Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Babar A, Anjum S, Ud Din N. Malignant melanotic nerve sheath tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuemmnst.html. Accessed April 2nd, 2025.
Definition / general
- Rare aggressive peripheral nerve sheath tumor uniformly composed of Schwann cells showing melanocytic differentiation, usually arising in association with spinal or visceral autonomic nerves (Adv Anat Pathol 2021;28:44)
- Previously classified as a benign tumor in the 2013 WHO classification; however, 2020 WHO classification includes this entity as malignant melanotic nerve sheath tumor (MMNST) due to its malignant behavior (World J Clin Cases 2022;10:8735, BMJ Case Rep 2022;15:e252107)
- Approximately 50% of cases are associated with Carney complex (Adv Anat Pathol 2021;28:44)
Essential features
- Peripheral nerve sheath tumor neoplasm comprised of Schwann cells showing melanocytic differentiation, commonly in association with spinal or visceral autonomic nerves
- Fascicular to sheet-like proliferation of heavily pigmented, relatively uniform plump spindle cells
- Co-expression of S100 / SOX10 and melanocytic markers (HMB45, MelanA)
- The behavior of MMNST is difficult to predict and metastases can occur in the absence of morphologically malignant features
- Loss of PRKAR1A expression suggests a link to Carney complex (Am J Surg Pathol 2014;38:94)
Terminology
- Preferable: malignant melanotic nerve sheath tumor
- Acceptable: melanotic schwannoma; psammomatous melanotic schwannoma; malignant melanotic Schwannian tumor
ICD coding
- ICD-O: 9540/3 - malignant peripheral nerve sheath tumor
- ICD-11: 2B5E & XH2XP8 - malignant nerve sheath tumor of peripheral nerves or autonomic nervous system, primary site & malignant peripheral nerve sheath tumor
Epidemiology
- Mean age of presentation is 41 years (range: 11 - 84 years) (Am J Surg Pathol 2014;38:94)
- No specific age, gender or geographic location predilection (Arch Pathol Lab Med 2018;142:1517)
