Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alexiev BA. Myopericytoma / myofibroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuemyopericytoma.html. Accessed March 27th, 2025.
Definition / general
- Myopericytoma is a distinctive perivascular myoid neoplasm that forms a morphological spectrum with myofibroma
Essential features
- Myopericytoma: bland, myoid spindled cells growing in a concentric pattern around numerous small blood vessels
- Myofibroma: biphasic growth pattern, with primitive cellular zones often showing mitotic activity, necrosis and calcification, surrounded by hyalinized nodules of myoid spindled cells
- PDGFRB mutations in myopericytoma and myofibroma
- SRF-RELA gene fusions in cellular myofibroma / myopericytoma
Terminology
- Not recommended: infantile hemangiopericytoma
ICD coding
- ICD-O: 8824/0 - myopericytoma
- ICD-11: 2E84.Y & XH0953 - benign fibrogenic or myofibrogenic tumor of other specified sites & myofibroma
Epidemiology
- Myopericytoma may occur at any age; most cases are seen in adults
- Myofibroma may be present at birth, appear in the first 2 years of life or arise in adults, with male predominance (Am J Surg Pathol 2006;30:104)
Sites
- Myopericytoma and myofibroma predominantly arise in the skin and subcutis of the extremities, head and neck and trunk (Histopathology 1993;22:335, Head Neck 2007;29:605)
- Rarely, these neoplasms arise in visceral locations and intracranial sites (Hum Pathol 2010;41:1500, Neuropathol Appl Neurobiol 2005;31:641)
- Infants with myofibromatosis may have involvement of visceral locations, including liver, heart, gastrointestinal tract, bone and brain (Cancer 1981;48:1807)
Pathophysiology
