Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zafar G, Ud Din N. Myositis ossificans and fibro-osseous pseudotumor of digits. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuemyositis.html. Accessed April 2nd, 2025.
Definition / general
- Myositis ossificans and fibro-osseous pseudotumor of digits are self limited, benign neoplasms composed of spindle cells and osteoblasts
- Myositis ossificans, fibro-osseous psedotumor and soft tissue aneurysmal bone cyst belong to the same neoplastic spectrum
Essential features
- Benign, reactive, ossifying soft tissue mass lesion, associated with trauma and characterized by zonal pattern
Terminology
- Not recommended:
- Pseudomalignant osseous tumor of soft tissue, myositis ossificans circumscripta, myositis ossificans traumatica
- Related entities:
- Panniculitis / fasciitis ossificans: similar histologic features but involves subcutis and tendons / fascia rather than muscle
ICD coding
- ICD-10: M61.00 - myositis ossificans traumatica, unspecified site
Epidemiology
- Usually physically active young males (second and third decade) with rapid growth of mass (Clin Case Rep 2021;9:e04608)
- 60 - 75% have history of trauma in prior 4 - 6 weeks (J Med Case Rep 2010;4:270)
- May also occur after elective surgery, severe burns, neurological injury
Sites
- Usually occurs in anterior muscle groups of thigh and arm (more prone to injury); e.g., brachialis, adductors and quadriceps (Curr Sports Med Rep 2018;17:290)
- Can also occur in head and neck region (Head Face Med 2018;14:23)
Pathophysiology
- Pathogenesis is poorly understood
