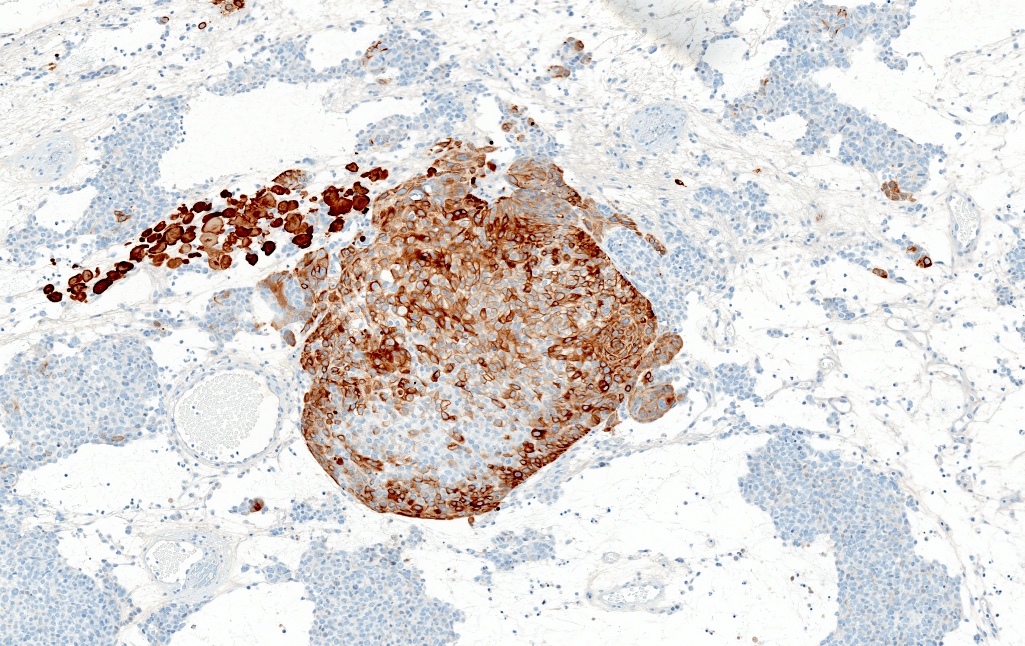
Microscopic (histologic) images
Positive staining - normal
- None known (Int J Cancer 2009;125:1243, Hum Pathol 2012;43:557)
Positive staining - disease
- Reported sensitivity 77 - 94% and specificity 94 - 100% compared to PCR (Int J Cancer 2009;125:1243, J Invest Dermatol 2017;137:819, J Clin Invest 2012;122:4645, Hum Pathol 2013;44:1912, Am J Surg Pathol 2009;33:1378, Diagn Pathol 2014;9:65)
- Positive in 63 - 79% of MCC with purely neuroendocrine morphology (pure MCC, MCPyV positive subtype) (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378, Hum Pathol 2013;44:1912)
- Positive in primary and metastatic MCPyV positive MCC, with reported 100% concordant staining between corresponding primary and metastatic tumors (Hum Pathol 2012;43:557, Hum Pathol 2015;46:443, Am J Surg Pathol 2009;33:1378, J Am Acad Dermatol 2010;63:400)
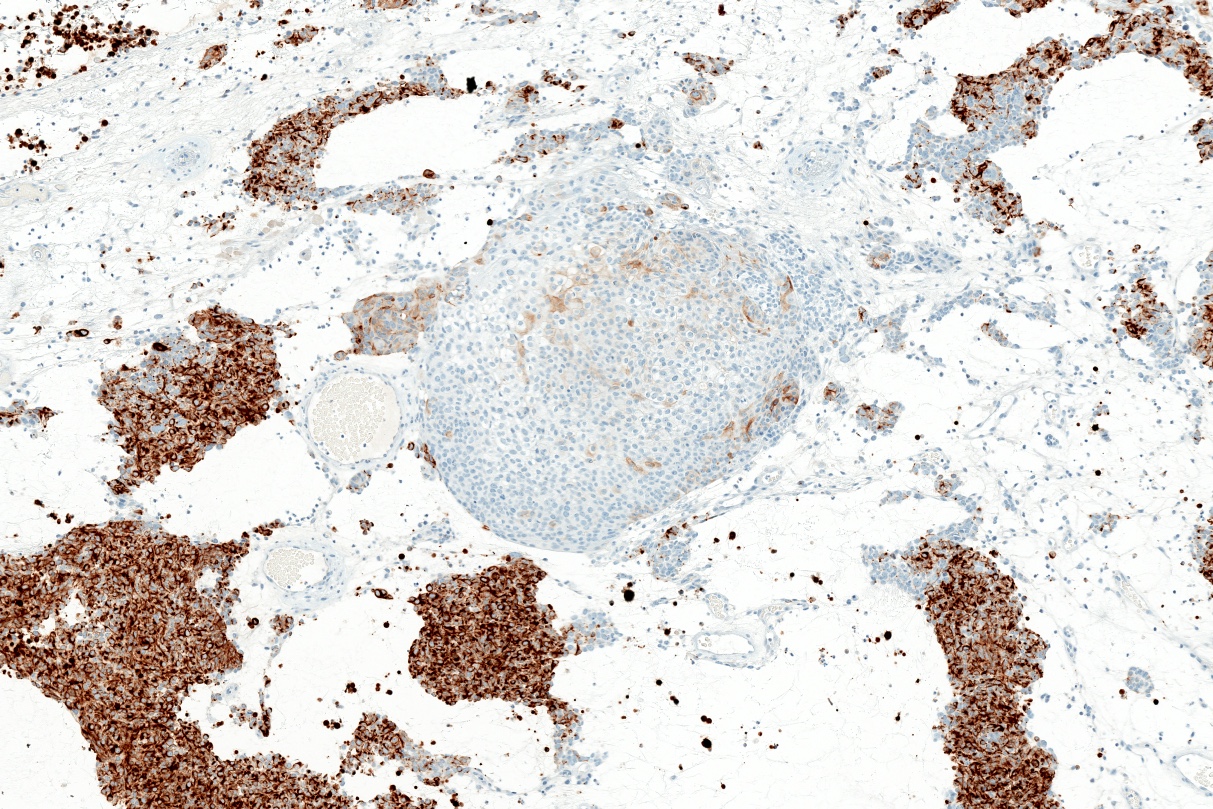
Negative staining
- CM2B4 negative in nontumor cells, including in skin and lymphoid tissues (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378)
- Negative in 21 - 37% of MCC with purely neuroendocrine morphology (pure MCC, MCPyV negative subtype) (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378)
- Negative in combined MCCs (which are uniformly MCPyV negative) (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378)
- Negative in tumors commonly in the differential diagnosis with MCC:
- Cutaneous lesions (basal cell carcinoma, squamous cell carcinoma, melanoma, etc.) (Hum Pathol 2012;43:557, J Am Acad Dermatol 2010;63:400, J Invest Dermatol 2017;137:819)