- Accounts for < 1% of all nerve sheath tumors
- Approximately 50% of cases are associated with Carney complex (CC) (Am J Surg Pathol 1990;14:206)
Sites
- Predilection for spinal nerve involvement, paraspinal sympathetic chain and gastrointestinal tract (esophagus and stomach) (Arch Pathol Lab Med 2018;142:1517)
- Rare sites include cerebellum, orbit, heart, trachea, bronchus, cervix, bone, soft tissue and skin (Arch Pathol Lab Med 2018;142:1517)
Pathophysiology
- Poorly understood, most tumors are sporadic
- Characterized by a complex karyotype with recurrent monosomy of band 22q, variable whole chromosomal gains and recurrent losses involving chromosomes 1, 21 and 17p
- 50 - 55% of psammomatous MMNST cases are associated with Carney complex, which shows mutation within chromosome 17 (affecting PRKAR1A / 17q24 band) (Nat Genet 2000;26:89, Genes Chromosomes Cancer 2015;54:463)
- Recent cytogenetic studies demonstrated trisomy 6p and ring chromosome 11 in MMNST, suggesting that the tumor may share some genetic aberrations with malignant melanoma; however, it lacks BRAF V600E as in malignant melanoma (Arch Pathol Lab Med 2018;142:1517)
- A missense DDR2 mutation of Q231K has been identified in 1 case report (Case Rep Oncol 2021;14:826)
Etiology
- Sporadic or as part of Carney complex (Am J Dermatopathol 2020;42:46, Arch Pathol Lab Med 2018;142:1517, Am J Surg Pathol 2014;38:94, Nat Genet 2000;26:89, Genes Chromosomes Cancer 2015;54:463)
Clinical features
- Local mass with associated pain and neurologic symptoms, depending on site and rate of growth or incidental
- Tumors associated with nerves (35.5% of patients) include motor and sensory abnormalities
- Pressure symptoms with large tumors
- Cutaneous lesions can manifest features similar to melanomas
- Asymptomatic presentations have been noted in 29% of cases
- Reference: Arch Pathol Lab Med 2018;142:1517
Diagnosis
- Clinical history
- CT scan / MRI remains the investigation of choice