- Mutations in the PDGFRB gene appear to represent a common pathogenesis for myopericytoma and myofibroma (Am J Surg Pathol 2017;41:1034, Am J Surg Pathol 2017;41:195) (see Molecular / cytogenetics description)
- Cellular myofibromas / myopericytomas are associated with SRF-RELA gene fusions (Am J Surg Pathol 2017;41:677)
Etiology
- Association between myopericytoma and EBV has been reported in patients with AIDS (Am J Surg Pathol 2009;33:1666)
- A subset of solitary or multiple forms of infantile myofibromatosis are familial, following an autosomal dominant mode of inheritance (J Am Acad Dermatol 2003;49:S148, Am J Med Genet A 2004;126A:261)
- Some reports have suggested an autosomal recessive inheritance (Clin Genet 2001;59:134)
Clinical features
- Myopericytoma and myofibroma usually present as a painless, slow growing mass, which can be present for years
- Most cases arise as a solitary lesion but multiple lesions (myopericytomatosis / myofibromatosis) involving a particular anatomical region or different regions are sometimes seen (Am J Surg Pathol 1998;22:513, Am J Surg Pathol 2006;30:104, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e59)
- Myofibromatosis affects almost exclusively infants and young children; 88% of cases occur before the age of 2 years (Cancer 1981;48:1807)
- Solitary infantile myofibromatosis is more common in males (Cancer 1981;48:1807)
- Multicentric infantile myobromatosis is more common in females (Cancer 1981;48:1807)
Diagnosis
- Tissue sampling is the gold standard for a definitive diagnosis
Radiology description