- Pulmonary small cell carcinoma and large cell neuroendocrine carcinoma (Hum Pathol 2012;43:557, Am J Surg Pathol 2009;33:1378)
- Gastrointestinal neuroendocrine tumors (Hum Pathol 2012;43:557)
- Hematolymphoid malignancies (B cell, T cell and myeloid) (Int J Cancer 2009;125:1243)
Molecular / cytogenetics description
- Genetic profiles for MCPyV positive and MCPyV negative MCCs are distinct
- MCPyV negative MCCs harbor TP53 and RB1 gene mutations, UV signature mutations and overall higher mutational burden (Oncotarget 2016;7:3403, Cancer Res 2015;75:5228)
Board review style question #1
Which of the following describes the oncogenic virus causally associated with the majority of Merkel cell carcinomas (shown above)?
- Herpesvirus with presence corresponding to cytoplasmic IHC expression
- Herpesvirus with presence corresponding to nuclear IHC expression
- Papillomavirus with presence corresponding to membranous IHC expression
- Papillomavirus with presence corresponding to nuclear IHC expression
- Polyomavirus with presence corresponding to dot-like paranuclear IHC expression
- Polyomavirus with presence corresponding to nuclear IHC expression
Board review style answer #1
F. Merkel cell polyomavirus (MCPyV) is a novel human polyomavirus causally associated with the majority of Merkel cell carcinomas (MCC) (up to ~80%). A nuclear pattern of CM2B4 immunoreactivity in MCC indicates MCPyV large T antigen expression (virus positivity).
Comment Here
Reference: MCPyV (CM2B4)
Comment Here
Reference: MCPyV (CM2B4)