Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Saggini A. Perineurioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueperineurioma.html. Accessed April 2nd, 2025.
Definition / general
- Perineuriomas are soft tissue neoplasms almost exclusively composed of cells resembling normal perineurium
- 2 main types of perineurioma are recognized: intraneural perineuriomas and soft tissue perineuriomas, including cutaneous and sclerosing perineuriomas
Essential features
- Perineurioma are soft tissue neoplasms almost exclusively composed of cells resembling normal perineurium
- 2 main types of perineurioma are recognized: intraneural perineuriomas and soft tissue perineuriomas, including cutaneous and sclerosing perineuriomas
- Perineurial cells have typical slender, fibroblast-like appearance with long, delicate cytoplasmic processes
- Perineuriomas express antigens that are identical to normal perineurium (EMA, GLUT1, claudin1)
Terminology
- Localized hypertrophic neuropathy: old designation of intraneural perineuriomas (not recommended)
- Hybrid benign peripheral nerve sheath tumors: rare tumors consisting of 2 intermingled neoplastic cell populations with neural differentiation, including hybrid perineurioma schwannoma and hybrid perineurioma neurofibroma
Epidemiology
- Intraneural perineurioma
- More frequent: adolescents and young adults
- M = F
- Soft tissue perineurioma
- More frequent: adults
- M = F
- References: Am J Surg Pathol 2005;29:845, Am J Surg Pathol 1997;21:164
Sites
- Intraneural perineurioma
- Predilection for upper limbs (radial, ulnar, median nerves) and lower limbs (sciatic nerve)
- Soft tissue perineurioma
- Predilection for superficial soft tissues of the extremities and trunk
- 30% of cases: deep soft tissues / visceral organs
- Sclerosing perineurioma: predilection for hands (fingers, palms) (Am J Surg Pathol 1997;21:1433)
Pathophysiology
- Intraneural perineurioma
- Intraneural clonal (neoplastic) proliferation of perineurial cells
