Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Uses by pathologists | Prognostic factors | Interpretation | Microscopic (histologic) images | Positive staining - normal | Positive staining - not malignant | Positive staining - malignant | Negative staining - normal | Negative staining - tumor / disease | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Maniar KP, Umphress B. Cytokeratin 7 (CK7, K7). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsCK7.html. Accessed March 30th, 2025.
Definition / general
- Type II keratin of simple nonkeratinizing epithelia; molecular weight 51.4 kDa (OMIM: Keratin 7, TYPE II; KRT7 [Accessed 14 September 2020])
- Expression similar to but more limited than keratins 8 and 18 in simple, pseudostratified and ductal epithelium, mesothelium and urothelium
Essential features
- Membranous / cytoplasmic marker with expression in many normal epithelia and epithelial tumors
- Despite wide distribution, useful as part of a panel in determining primary site of metastatic carcinoma
- Generally expressed (with some variation) in adenocarcinoma of lung, breast, thyroid, endometrium, cervix, ovary, salivary gland, upper GI tract, urothelial carcinoma, papillary renal cell carcinoma and Paget disease
- Generally negative (with some variation) in colorectal carcinoma, Merkel cell carcinoma, hepatocellular carcinoma, prostatic adenocarcinoma, adrenocortical tumors and squamous cell carcinoma
Terminology
- Also known as keratin 7, CK7, KRT 7, K7
Pathophysiology
- Like other keratins, component of intermediate filaments forming cytoskeleton of epithelial cells (J Anat 2009;214:516)
- Type II keratins, arranged in pairs of heterotypic keratin chains, are expressed during differentiation of certain epithelial tissues (NCBI - Gene - KRT7)
Uses by pathologists
- CK7 / CK20 profiles (general patterns, specificity varies):
- CK7+ / CK20+:
- Extrahepatic carcinoma of the bile duct (majority) (Pathol Res Pract 2003;199:65)
- Gastric adenocarcinoma, subset (majority are CK7+ / CK20-) (see below)
- Pancreatic adenocarcinoma, minor subset (co-expression associated with worse prognosis, however, majority are CK7+ / CK20-) (see below) (Cancer 2006;106:693)
- Primary mucinous tumors of the ovary (74%) (Am J Surg Pathol 2006;30:1130)
- Pulmonary invasive mucinous adenocarcinoma subset (17%) (Oncol Lett 2018;15:489)
- Sinonasal adenocarcinoma of intestinal type (CK20+ with variable CK7+) (Head Neck Pathol 2016;10:68)
- Small intestinal adenocarcinoma (67%) (Am J Surg Pathol 2004;28:1352)
