Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Warmke L, Meis J. Proliferative fasciitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueproliferativefasciitis.html. Accessed March 31st, 2025.
Definition / general
- Proliferative fasciitis is a pseudosarcomatous proliferation of myofibroblastic / fibroblastic cells with large ganglion-like cells involving subcutaneous tissue
- First formally recognized as a distinct entity from nodular fasciitis in 1975 (Cancer 1975;36:1450)
Essential features
- Myofibroblastic / fibroblastic proliferation with scattered ganglion-like cells
- Variable collagenous to myxoid stroma
- Subcutaneous / fascial involvement
ICD coding
Epidemiology
- Rare, much less common than nodular fasciitis
- Occurs predominantly in middle aged adults (mean age: 51 years) (Pathol Res Pract 2012;208:126)
- Rare subtype of proliferative fasciitis has been described in children (Am J Surg Pathol 1992;16:364)
- Equally distributed in both sexes
Sites
- Subcutaneous by definition (whereas proliferative myositis is intramuscular)
- Usually located between the subcutis and underlying muscle, in the region of the superficial fascia (Cancer 1975;36:1450)
- Majority (74%) originate in the extremities (Cancer 1975;36:1450)
- Most commonly involves the subcutaneous tissue of upper extremity, particularly the forearm, followed by lower extremity and trunk
- May also arise in dermis (J Cutan Pathol 2011;38:59)
Pathophysiology
- Subset of cases has a recurrent FOS gene rearrangement (Mod Pathol 2021;34:942)
Etiology
- Unknown
- Approximately 20% of cases are associated with previous trauma (Mod Pathol 2021;34:942)
Clinical features
- Small, firm subcutaneous mass that is moveable
- Often demonstrates rapid growth
- Usually excised within 2 months from the time it is first noticed
- Almost always measures < 5 cm (most < 3 cm)