- Thought to develop from differentiation of fibroblast to osteoblast secondary to inflammatory cytokine activity, particularly bone morphogenetic protein 1 (BMP1), BMP2 and transforming growth factor (TGF)
- These cytokines promote differentiation of perivascular mesenchymal cells into osteoblasts and chondroblasts, which then undergo endochondral ossification (J Am Acad Orthop Surg 2015;23:612)
Etiology
- Most of the cases occur secondary to trauma (can be repetitive microtrauma) (BMJ Case Rep 2020;13:e233210)
- Intramuscular hematoma, previous surgery and neurological injury (Clin Case Rep 2021;9:e04608)
- Nontraumatic myositis ossificans can result from some bacterial or viral illness, leading to activation of inflammatory cascade (Autops Case Rep 2021;11:e2021316, Exp Ther Med 2021;21:531)
Clinical features
- Divided into 3 phases (Curr Sports Med Rep 2018;17:290, Indian J Radiol Imaging 2012;22:35, Ital J Pediatr 2020;46:110):
- Early (days to a few weeks): diffuse, tender soft tissue swelling with decreased range of motion
- Intermediate (1 - 2 months): more circumscribed, indurated, firm to stony hard soft tissue mass with persistent pain and decreased range of motion
- Late, mature (> 2 months): stony hard soft tissue mass is palpable with subsided pain and improved range of motion
- If swelling develops near neurovascular structures, it can cause paresthesia and muscle weakness (J Int Med Res 2021;49:3000605211002680)
Diagnosis
- Diagnosis requires correct clinical history (history of trauma), physical examination (soft tissue mass, restricted range of motion), radiological and histological findings (described below) (J Int Med Res 2021;49:3000605211002680, Head Face Med 2018;14:23)
Laboratory
- Usually not required for diagnosis