- Urothelial carcinoma (60%) (Hum Pathol 2002;33:1136)
- CK7+ / CK20-:
- Breast carcinoma (Ann Diagn Pathol 1999;3:350)
- Cervical squamous cell carcinoma and adenocarcinoma (Mod Pathol 2000;13:962)
- Endometrial adenocarcinoma (Int J Gynecol Pathol 2002;21:4)
- Esophageal adenocarcinoma (Am J Surg Pathol 2002;26:1213)
- Gastric adenocarcinoma (71% CK7+, 30% CK20+) (Hum Pathol 2004;35:576)
- Intrahepatic carcinoma of the bile duct (Pathol Res Pract 2003;199:65)
- Lung acinar adenocarcinoma (BMC Cancer 2006;6:31)
- Mesothelioma (pleural and peritoneal) (Cancer. 2001;92:2727, Arch Pathol Lab Med 2018;142:236)
- Ovarian adenocarcinoma, including endometrioid, clear cell, serous, seromucinous (Am J Surg Pathol 2015;39:983, Am J Surg Pathol 2004;28:1499)
- Pancreatic adenocarcinoma (majority but see also above) (Arch Pathol Lab Med 2000;124:1196)
- Renal cell carcinoma, papillary, chromophobe and clear cell papillary types
- Salivary gland carcinoma (93%) (Mod Pathol 2004;17:407)
- Thyroid tumors (adenoma and carcinoma) (Appl Immunohistochem Mol Morphol 2000;8:189)
- Urothelial carcinoma (30%) (Hum Pathol 2002;33:1136)
- CK7- / CK20+:
- Colorectal carcinoma (particularly early stage) (Hum Pathol 2005;36:275)
