Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Perret R. Pleomorphic hyalinizing angiectatic tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuephat.html. Accessed April 2nd, 2025.
Definition / general
- Rare and underrecognized soft tissue tumor of intermediate malignancy (locally aggressive) characterized by the presence of pleomorphic cells, low mitotic activity, ectatic blood vessels with damaged walls and no necrosis
Essential features
- Soft tissue tumor of intermediate malignancy (locally aggressive), with no metastatic potential
- Characterized by the presence of pleomorphic cells, low mitotic activity, ectatic blood vessels with damaged walls and no necrosis
- Most cases are positive for CD34 and lack expression of S100, desmin, pankeratin and STAT6
- Recommended treatment is complete surgical excision with negative margins
Terminology
- Initially characterized by Smith et al. as pleomorphic hyalinizing angiectatic tumor of soft parts (Am J Surg Pathol 1996;20:21)
- Controversial terminology: early pleomorphic hyalinizing angiectatic tumor (also known as hemosiderotic fibrolipomatous tumor) is considered in the spectrum of pleomorphic hyalinizing angiectatic tumor (PHAT) by some experts (Am J Surg Pathol 2004;28:1417)
ICD coding
- ICD-O: 8802/1 - pleomorphic hyalinizing angiectatic tumor
- ICD-11: 2F7C & XH2193 - neoplasms of uncertain behavior of connective or other soft tissue and pleomorphic hyalinizing angiectatic tumor
Epidemiology
- Exact epidemiology is uncertain due to the controversial diagnostic criteria and the lack of contemporary series
- Most cases seem to affect adults (median 51 years, range 10 - 79 years), with a slight female predominance (Am J Surg Pathol 2004;28:1417)
