Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Virtual slides | Cytology images | Positive staining - normal | Positive staining - disease | Negative staining | Sample pathology report | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Chen-Yost HI, Antic T. Epithelial membrane antigen (EMA). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsEMA.html. Accessed March 30th, 2025.
Definition / general
- Transmembrane protein normally expressed in glandular or luminal epithelial cells and hematopoietic cells and absent in skin epithelium and mesenchymal cells (J Mammary Gland Biol Neoplasia 2001;6:339, Cell Immunol 2000;201:83)
Essential features
- EMA (aka MUC1) a glycoprotein that provides barrier function
- Overexpression is common in malignancies and leads to tumorigenesis
- Immunohistochemical stain is positive in most carcinomas, often used alongside other cytokeratin stains
- For noncarcinomas, EMA is useful to distinguish meningioma, some hematopoietic tumors and malignant mesothelioma
Terminology
- Other names: CD227, MUC1, CA15-3, episialin (Cell Mol Life Sci 2015;72:4475)
Pathophysiology
- Normal
- Localized to the apical membranes and provides barrier function (Nat Rev Cancer 2009;9:874)
- Blocks cell to cell and cell to extracellular matrix interactions
- Inhibits formation of E-cadherin / beta catenin complex (Ann Pathol 2006;26:257)
- Localized to the apical membranes and provides barrier function (Nat Rev Cancer 2009;9:874)
- Abnormal (Trends Mol Med 2014;20:332)
- Overexpressed and loses cell polarity
- Redistributed in cell surface and cytoplasm
- Abnormal distribution leads to expression of PDGFA
- Promotes proliferation and invasion of cells
- Interacts with and stabilizes HIF1α
- Enhances glucose uptake genes
- Induces expression of proangiogenic factors (CTGF, PDGFB, VEGFA)
- Upregulates expression of inducers that lead to destabilization of adherens junctions and leads to cytoskeleton rearrangements (Oncogene 2011;30:1449)
- Facilitates basement membrane invasion
- Overexpressed and loses cell polarity
Clinical features
- Highly expressed by most carcinomas (especially adenocarcinomas) and hematologic cancers (Trends Mol Med 2014;20:332)
- Soluble forms shed into the bloodstream are used in commercial serum tumor marker assays for breast cancer (CA15-3) (Clin Chim Acta 2010;411:1869)