- Early stage (0 - 4 weeks):
- Serum alkaline phosphatase (SAP): normal
- C reactive protein (CRP) and erythrocyte sedimentation rate (ESR): elevated
- Creatinine phosphokinase (CPK): elevated
- Intermediate stage (4 - 8 weeks):
- SAP: elevated
- CRP and ESR: normal to mildly elevated
- CPK: elevated
- Mature, late stage (> 8 weeks):
- SAP: elevated
- CRP and ESR: normal
- CPK: normal to mildly elevated
- Reference: Curr Sports Med Rep 2018;17:290
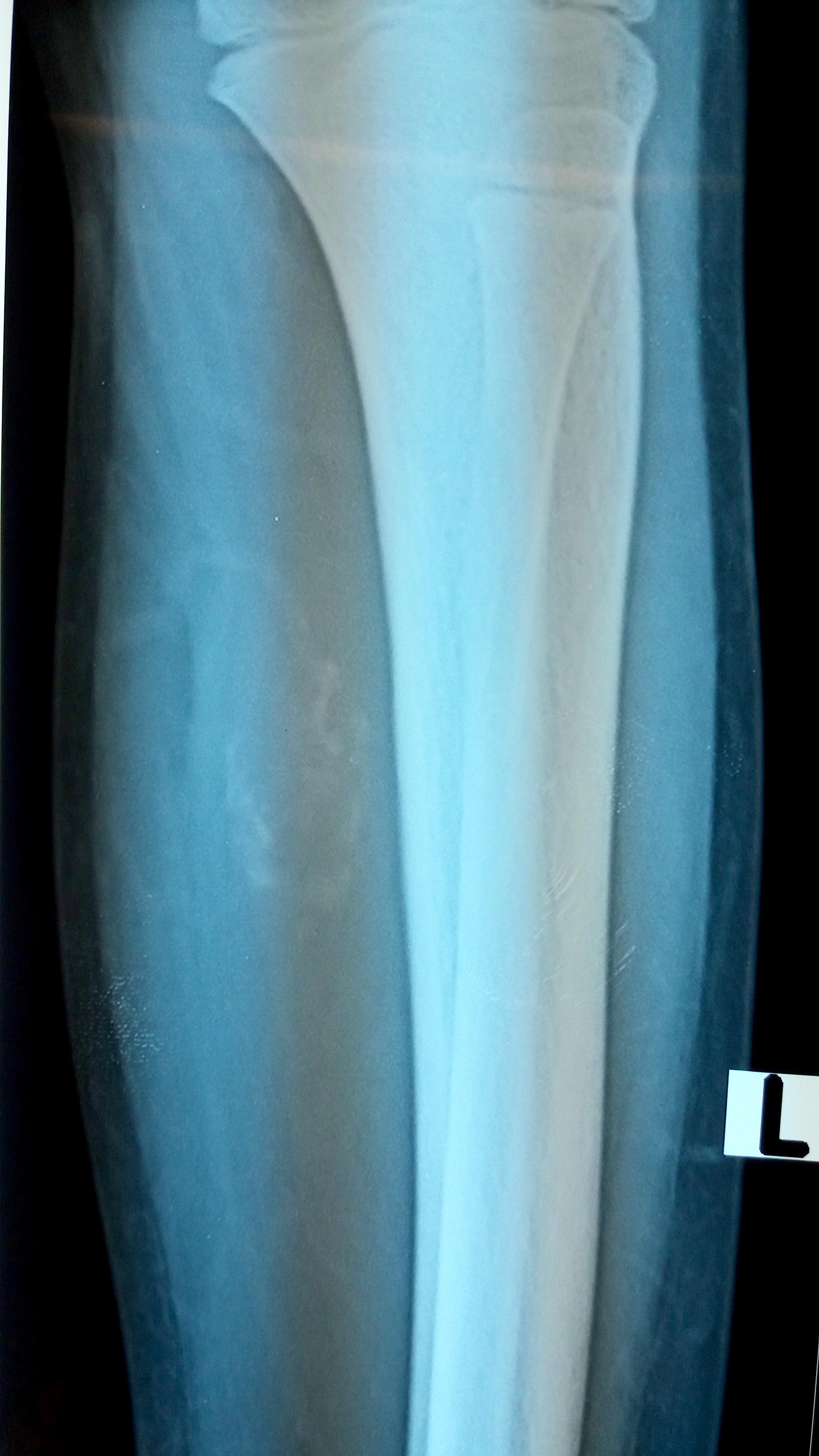
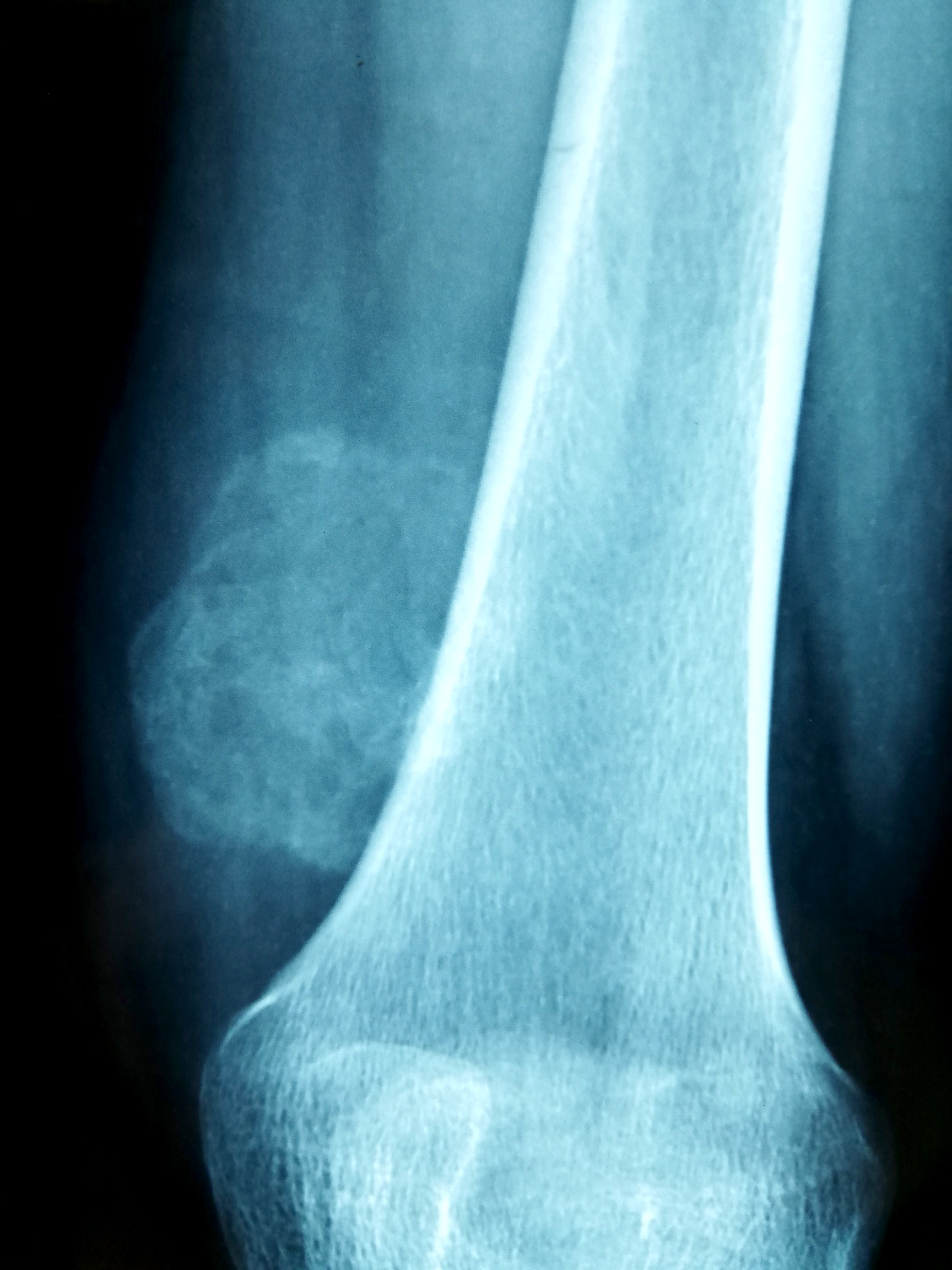
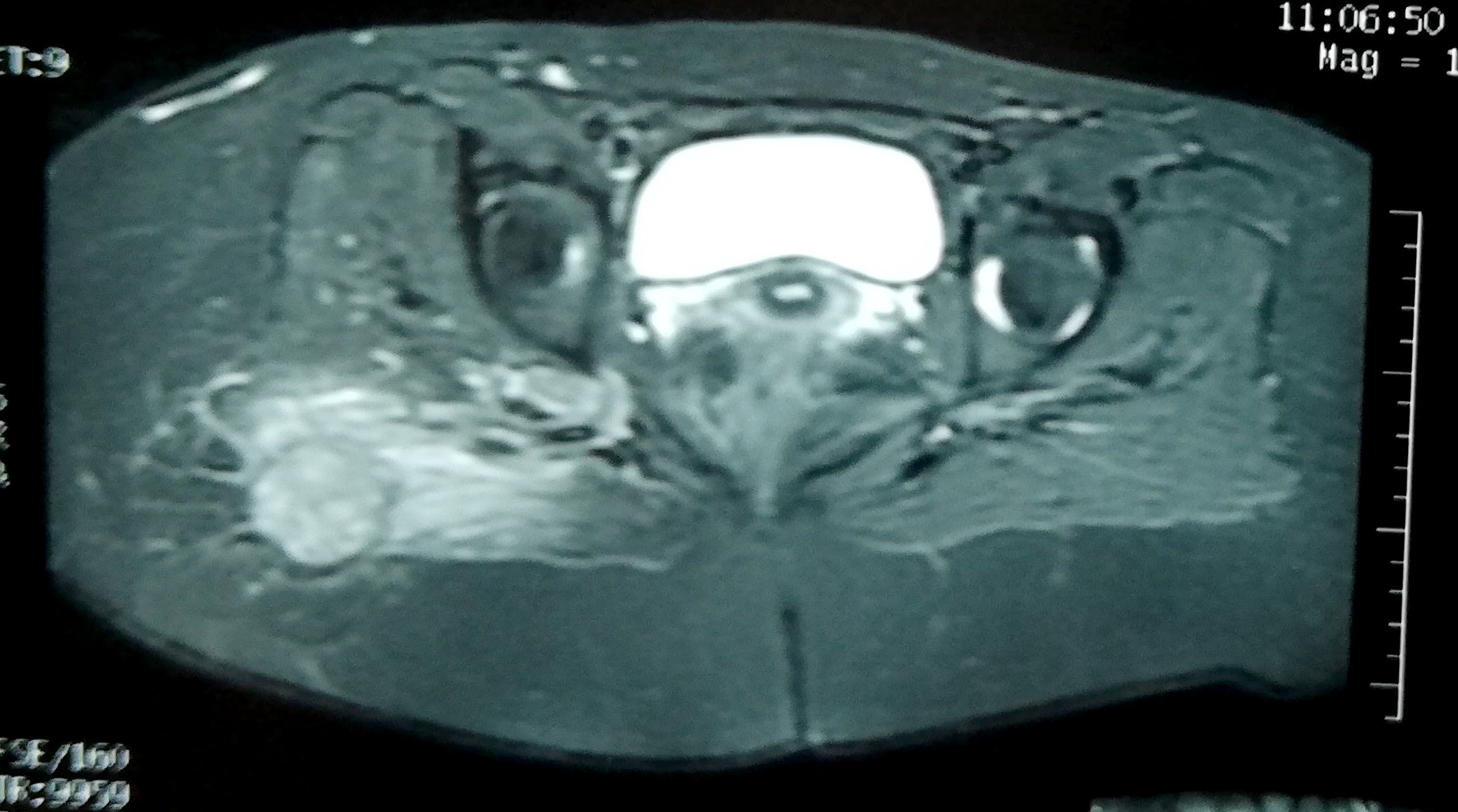
Radiology description
- Early stage:
- Xray: normal to faint calcification (flocculent radiopacities: dotted veil pattern)
- CT scan: soft tissue edema
- MRI: isodense on T1 and hyperintense on T2
- Intermediate stage:
- Xray: peripheral calcified rim with central lucency
- CT scan: peripheral mineralization with central low attenuation (calcification proceeds from periphery to center)
- MRI: isodense / hypodense to adjacent skeletal muscle on all images
- Mature, late stage:
- Xray: diffuse soft tissue calcification
- CT scan: diffuse ossification pattern (even in late lesions, the central core may remain uncalcified)
- MRI: well defined soft tissue mass and isodense to fat on all images
- References: Curr Sports Med Rep 2018;17:290, J Clin Orthop Trauma 2021;17:123
Radiology images
Prognostic factors
- Benign process with excellent prognosis
- Does not recur if completely excised
- If incompletely excised at early stage, it may continue to grow
- Spontaneous regression has also been observed (Autops Case Rep 2021;11:e2021316)
- Very rarely malignant transformation into extraskeletal osteosarcoma has been noted (Am J Orthop (Belle Mead NJ) 2014;43:E25)