- TRAF7 mutations (60% of cases) (Ann Neurol 2017;81:316)
- Soft tissue perineurioma
- No evidence of association with neurofibromatosis syndromes (-1 or -2)
- Association with mutually exclusive deletions involving NF1 or NF2 (Am J Surg Pathol 2018;42:1708)
- No evidence of TRAF7 mutations (Am J Surg Pathol 2018;42:1708)
Clinical features
- Intraneural perineurioma
- Muscle weakness, progressive loss of sensory function, muscle atrophy if untreated
- Soft tissue perineurioma
- Solitary, slowly growing nodule / tumor
- Painful in a minority of cases
- Reference: Arch Pathol Lab Med 2007;131:625
Diagnosis
- Intraneural perineurioma
- Electromyography: denervation changes
- MRI: determination of extent of nerve involvement (Skeletal Radiol 2014;43:375)
- Soft tissue perineurioma
- MRI: determination of localization if involvement of deep soft tissues / visceral organs (Skeletal Radiol 2020;49:109)
Radiology images
Images hosted on other servers:
Prognostic factors
- Intraneural perineurioma
- Typically benign behavior
- Only 1 reported case of malignant intraneural perineurioma (Int J Clin Exp Pathol 2014;7:4503)
- Soft tissue perineurioma
- Typically benign behavior
- Atypical perineuriomas: overall benign behavior
- Malignant perineurioma: exceptionally rare, regarded as variant of malignant peripheral nerve sheath tumor
Case reports
- Intraneural perineurioma
- 21 year old man with chronic weakness and atrophy in the left leg (Clin Case Rep 2016;4:777)
- 42 year old man with an asymptomatic nodule on the second finger of the right hand (Am J Dermatopathol 2013;35:e45)
- Soft tissue perineurioma
- 3 month old girl with well circumscribed, nontender mass over the scalp (Asian J Neurosurg 2016;11:70)
- 20 year old man with a painless left dorsal tongue mass (J Oral Maxillofac Surg 2019;77:329.e1)
- 42 year old woman with a firm, painful nodule on the dorsum of the right wrist (Dermatol Online J 2014;20:13030)
Treatment
- Intraneural perineurioma
