Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Abdellatif E, Kamel D, Mantilla JG. Schwannoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueschwannoma.html. Accessed March 31st, 2025.
Definition / general
- Benign nerve sheath tumor arising from differentiated Schwann cells
Essential features
- Encapsulated, well circumscribed
- Most cases have a zonal pattern composed of cellular areas (Antoni A) with nuclear palisading (Verocay bodies) and a hypocellular component (Antoni B)
Terminology
- Neurilemoma (acceptable)
ICD coding
- ICD-10: D36.10 - benign neoplasm of peripheral nerves and autonomic nervous system, unspecified
Epidemiology
- All ages can be affected
- More common in 30 - 60 years of age
- M = F
- 90% are sporadic, 3% with neurofibromatosis type 2, 2% with schwannomatosis, 5% with meningiomatosis with or without neurofibromatosis type 2 (StatPearls: Schwannoma [Accessed 10 November 2021])
Sites
- More frequently on the limbs with a predilection to the upper limbs, followed by the head and neck area, including the oral cavity, orbit and salivary glands
- Deeply seated tumors are mainly in the posterior mediastinum and retroperitoneum
- Other areas include posterior spinal roots, bone, gastrointestinal tract, pancreas, liver, thyroid, adrenal glands and lymph nodes
- Rare sites include penis and vulva (Urol Ann 2017;9:301, World J Surg Oncol 2015;13:139)
Pathophysiology
- May occur spontaneously
- Can occur in familial tumor syndromes, such as neurofibromatosis type 2 (NF2), schwannomatosis or Carney complex (StatPearls: Carney Complex [Accessed 13 August 2018])
- Loss of function of the tumor suppressor gene merlin (schwannomin)