- At magnetic resonance imaging, tumors are most commonly superficial, may be well defined (myopericytoma) or ill defined (myopericytomatosis) and demonstrate highly vascularized, avidly enhancing soft tissue, often with areas of internal hemorrhage (Radiol Case Rep 2017;13:275)
Prognostic factors
- Most myopericytomas and myofibromas do not recur
- Small subset of myofibromas / myopericytomas shows atypical features (diffuse hypercellularity, infiltrative growth pattern and increased mitotic figures) that do not adversely affect outcome (Am J Surg Pathol 2014;38:1649)
- Malignant myopericytomas are associated with aggressive clinical behavior (Histopathology 2002;41:450)
- Multicentric myofibroma (referred to as infantile myofibromatosis) is a life threatening disease (JAMA Dermatol 2019;155:946)
Case reports
- 18 year old woman with a mass involving the external auditory canal and tragus (J Laryngol Otol 2013;127:805)
- 26 year old man with multiple pulmonary nodules (Intern Med 2012;51:639)
- 33 year old man with painless swelling and erythema of the pulp of his left index finger (J Hand Microsurg 2017;9:32)
- 48 year old woman with a mass next to the inner corner of her left eye (Dermatol Online J 2018;24:13030)
- 58 year old man with a mass of the hypothenar eminence (Hand (N Y) 2015;10:349)
- 64 year old woman with a mass at the craniocervical junction (Neurosurgery 2019;85:E360)
- 71 year old man with a subcutaneous mass on the right dorsal foot (Eur J Dermatol 2020;30:736)
Treatment
- Surgery is the first choice of treatment and results in good clinical outcomes (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:393)
- Identification of PDGFRB alterations suggests tyrosine kinase inhibition as a potential therapeutic strategy in myopericytic neoplasms, if needed (Am J Surg Pathol 2017;41:1034)
