Table of Contents
Definition / general | Uses by pathologists | Microscopic (histologic) images | Positive staining - normal | Positive staining - not malignant | Positive staining - malignant | Negative stainingCite this page: Pernick N. Cytokeratin 20 (CK20, K20). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsCK20.html. Accessed March 31st, 2025.
Definition / general
- Epithelial marker (MW 46 kDa) with restricted expression compared to CK7 (OMIM #608218)
Uses by pathologists
- General patterns (specificity varies)
- CK7+ / CK20+ in carcinomas of bile duct (extrahepatic / gallbladder, often, Pathol Res Pract 2003;199:65), lung-mucinous bronchioloalveolar (Am J Clin Pathol 2004;122:421), pancreas (Cancer 2006;106:693, but see Arch Pathol Lab Med 2000;124:1196)
- Urothelium (often, Arch Pathol Lab Med 2001;125:921, Hum Pathol 2002;33:1136)
- Also primary mucinous tumors of ovary (74%), upper GI tract (78%) and endocervix (88%, Am J Surg Pathol 2006;30:1130)
- CK7+ / CK20- in carcinomas of bile duct (intrahepatic, Pathol Res Pract 2003;199:65), breast (Ann Diagn Pathol 1999;3:350), endocervical and endometrial adenocarcinoma (Pathol Res Pract 2003;199:65), esophagus (distal, Am J Surg Pathol 2002;26:1213), lung (not mucinous bronchioloalveolar, BMC Cancer 2006;6:31), salivary gland (Pathol Int 2005;55:386), thyroid (Appl Immunohistochem Mol Morphol 2000;8:189)
- Also mesothelioma (Cancer 2001;92:2727)
- CK7- / CK20+ in carcinoma of colon (particularly early stage, Hum Pathol 2005;36:275)
- CK20 is less sensitive for poorly differentiated colonic carcinoma (Chin J Physiol 2006;49:298)
- Primary mucinous tumors of lower GI tract (79%, Am J Surg Pathol 2006;30:1130) and primary bladder adenocarcinomas (29%, Am J Surg Pathol 2001;25:1380)
- CK7- / CK20- in carcinomas of adrenal cortex and prostate (Mod Pathol 2000;13:962)
- To distinguish primary lung carcinoma (CK7+ / CK20-) from metastatic colonic carcinoma to lung (CK7- / CK20+, BMC Cancer 2006;6:31)
- To help distinguish colon carcinoma (80% are CK20+) and poorly differentiated prostatic carcinoma (90% are CK20-) at biopsy (Arch Pathol Lab Med 2007;131:599)
- To distinguish Merkel cell carcinoma (CK20+, dot-like, TTF1-) and metastatic small cell carcinoma of lung (CK20-, TTF1+, Am J Dermatopathol 2006;28:99)
- To distinguish anal carcinoma (CK7+ / CK20-) from downward growth of colorectal carcinoma (CK7- / CK20+, Arch Pathol Lab Med 2001;125:1074)
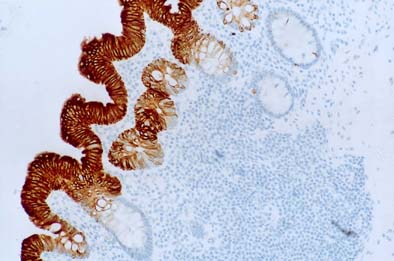
- May confirm Barrett’s mucosa, which has strong diffuse CK7+ surface and crypt epithelium, strong CK20+ surface and superficial crypt staining
- Interpretation is affected by fixative (Hum Pathol 2005;36:58, but see Mod Pathol 2002;15:611)
- Pattern may help distinguish short segment Barrett’s from cardiac intestinal metaplasia (World J Gastroenterol 2005;11:6360)
- To distinguish Rathke cleft cysts and pituitary gland pars intermedia (CK8+, CK20+) from craniopharyngioma (CK8-, CK20-, Arch Pathol Lab Med 2002;126:1174)