- Direct genetic change involving the NF2 gene on chromosome 22 or secondarily to merlin inactivation
- Can occur in NF2 and spontaneous schwannomas
- Can cause other neoplasms including meningioma, mesothelioma, glioma multiforme and carcinomas of breast, colon and rectum, kidney (clear cell type), liver, prostate and skin
Clinical features
- Pain and neurological symptoms are uncommon unless the tumor is large
- Tumor waxes and wanes in size, which may be related to cystic degeneration (J Lab Physicians 2013;5:60)
Diagnosis
- Histologic findings in the appropriate clinical and imaging context
Radiology description
- Well circumscribed masses that displace adjacent structures without direct invasion
- Cystic and fatty degeneration can be seen
- Hemorrhage and calcification are less frequent
- Cystic degeneration or hemorrhage can be seen as areas of heterogeneity in large tumors (Radiographics 2004;24:1477, Radiographics 1999;19:1253)
Prognostic factors
- Most cases have an indolent course
- Malignant transformation is exceedingly rare:
- Most commonly reported after receiving stereotactic radiation (typically in acoustic schwannoma) (Front Oncol 2021;11:655260, Otol Neurotol 2015;36:1301)
- Sporadic malignant transformation may occur in very rare cases (Asian J Neurosurg 2018;13:810, Otol Neurotol 2015;36:1301)
- To malignant peripheral nerve sheath tumor (BMJ Case Rep 2021;14:e246445, Front Oncol 2021;11:655260)
Case reports
- 12 year old boy with painless subconjunctival mass in the left eye (Indian J Ophthalmol 2015;63:620)
- 12 year old girl with solitary superficial tumor of back; plexiform schwannoma (Case #50)
- 15 year old girl with a rapidly enlarging mass of the nose suspected to be malignant (BMJ Case Rep 2013;2013:bcr2012008435)