- No standard treatment guidelines
- Complete resection with nerve grafting (but variable loss of neural function may be inevitable)
- Soft tissue perineurioma
- Complete excision (recurrences are uncommon)
Clinical images
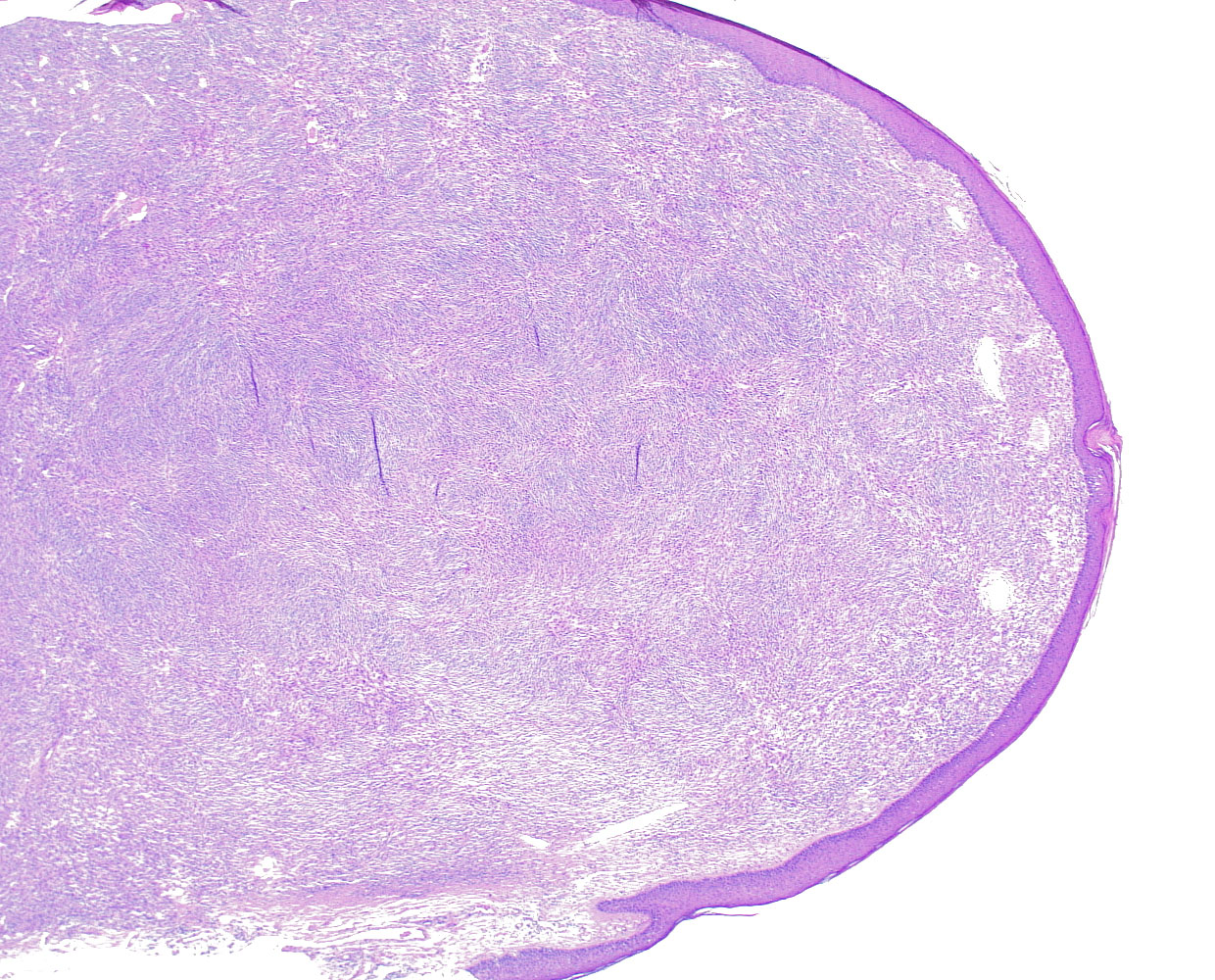
Gross description
- Intraneural perineurioma
- Fusiform expansion of affected nerve, extending several centimeters in length
- Soft tissue perineurioma
- Circumscribed white masses (1 - 20 cm in diameter)
- Reference: Am J Surg Pathol 2005;29:845
Gross images
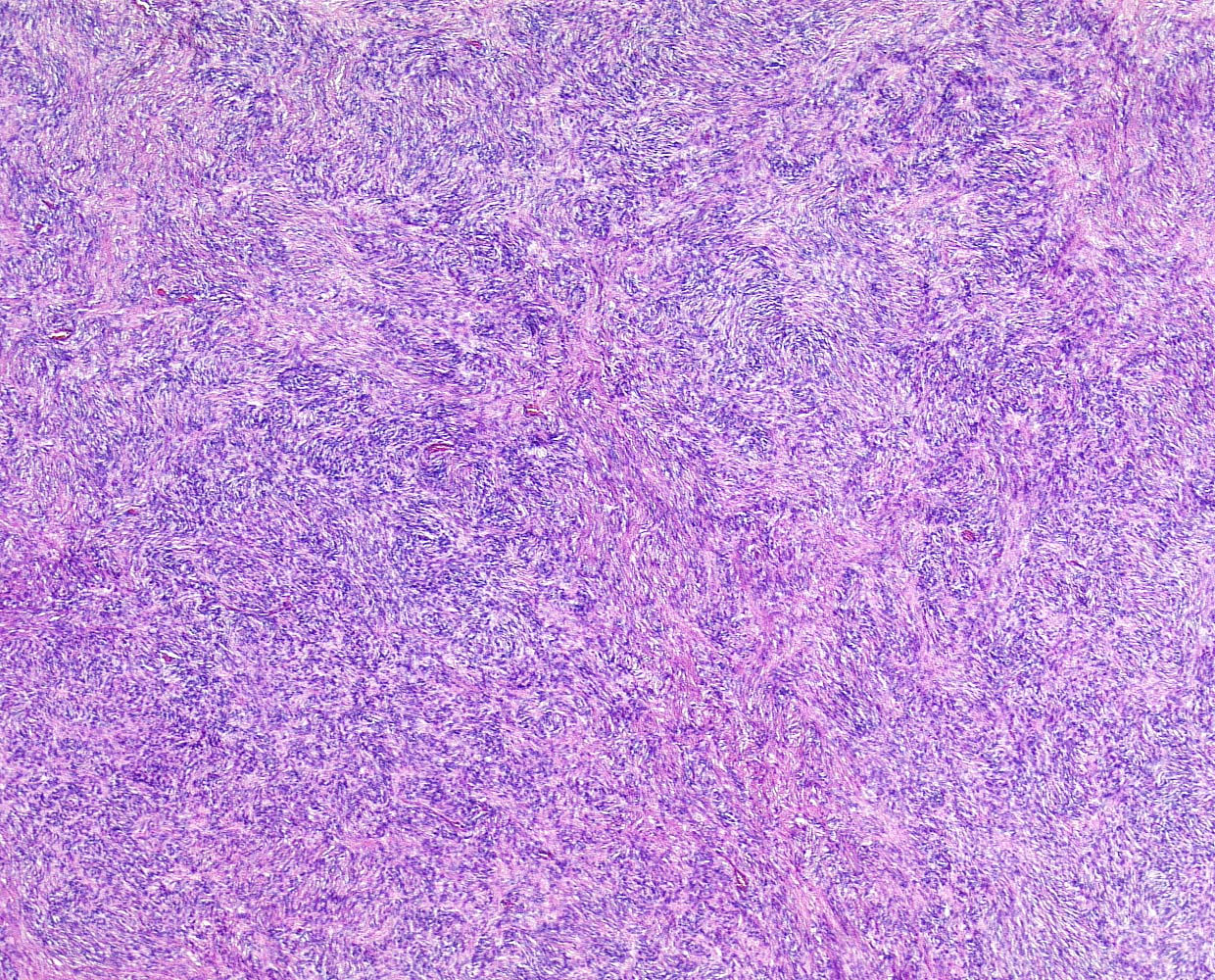
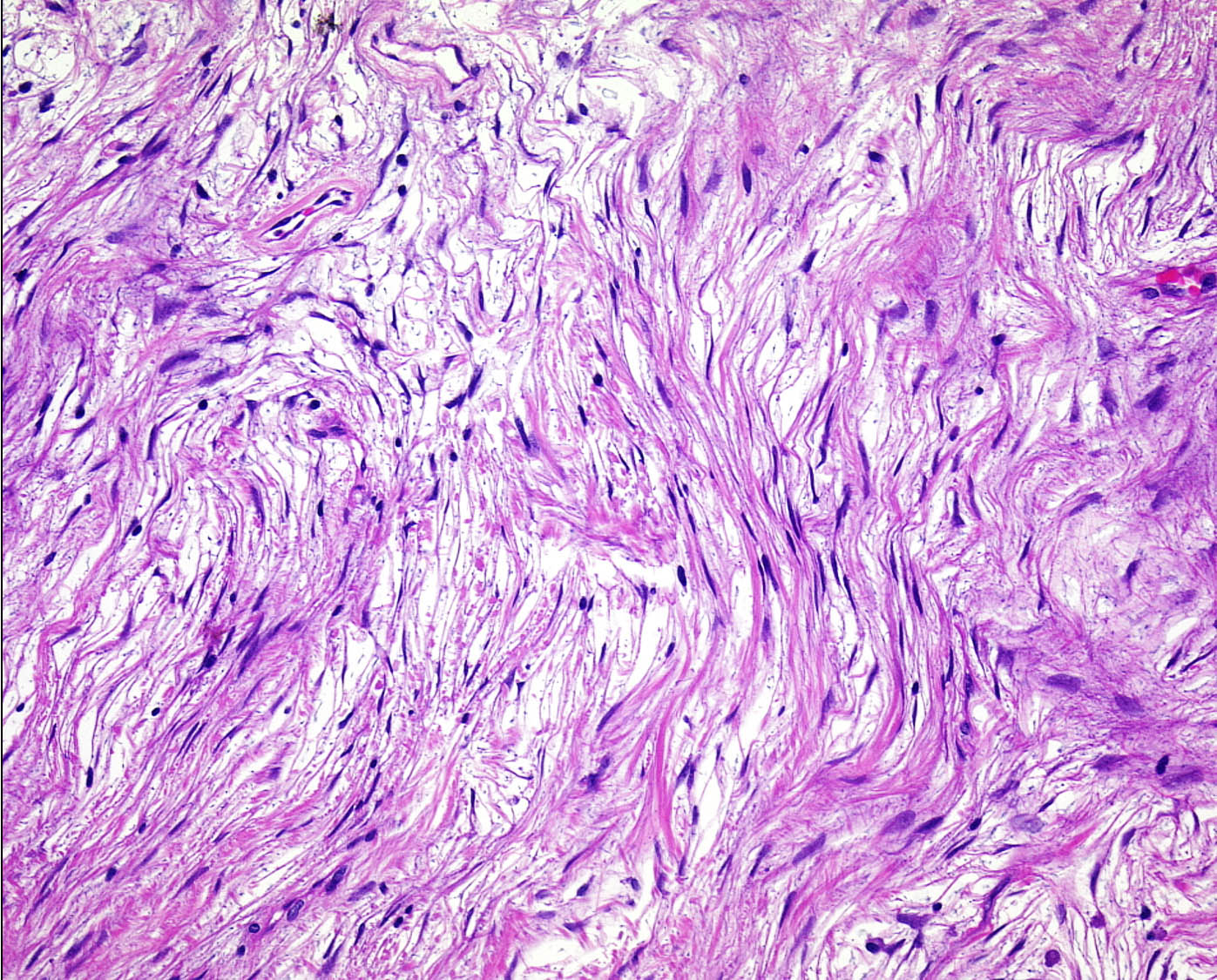
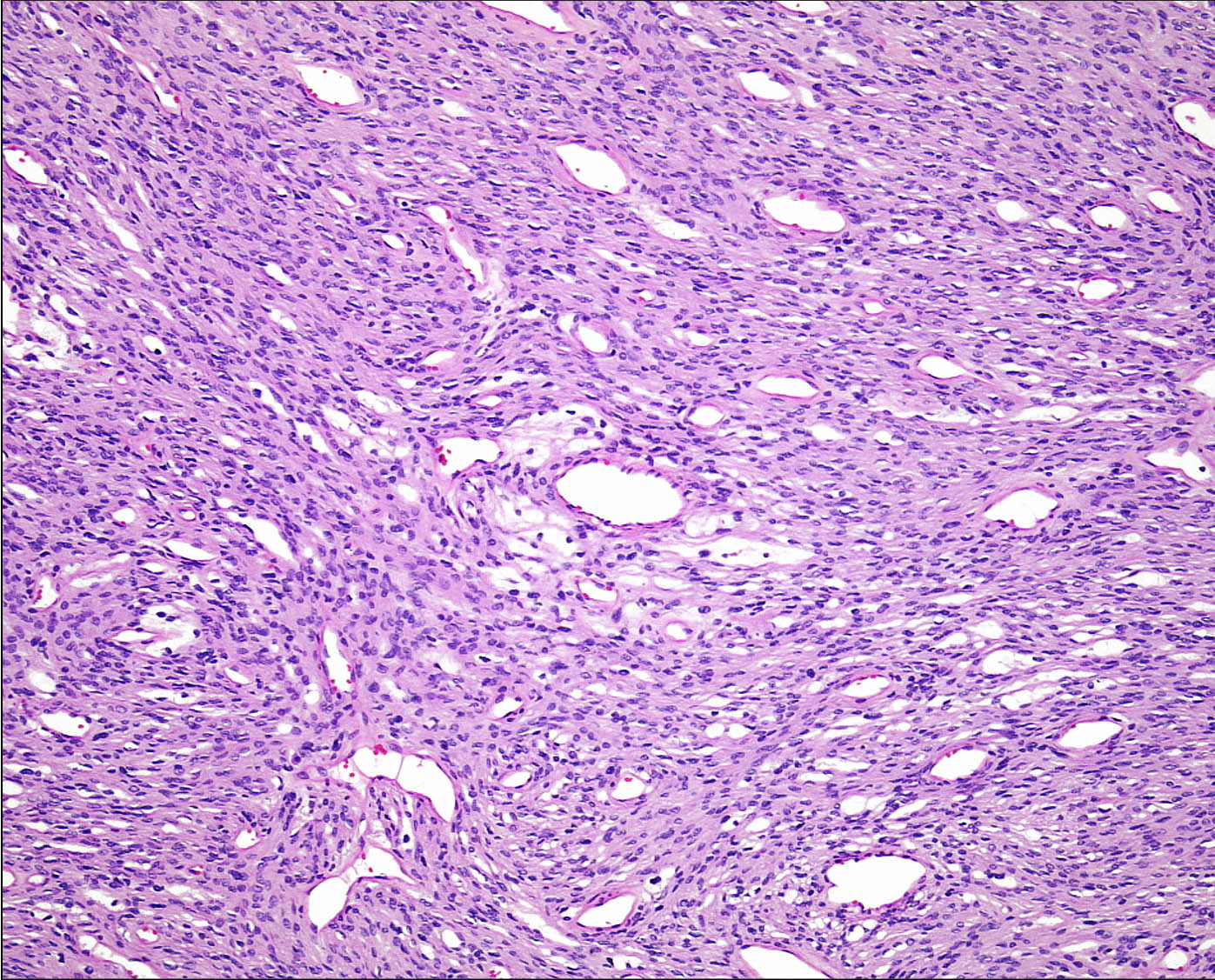
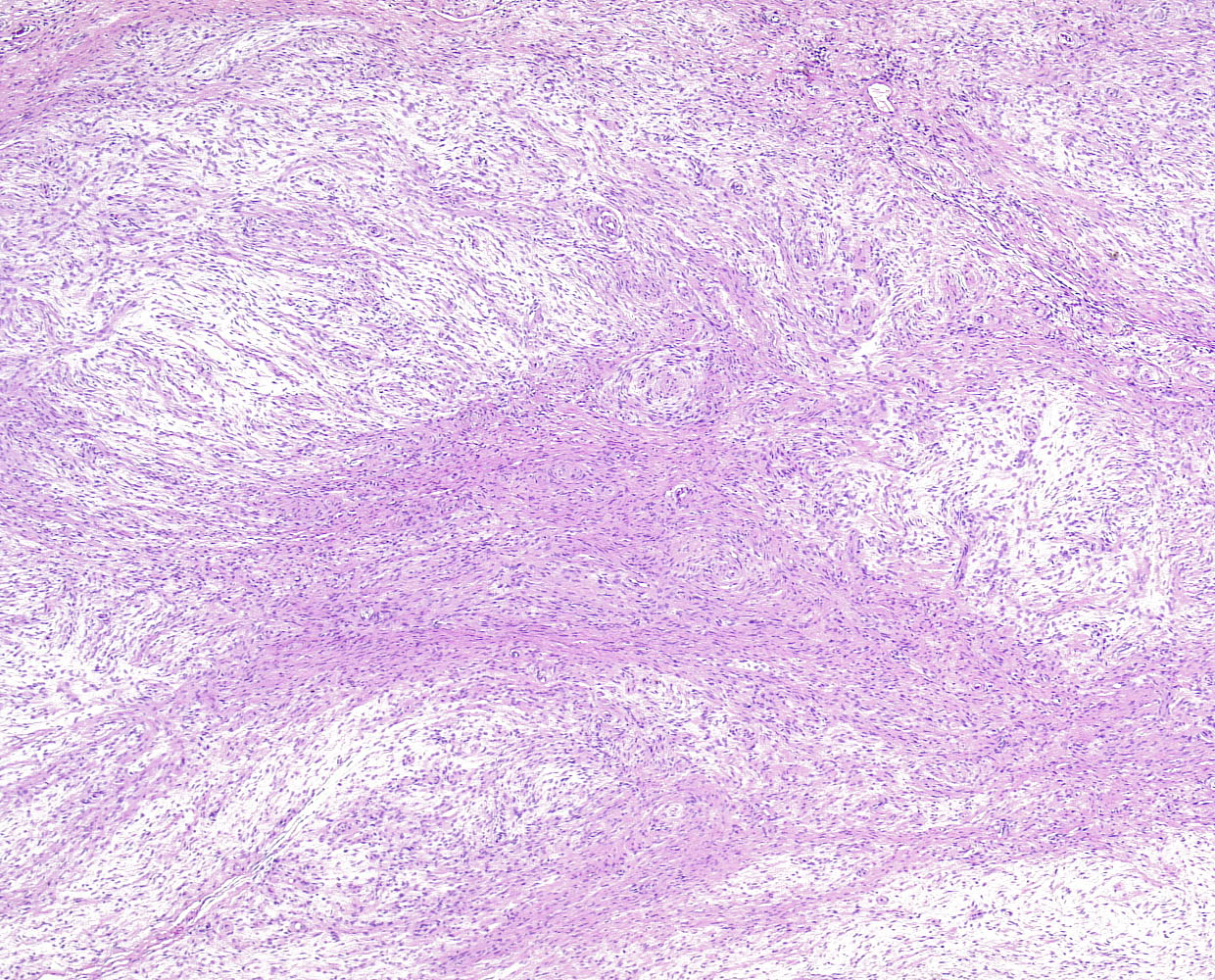
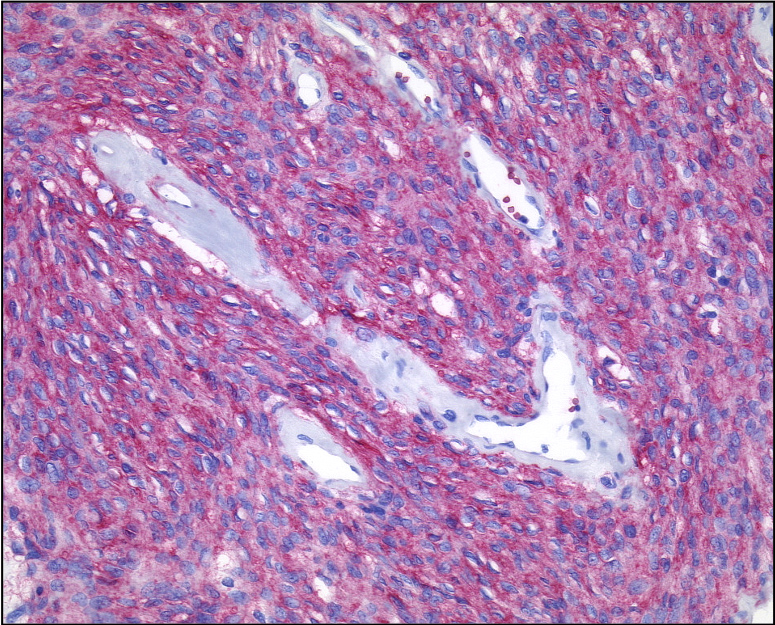
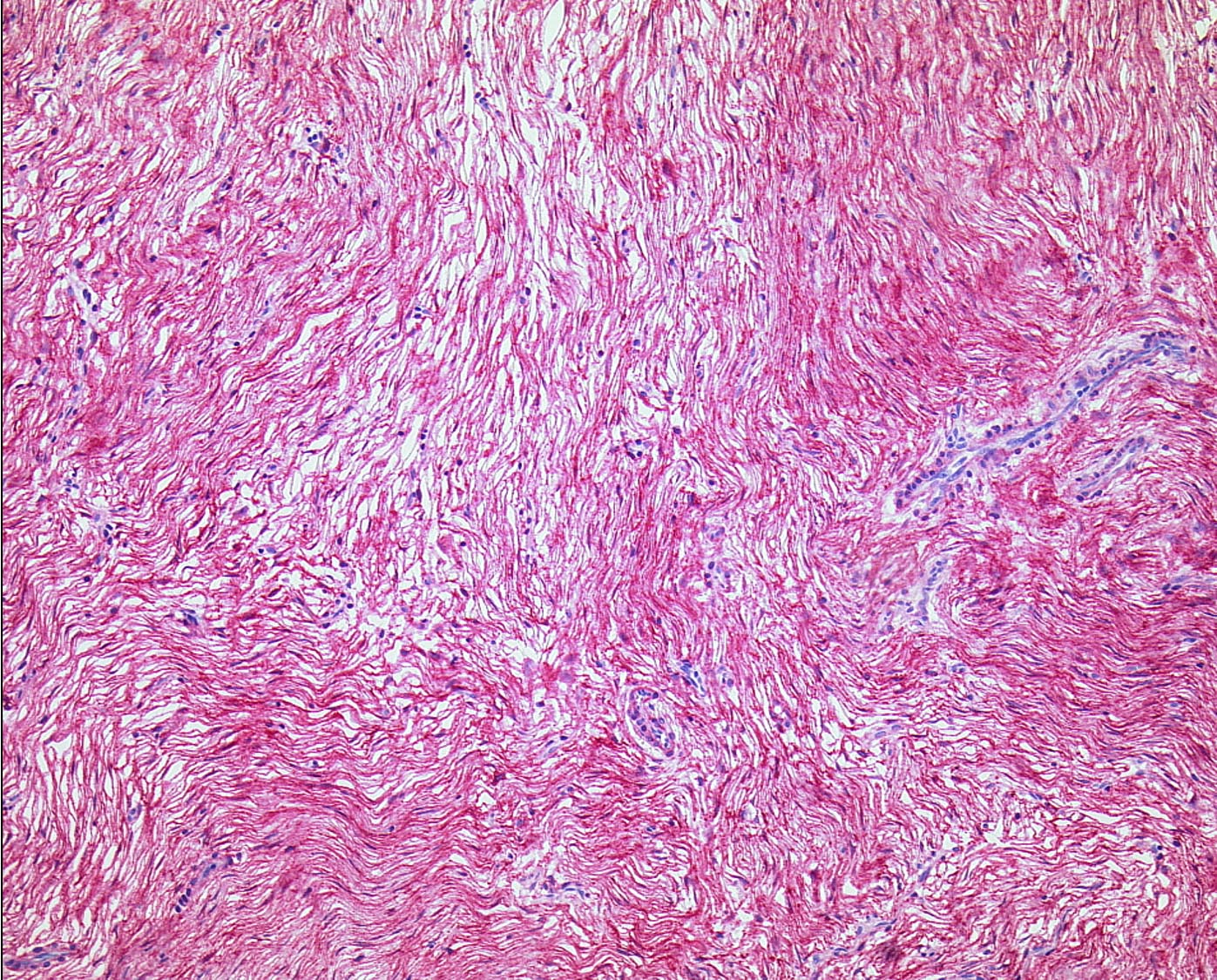
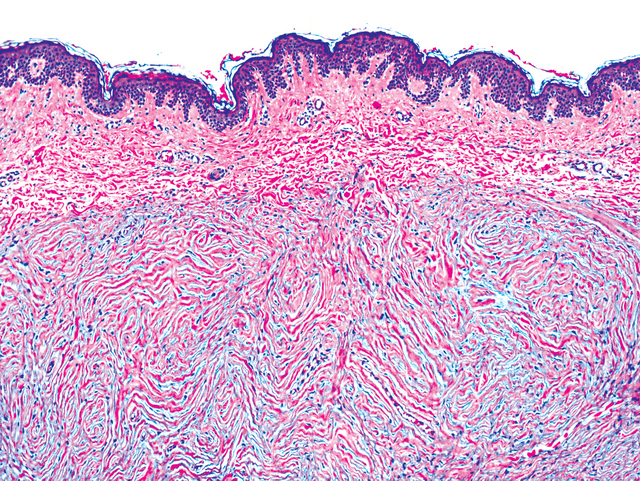
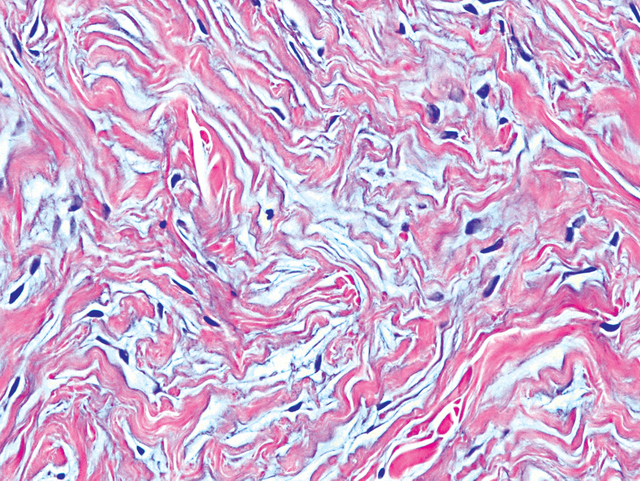
Microscopic (histologic) description
- Intraneural perineurioma
- Multiple small "onion bulbs" expanding the affected nerve, consisting of concentric layers of perineurial cells ensheathing a central axon and Schwann cell