- Merkel cell carcinoma (88% CK20+ with a perinuclear punctate or dot-like pattern, 23% CK7+) (Appl Immunohistochem Mol Morphol 2000;8:310)
- CK7- / CK20-:
- Adrenal cortical carcinoma and adenoma
- Germ cell tumor, seminoma and embryonal carcinoma subtypes
- Hepatocellular carcinoma
- Pituitary adenoma
- Prostatic adenocarcinoma
- Renal cell carcinoma, clear cell type
- Squamous cell carcinoma (with exception of cervix, a subset of head and neck squamous cell carcinomas and a subset of cutaneous squamous cell carcinomas, particularly poorly differentiated tumors, which can express focal-to-partial positivity for CK7) (Head Neck Pathol 2018;12:448, J Cutan Pathol 2010;37:966)
- CK7+ / CK20+:
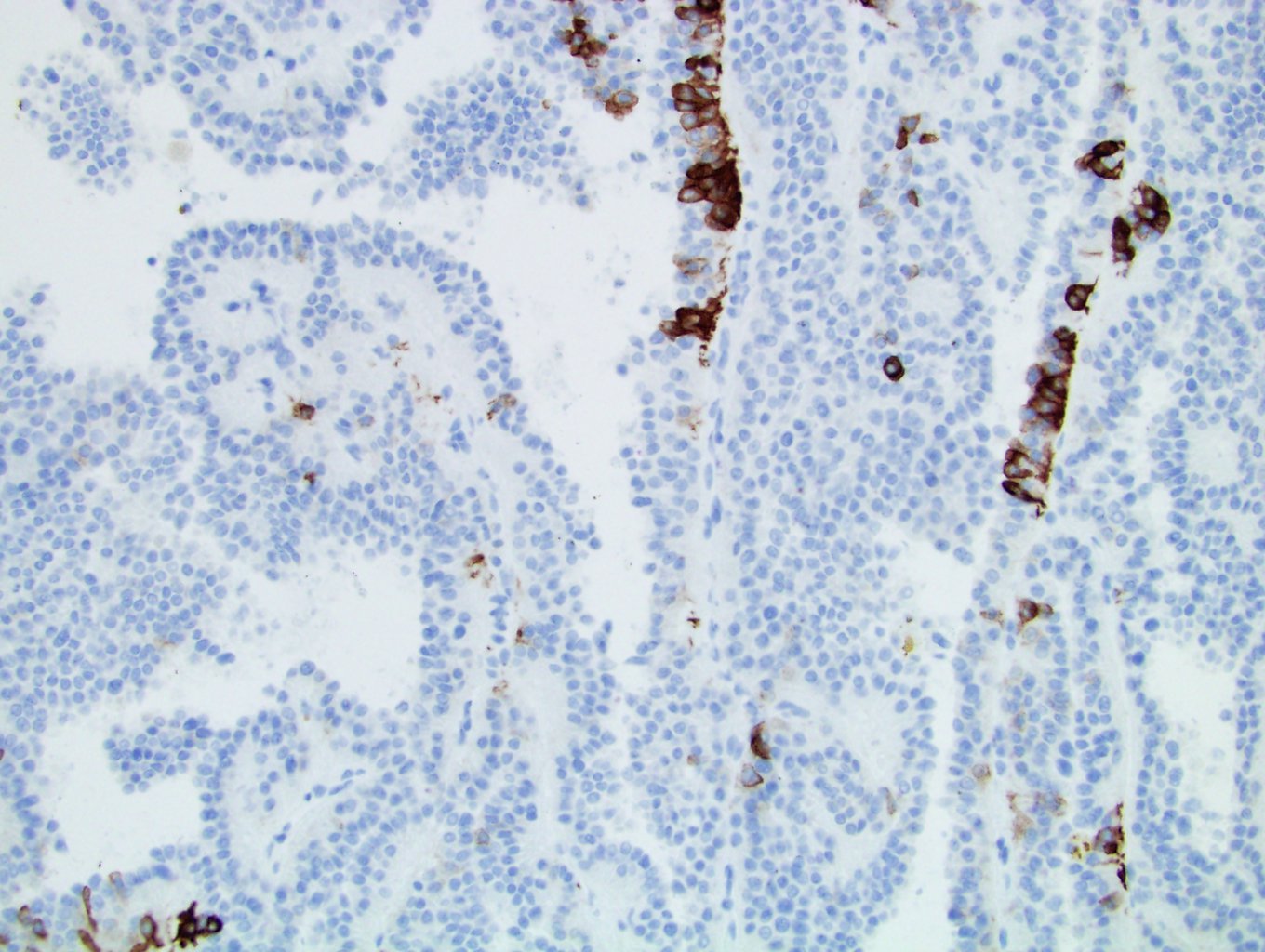
- Other uses - to distinguish:
- Renal tumors
- Chromophobe renal cell carcinoma (diffuse CK7+) from oncocytoma (rare sprinkled cells express CK7-) (Anal Quant Cytol Histol 2006;28:228)
- Addition of Claudin-7 and CD117 to CK7 or the “three 7 markers” further increases specificity for chromophobe renal cell carcinoma versus other histologic mimics (Dis Markers 2019;2019:4708154)