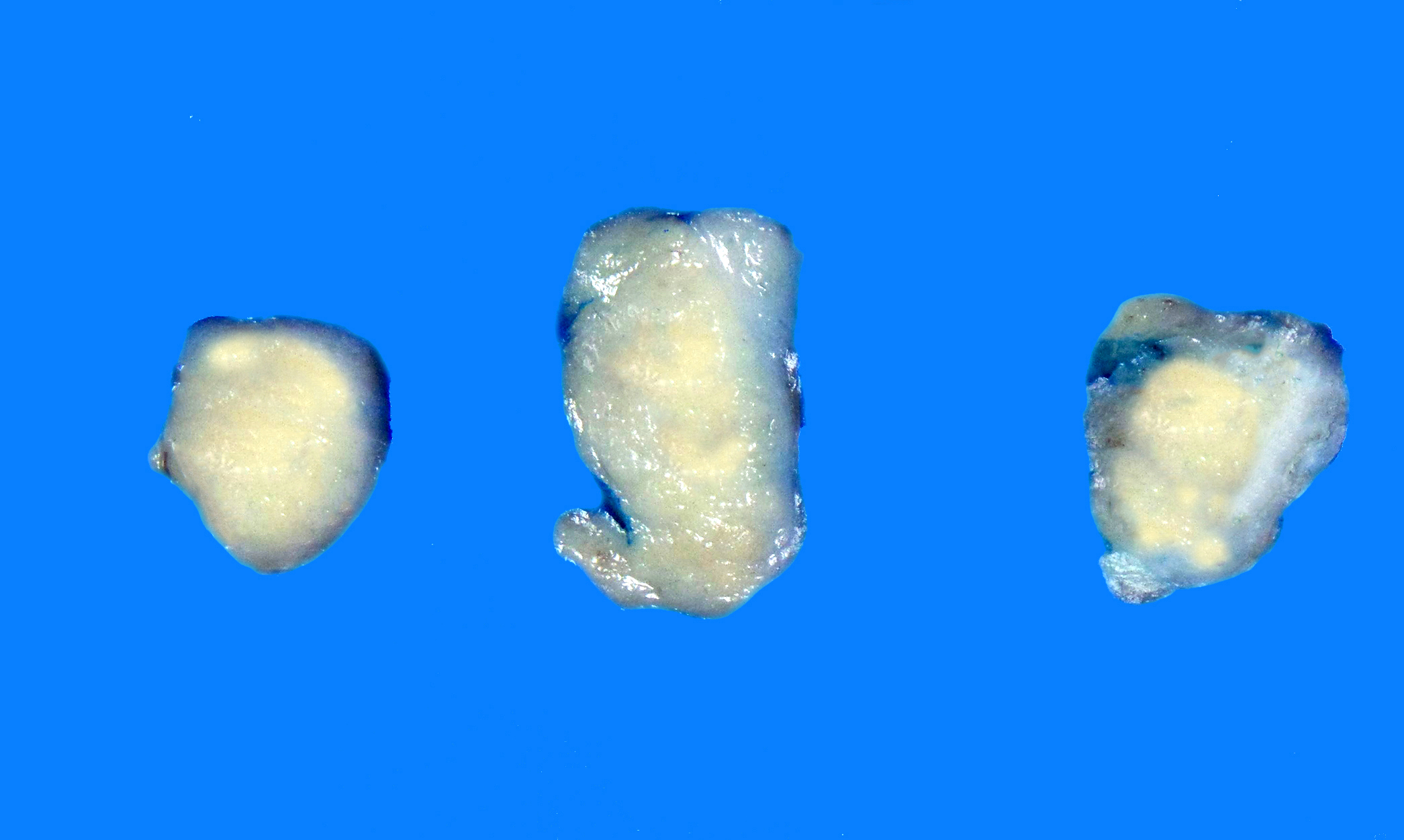
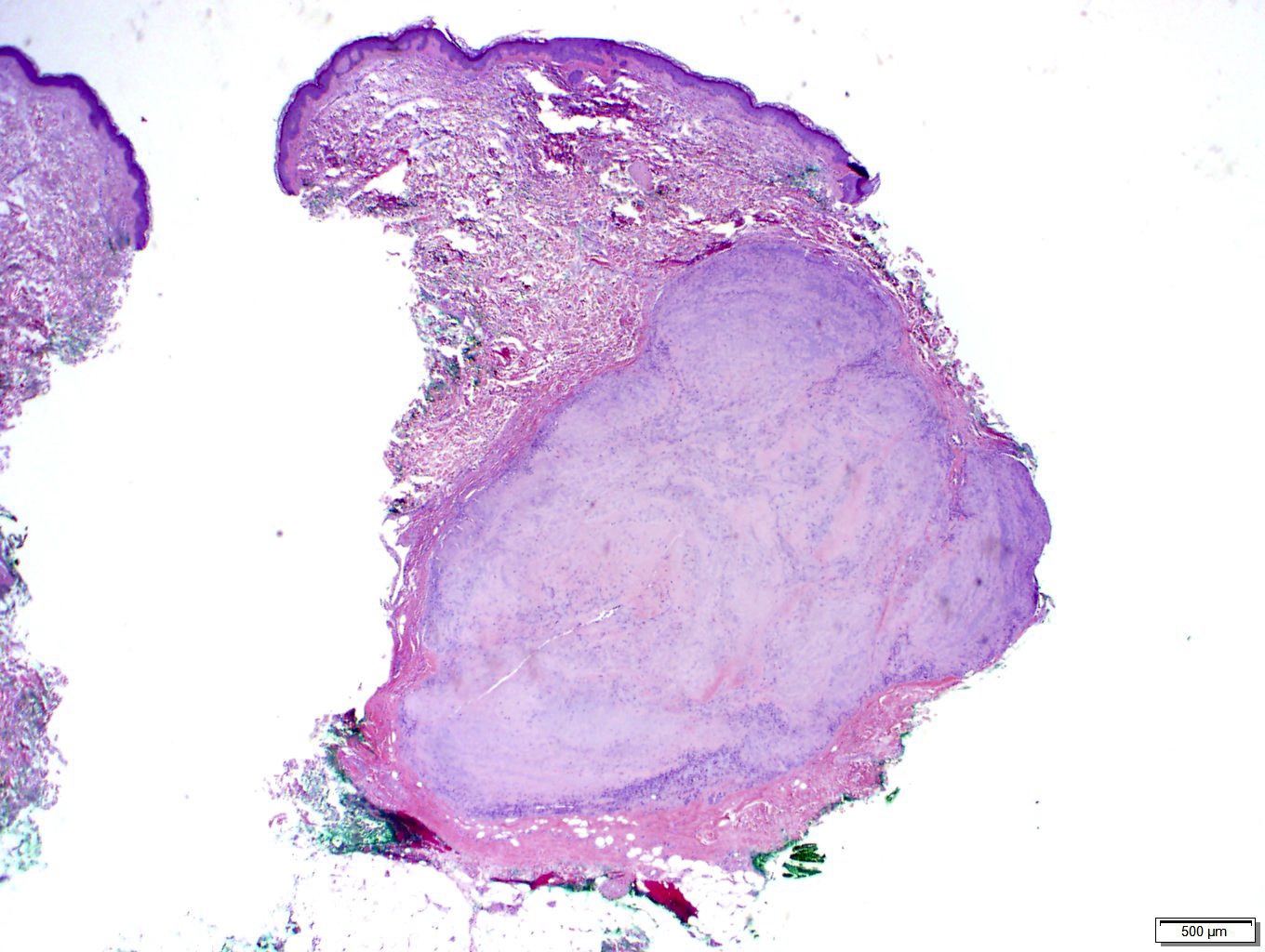
Gross description
- In superficial locations, myopericytoma tends to be well circumscribed, with nodules measuring < 2 cm
- Larger neoplasms may be seen in deep soft tissue (Am J Surg Pathol 2006;30:104)
- Tan-white, firm cut surface
Frozen section description
- Concentric, perivascular growth of plump spindled, myoid cells
Microscopic (histologic) description
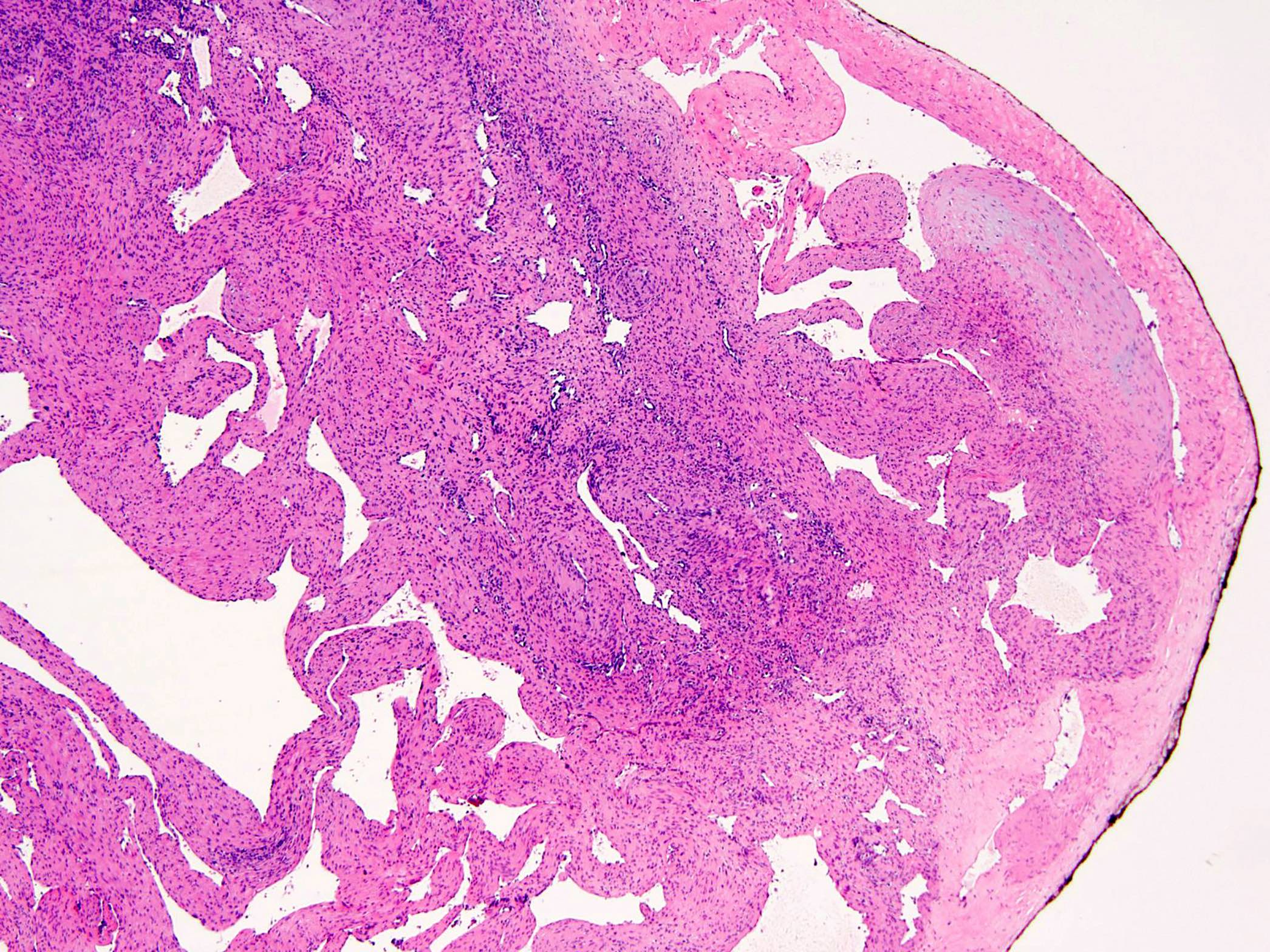
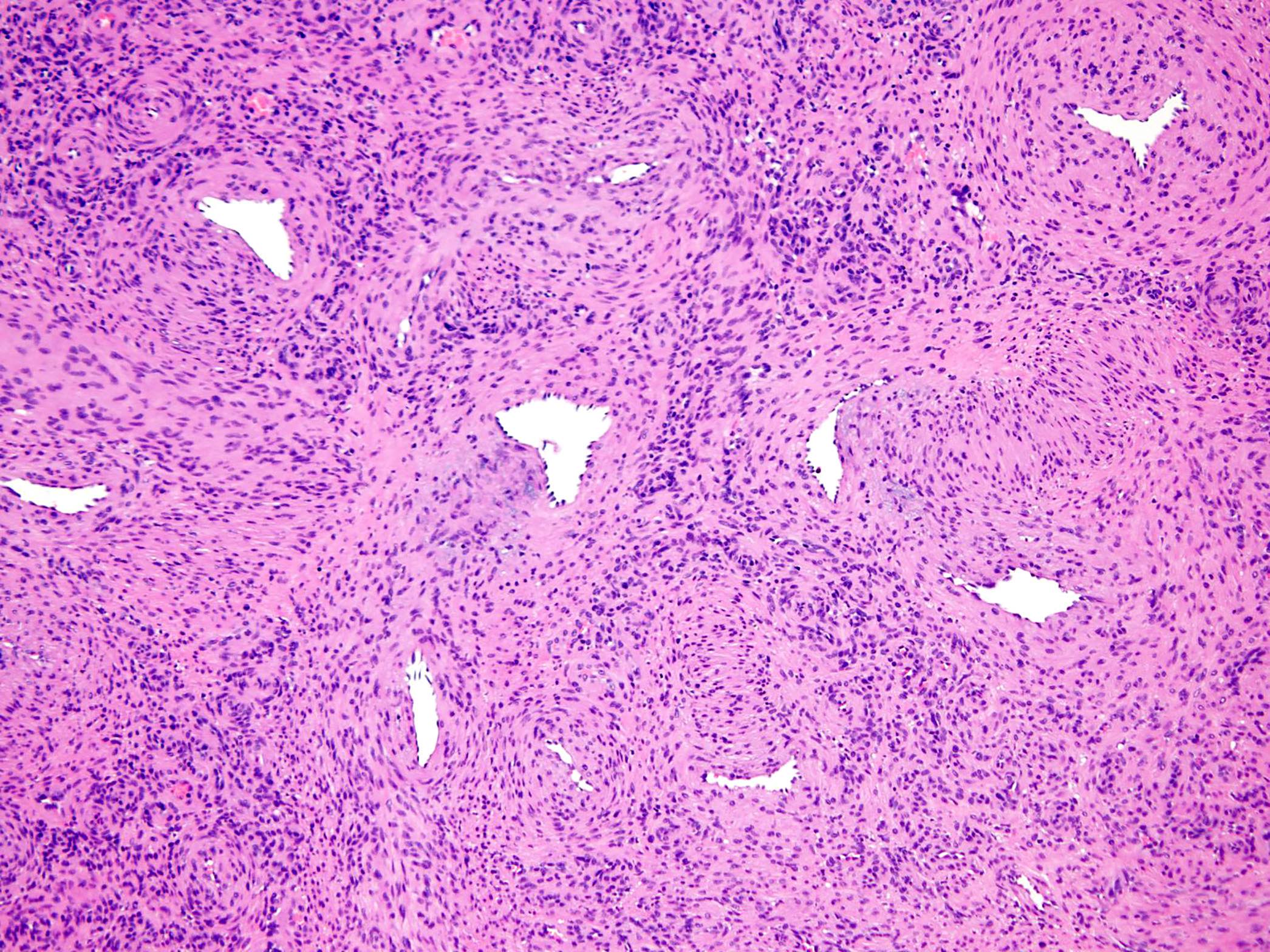
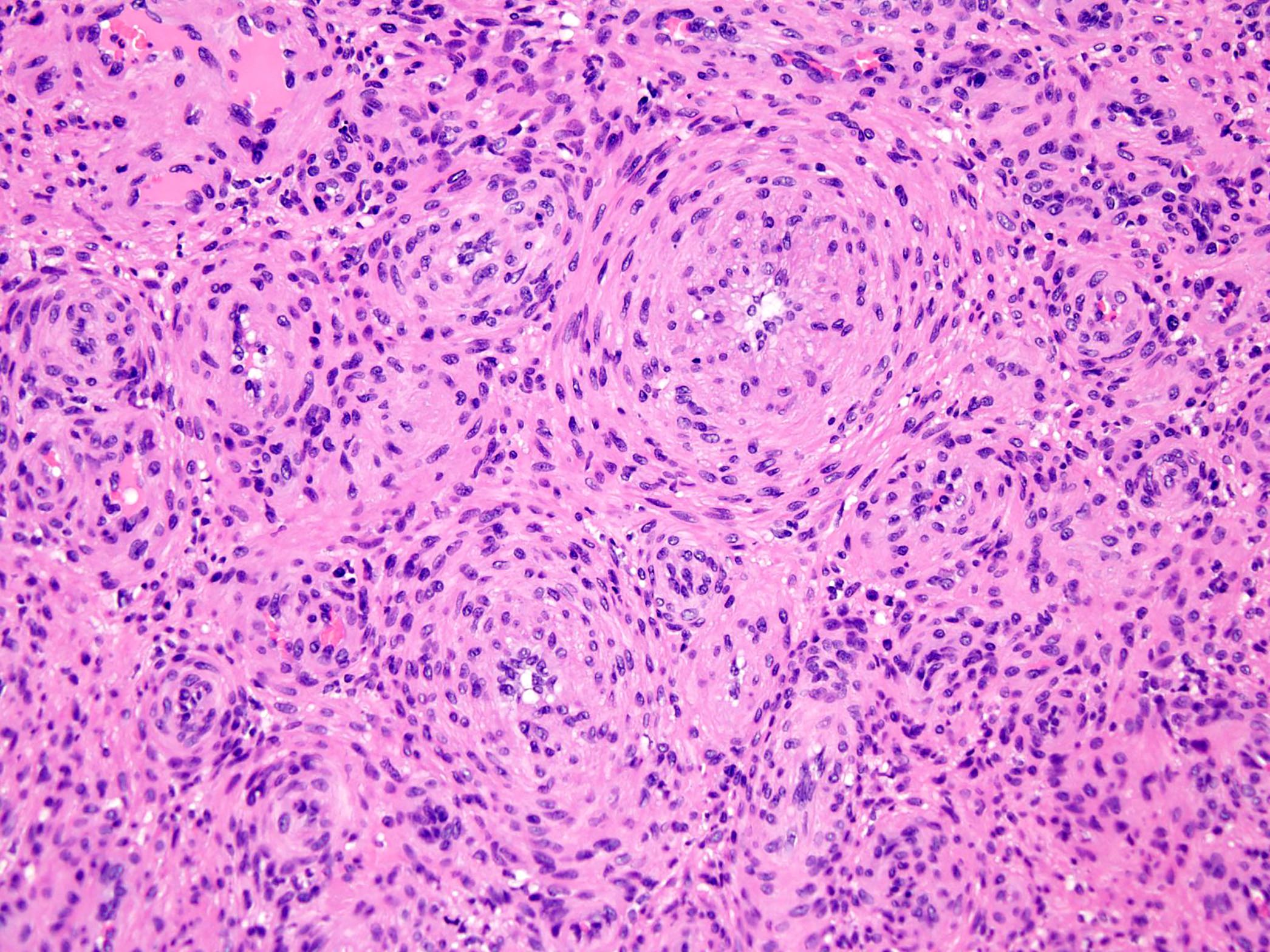
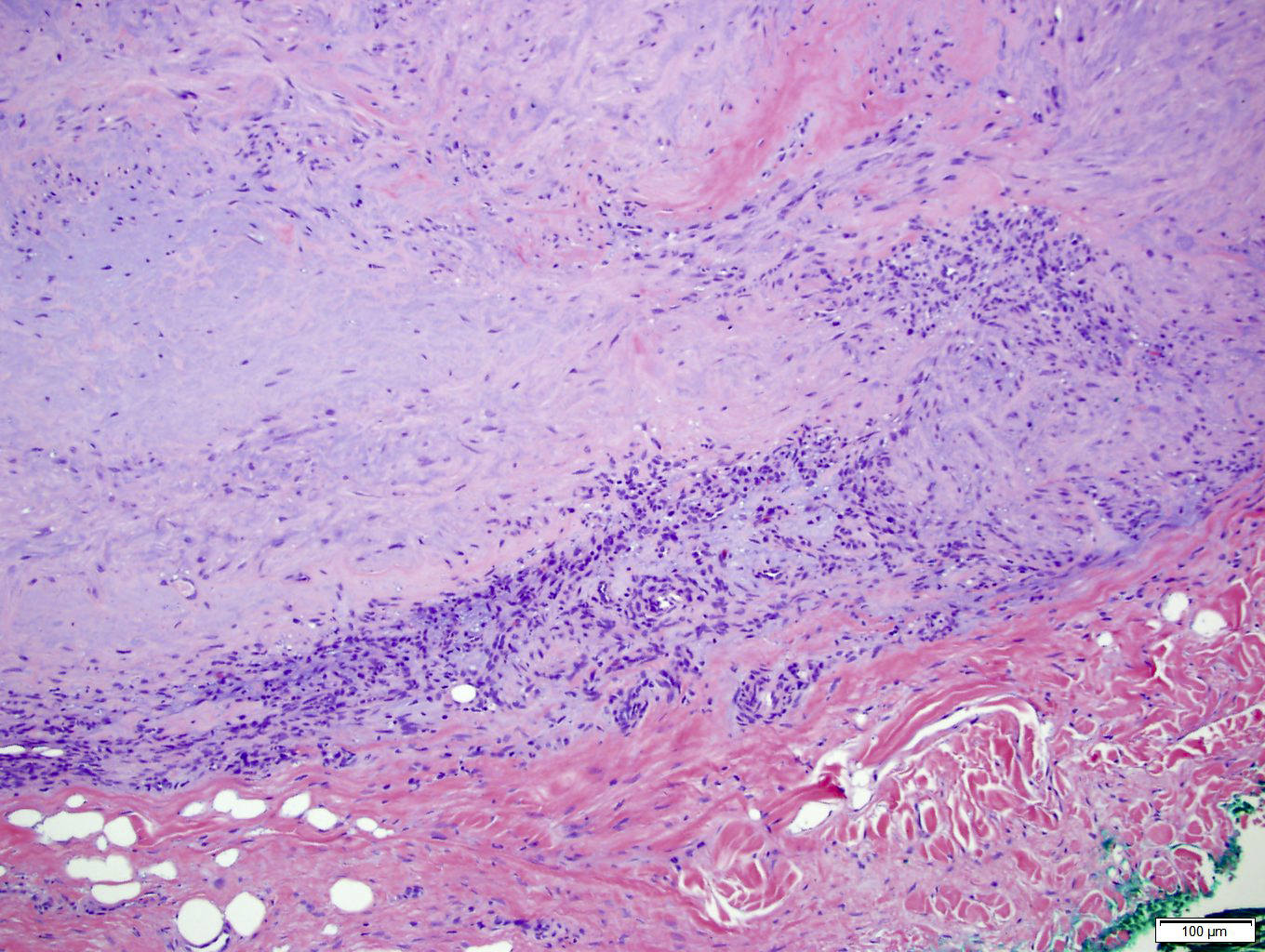
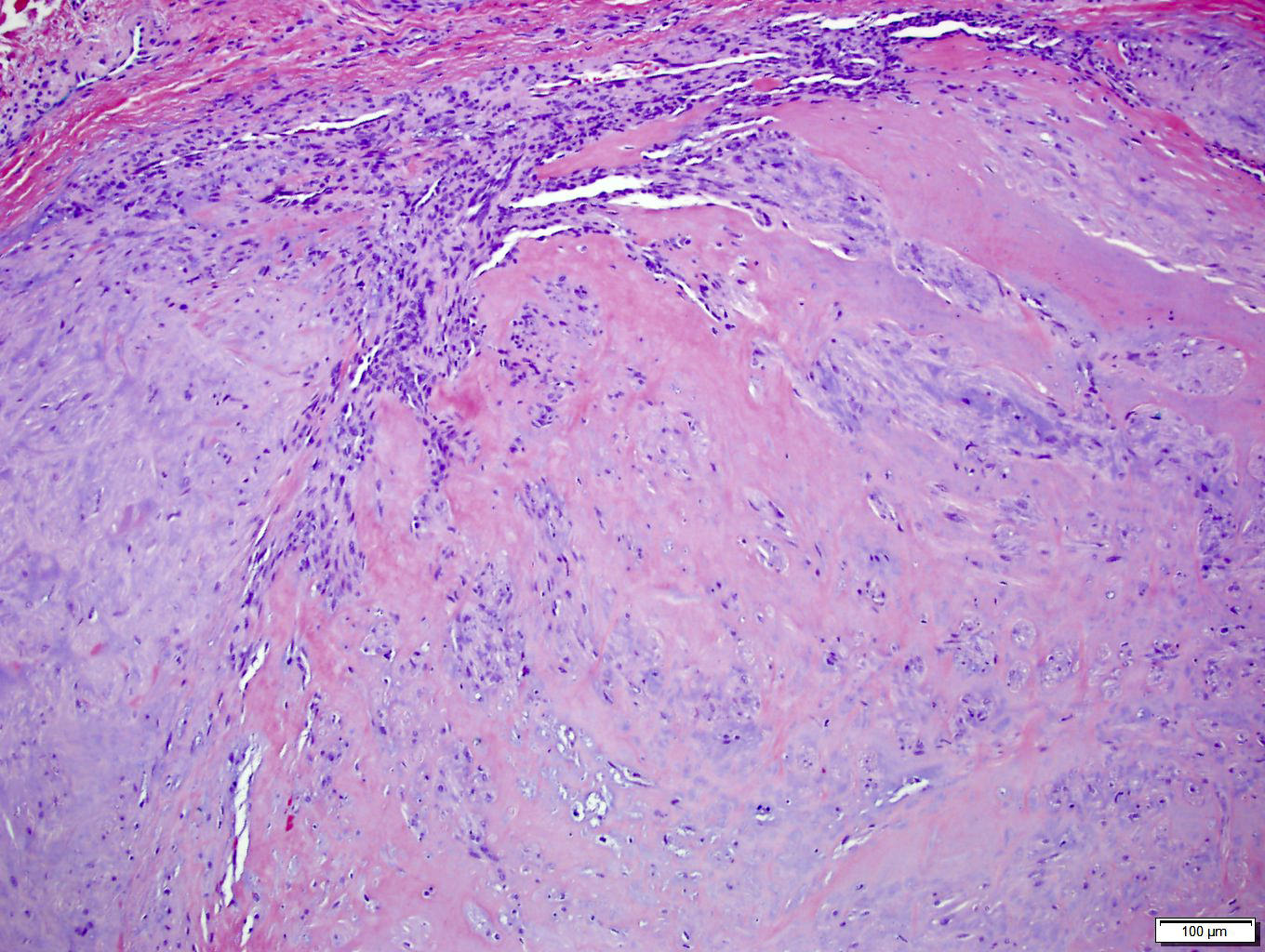
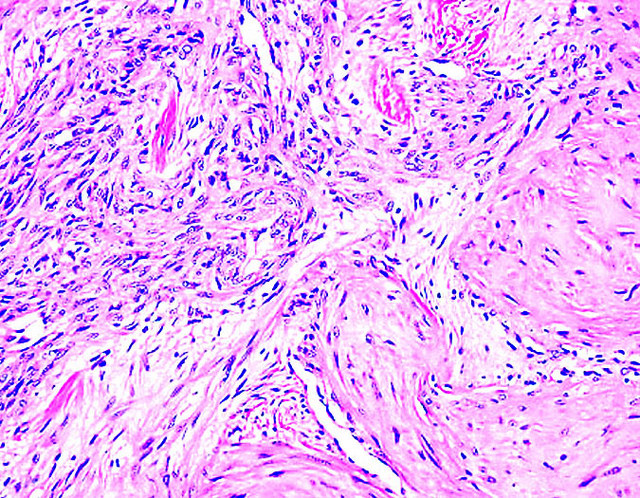
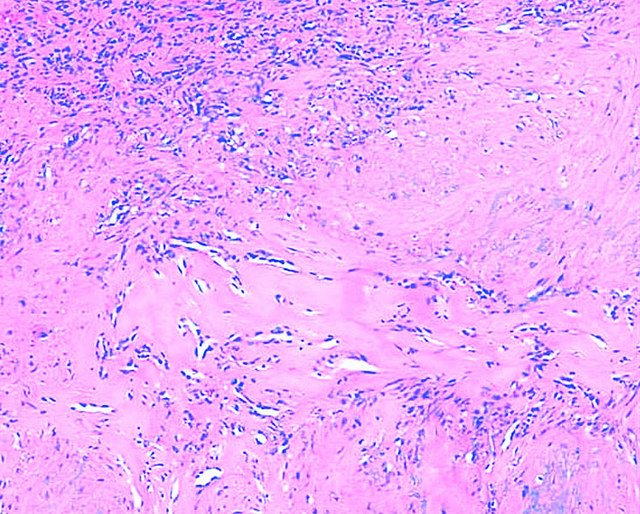
- Myopericytoma
- Well circumscribed, nodular or lobular lesions
- Bland, oval to spindle shaped, myoid cells
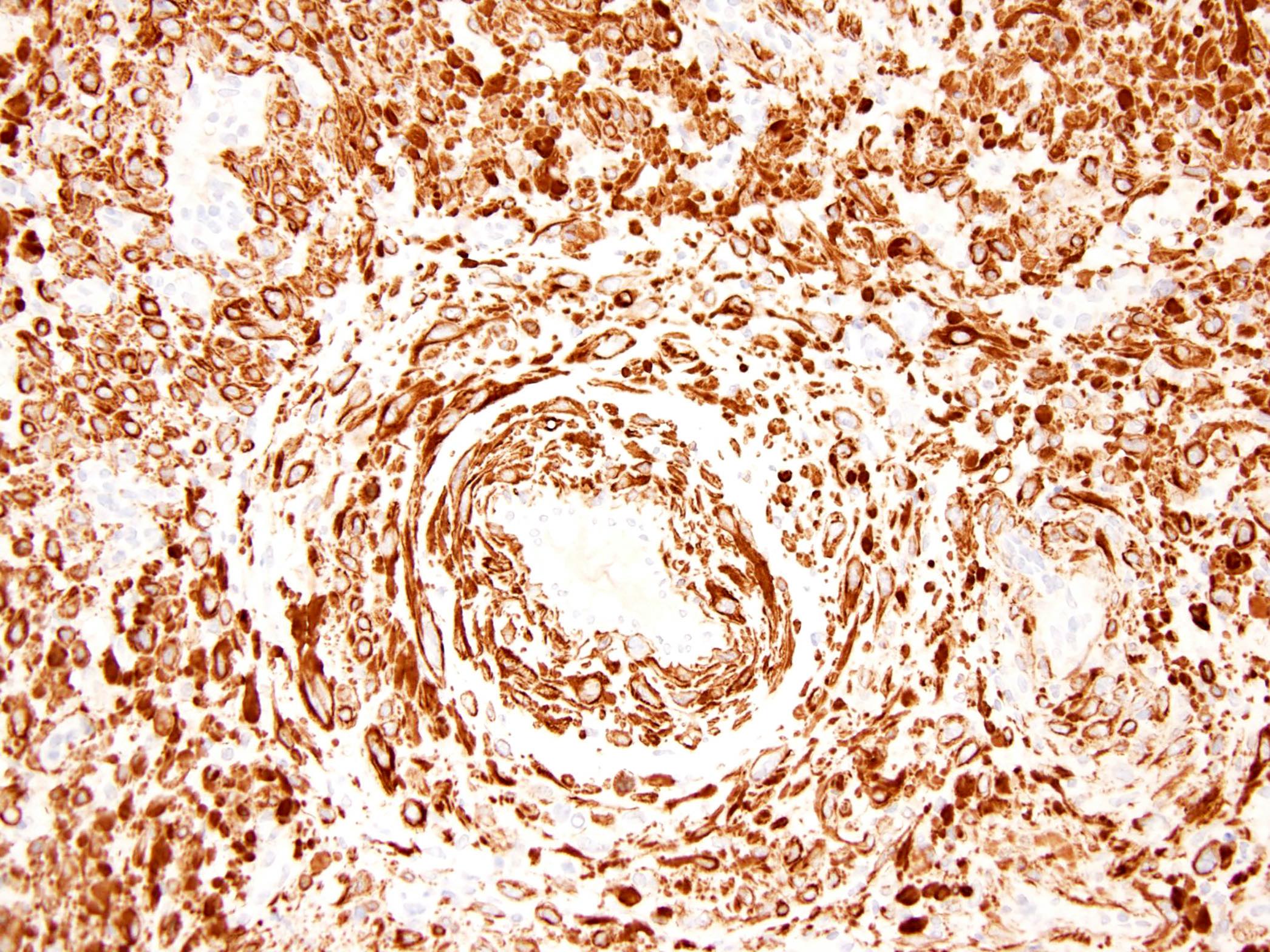
- Characteristic multilayered, concentric growth around numerous small vessels
- Variable cellularity, ranging from cellular and solid appearing to hypocellular and collagenous / myxoid (Am J Surg Pathol 2006;30:104)
- Numerous blood vessels and variable in size; branching, hemangiopericytoma-like blood vessels may be present
- In some cases, a more prominent fascicular arrangement of neoplastic cells is present
- Some myopericytomas may show degenerative changes (symplastic nuclear atypia, stromal hyalinization and cystic change)
- Myopericytomatosis is a rare, diffuse benign variant of myopericytoma that typically involves superficial soft tissue in adults with innumerable microscopic myopericytomatous nodules (Am J Surg Pathol 2017;41:1034)
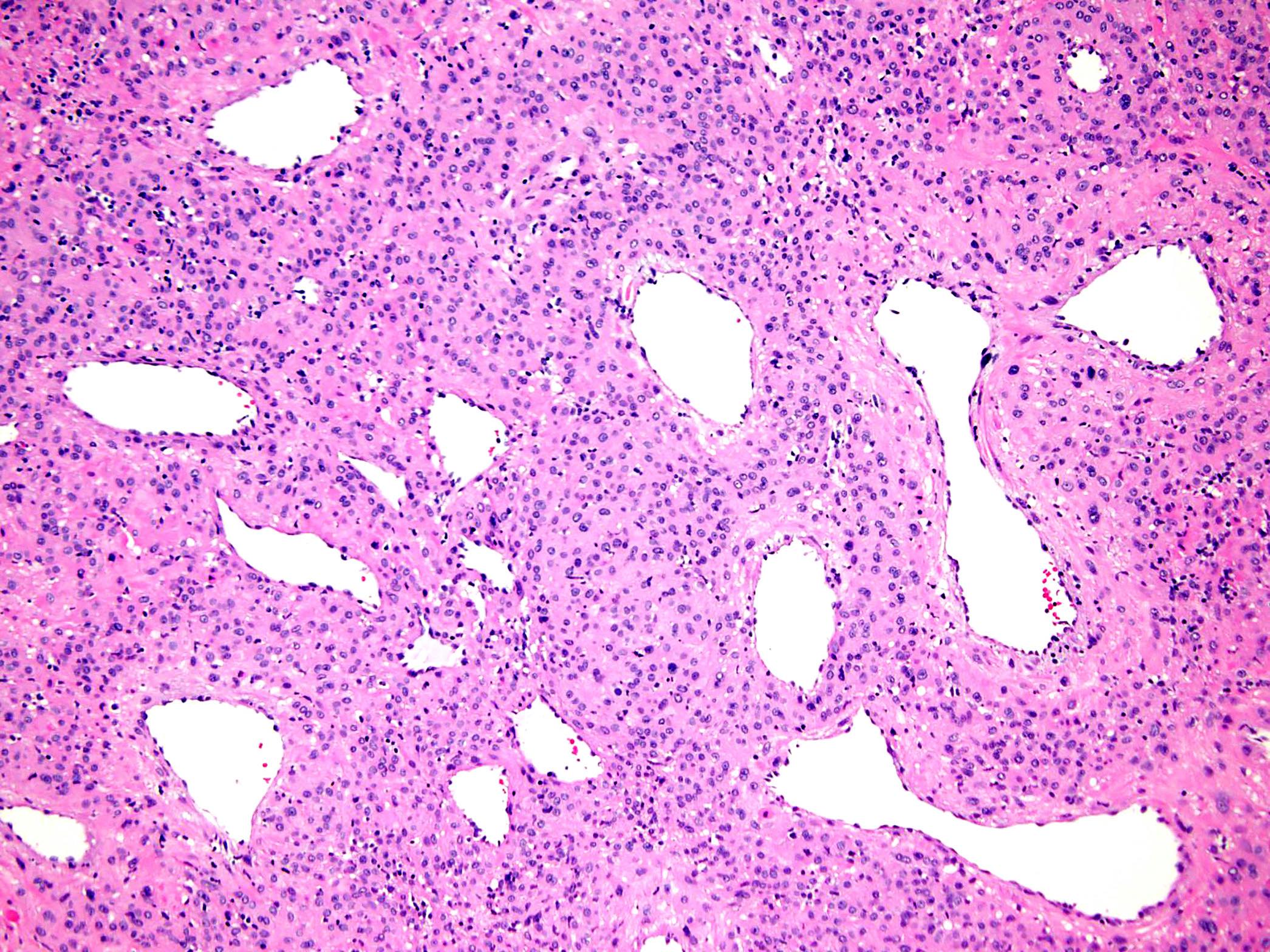
