Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Clinical images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Esteves GF, Félix A. Dermal nerve sheath myxoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuenervesheathmyxoma.html. Accessed March 30th, 2025.
Definition / general
- Benign tumor, usually cutaneous, derived from Schwann cells (peripheral nerve sheath) but without the characteristic features of conventional schwannoma
- Probably a myxoid variant of schwannoma
Essential features
- Benign tumor with Schwannian differentiation
- Multilobulated and myxoid without the characteristic features of conventional schwannoma
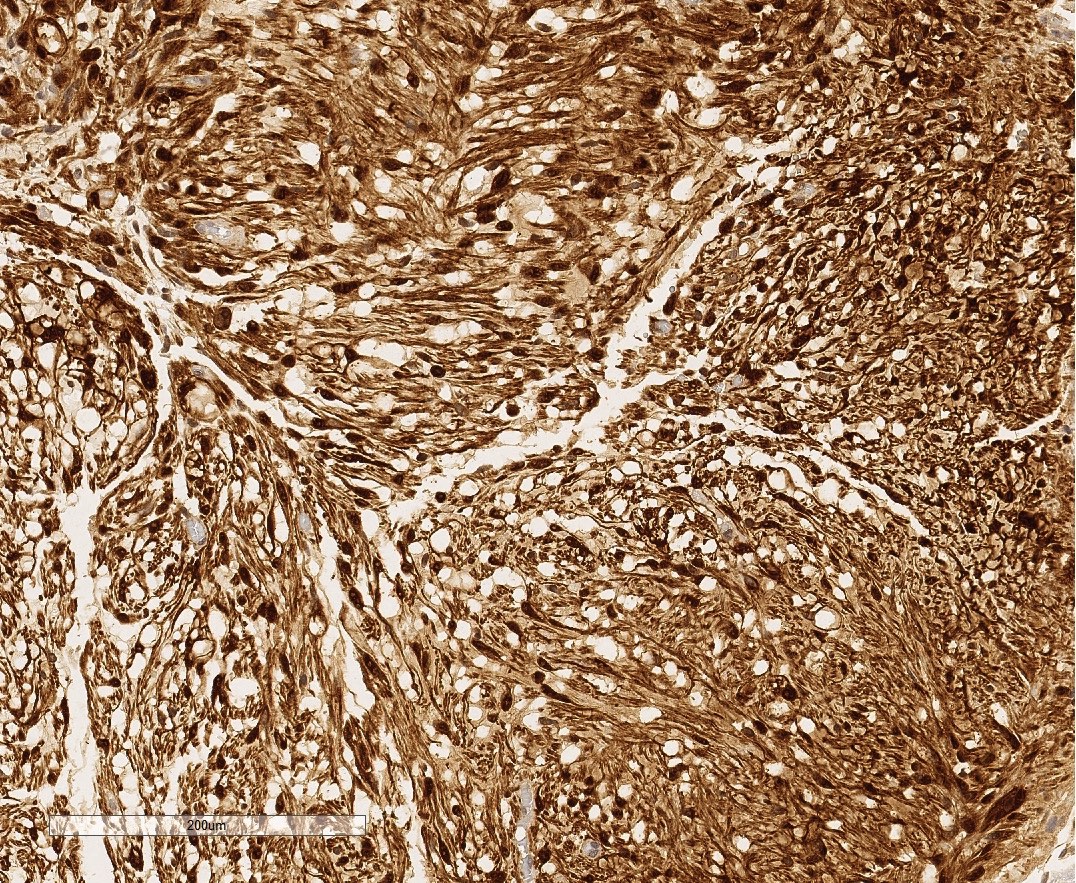
- Diffuse S100 positivity is key to distinguishing it from neurothekeoma
Terminology
- Historically it has been equated with the classic or myxoid variant of neurothekeoma but given their altogether different clinical, immunohistochemical, ultrastructural and molecular features, that is no longer considered to be true by most authors
ICD coding
- ICD-O: 9562/0 - Neurothekeoma, nerve sheath myxoma
Epidemiology
- All ages but mainly young and middle aged adults are affected
- M = F