- Fluorodeoxyglucose (FDG) PET / CT one stop examination can detect tumors and determine whether they are malignant based on their glucose metabolism before morphological changes occur (Medicine (Baltimore) 2021;100:e24803)
- Biopsy followed by histopathology
Radiology description
- MRI: signal variability due to distribution and contents of melanin within the tumor and hemorrhage, if present, exhibits hyperintensity on T1WI and hypointensity on T2WI due to paramagnetic effect of melanin (Neuroradiol J 2019;32:335, World J Clin Cases 2022;10:8735, J Belg Soc Radiol 2018;102:15)
- CT scan: an iso / hyperattenuating lesion which may have areas of calcification; underlying bone remodeling and erosion can be observed (Neuroradiol J 2019;32:335, J Belg Soc Radiol 2018;102:15)
- FDG PET / CT has a unique and important value in the differential diagnosis of benign / malignant lesions, in detecting occult metastases, monitoring the treatment response and assessing the prognosis (Medicine (Baltimore) 2021;100:e24803)
Radiology images
Prognostic factors
- In the past, it was thought that most of these lesions had a benign, indolent course (Am J Surg Pathol 1990;14:206)
- More recent reports have shown frequent aggressive behavior, with a local recurrence rate and metastatic risk of 26 - 44% (Histopathology 1999;35:558, Skeletal Radiol 2016;45:29, Am J Surg Pathol 2014;38:94)
- The behavior of MMNST is difficult to predict and metastases can occur in the absence of morphologically malignant features (Am J Surg Pathol 2014;38:94)
- Only a mitotic rate > 2/10 HPF correlates with metastases (Am J Surg Pathol 2014;38:94)
- Recurrence and metastases are observed even 20 years after diagnosis (J Belg Soc Radiol 2018;102:15)
- Average local recurrence in 35% of cases and distant metastases in 42% of cases (BMJ Case Rep 2022;15:e252107)
- Frequent metastasis to lung and pleura; however, mediastinum, diaphragm, pericardium, endocardium, bone, liver and spleen have also been reported (J Belg Soc Radiol 2018;102:15, Arch Pathol Lab Med 2018;142:1517)