- Reference: Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2019
Case reports
- 5 year old girl with hard swelling on right side of lower back (World Neurosurg 2019;123:208)
- 12 year old girl with painful axillary mass (Autops Case Rep 2021;11:e2021316)
- 25 year old man with discharging wound on left arm (J Orthop Case Rep 2014;4:57)
- 28 year old man with left elbow myositis ossificans causing ulnar neuropathy (J Int Med Res 2021;49:3000605211002680)
- 71 year old man with multifocal masticatory muscle myositis ossificans (Braz J Otorhinolaryngol 2019;85:259)
Treatment
- Surgical excision
- Spontaneous regression has also been noted (Autops Case Rep 2021;11:e2021316)
- References: Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2019, Mol Clin Oncol 2018;8:749
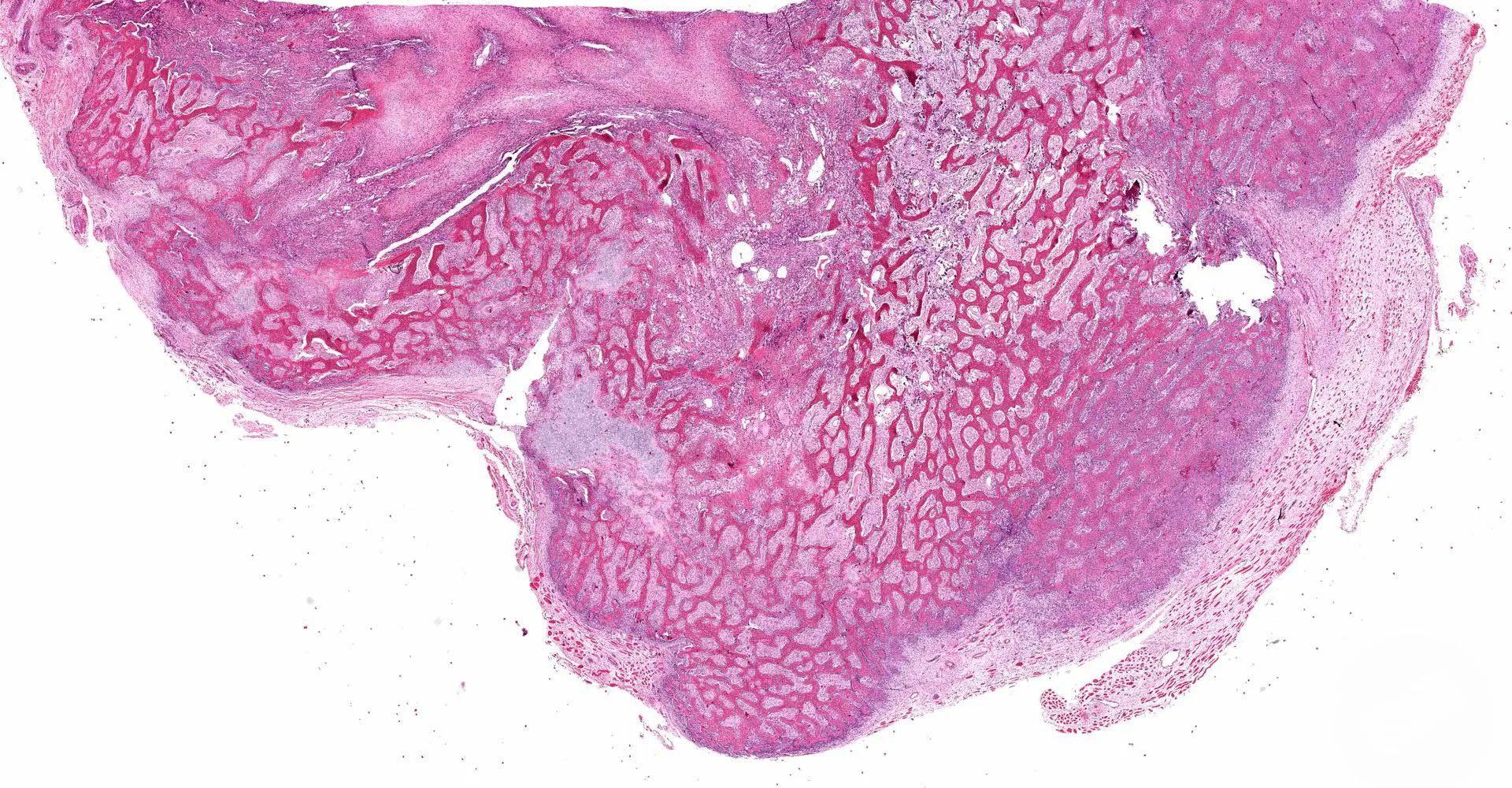
Gross description
- Well circumscribed mass with firm, gritty cut surface (Indian J Thorac Cardiovasc Surg 2020;36:657)
- Center of the lesion is usually soft, gelatinous or hemorrhagic
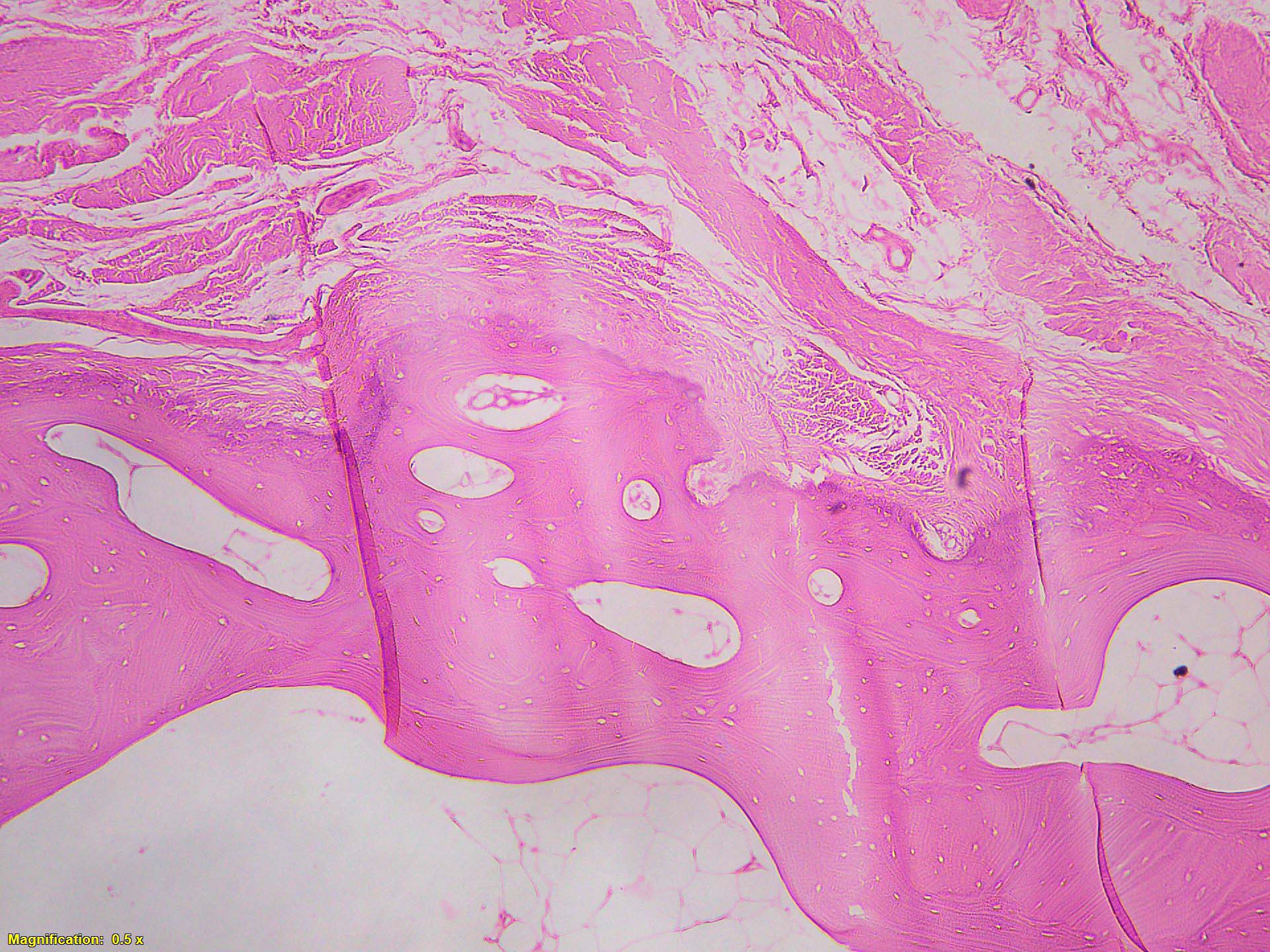
Microscopic (histologic) description
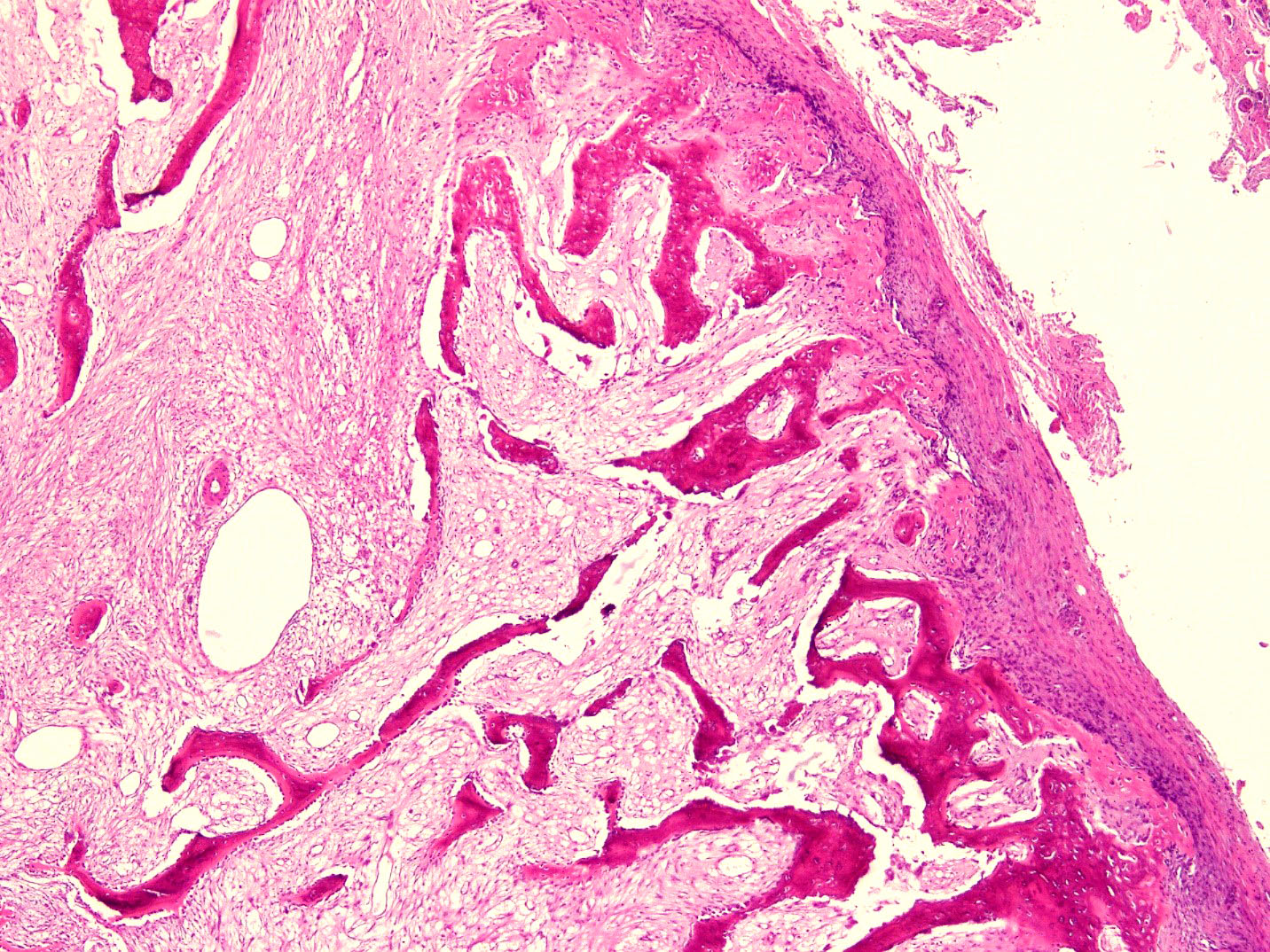
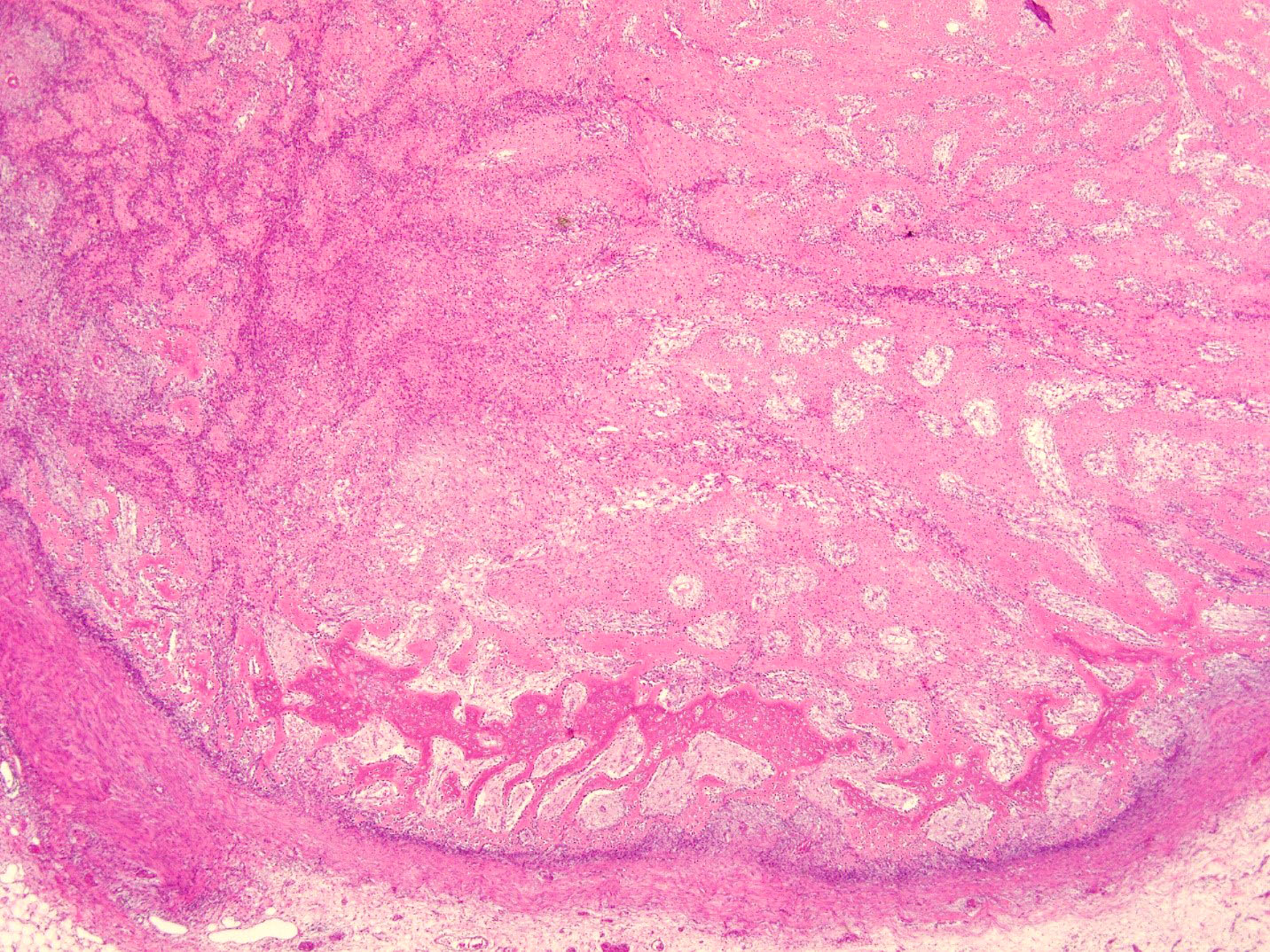
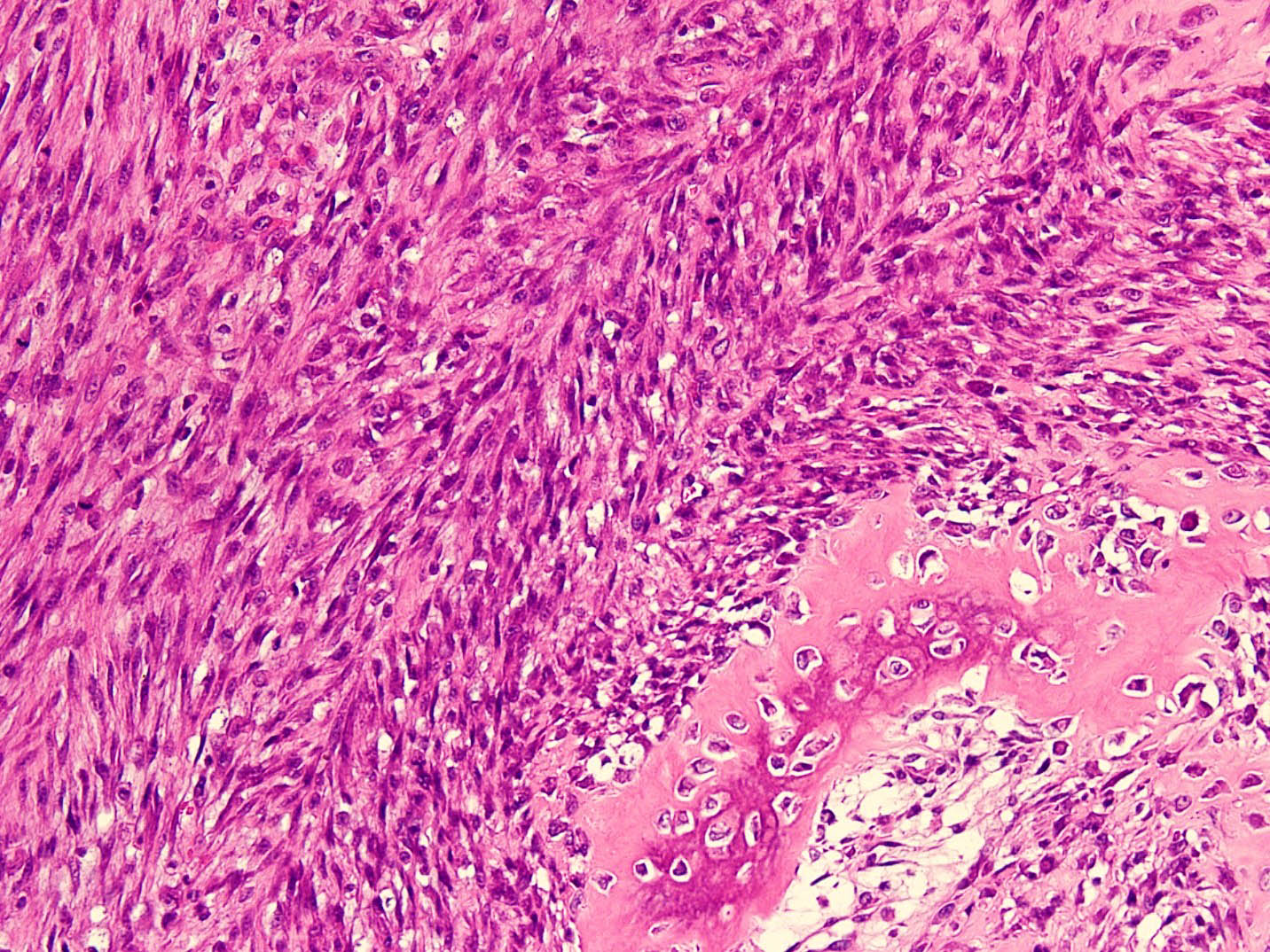
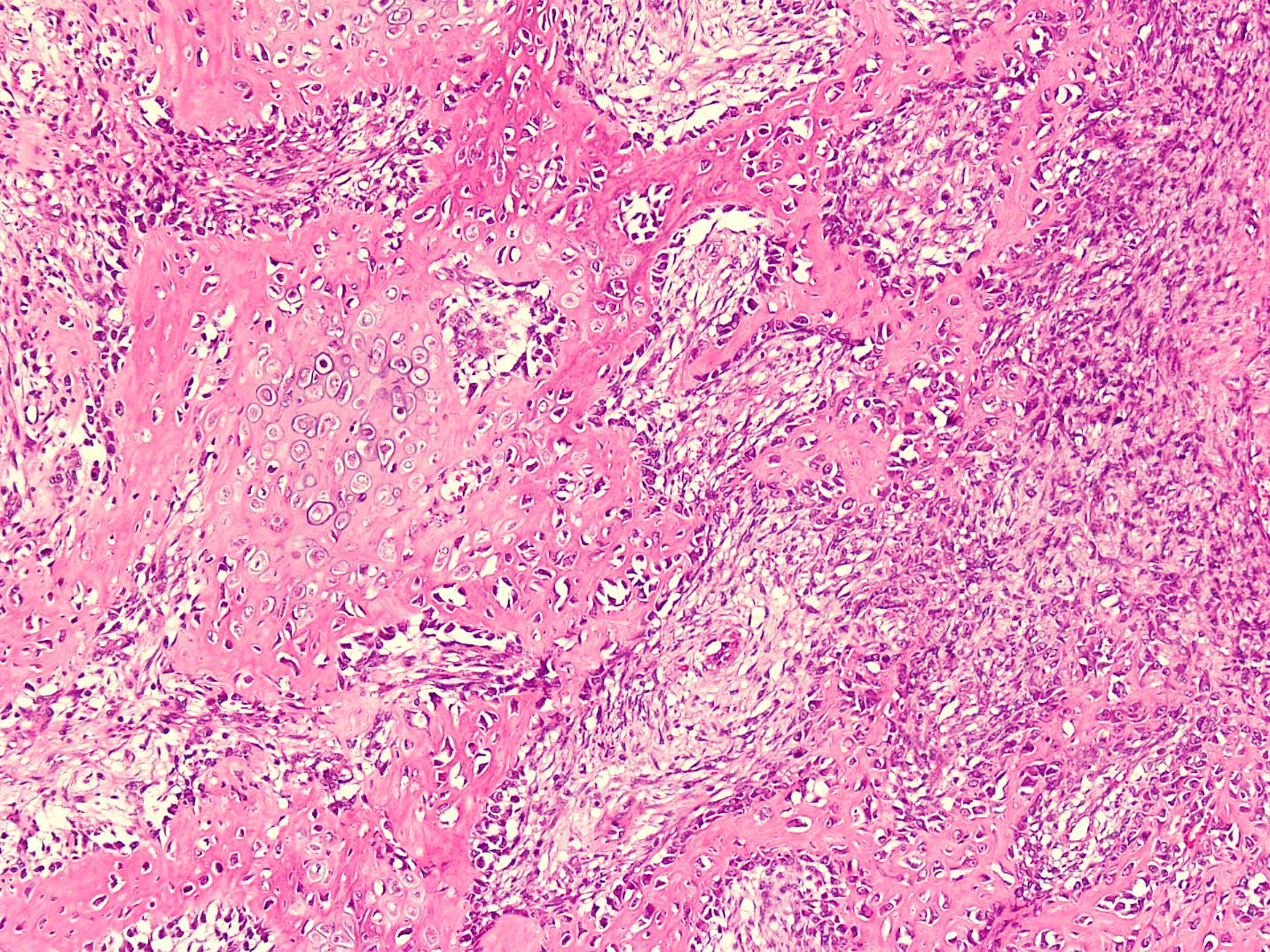
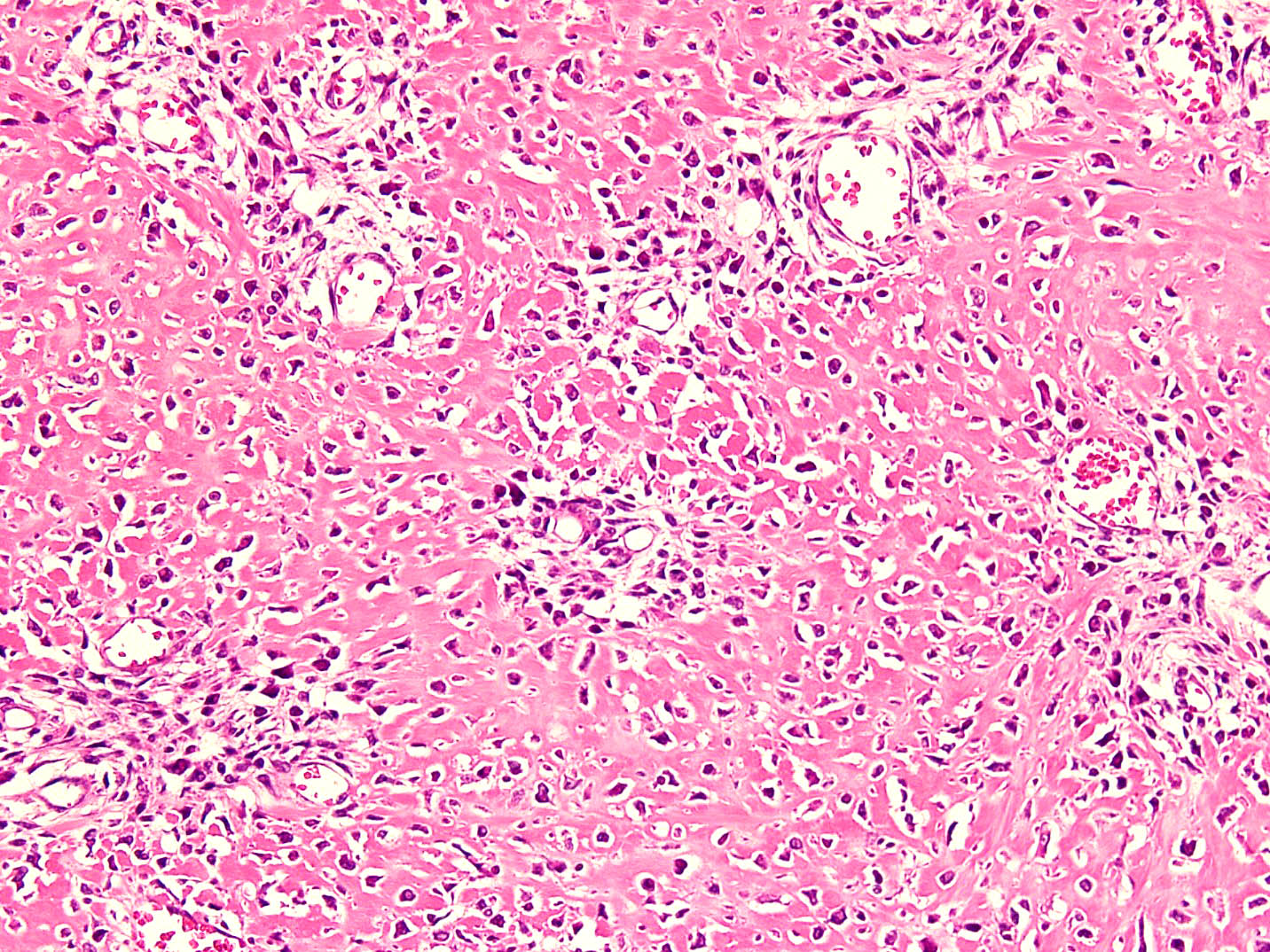
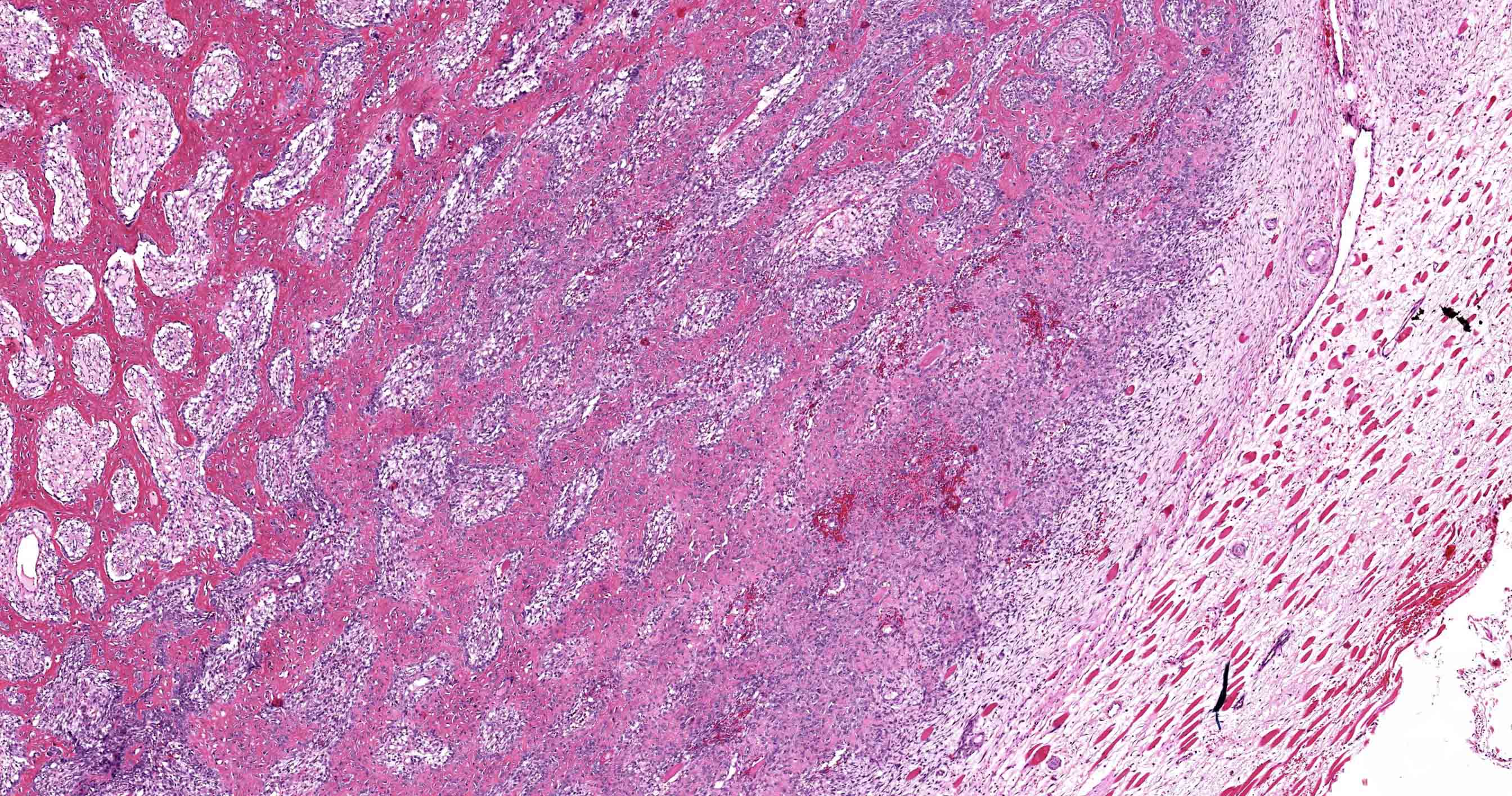
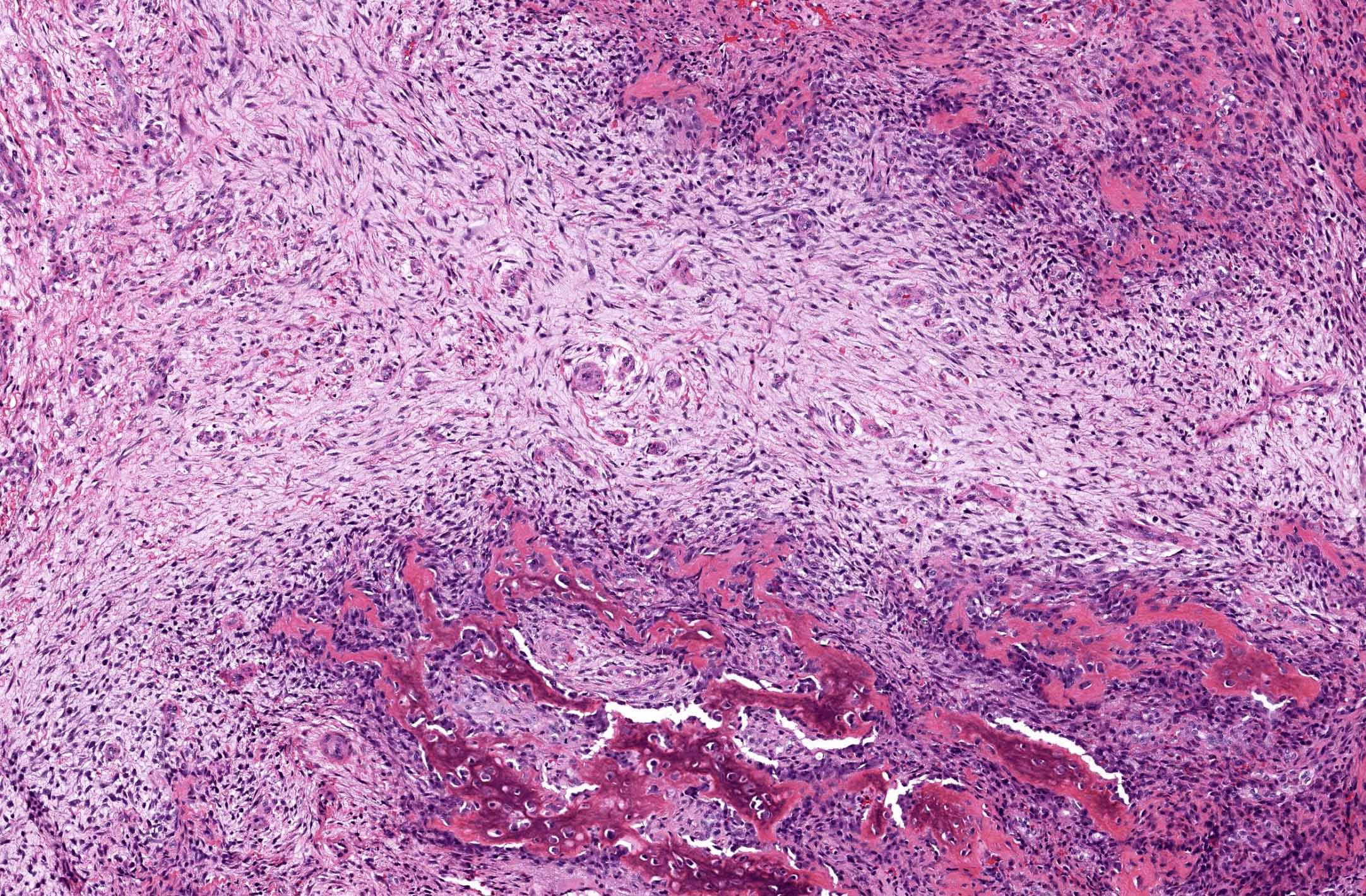
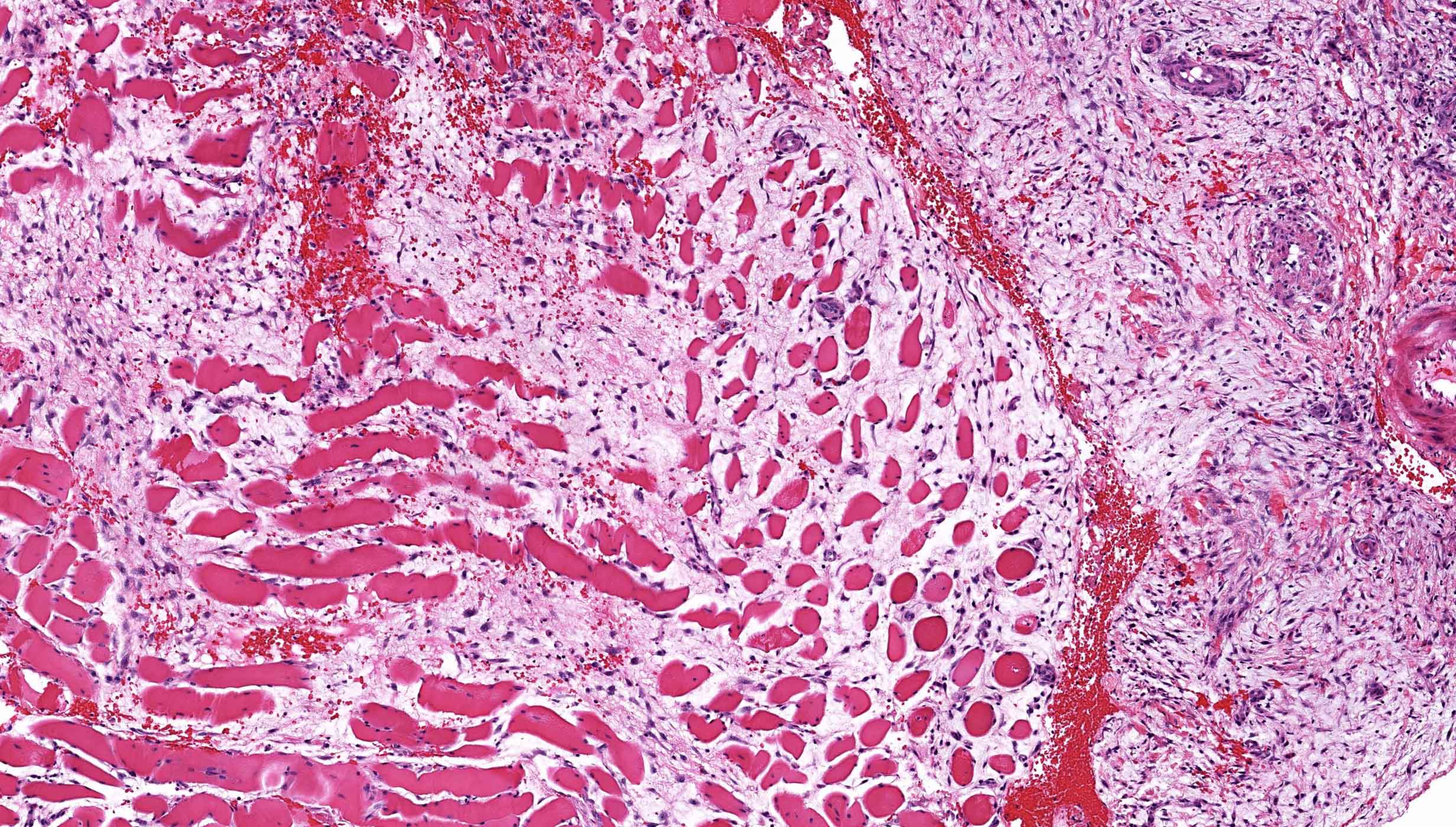
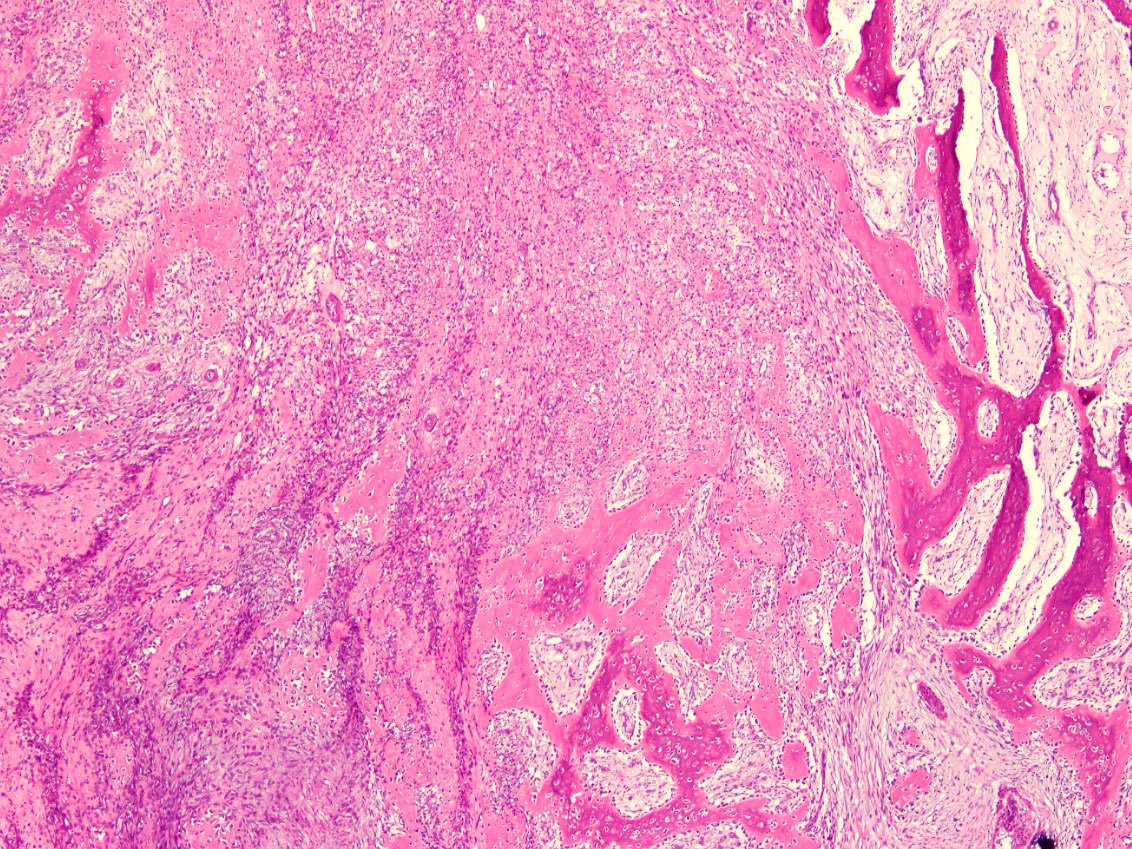
- Histologically, zonal pattern is characteristic with different degrees of cellular differentiation (inner zone, intermediate zone and peripheral zone)
- Inner central zone:
- Composed of fibroblastic / myofibroblastic proliferation, which is richly vascular, rich in inflammatory cells and resembles nodular fasciitis; some multinucleated giant cells may also be seen
- Cells show mild degree of pleomorphism and brisk mitosis
- Areas of hemorrhage, fibrin, endothelial proliferation and entrapped atrophic muscle fibers are noted
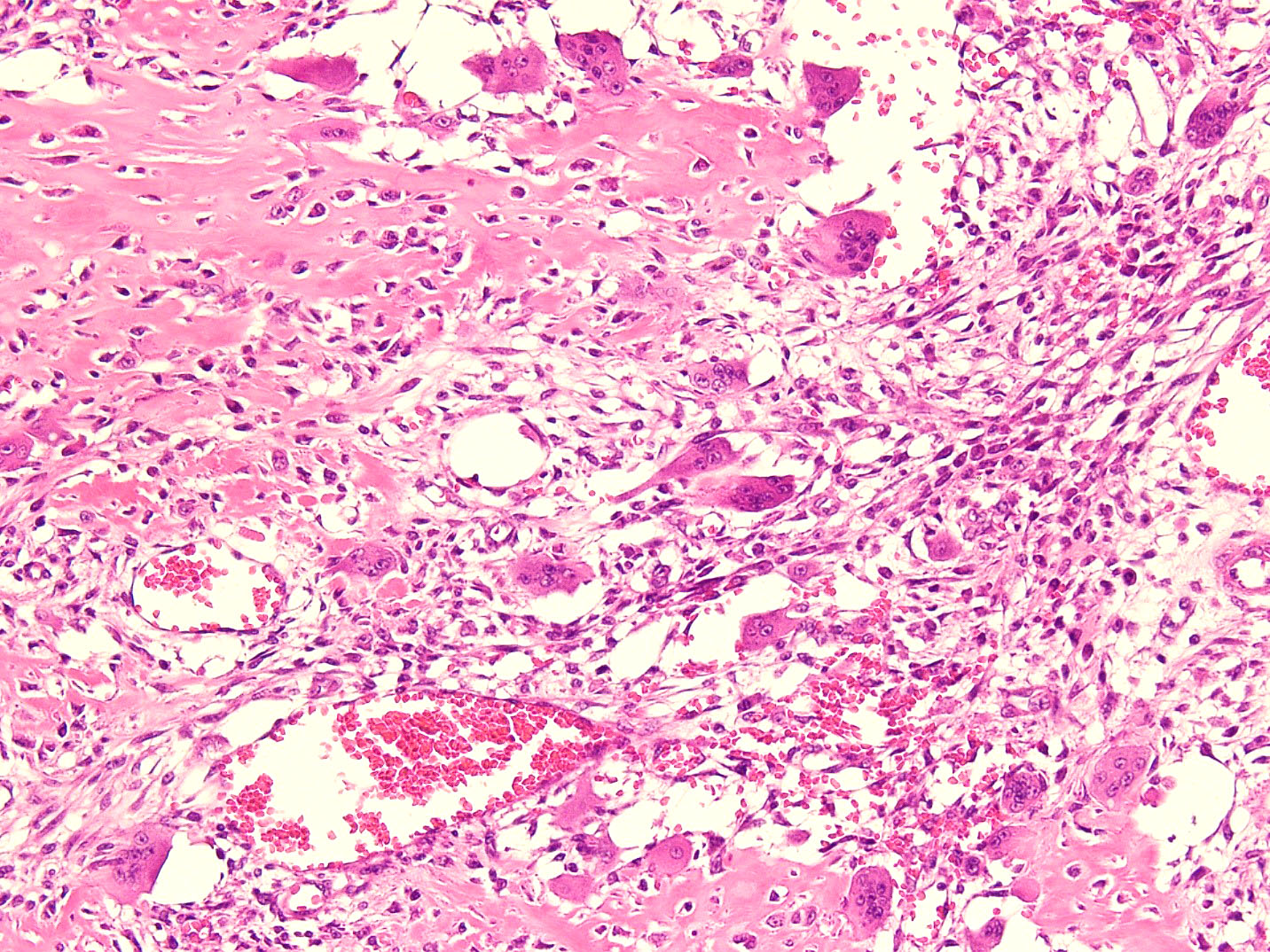
- Intermediate zone:
- There is a mixture of fibroblasts and osteoblasts along with erratic osteoid separated by small sized vessels
- Scattered chondrocytes may be appreciated
- Peripheral zone:
- Osteoid undergoes calcification and leads to lamellar bone formation
- Islands of mature or immature cartilage may be present
- Extreme periphery / margin shows mature bone with osteoblastic rimming and little to no pleomorphism
- Lesion is separated from the normal tissue (muscle) by a zone of loose, myxoid fibrous tissue
- Inner central zone:
- Early stage (0 - 4 weeks):
- Mass shows central zone morphology with only rare foci showing osteoid
- Zonal pattern is not very much appreciated
- Intermediate stage (4 - 8 weeks):
- Zonal pattern is appreciated with central zone, intermediate zone and peripheral zone
- Late, mature stage (> 8 weeks):
- Mass is mostly composed of mature bone
- Very old lesions show only lamellar bone separated by fibrovascular stroma, mimicking osteoma
- References: Curr Sports Med Rep 2018;17:290, Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2019, Exp Ther Med 2021;21:531, Mol Clin Oncol 2018;8:749, Autops Case Rep 2021;11:e2021316
Microscopic (histologic) images
Cytology description
- Cytological findings reflect different stages and zones that have been aspirated