Sites
- Most arise in the superficial soft tissues of the distal lower extremities, particularly the leg, ankle and foot (Am J Surg Pathol 2004;28:1417)
- Other areas of the body rarely affected include upper extremities, trunk and head and neck
- Visceral or intracavitary locations have not been thoroughly documented
Pathophysiology
- Currently unknown
Etiology
- Currently unknown
Clinical features
- Patients frequently report lesions evolving for variable amounts of time (months to years) before consultation (Am J Surg Pathol 1996;20:21, Am J Surg Pathol 2004;28:1417)
- Tumors may appear clinically as hematomas due to vessel wall damage and chronic erythrocyte extravasation
Diagnosis
- Imaging features are poorly characterized, diagnosis depends on histologic findings and molecular features (selected cases)
Radiology description
- Imaging findings are poorly characterized and nonspecific (Oncol Lett 2018;15:4720)
- MRI:
- Well circumscribed to infiltrative lesions with heterogeneous T1 and T2 signal intensity
- Heterogeneous contrast enhancement
- Ultrasound:
- Hypoechoic lesions with internal punctate hyperechogenic areas
Prognostic factors
- Soft tissue tumor of intermediate malignancy (locally aggressive) with no metastatic potential
- Reported local recurrence rate varies from 25 - 50% of cases (Ann Diagn Pathol 2016;20:40, Chin Med J (Engl) 2007;120:876, Am J Surg Pathol 2004;28:1417)
- Sporadic cases have shown transformation to myxoid sarcoma and SMARCA4 deficient undifferentiated sarcoma (Am J Surg Pathol 2004;28:1417, Pathol Int 2007;57:281, Appl Immunohistochem Mol Morphol 2012;20:96, Virchows Arch 2021 Aug 14 [Epub ahead of print])
Case reports
- 35 year old man with a dorsal hand mass (Hand (N Y) 2016;11:NP20)