Interpretation
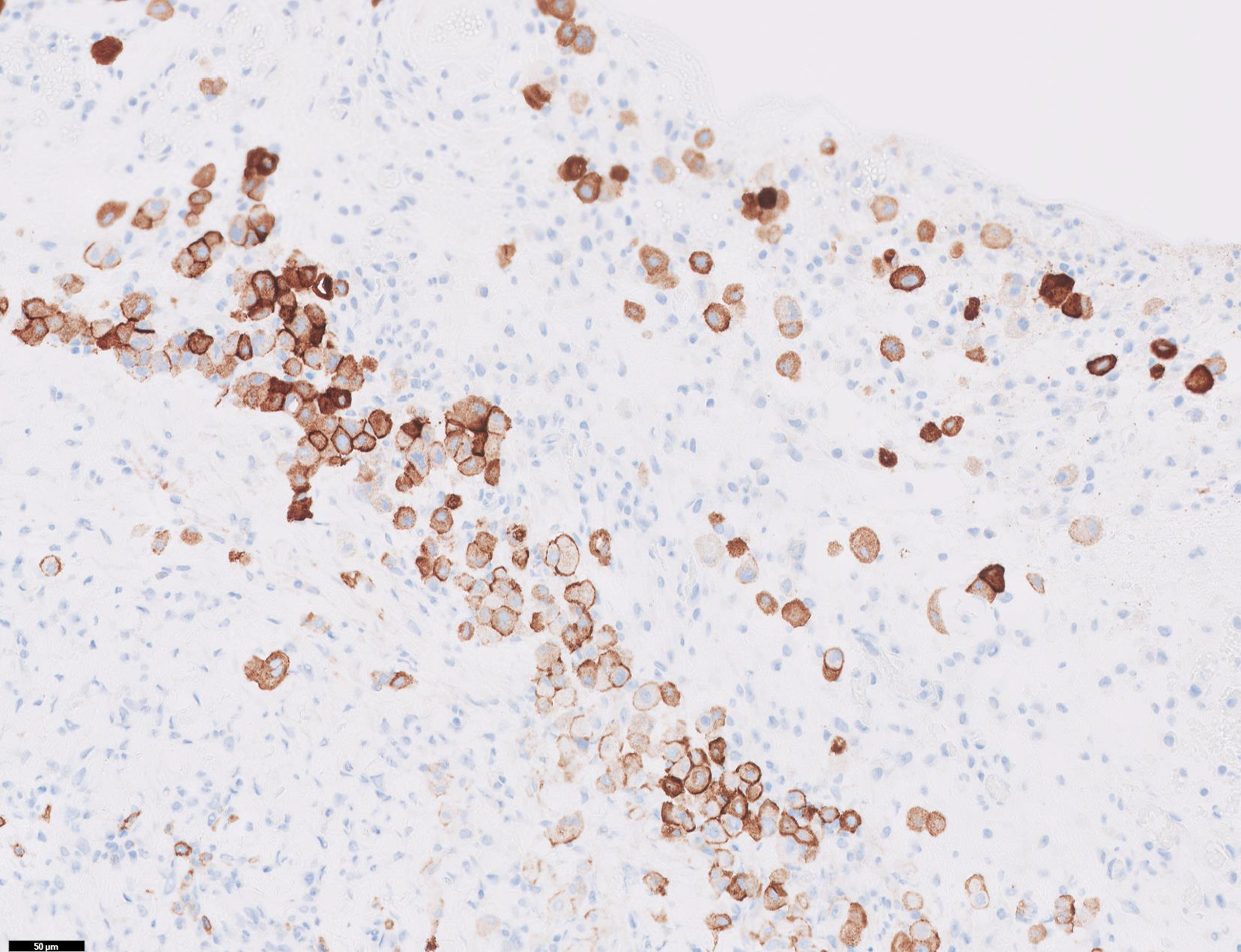
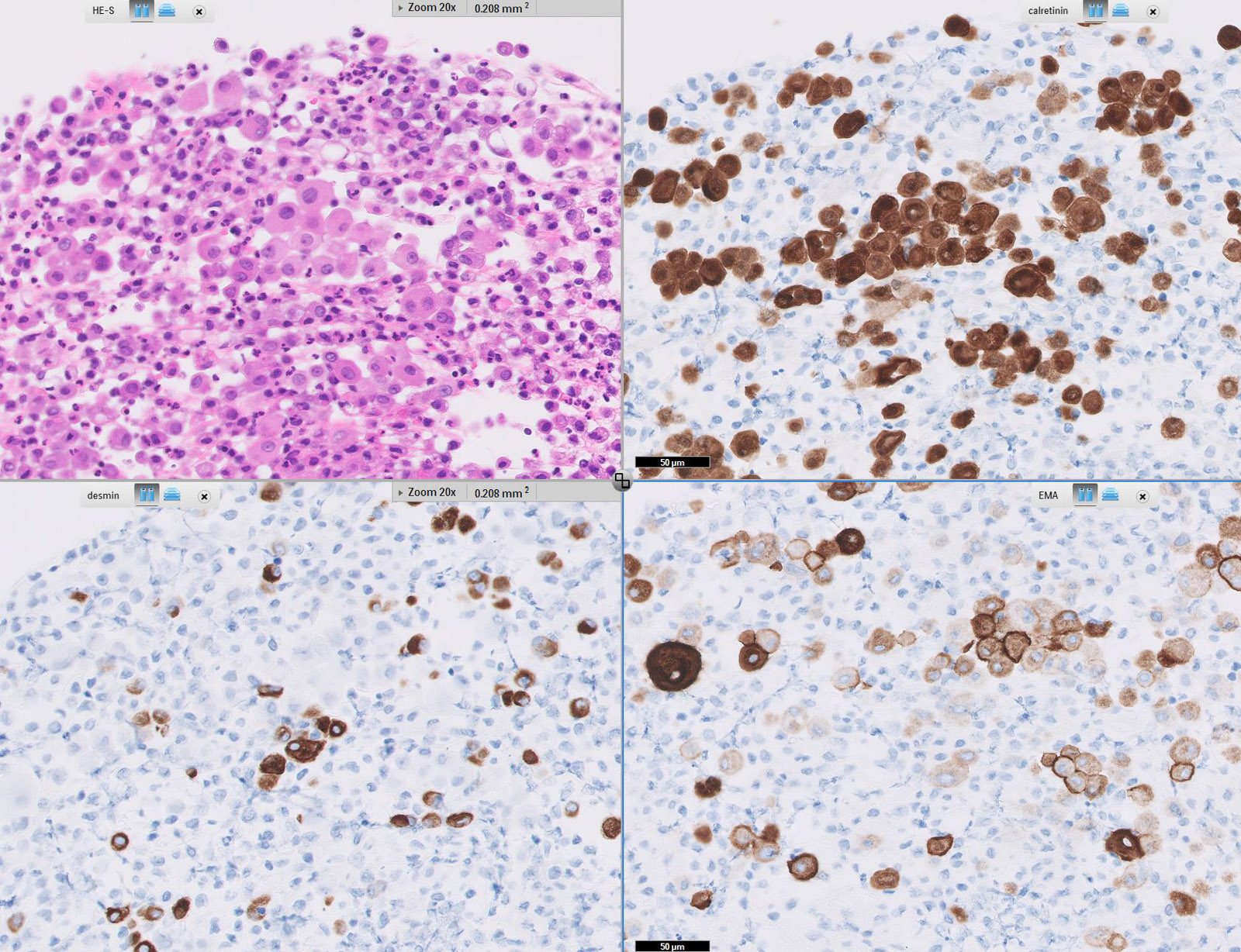
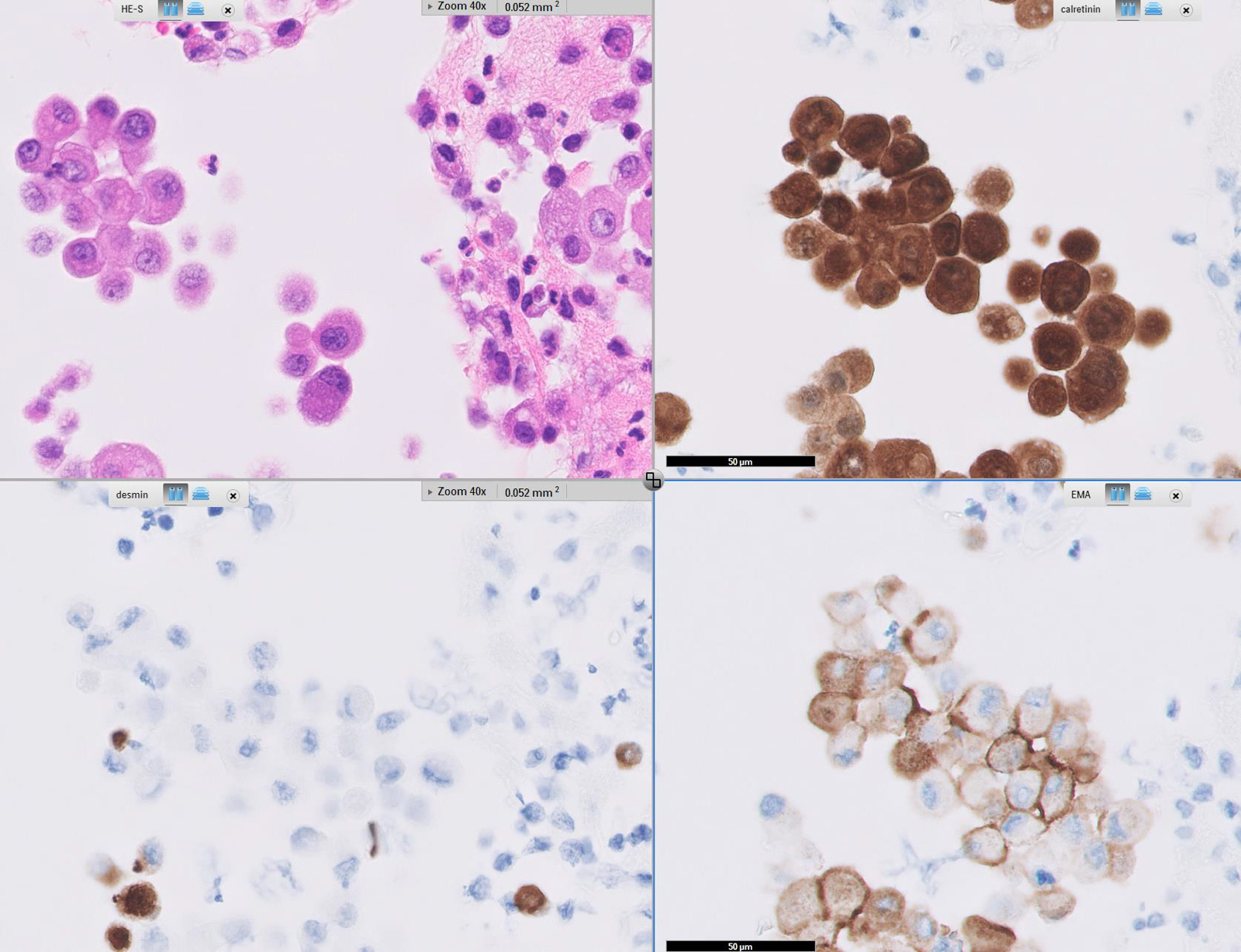
- Membranous staining: mesothelioma cells (Cancer Cytopathol 2010;118:90)
- Cytoplasmic staining: carcinoma cells (Hum Pathol 1985;16:929)
- Apical luminal membrane staining can also be observed
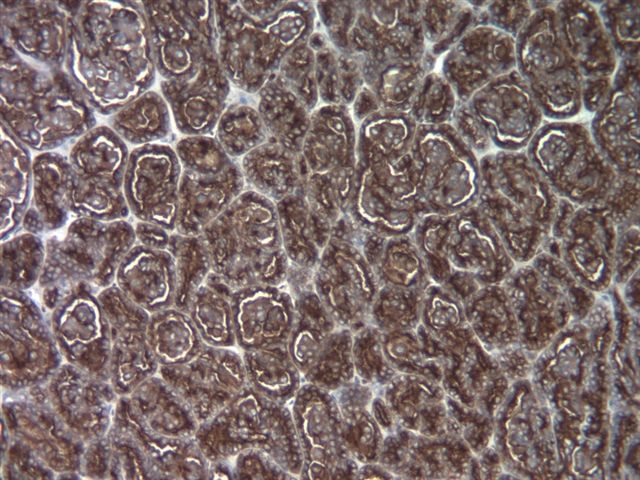
- Dot-like / ring-like staining pattern in ependymal cells (Appl Immunohistochem Mol Morphol 2018;26:71)
Uses by pathologists
- Common epithelial marker, commonly used alongside other cytokeratin stains (Dabbs: Diagnostic Immunohistochemistry, 3rd Edition, 2011)
- Marker of Paget disease (Am J Surg Pathol 2001;25:1469)
- Partial reverse cell polarity (prominent linear EMA reactivity on the periphery of tumor cell clusters with decreased cytoplasmic staining) may identify breast carcinomas that represent part of the spectrum of invasive micropapillary carcinoma but lack its morphology (Am J Surg Pathol 2010;34:1637)
- Distinguishes
- Meningioma (EMA+) from schwannoma (EMA-) (J Neuropathol Exp Neurol 2017;76:289)
- Systemic anaplastic large cell lymphoma (EMA+) from cutaneous anaplastic large cell lymphoma (usually EMA-) (Am J Surg Pathol 2008;32:1421)