- More than 5 times rarer than neurothekeoma
Sites
- Extremities (85%), most often the fingers
- Only rarely does it involve the head and neck region
Etiology
- Unknown
Clinical features
- A solitary, small, mobile and flesh colored to translucent nodule, undergoing slow, usually painless growth
- Frequently presents as a longstanding mass (up to more than 20 years) (Am J Surg Pathol 2005;29:1615)
- Nonpolarized contact dermoscopy showed diffuse gray to yellow background, cobblestone-like areas, and gray structureless areas with hairpin, linear and twisted vessels around them (Clin Exp Dermatol 2019;44:206)
Diagnosis
- No specific clinical diagnostic features have been described associated with this entity
- Diagnosis is made by pathology examination in excised lesions
Case reports
- 34 year old man with a thrice recurring tumor on eyelid misdiagnosed as mucocele (Korean J Ophthalmol 2019;33:202)
- 35 year old man with a perianal tumor (Indian J Pathol Microbiol 2017;60:610)
- 43 year old woman with a tongue tumor (Clin Case Rep 2017;6:302)
- 55 year old woman with a scalp tumor (Int J Trichology 2019;11:34)
Treatment
- Complete local excision with free margins and subsequent follow up is advisable, as a high recurrence rate (47%) was found to be associated with simple excision (Am J Surg Pathol 2005;29:1615)
- It is an otherwise totally benign tumor
Gross description
- Majority < 2.5 cm in greatest axis (0.4 - 4.5 cm)
- Rubbery to firm consistency
- Well demarcated, translucent to white, mucoid and glistening upon sectioning
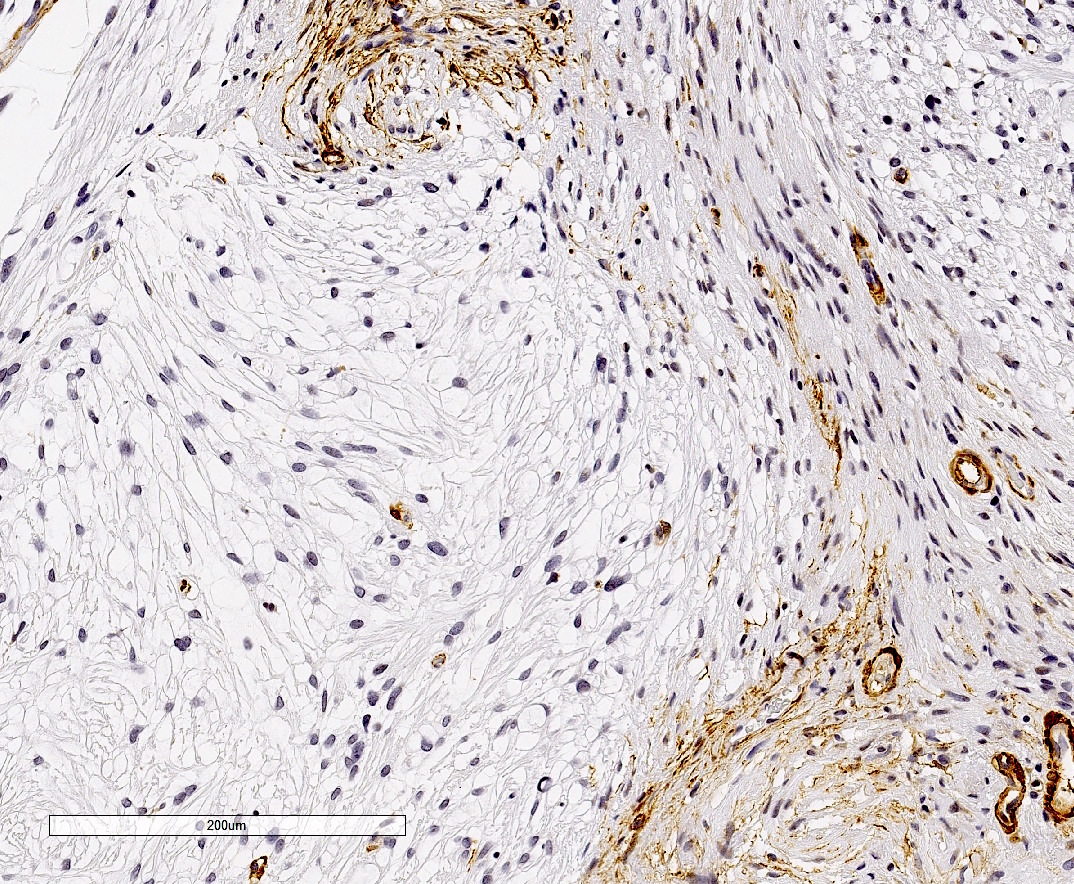
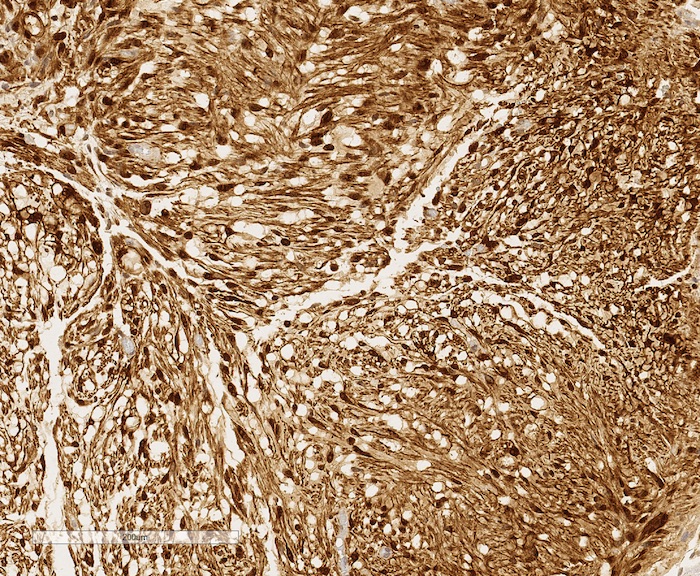
Microscopic (histologic) description
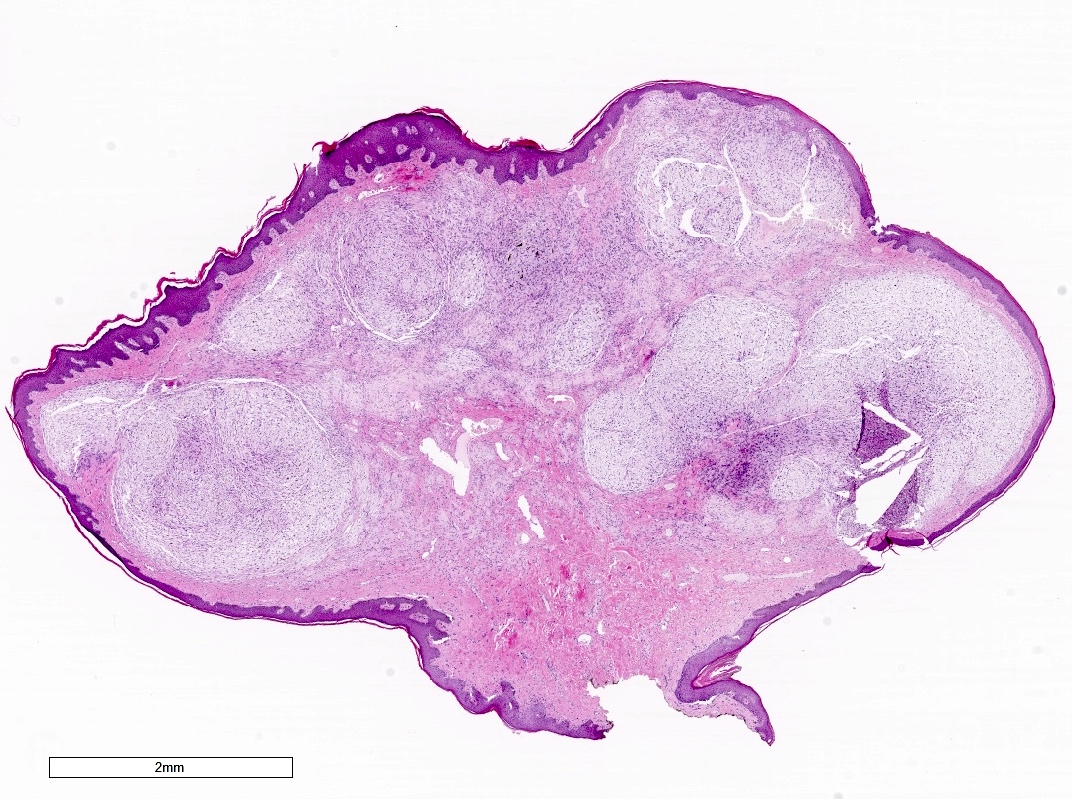
- Unencapsulated multilobulated tumor occupying dermis or subcutis
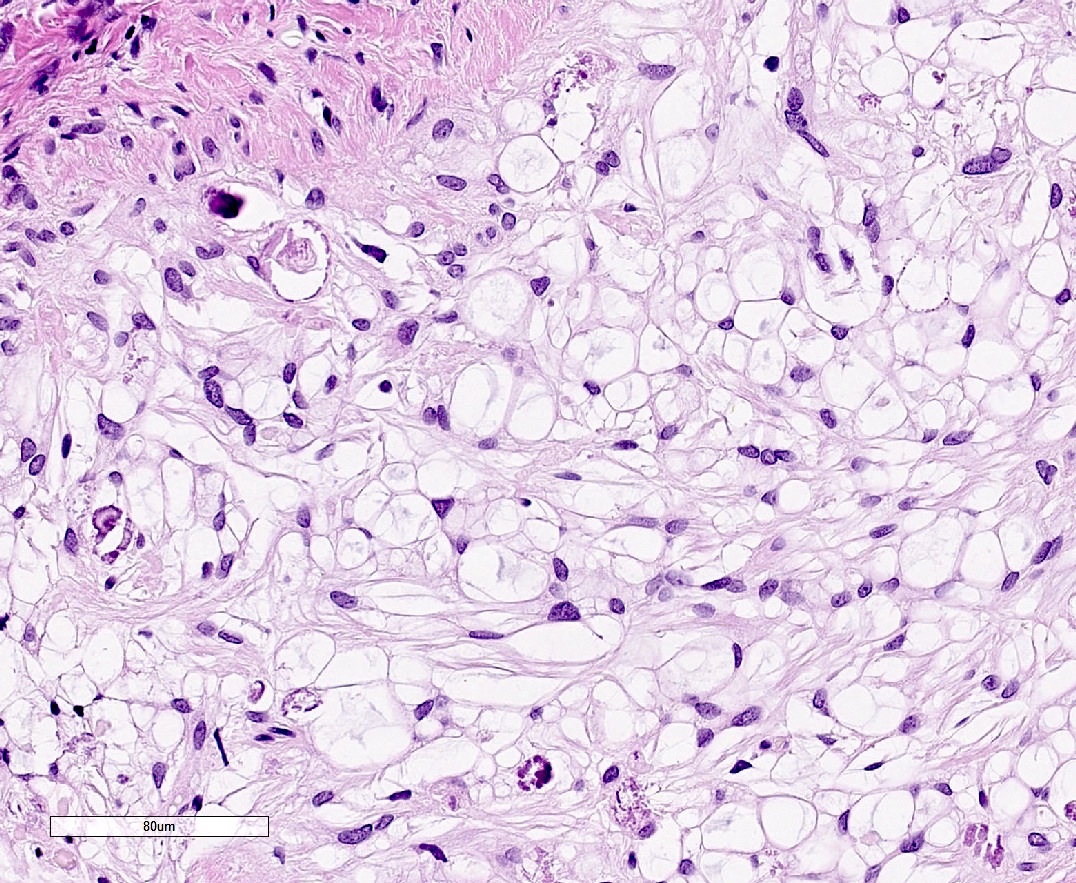
- Well circumscribed myxoid lobules with fibrous rims
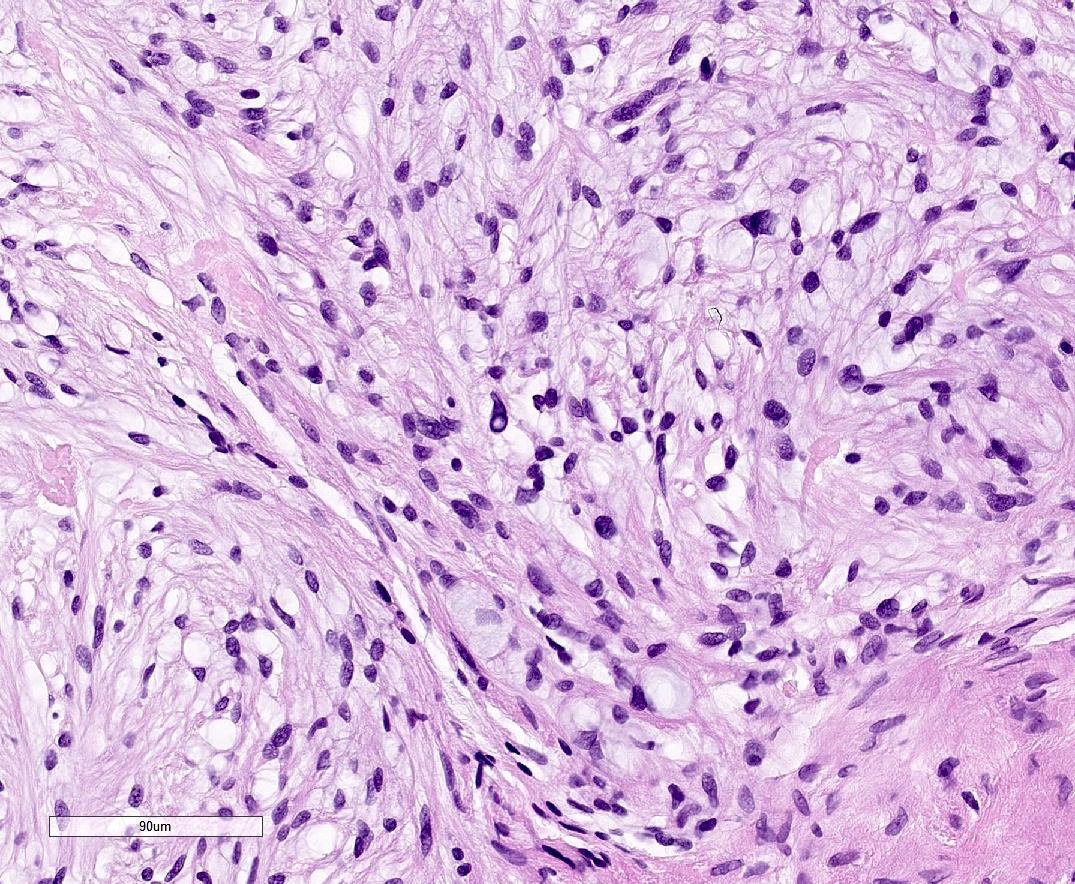
- Neoplastic cells are small and may be spindled, stellate, epithelioid and ring shaped (often with cytoplasmic nuclear invaginations)
- Mild nuclear atypia at the most, with rare or no mitotic figures
- Scant eosinophilic cytoplasm envelops small round nuclei, with thin bipolar or multipolar (spider-like) processes
- Cellular interconnections are common so cord-like, nested and syncytial arrangements may develop