- Tenderness or pain is present in approximately 67% of patients (Cancer 1975;36:1450)
Diagnosis
- Small, palpable rapidly growing nodule
- Subcutaneous / fascial involvement (Cancer 1975;36:1450)
- Myofibroblastic / fibroblastic proliferation with ganglion-like cells
Radiology description
- Ultrasound (J Clin Ultrasound 2017;45:445):
- Ill defined subcutaneous lesion
- Hyperechoic relative to subcutaneous fat
- Hypoechoic striae may be present
- Color Doppler reveals mild vascularity
- MRI (Skeletal Radiol 2004;33:300):
- Isointense to muscle on T1 weighted image
- Hyperintense on T2 weighted image
Prognostic factors
- Benign clinical course
- Usually self limited, disappearing within 1 - 12 weeks (Acta Cytol 2002;46:1049)
- Rarely recurs after conservative local excision
- Does not metastasize
Case reports
- 13 year old boy with dermal lesion (J Cutan Pathol 2011;38:59)
- 16 year old boy with orbital mass (Ophthalmic Plast Reconstr Surg 2017;33:S151)
- 16 year old girl with orbital mass (Orbit 2021 Sep 2 [Epub ahead of print])
- 30 year old woman with metachronous orbital and forearm masses (Pathol Res Pract 2012;208:126)
- 43 year old woman with a painful thigh mass (J Clin Ultrasound 2017;45:445)
- 62 year old woman with palpable breast mass (Breast J 2020;26:2072)
Treatment
- Spontaneous resolution can occur in 1 - 12 weeks (mean: 4.7 weeks) (Acta Cytol 2002;46:1049)
- Initially may be managed nonsurgically with follow up (Acta Cytol 2002;46:1049)
- Adequately treated by simple / conservative local excision
- No indication for radical surgery
Gross description
- Solitary, mobile mass in the subcutaneous tissue
- Poorly demarcated, stellate and firm mass that extends along preexisting fibrous septae or fascial planes (Arch Pathol Lab Med 2008;132:579)
- Grayish white, yellowish tan or reddish pink firm tissue (Cancer 1975;36:1450)
- Variable infiltration into surrounding adipose tissue