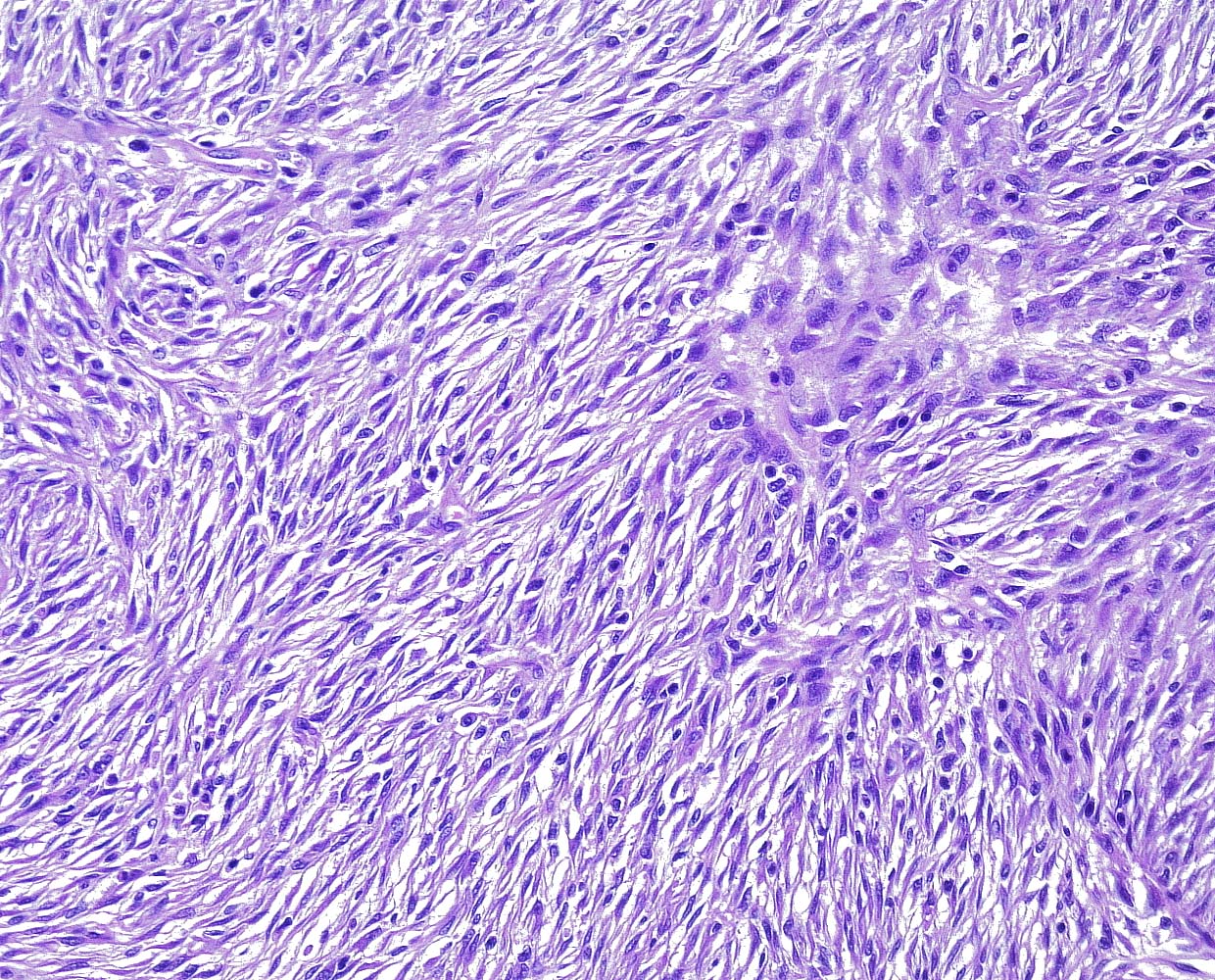
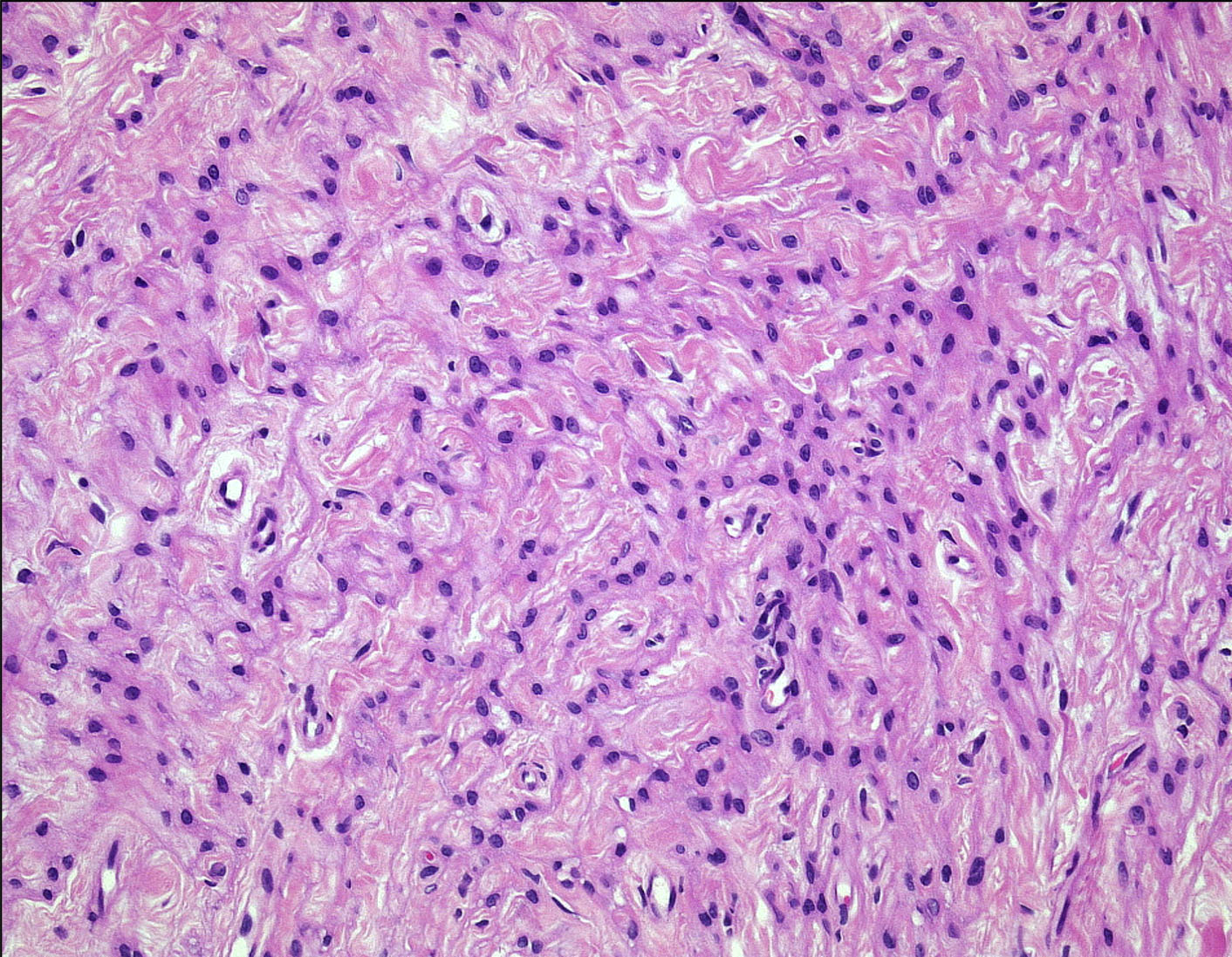
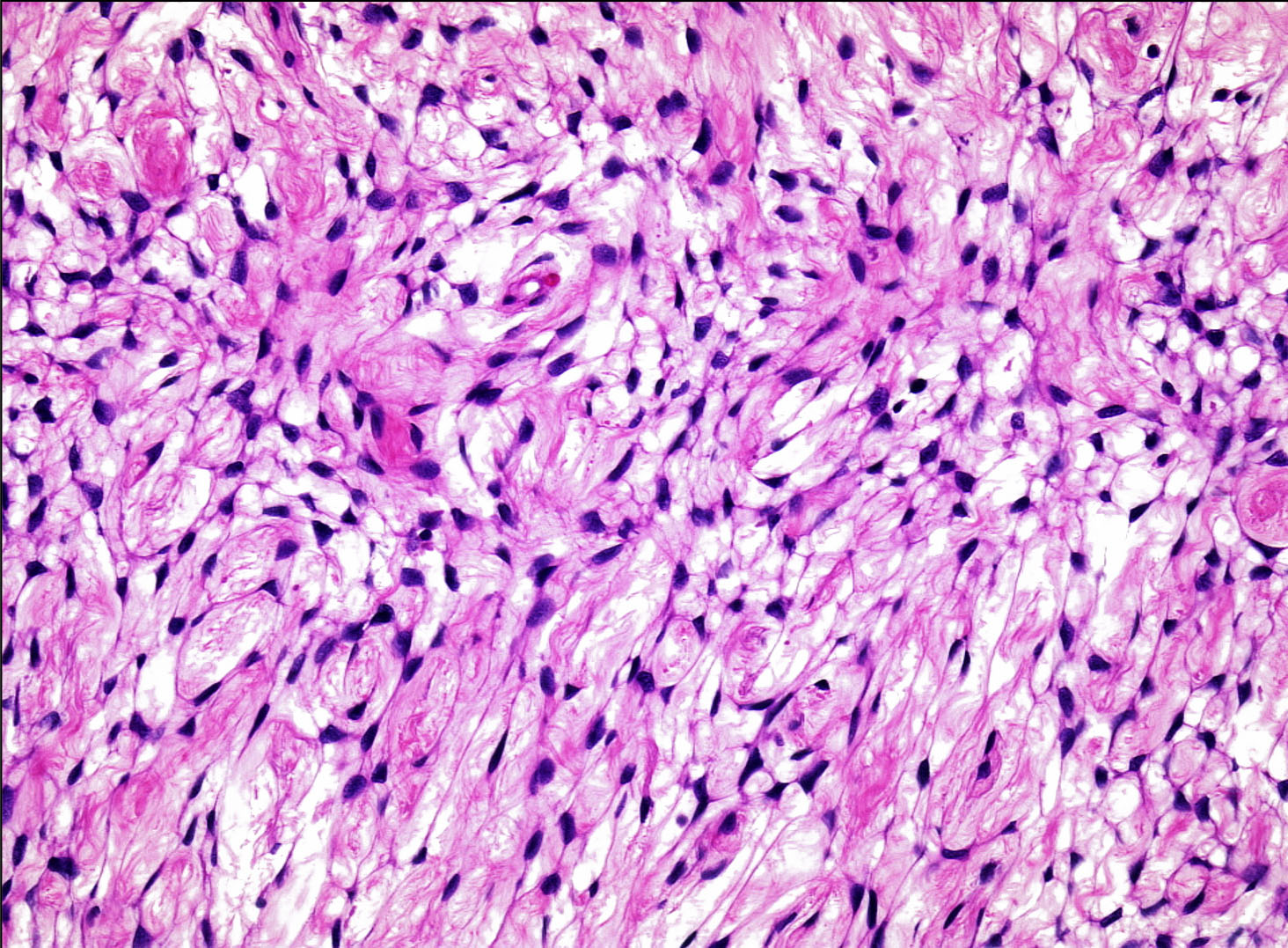
- Soft tissue perineurioma
- Nonencapsulated, well demarcated spindle cell tumor (Am J Surg Pathol 2005;29:845)
- Perineurial cells have typical slender, fibroblast-like appearance with long, delicate cytoplasmic processes
- Variable degree of cellularity, from paucicellular to densely cellular
- Fibrotic / sclerotic stroma but frequent foci of myxoid degeneration
- Metaplastic ossification (rare)
- Storiform, whorled, lamellar or short fascicular patterns may be observed
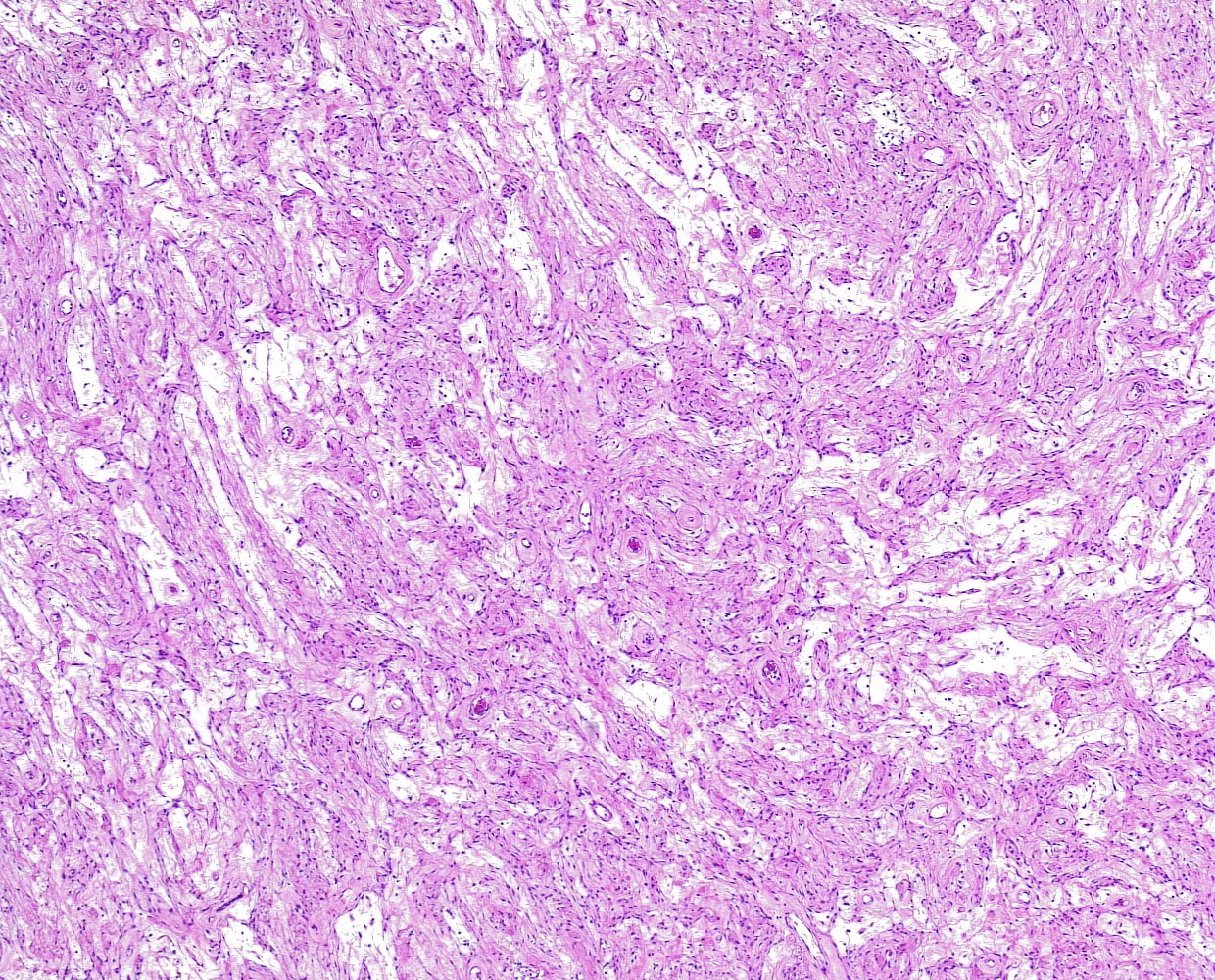
- Sclerosing perineurioma: spindled to rounded cells with pale cytoplasm with indistinct cell borders, arranged in cords / trabeculae / chains within a densely sclerotic stroma (Am J Surg Pathol 1997;21:1433)
- Reticular perineurioma: lace-like arrangement of cells, resulting in formation of microscopic cysts (Virchows Arch 2005;447:677)
