Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Obeidin F, Alexiev BA. Synovial sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuesynovialsarc.html. Accessed April 1st, 2025.
Definition / general
- Malignant soft tissue tumor of uncertain histogenesis with variable epithelial differentiation
Essential features
- Can occur in or around any tissue in the body
- Multiple morphologies, including monophasic spindle cell, biphasic, poorly differentiated, myxoid, ossifying and monophasic epithelial
- Monotonous spindle cells with vesicular, plump and overlapping nuclei with hemangiopericytic vessels
- TLE1+, cytokeratin+, EMA+, BCL2+, CD99+
- Has a characteristic chromosomal translocation t(X;18)(p11;q11) involving genes SS18 and either SSX1, SSX2 or SSX4
Terminology
- Obsolete terms: malignant synovioma
ICD coding
- ICD-O: 9040/3 - synovial sarcoma, NOS
- ICD-11: 2B5A.Y & XH9B22 - synovial sarcoma, other specified primary site & synovial sarcoma, NOS
Epidemiology
- Accounts for 5 - 10% of all soft tissue sarcomas
- Median age: 35
- Age range: 0 - 85+
- Slight male predominance (M:F = 1.2:1)
- 17.6% of cases occur in children and young adults ages 0 - 19 (Pediatr Blood Cancer 2011;57:943)
Sites
- Can occur anywhere in the body
- Primary site distribution (Pediatr Blood Cancer 2011;57:943):
- Extremities: 68.7%
- Trunk: 15.7%
- Head and neck: 6.3%
- Intrathoracic: 5.3%
- Intra-abdominal: 1.8%
- Other: 2.2%
Pathophysiology