- Spindle cells with uniform, smooth bordered oval nuclei with inconspicuous nucleoli and elongated cytoplasm (Diagn Cytopathol 2008;36:50)
- Osteoclast-like giant cells may be seen (Kor J Cytopathol 1998;9:123, Diagn Cytopathol 2008;36:50)
Positive stains
- Not usually required for diagnosis
- Vimentin and SMA highlights the myofibroblasts in the central zone (Exp Ther Med 2021;21:531, Mol Clin Oncol 2018;8:749)
- SATB2 highlights the osteoblasts in the intermediate and peripheral zone
Negative stains
- MDM2 and CDK4 (Mod Pathol 2010;23:1279)
Electron microscopy description
- Fibroblasts and myofibroblasts have dilated rough endoplasmic reticulum and aggregates of cytoplasmic filaments variably associated with dense bodies; osteoblasts have numerous mitochondria and abundant, dilated rough endoplasmic reticulum
Molecular / cytogenetics description
- USP6 gene rearrangements, mostly with COL1A1 (Hum Pathol 2019;88:39)
- Novel partner gene ANGPTL2 also reported (Mod Pathol 2020;33:1492)
Videos
Myositis ossificans (benign mimic of sarcoma) bone / soft tissue pathology & radiology correlation
Sample pathology report
- Thigh mass, excision:
- Myositis ossificans (see comment)
- Comment: The sections from the mass show a circumscribed lesion with characteristic zonal pattern, with inner zone showing tissue culture-like background, against which are seen plump fibroblasts and myofibroblasts. This area is rimmed by immature bone in the middle and mature lamellar bone at the periphery.
Differential diagnosis
- Extraskeletal osteosarcoma:
- Usually occurs in sixth or seventh decade