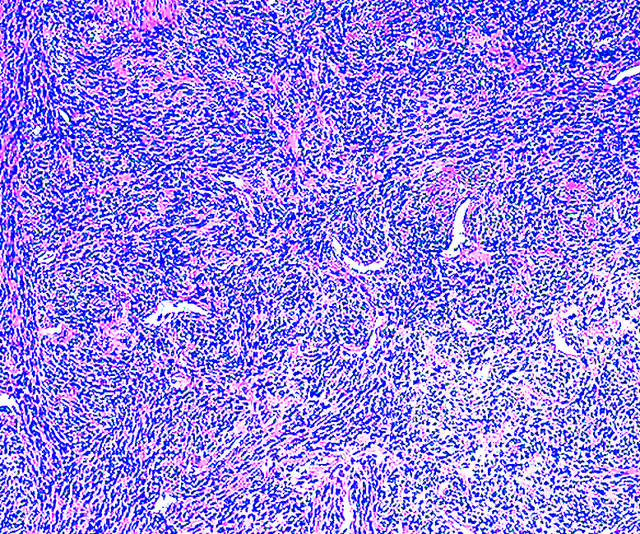
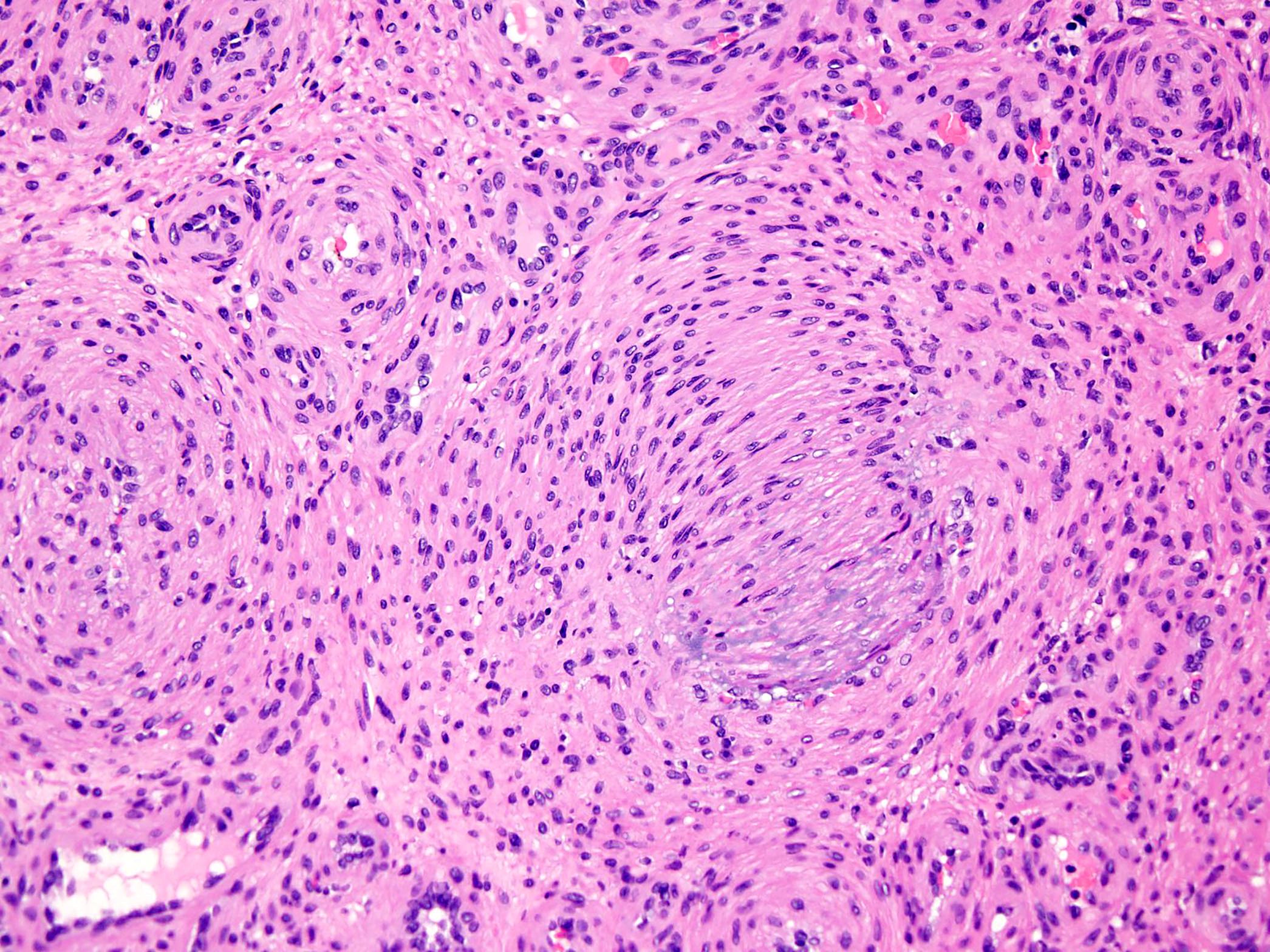
- Myofibroma
- Well circumscribed, nodular neoplasms characterized by a distinctive biphasic growth pattern (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:57)
- Center of the lesion is composed of immature appearing, plump, spindled tumor cells associated with hemangiopericytoma-like branching blood vessels
- Periphery of the lesion consists of nodules and fascicles of variably hyalinized, myoid appearing cells
- Pattern of zonation may be more haphazard or even reversed (Histopathology 1993;22:335)
- Mitotic figures are variable in number
- Cellular zones may undergo necrosis and calcification
- In infants, myofibromas may be composed almost entirely of primitive, cellular zones; such cases were historically labeled infantile hemangiopericytoma (Am J Surg Pathol 1994;18:922)
- Morphological features of the cellular zones of myofibroma share some features with myopericytoma, suggesting that these are related entities
- Myofibromatosis is defined by the presence of multiple myofibromas
- Myofibroma / myopericytoma with cellular / atypical features
- Solid or focally infiltrative growth
- Increased cellularity (Am J Surg Pathol 2017;41:677)
- Increased mitotic activity (> 10 mitotic figures/10 high power fields)
- Areas of infarction type necrosis (Am J Surg Pathol 2017;41:677)
- No pleomorphism
- No tumor necrosis
- Malignant myopericytoma
- Highly mitotic myoid appearing ovoid to spindle cells
- Marked nuclear atypia / pleomorphism
- Tumor necrosis
- At least focally striking perivascular orientation resembling that seen in benign myopericytoma (Histopathology 2002;41:450)