- 28 year old with neck mass and challenging FNA (Am J Case Rep 2014;15:538)
- 36 year old man with melanotic schwannoma of the L5 root (Neuroradiol J 2016;29:219)
- 43 year old woman with pelvic mass (World J Gastroenterol 2014;20:1371)
- 53 year old woman with rapidly growing palpable mass in thigh (Br J Radiol 2010;83:e154)
- 56 year old woman with a large lytic lesion in her lower femur (J Med Case Rep 2017;11:147)
- 56 year old man with lower back pain and hematuria (World J Surg Oncol 2016;14:29)
- 58 year old woman with painless palpable vulvar mass (Case Rep Dermatol 2018;10:41)
- 61 year old woman with mass in right mandible (Medicine (Baltimore) 2015;94:e1974)
- 64 year old woman with abdominal wall mass (BMC Surg 2010;10:1)
Treatment
- Surgical excision is the treatment of choice
- Local recurrence is uncommon
- Delayed facial nerve palsy can occur after surgical removal of vestibular schwannoma (Neurosurgery 2016;78:251)
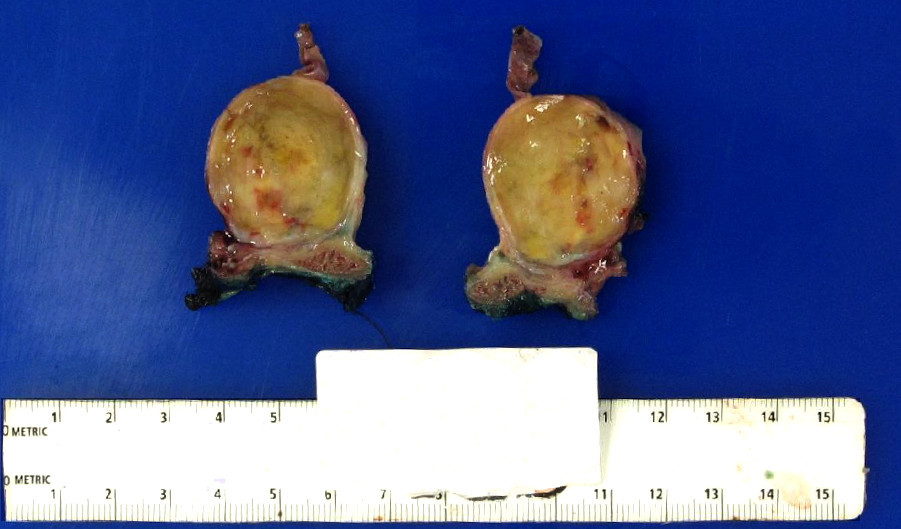
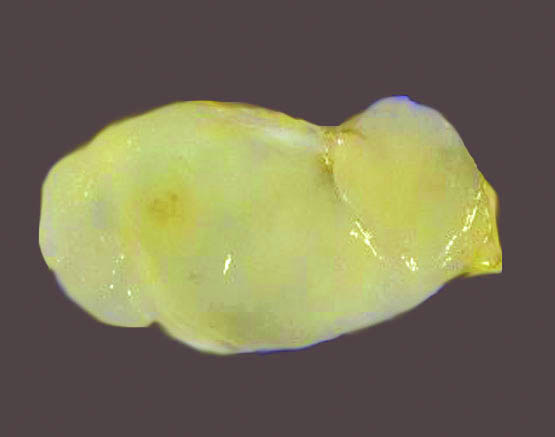
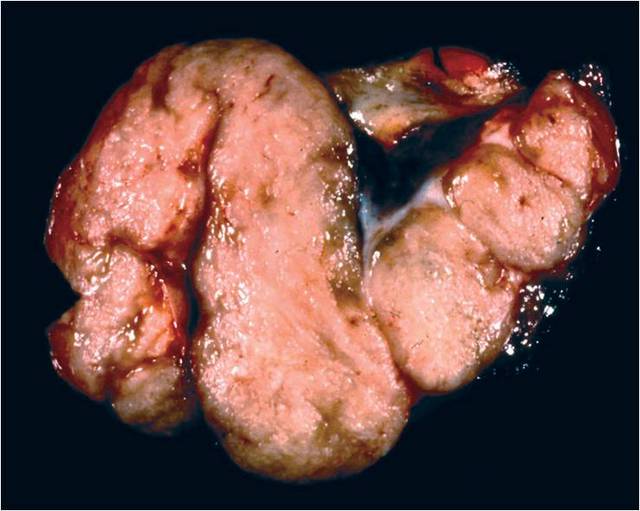
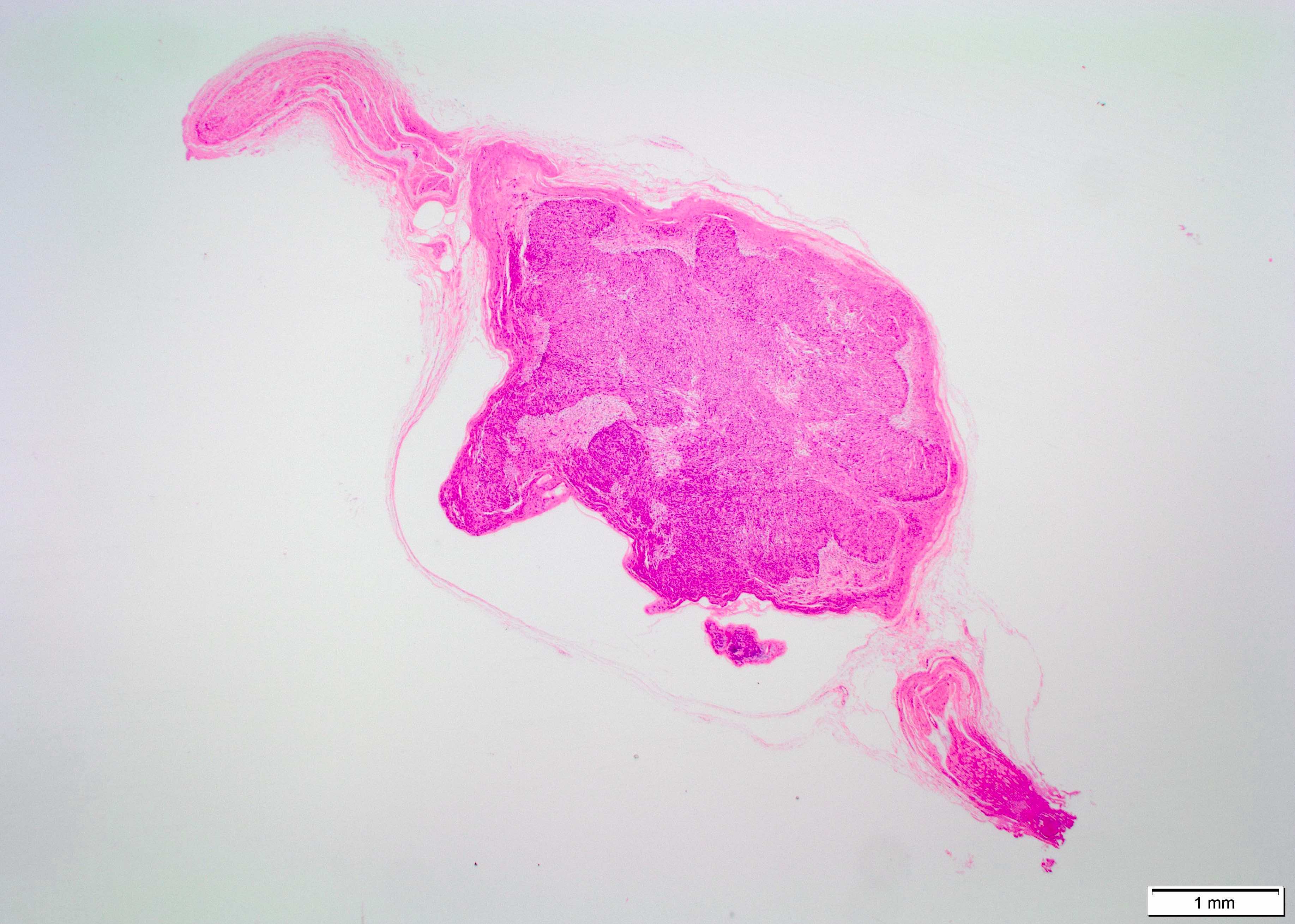
Gross description
- Usually solitary
- Most lesions are completely encapsulated
- Nerve of origin may be present at the periphery - does not penetrate substance of tumor
- Large tumors have an eccentric position in relation to the nerve
- Cut section is light tan and glistening and may show yellow patches
- Large, longstanding tumors may be cystic
- Areas of hemorrhage may be seen (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2020)
Gross images
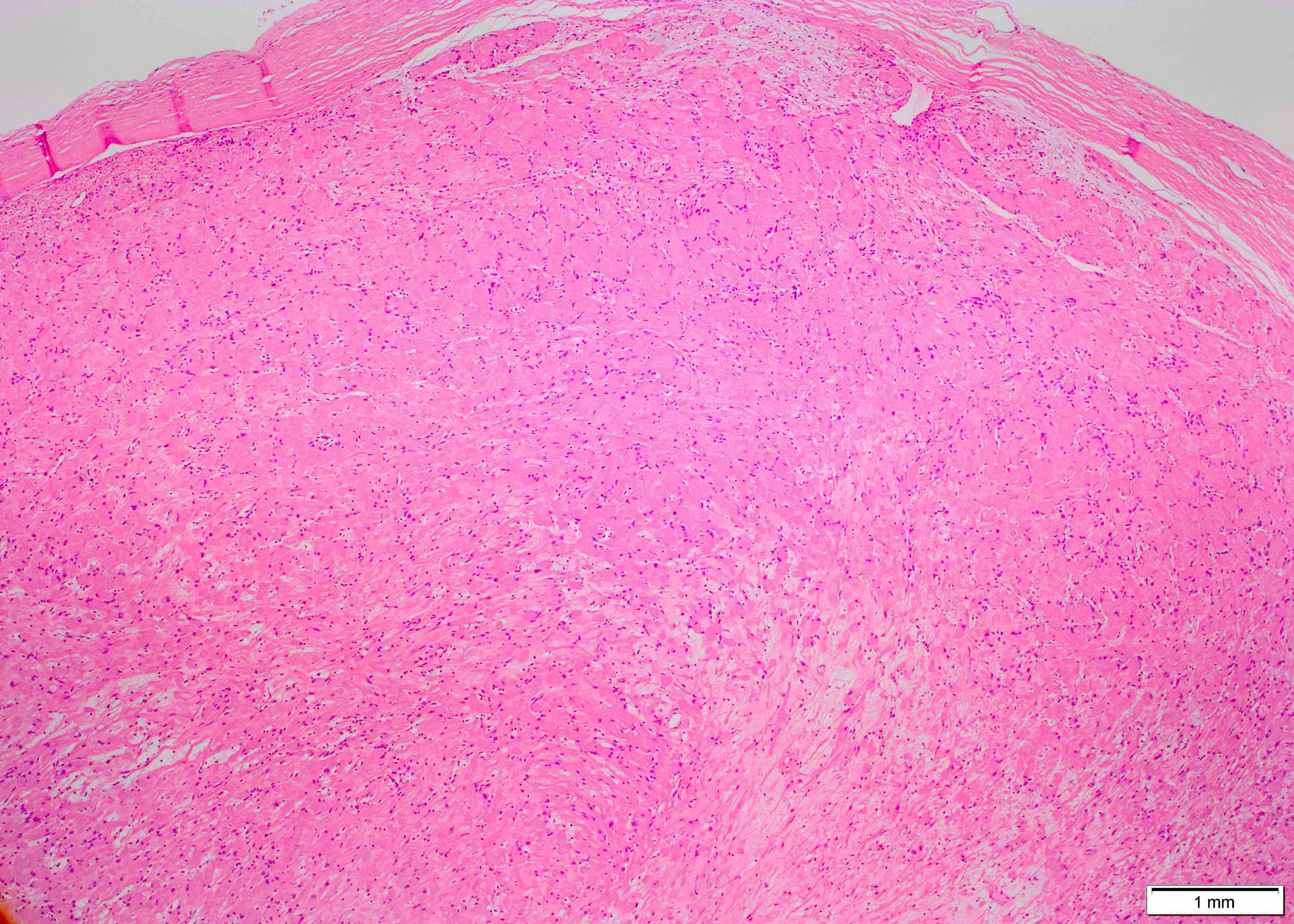
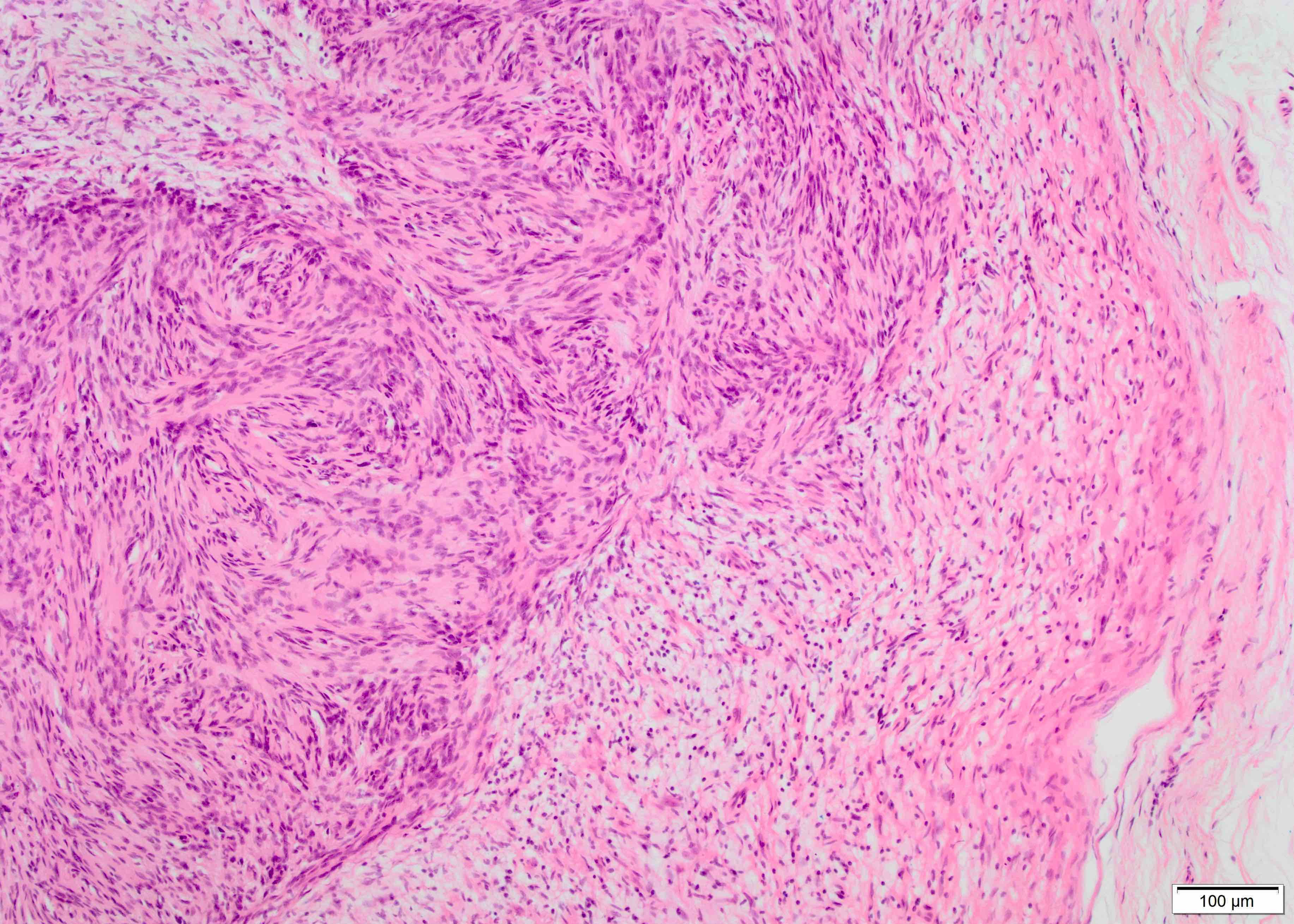