- May extend horizontally along fascia and fibrous septa of subcutaneous tissue
- Rare childhood type is often better circumscribed and less infiltrative
- Ranges in size from 1.0 - 6.9 cm in diameter, usually < 4 cm (Arch Pathol Lab Med 2008;132:579)
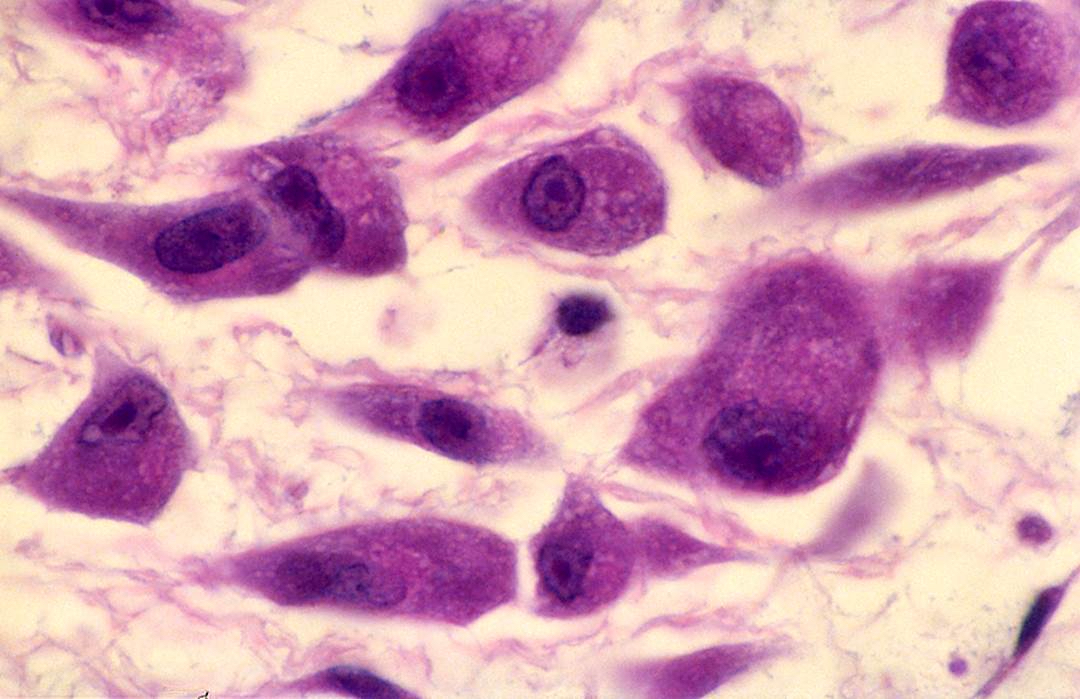
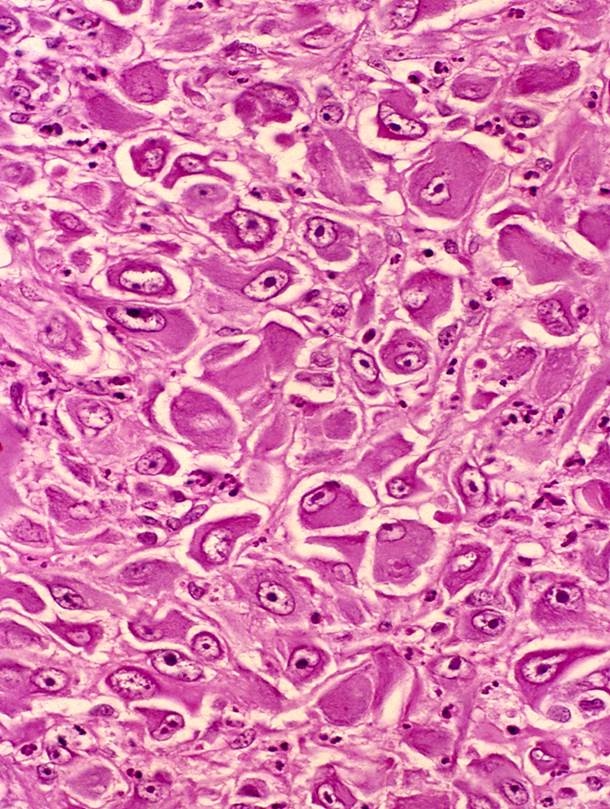
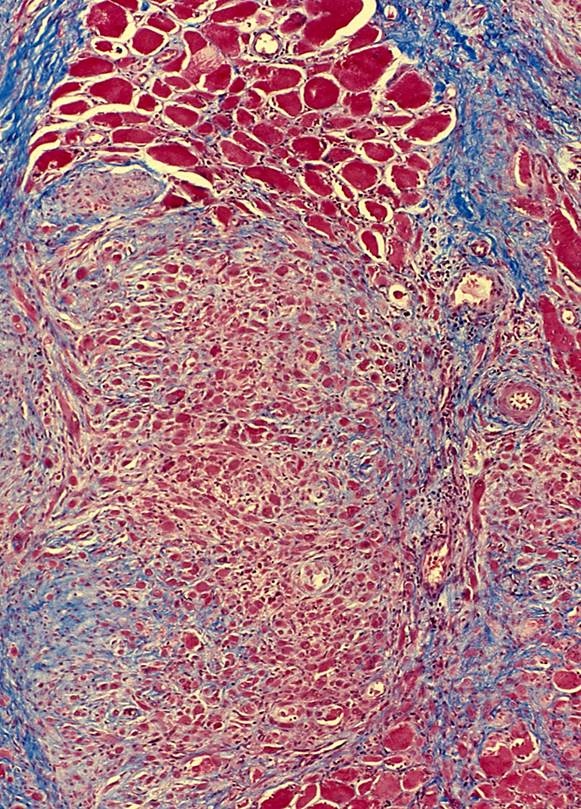
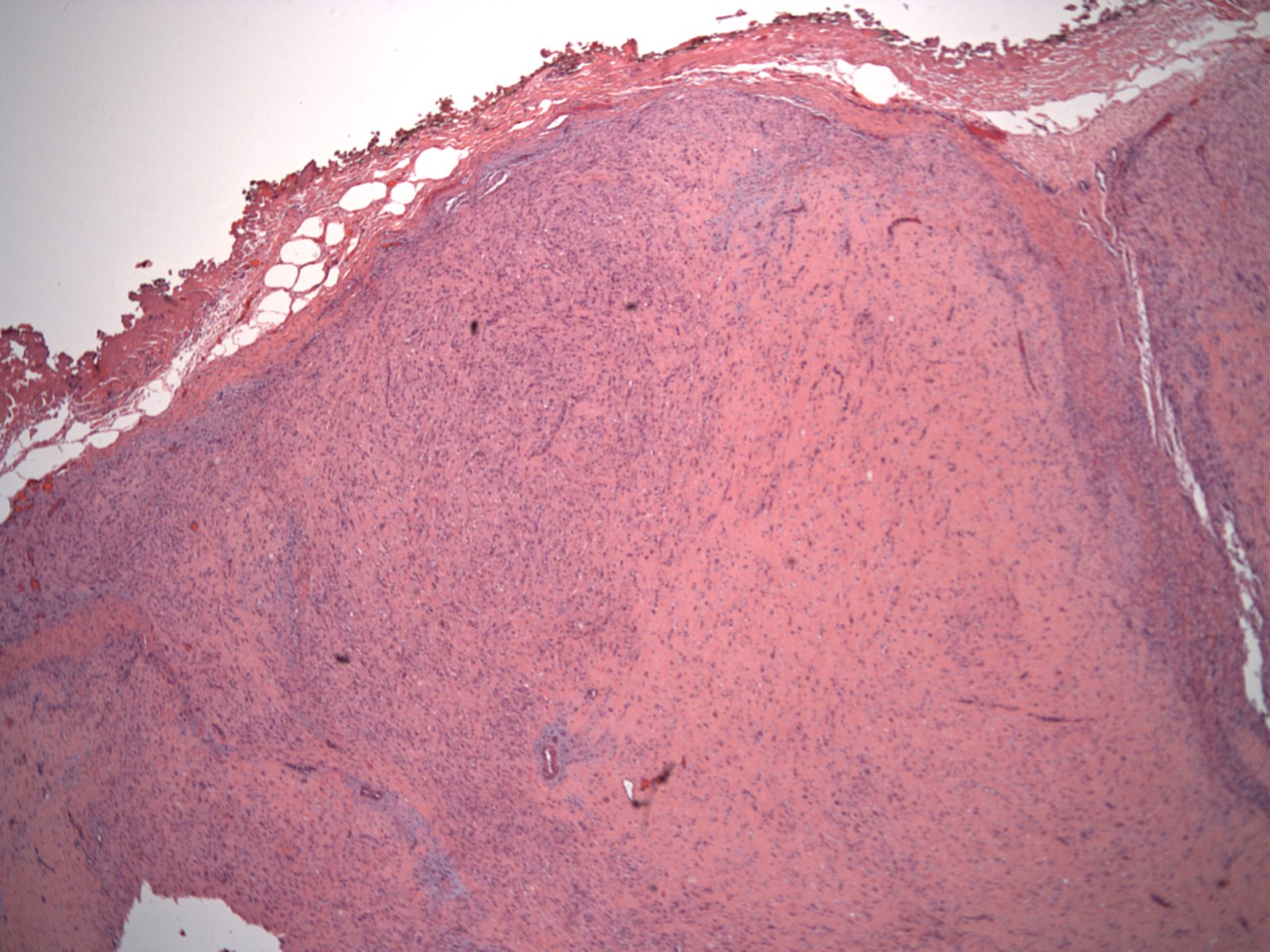
Microscopic (histologic) description
- Similar morphologic features to nodular fasciitis
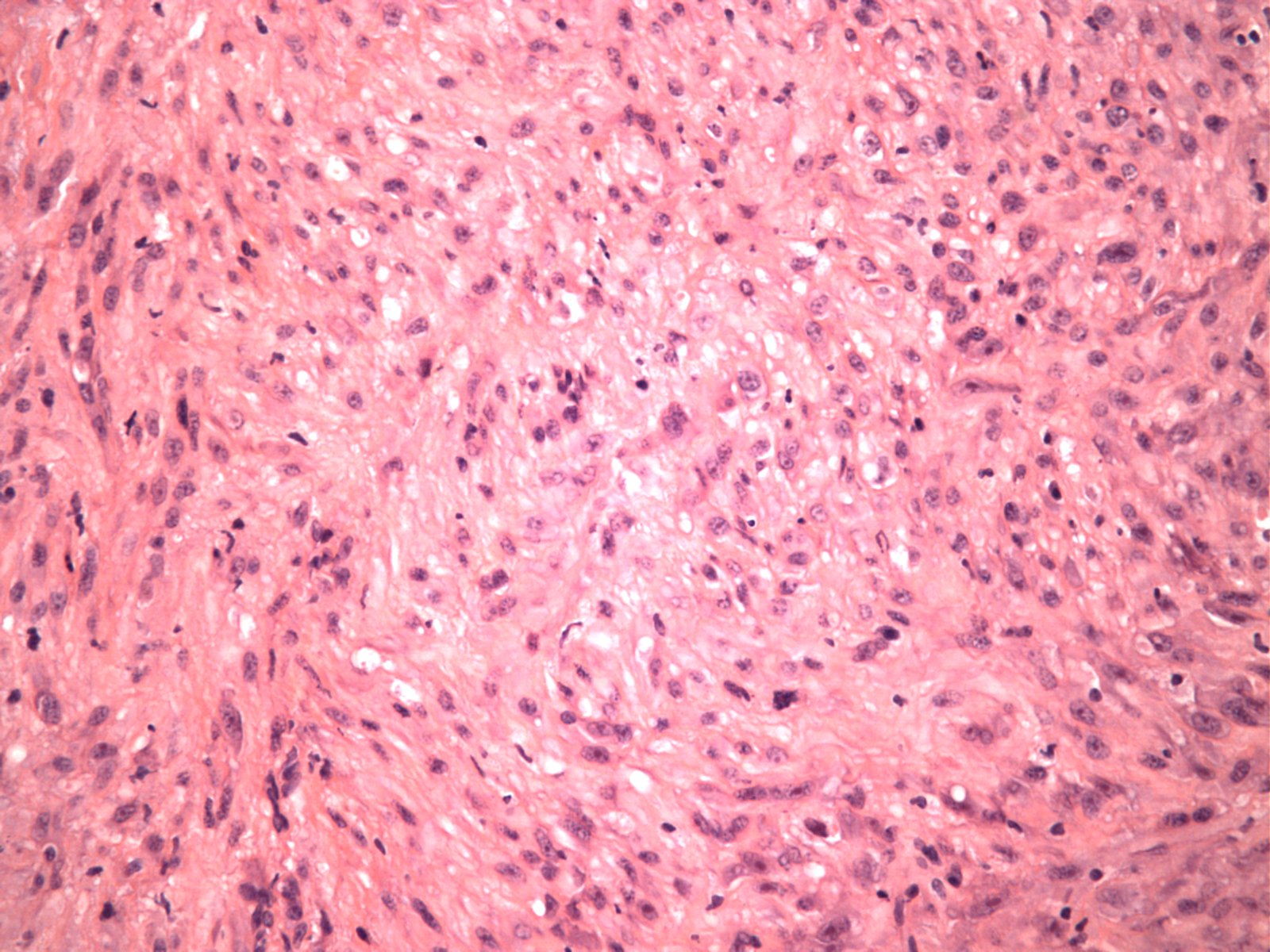
- Plump myofibroblastic / fibroblastic spindle cells
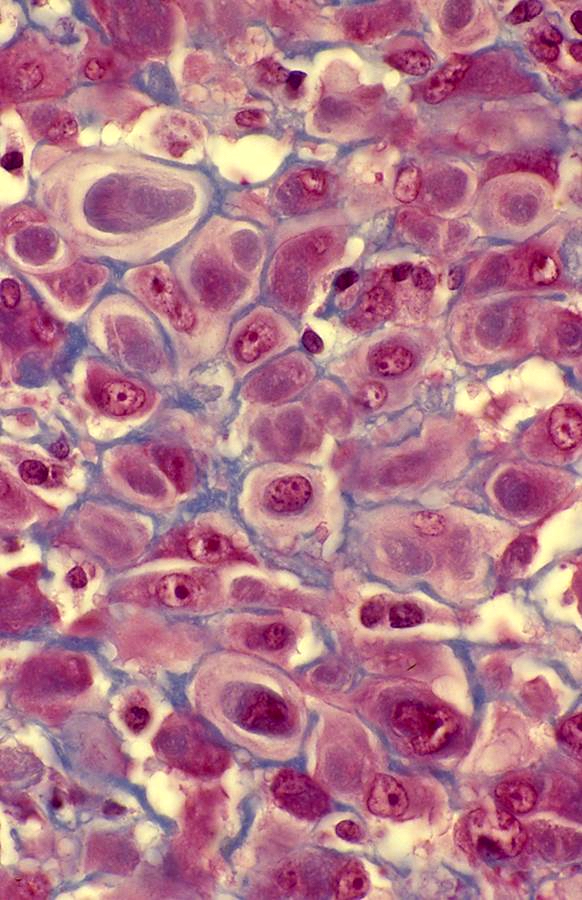
- Large ganglion-like cells with round nuclei, prominent nucleoli and abundant amphophilic cytoplasm (Cancer 1975;36:1450)
- Density of ganglion-like cells (modified fibroblasts) varies
- Mitotic figures are found in both spindle and ganglion-like cells and may be numerous