- Driven by the chromosomal translocation t(X;18)(p11;q11) involving genes SS18 and either SSX1, SSX2 or SSX4
- Translocation has multiple effects on oncogenetic pathways, including the SWI / SNF chromatin remodeling complex, polycomb repressor complex and canonical Wnt pathway (Cancer Discov 2015;5:124)
- Translocation partner affects epithelial differentiation (Int J Clin Exp Pathol 2013;6:2272):
- SS18-SSX1: 60 - 70% monophasic, 30 - 40% biphasic
- SS18-SSX2: 97% monophasic, 3% biphasic
- SS18-SSX1 inhibits Snail gene while SS18-SSX2 inhibits Slug gene (OMIM: Snail Family Transcriptional Repressor 1; SNAI1 [Accessed 9 July 2021])
- Interfering with Snail leads to stronger derepression of E-cadherin than does interfering with Slug
- Stronger E-cadherin and increased extracellular matrix protein MMP2 expression are needed for biphasic morphology to develop
Etiology
- Despite the name, the cells of origin are not synovial cells
- Histogenesis is still debated
- 1 study has shown stem cell marker expression, suggesting that origin may be a multipotent mesenchymal stem cell (Stem Cells 2010;28:1119)
- 1 study using mice identified satellite cells (immature myoblasts) as a potential source (Cancer Cell 2007;11:375)
Clinical features
- Very rarely associated with prior radiation therapy (Mod Pathol 2002;15:998)
- Not classically known to be associated with any syndromes
Diagnosis
- Biopsy is required for definitive diagnosis