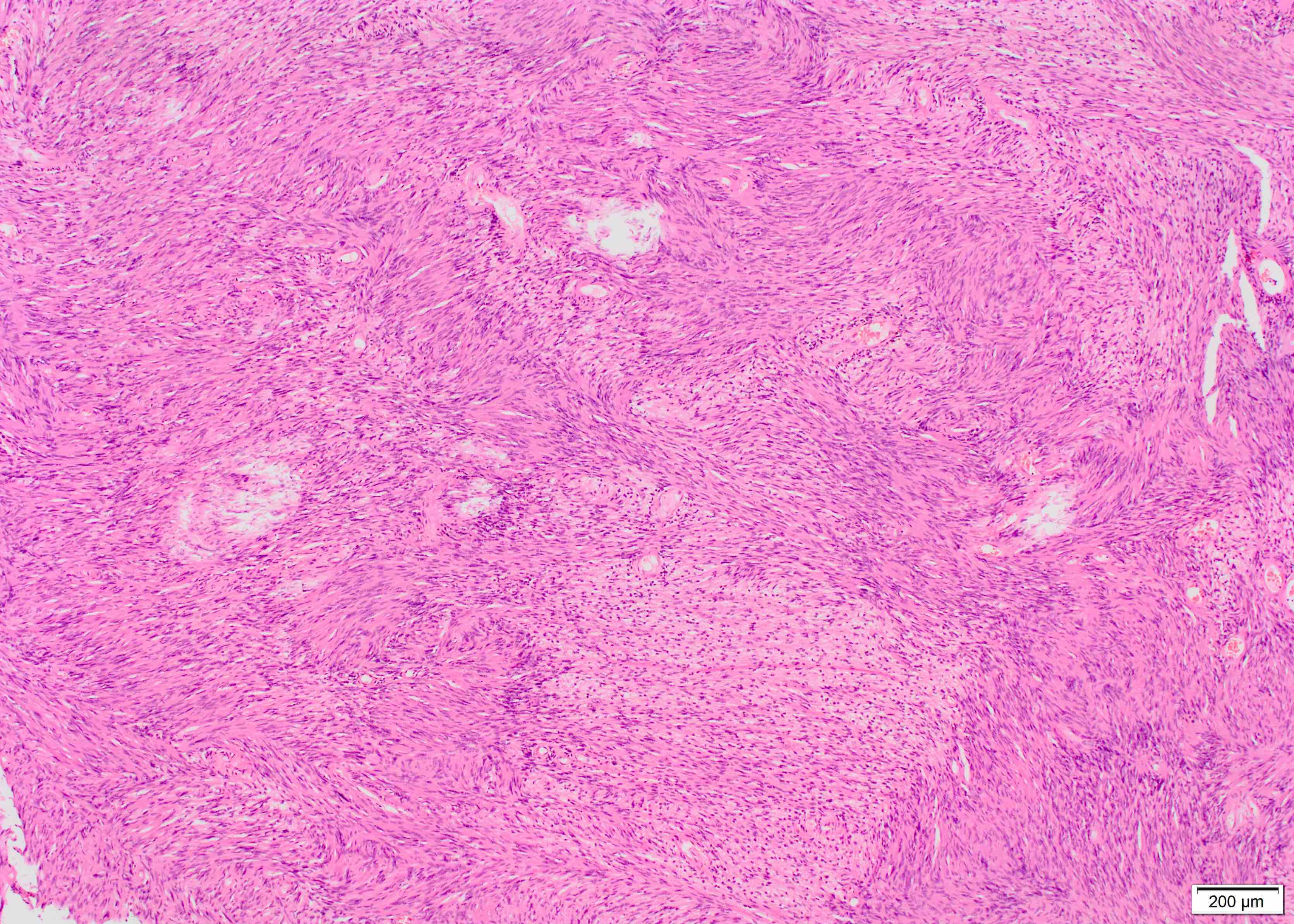
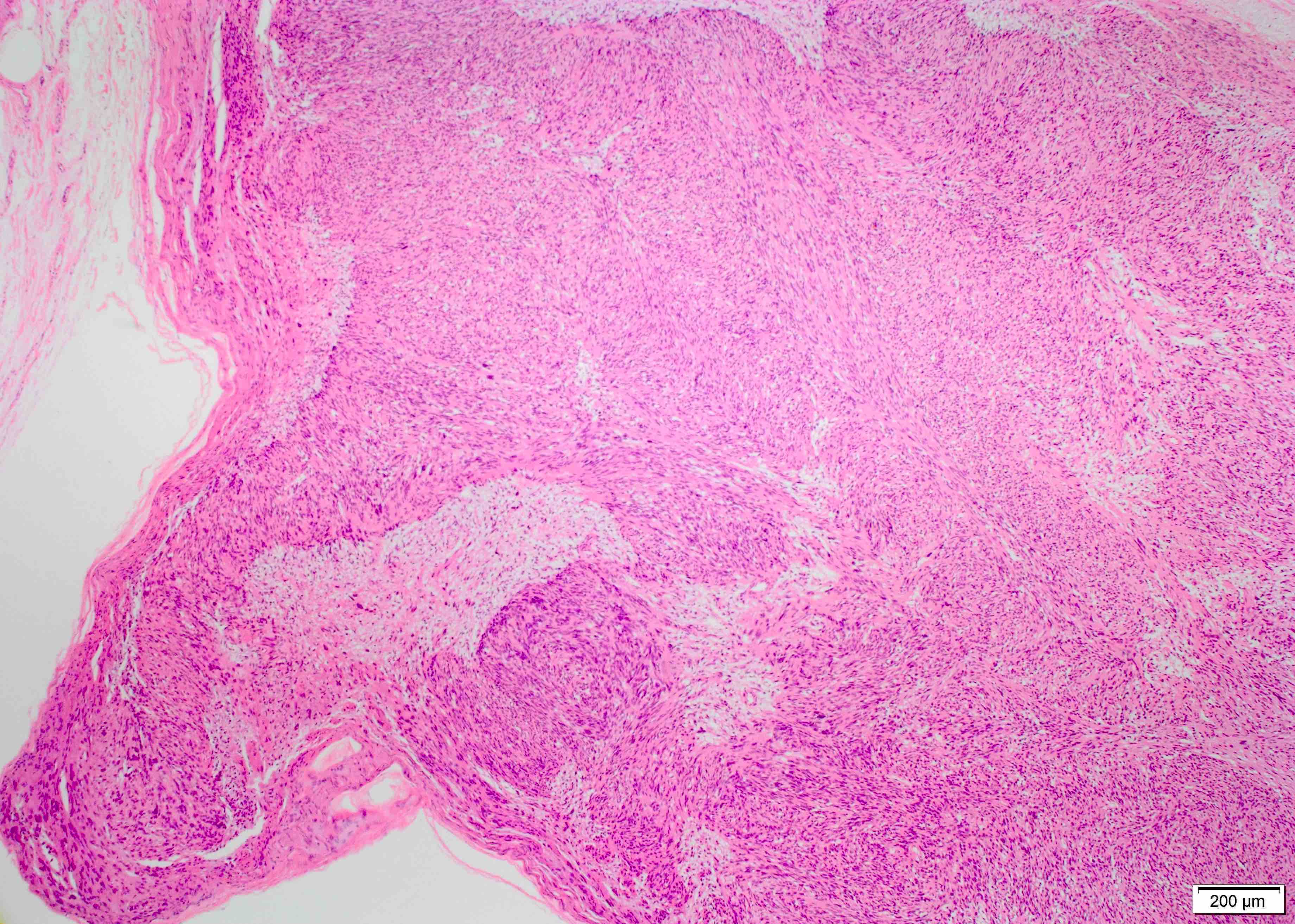
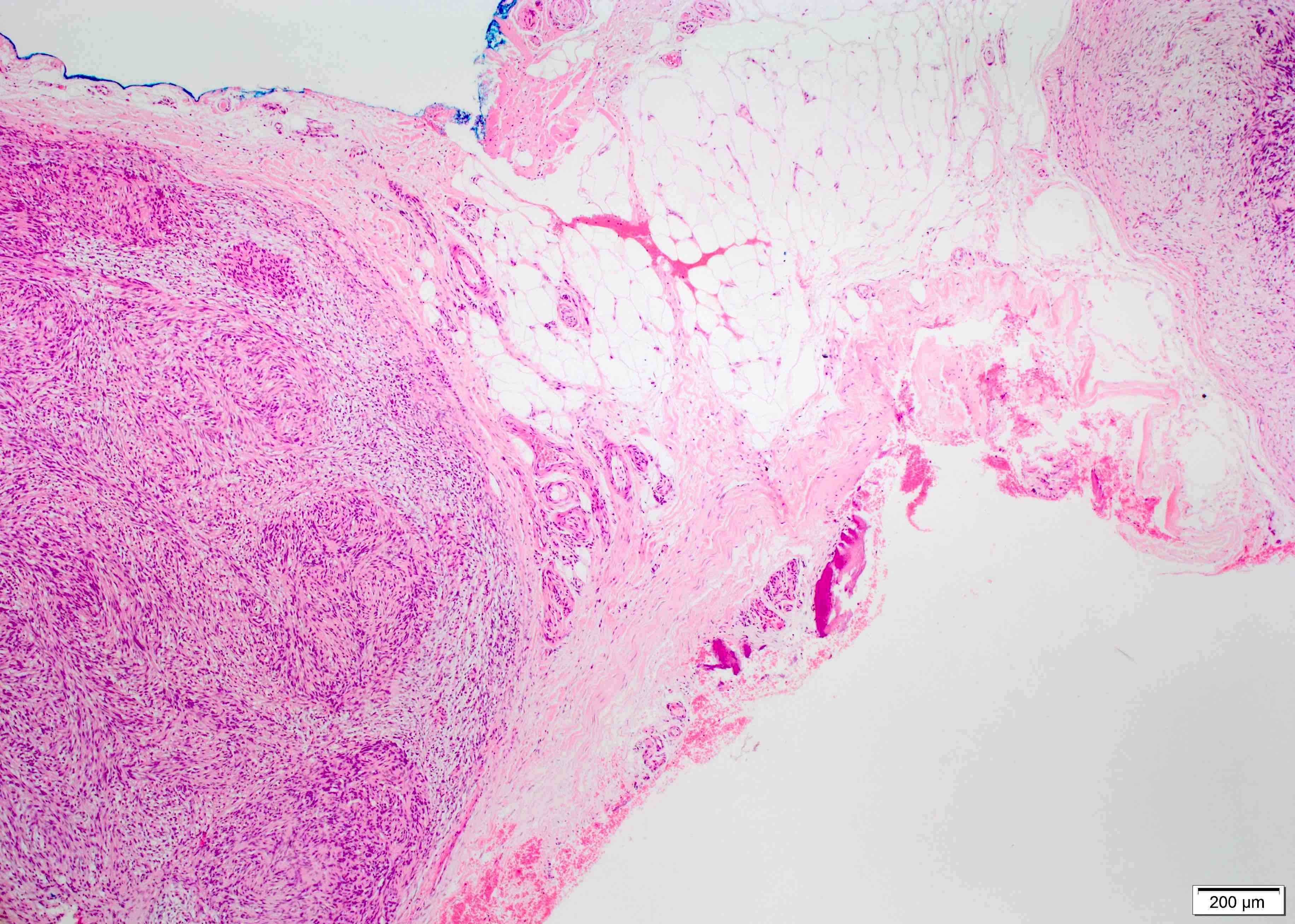
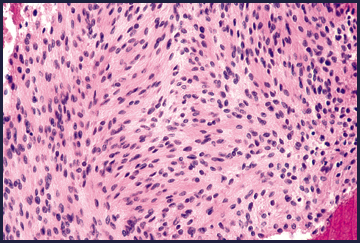
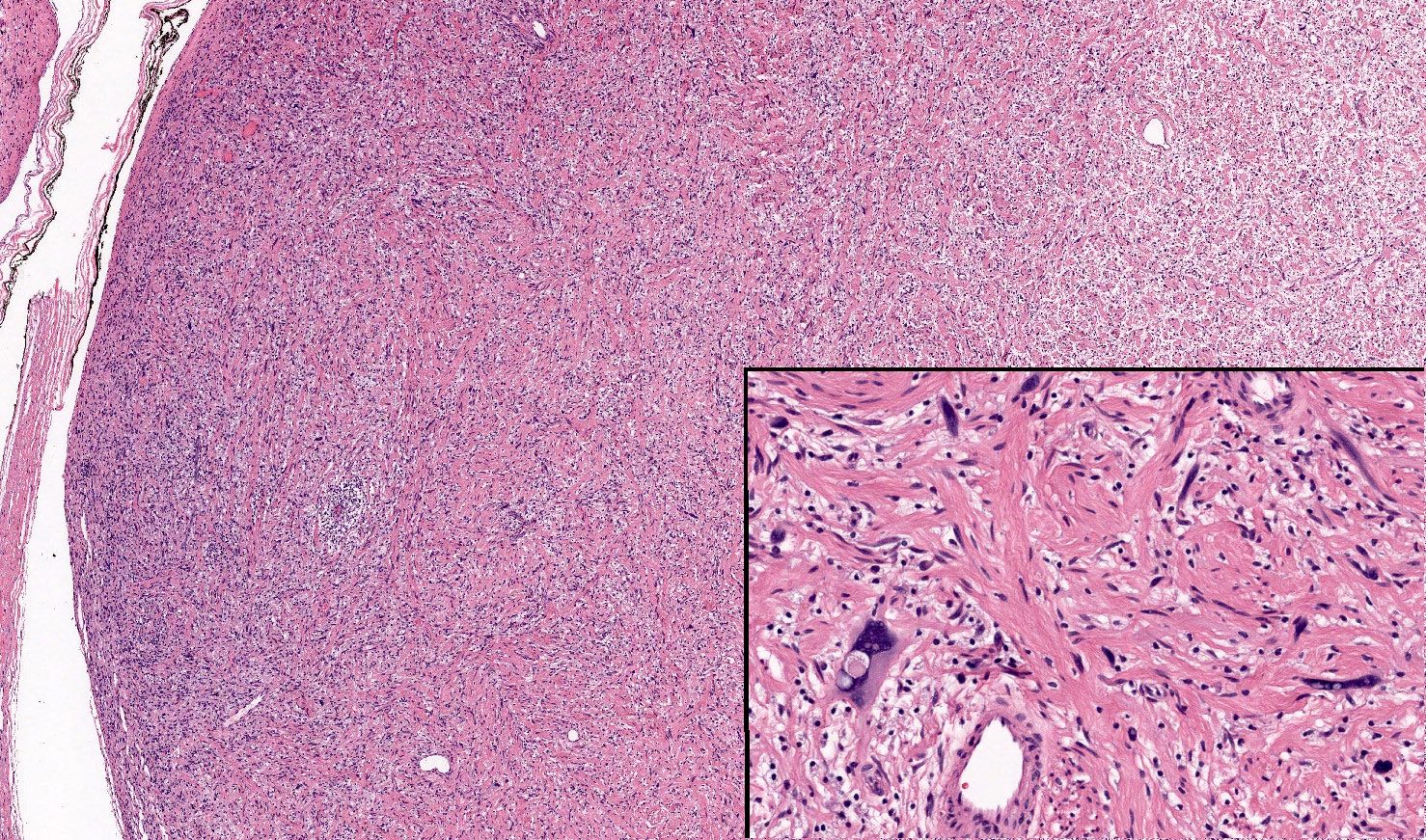
Microscopic (histologic) description
- Biphasic: compact hypercellular Antoni A areas and myxoid hypocellular Antoni B areas (may be absent in small tumors)
- Nuclear palisading around fibrillary process (Verocay bodies) is often seen in cellular areas
- Cells are narrow, elongated and wavy with tapered ends interspersed with collagen fibers
- Tumor cells have ill defined cytoplasm, dense chromatin
- May have degenerative nuclear atypia, cystic degeneration and hemorrhage (ancient change)
- Blood vessels may have thickened hyalinized walls and thrombi
- Pseudoglandular spaces: uncommon; cystic spaces lined by Schwann cells; may represent degenerative Verocay bodies (Ann Diagn Pathol 2016;20:24, Arch Pathol Lab Med 2005;129:1106)
- Amianthoid fibers or collagenous spherules: large nodular masses of collagen with radiating edges
- Mitotic figures are rarely seen
- No intratumoral axons
- Tumors in the GI tract typically have a prominent lymphocytic rim
- Variants:
- Ancient schwannoma:
- Features include hyalinization, nuclear atypia, hemosiderin deposition
- Should not have conspicuous mitotic activity or other features suggestive of malignancy
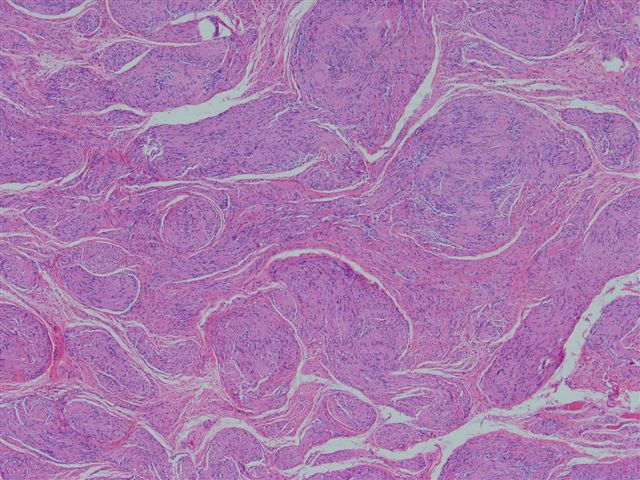
- Cellular schwannoma:
- Composed entirely of Antoni A tissue and devoid of Verocay bodies
- Most common in the paravertebral region
- Epithelioid schwannoma:
- Single or small groups of epithelioid schwann cells with moderate amphophilic cytoplasm and occasional nuclear pseudoinclusions (Am J Surg Pathol 2016;40:704):