- Classically, clear cell renal cell carcinoma (CK7-) from other renal cell carcinoma subtypes (including papillary, chromophobe and clear cell papillary); however, CK7 immunoreactivity in clear cell renal cell carcinomas can be variable with low grade clear cell RCC, multicystic renal neoplasm of low malignant potential and clear cell papillary RCC-like groups exhibiting the highest degree of positivity, ranging from 60 - 93% (Histopathology 2019;74:608, Arch Pathol Lab Med 2012;136:410)
- Papillary renal cell carcinoma (CK7+) from metanephric adenoma (CK7-) (Mod Pathol 2006;19:218)
- Adenocarcinoma of distal esophagus from proximal stomach (variable CK7 / CK20 patterns but CK7+ / CK20- pattern favors esophageal origin) (Am J Surg Pathol 2002;26:1213)
- Appendiceal mucinous neoplasms (31% CK7+) from primary ovarian mucinous neoplasms (97% CK7+) (Histopathology 2016;68:977)
- Barrett esophagus from gastric cardiac intestinal metaplasia: Barrett pattern is diffuse CK7+ / surface and crypt epithelium CK20+ but interpretation is affected by fixative and not consistent between laboratories (Hum Pathol 2005;36:58, Mod Pathol 2002;15:611, World J Gastroenterol 2005;11:6360)
- Endometrioid and clear cell carcinoma (CK7+) from yolk sac tumors (CK7- or focal) (Am J Surg Pathol 2004;28:1499)
- Metastatic Krukenberg tumors of the ovary originating from the stomach (93% CK7+) versus colorectum (8% CK7+) (Am J Surg Pathol 2018;42:160)