- Diagnosis confirmed by molecular or cytogenetic testing for SS18-SSX fusion; commonly used methods include FISH, RT-PCR and NGS (Cancer Res 2002;62:135, Genes Chromosomes Cancer 2001;30:1)
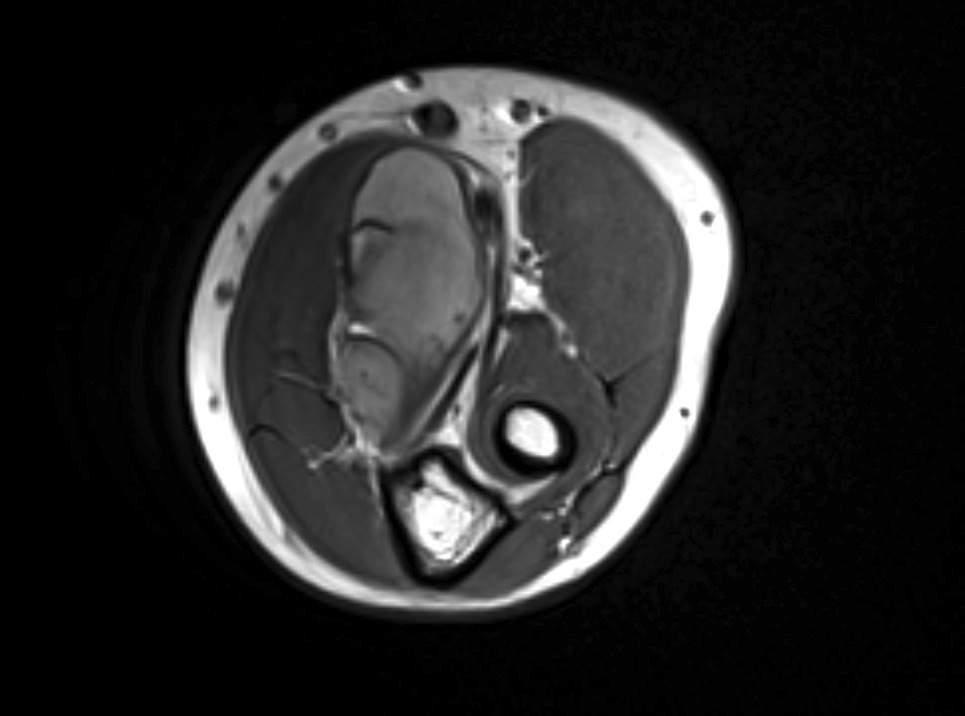
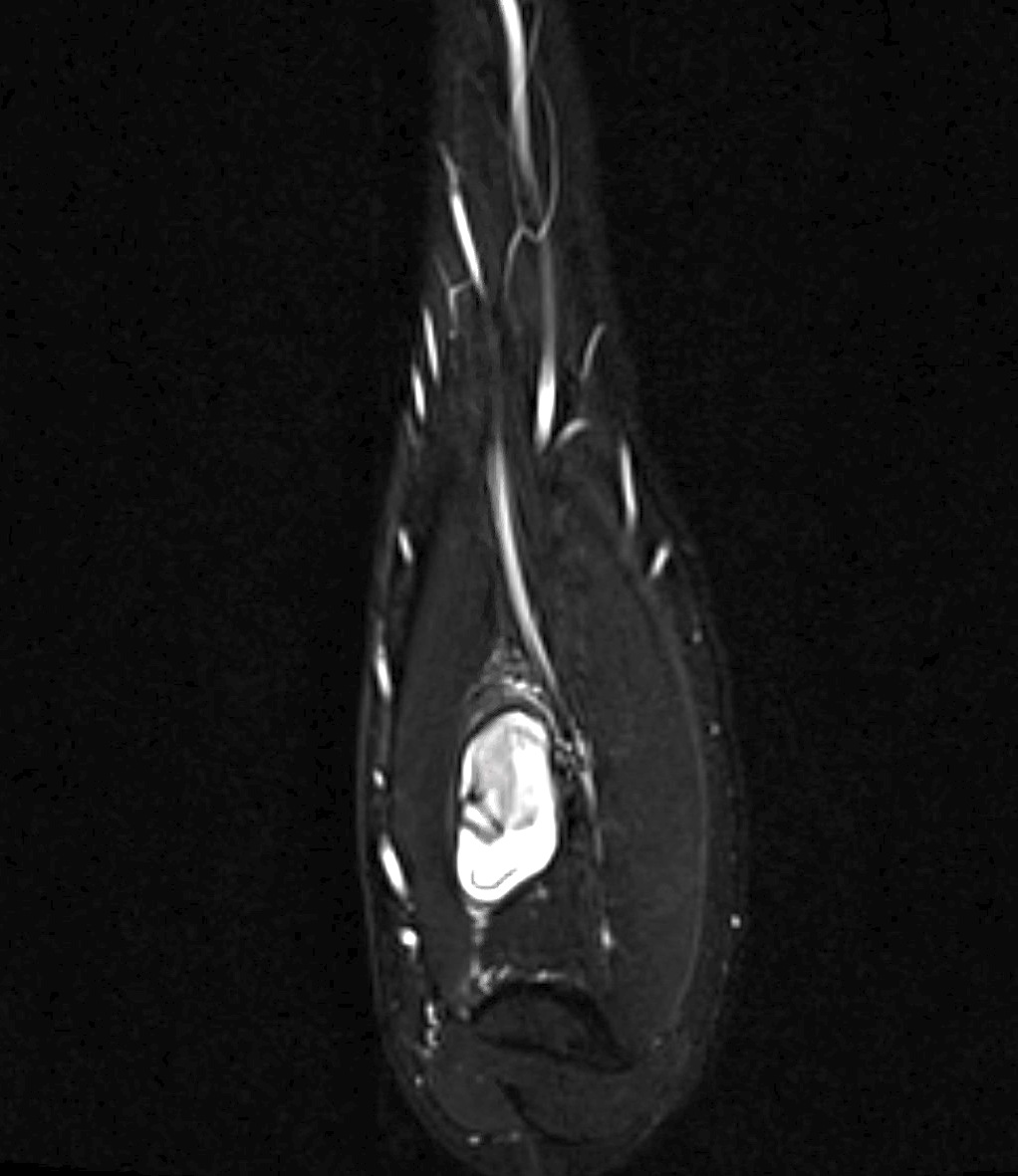
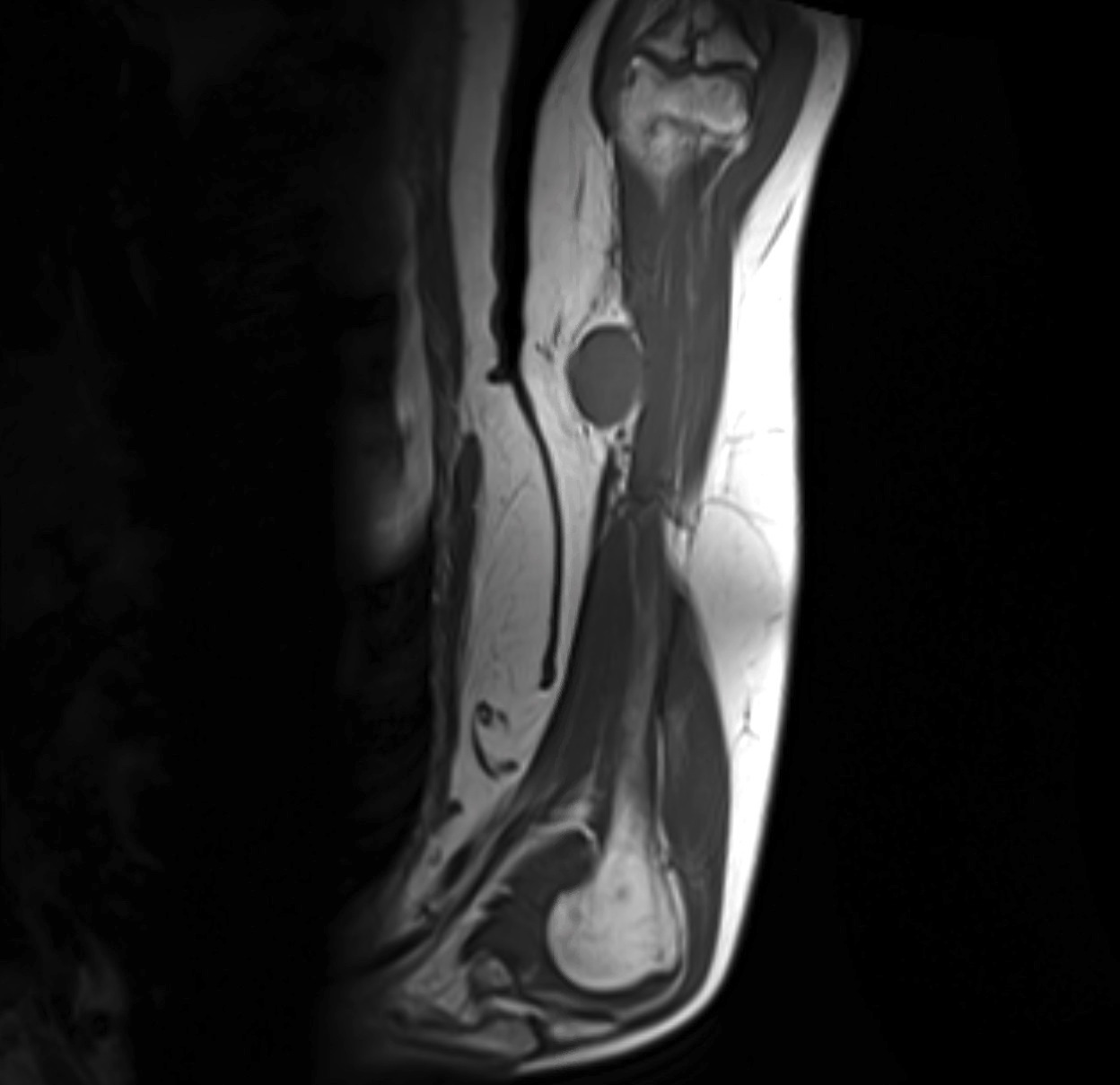
Radiology description
- Most present as round to oval, lobulated masses
- Bone involvement is rare
- Ossifying synovial sarcomas have characteristic spotty radiopacities caused by focal calcifications (Pathol Res Pract 2009;205:195)
Prognostic factors
- Poor prognostic factors:
- SS18-SSX1 translocation
- Monophasic and poorly differentiated subtypes (Cancer Med 2014;3:1404)
- Male gender (J Surg Oncol 2015;111:158)
- Older age at diagnosis (Br J Cancer 2015;113:1602)
- Size ≥ 5 cm (Cancer 2009;115:2988)
- Nonextremity location (Cancer 2009;115:2988)
- Deep seated tumors (Ann Surg Oncol 2013;20:73)
- Higher percentage of tumor necrosis (Am J Clin Oncol 2004;27:113)
- Mitotic activity ≥ 10/high power field or higher Ki67 activity (J Cancer Res Ther 2014;10:73)
- Tumor grade based on Fédération Nationale des Centres de Lutte Contre le Cancer (FNCLCC) (J Clin Oncol 2004;22:4040)
- Immunohistochemical expression of CXCR4 and IGF1R (Orphanet J Rare Dis 2015;10:6)
- Positive surgical margins
- H3K27me3 and VEGF expression associated with histologic grade, distant metastasis and stage (Pathol Res Pract 2018;214:974)
- Grading:
- In adults: grade based on FNCLCC