Treatment
- Complete surgical excision with negative margins
- Cases with sarcomatous transformation may need adjuvant therapy (Virchows Arch 2021 Aug 14 [Epub ahead of print])
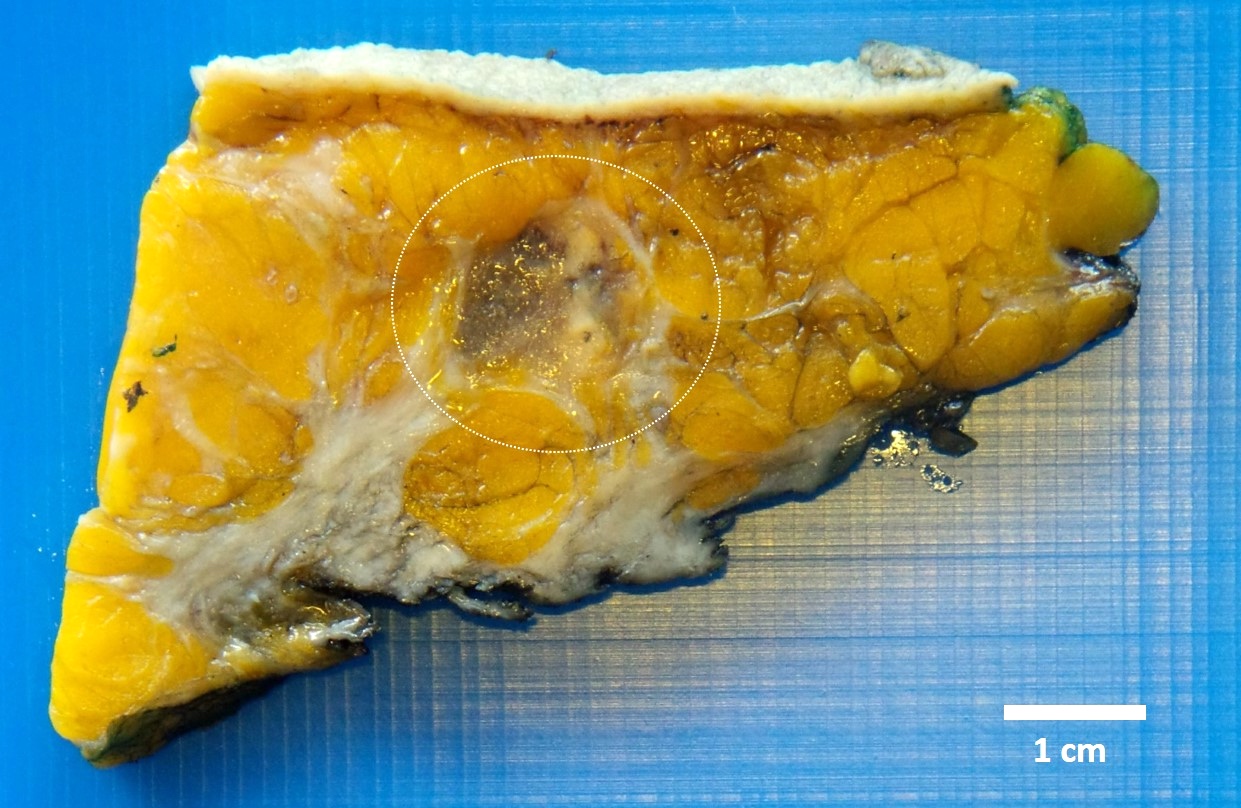
Gross description
- Well circumscribed to infiltrative masses with tan to maroon cut surfaces (Am J Surg Pathol 1996;20:21)
- Cystic, gelatinous or hemorrhagic areas can be present
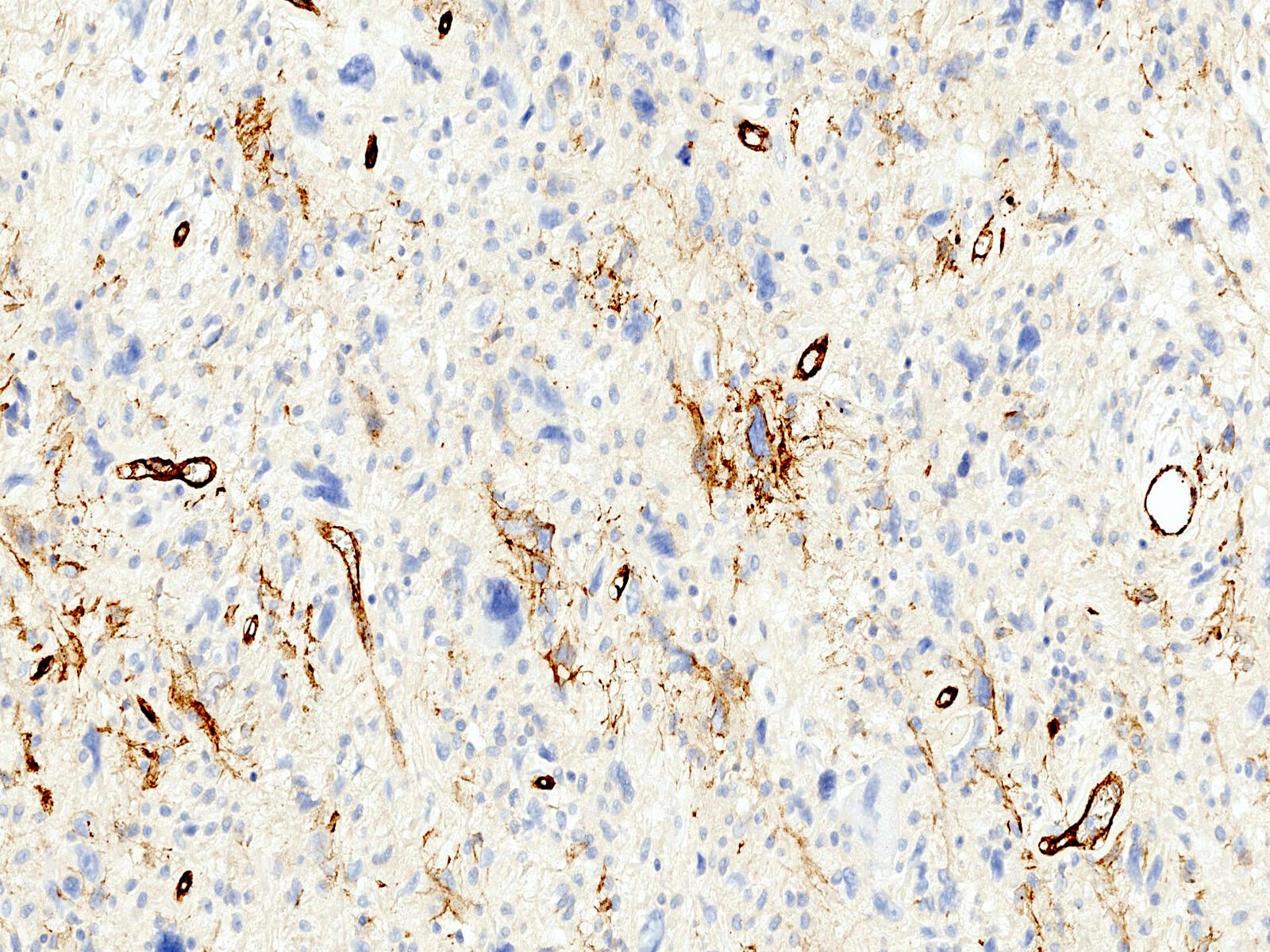
Microscopic (histologic) description
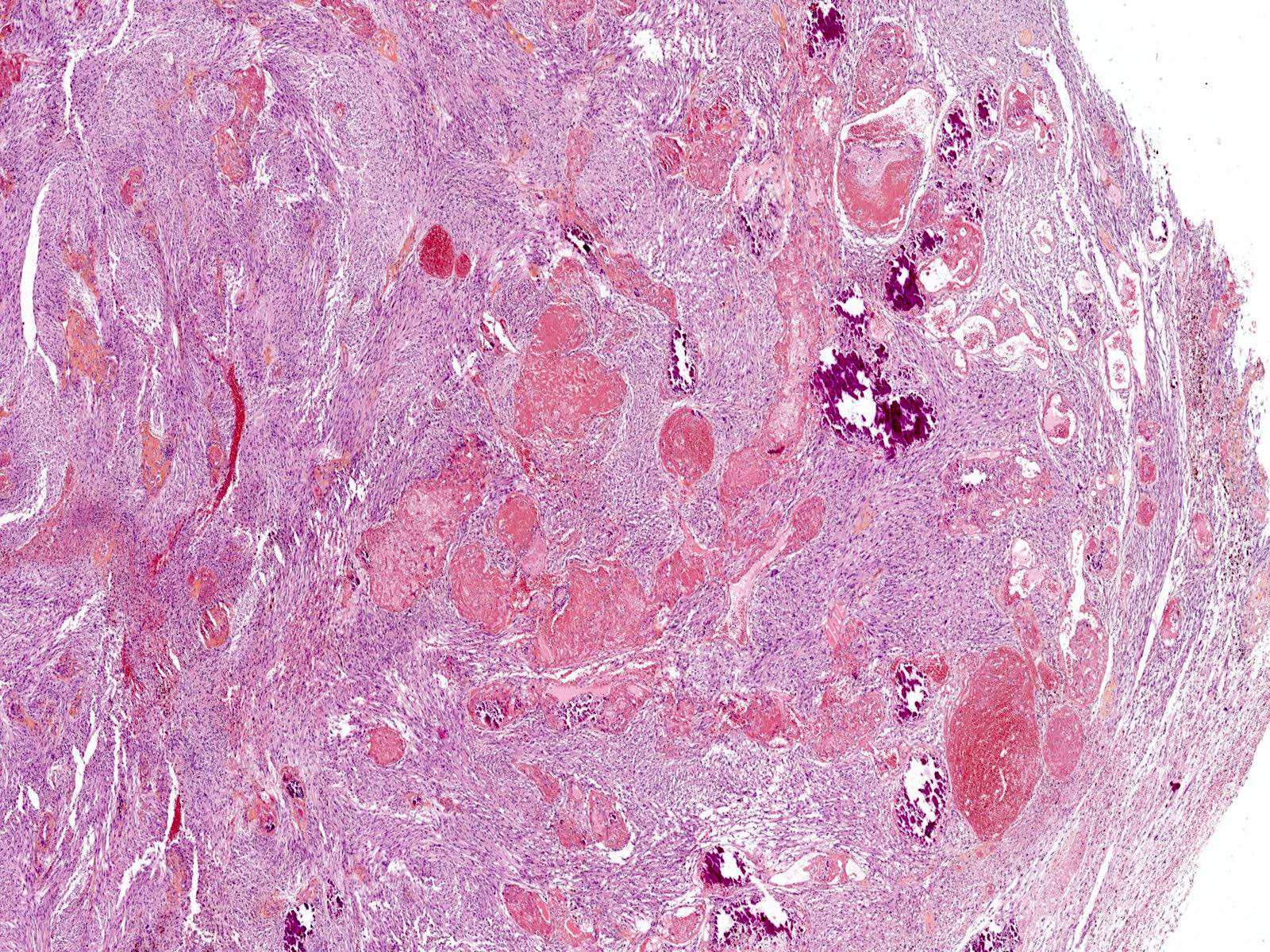
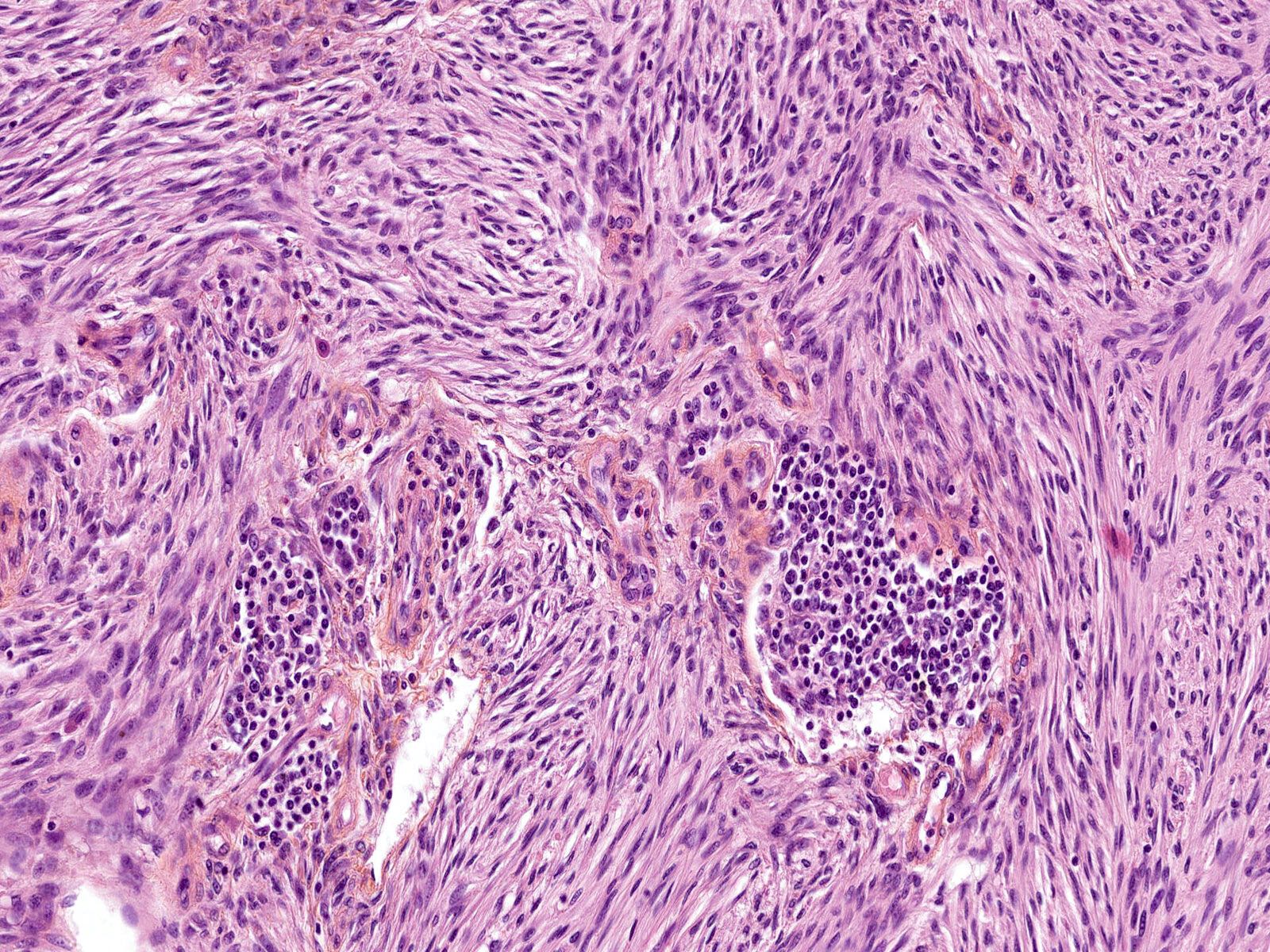
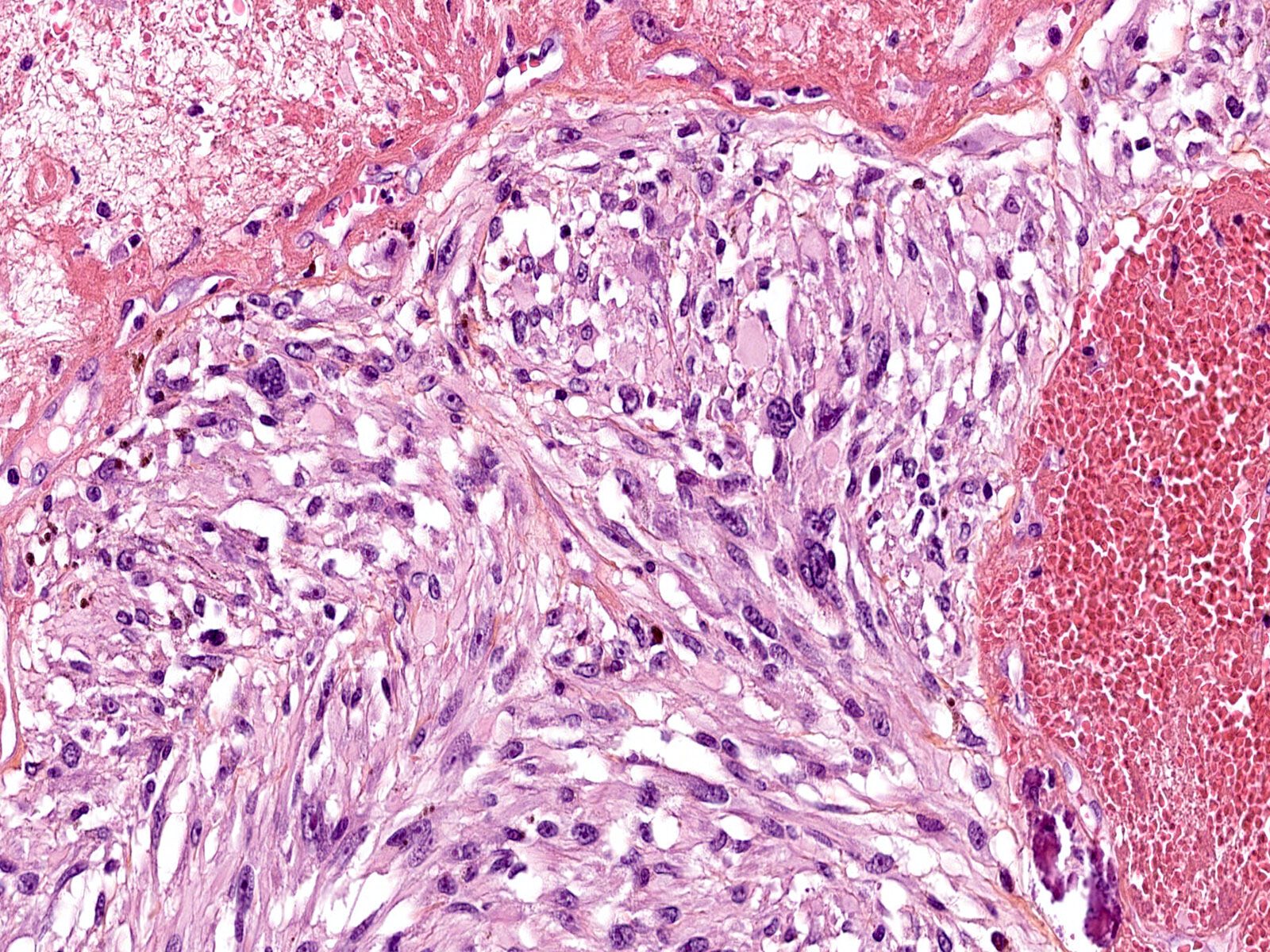
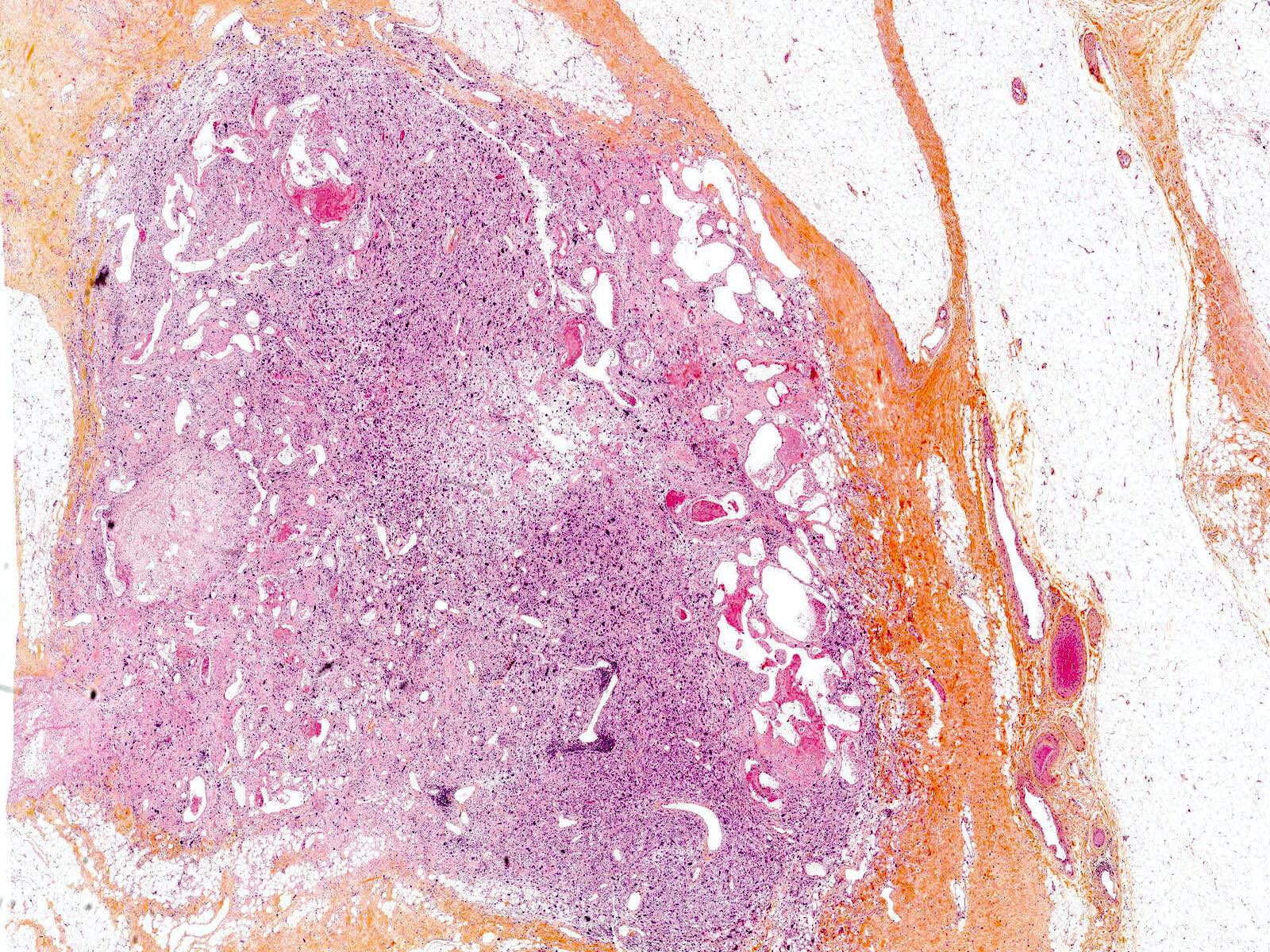
- Relatively well circumscribed silhouette with jagged borders to infiltrative (Am J Surg Pathol 1996;20:21)
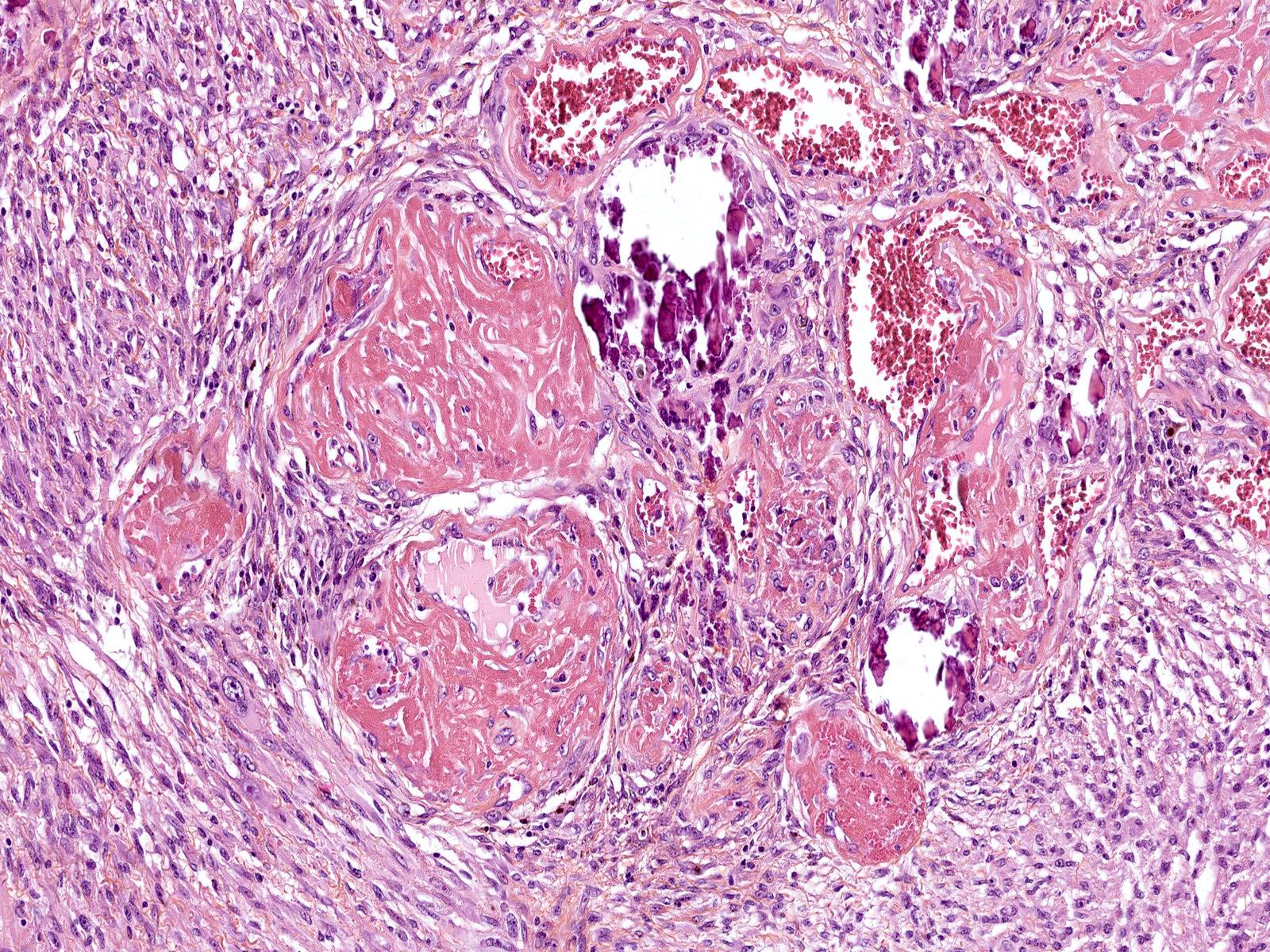
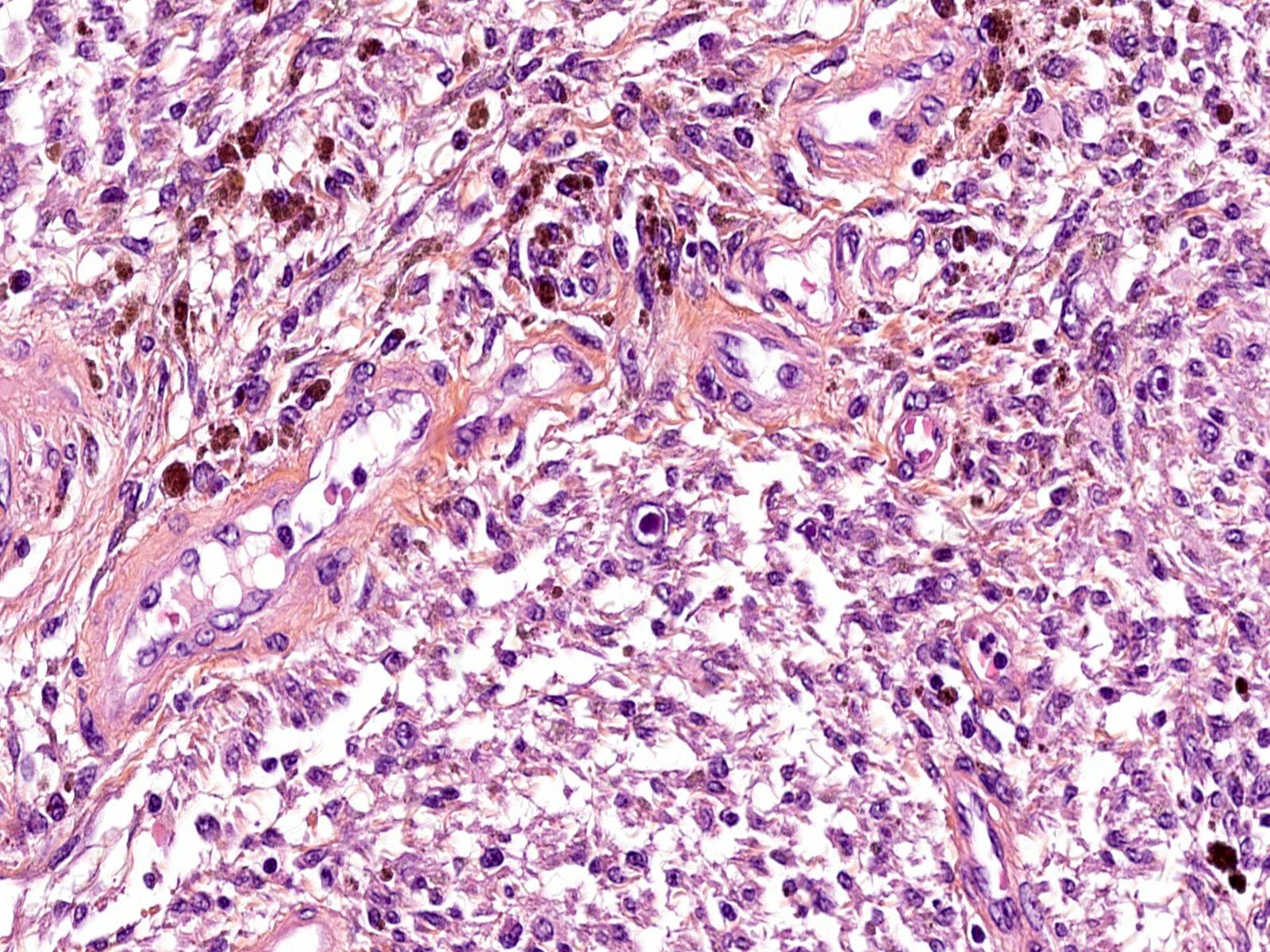
