Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rehman OU, Dehner C. Plexiform fibrohistiocytic tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueplexiformfh.html. Accessed April 2nd, 2025.
Definition / general
- Uncommon, biphasic dermal or subcutaneous mesenchymal neoplasm
- Variable mixture of fibroblasts and histiocyte-like cells in a plexiform or multinodular arrangement
Essential features
- Neoplasm involving the dermis or subcutis
- Nodules of histiocytoid cells surrounded by fascicles of myofibroblastic spindle cells
- Plexiform growth pattern
- Osteoclast-like giant cells
Terminology
- First described in 1988 (Am J Surg Pathol 1988;12:818)
- Abbreviations: plexiform fibrohistiocytic tumor (PFHT)
- Other name(s): plexiform fibrous histiocytoma
ICD coding
- ICD-O: 8835/1 - plexiform fibrohistiocytic tumor
- ICD-11: 2F7C & XH4GL1 - neoplasms of uncertain behavior of connective or other soft tissue & plexiform fibrohistiocytic tumor
Epidemiology
- Most common in infants, children and young adults
- Rarely occurs after the age of 30 (Int J Clin Exp Pathol 2016;9:4693)
- F > M (Arch Pathol Lab Med 2007;131:1135, Ann Diagn Pathol 2007;11:313, Am J Surg Pathol 1999;23:662)
Sites
- Most common: upper extremity (40 - 50%), usually fingers, hand, wrist
- Other sites: lower extremity (9 - 20%), trunk (8 - 15%), head and neck (7 - 10%) (Case Reports Plast Surg Hand Surg 2021;8:164, Ann Diagn Pathol 2007;11:313, Am J Surg Pathol 1999;23:662, Histopathology 1991;19:503, Am J Surg Pathol 1988;12:818)
Pathophysiology