- Myxoid to hyalinized stroma, often with thick walled vessels
- Microcystic / reticular variant (Am J Surg Pathol 2008;32:1080):
- Has a preference for the GI tract and rarely in subcutaneous soft tissue
- Formed of strands of bland spindle cells in a myxoid background, with various proportions of microcystic structures
- No alternating Antoni A, Antoni B areas or Verocay bodies
- Neuroblastoma-like variant:
- Rare variant defined by large, collagenous, rosette-like structures surrounded by small, round, hyperchromatic Schwann cells (Int J Health Sci (Qassim) 2015;9:478)
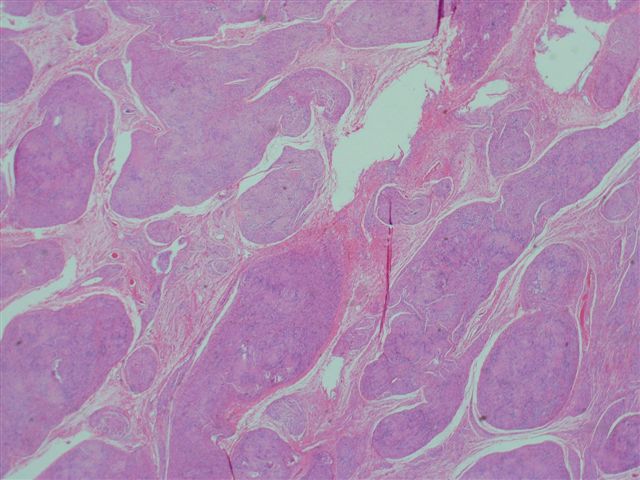
- Plexiform schwannoma:
- Rare
- May involve multiple nerve fascicles, making complete resection challenging
- Typically associated with NF2 and schwannomatosis
- Ancient schwannoma:
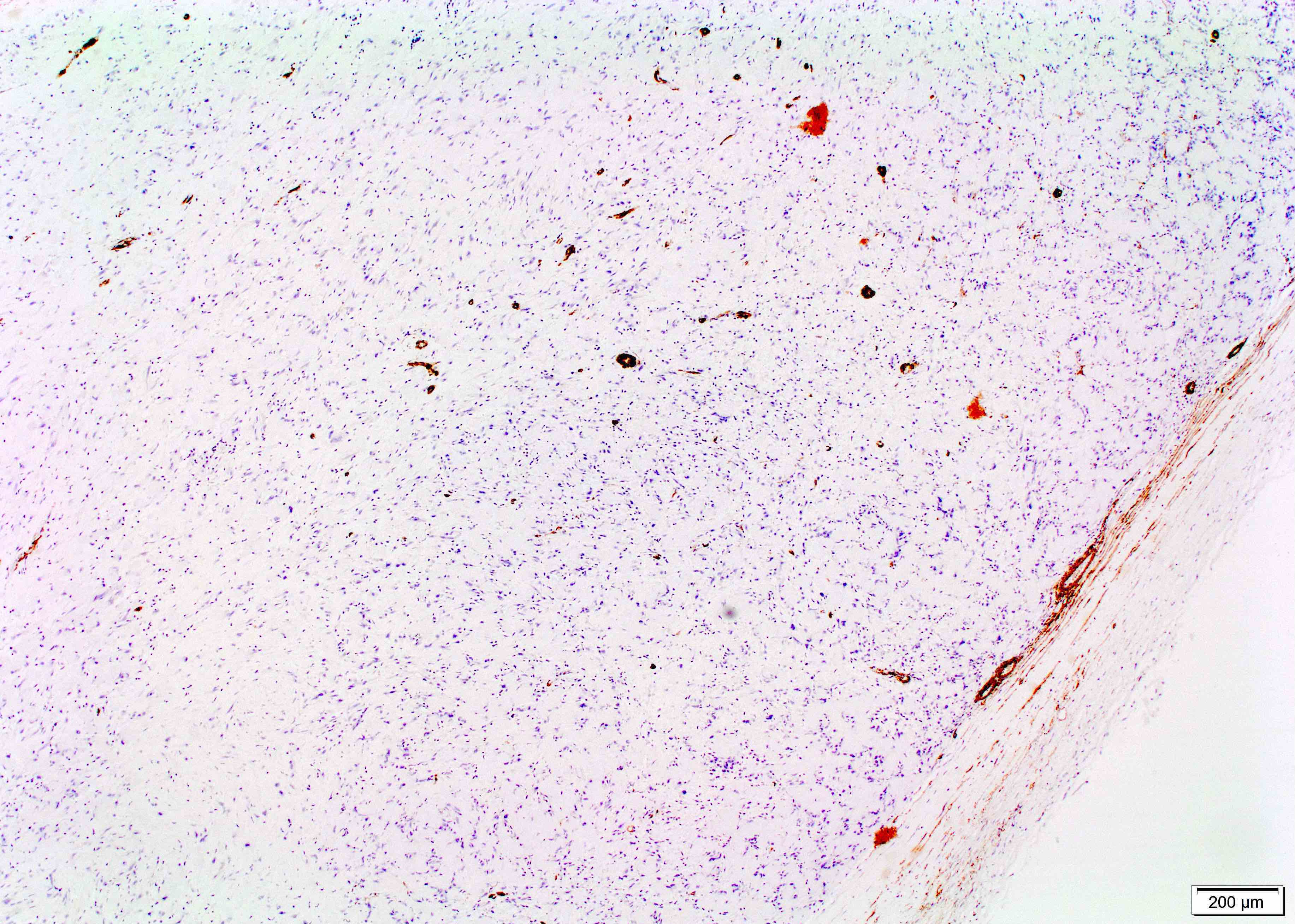
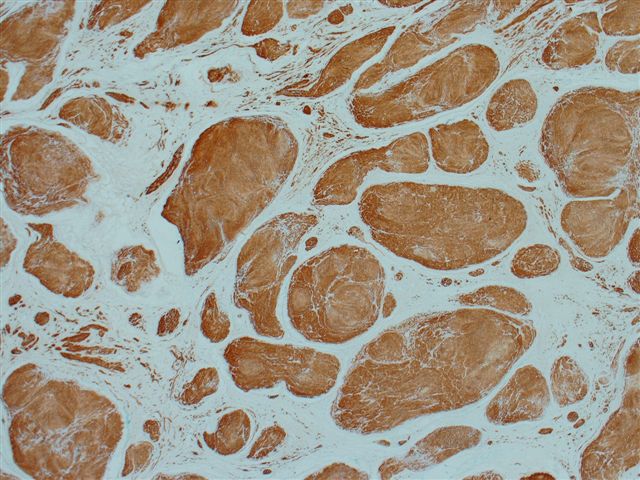
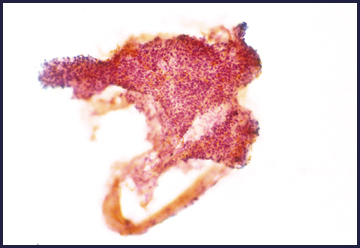
Microscopic (histologic) images
Contributed by Dia Eldin Kamel, M.D., Ph.D. and Case #50
Plexiform schwannoma:
Images hosted on other servers:
Microcystic / reticular schwannoma:
Virtual slides
Cytology description
- Aggregates of spindled cells with indistinct cytoplasm and elongated nuclei with blunt pointed ends (World J Gastroenterol 2011;17:3459)
- Ancient changes can show nuclear pleomorphism and occasionally nuclear inclusions
Cytology images
Positive stains
- S100 (strong and diffuse staining)
- Calretinin, CD56, SOX10, podoplanin
- Weak, variable CD34
- Other stains include laminin, type IV collagen, vimentin, CD68
Negative stains
- Keratin (cytokeratin) immunoreactivity may be seen in some cellular schwannomas, which may represent cross reactivity with GFAP (Acta Neuropathol 2012;123:295)