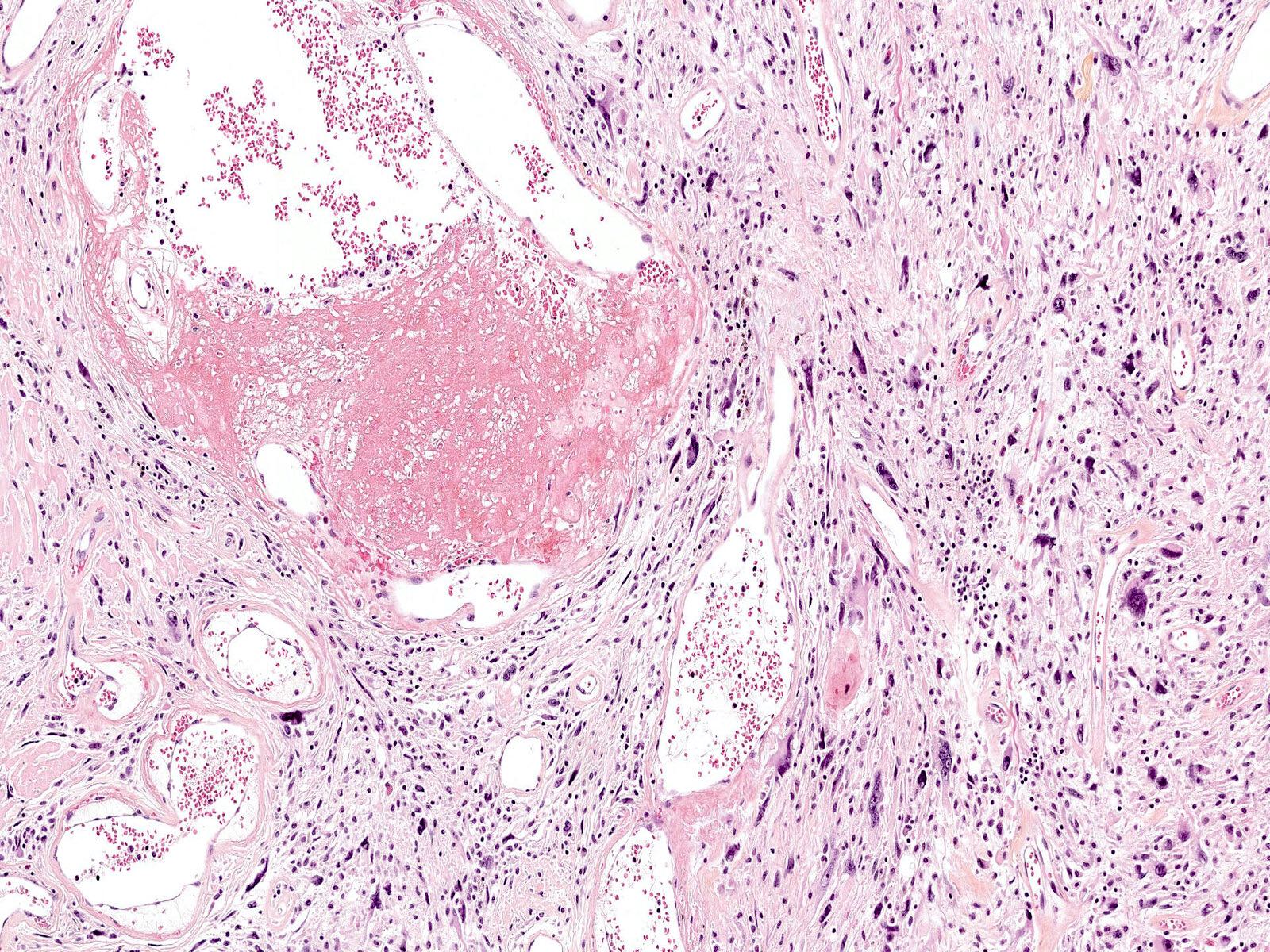
- Abundant clusters of ectatic and variably thrombotic blood vessels with damaged walls (hyalinization or fibrinous deposits) (Am J Surg Pathol 1996;20:21)
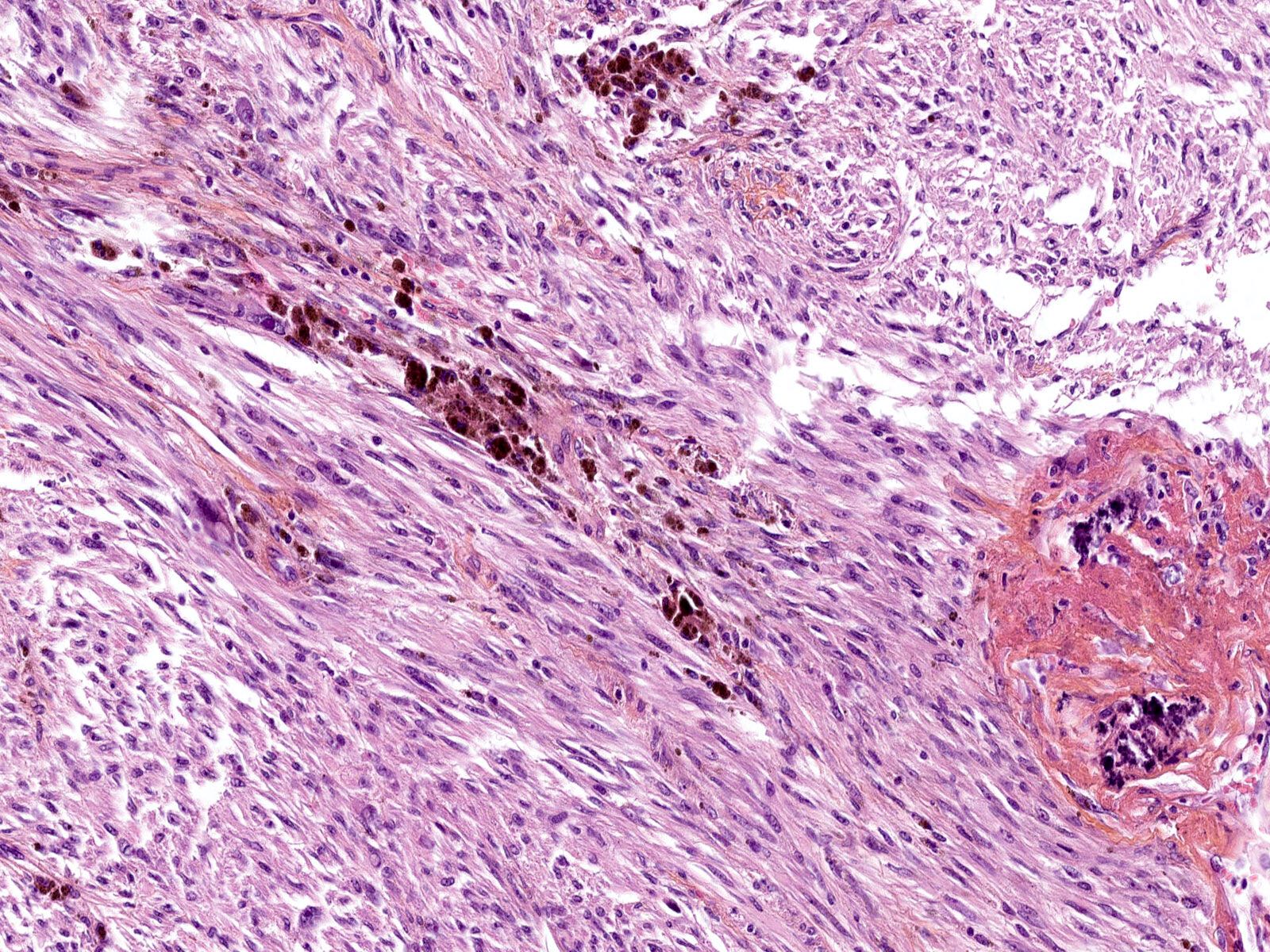
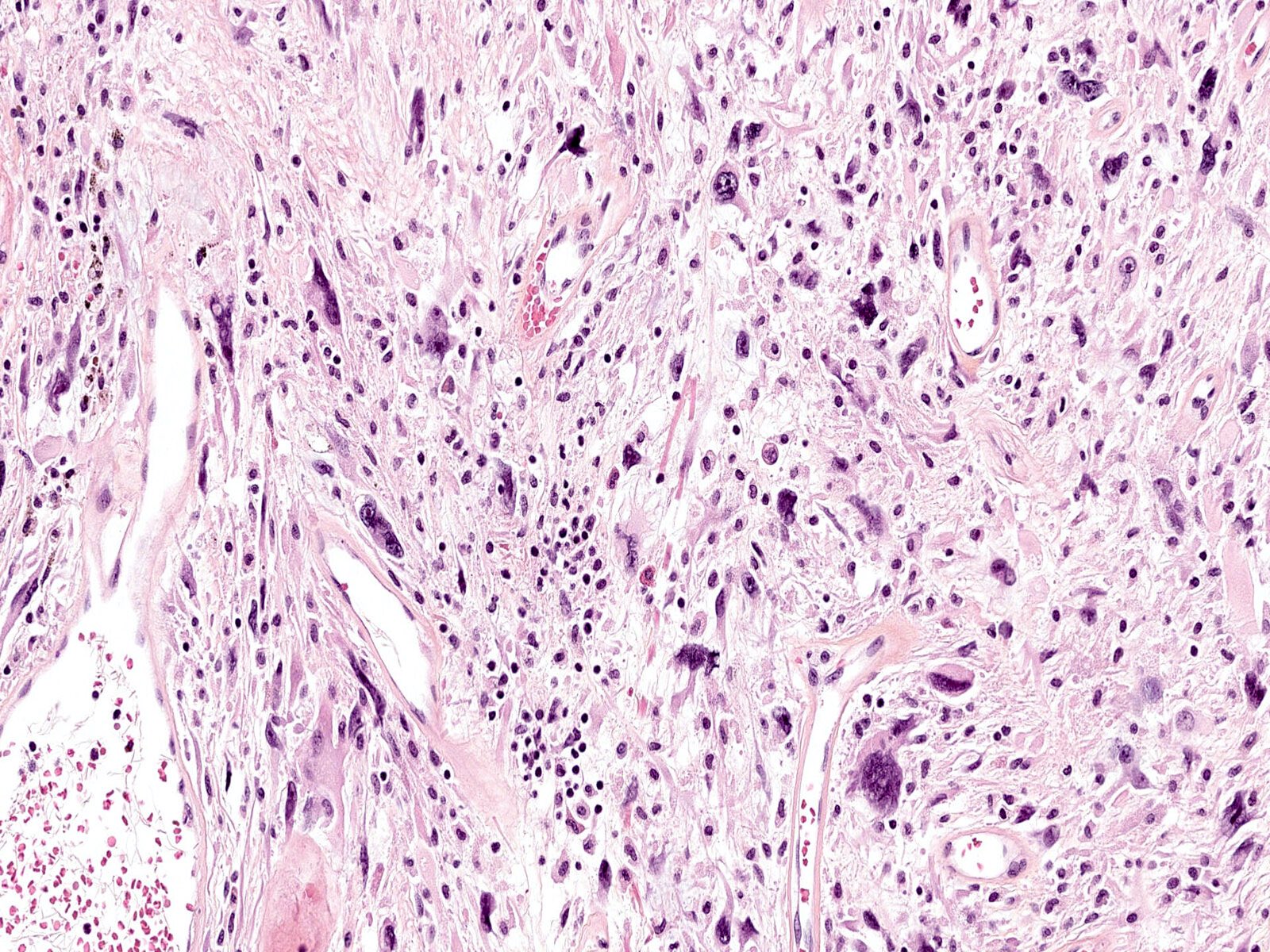
- Sheets and fascicles of a varying proportion of spindle and pleomorphic cells (Am J Surg Pathol 1996;20:21, Am J Surg Pathol 2004;28:1417)
- Spindle cells show slender to plump cytoplasm and ovoid to wavy nuclei with low pleomorphism (Am J Surg Pathol 2004;28:1417)
- Pleomorphic cells show abundant cytoplasm and large, irregular, vesicular nuclei with prominent eosinophilic nucleoli (resembling virocyte-like cells) (Am J Surg Pathol 2004;28:1417, Ann Diagn Pathol 2016;20:40)
- Intranuclear pseudoinclusions and hyperchromasia can be present (Am J Surg Pathol 2004;28:1417, Cancer Genet 2012;205:673)