- Exact etiology and pathophysiology unknown (Virchows Arch 2022;481:739)
- Preceding trauma reported in a few cases (Arch Pathol Lab Med 2007;131:1135)
- Congenital cases identified in 2 series (Arch Pathol Lab Med 2007;131:1135)
Etiology
- Unknown
Clinical features
- Small (1 - 3 cm, rarely larger) dermal or subcutaneous mass
- Slow growing, usually asymptomatic
- Overlying skin is usually raised and firm with ill defined borders
- Rarely: central depression, discoloration, ulceration
- Can also occur as a flattened, indurated plaque (less frequently)
- Reference: Case Reports Plast Surg Hand Surg 2021;8:164
Diagnosis
- Combined history, physical examination, imaging (ultrasound, MRI) and pathological diagnosis
Radiology description
- Ultrasound: hypoechoic nodule or discrete mass with some vascularity on color Doppler
- MRI: poorly demarcated, infiltrative mass
- Can appear as a plaque-like or infiltrative lesion in the subcutaneous tissues, sometimes without a discrete mass (Skeletal Radiol 2019;48:437)
- Isointense on T1 weighted images, hyperintense on fluid sensitive images and enhancing after gadolinium administration
- Can show contact with or abutment of underlying connective tissues (tendons, muscles, bone)
Radiology images
Prognostic factors
- No well documented prognostic factors
- Overall prognosis is good after complete excision (J Clin Diagn Res 2022;16:ED01)
- High local recurrence rate after incomplete excision
- Rare cases of lymph node and distant metastasis have been reported (Am J Surg Pathol 1988;12:818, Am J Surg Pathol 1997;21:469, Am J Surg Pathol 1999;23:662)