- A hyperplastic and hyperpigmented epidermal reaction, similar to benign fibrous histiocytomas, was reported (Clin Exp Dermatol 2019;44:206)
Microscopic (histologic) images
Cytology description
- Fine needle aspiration yields a greyish jelly-like material
- Isolated round to stellate cells with bland nuclei
- Metachromatic fibrillary myxoid stroma (pink on Diff-Quik stain and pale blue on Papanicolaou stain)
- Some cells may appear in cords and loose clusters (Diagn Cytopathol 2002;27:173)
- Multiple elongated cytoplasmic processes may be apparent (J Clin Diagn Res 2015;9:ED07)
- Binucleated and multinucleated cells may be present
- Consider also the differential diagnoses of myxoid neurofibroma, myxoid schwannoma, myxoid neurothekeoma and cutaneous mucinosis, from which it is usually impossible to distinguish on cytology grounds
Positive stains
- S100 (diffuse staining)
- GFAP, CD57 (Leu-7), neuron-specific enolase (NSE), p75 (neurotrophin receptor)
- Collagen IV (strong pericellular expression)
- EMA limited to some perineurial cells (in more than 50% of the cases) and CD34 to some intraneural fibroblasts
- Rare neoplastic cells may react with AE1 / AE3 cytokeratin cocktail