- In children: new grading system by the Pediatric Oncology Group (POG) for nonrhabdomyosarcoma soft tissue sarcoma in children showed discrepant higher grading for synovial sarcoma compared with FNCLCC
Case reports
- 11 year old girl with left popliteal fossa mass arising from her tibial nerve (Rare Tumors 2018;10:2036361318776495)
- 17 year old boy with a retroperitoneal mass (JRSM Open 2018;9:2054270418760437)
- 31 year old woman with a left forearm nodule (Am J Dermatopathol 2018;40:772)
- 35 year old man with a mass on the left lateral border of the tongue (Ann R Coll Surg Engl 2018;100:e118)
- 37 year old woman with a large mediastinal mass (J Cancer Res Ther 2018;14:682)
Treatment
- Primarily surgical
- Radiotherapy and adjuvant chemotherapy have been evaluated in high risk situations (tumors > 5 cm or difficult to resect)
- Radiation therapy: adjuvant use has shown improvement in oncologic outcome and overall survival (J Surg Oncol 2015;111:158)
- Adjuvant chemotherapy:
- Data is conflicting on its use but can be considered in high risk patients
- Ifosfamide was shown to increase disease specific survival (Ann Surg 2007;246:105)
- 2 large European Organization for Research and Treatment of Cancer (EORTC) database clinical trials showed no benefit of doxorubicin on overall survival (Ann Oncol 2014;25:2425)
- Novel therapies:
- Initial PDL1 and CTLA4 studies have shown no benefit (Sarcoma 2013;2013:168145)
- Receptor tyrosine kinase inhibitor pazopanib has a promising trend toward better overall survival