Case reports
- Newborn boy with a painful congenital ulcerated plaque on left foot (Pediatr Dermatol 2018;35:e360)
- 4 year old boy with a foot nodule since birth (Case Reports Plast Surg Hand Surg 2021;8:164)
- 9 year old boy with a slow growing, painless mass lesion in the left back region (Case Rep Pathol 2013;2013:547372)
- 12 year old girl with a lesion on the back of her hand (Actas Dermosifiliogr 2022;113:821)
- 23 year old woman with a nodular lesion in vulva (Rev Bras Cancerol 2021;67:e141269)
- 40 year old woman with a central neck mass clinically mimicking a thyroglossal duct cyst (Head Neck Pathol 2020;14:262)
- 45 year old woman with a lesion in the right popliteal fossa; tumor showed myxoid changes (Case Rep Pathol 2017;2017:5370894)
- 46 year old woman with tumor involving frontal region of head with underlying frontal bone invasion (J Clin Diagn Res 2022;16:ED01)
Treatment
- Complete surgical resection with wider margins to prevent local recurrence
- High local recurrence rate (Arch Pathol Lab Med 2007;131:1135)
- Long term follow up is recommended to detect nodal or pulmonary metastasis
Clinical images
Gross description
- White-gray tumor, averaging 1 - 3 cm in size (range: 0.3 - 8.5 cm) (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
- Firm consistency
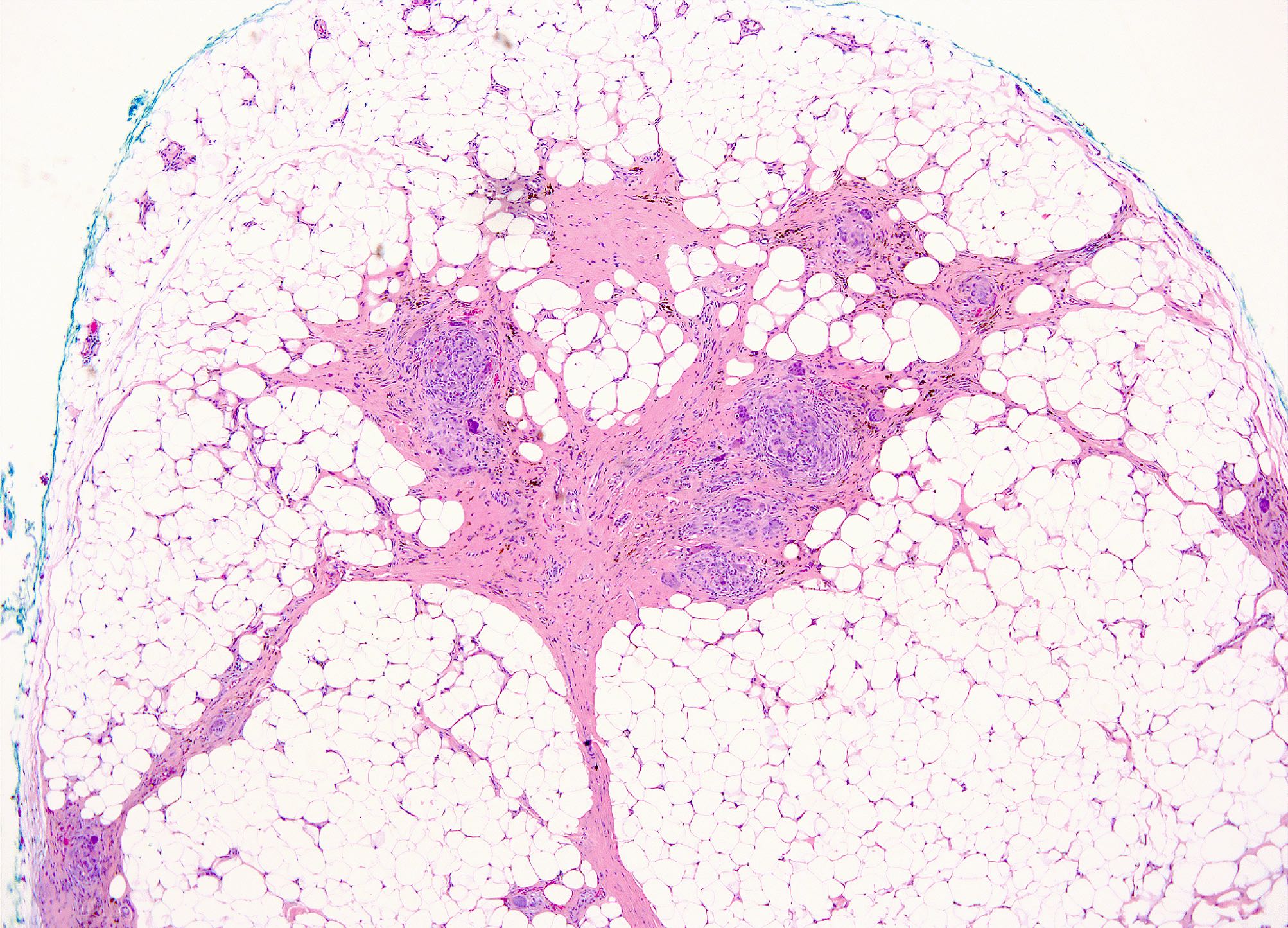
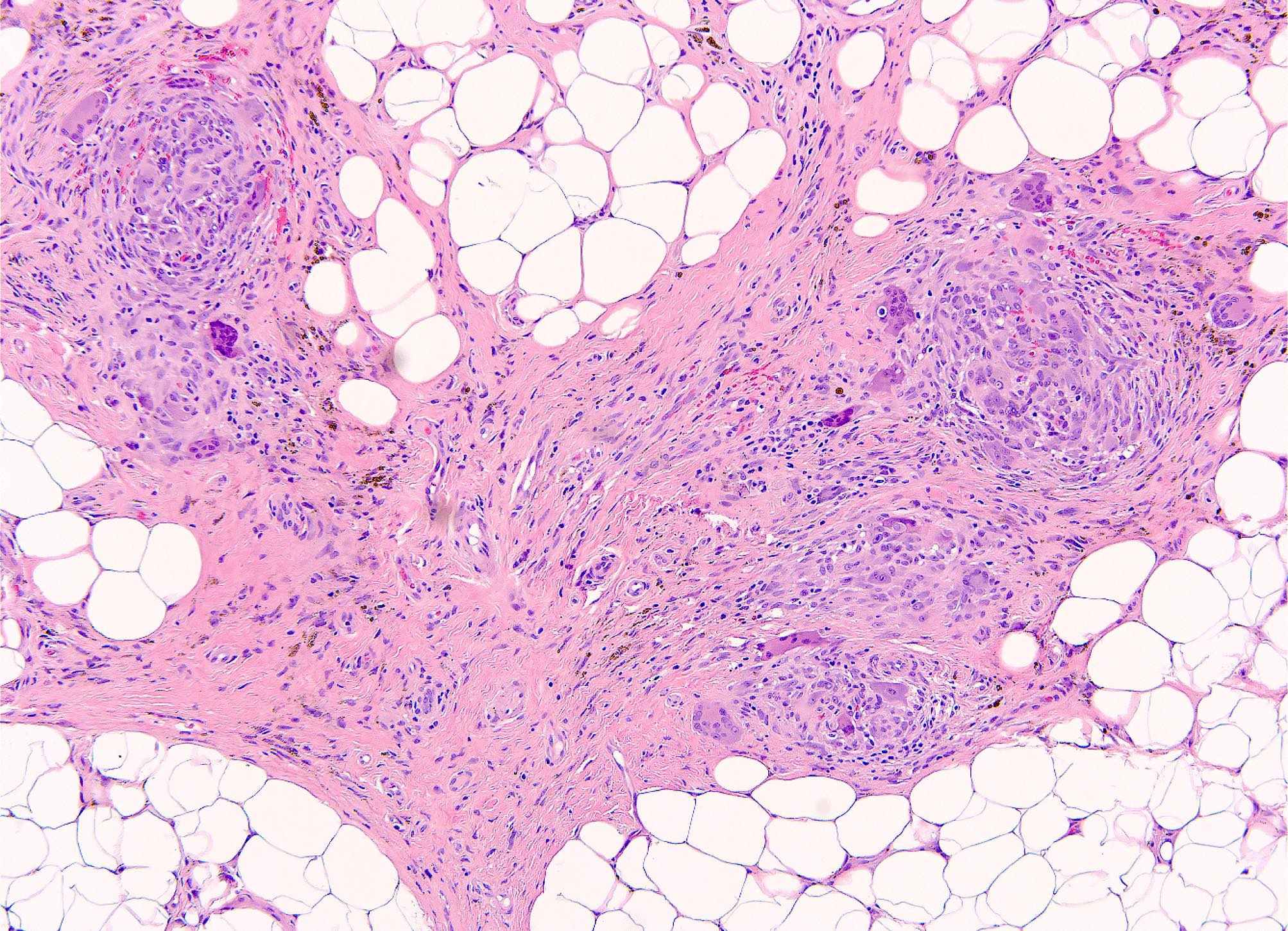
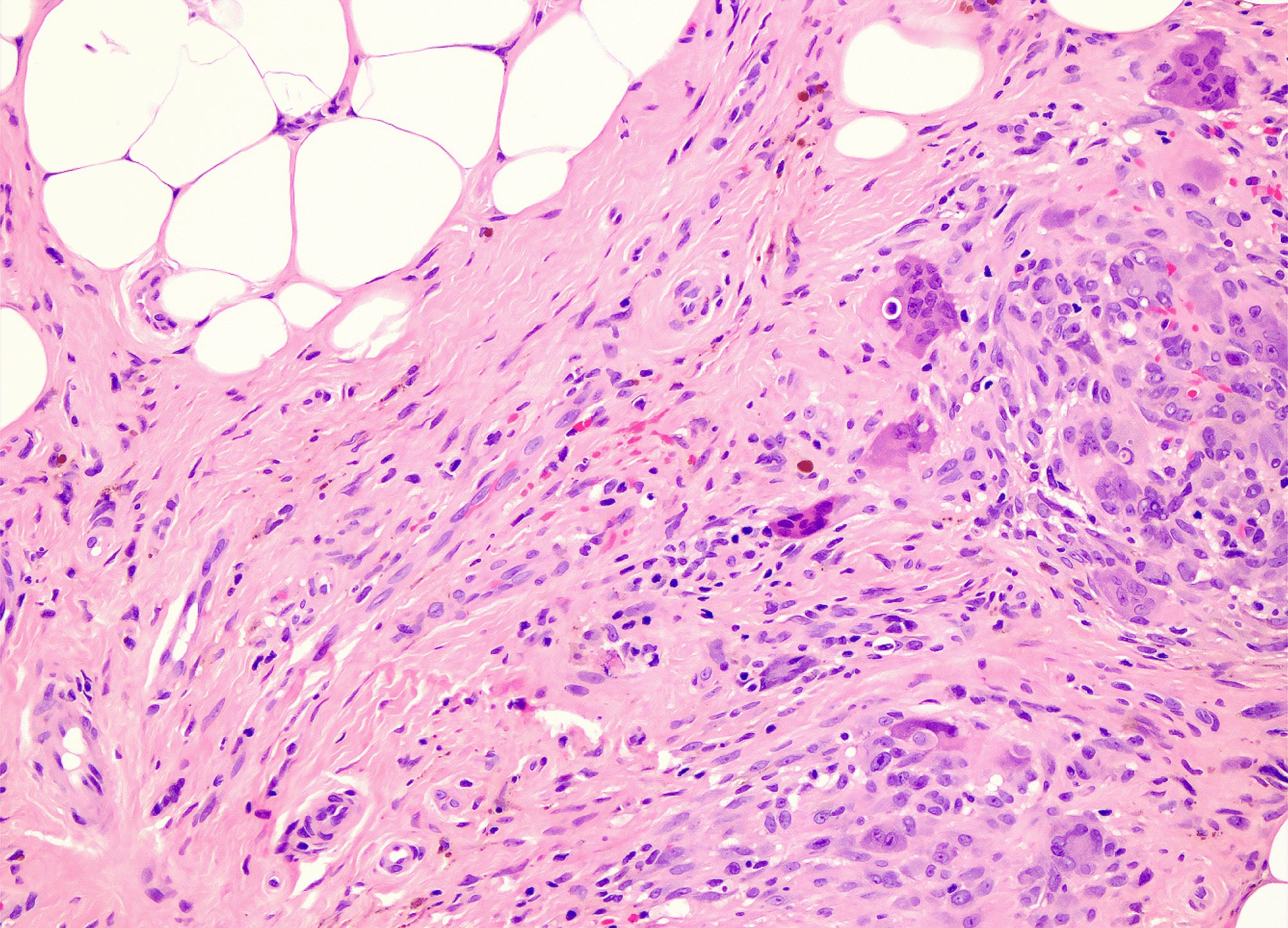
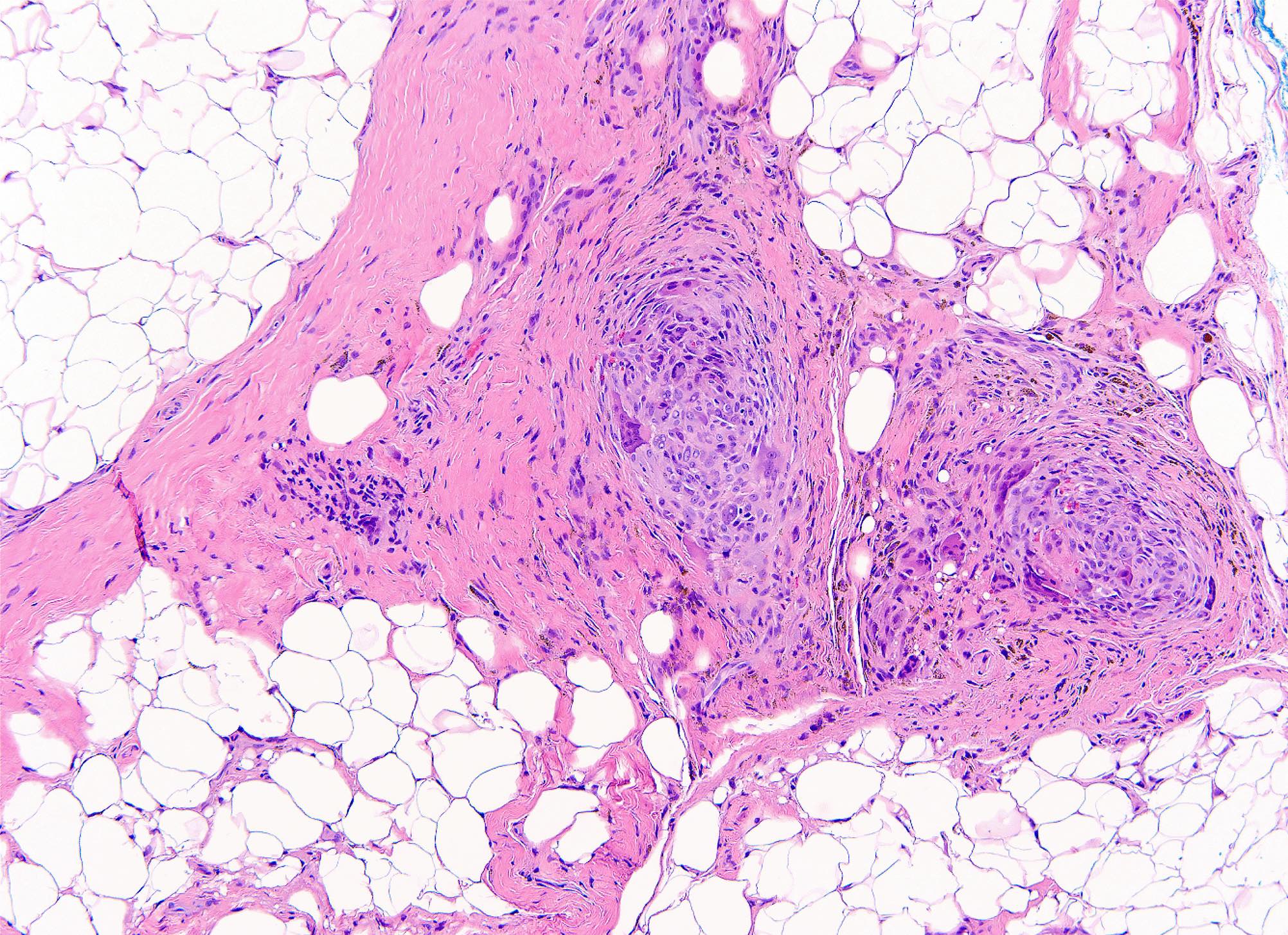
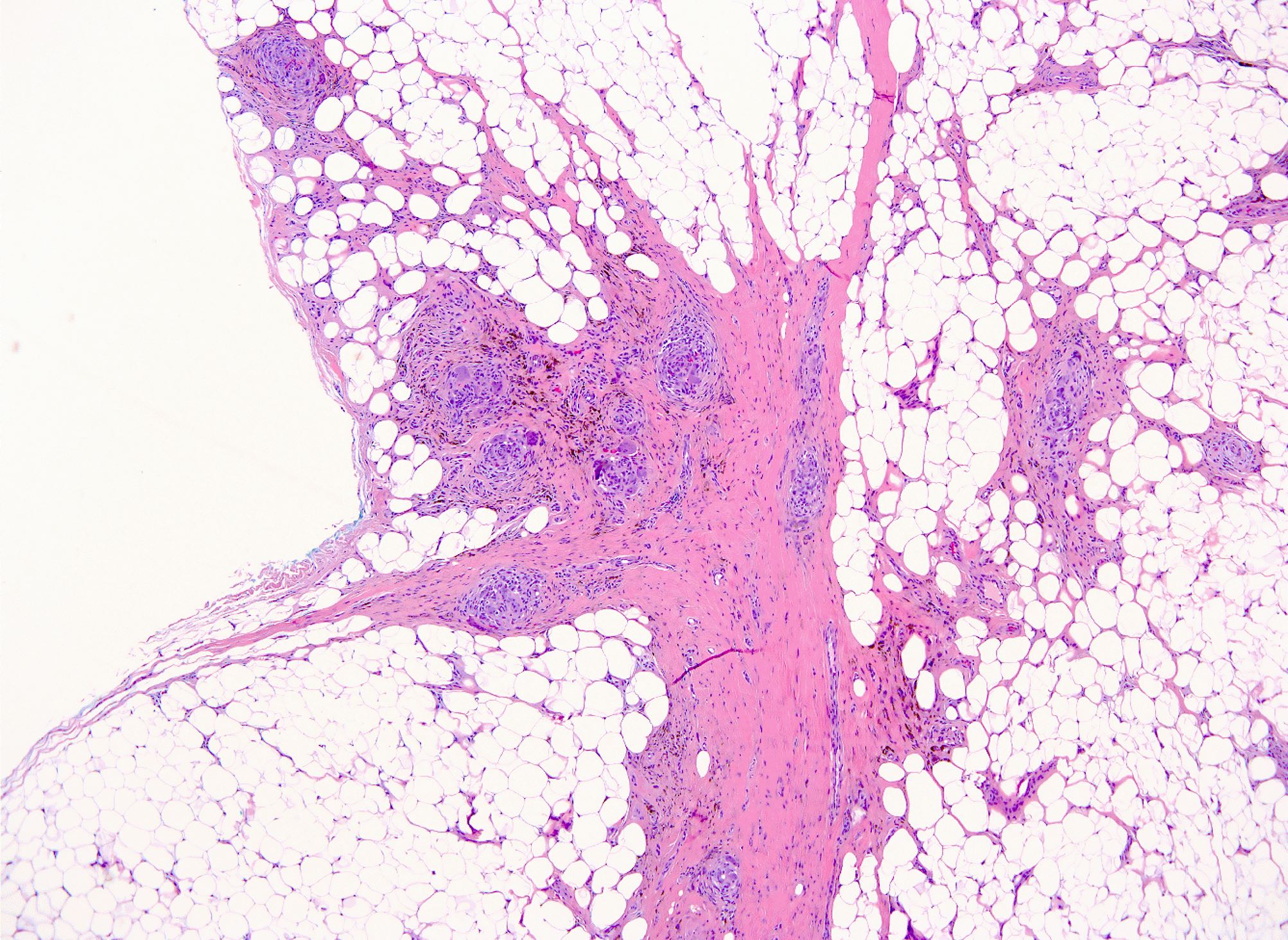
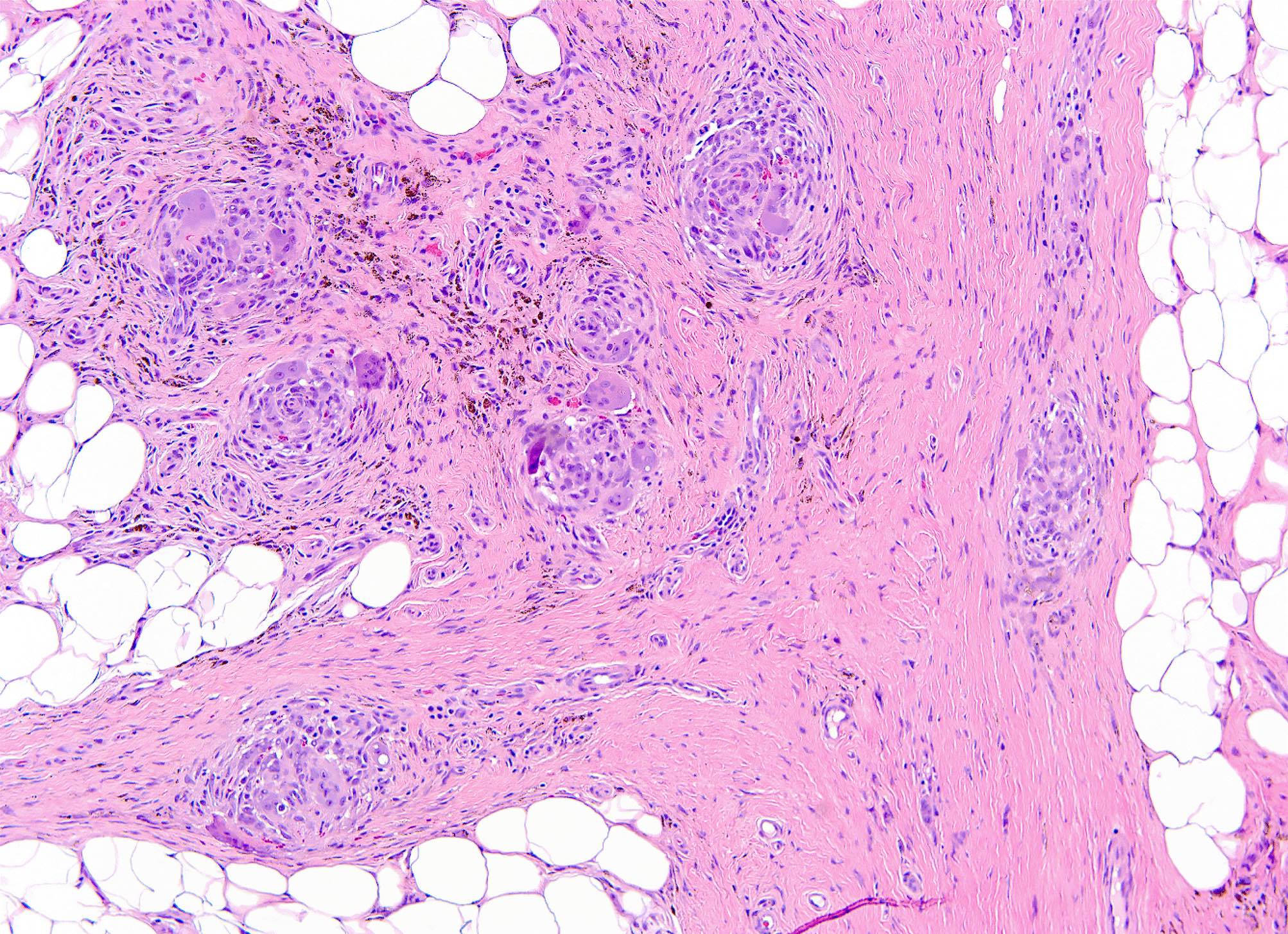