- To distinguish adenocarcinoma of distal esophagus (CK7+ / CK19+: 90%, CK7+ / CK20-: 74%) from proximal stomach (CK7+ / CK19+: 44%, CK7+ / CK20-: 24%, Am J Surg Pathol 2002;26:1213)
- To detect occult nodal tumor cells in colorectal adenocarcinoma (Hum Pathol 2006;37:1259, Br J Cancer 2006;95:218)
- RT-PCR to detect tumor cells of breast and colorectal carcinoma in blood (J Mol Diagn 2006;8:105)
- RT-PCR assessment in peritoneal wash may predict recurrence in gastric carcinoma (Oncol Rep 2007;17:667)
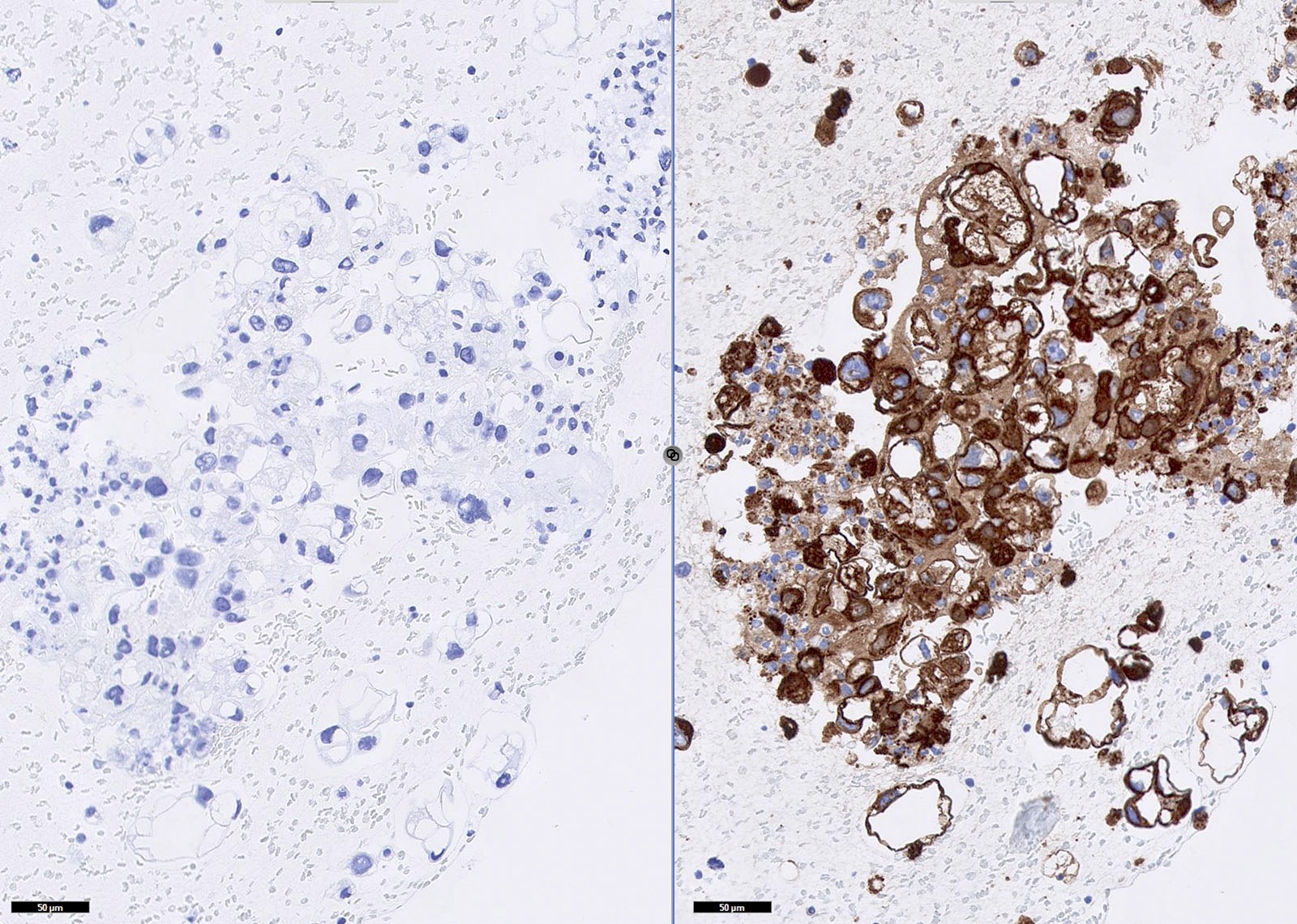
Urothelial carcinoma:- CK20+ p53+ CD44- favors urothelial carcinoma in situ vs. reactive urothelium (Am J Surg Pathol 2001;25:1074)
- CIS shows CK20 staining of deep urothelial cells compared with surface cells only in non-neoplastic lesions (Appl Immunohistochem Mol Morphol 2006;14:260)
- CK20+ in voided urine by RT-PCR is sensitive and specific for bladder carcinoma (Clin Biochem 2004;37:803, J Egypt Natl Canc Inst 2006;18:82, but see J Urol 2003;169:86)
- In papillary urothelial neoplasms, CK20+ is associated with increasing tumor grade and stage in pTa and pT1 patients (Mod Pathol 2000;13:1315)
Microscopic (histologic) images
Positive staining - normal
- Colon, Merkel cells, small intestine (Am J Surg Pathol 2004;28:1352) and stomach
- Urothelium (umbrella cells, Am J Surg Pathol 2001;25:1074)
- Uterus
Positive staining - not malignant
- Bladder intestinal metaplasia (Mod Pathol 2006;19:1395)
- Fibroepithelioma of Pinkus (Am J Dermatopathol 2007;29:7)
- GI carcinoid (25%)
- Hydatidiform mole (complete-100%, partial-50%, Gynecol Oncol 2002;87:34)
- Renal oncocytoma (dot-like pattern, J Histochem Cytochem 2001;49:919)
Positive staining - malignant
- Ampullary (variable, Am J Surg Pathol 2005;29:359)
- Anal (variable-Br J Dermatol 2000;142:243, Cancer 2001;92:2045)
- Appendiceal epithelial neoplasms (benign and malignant, 100%, Hum Pathol 2005;36:1217)
- Biliary papillary tumors (benign and malignant, Hepatology 2006;44:1333)
- Colon (references above)
- Gastric (18-31%, Appl Immunohistochem Mol Morphol 2006;14:303, reduced if high levels of microsatellite instability, Am J Surg Pathol 2004;28:712)
- Hepatocellular (20% positive, Hum Pathol 2005;36:1226)
- Hepatoid adenocarcinoma (Am J Surg Pathol 2003;27:1302)
- Lung mucinous bronchioloalveolar (Hum Pathol 2002;33:915)
- Merkel cell (dot like, references above)
- Ovarian (Mod Pathol 2006;19:1421)
- Paget’s disease (secondary only, Br J Dermatol 2000;142:243)
- Pancreatic ductal (Cancer 2006;106:693)
- Prostatic (variable)
- Sinonasal adenocarcinoma (50%, (Arch Pathol Lab Med 2007;131:530)
- Small cell of major salivary glands (Am J Surg Pathol 2004;28:762), urothelial (references above)
- Vulvar Paget’s disease secondary to anorectal or urothelial carcinoma but not primary (Hum Pathol 2002;33:545)
Negative staining
- Anal glands (Arch Pathol Lab Med 2001;125:1074)
- Inverted urothelial papilloma (Hum Pathol 2004;35:1499)