- Malignant mesothelioma (EMA+) from reactive mesothelium (EMA-) (Cancer Cytopathol 2010;118:90)
- Squamous cell carcinoma and sebaceous carcinoma (EMA+) from basal cell carcinoma (EMA-) (Histopathology 2000;37:218)
- Ovarian epithelial cancers (EMA+) from sex cord stromal tumors (EMA-) (Hum Pathol 2004;35:1014, Mod Pathol 2003;16:584)
Prognostic factors
- Increased expression is associated with poor prognosis of most carcinomas, including those involving breast, cervical, pancreatic, colorectal (Clin Cancer Res 2020;26:2411, J Cancer Res Clin Oncol 2018;144:1899, World J Surg Oncol 2007;5:31, Oncol Rep 2019;41:801)
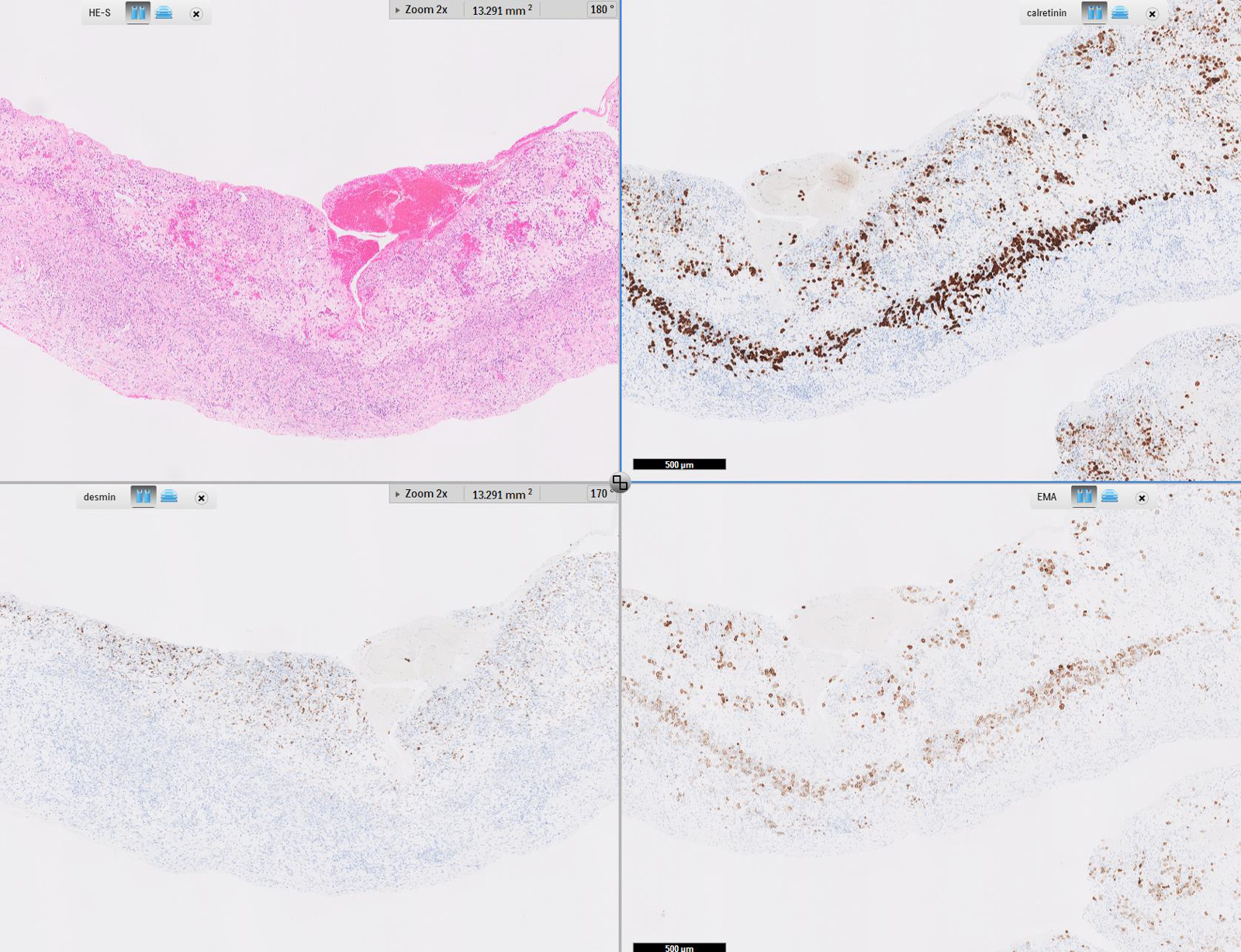
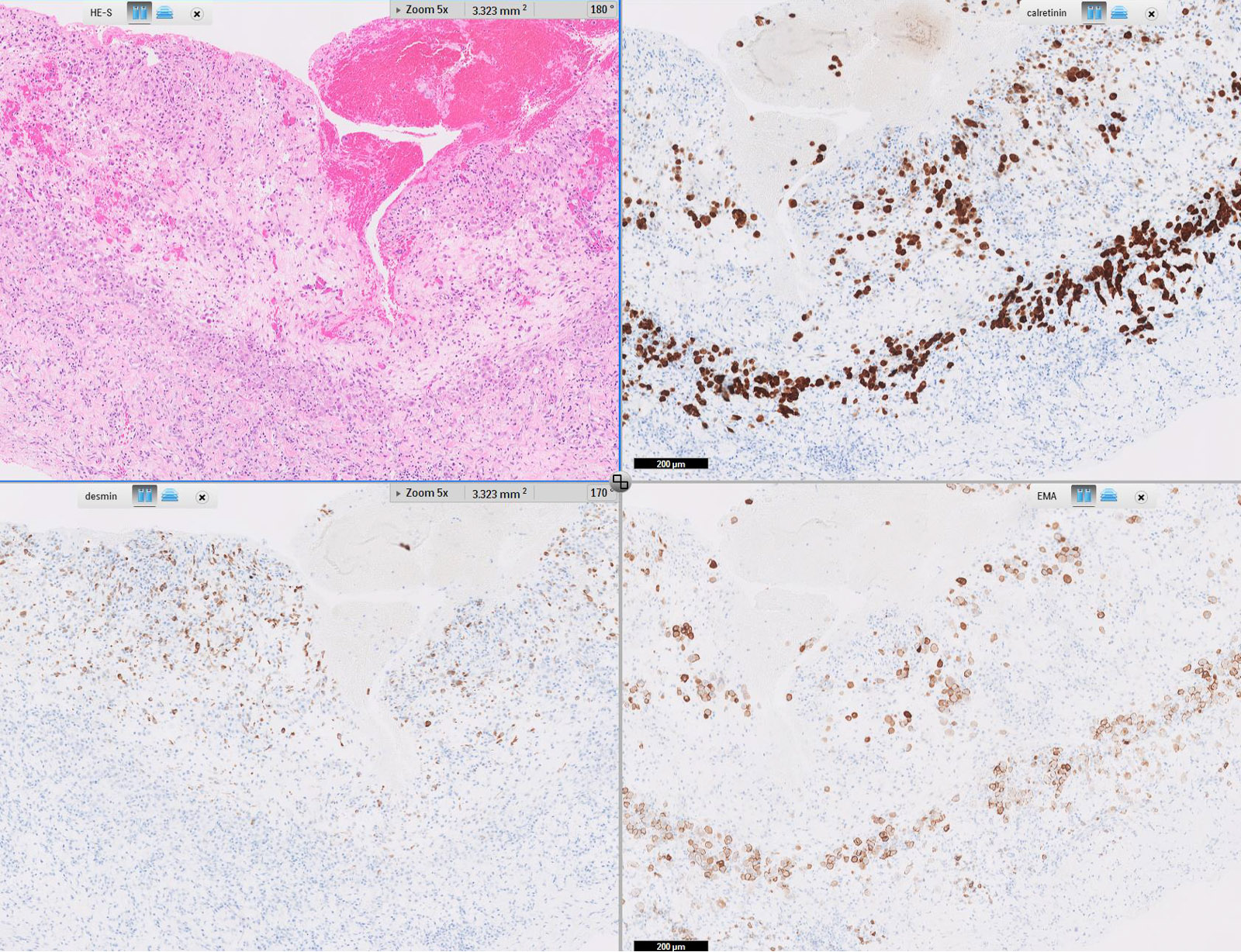
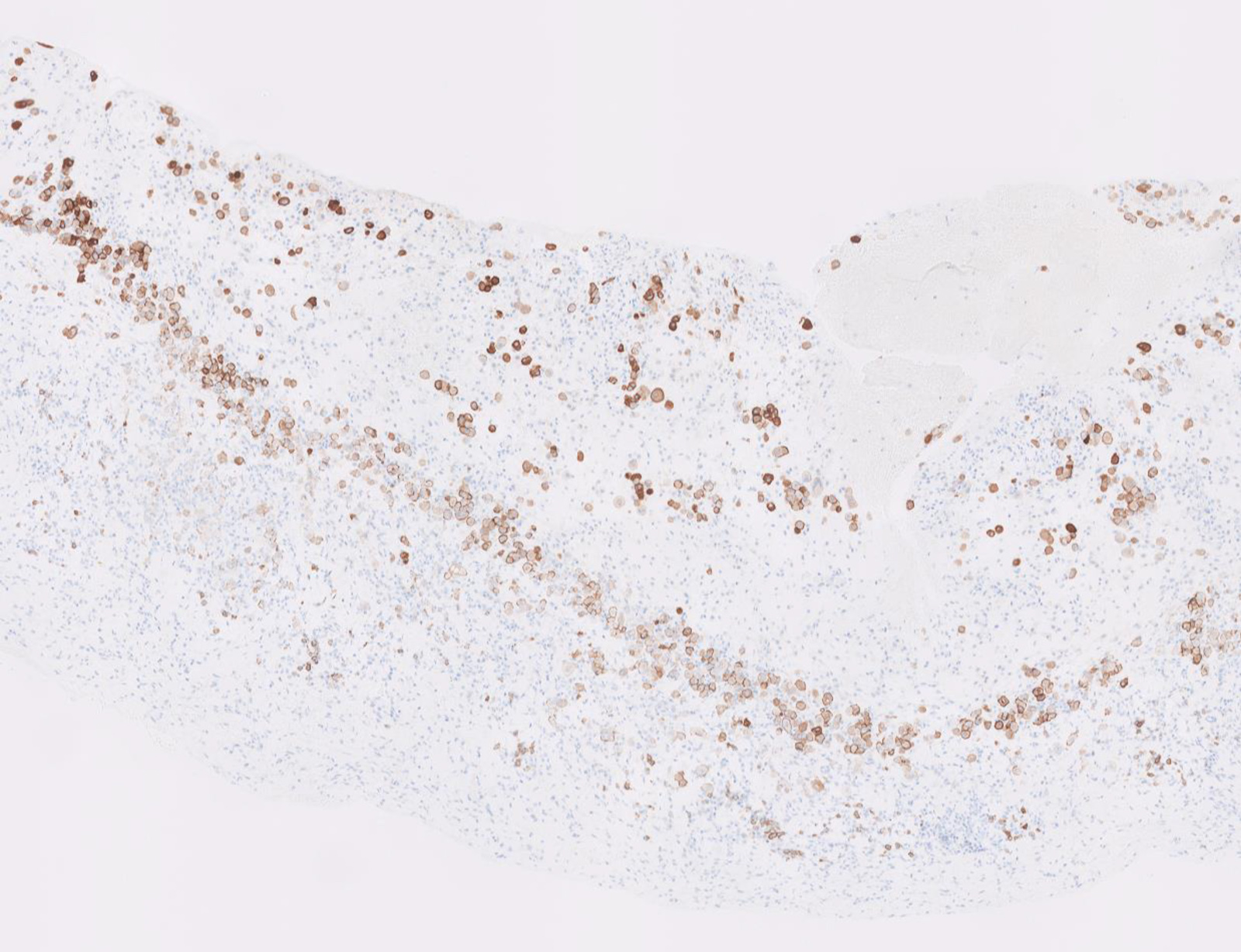
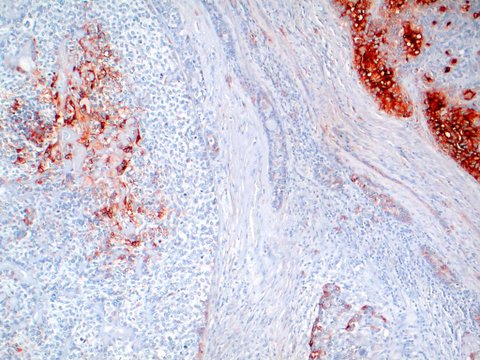
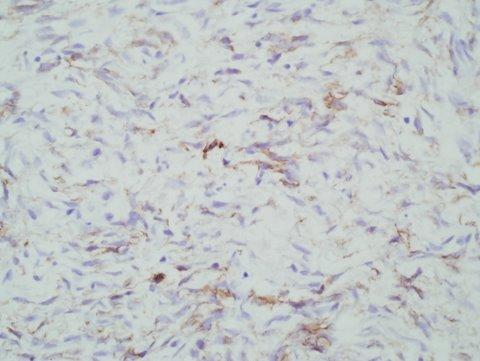
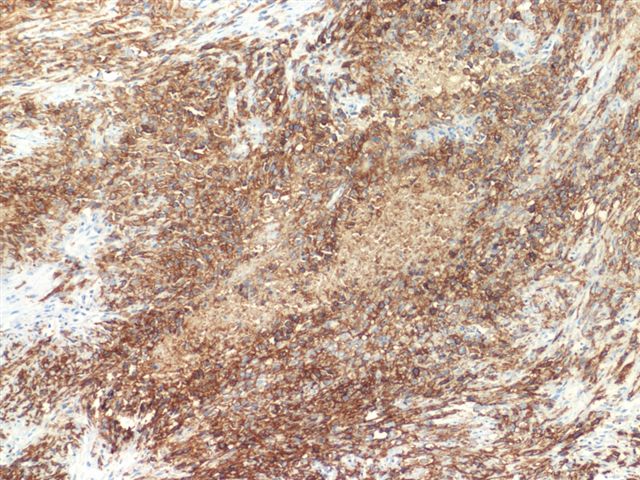
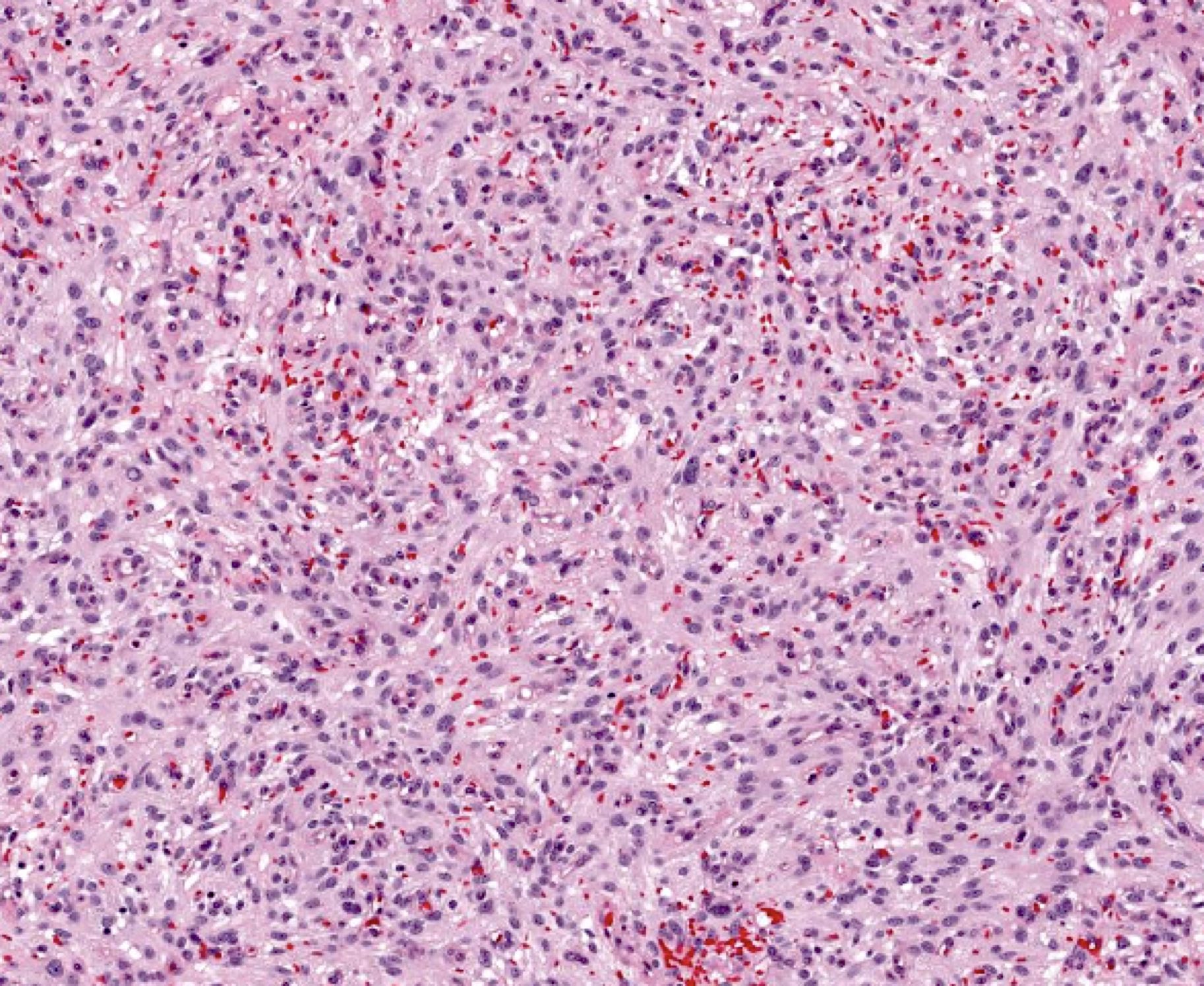
Microscopic (histologic) images
Virtual slides
Cytology images
Positive staining - normal
- Apical surface of almost all glandular and ductal epithelial cells, including respiratory, gastrointestinal, urogenital, hepatobiliary tracts, sebaceous and salivary glands (Cell Mol Life Sci 2015;72:4475, see Table 1 for more details)