- Rare histologic variants:
- Plexiform perineurioma (Virchows Arch 2005;447:677)
- Pacinian-like perineurioma (Histopathology 2001;39:498)
- Pseudolipoblastic perineurioma (Hum Pathol 2016;57:22)
- Granular perineurioma (Am J Dermatopathol 2008;30:163)
- Atypical perineurioma: variable combination of scattered cytological atypia, mildly increased mitotic activity, increased cellularity or infiltration of muscle (Am J Surg Pathol 2005;29:845)
- Malignant perineurioma (malignant peripheral nerve sheath tumor variant): diffuse cytological atypia, increased mitotic activity (> 13 figures/30 high power fields), necrotic foci (Clin Neuropathol 2012;31:424)
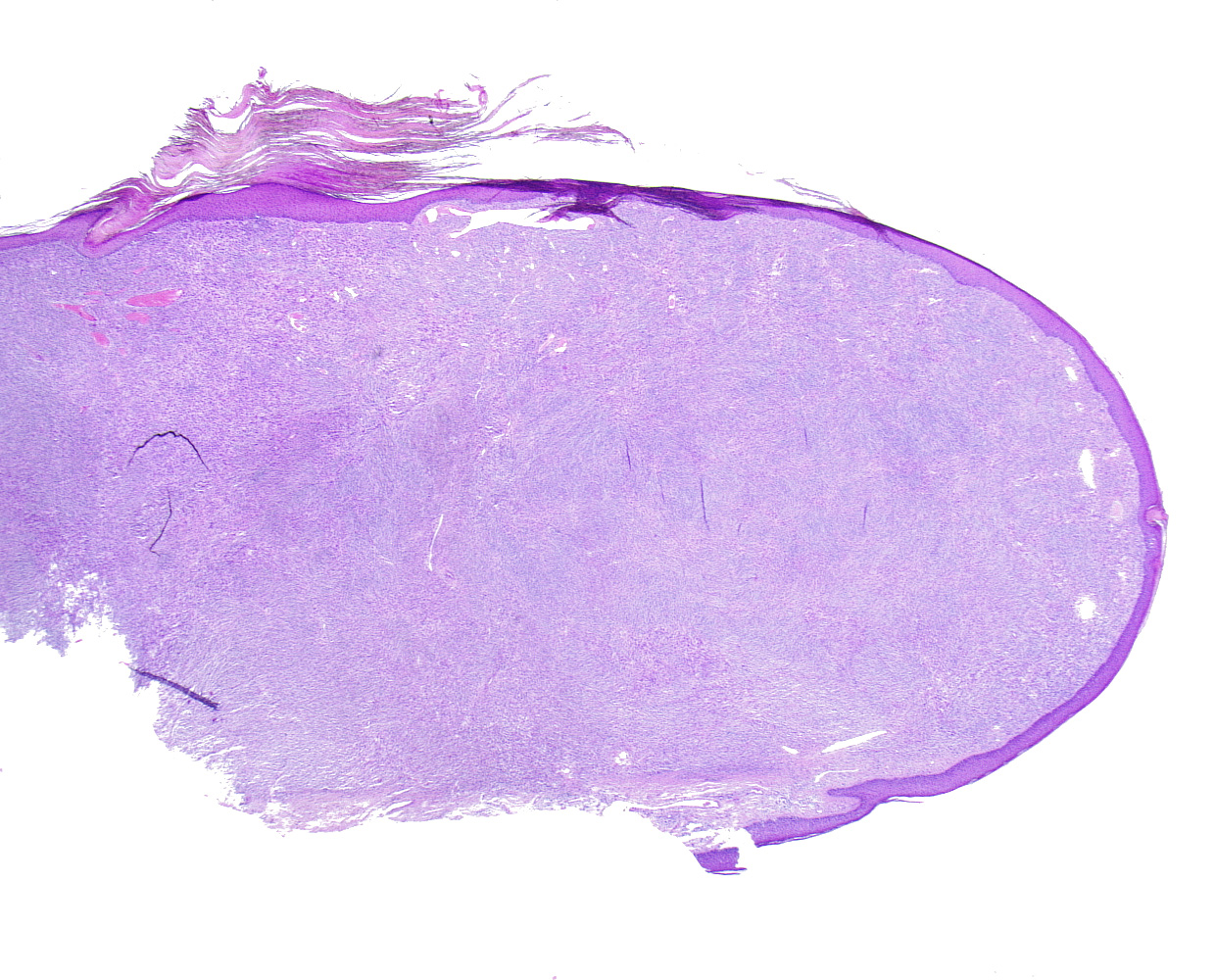
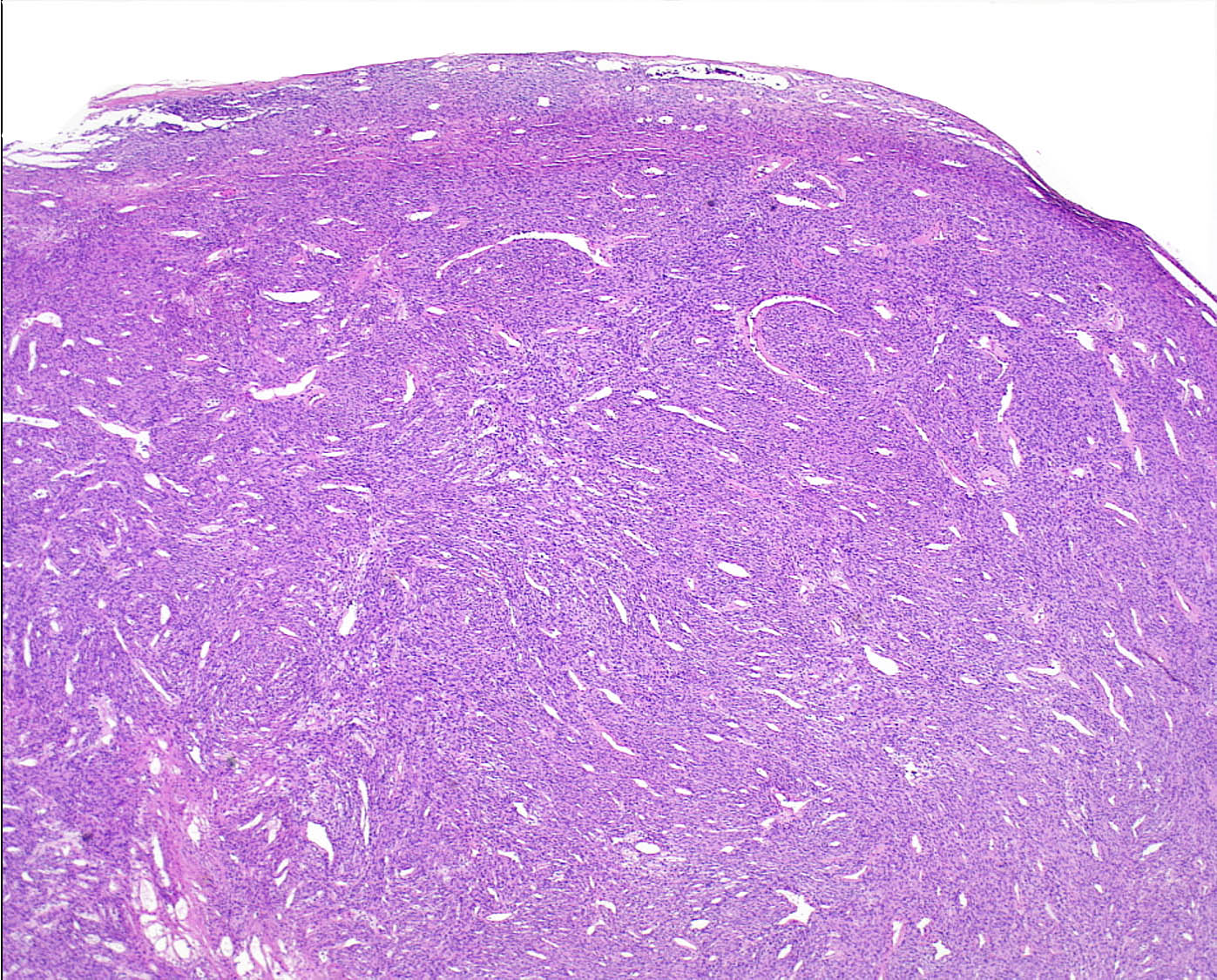
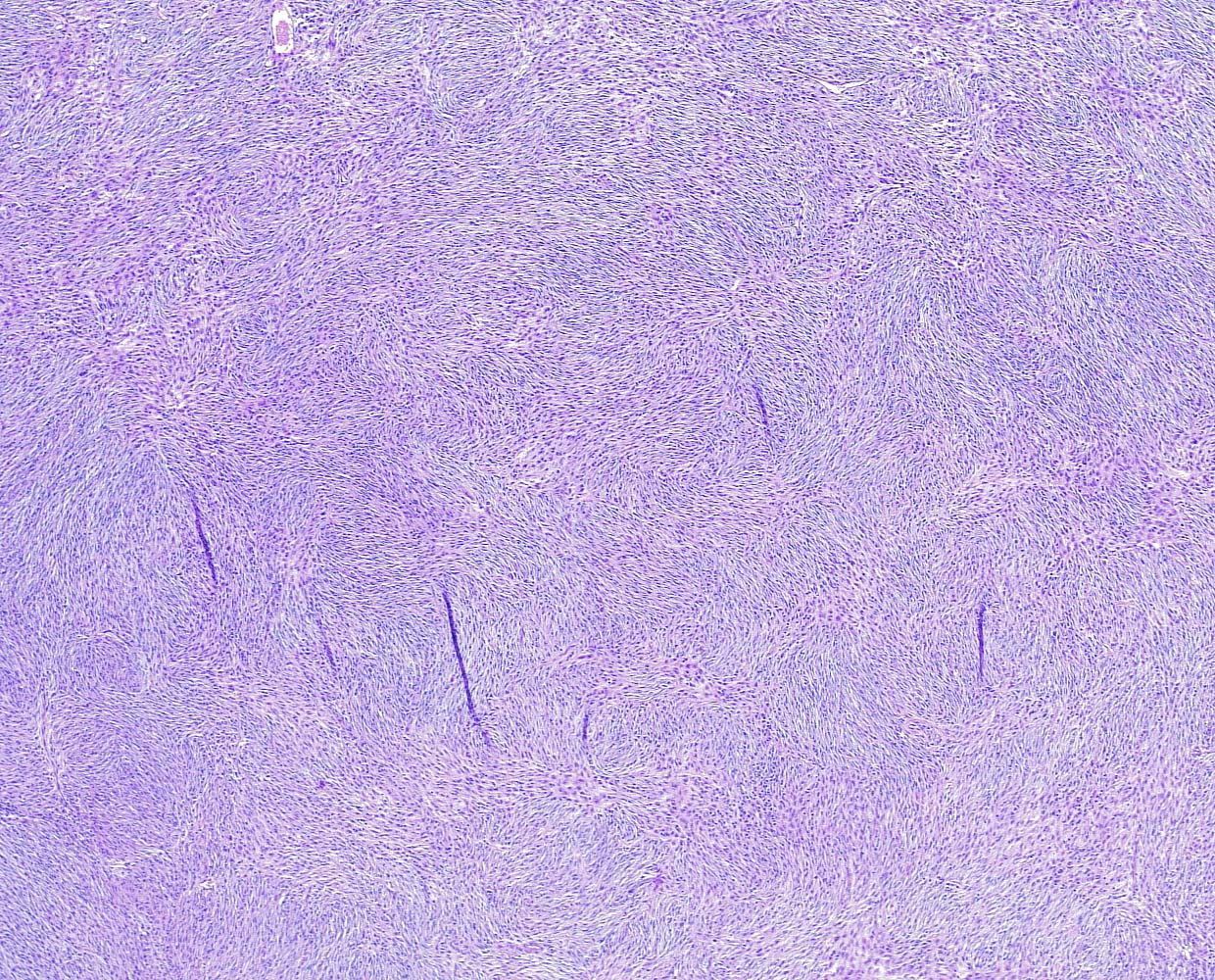
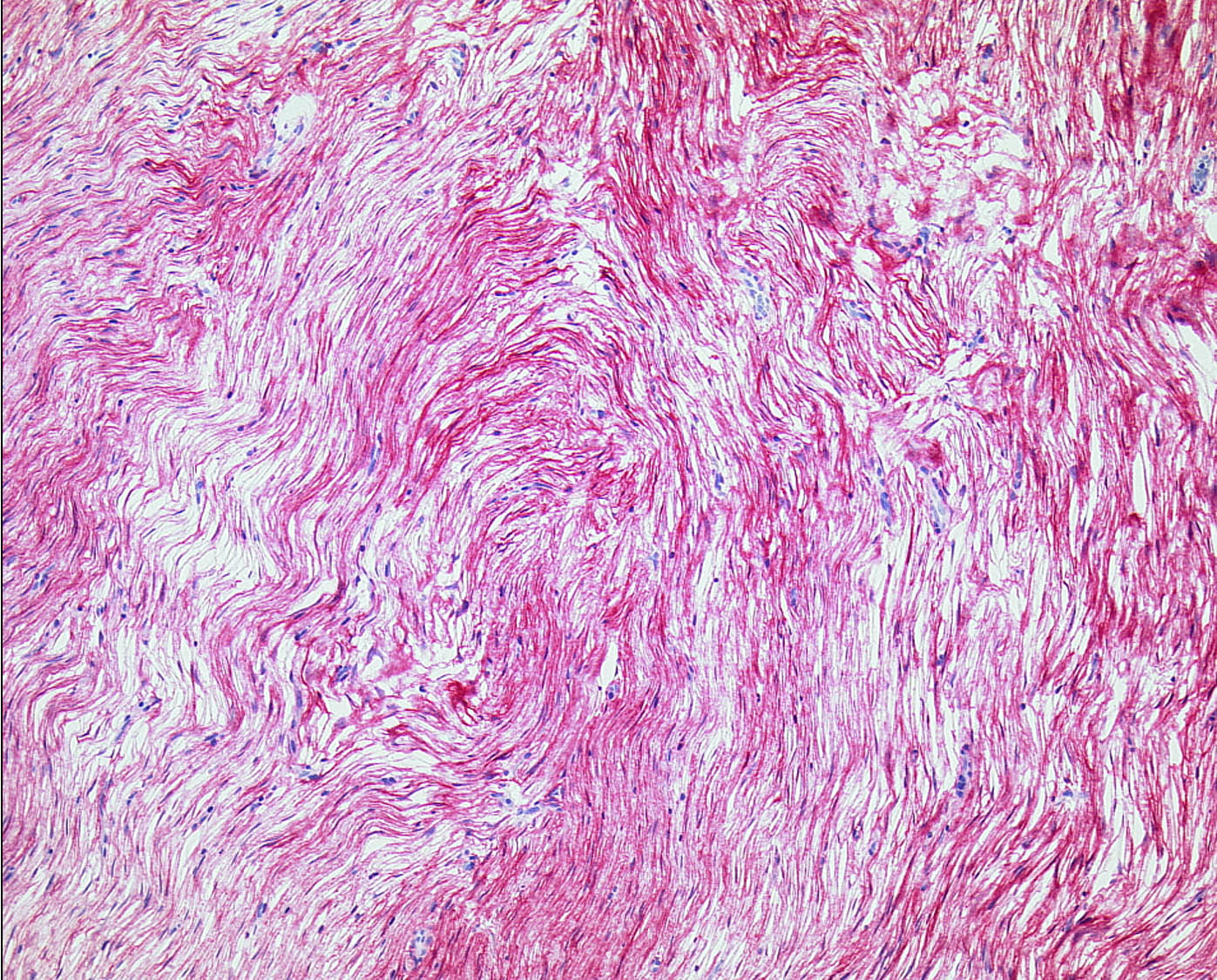
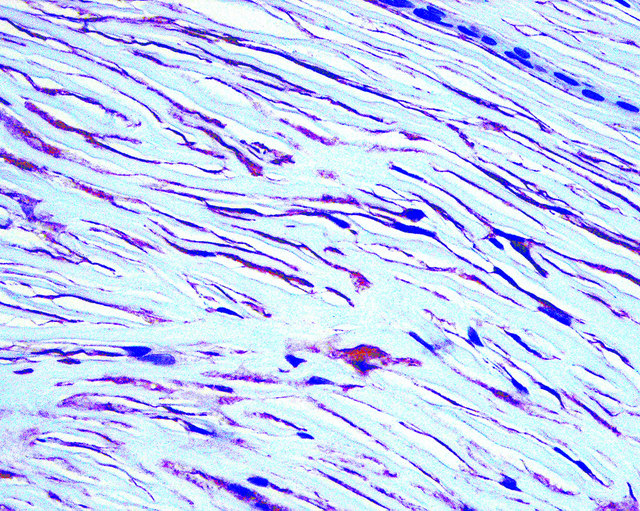
Microscopic (histologic) images
Contributed by Andrea Saggini, M.D. and Mark R. Wick, M.D.