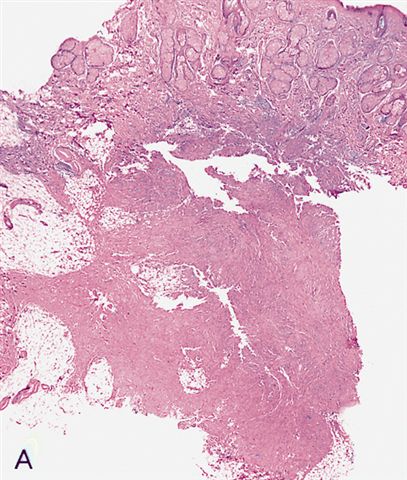
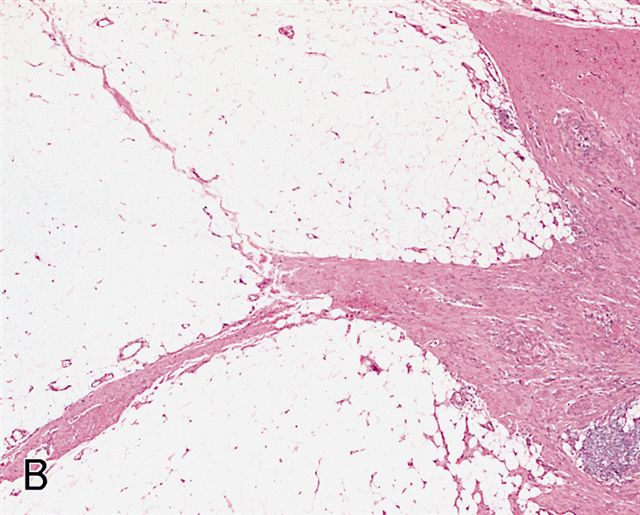
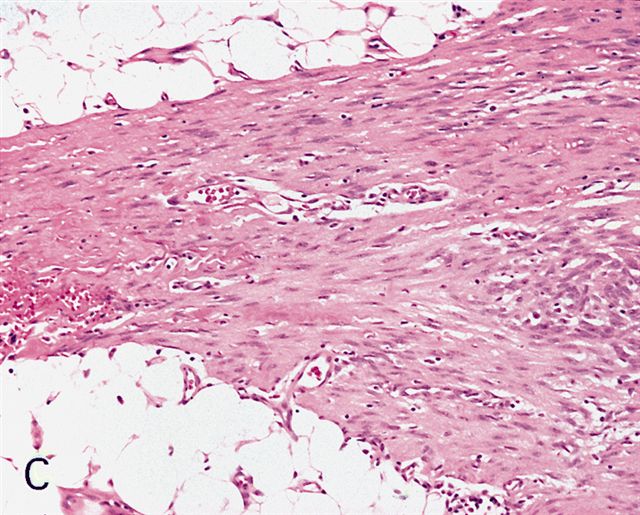
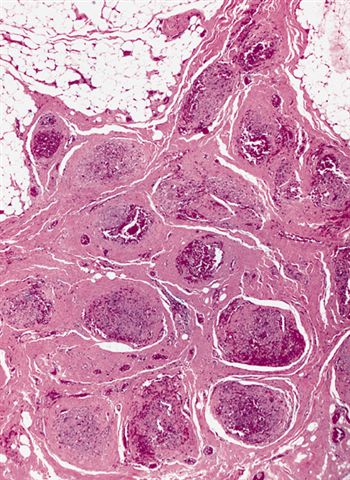
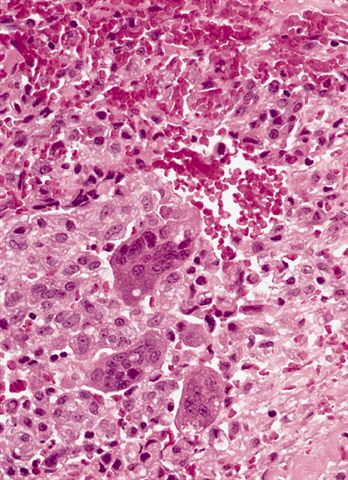
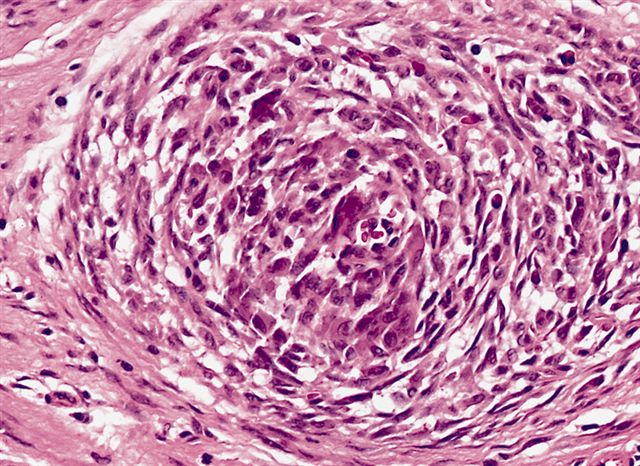
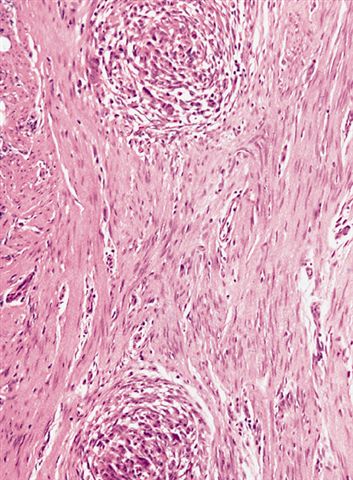
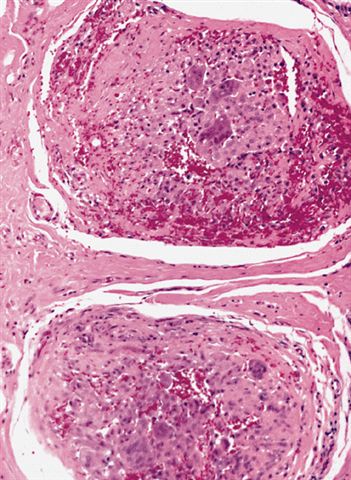
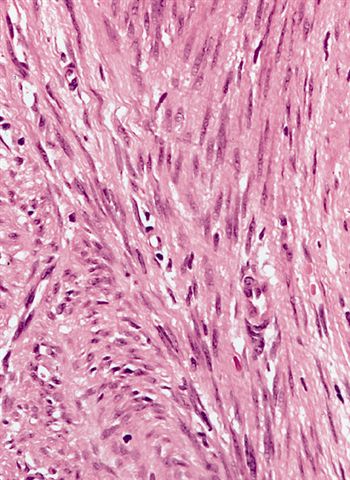
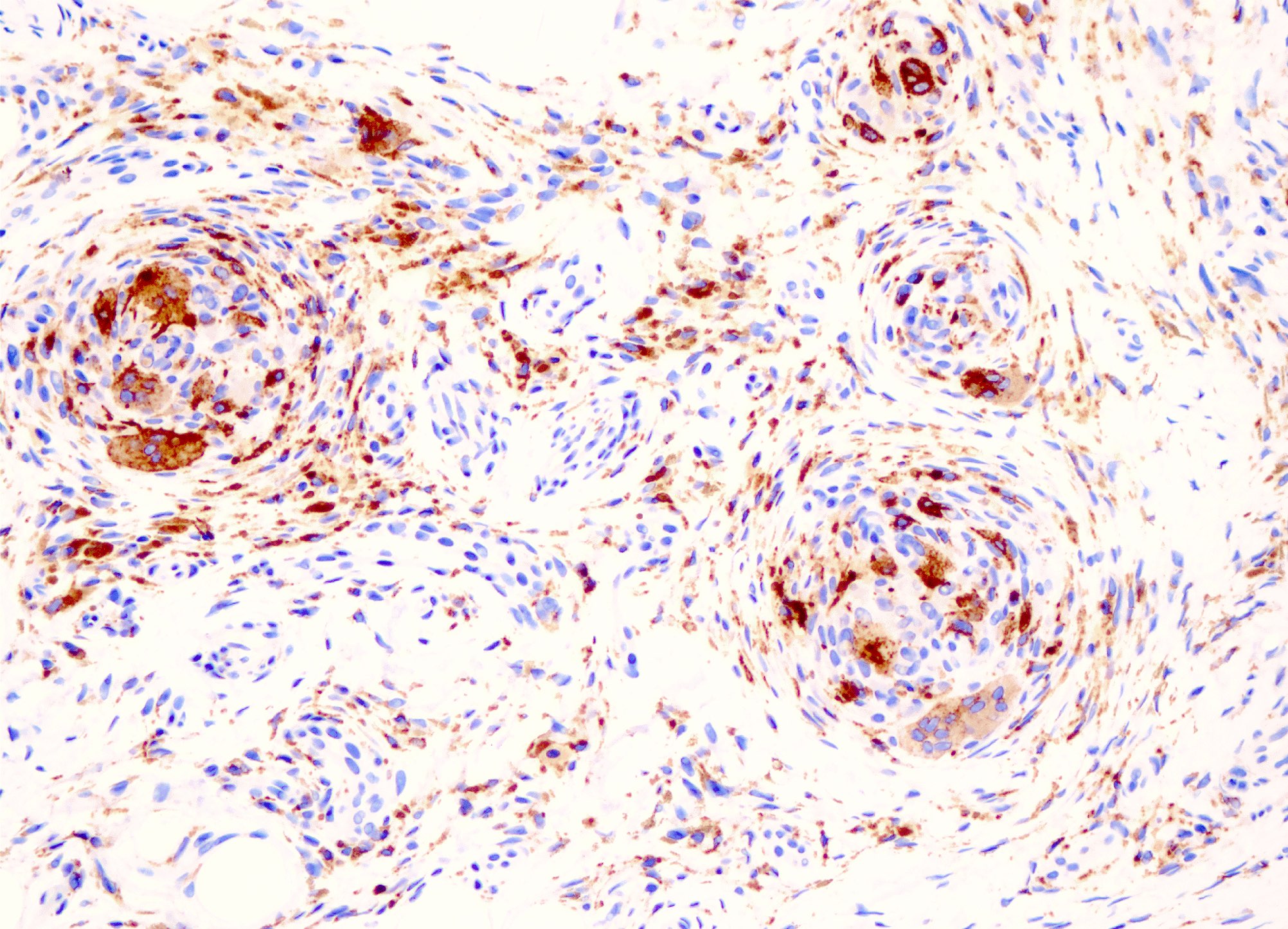
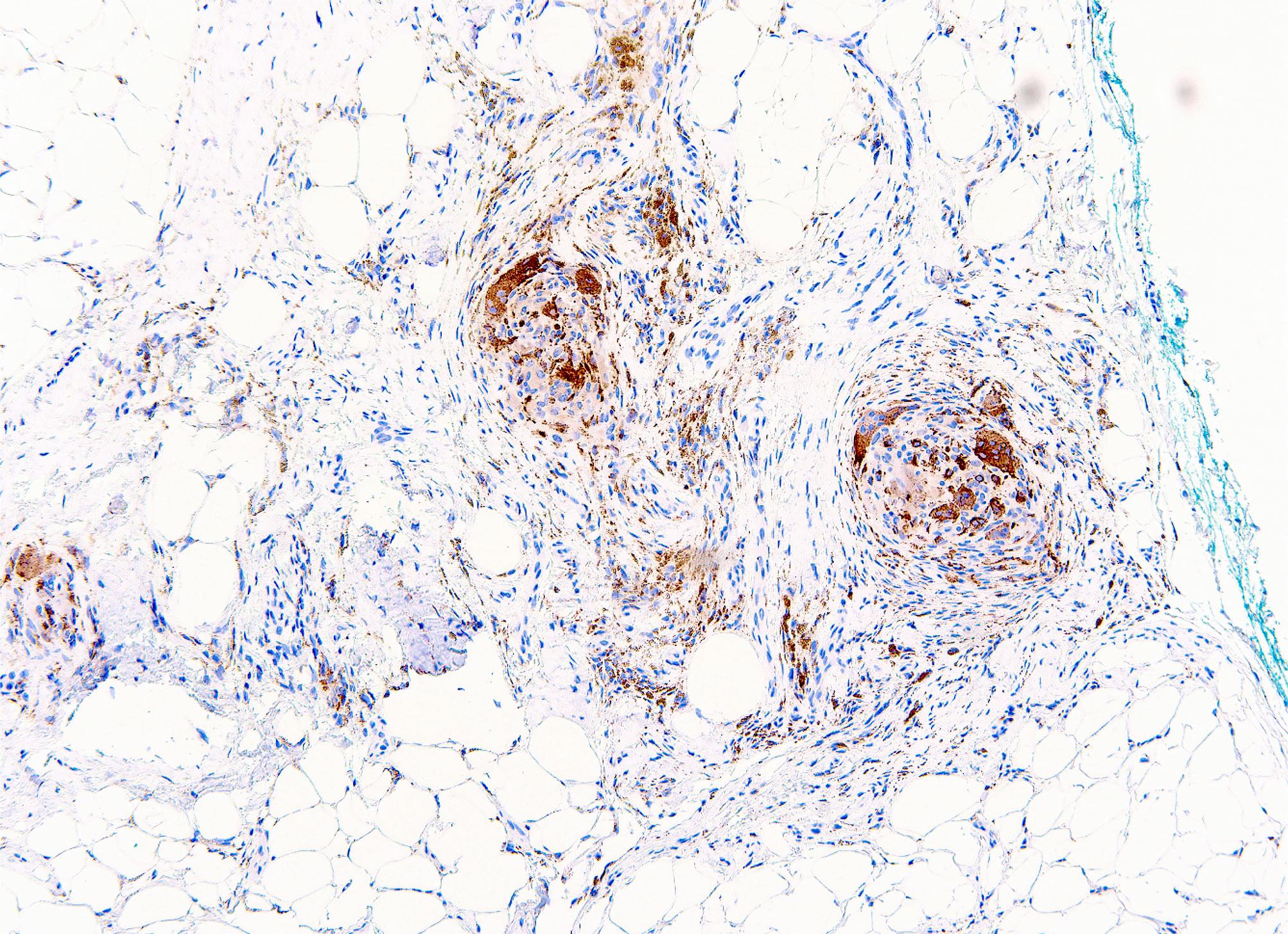
Microscopic (histologic) description
- Centered on dermal / subcutaneous junction
- Multinodular and plexiform architecture, can often be infiltrative
- Normal overlying epidermis (usually)
- Mixture of fascicles of spindle cells and nodular aggregates of histiocytoid cells in variable proportion
- Fascicles of uniform, eosinophilic (myo)fibroblasts
- Nodules of histiocytoid cells, often with osteoclast-like giant cells
- No atypia or pleomorphism
- Low mitotic count (usually 0 - 2 mitotic figures [MF]/10 high power fields [HPF]), no necrosis
- Stroma can show hyalinization or myxoid change; rarely metaplastic bone formation
- Microhemorrhage and hemosiderin deposition can occur
- Invasion into underlying skeletal muscle can occur
- Vascular invasion in ~20% of cases (Fletcher: Diagnostic Histopathology of Tumors, 5th Edition, 2020)
- Variants: fibroblastic, histiocytic, mixed (Am J Surg Pathol 1999;23:662, Ann Diagn Pathol 2007;11:313)
- Fibroblastic
- Fascicles of spindled (myo)fibroblasts
- Plexiform to infiltrative growth pattern
- Ray-like extensions into subcutaneous tissue
- Chronic inflammation
- Histiocytic