- Neurofilament (rare staining)
- Desmin, SMA
- EMA (expressed in the capsule / perineural fibroblasts)
Electron microscopy description
- Basal lamina consisting of electron dense material coats the surface of Schwann cells (Cancer 1981;48:1381, Acta Cytol 1983;27:441)
- Elongated cells with continuous basal lamina, thin cytoplasmic processes, aggregates of intracytoplasmic microfibrils, peculiar intracytoplasmic lamellar bodies, extracellular long spacing collagen
- Basal lamina is fragmented in Antoni B areas, suggesting that these areas are degenerated Antoni A areas
- Contains lipid
- Has characteristic Luse bodies (collagen fibers with abnormally long spacing exceeding 100 nm between electron dense bands)
Molecular / cytogenetics description
- May occur spontaneously
- Can occur in familial tumor syndromes such as neurofibromatosis type 2 (NF2), schwannomatosis or Carney complex
- Can be caused by loss of function of the tumor suppressor gene, merlin (schwannomin)
- Merlin acts as a tumor suppressor gene
- Overexpression can hinder cell proliferation and the changes induced by oncogenes
- Its downregulation leads to neoplastic transformation
- Mutations affecting SMARCB1 have a role in the pathogenesis of a small subset of spinal schwannomas and biallelic inactivation of SMARCB1 may cooperate with deficiency of NF2 function (J Neurooncol 2018;137:33)
Sample pathology report
- Chest wall mass, excision:
- Schwannoma (see comment)
- Tumor size: 3.5 cm in greatest dimension