Positive stains
- Perineuriomas express antigens that are identical to normal perineurium (EMA, GLUT1, claudin1)
- Intraneural perineurioma
- Soft tissue perineurioma (Histopathology 2014;65:60)
- EMA (100% of cases; membranous staining that may be difficult to appreciate if the cell processes are widely separated) (Am J Surg Pathol 1988;12:678)
- GLUT1 (> 75%)
- Claudin1 (> 75%) (Am J Surg Pathol 2002;26:1620)
- Positivity for 2 out of 3 perineurial markers is normally sufficient to prove perineurial phenotype (J Cutan Pathol 2020;47:195)
- CD34 (50%) (Am J Surg Pathol 2005;29:845)
- Type IV collagen and laminin highlight basement membrane material around perineurial cells (nonspecific)
- Laminin (nonspecific)
- CD10 (nonspecific)
Negative stains
- Soft tissue perineurioma
- S100
- SOX10
- Neurofilament
- GFAP
- CD57
- Melanocytic markers (MelanA, HMB45, tyrosinase)
- Cytokeratins
- Alpha smooth muscle actin (+ in 20%)
- Desmin
- References: Arch Pathol Lab Med 2007;131:625, Adv Anat Pathol 2008;15:147
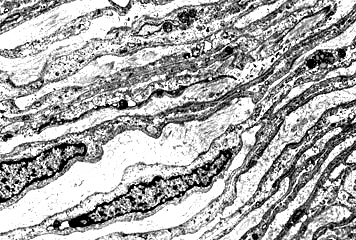
Electron microscopy description
- Soft tissue perineurioma
- Slender, nontapered processes containing large numbers of pinocytotic vesicles and partial encasement by basal lamina
Molecular / cytogenetics description
- See Pathophysiology
Sample pathology report
- Soft tissue of arm, incisional biopsy:
- Benign spindle cell tumor with morphological and immunophenotypical features (EMA+, claudin1+, S100-, pancytokeratin-, alpha smooth muscle actin-) consistent with soft tissue perineurioma, extending to all the specimen margins. Despite the apparent lack of cytological atypia, complete excision of the neoplasm is advisable.
Differential diagnosis
- Dermatofibrosarcoma protuberans:
- Storiform architecture and uniform spindle cell morphology (Ann Diagn Pathol 2016;25:64)
- Diffusely infitrative growth with honeycomb pattern in the subcutis
- CD34+ but negative perineurial markers (EMA, GLUT1, claudin1)
- PDGFB rearrangements (FISH)
- Benign fibrous histiocytoma:
- Variably fascicular and storiform architecture (Mod Pathol 2020;33:56)
- Uniform spindle cells with fine chromatin and pale eosinophilic cytoplasm
- Relative circumscription, overlying epidermal hyperplasia and lateral entrapment of hyaline dermal collagen
- EMA may be positive
- GLUT1 and claudin1 are not expressed
- Sclerotic fibroma:
- Well demarcated hypocellular, dermal fibrocollagenous proliferations
- Hyalinized eosinophilic collagen bundles arranged in interwoven pattern with prominent clefts (Am J Dermatopathol 1996;18:620)
- EMA may be positive
- GLUT1 and claudin1 are not expressed
- Solitary fibrous tumor:
- Patternless distribution of both oval and spindle shaped cells with uniform spindled nuclei and scant cytoplasm in a variably collagenous stroma
- Branched, often thick walled, hemangiopericytoma-like vessels (Ann Diagn Pathol 2018;34:142)
- EMA+ and CD34+ as in perineurioma
- STAT6+ (specific marker)
- NAB2-STAT6 fusion
- Neurofibroma (particularly myxoid variant):
- Epithelioid fibrous histiocytoma:
- Plump epithelioid cells occasionally with a spindle cell component (Mod Pathol 2018;31:753)
- Round - ovoid nuclei with minimal atypia, vesicular chromatin and scattered binucleation and trinucleation
- ALK+
- ALK rearrangements (FISH)
- Melanocytic neoplasms (desmoplastic nevus, desmoplastic melanoma):
- Desmoplastic (sclerotic) nevus: spindle shaped nevus cells within a fibrotic stroma (Am J Surg Pathol 1999;23:786)
- Desmoplastic melanoma: paucicellular proliferation of malignant spindled melanocytes within an abundant collagenous / myxoid (desmoplastic) stroma (J Surg Oncol 2019;119:208)
- S100+, SOX10+
- Cellular neurothekeoma:
- Nests of epithelioid to slightly spindled tumor cells with a subtle whorling pattern (StatPearls: Neurothekeoma [Accessed 7 April 2021])
- Relatively abundant eosinophilic cytoplasm and round to oval nuclei with small pinpoint nucleoli
- Perineurial markers (EMA, GLUT1, claudin1) not expressed
- Low grade fibromyxoid sarcoma:
- Low to moderate cellularity and consists of bland spindle cells with small, angulated nuclei and scant, wispy cytoplasm (Ann Diagn Pathol 2017;28:60)
- Whorled growth pattern with abrupt transition from myxoid to fibrous areas
- EMA+ and claudin1+
- MUC4+ (specific marker)
- FUS-CREB3L2 fusion in majority of cases
Board review style question #1
A 34 year old man presented with a fibroma-like nodule on the left thigh. The tumor was completely excised. Histologic details are shown in the image above. Regarding this entity, which of the following statements is true?
- EMA positivity is sufficiently sensitive and specific for the diagnosis
- Positivity for claudin1 is often observed and may be helpful for diagnostic purposes
- S100 may be diffusely positive due to the neural differentiation of the neoplasm
- SOX10 is always positive
Board review style answer #1
B. Positivity for claudin1 is often observed and may be helpful for diagnostic purposes
The picture shows a nonencapsulated, well demarcated tumor consisting of a population of benign spindle cells with slender, fibroblast-like appearance and long, delicate cytoplasmic processes; the degree of cellularity is intermediate and the vascularity is increased at the periphery of the tumor.
EMA positivity is typically observed in the normal perineurium as well as in neoplastic cells with perineurial differentiation but EMA positivity alone is not specific for perineurial differentiation and requires concomitant positivity for at least another perineurial marker among GLUT1 and claudin1. S100 and SOX10 are typically negative in perineuriomas, due to the lack of cells with Schwannian differentiation; an exception is represented by hybrid neural tumors with concomitant perineurial and schwannomatous / neurofibromatous differentiation.
Comment Here
Reference: Perineurioma
The picture shows a nonencapsulated, well demarcated tumor consisting of a population of benign spindle cells with slender, fibroblast-like appearance and long, delicate cytoplasmic processes; the degree of cellularity is intermediate and the vascularity is increased at the periphery of the tumor.
EMA positivity is typically observed in the normal perineurium as well as in neoplastic cells with perineurial differentiation but EMA positivity alone is not specific for perineurial differentiation and requires concomitant positivity for at least another perineurial marker among GLUT1 and claudin1. S100 and SOX10 are typically negative in perineuriomas, due to the lack of cells with Schwannian differentiation; an exception is represented by hybrid neural tumors with concomitant perineurial and schwannomatous / neurofibromatous differentiation.
Comment Here
Reference: Perineurioma
Board review style question #2
A 36 year old woman presented with a subcutaneous nodule on the left buttock. The nodule was completely excised and the final histopathologic report rendered a diagnosis of soft tissue perineurioma. Regarding this entity, which of the following statements is true?
- Atypical soft tissue perineuriomas exhibit clinically indolent behavior
- EMA is a useful immunohistochemical marker in the differential diagnosis with meningioma
- FISH plays no role in the diagnostic process of soft tissue perineurioma
- Immunohistochemical expression of alpha smooth muscle actin virtually rules out a diagnosis of soft tissue perineurioma
Board review style answer #2
A. Atypical soft tissue perineuriomas exhibit clinically indolent behavior
Atypical soft tissue perineuriomas are defined by presence (in variable combination) of scattered cytological atypia, mildly increased mitotic activity (> 13 figures/30 high power fields), increased cellularity or infiltration of muscle. Despite such partially worrisome histopathologic features, they normally exhibit clinically indolent behavior.
Immunohistochemical expression of alpha smooth muscle actin (patchy or rarely, diffuse) may be observed in up to 20% of soft tissue perineuriomas, while expression of desmin should be never observed. FISH may be employed to rule out the presence of PDGFB rearrangements in cases characterized by strong positivity for CD34 coupled with a storiform pattern suspicious for dermatofibrosarcoma protuberans. EMA is also positive in meningiomas; the differential diagnosis with the latter may be aided by immunohistochemical staining for SSTR2A and PR (which are negative in perneurioma but positive in most meningiomas).
Comment Here
Reference: Perineurioma
Atypical soft tissue perineuriomas are defined by presence (in variable combination) of scattered cytological atypia, mildly increased mitotic activity (> 13 figures/30 high power fields), increased cellularity or infiltration of muscle. Despite such partially worrisome histopathologic features, they normally exhibit clinically indolent behavior.
Immunohistochemical expression of alpha smooth muscle actin (patchy or rarely, diffuse) may be observed in up to 20% of soft tissue perineuriomas, while expression of desmin should be never observed. FISH may be employed to rule out the presence of PDGFB rearrangements in cases characterized by strong positivity for CD34 coupled with a storiform pattern suspicious for dermatofibrosarcoma protuberans. EMA is also positive in meningiomas; the differential diagnosis with the latter may be aided by immunohistochemical staining for SSTR2A and PR (which are negative in perneurioma but positive in most meningiomas).
Comment Here
Reference: Perineurioma