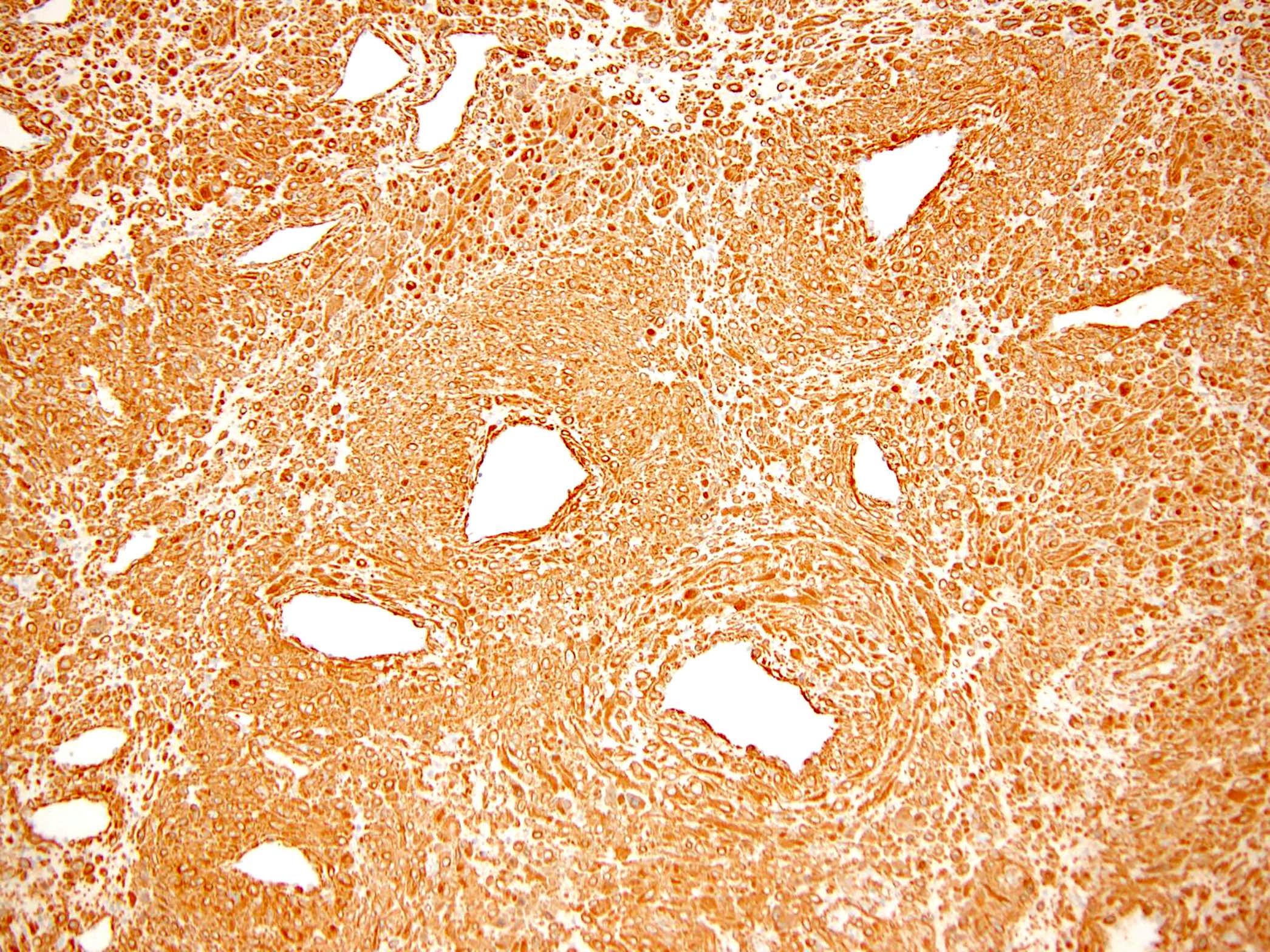
Microscopic (histologic) images
Contributed by Borislav A. Alexiev, M.D., Hillary Rose Elwood, M.D. and Mark R. Wick, M.D.
Positive stains
Negative stains
Molecular / cytogenetics description
- PDGFRB alterations in:
- Sporadic infantile / solitary adult myofibromas (Am J Surg Pathol 2017;41:195)
- Sporadic infantile myofibromatosis (Hum Mol Genet 2017;26:1801)
- Myopericytomatosis and conventional myopericytoma (Am J Surg Pathol 2017;41:1034)
- PDGFRB mutation N666K is noted in myopericytomatosis but not in conventional myopericytoma (Am J Surg Pathol 2017;41:1034)
- Recurrent SRF-RELA gene fusions in cellular myofibroma / myopericytoma (Am J Surg Pathol 2017;41:677)
Sample pathology report
- Right foot mass, excision:
- Myopericytoma (see comment)
- Comment: Histologically, the neoplasm has a well circumscribed margin and is composed of numerous thick walled vessels, with a concentric, perivascular arrangement of ovoid, plump spindled to round myoid tumor cells with an abundant cytoplasm and spindled or round nuclei with evenly distributed chromatin. Areas with hemangiopericytoma type growth pattern, characterized by dilated branching thin walled vessels surrounded by evenly distributed spindled neoplastic cells are also noted. Degenerative stromal changes, such as stromal fibrosis, hyalinization and myxoid change, are seen. Mitotic figures, tumor necrosis and vascular invasion are not identified. Immunohistochemically, the tumor stains positively for SMA and h-caldesmon, while all of the following are negative: S100, desmin, keratin AE1 / AE3 and HMB45. The morphological features and immunohistochemical profile support the above diagnosis.