- Primary lung carcinoma (CK7+ / CK20-) from metastatic colonic carcinoma to lung (CK7- / CK20+) (BMC Cancer 2006;6:31)
- Primary ovarian mucinous tumors can be differentiated from lower gastrointestinal primaries by utilizing a two marker combination of CK7 and SATB2 with greater than 95% accuracy (in many cases primary ovarian mucinous tumors are CK7+, SATB2-) (Modern Pathol 2019;32:1834)
- Renal tumors
Prognostic factors
- CK7 expression in esophageal squamous cell carcinoma is an independent prognostic factor for poor overall survival (Neoplasma 2018;65:469)
- CK7 / CK19 index is an independent adverse prognostic factor for postoperative survival in intrahepatic cholangiocarcinoma patients (J Surg Oncol 2018;117:1531)
- No association with prognosis when used as a marker for intestinal versus pancreaticobiliaryorigin in ampullary carcinoma (Am J Surg Pathol 2017;41:865)
- Expression in cervical low grade squamous intraepithelial lesion (LSIL / CIN 1) associated with higher rates of subsequent HSIL but clinical utility potentially limited by low magnitude of risk difference and interpretive variability; no prognostic utility in CIN 2 (Am J Surg Pathol 2013;37:1311, Am J Surg Pathol 2017;41:143, Am J Surg Pathol 2018;42:479)