- Tazemetostat, an EZH2 inhibitor, has also been studied in INI1 deficient tumors, including synovial sarcoma (Curr Treat Options Oncol 2018;19:13)
- Early studies on T cell receptor based immunotherapy directed towards NY-ESO-1 in HLA-A*0201+ patients have demonstrated radiological and clinical benefit (J Clin Oncol 2011;29:917)
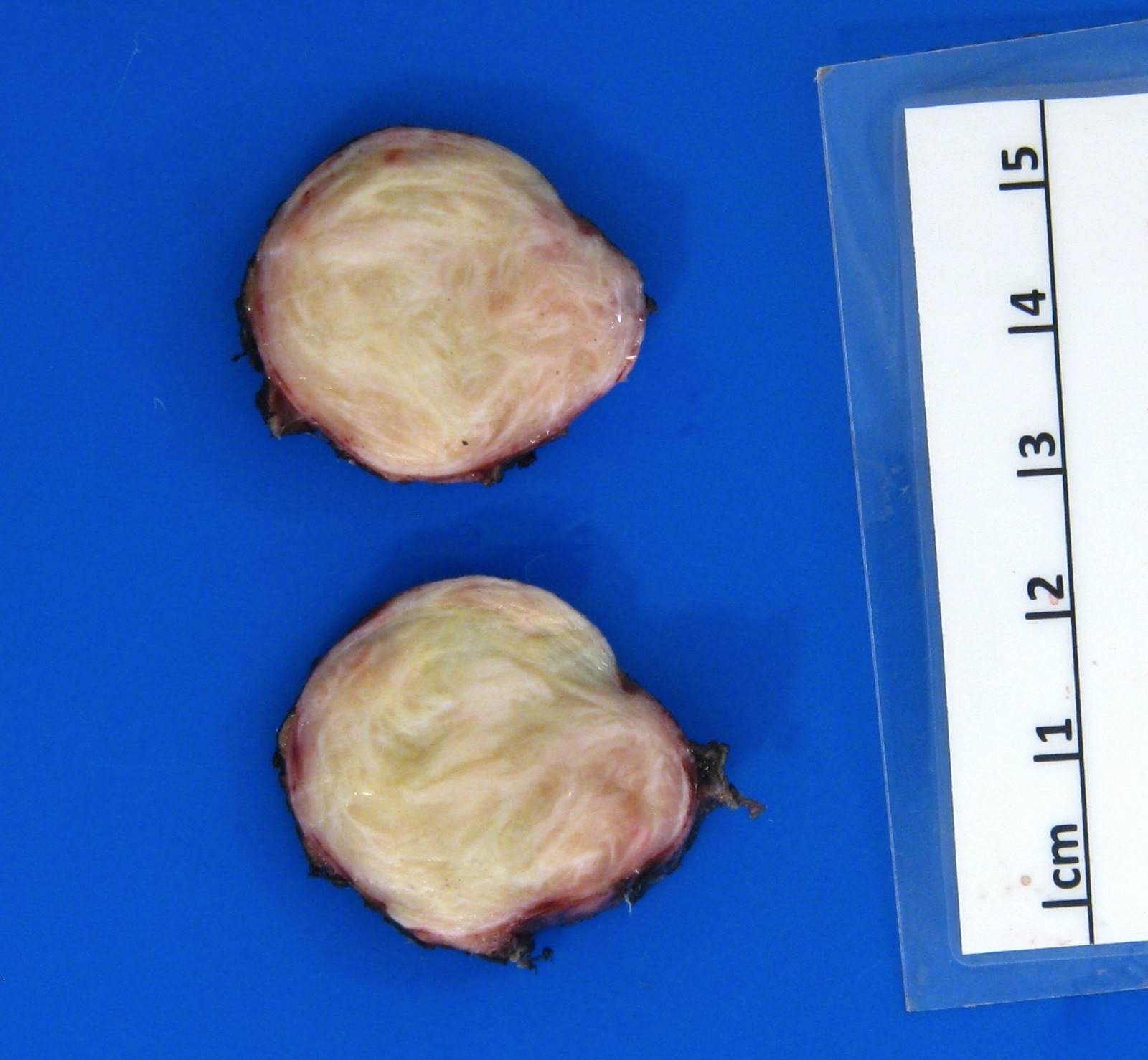
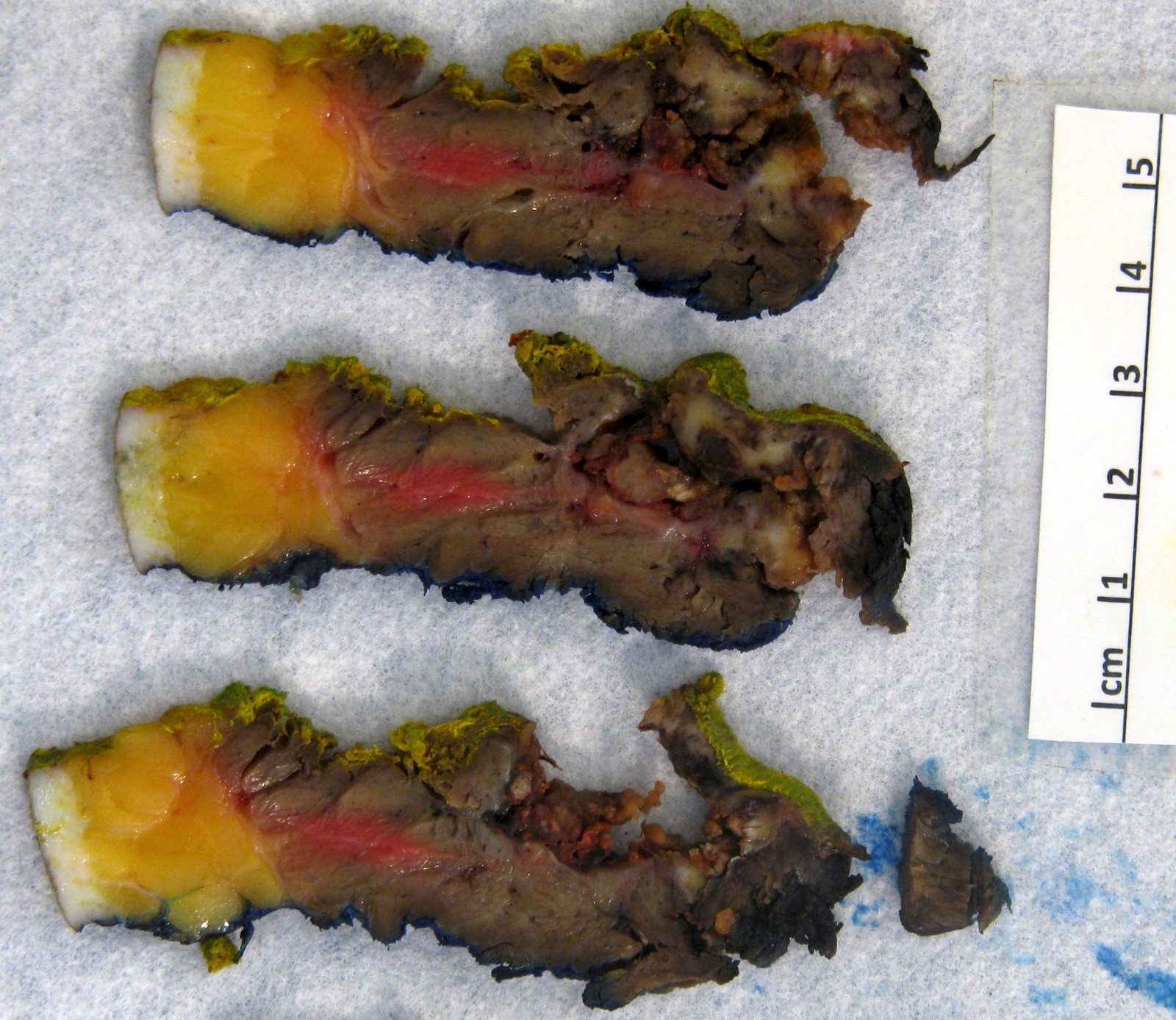
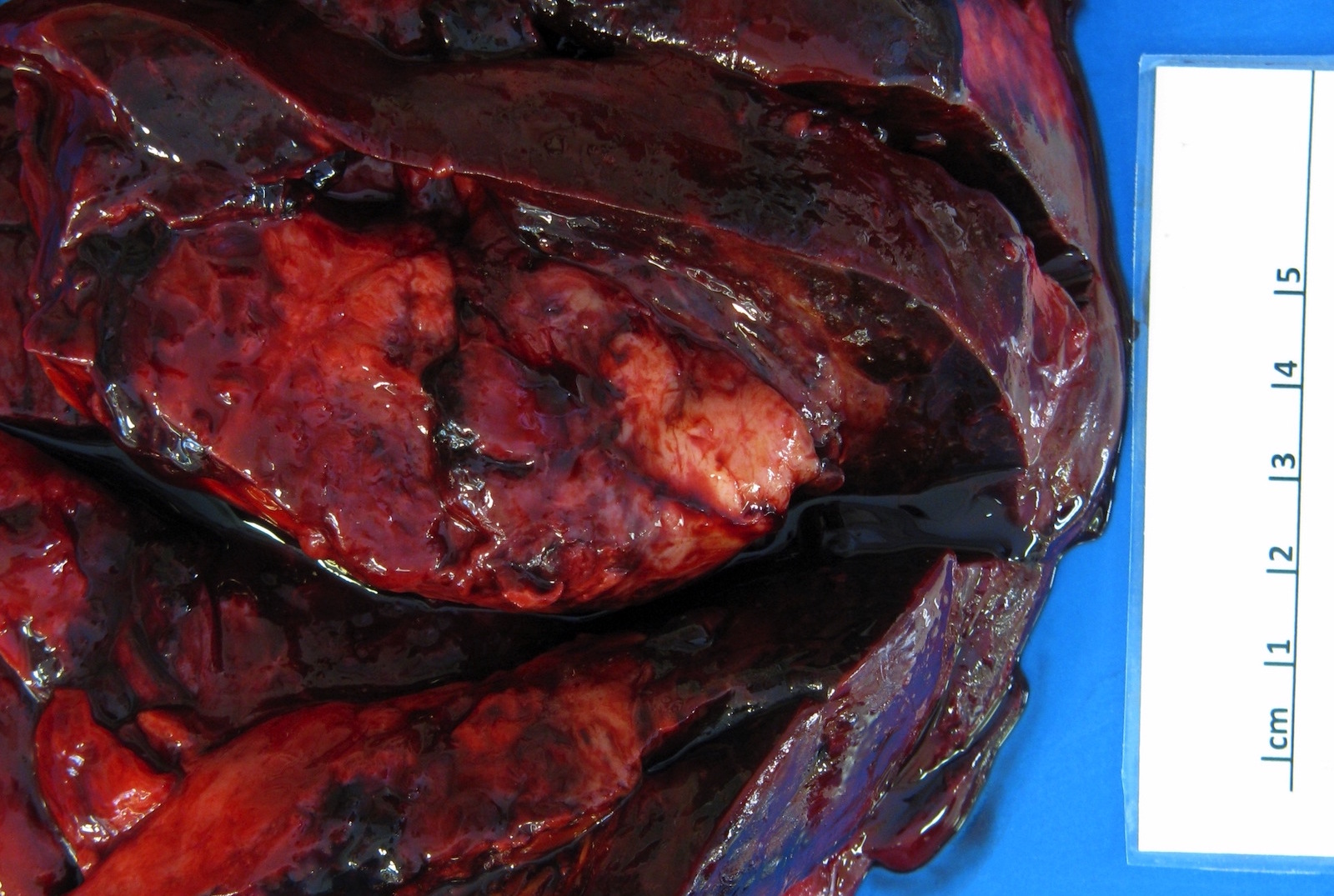
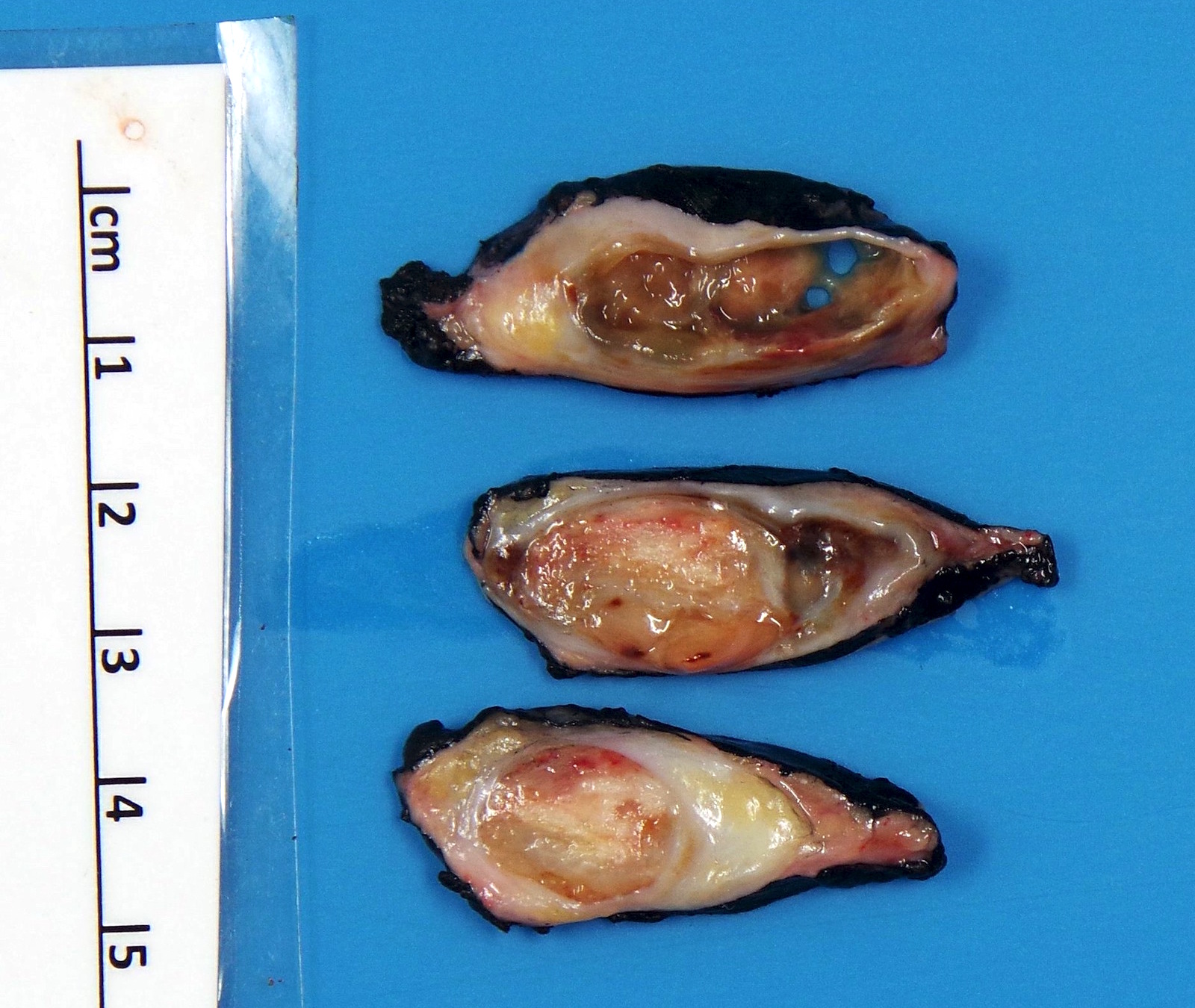
Gross description
- Tumor is well circumscribed and frequently multinodular
- Most tumors are 3 - 10 cm in greatest dimension at time of diagnosis
- Minute lesions (< 1 cm) occur, especially in hands and feet (Am J Surg Pathol 2006;30:721)
- Cut surface may be tan or grey, yellow or pink and soft or firm (Pathol Annu 1980;15:309)
- Myxoid change, necrosis, calcifications and metaplastic ossification may be present
Gross images
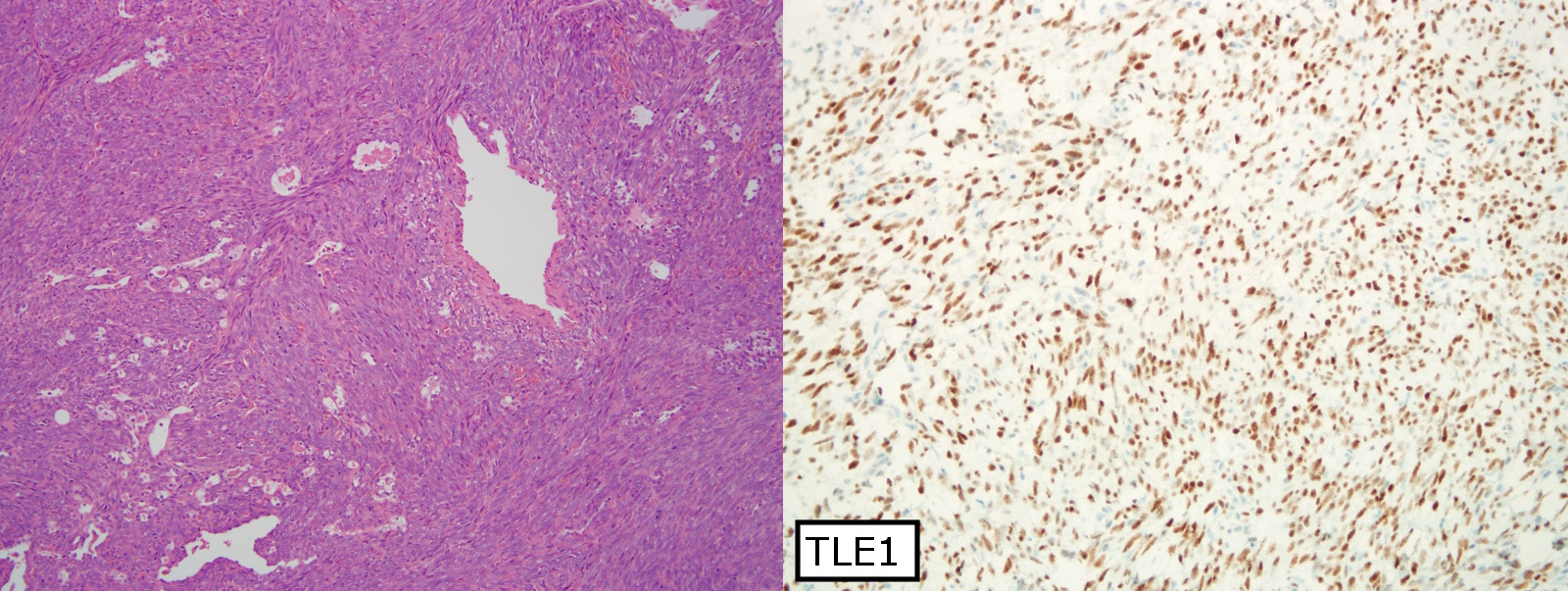
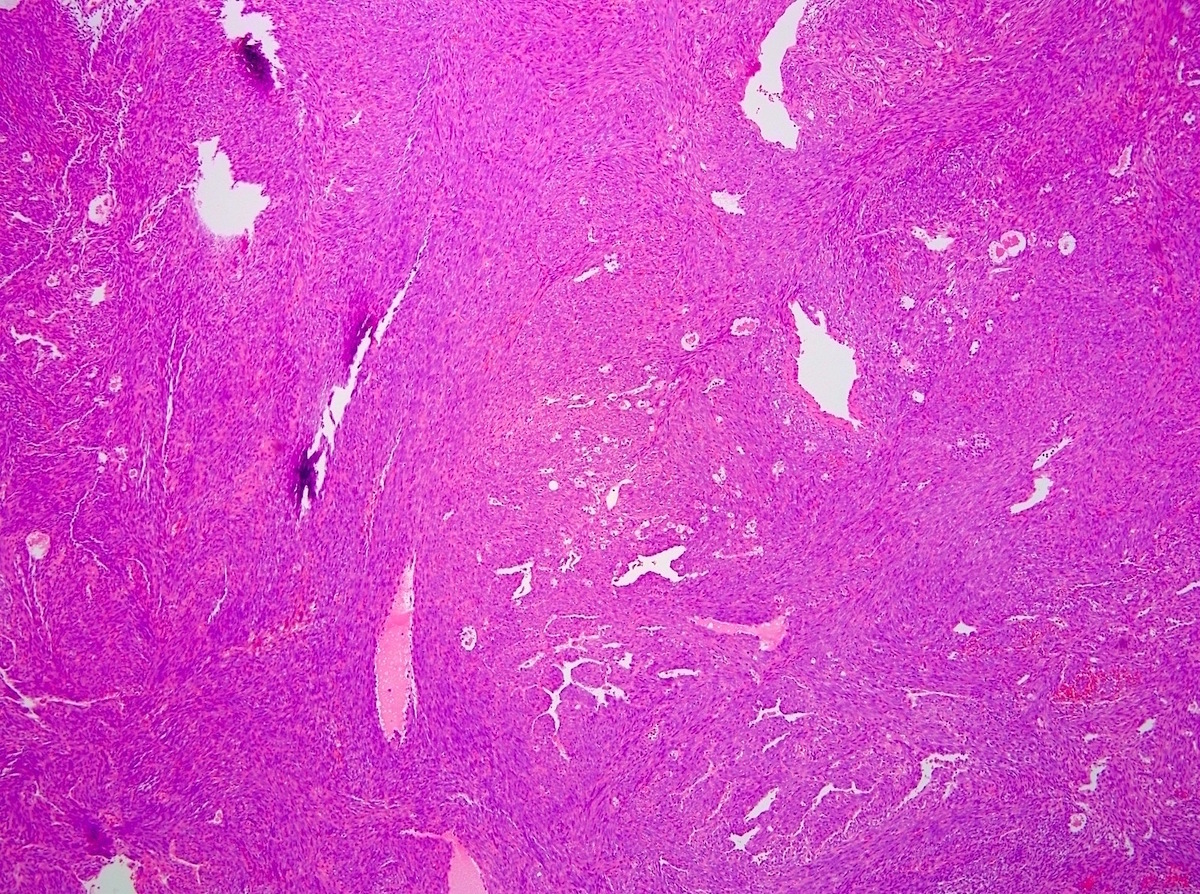
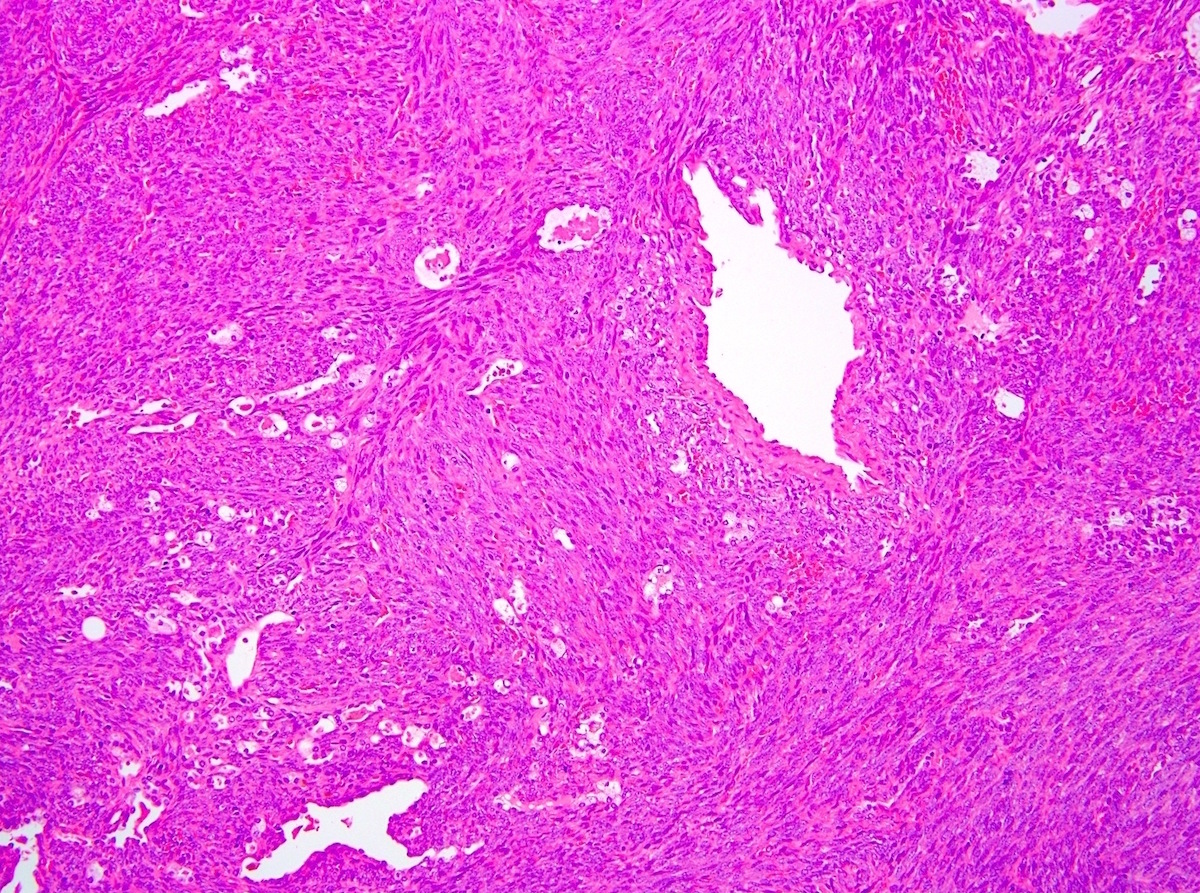
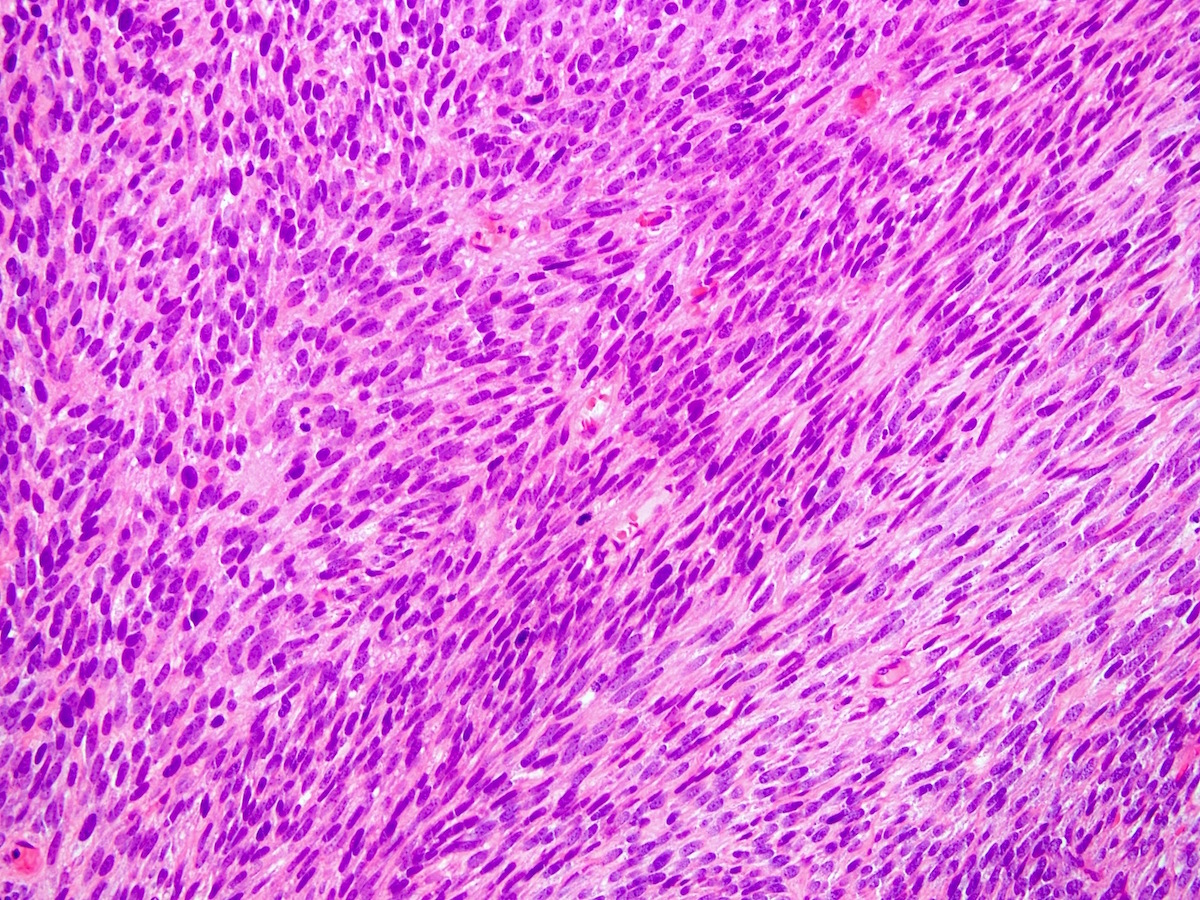
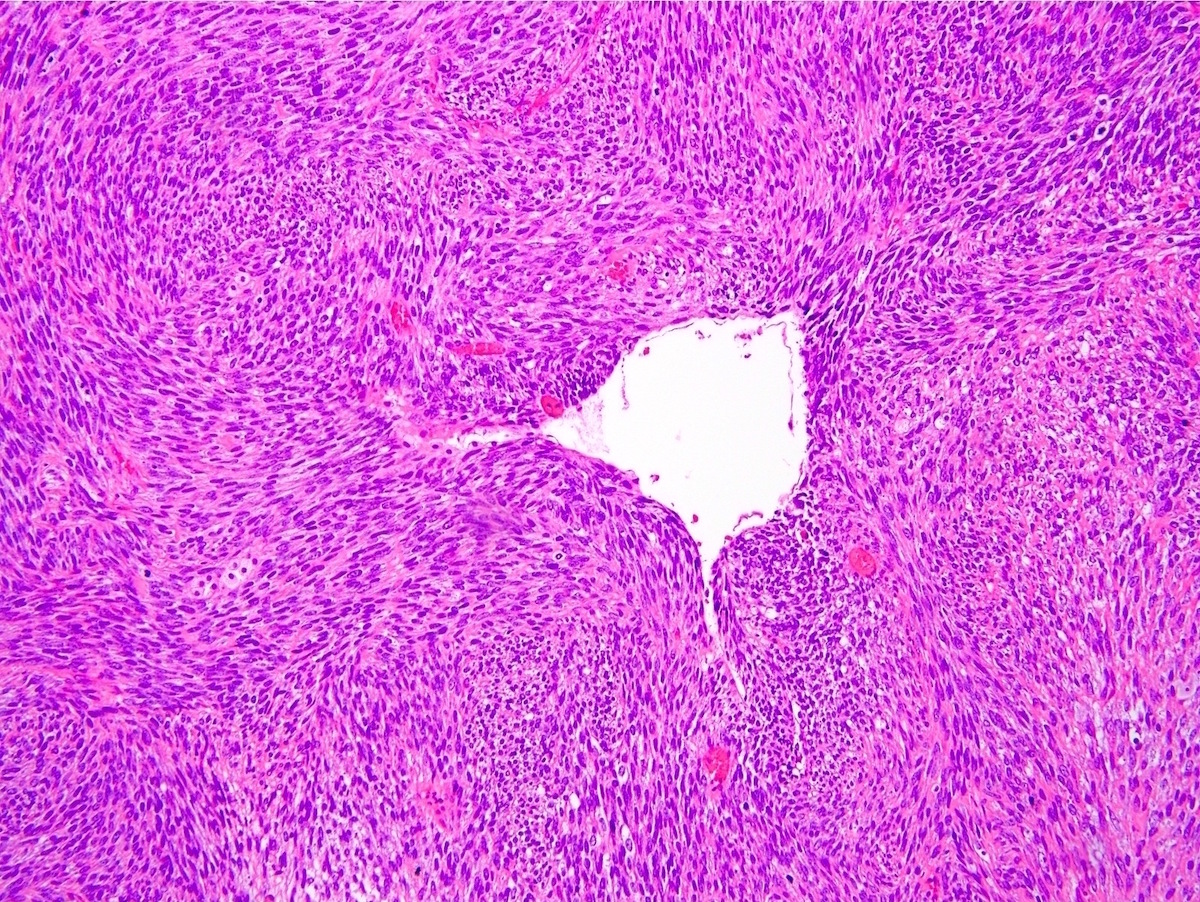
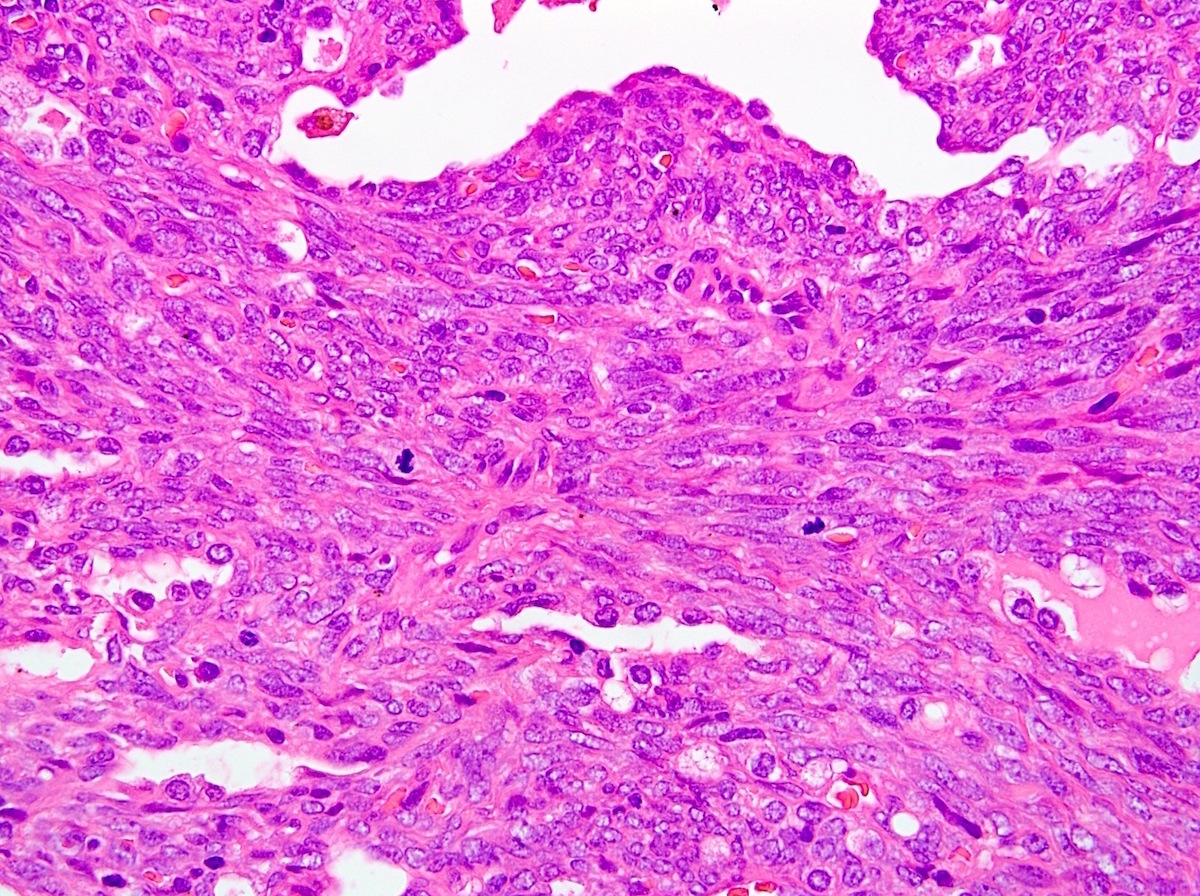
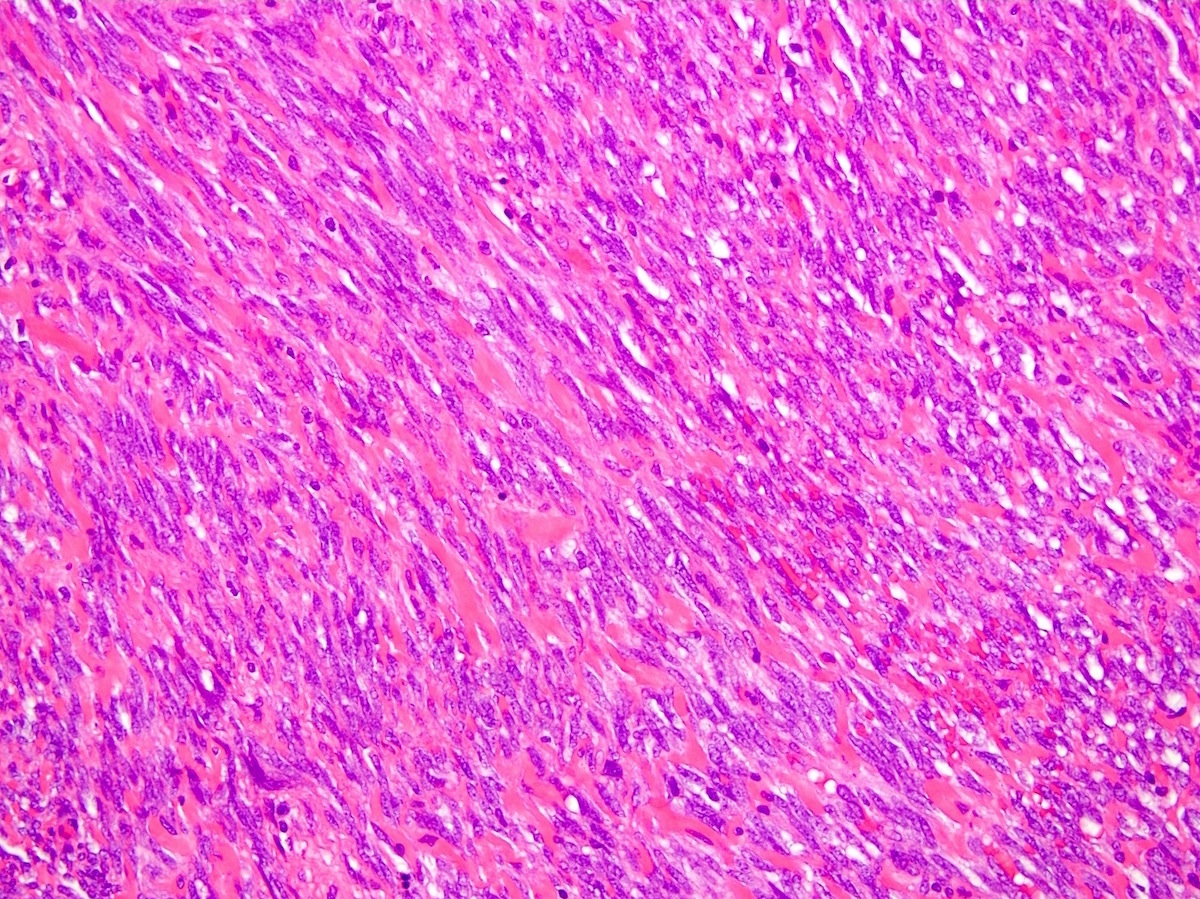
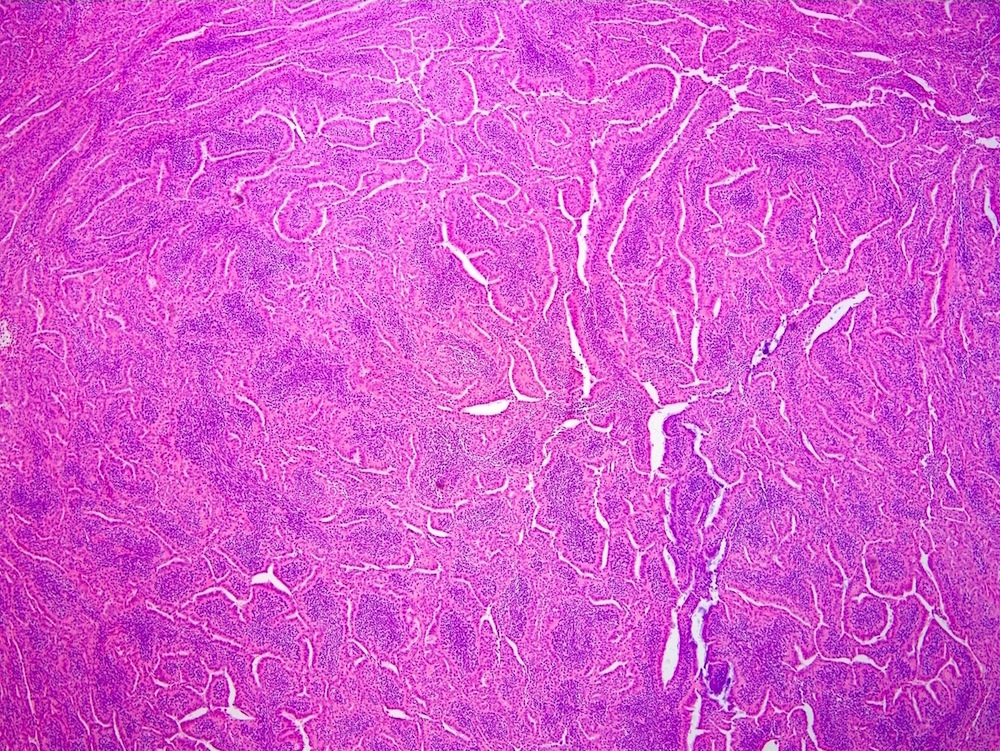
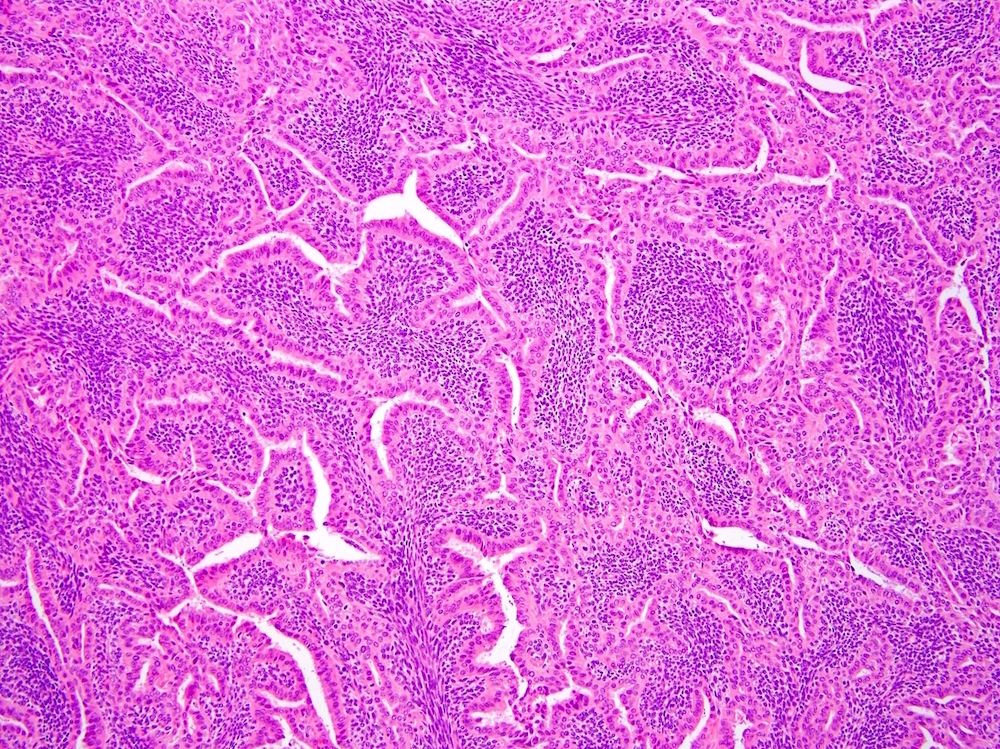
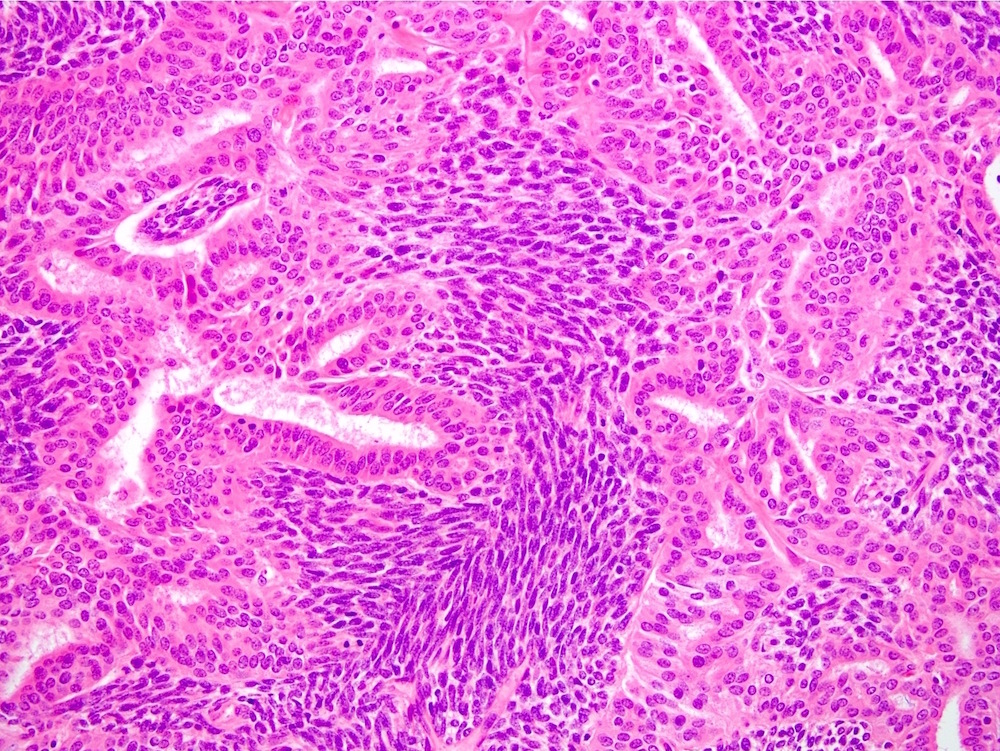
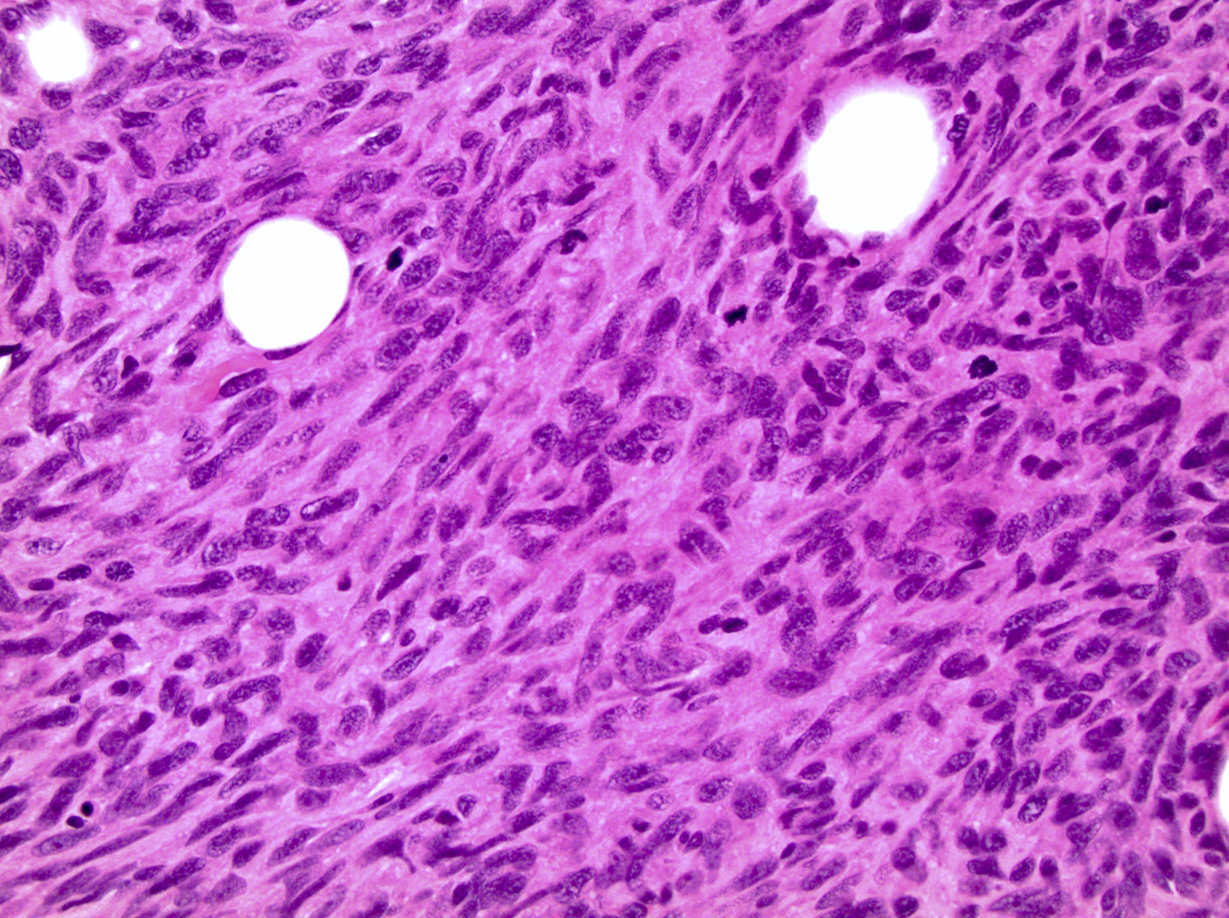
Microscopic (histologic) description
- General (Ann Diagn Pathol 2014;18:369):