- Mononuclear histiocytoid cells
- Multinodular growth
- Multinucleated osteoclast-like giant cells
- Mixed
- Nodules of histiocytoid cells separated by fascicles of spindle cells
- Fibroblastic
Microscopic (histologic) images
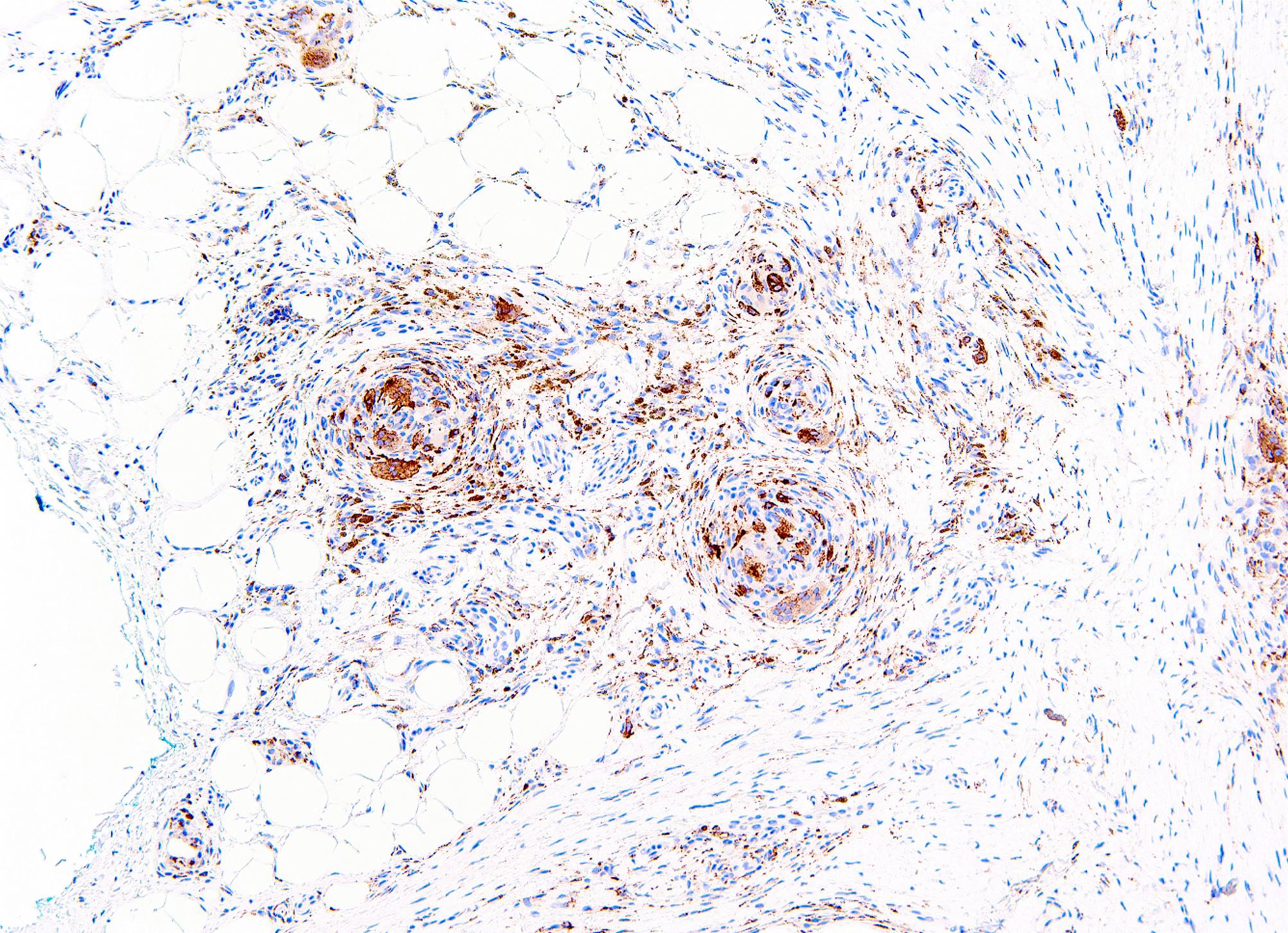
Contributed by Carina Dehner, M.D., Ph.D. and AFIP
Cytology description
- Plump fibroblastic spindle cells and histiocytoid cells
- Scattered multinucleated osteoclast-like giant cells (Arch Pathol Lab Med 2007;131:1135)
- No significant pleomorphism (Head Neck Pathol 2020;14:262)
- Fine, granular myxoid background
Positive stains
Electron microscopy description
- Tumor cells have features of myofibroblasts and histiocyte-like cells (Pathol Res Pract 1992;188:350)
- Myofibroblast-like cells have abundant thin cytoplasmic filaments associated with dense bodies (Histopathology 1991;19:503, Pathol Res Pract 1992;188:350)
- Histiocyte-like cells have lysosomes and multiple filopodia (Pathol Res Pract 1992;188:350)
Molecular / cytogenetics description
- Specific chromosomal abnormalities have not been identified
- So far, no specific molecular aberrations have been identified (Virchows Arch 2022;481:739)
- CSF1 chromogenic in situ hybridization (CISH) shows null cell population (Virchows Arch 2022;481:739)
Videos
Plexiform fibrohistiocytic tumor (case 3) by Dr. Melanie Bourgeau
Kaposiform hemangioendothelioma, plexiform fibrohistiocytic tumor, etc. by Dr. Jerad Gardner
Sample pathology report
- Soft tissue, right small finger, excision:
- Fibrohistiocytic neoplasm involving adipose tissue, consistent with plexiform fibrohistiocytic neoplasm, extends to inked tissue edges (see comment)
- Comment: Sections show a neoplasm composed of a mix of nodules containing epithelioid histiocytes with scattered osteoclast type giant cells and fascicles of spindled fibroblastic cells involving adipose tissue. The cytomorphology of the tumor cells is bland without significantly increased mitotic activity or nuclear pleomorphism. Immunohistochemical stains show that the histiocytes are positive for CD68, while S100, MITF and keratin AE1 / AE3 are negative. CD34 is patchy positive. Given that the tumor extends to the inked tissue edges, a narrow re-excision to obtain clear margins and to reduce the risk of local recurrence could be considered.
Differential diagnosis
- Cellular neurothekeoma:
- Epithelioid to spindled cells arranged in nests divided by dense fibrous septa
- Myxoid change is common
- Nuclear pleomorphism (25%)
- Mitotic activity is common, can have atypical mitoses
- Osteoclastic or Touton multinucleated giant cells
- Podoplanin positive
- CD63 (NKI-C3), PGP9.5 and MITF positive
- Dermatofibroma:
- Older patients
- No nodules of histiocytoid cells
- No osteoclast-like giant cells
- No plexiform extensions of fibrous tissue
- Giant cell tumor of soft tissue:
- Prominent nodules with abundant osteoclast-like giant cells
- No infiltrative spindle cell component
- Peripheral shell or rim of woven bone (~50%)
- Frequent mitoses
- Fibromatosis:
- No nodules of histiocytoid and osteoclast-like giant cells
- Characteristic stromal vasculature