- No atypical mitotic figures
- Loose tissue culture, myxoid to collagenous stroma
- Older lesions may have abundant hyalinized collagen
- Extravasated red blood cells and stromal lymphocytes are common
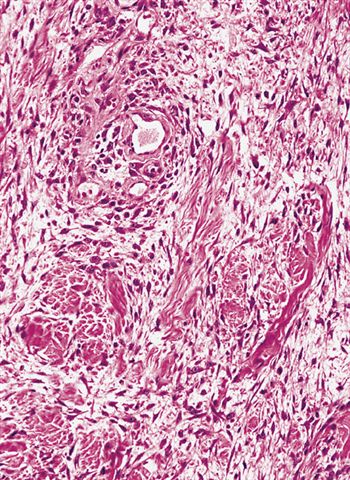
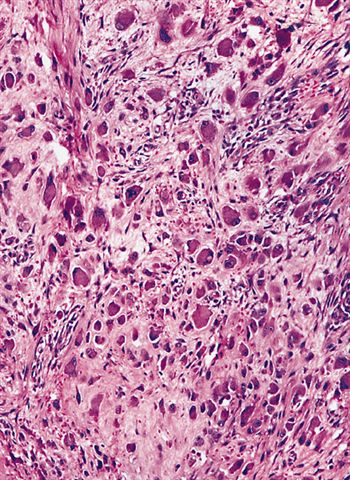
- Borders of lesion are typically infiltrative or ill defined
- Often grows along fibrous connective tissue septa
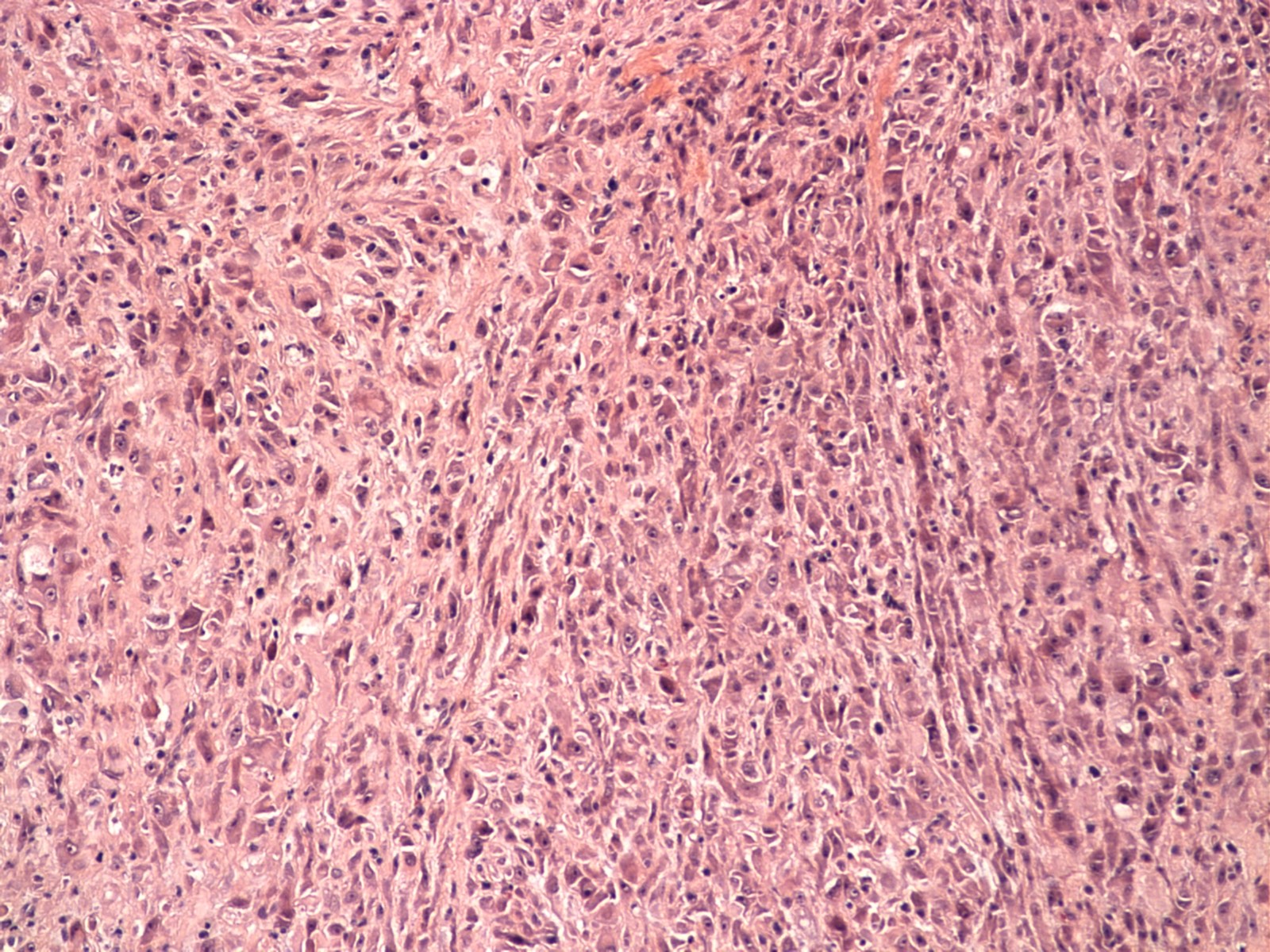
- Childhood subtype generally has better delineated borders, greater cellularity, less collagen production, increased mitotic activity, less myxoid change and a predominance of ganglion-like cells (Am J Surg Pathol 1992;16:364)
- Focal necrosis and acute inflammation may be present in pediatric cases (Am J Surg Pathol 1992;16:364)
- Focal metaplastic bone is rare
Microscopic (histologic) images
Contributed by Jeanne Meis, M.D. and AFIP
Contributed by Meggen Walsh, D.O., M.S., P.A. and Dana Richards, M.D.