- Human corneal and conjunctival epithelial cells (Cornea 2002;21:691)
- Eustachian tube and middle ear epithelium (Laryngoscope 2007;117:1666)
- Clear cells of Toker (J Cutan Pathol 2003;30:256)
- Perineural cells (Histopathology 2005;47:159)
- Hematopoietic cells
- Proerythroblasts and erythroblasts (Br J Haematol 2003;120:344)
- T cells and B cells (Exp Cell Res 2002;280:107)
- Dendritic cells (J Leukoc Biol 2002;72:692)
- Monoblasts, monocytes (Pathology 2003;35:422)
- Plasma cells (Histol Histopathol 2007;22:889)
- Reed-Sternberg (both with classical Hodgkin lymphoma and Reed-Sternberg-like cells) (Diagnostics (Basel) 2020;10:1019)
Positive staining - disease
- Adenocarcinomas (breast, colorectal, pancreatic, other) (Med Res Rev 2017;37:1518)
- Chordoma (Appl Immunohistochem Mol Morphol 2009;17:131)
- Choriocarcinoma (Int J Clin Exp Pathol 2015;8:5650)
- Desmoplastic small round cell tumor (Clin Case Rep 2016;4:520)
- Ductal adenoma of breast (Pathol Int 2008;58:801)
- Epithelioid sarcoma (Pediatr Dev Pathol 2019;22:59)