- Myopericytoma is a benign tumor that rarely recurs following marginal or even intralesional excision. Simple surgical excision is adequate treatment.
Differential diagnosis
- Glomus tumor:
- Prominent perivascular proliferation of small, uniform round cells with round to oval nuclei arranged in multicellular layers around blood vessels (Int J Surg Pathol 2015;23:181)
- Coexpression of alpha smooth muscle actin and CD34 (J Cutan Pathol 2002;29:421)
- Half of the glomus tumors show NOTCH gene fusions and a smaller subset BRAF V600E mutations (Am J Surg Pathol 2020;44:1556)
- Angioleiomyoma:
- Well differentiated smooth muscle proliferations associated with variable but usually prominent vascular component (Head Neck Pathol 2015;9:463)
- Smooth muscle cells arranged in intersecting bundles and whorls encasing or surrounding numerous vascular channels
- Smooth musculature of the vessel walls merge gradually and imperceptibly with the surrounding smooth muscle bundles
- Variable amounts of mature fat may be observed (Head Neck Pathol 2015;9:463)
- Desmin is diffusely positive in angioleiomyomas, whereas most of the myopericytomas are negative (Hum Pathol 2007;38:645)
- PEComa:
- Distinctive epithelioid or spindle cells typically arranged around blood vessels and appear to form the vessel wall, often infiltrating the smooth muscle of small to medium sized vessels (Ann Diagn Pathol 2015;19:359)
- Expression of both smooth muscle and melanocytic markers:
- PEComas harbor loss of function TSC1 / TSC2 mutations; a small subset were reported to carry TFE3 gene rearrangements (Am J Surg Pathol 2015;39:813)
- Infantile fibrosarcoma:
- Morphologic overlap between infantile myofibromatosis and infantile fibrosarcoma (Pediatr Dev Pathol 2008;11:355)
- No biphasic pattern
- Atypical mitoses common
- Immunohistochemistry shows NTRK3 expression (Am J Clin Pathol 2001;115:348)
- ETV6-NTRK3 gene fusion (Pediatr Dev Pathol 2008;11:355)
Board review style question #1
Which of the following is true about myofibroma / myofibromatosis?
- Multicentric infantile myofibromatosis is more common in males
- Multiple lesions with visceral involvement can affect virtually any internal organ and are associated with a poor prognosis
- Solitary infantile myofibromatosis is more common in females
- Tumor is positive for keratin
- Tumor is positive for NOTCH gene fusions
Board review style answer #1
B. Multiple lesions with visceral involvement can affect virtually any internal organ and are associated with a poor prognosis
Comment Here
Reference: Myopericytoma / myofibroma
Comment Here
Reference: Myopericytoma / myofibroma
Board review style question #2
A 38 year old man presented with a left thigh mass. Hematoxylin eosin stains demonstrate a well circumscribed tumor in the dermis and subcutaneous fat composed of bland, oval to spindle shaped cells with multilayered concentric growth around numerous small thick walled blood vessels. Neither necrosis nor mitotic activity is identified. Immunohistochemical stains for SMA and h-caldesmon are positive in tumor cells, while all of the following are negative: keratin AE1 / AE3, CD34, desmin, HMB45, S100 and STAT6.
Which of the following is most likely the correct diagnosis?
- Leiomyoma
- Myofibroblastoma
- Myopericytoma
- PEComa
- Solitary fibrous tumor
Board review style answer #2