- No zoning pattern is seen (backward zonation is appreciated; that is, most mature bone in the center with woven bone at the periphery) (Czerniak: Dorfman and Czerniak's Bone Tumors, 2nd Edition, 2015, Clin Case Rep 2019;7:2260)
- There is a mixture of atypical spindle cells with moderate to marked degree of pleomorphism and increased mitoses
- Osteoid is seen directly produced by these atypical cells
- Parosteal osteosarcoma:
- Can cause diagnostic difficulty, especially when myositis ossificans is located near the surface of a major long tubular bone
- Radiology shows central heavy mineralization as opposed to myositis ossificans
- Connection with underlying bone is seen in parosteal osteosarcoma
- Parosteal osteosarcoma shows well developed tumor bone, unlike zonal pattern of myositis ossificans
- Periosteal osteosarcoma:
- Connection with the bone surface is identifiable with periosteal reaction
- Direct tumor bone formation identified
- No zonal pattern
- Fibrodysplasia ossificans progressiva:
- Multifocality and specific hypoplasia of the first metacarpal and metatarsal bones
- Rare genetic disorder that spreads along the muscle planes
- Calcified / ossified synovial sarcoma:
- Can become extensively calcified with secondary bone formation
- Lacks zoning pattern
- Highly hyperchromatic tumor cells express SS18::SSX and TLE1 immunostains
Additional references
Board review style question #1
A 36 year old boxer presented with a painful mass in the right arm for the last 1.5 months. On radiology, an intramuscular mass was seen with peripheral mineralization and central latency. It was biopsied, which showed the morphology in the image above. What is the most likely diagnosis?
- Extraskeletal osteosarcoma