- Comment: Histologic sections contain an encapsulated neoplasm composed of cytologically bland spindle cells arranged in short fascicles, containing more densely cellular areas with nuclear palisading (Antoni A), alternating with paucicellular areas (Antoni B). There are focal areas of hemorrhage and myxoid degeneration. No histologic features of malignancy are identified.
Differential diagnosis
- Leiomyoma and leiomyosarcoma:
- May show palisading and extensive degenerative changes in the form of hyalinization, calcification, myxoid changes and ancient nuclear atypia
- Cells are elongated with eosinophilic or occasional fibrillar cytoplasm with distinct cell membranes
- S100-
- SMA+ and desmin+
- Ultrastructurally evidence of leiomyogenic differentiation
- Malignant melanoma:
- Malignant melanotic nerve sheath tumor:
- Formerly known as melanotic schwannoma (misnomer)
- Often arises in the paraspinal region
- Tumors are usually heavily pigmented
- Malignant peripheral nerve sheath tumor (MPNST):
- Infiltrative growth
- Hypercellular, pleomorphic nuclei and high mitotic activity
- Areas of geographic necrosis can show divergent differentiation
- Patchy S100 or negative
- Neurofibroma:
- Usually lacks capsule, formed of spindle cells, shredded carrot collagen and mast cells
- Hypocellular, myxoid areas without hypercellular areas
- Weaker S100, focal calretinin, stronger CD34, factor XIIIa+
- Pleomorphic hyalinizing angiectatic tumor (PHAT) (J Clin Diagn Res 2017;11:ED15):
- Solitary circumscribed neuroma (palisaded encapsulated neuroma):
- Encapsulated dermal or subcutaneous tumor, which may be seen with club-like extension in the subcutaneous tissue
- May show nuclear palisading
- Silver stains show the axons traversing the Schwann cells; however, they are near the capsule in schwannomas
- Peripheral delicate EMA positivity
Board review style question #1