- Ependymomas (Appl Immunohistochem Mol Morphol 2018;26:71)
- Ewing sarcoma (membranous staining) (Histopathology 2014;64:101)
- Follicular dendritic cell sarcoma, interdigitating dendritic cell / reticulum cell sarcoma
- Lymphomas
- ALK positive anaplastic large cell lymphoma (J Clin Pathol 2001;54:933)
- ALK positive diffuse large B cell lymphoma (Pol J Pathol 2005;56:37)
- Plasmablastic lymphoma (variable) (Diagn Pathol 2015;10:78)
- Lymphocyte predominant Hodgkin lymphoma (variable) (Blood 2000;96:1889)
- Primary effusion lymphoma (Blood Cancer J 2014;4:e190)
- Meningioma (Kaye: Brain Tumors, 3rd Edition, 2012)
- Mesotheliomas (epithelioid) (J Clin Diagn Res 2017;11:EC36)
- Micropapillary carcinoma of the breast (reverse polarity) (Pathol Res Pract 1994;190:668)
- Myoepithelial tumor of bone (Surg Pathol Clin 2017;10:657)
- Paget disease (Am J Surg Pathol 2001;25:1469)
- Perineural cell tumors (benign and malignant) (Mod Pathol 2003;16:293)
- Plasma cell diseases: myeloma, plasmacytoma (Histol Histopathol 2007;22:889)
- Pulmonary sclerosing hemangiomas (Interact Cardiovasc Thorac Sug 2012;15:171)
- Renal cell carcinomas (Rom J Morphol Embryol 2011;52:1019)