Childhood variant
Cytology description
- Spindle cells with long cytoplasmic processes to plumb cells with round to oval nuclei
- Collagen fragments and large ganglion-like cells with dense cytoplasm and prominent nucleoli (Am J Clin Pathol 2009;132:857)
- Ganglion-like cells with 1 - 2 large eccentric nuclei
- Giant ganglion-like cells are at least twice the size of plump fibroblasts (Acta Cytol 2002;46:1049)
- Nuclei of ganglion-like cells are cytologically benign with thin, smooth nuclear membranes and fine chromatin (Acta Cytol 2002;46:1049)
Positive stains
- Vimentin
- Spindle cells usually express SMA and MSA, which may be weak and focal in ganglion-like cells (APMIS 1992;100:437, Am J Surg Pathol 1992;16:364)
- Epithelioid cells show diffuse strong expression of c-FOS (Mod Pathol 2021;34:942)
- Small subset has diffuse expression of FOSB (Am J Surg Pathol 2017;41:596)
- CD68 may show focal or limited staining (Am J Surg Pathol 1992;16:364)
Negative stains
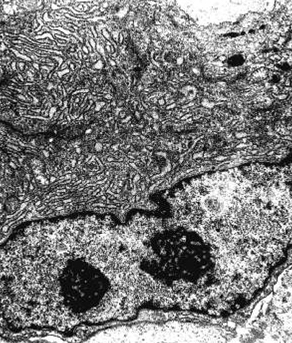
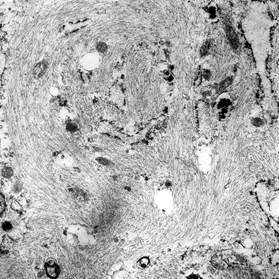
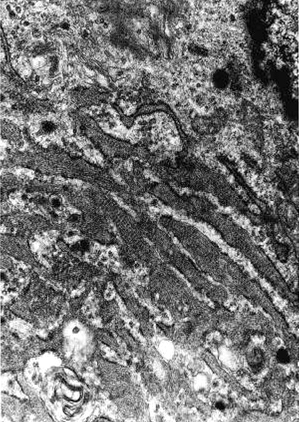
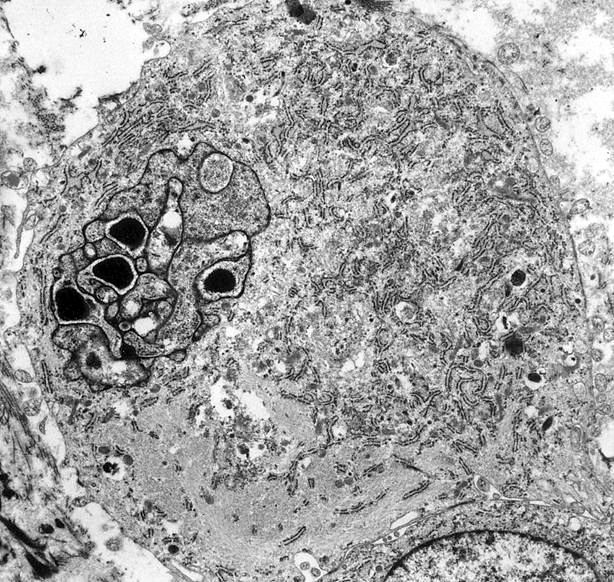
Electron microscopy description
- Numerous cytoplasmic thin filaments with occasional dense bodies, abundant rough endoplasmic reticulum and cellular membrane based vesicles (Arch Pathol Lab Med 1981;105:542)
- Ganglion-like cells are modified myofibroblasts with abundant rough endoplasmic reticulum, thin filaments and intracytoplasmic collagen production
- Extracellular matrix consists of collagen fibrils (Am J Surg Pathol 1992;16:364)
Electron microscopy images
Molecular / cytogenetics description
- Adult tumors have shown FOS gene rearrangements, including FOS::VIM fusion (Mod Pathol 2021;34:942)
Molecular / cytogenetics images
Videos
Proliferative fasciitis: 5 minute pathology pearls
Proliferative fasciitis & myositis explained by a soft tissue pathologist
Sample pathology report
- Soft tissue, right forearm, excision:
- Proliferative fasciitis (see comment)
- Comment: This excision specimen shows a small subcutaneous nodule (1.5 cm) composed of proliferating myofibroblasts with scattered large ganglion-like cells. Several mitotic figures are present; however, no atypical mitotic figures and no areas of necrosis are identified. Immunohistochemical stains show that the lesional cells are positive for vimentin and SMA, while they are essentially negative for desmin, keratin and S100 protein. These results support the above diagnosis. All control slides stained appropriately.