- Myositis ossificans
- Periosteal osteosarcoma
- Synovial sarcoma with bone formation
Board review style answer #1
B. Myositis ossificans. The given history in this case shows that the patient is physically active and provides short duration history of the lesion. The radiological findings suggest a lesion with maturation at periphery. The microscopic image shows characteristic zonation. These are all features of myositis ossificans.
Comment Here
Reference: Myositis ossificans
Comment Here
Reference: Myositis ossificans
Board review style question #2
Biopsy from a thigh mass in a 31 year old man shows a circumscribed lesion rimmed entirely by skeletal muscle and comprised of a haphazard arrangement of spindle cells with mild nuclear pleomorphism, prominent nucleoli and increased mitotic figures. The background is highly fibrovascular and shows extravasated red blood cells, inflammatory cells and myxoid change. At the advancing edge of the lesion, there is focal, mature lamellar bone present. What is the likely diagnosis?
- Extraskeletal osteosarcoma
- Myositis ossificans
- Nodular fasciitis
- Ossified hemangioma
Board review style answer #2
B. Myositis ossificans. The question describes a detailed microscopic description of myositis ossificans. The lesion is not osteosarcoma because it is circumscribed and shows zonation in the form of mature periphery and immature center. This is contrary to osteosarcoma. Nodular fasciitis does not show heterotopic ossification and zonal pattern, although the center of myositis ossificans is reminiscent of nodular fasciitis.
Comment Here
Reference: Myositis ossificans
Comment Here
Reference: Myositis ossificans