- 2 main subtypes: biphasic and monophasic spindle cell
- Rarer subtypes: poorly differentiated (round cell), monophasic epithelial, calcifying / ossifying and myxoid
- Biphasic:
- Architecture:
- 2 components: spindle cells and gland-like epithelial structures
- Glandular lumina contain mucin
- Cytologic features:
- Epithelial component has moderate, distinct amphophilic cytoplasm with round to ovoid nuclei
- Rarely, squamous metaplasia can occur
- Architecture:
- Monophasic:
- Architecture:
- Infiltrative borders
- Hypercellular fascicular architecture with little intervening stroma
- Can rarely show hyalinization or myxoid change
- Ill defined nuclear palisading may be seen
- Cytologic features:
- Monotonous cells with scant amphophilic cytoplasm, ovoid to spindled vesicular nuclei with evenly dispersed chromatin and inconspicuous nucleoli
- Nuclei often close enough to overlap with adjacent nuclei
- Architecture:
- Poorly differentiated: highly cellular round cells with hyperchromatic nuclei and frequent mitotic activity and necrosis
- Additional features:
- Characteristically features focal staghorn (or hemangiopericytic), branching vascular pattern, reminiscent of solitary fibrous tumor
- Mast cells are common
- Focal calcification can be seen in 33% of cases
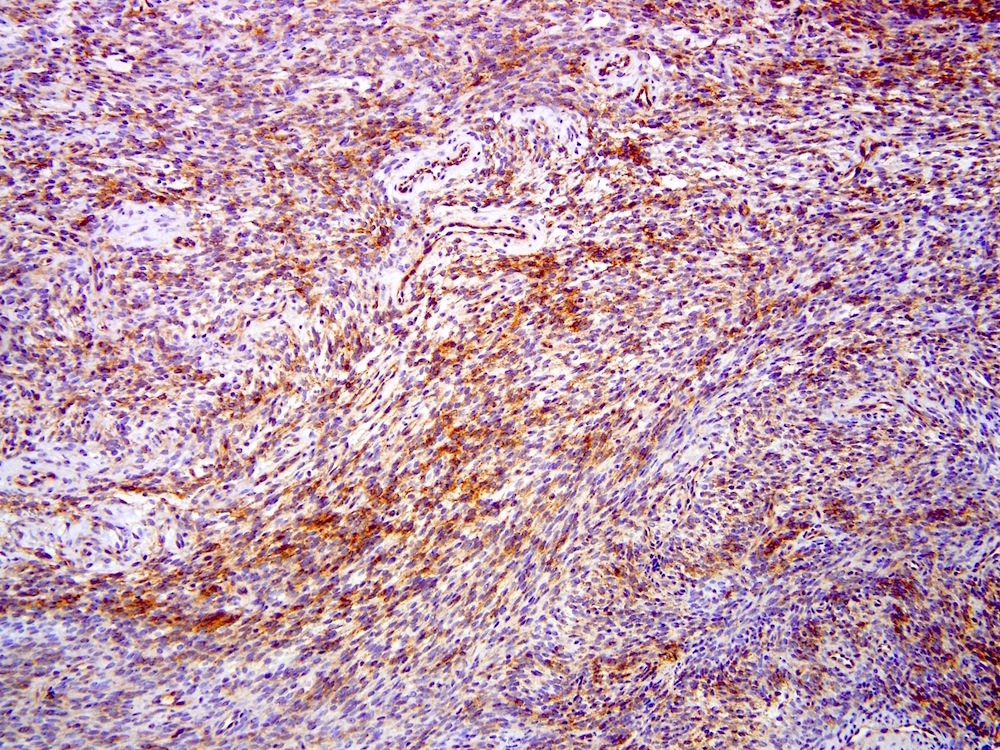
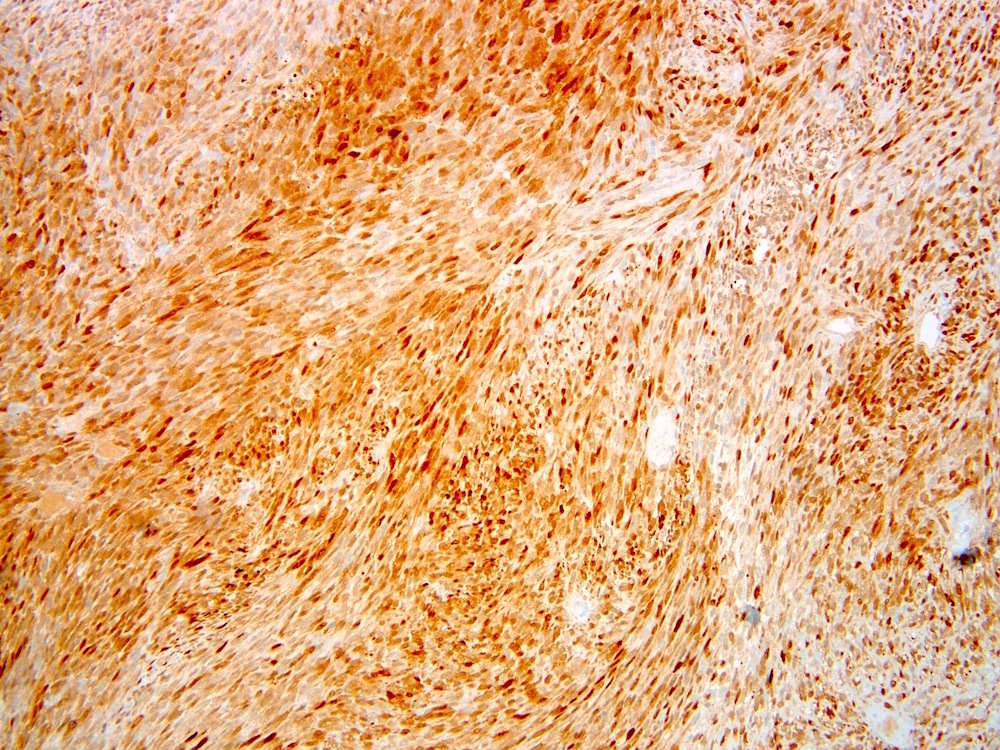
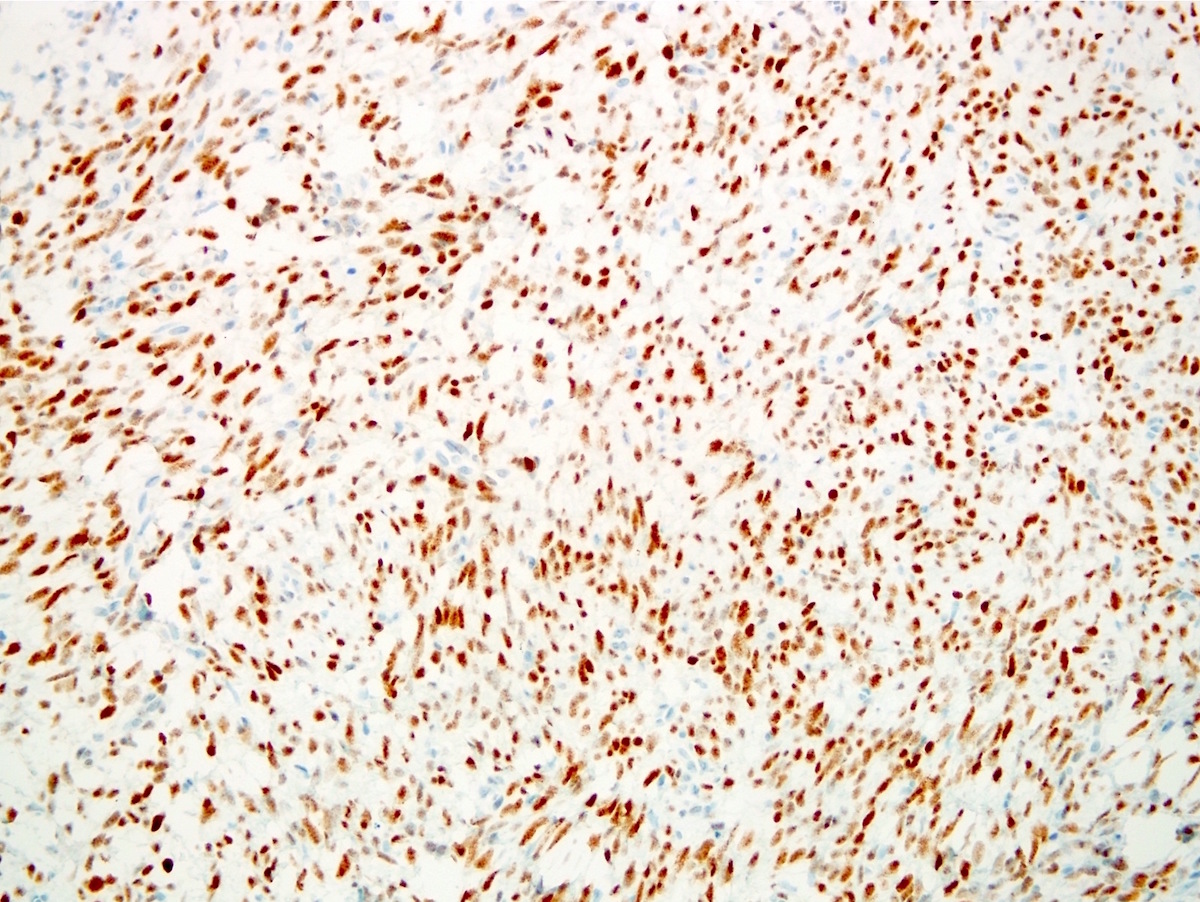
Microscopic (histologic) images
Contributed by Farres Obeidin, M.D.