- Salivary gland tumors (Ann Diagn Pathol 2019;43:151408)
- Small cell carcinoma of hypercalcemic type (Arc Pathol Lab Med 2015;139:39)
- Squamous cell carcinoma (Otolaryngol Head Neck Surg 1987;97:288)
- Synovial sarcoma (epithelial areas) (Mod Pathol 2006:19;659)
- Thymic carcinoma (more than thymomas) (Diagn Pathol 2007;2:13)
- Undifferentiated endometrial carcinoma (Int J Gynecol Pathol 2018;37:564)
Negative staining
- Normal (Cell Mol Life Sci 2015;72:4475)
- Skin epidermal cells
- Mesenchymal tissue
- Erythrocytes
- Natural killer cells
- Benign mesothelium
- Disease
- Adrenal cortical tumors (Appl Immunohistochem Mol Morphol 2012;20:141)
- Acquired cystic disease associated renal cell carcinoma (Mod Pathol 2006;19:780)
- Basal cell carcinoma (Histopathology 2000;37:218)
- Gynecologic (Arc Pathol Lab Med 2015;139:39)
- Dysgerminoma
- Yolk sac tumor
- Granulosa cell tumor
- Sertoli stromal tumors
- Female adnexal tumor of Wolffian origin (FATWO)
- Hemangiopericytoma (Hum Pathol 2004;35:1413)
- Melanoma (Histopathology 2007:52;119)
- Olfactory neuroblastoma (Head and Neck Pathol 2009;3:252)
- Paraganglioma / pheochromocytoma (Mod Pathol 2011;24:S58)
- Reactive gastropathy (Arch Pathol Lab Med 2007;131:86)
- Solitary fibrous tumor (J Neuropathol Exp Neurol 2017;76:289)
- Schwannoma (J Neuropathol Exp Neurol 2017;76:289)
Sample pathology report
- Left frontal tumor, craniotomy and resection:
- Meningioma, WHO grade 1 (see comment)
- Comment: The histologic features fit well for a meningioma with fibroblastic features. EMA shows positive cytoplasmic staining in the spindle cells. There are no atypical features and mitoses are sparse. The MIB1 labeling is low (less than 4%).
Additional references
Board review style question #1
Board review style answer #1
C. EMA. Warning: EMA can highlight the perineural fibroblasts in schwannomas but is not positive within the mass.
AE1 / AE3 is not typically positive in meningiomas. CD34 is better for differentiating solitary fibrous tumors from meningioma and is typically negative in schwannoma. MelanA differentiates meningioma from melanoma. MelanA is negative in most schwannomas. S100 can be positive in both schwannoma and in fibrous meningioma
(J Neuropathol Exp Neurol 2017;76:289).
Comment Here
Reference: Epithelial membrane antigen (EMA)
Comment Here
Reference: Epithelial membrane antigen (EMA)