- Colorectal tumor cells expressing CK7 may demonstrate invasive capability with metastatic potential (J Cancer 2019;10:2510)
- High CK7 expression in BRAF-V600E mutated metastatic colorectal cancer confers worse overall survival (Br J Cancer 2019;121:593)
Interpretation
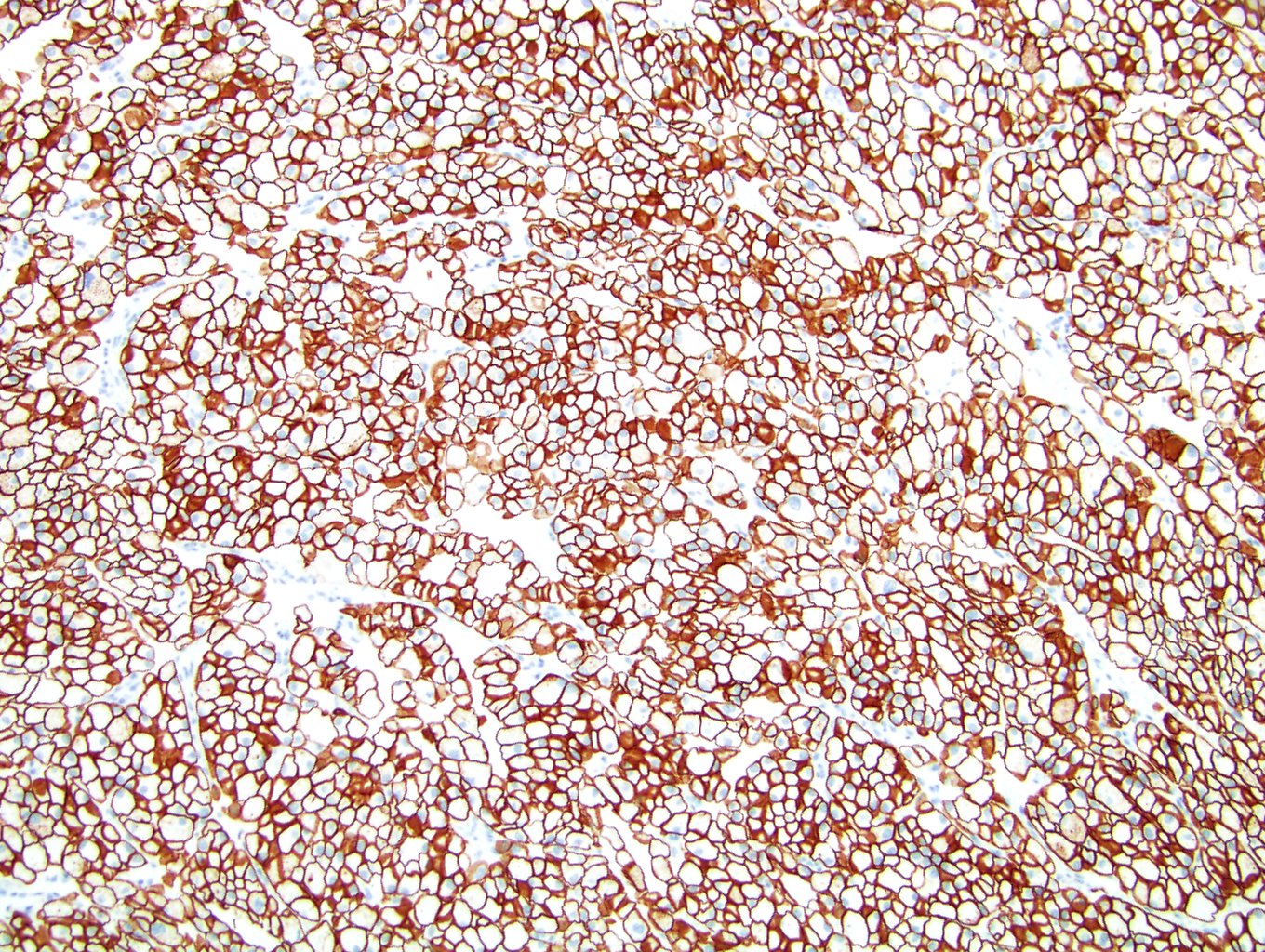
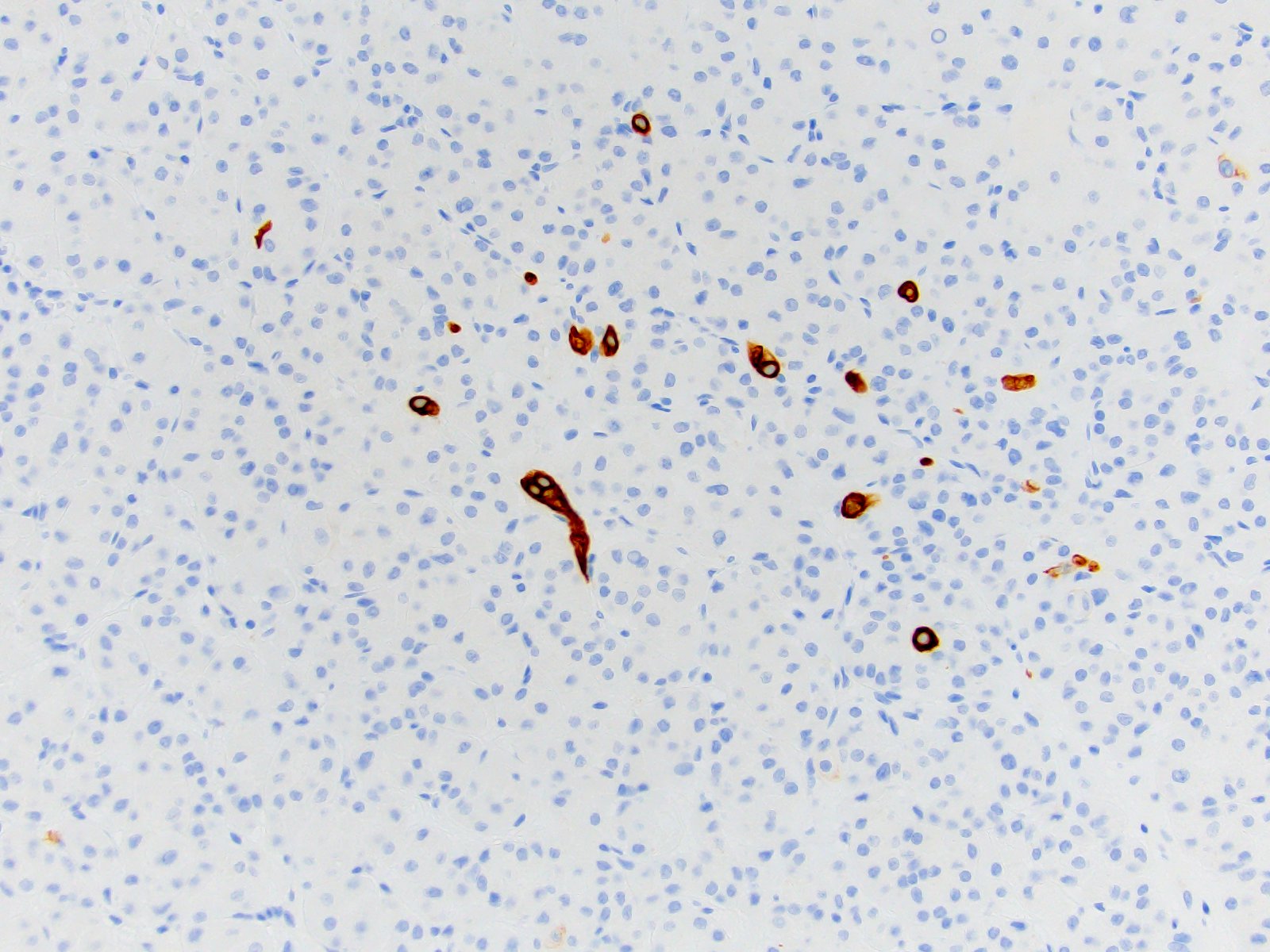
- Membranous / cytoplasmic staining, ranging from weak / focal to strong / diffuse
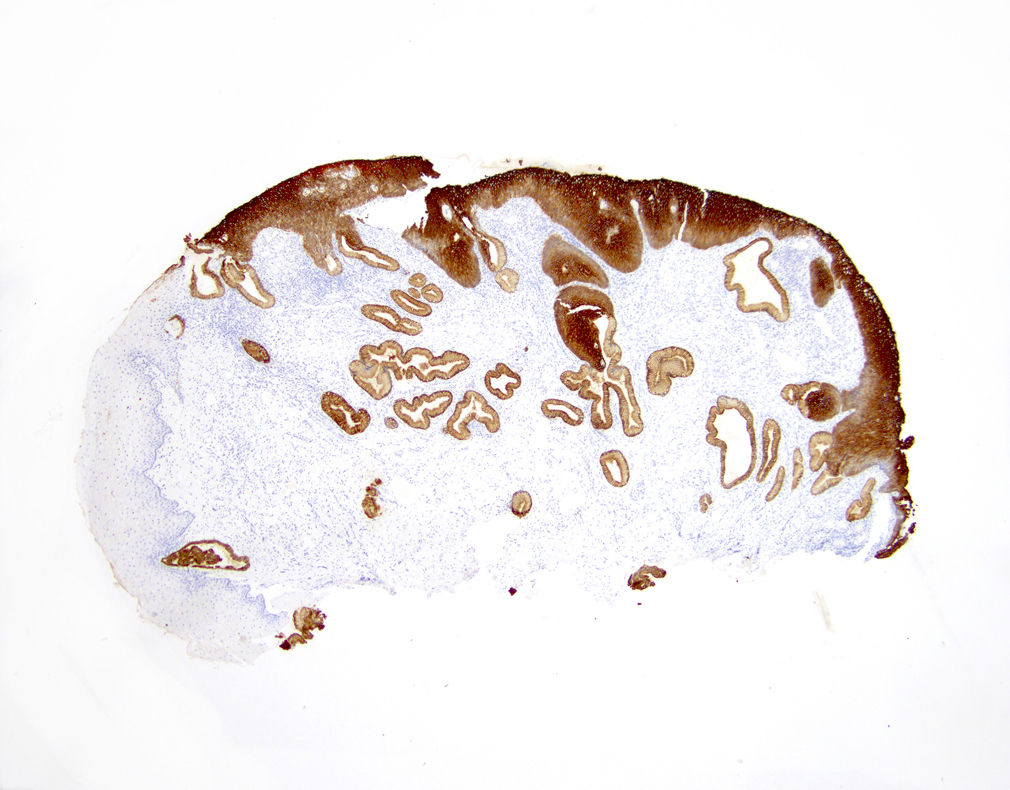
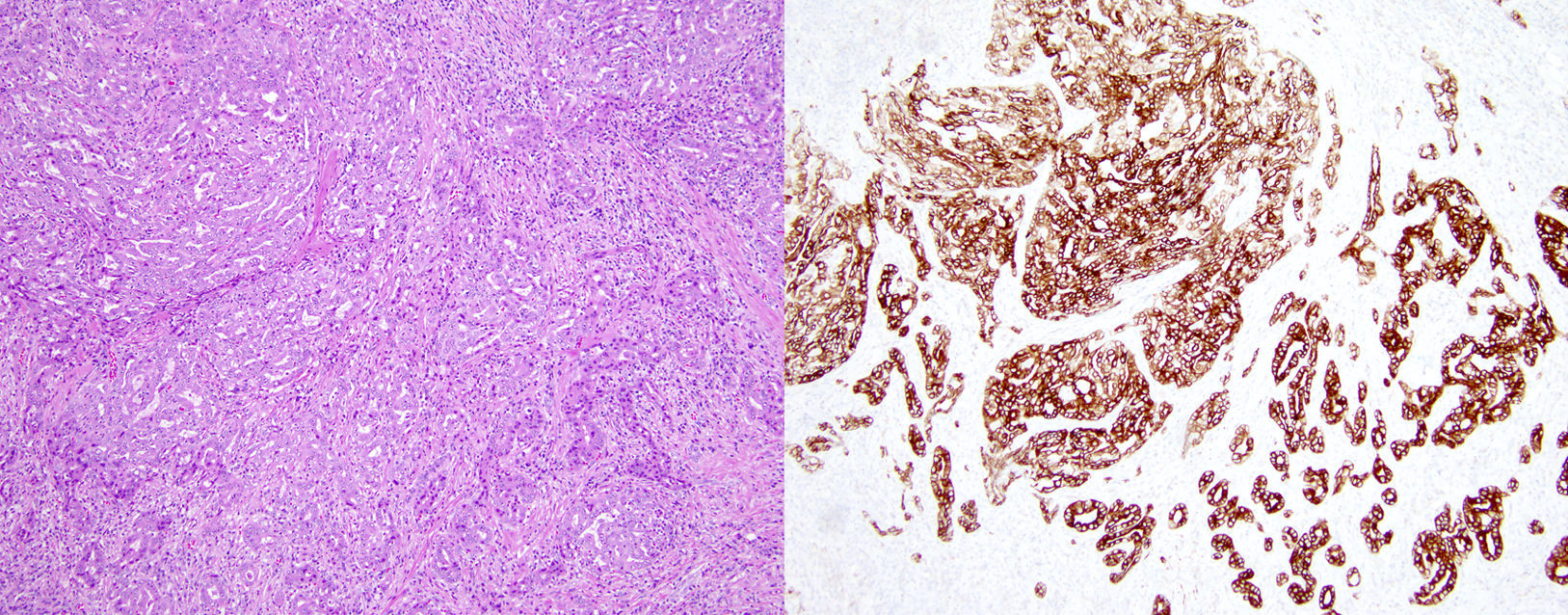
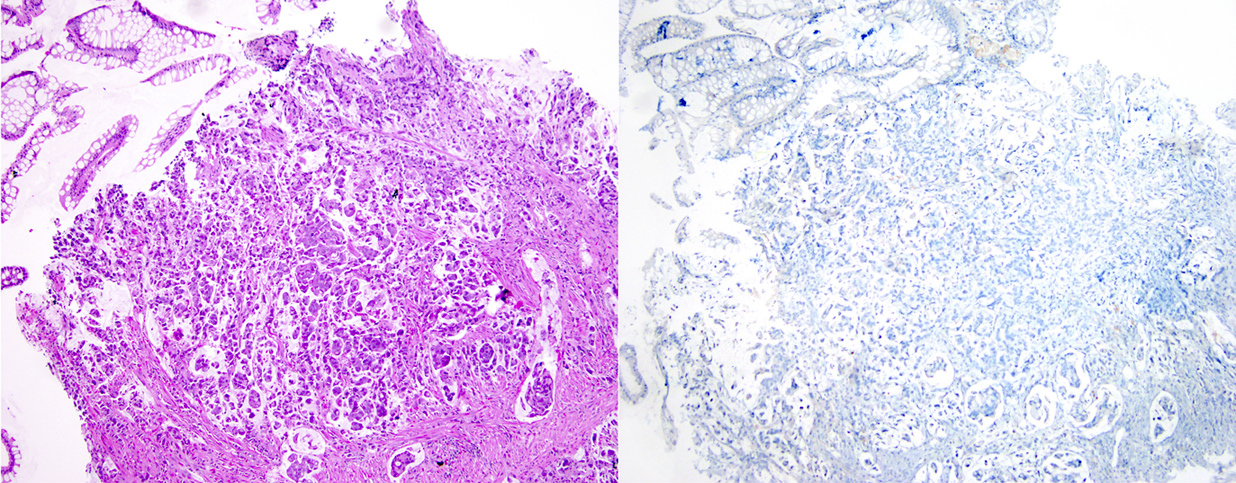
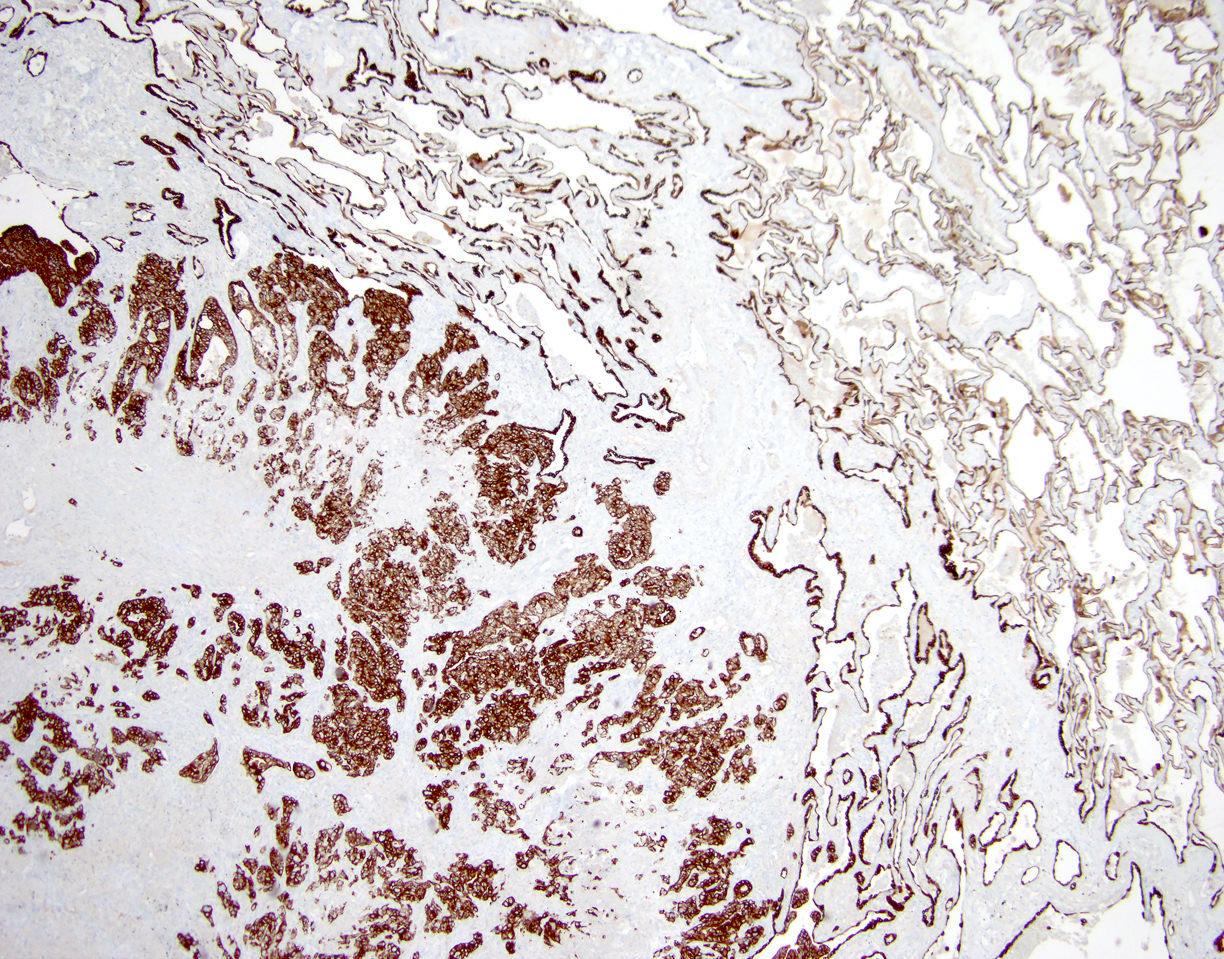
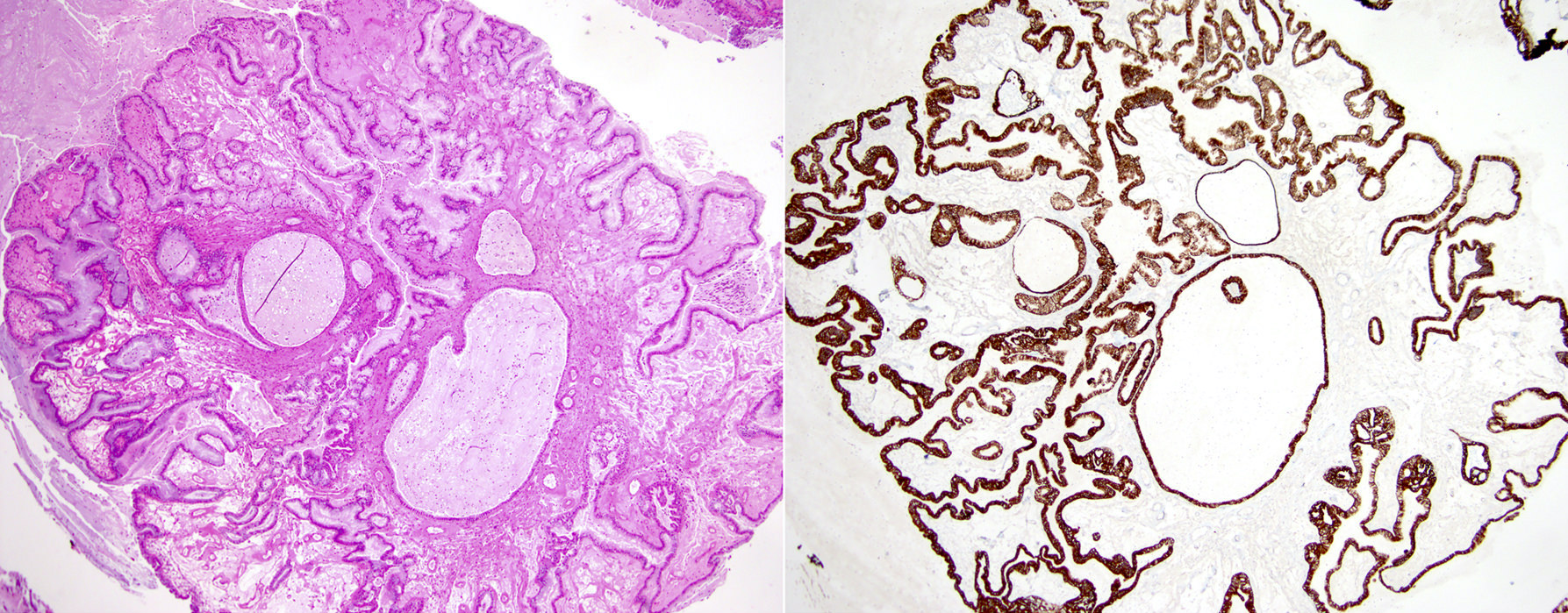
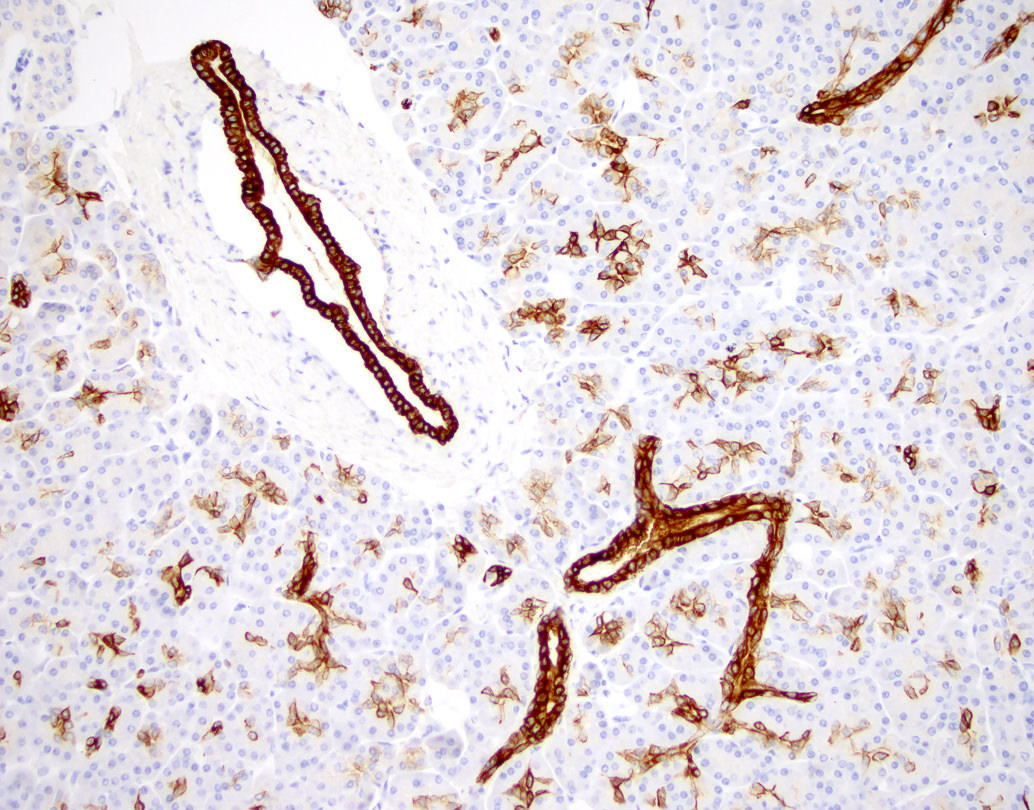
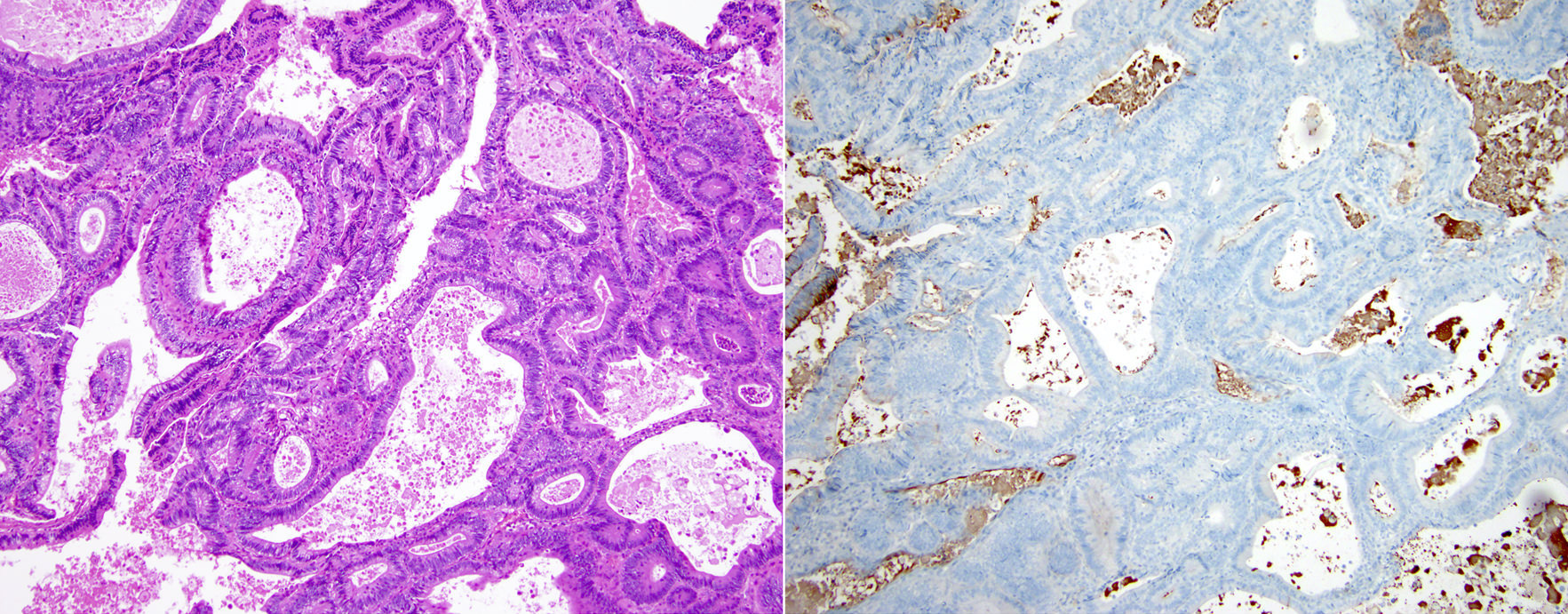
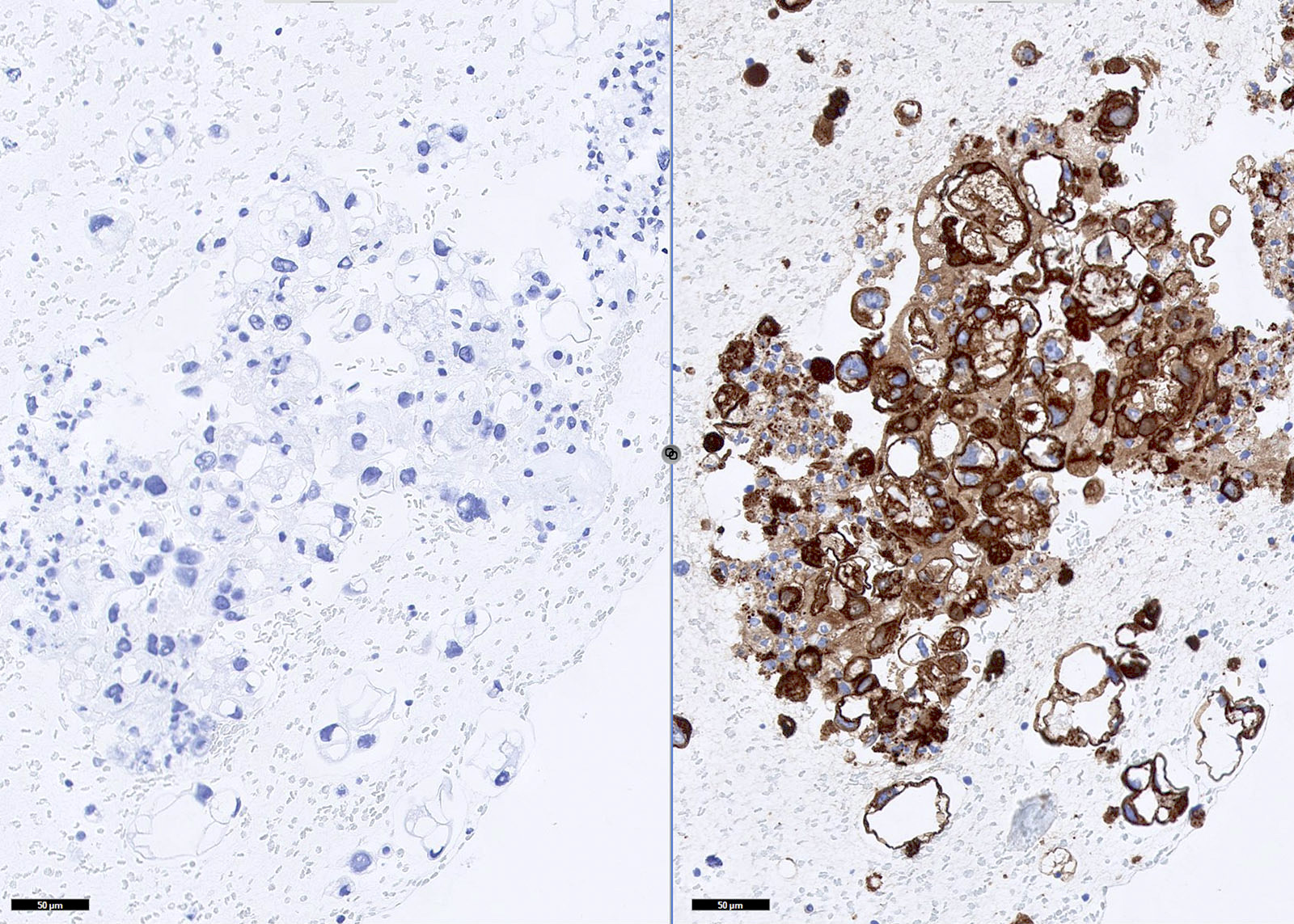
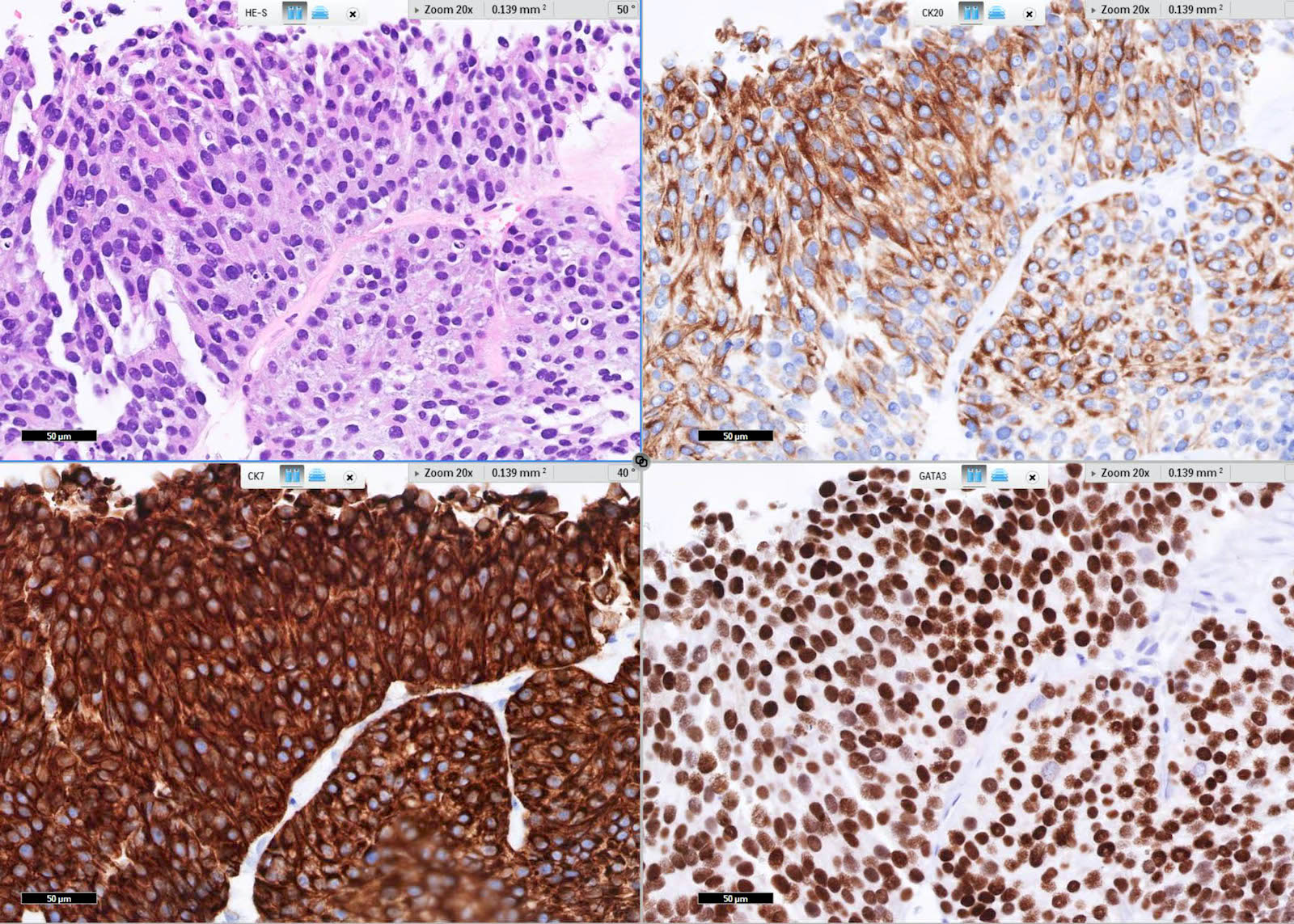
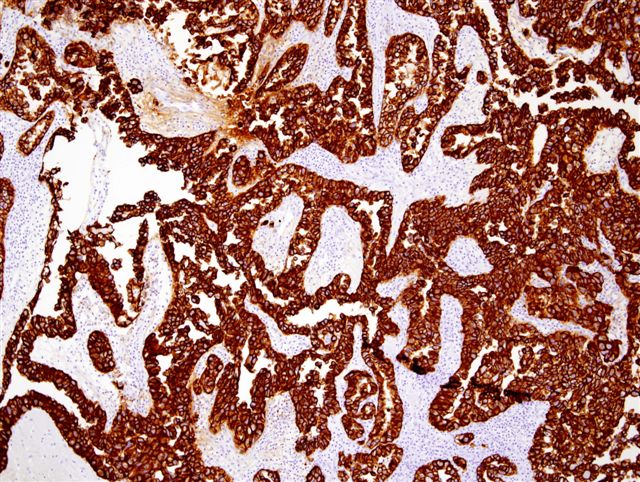
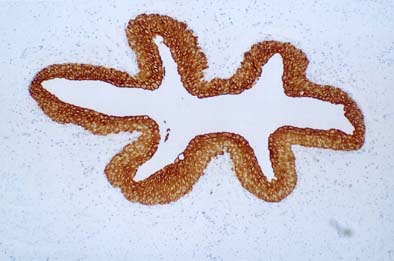
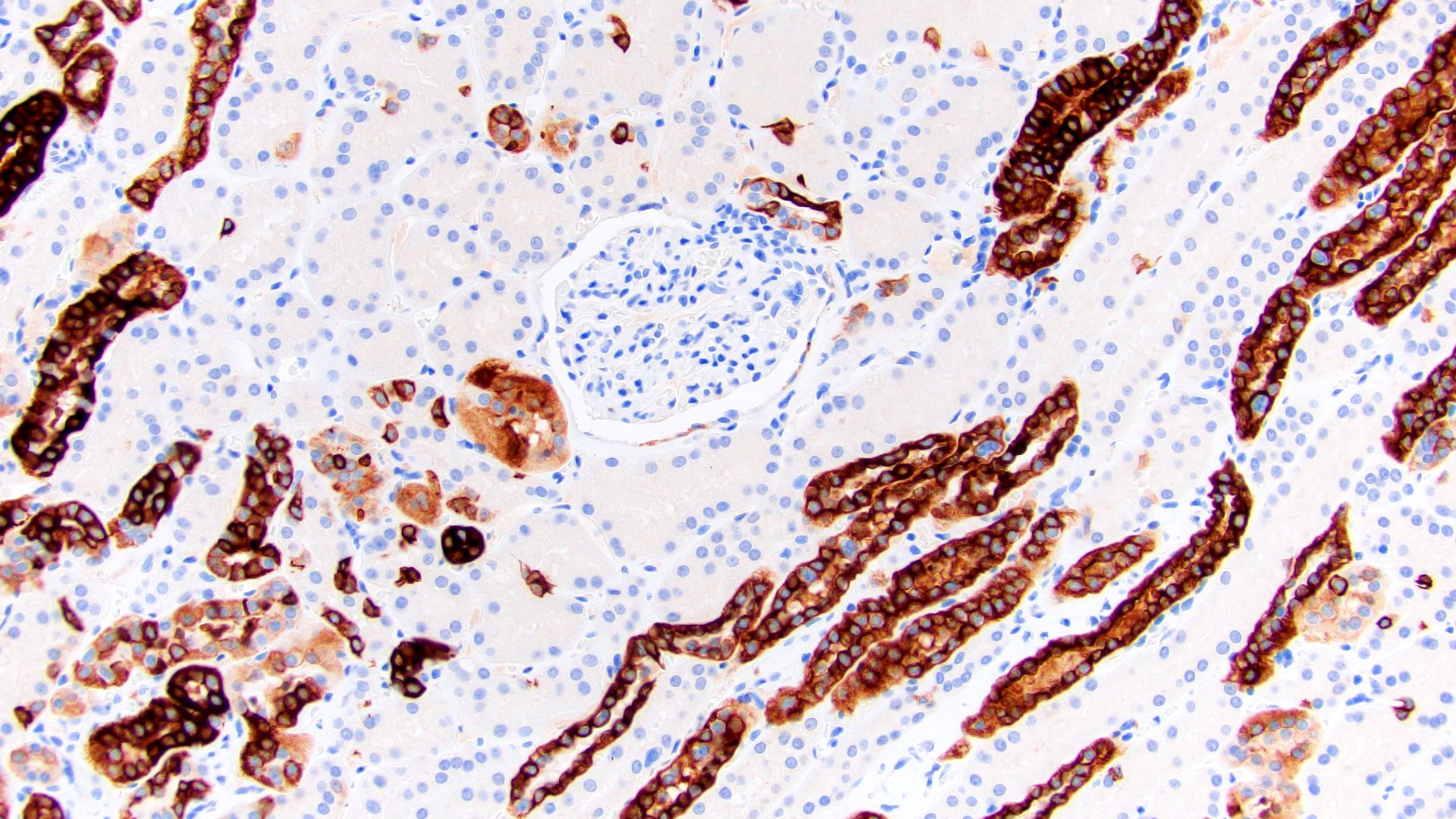
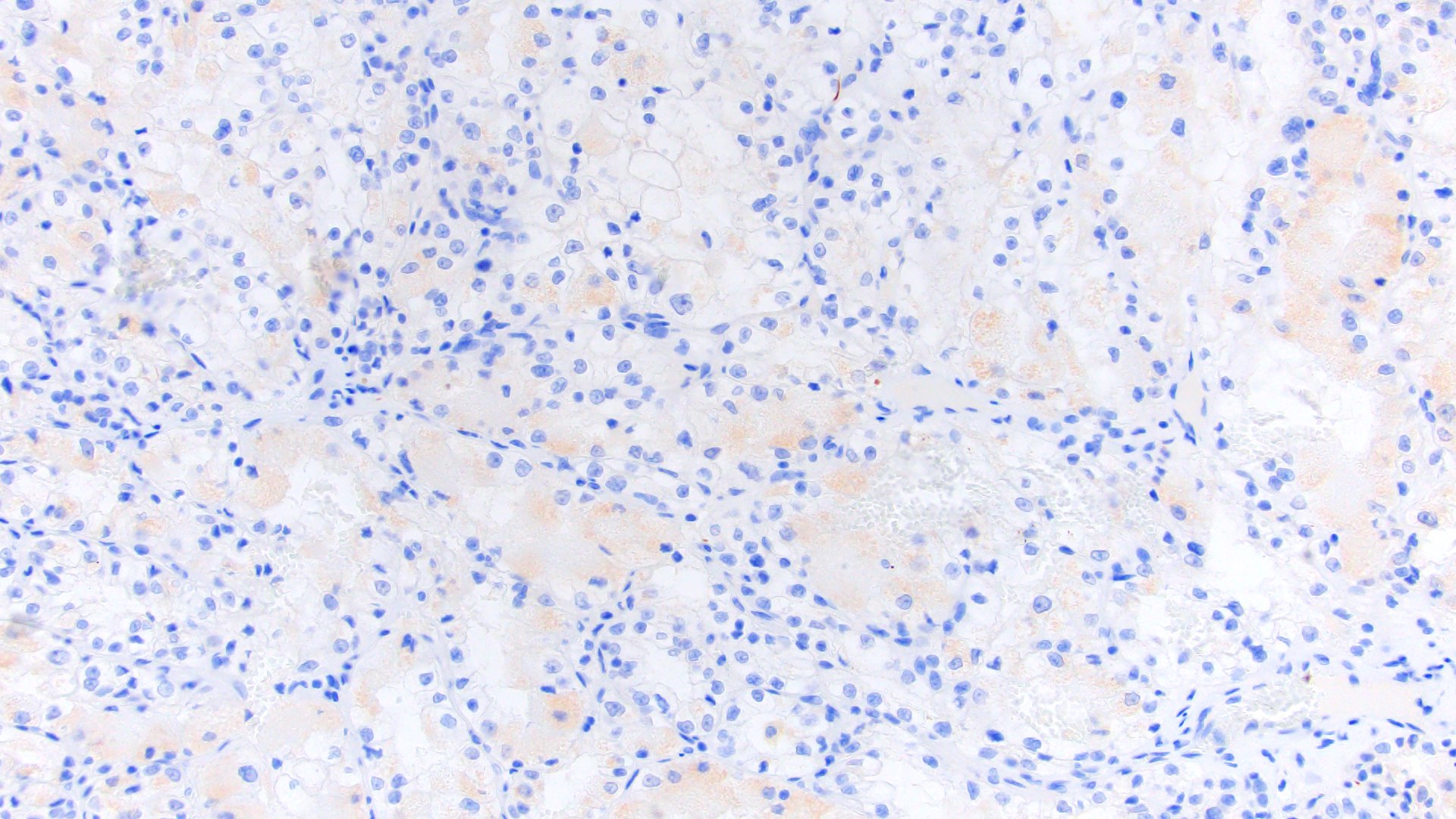
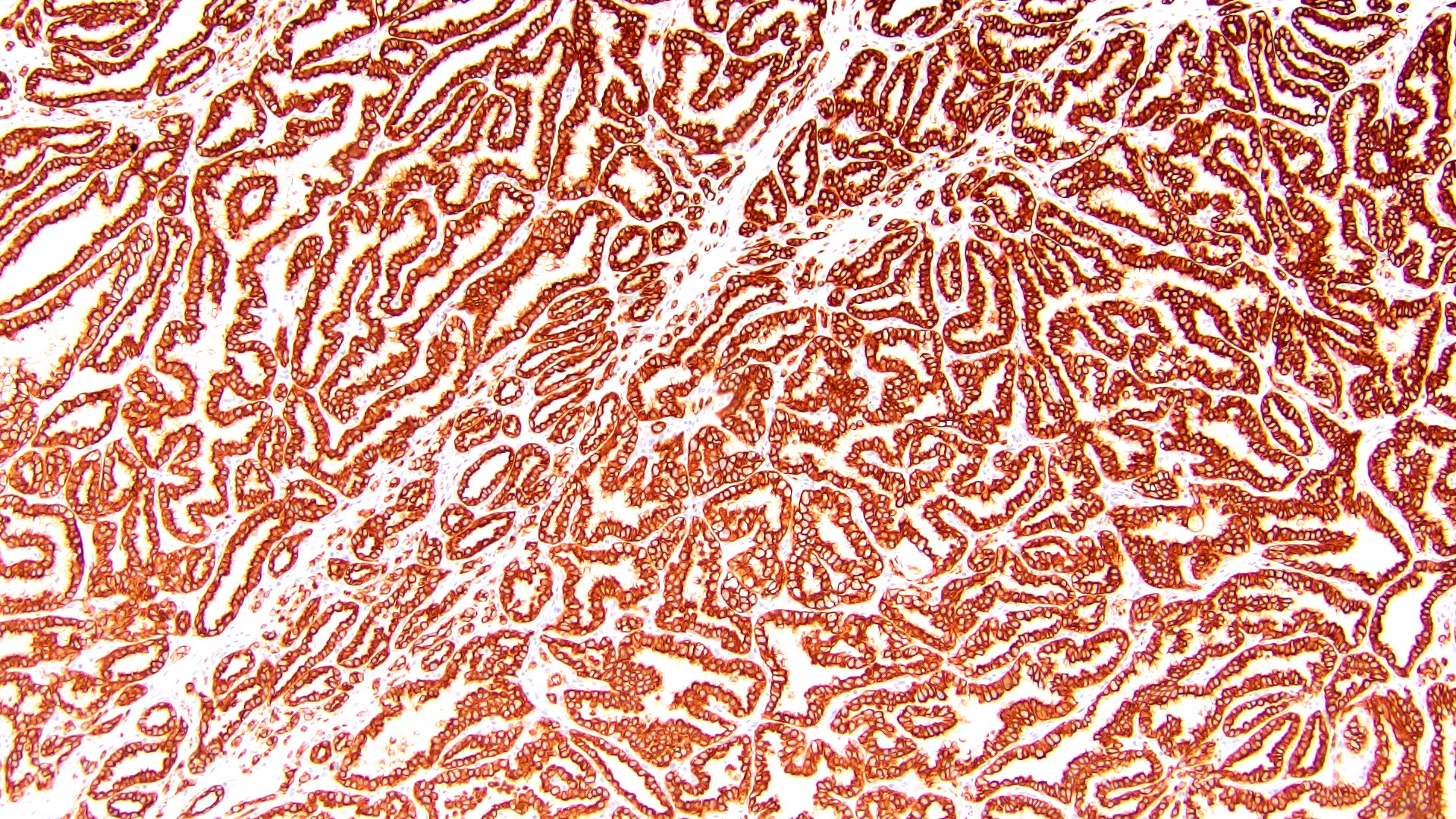
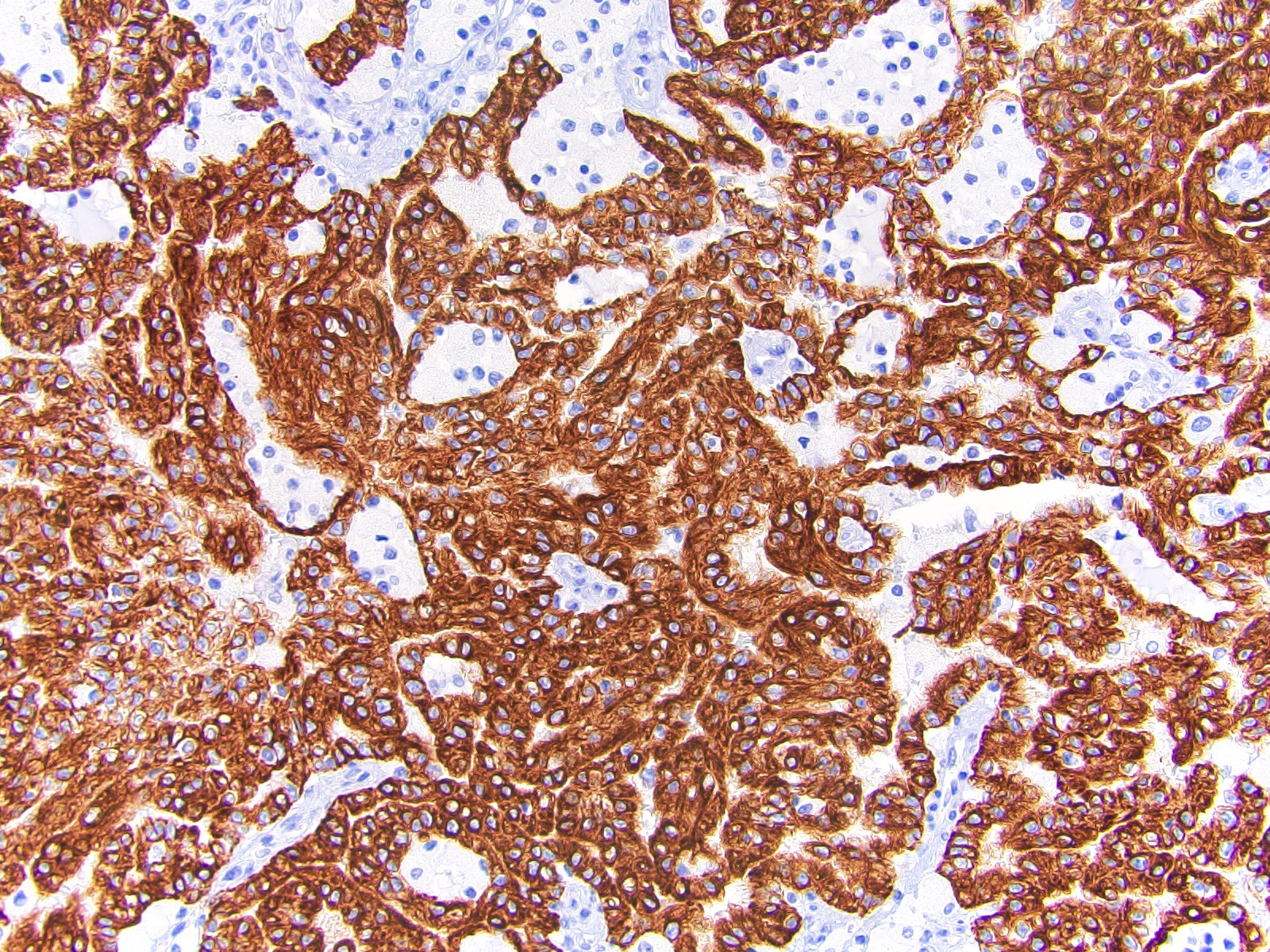
Microscopic (histologic) images
Contributed by Kruti P. Maniar, M.D.
Contributed by Andrey Bychkov, M.D., Ph.D., Eddie Fridman, M.D. (Case #194) and Leica Microsystems
Contributed by Maria Tretiakova, M.D., Ph.D.