Contributed by Debra Zynger, M.D.
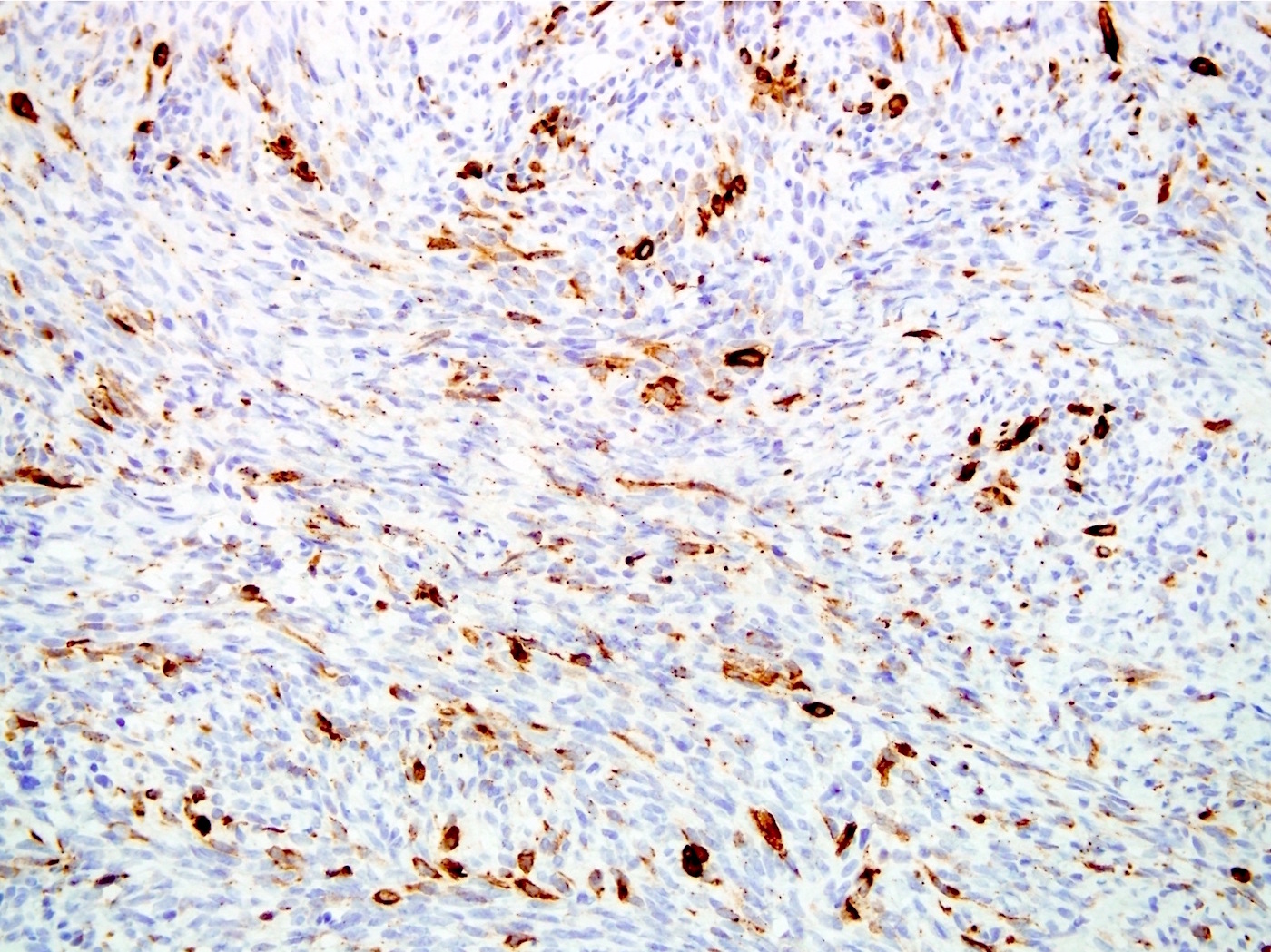
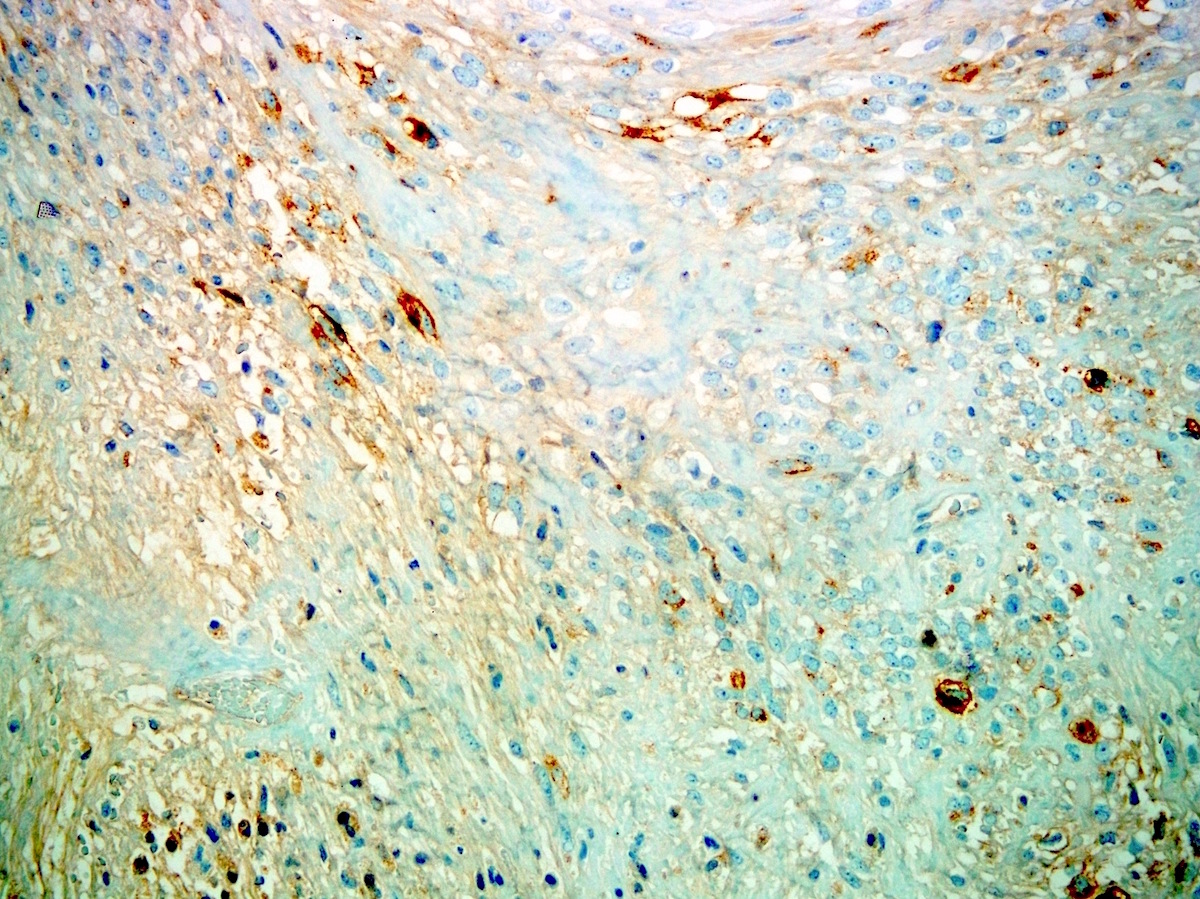
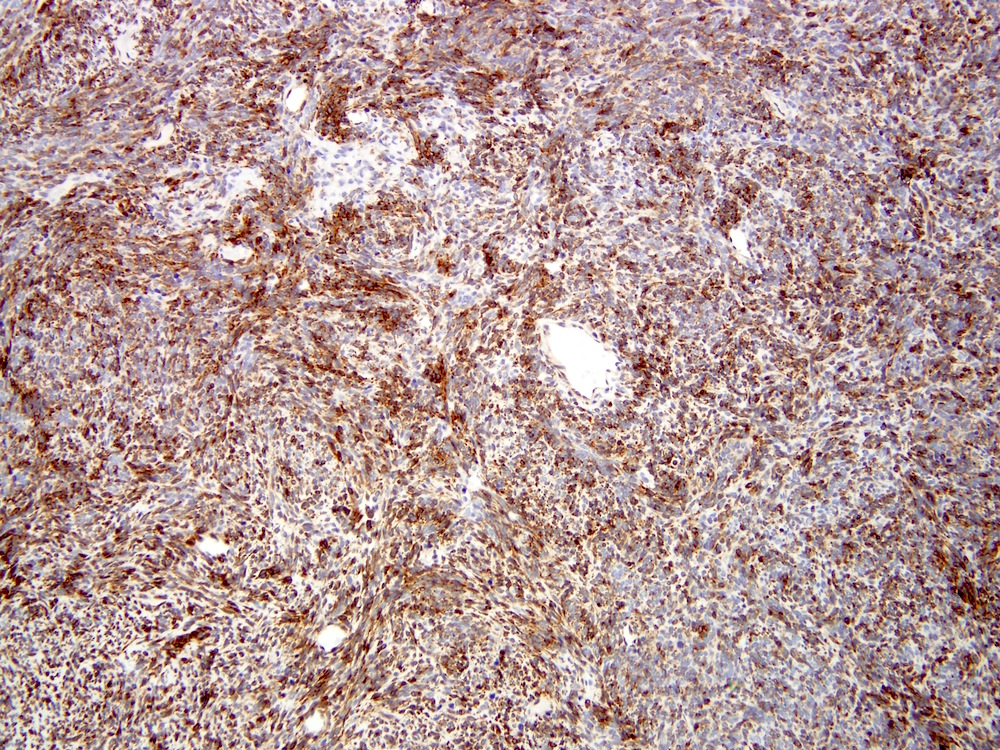
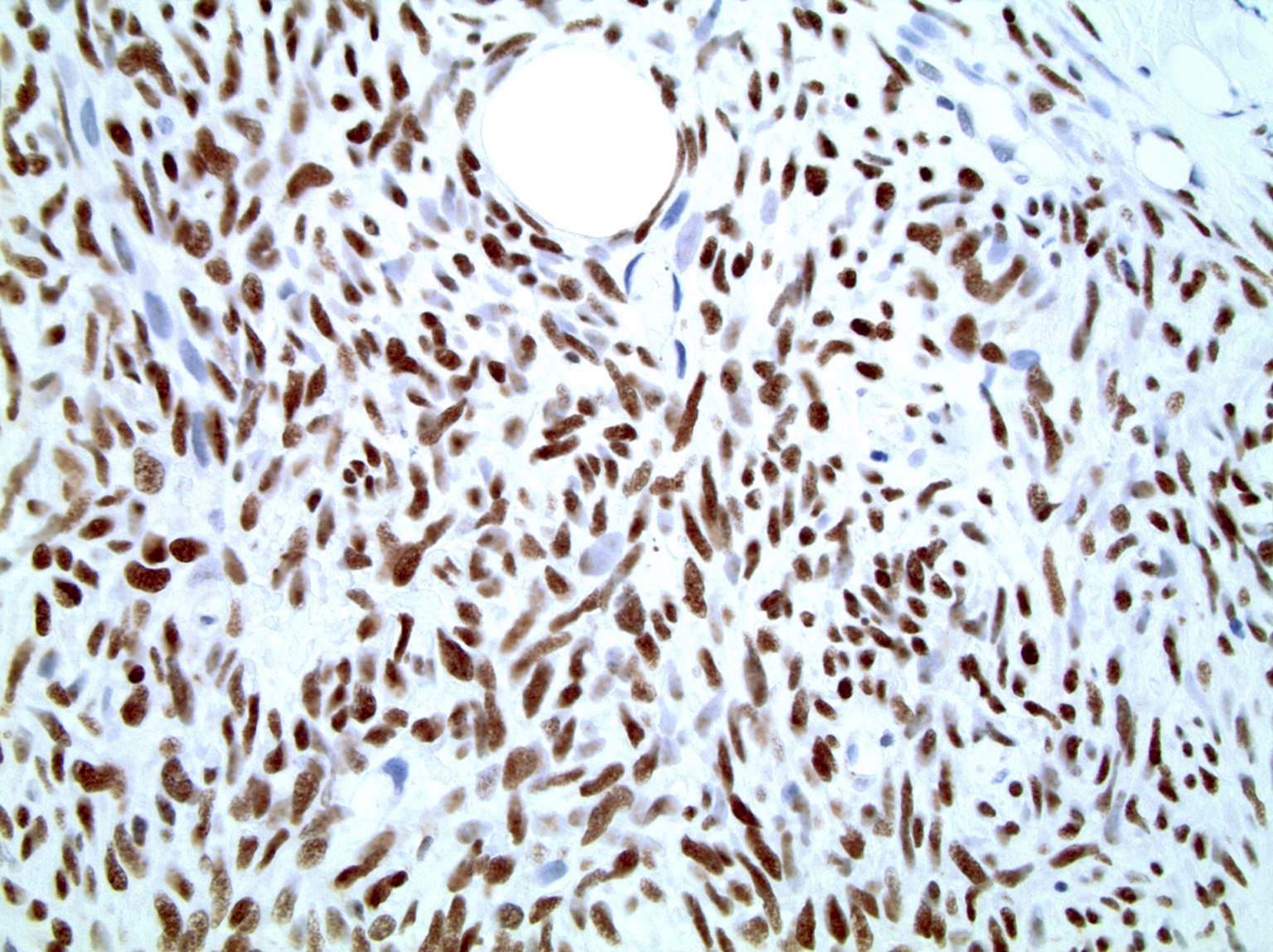
Positive stains
- TLE1: 80 - 90%, relatively specific and sensitive marker but studies have found more tumors with TLE1 positivity (Am J Clin Pathol 2011;135:839, Mod Pathol 2009;22:872)
- Cytokeratins: ~90%, variable positivity, depending on the keratin polypeptide and the component (Virchows Arch 2000;437:275)
- EMA: 29 - 90%, variable and focal, generally less than cytokeratins (Hum Pathol 1990;21:733, Am J Surg Pathol 2002;26:1434)
- BCL2: 79 - 100% (Cancer Genet Cytogenet 2009;193:1)
- Beta catenin: 30 - 73% (Oncogene 2014;33:5006)
- Calponin: at least focally positive in all tested cases (Histopathology 2003;42:588)
- CD99 (91%), CD56 (100%), CD57 (90%), calretinin (56 - 71%)
- SS18-SSX fusion specific antibody: 95% sensitive, 100% specific
- SSX C terminus antibody: 100% sensitive, 96% specific (Am J Surg Pathol 2020;44:922)
- NY-ESO-1: 76%, strong and diffuse staining (Mod Pathol 2012;25:854)
Negative stains
- CD34, desmin, h-caldesmon, myogenin, MyoD1, FLI1, WT1 (nuclear staining)
- SOX10: 93% negative (Mod Pathol 2014;27:55)
- S100: 40% (Am J Clin Pathol 1999;112:641)
- H3K27me3: 60% show loss
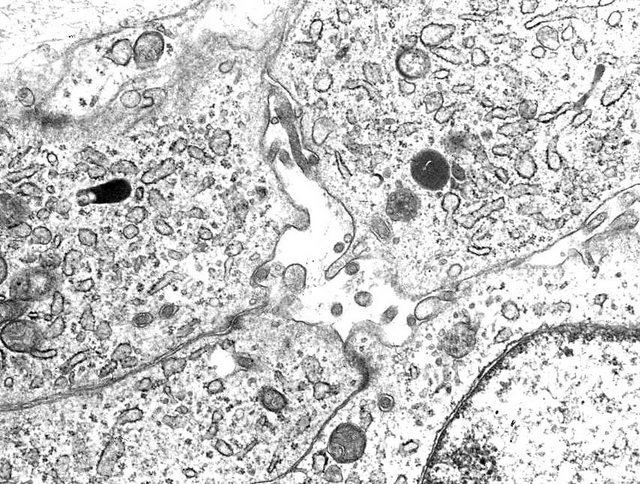
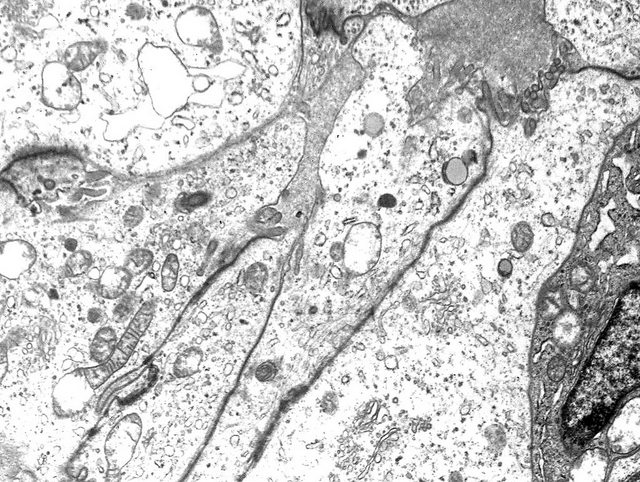
Electron microscopy description
- Glandular formation of epithelioid tumor cells with sparse luminal microvilli
Electron microscopy images
Molecular / cytogenetics description
- t(X;18)(p11.2; q11): SYT-SSX1 fusion in 90%, can detect via RT-PCR
- Also t(X;18)(p11.21;q11): SYT-SSX2 fusion, variants can be detected by optimizing RT-PCR (Mod Pathol 2002;15:679, Hum Pathol 2001;32:105)
- p16INK4A gene deletion in 74% (Am J Clin Pathol 2006;126:866)
- High expression of EZH2 helps to distinguish poorly differentiated synovial sarcoma from monophasic and biphasic subtypes (J Transl Med 2012;10:216)
Molecular / cytogenetics images
Sample pathology report
- Right lower extremity, core needle biopsy:
- Synovial sarcoma, monophasic type, FNCLCC grade 2 (see comment)
- Comment: Histologic sections demonstrate a densely cellular spindle cell neoplasm with plump, hyperchromatic and monomorphic tumor cells in a fascicular to herringbone architecture. Scattered mitotic figures are present (up to 2 mitotic figures/10 HPFs) and no tumor necrosis is seen. Immunohistochemical stains are performed and show focal positivity for EMA and pancytokeratin AE1 / AE3 and diffuse positivity for SSX::SS18 antibody. Desmin, myogenin, SOX10 and STAT6 are negative. The overall findings are consistent with a diagnosis of synovial sarcoma.
Differential diagnosis
- Biphasic:
- Adenocarcinoma:
- Lack spindle cell areas and are typically TLE1-
- Biphasic mesothelioma:
- Can show sarcomatoid features and cytokeratin positivity but WT1+ and lacks the SSX translocation
- Glandular nerve sheath tumors:
- Very rarely, malignant peripheral nerve sheath tumor and schwannoma can show glandular features
- Branchial anlage mixed tumor (ectopic hamartomatous thymoma):
- Adenocarcinoma:
- Monophasic:
- Malignant peripheral nerve sheath tumor (MPNST):
- Hypo and hypercellular areas
- SOX10, molecular studies and clinical history are useful in making the diagnosis; often shows focal keratin positivity and TLE1+ in up to 30%
- Also can have loss of H3K27me3 in 34% of cases (Mod Pathol 2016;29:582)
- Cellular schwannoma:
- Solitary fibrous tumor:
- Leiomyosarcoma:
- Often shows more nuclear pleomorphism with brighter eosinophilic cytoplasm
- May be desmin+, SMA+, calponin+, h-caldesmon+
- Spindle cell rhabdomyosarcoma:
- Adult fibrosarcoma:
- Diagnosis of exclusion when other spindle cell sarcomas have been ruled out
- Dermatofibrosarcoma protuberans with fibrosarcomatous transformation:
- Usually CD34+ and has an area with more classic histology
- Epithelioid sarcoma:
- Biphenotypic sinonasal sarcoma:
- Sarcomatoid carcinoma:
- Malignant peripheral nerve sheath tumor (MPNST):
- Poorly differentiated:
- Small round blue cell tumors:
- SS18-SSX translocation studies and lineage specific markers, such as myogenin, MyoD1, desmin, FLI1 are useful
- Molecular studies for PAX3 / PAX7 rearrangements, EWSR rearrangements, CIC-DUX4 and BCOR rearrangements help rule out alveolar rhabdomyosarcoma, Ewing sarcoma and undifferentiated round cell sarcoma (previously Ewing-like sarcomas)
- Small round blue cell tumors:
Additional references
Board review style question #1
Board review style answer #1
E. Synovial sarcoma has fusion of SS18 with SSX1, SSX2 or SSX4. It typically occurs in younger patients, with the peak incidence in the third to fourth decade and in most cases shows at least focal cytokeratin expression. It is not associated with PAX3 rearrangements, a typical finding in alveolar rhabdomyosarcoma and biphenotypic sinonasal sarcoma. HHV8 is seen in Kaposi sarcoma.
Comment Here
Reference: Synovial sarcoma
Comment Here
Reference: Synovial sarcoma
Board review style question #2
- Which morphologic feature is commonly seen in synovial sarcoma?
- Chicken wire calcifications
- Extravasated red blood cells
- Hemangiopericytic vessels
- Nuclear pleomorphism
- Prominent storiform pattern
Board review style answer #2
C. Hemangiopericytic vessels and monotonous nuclei are commonly seen in synovial sarcoma. Chicken wire calcifications are typically seen with chondroblastoma. Extravasated red blood cells are common in nodular fasciitis, fibromatosis and Kaposi sarcoma. A storiform pattern is characteristic of dermatofibrosarcoma protuberans.
Comment Here
Reference: Synovial sarcoma
Comment Here
Reference: Synovial sarcoma








insituhybridization.jpg)
cartoon.jpg)