Differential diagnosis
- Nodular fasciitis:
- More common in younger adults
- Histologically similar
- Lacks ganglion-like cells
- Well circumscribed
- USP6 gene rearrangement (most commonly MYH9::USP6)
- Reactive myofibroblastic proliferations:
- Intra-abdominal adhesions or incarcerated hernias
- Often have a prominent component of adipose tissue
- Clinical presentation is different
- Inflammatory myofibroblastic tumor (IMT):
- Myofibroblastic nature of tumor cells
- Usually arises in lungs or abdominal soft tissue of children and young adults
- Occasional ganglion-like cells are common in conventional IMT (Am J Surg Pathol 2011;35:135)
- Epithelioid variant has more prominent epithelioid / round cell morphology
- 50% harbor ALK gene rearrangements
- Diffuse cytoplasmic or perinuclear (in epithelioid variant) staining pattern with ALK
- Inflammatory infiltrate composed of plasma cells, lymphocytes or neutrophils (in epithelioid variant)
- May show strong expression of desmin
- Ganglioneuroblastoma:
- Mixture of immature neuroblasts and ganglion cells
- Most occur in first 4 years of life, rarely occurs in adults
- Neuroblasts positive for NSE, CD56, synaptophysin and chromogranin
- Ganglion cells positive for S100 protein, synaptophysin and neurofilament protein
- Embryonal rhabdomyosarcoma:
- Pleomorphic rhabdomyosarcoma:
- Undifferentiated pleomorphic sarcoma:
- Older adults
- Usually large, intramuscular tumors
- Markedly pleomorphic cells
- More irregular nuclear features and chromatin pattern
- Numerous atypical mitotic figures and necrosis
- Fibrosarcoma:
- Predominantly composed of spindle cells
- Usually lacks pleomorphic cells
- Deep, large mass of longer duration
- Osteosarcoma:
- True tumor osteoid production, as opposed to stromal hyalinization
- Epithelioid osteoblasts may resemble ganglion-like cells
- Osteoblasts positive for SATB2
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2
A. FOS. A subset of cases of proliferative fasciitis have been described as having FOS gene rearrangements, similar to epithelioid hemangioma and osteoid osteoma / osteoblastoma. USP6 gene rearrangements, including MYH9::USP6 fusion, have been described in nodular fasciitis, while GNAS gene rearrangements have been described in fibrous dysplasia and intramuscular myxoma.
Comment Here
Reference: Proliferative fasciitis
Comment Here
Reference: Proliferative fasciitis