- Nuclear beta catenin positive
- Low grade myofibroblastic sarcoma:
- Predominantly adults
- Frequently in head and neck region
- Arises in deep subcutaneous tissue or skeletal muscle
- Diffusely infiltrative, often with checkerboard pattern
- At least focal mild to moderate atypia (enlarged nuclei, hyperchromasia)
- SMA positive / myofibroblastic immunophenotype
- Nodular fasciitis:
- Small, rapidly growing, well circumscribed
- Myxoid stroma, especially in early stages
- No multinodular or plexiform growth
- MYH9::USP6 fusion
- Fibrous hamartoma of infancy:
- Predominantly infants
- Common in axilla
- Foci of immature mesenchymal tissue, myxoid stroma
- Pilar leiomyoma:
- Neurofibroma:
- No distinct nodule formation
- S100 positive
Board review style question #1
Board review style answer #1
D. Plexiform fibrohistiocytic tumor (PFHT). The image shows a tumor consisting of nodules of mononuclear histiocytoid cells and many multinucleated osteoclast type giant cells. Between the nodules are fascicles of spindle cells (myofibroblasts). This is the appearance of plexiform fibrohistiocytic tumor. The age, size and location are also supportive of this diagnosis. Answer A is incorrect because a cellular neurothekeoma does not show this pattern of nodular and plexiform growth and it commonly shows mitotic activity and dense collagen septa. Answer E is incorrect because a schwannoma has hypercellular Antoni A areas (often with Verocay bodies) and myxoid hypocellular Antoni B areas, which are not seen here. Answer B is incorrect because fibromatosis does not contain