Negative stains
- CD10, HMB45
- CD63 (NKI/C3), SMA
- Neurofilament (rare cases may have some axons highlighted)
Molecular / cytogenetics description
- Very similar molecular genetic signatures to dermal schwannoma, in contrast to that of neurothekeoma, which more closely resembles cellular fibrous histiocytomas (Mod Pathol 2011;24:343)
Sample pathology report
- Finger, left middle, excision:
- Dermal nerve sheath myxoma, 0.8 cm
- Surgical margins, negative for tumor
Differential diagnosis
- Neurothekeoma (especially myxoid and mixed variants)
- More often affects females and the head and neck region
- Multilobulated or micronodular tumor but with spindled and epithelioid cells
- Nonspecific immunophenotype (ie, uncertain histogenesis): positive for CD63, NSE (89%) and sometimes at least focally for SMA (34 - 60%)
- Negative for S100 and GFAP
- Consistently positive for CD10 (Mod Pathol 2014;27:701)
- Myxoid schwannoma
- Usually encapsulated as a whole, not in individual lobules
- Distinctive morphologic features include alternating Antoni A and B areas, nuclear palisading (Verocay bodies) and hyalinized vessels
- Superficial acral fibromyxoma (digital fibromyxoma)
- Cutaneous myxoma (superficial angiomyxoma)
- Reported in half of patients with Carney complex
- Most common in the head, neck and trunk
- Well circumscribed, vaguely lobulated tumor with prominent mucinous matrix and vascularity
- Contains variably shaped fibroblasts but is less cellular
- Accompanying inflammatory infiltrate containing neutrophils
- Up to 25% of cases have entrapped epithelial structures
- Expresses CD34 but not S100 (Am J Surg Pathol 1999;23:910)
- Dermal mucinosis
- Group of essentially disparate nonneoplastic diseases (except for cutaneous myxoma), having in common only dermal mucin deposition
- May be cell poor, with few stellate-like forms (e.g. pretibial myxedema, scleredema), or show some degree of fibroblastic proliferation (e.g. scleromyxedema)
- A perivascular lymphocytic infiltrate is usually present
- No sharply demarcated lobules
Board review style question #1
Board review style answer #1
Board review style question #2
- Which of the following is a purely neural tumor?
- Neurofibroma
- Dermal nerve sheath myxoma
- Neurothekeoma
- Chondroid syringoma
- Benign Triton tumor
Board review style answer #2