- Mitotic activity is very low (< 1/mm²) and necrosis is rare (Am J Surg Pathol 2004;28:1417)
- Some cases have a component of hemosiderotic fibrolipomatous tumor (usually in the periphery) (Am J Surg Pathol 2004;28:1417)
- Other findings: hemosiderin deposits, hemorrhagic areas, mixed inflammatory infiltrates and calcifications (Am J Surg Pathol 2004;28:1417)
- Sarcomatous transformation (very rare): transition to myxofibrosarcoma-like areas (high mitotic activity, arciform vessels and myxoid stroma) or epithelioid sarcoma, proximal type-like areas (high mitotic activity, sheets of rhabdoid cells and necrosis) (Pathol Int 2007;57:281, Virchows Arch 2021 Aug 14 [Epub ahead of print])
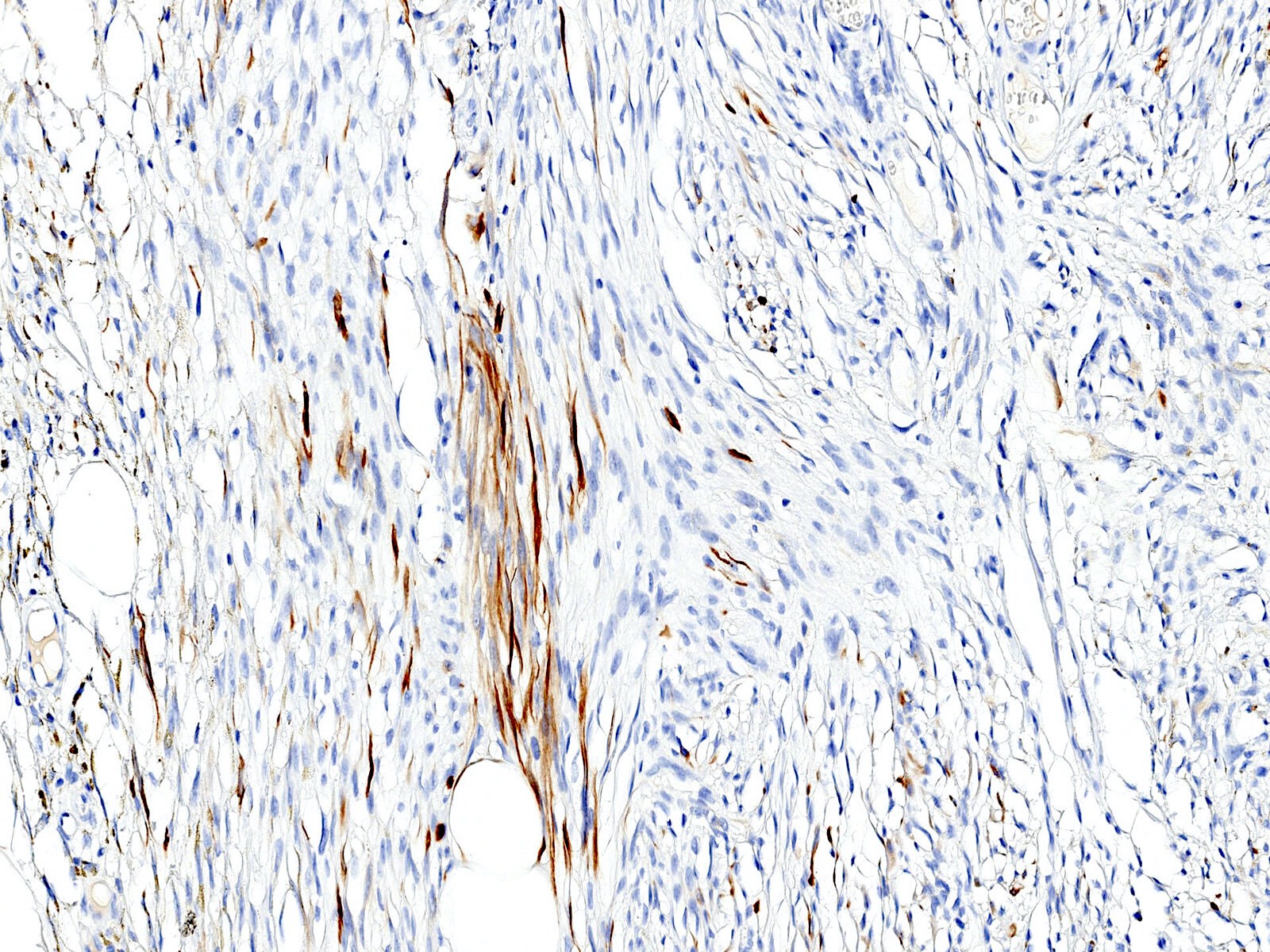
Microscopic (histologic) images
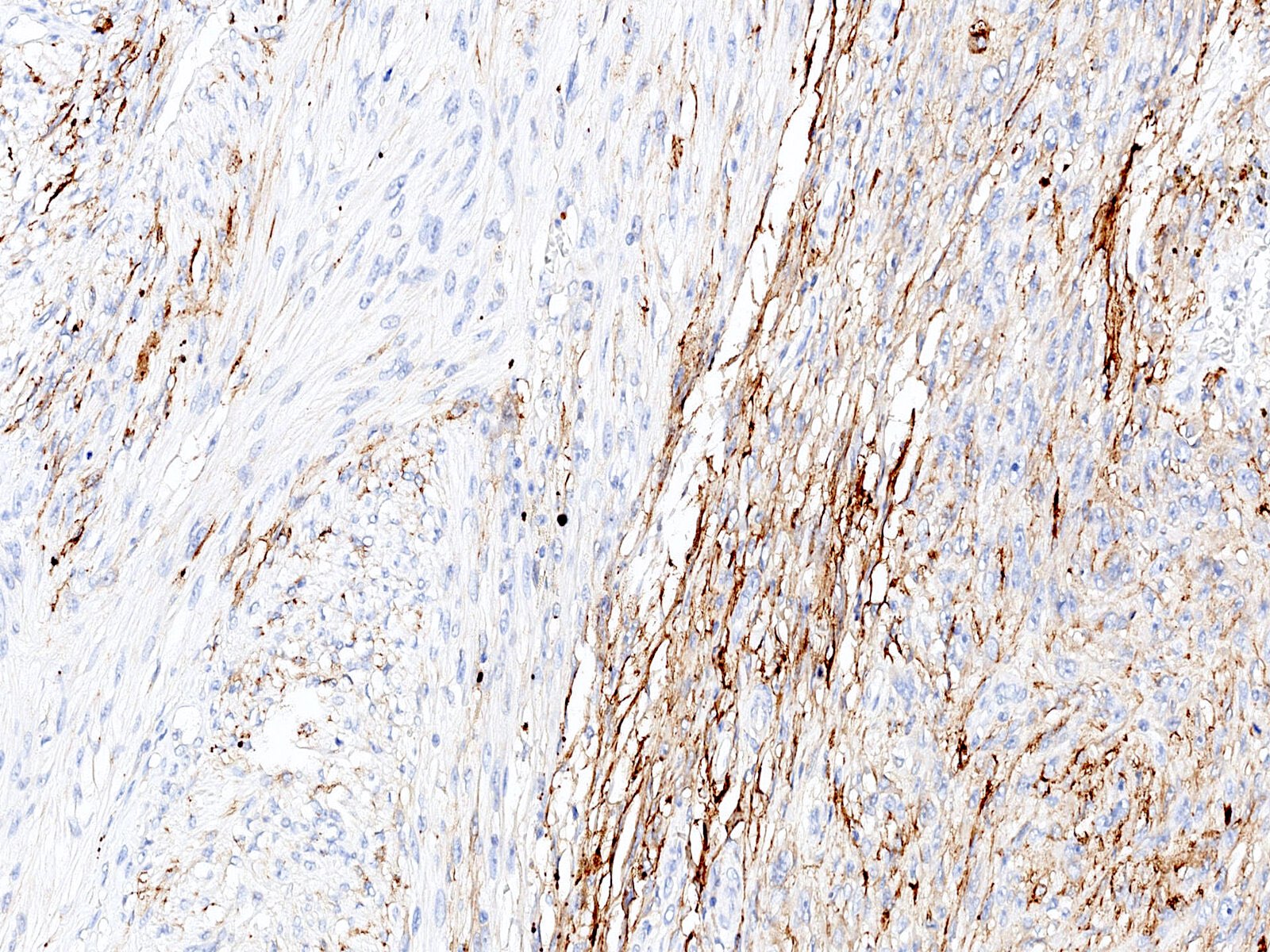
Contributed by Raul Perret, M.D., M.Sc.