Which of the following immunohistochemical stains best differentiates schwannoma from neurofibroma?
- Calretinin
- CK5/6
- MNF116
- p63
- S100
Board review style answer #1
E. S100 shows strong and almost diffuse positivity with schwannoma in contrast to neurofibroma, which variably expresses the antigen due to the presence of other cell populations.
Comment Here
Reference: Schwannoma
Comment Here
Reference: Schwannoma
Board review style question #2
Which of the following is true regarding the tumor represented in the picture?
- Its cytologic atypia is degenerative in nature
- The degree of cytologic atypia suggest malignant transformation
- Melanin pigment may be seen in some of these lesions
- These tumors are usually poorly circumscribed and difficult to excise
- Local recurrence and malignant transformation are common
Board review style answer #2
A. The picture represents schwannoma with degenerative changes (ancient schwannoma). Tumors with extensive degenerative changes may have extensive hyalinization with loss of their characteristic architectural features, as well as conspicuous degenerative cytologic atypia. Malignant transformation of schwannoma is exceedingly rare and most commonly reported in the setting of stereotactic radiation. Malignant melanotic nerve sheath tumor (formerly called melanotic schwannoma) is a rare tumor with metastatic potential, which often arises in the paraspinal region. Given its different biological behavior, it should not be labeled as schwannoma. Most schwannomas are encapsulated and easily separated from their nerve of origin. Local recurrence is rare after excision.
Comment Here
Reference: Schwannoma
Comment Here
Reference: Schwannoma