Positive staining - normal
- Anal glands and anal transition zone (Arch Pathol Lab Med 2001;125:1074)
- Bile ducts (Exp Cell Res 1987;170:235)
- Breast (Exp Cell Res 1987;170:235)
- Cervix: endocervical glands and squamocolumnar junction cells (Proc Natl Acad Sci USA 2012;109:10516, Obstet Gynecol 1993;82:465)
- Conjunctiva (Am J Ophthalmol 2013;156:830)
- Endometrium
- Fallopian tube
- Gallbladder
- Kidney collecting ducts (Exp Cell Res 1987;170:235)
- Lung (Exp Cell Res 1987;170:235)
- Mesothelium (Exp Cell Res 1987;170:235)
- Pancreatic ducts (Am J Ophthalmol 2013;156:830)
- Salivary gland: acini and intercalated ducts (Am J Surg Pathol 2009;33:1322, Mod Pathol 2004;17:803)
- Rete testes (Appl Immunohistochem Mol Morphol 2016;24:e50)
- Thyroid epithelium
- Toker cells (Am J Dermatopathol 2005;27:185)
- Trophoblast (J Immunol Methods 2004;286:21)
- Urothelium (Exp Cell Res 1987;170:235, Eur J Cell Biol 2004;83:27)
Positive staining - not malignant
- Barrett esophagus (Mod Pathol 2002;15:611)
- Cervix: high grade squamous intraepithelial lesions (HSIL / CIN 2 - 3) (Proc Natl Acad Sci USA 2012;109:10516)
- Cystitis glandularis (bladder) of usual type (Mod Pathol 2006;19:1395)
- Ependymoma: extra-axial (80%), minor subset of CNS (10%) (Am J Surg Pathol 2008;32:710)
- Eye: Fuchs endothelial dystrophy (Cornea 2006;25:956)
- Liver: bile duct adenoma, mesenchymal hamartoma, hepatocytes in chronic allograft rejection (Am J Clin Pathol 2011;135:238)
- Lymph nodes: individual / clusters of neuroendocrine cells (Am J Surg Pathol 2010;34:1701)
- Nephrogenic adenoma of GU tract (Am J Surg Pathol 2009;33:1654)
- Pancreas: lymphoepithelial cyst (Mod Pathol 2010;23:1467)
- Salivary gland oncocytoma and lymphadenoma (Mod Pathol 2012;25:26, Laryngoscope 2005;115:1097)
Positive staining - malignant
- Anal duct carcinoma (Hum Pathol 2012;43:216)
- Appendiceal mucinous neoplasms, subset (31%) (Histopathology 2016;68:977)
- Basaloid squamous cell carcinoma of Waldeyer ring (Hum Pathol 2000;31:1096)
- Bile duct carcinoma (Pathol Res Pract 2003;199:65)
- Bladder adenocarcinoma (63%) (Appl Immunohistochem Mol Morphol 2005;13:358)
- Breast carcinoma (Ann Diagn Pathol 1999;3:350)
- Cervical adenocarcinoma (HPV related and gastric type) and squamous cell carcinoma (Mod Pathol 2000;13:962, Am J Clin Pathol 2009;132:531, Am J Surg Pathol 2016;40:636)
- Colon adenocarcinoma, small subset including those related to ulcerative colitis (59%) and some rectal adenocarcinoma; also see above as CK7 expression relates to prognostication of some colorectal adenocarcinomas (Am J Surg Pathol 2011;35:1830, Virchows Arch 2006;448:756)
- Endometrial adenocarcinoma (Int J Gynecol Pathol 2002;21:4)
- Esophageal adenocarcinoma (Am J Surg Pathol 2002;26:1213)
- Gastric adenocarcinoma (71%) (Hum Pathol 2004;35:576)
- Hepatocellular carcinoma, subset (10 - 34%), particularly scirrhous and fibrolamellar types and those in patients ≤ 30 years (Am J Clin Pathol 2005;124:512, Histopathology 2005;47:382, Int J Surg Pathol 2010;18:313, Mod Pathol 2006;19:460)
- Lung: adenocarcinoma and primary pulmonary mucoepidermoid carcinoma (PLoS One 2015;10:e0143169, Hum Pathol 2006;37:542)
- Merkel cell carcinoma, subset (23%); it is also noted that CK7-/CK20- negative Merkel cell carcinomas have been described (Appl Immunohistochem Mol Morphol 2000;8:310, Am J Dermatopathol 2017;39:208)
- Mesothelioma, pleural and peritoneal (Cancer. 2001;92:2727, Arch Pathol Lab Med 2018;142:236)
- Ovarian endometrioid, clear cell, serous and seromucinous carcinoma and most primary mucinous carcinoma (74%) (Am J Surg Pathol 2006;30:1130, Am J Surg Pathol 2015;39:983, Am J Surg Pathol 2004;28:1499)
- Ovarian carcinoid, subset (24%); Sertoli cell tumors, small subset (13%) (Am J Surg Pathol 2007;31:255)
- Paget disease, mammary and extramammary (breast, anal, vulvar and esophageal), except vulvar secondary to anorectal carcinoma (Am J Surg Pathol 1998;22:170, Hum Pathol 2002;33:545, Am J Surg Pathol 2008;32:1068)
- Pancreatic adenocarcinoma, including intestinal type (Ann Diagn Pathol 2007;11:3, Arch Pathol Lab Med 2000;124:1196)
- Renal cell carcinoma (chromophobe, papillary, clear cell papillary, collecting duct types) (Arch Pathol Lab Med 2012;136:410)
- Salivary gland carcinoma (Mod Pathol 2004;17:407)
- Sebaceous carcinoma (Am J Dermatopathol 2015;37:809)
- Sinonasal adenocarcinoma, including subset of SMARCB1 (INI-1) deficient sinonasal carcinoma (48%) (Am J Surg Pathol 2017;41:458, Ann Otol Rhinol Laryngol 2006;115:59, Head Neck Pathol 2016;10:68)
- Small intestinal adenocarcinoma (Am J Surg Pathol 2004;28:1352)
- SMARCA4 deficient pulmonary adenocarcinoma (CK7 +, TTF-1 -, HepPar1 +) (Virchows Arch 2017;471:599)
- Synovial sarcoma (many) (Mod Pathol 2006;19:659)
- Thyroid carcinoma (Appl Immunohistochem Mol Morphol 2000;8:189)
- Urothelial carcinoma (Arch Pathol Lab Med 2001;125:921, Hum Pathol 2002;33:1136)
- Yolk sac tumors of somatic derivation, tumors of germ cell derivation usually negative) (Histopathology 2016;69:739)
Negative staining - normal
- Blood vessels (Exp Cell Res 1987;170:235)
- Cervical squamous epithelium
- Connective tissue
- Gastrointestinal epithelium (including esophagus, stomach, small intestine and colon)
- Hepatocytes
- Kidney: glomeruli and proximal tubules
- Prostate acinar and basal cells
- Skin (stratified squamous epithelium)
Negative staining - tumor / disease
- Adrenocortical carcinoma and adenoma (Hum Pathol 2002;33:1136)
- Ameloblastoma, including with adenoid features (Acta Histochem 2018;120:468)
- Endometrial stromal sarcoma (high grade or low grade) (Hum Pathol 2008;39:1459)
- Germ cell tumors, seminoma, embryonal carcinoma and yolk sac tumor (Am J Surg Pathol 2004;28:1499, Mod Pathol 2000;13:962)
- Kidney: carcinoid (may have focal staining, clear cell renal cell carcinoma (usually), oncocytoma (Am J Surg Pathol 2007;31:1539)
- Nasal cavity: nonkeratinizing squamous cell carcinoma and nasopharyngeal type undifferentiated carcinoma (Am J Surg Pathol 2002;26:1597)
- Ovarian mucinous carcinoma with pseudomyxoma ovarii (suggesting teratomatous derivation) (Am J Surg Pathol 2007 Jun;31:854)
- Pituitary adenoma (Endocr Pathol 2005;16:201)
- Prostate adenocarcinoma but prostatic mucin producing urothelial type carcinoma is usually CK7+ (83%) (Am J Surg Pathol 2007;31:1323, Mod Pathol 2000;13:962)
- Squamous cell carcinoma (most cases are negative with exception of cervical squamous cell carcinoma and subsets of cutaneous and head and neck squamous cell carcinomas, see above) (Mod Pathol 2000;13:962)
Sample pathology report
- Skin, shoulder, biopsy:
- Metastatic adenocarcinoma, consistent with breast origin (see comment)
- Comment: Immunohistochemical staining demonstrates diffuse tumor positivity for CK7, GATA3, ER and PR and negativity for CK20, TTF-1, WT-1 and Pax-8. The morphologic and immunophenotypic findings are consistent with metastatic breast adenocarcinoma. Clinical correlation is recommended.
- Vulva, biopsy:
- Intraepidermal adenocarcinoma, consistent with Paget disease (see comment)
- Comment: Histologic sections demonstrate atypical epithelioid cells with prominent nucleoli and clear-to-pale cytoplasm exhibiting intraepidermal growth in a pagetoid-like fashion. No dermal invasion is identified. Immunohistochemical studies show the cells to be positive for CK7, CAM5.2 and HER2 while negative for SOX10, p63, CK5/6, CK20 and adipophilin. The morphologic and immunophenotypic findings are consistent with primary Paget disease of the vulva. Clinical correlation is recommended to exclude metastasis from an extracutaneous site.
Board review style question #1
A 54 year old woman presents with a 10 cm right ovarian mass. Histology demonstrates a mucinous carcinoma and the tumor cells are negative for CK7 and positive for CK20. Which of the following tumors is most likely to demonstrate this immunohistochemical profile?
- Metastatic breast adenocarcinoma
- Metastatic cervical adenocarcinoma
- Metastatic colonic adenocarcinoma
- Metastatic gastric adenocarcinoma
- Primary ovarian mucinous carcinoma
Board review style answer #1
C. Adenocarcinoma of the colon is most often CK7- / CK20+. Breast carcinoma is usually CK7+ / CK20-, cervical adenocarcinoma is usually CK7+ / CK20-, gastric carcinoma can be either CK7+ / CK20- (majority) or CK7+ / CK20+ and primary ovarian mucinous carcinoma is either CK7+ / CK20+ or CK7+ / CK20 variable (although lower GI type mucinous tumors arising in teratoma can be CK7-).
Comment Here
Reference: Cytokeratin 7 (CK7, K7)
Comment Here
Reference: Cytokeratin 7 (CK7, K7)
Board review style question #2
Which of the following is the best immunohistochemical marker for the diagnosis of primary, extramammary Paget disease?
- CK7
- CK20
- p63
- SOX10
- Uroplakin
Board review style answer #2
A. Of the above, CK7 is the best screening marker for primary, extramammary Paget disease. Sox10 would be positive in a melanocytic lesion (i.e. melanoma in situ), p63 positive in squamous cell carcinomas or primary adnexal neoplasms and uroplakin is positive in pagetoid urothelial intraepithelial neoplasia (PUIN). CK20 could be expressed in either metastatic colorectal adenocarcinoma or intraepidermal Merkel cell carcinoma (demonstrating perinuclear dot-like positivity).
Comment Here
Reference: Cytokeratin 7 (CK7, K7)
Comment Here
Reference: Cytokeratin 7 (CK7, K7)
Board review style question #3
Which staining pattern would most likely be appreciated in chromophobe renal cell carcinoma?
- CK7-/c-Kit-/Hale’s Colloidal Iron-
- CK7+/c-Kit-/Hale’s Colloidal Iron-
- CK7+/c-Kit+/Hale’s Colloidal Iron-
- CK7+/c-Kit+/Hale’s Colloidal Iron+
Board review style answer #3
D. Classically, chromophobe renal cell carcinoma would be positive for CK7, c-Kit (or CD117) and Hale’s colloidal iron. Oncocytoma may demonstrate scattered CK7 positivity while conventional clear cell RCC is usually CK7 negative. Additionally, chromophobe RCC can stain diffusely for Hale’s colloidal iron while oncocytoma may show apical, non-diffuse staining. It must also be noted that, despite the above immunohistochemical studies, the distinction between different oncocytic / eosinophilic neoplasms can often be challenging as many of the entities may demonstrate significant morphologic overlap.
Comment Here
Reference: Cytokeratin 7 (CK7, K7)
Comment Here
Reference: Cytokeratin 7 (CK7, K7)