nodules of histiocytoid and osteoclast-like giant cells and it has a characteristic stromal vasculature. Answer C is incorrect because giant cell tumor of soft tissue commonly shows mitotic activity (sometimes brisk) and a peripheral rim of metaplastic bone. The osteoclastic giant cells are also more evenly distributed throughout the tumor as compared to PFHT.
Comment Here
Reference: Plexiform fibrohistiocytic tumor
Comment Here
Reference: Plexiform fibrohistiocytic tumor
Board review style question #2
Which of the following is a frequent occurrence in plexiform fibrohistiocytic tumor?
- Brisk mitotic activity
- Characteristic vasculature
- Involvement of epidermis
- Multinucleated giant cells
- Nuclear pleomorphism
Board review style answer #2
D. Multinucleated giant cells. Plexiform fibrohistiocytic tumor frequently contains multinucleated osteoclast type giant cells. Answer A is incorrect because plexiform fibrohistiocytic tumor (PFHT) does not have significantly increased mitotic activity. Brisk mitoses should lead to consideration of other diagnoses. Answer E is incorrect because cells of PFHT are usually bland and exhibit no significant nuclear pleomorphism. Answer C is incorrect because PFHT predominantly affects the dermal / subcutaneous junction and the overlying epidermis is usually uninvolved. Answer B is incorrect because PFHT does not exhibit a characteristic vasculature, such as that seen in fibromatosis or other tumors.
Comment Here
Reference: Plexiform fibrohistiocytic tumor
Comment Here
Reference: Plexiform fibrohistiocytic tumor