Cytology description
- Tumor cells of varying size and shape with pleomorphic nuclei, pseudoinclusions and intracytoplasmic hemosiderin pigment (Diagn Cytopathol 2015;43:407)
- Cytological findings alone are nonspecific and should not be used for diagnostic confirmation
Positive stains
- Most cases show CD34 expression ranging from focal to diffuse (Am J Surg Pathol 2004;28:1417)
- Other IHC is often obtained but is not actually useful for this diagnosis because they are so nonspecific; this includes VEGF, vimentin (consistently positive but extremely nonspecific), CD99 (useful for round cell tumors but nonspecific) and Factor XIII (also very nonspecific with limited utility) (Arch Pathol Lab Med 2000;124:423, Arch Pathol Lab Med 2019;143:212, Am J Surg Pathol 2004;28:1417, Appl Immunohistochem Mol Morphol 2012;20:96)
Negative stains
- Pancytokeratin (AE1 / AE3)
- S100 (Am J Surg Pathol 2004;28:1417)
- Desmin: rare cases may show focal expression
- MDM2
- STAT6
Electron microscopy description
- Bizarre nuclei, nuclear cytoplasmic inclusions and no intercellular junctions
- Abundant cytoplasmic intermediate filaments and granular endoplasmic reticulum network (Ultrastruct Pathol 2006;30:59)
Molecular / cytogenetics description
- Variably complex karyotypes with OGA (MGEA5) or TGFBR3 rearrangements in some cases (Cancer Genet 2012;205:673, Genes Chromosomes Cancer 2011;50:757, Am J Surg Pathol 2014;38:1182)
- OGA and TGFBR3 rearrangements are complex and do not generally derive in a functional transcript detectable by conventional RNA sequencing techniques
- Single case with a TGFBR3-FBXW4 fusion has been reported (Virchows Arch 2019;475:251)
Videos
PHAT: pleomorphic hyalinizing angiectatic tumor
Sample pathology report
- Knee mass, excision:
- Pleomorphic hyalinizing angiectatic tumor (see comment)
- Comment: Microscopic examination reveals a relatively well circumscribed lesion with jagged borders centered in the hypodermis. The lesion comprises sheets and fascicles of spindle and pleomorphic cells associated with hemosiderin deposits and clusters of variably thrombotic and ectatic blood vessels. The tumor cells have hyperchromatic nuclei, which are irregular in size and shape. Mitotic activity is low and tumor necrosis is absent. Immunohistochemically, the tumor cells are positive with CD34 and negative with S100, pancytokeratin, MDM2 and STAT6.
- These histological and immunohistochemical findings are in keeping with pleomorphic hyalinizing angiectatic tumor. If incompletely excised, these intermediate malignancy mesenchymal tumors tend to recur locally, while distant spread is not typically seen.
Differential diagnosis
- Undifferentiated pleomorphic sarcoma:
- Predominantly affects adults (> 50 years old)
- Frequently deep seated (subfascial) and infiltrating
- High mitotic rate (including abnormal mitotic figures)
- Tumor necrosis
- CD34 generally not expressed
- Lacks OGA or TGFBR3 rearrangements
- Solitary fibrous tumor:
- Variation in cellular density
- Bland spindle cells with ovoid nuclei and abundant ramified capillaries (staghorn shaped)
- Nuclear pleomorphism is very rare
- Diffuse expression of STAT6 (Mod Pathol 2014;27:390)
- Schwannoma:
- Encapsulated nodule
- Variation in cellular density (Antoni A and Antoni B) and nuclear palisading
- Diffuse and strong expression of S100
- Cellular angiofibroma:
- Mainly affects the genital region of adults (Am J Surg Pathol 2004;28:1426)
- Bland spindle cells and abundant small to medium sized blood vessels with hyalinized walls
- Rare cases with nuclear atypia (sarcomatous transformation)
- Loss of RB1 expression and frequent expression of ER and PR
- Superficial CD34 positive fibroblastic tumor:
- Can show significant morphological overlap with PHAT (Histopathology 2021;79:810)
- Focal pancytokeratin (AE1 / AE3) expression in ~75% of cases
- Diffuse and strong (en bloc) CD34 expression
- Presence of PRDM10 fusions in a subset of cases
- Lacks OGA or TGFBR3 rearrangements (Mod Pathol 2014;27:294)
- Myxoinflammatory fibroblastic sarcoma:
- Multinodular architecture, frequently extending deep into the fascia (Am J Surg Pathol 2014;38:1)
- Alternating myxoid and collagenous areas
- Clusters of ectatic and thrombosed vessels can be seen but are not abundant
- CD34 expression is generally focal and dim (Am J Surg Pathol 2014;38:1)
- VGLL3 amplification (~40%) (Mod Pathol 2020;33:2520)
Board review style question #1
A 53 year old woman presented with a knee mass that had been evolving for 2 years. Histology shows a relatively well circumscribed hypodermal mass composed of bizarre looking pleomorphic cells and abundant clusters of ectatic blood vessels with damaged walls. Mitotic activity is very low (< 1/10 high power fields) and necrosis is absent. On immunohistochemistry, the tumor cells stain for CD34, while S100, pancytokeratin, MDM2 and STAT6 are negative. Which of the following is most likely the correct diagnosis?
- Atypical dermatofibroma
- Dermatofibrosarcoma protuberans
- Pleomorphic hyalinizing angiectatic tumor
- Solitary fibrous tumor
- Undifferentiated pleomorphic sarcoma
Board review style answer #1
C. Pleomorphic hyalinizing angiectatic tumor
Comment Here
Reference: Pleomorphic hyalinizing angiectatic tumor
Comment Here
Reference: Pleomorphic hyalinizing angiectatic tumor
Board review style question #2
Which of the following is true about pleomorphic hyalinizing angiectatic tumor (PHAT)?
- Desmin is usually diffusely and strongly positive
- It is an intermediate malignancy tumor (locally recurring)
- Mitotic rate is generally high
- Most cases show sarcomatous transformation
- OGA (MGEA5) or TGFBR3 rearrangements are present in all cases
Board review style answer #2
B. It is an intermediate malignancy tumor (locally recurring)
Comment Here
Reference: Pleomorphic hyalinizing angiectatic tumor
Comment Here
Reference: Pleomorphic hyalinizing angiectatic tumor