Case reports
- 11 year old girl with cystic lesion adjacent to right adrenal gland, mimicking adrenal cyst (Ann Pediatr Surg 2022;18:51)
- 34 year old woman underwent excision of a nodule on the right labia, clinically suspicious for a skin tag (Am J Dermatopathol 2020;42:46)
- 44 year old man with enlarging growth on his chest (J Cutan Pathol 2019;46:93)
- 48 year old man with low back pain, left sciatic pain and slight urination difficulty for last 6 months (NMC Case Rep J 2020;7:107)
- 64 year old woman with a 6 month history of right sided trigeminal paresthesia (J Belg Soc Radiol 2018;102:15)
- 70 year old man with incidentally found large pararenal mass (BMJ Case Rep 2022;15:e252107)
Treatment
- Surgical resection is the treatment of choice (J Belg Soc Radiol 2018;102:15, Ann Pediatr Surg 2022;18:51)
- Adjuvant radiotherapy remains controversial; without histologic signs of malignancy, adjuvant treatment should not be performed and only strict radiologic and clinical follow up is required (J Belg Soc Radiol 2018;102:15)
- Adjuvant radiotherapy can be considered in cases showing histologic criteria for malignancy, incomplete surgical resection, tumor recurrence or metastases (J Belg Soc Radiol 2018;102:15)
- No treatment protocol is available for radiotherapy (J Belg Soc Radiol 2018;102:15)
- Stereotactic spine radiosurgery for spinal tumors (Arch Pathol Lab Med 2018;142:1517)
Gross description
- Most MMNSTs are > 5 cm in diameter (Arch Pathol Lab Med 2018;142:1517)
- Well circumscribed and covered by a thin fibrous membrane and arising in relation to a nerve
- Solid cysts can be found on the surface; cut surface has the consistency of tar and varies from gray to pitch black
- Erosion of the adjacent bone may be seen (Arch Pathol Lab Med 2018;142:1517)
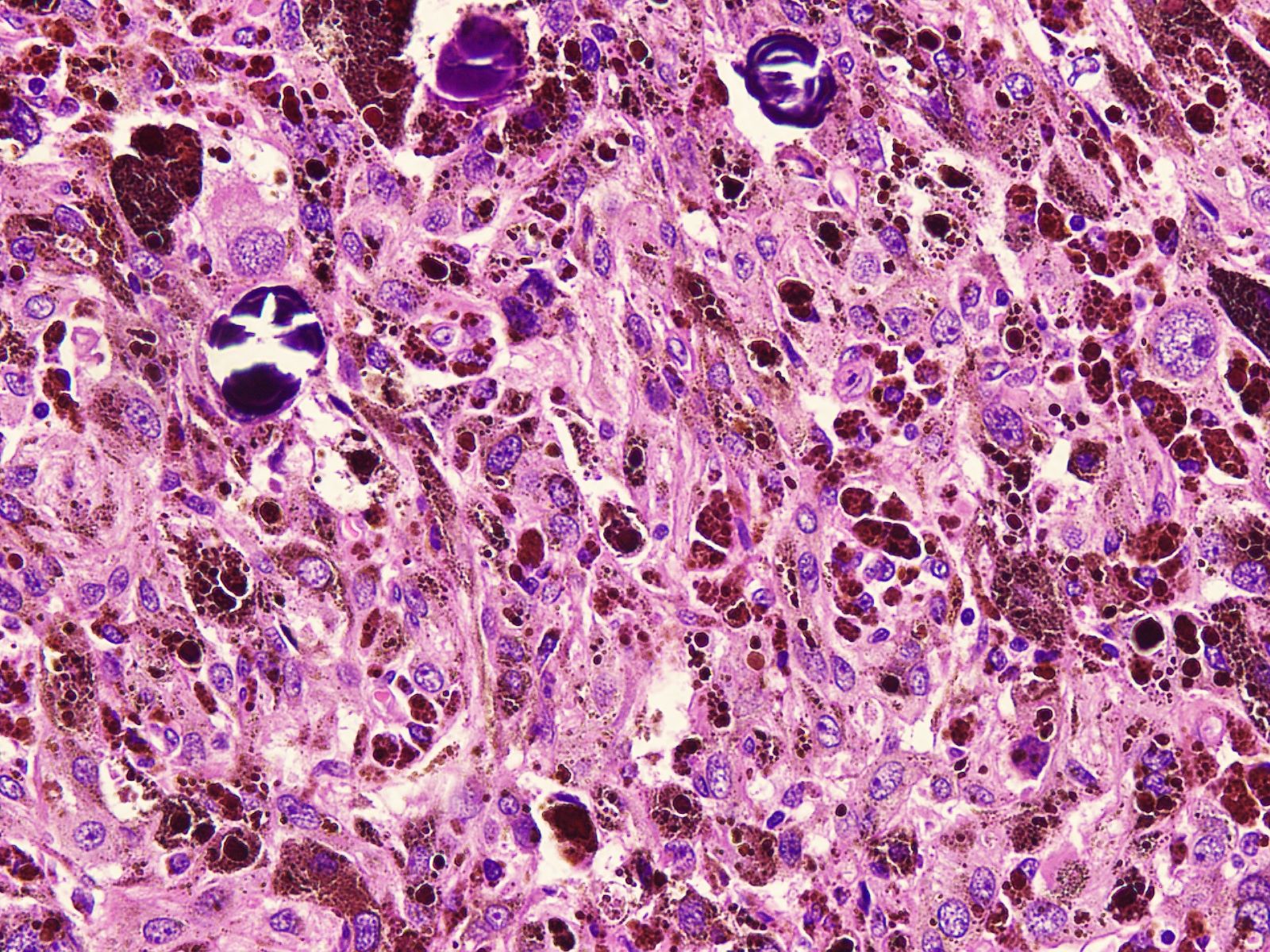
Microscopic (histologic) description
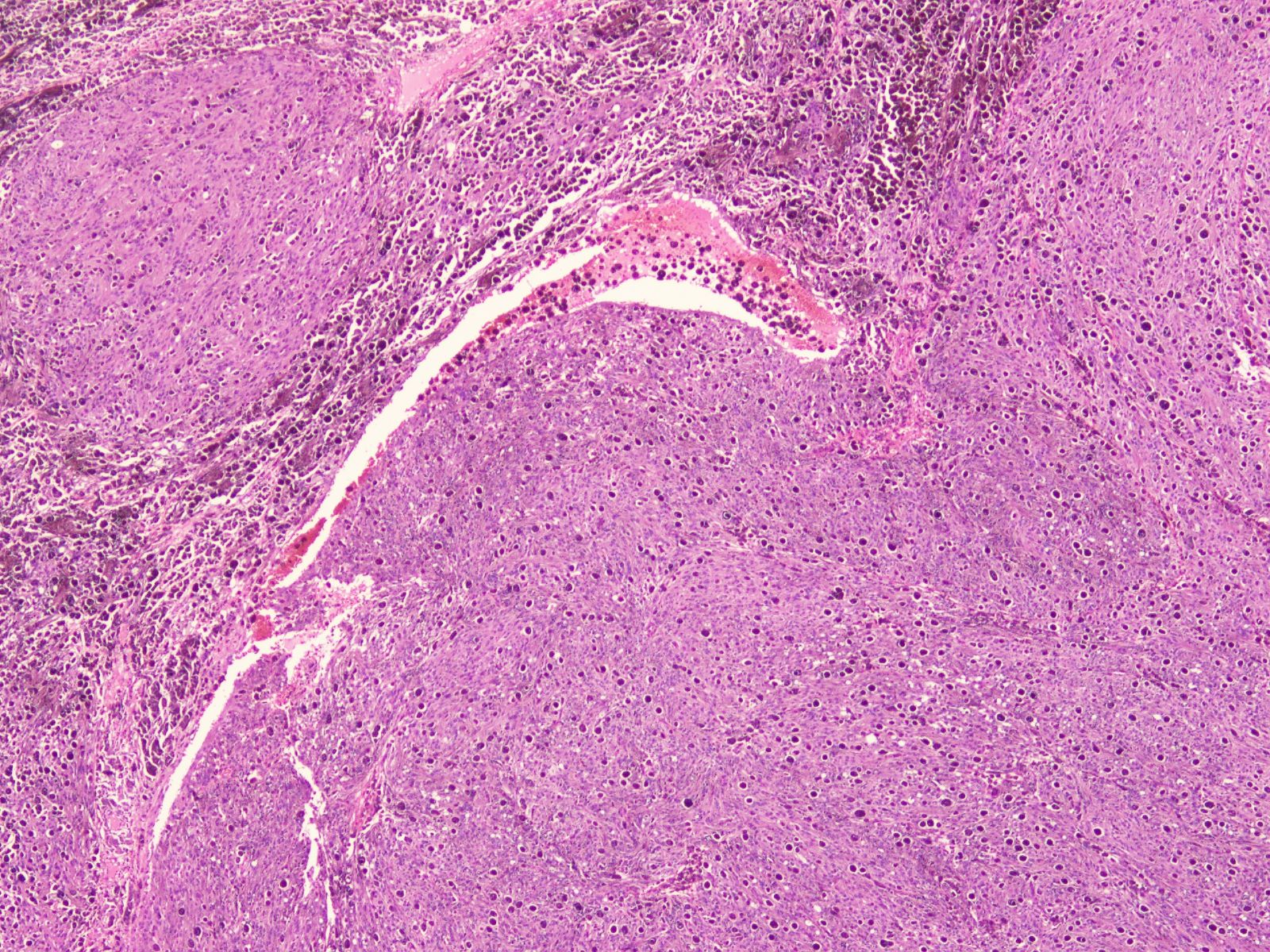
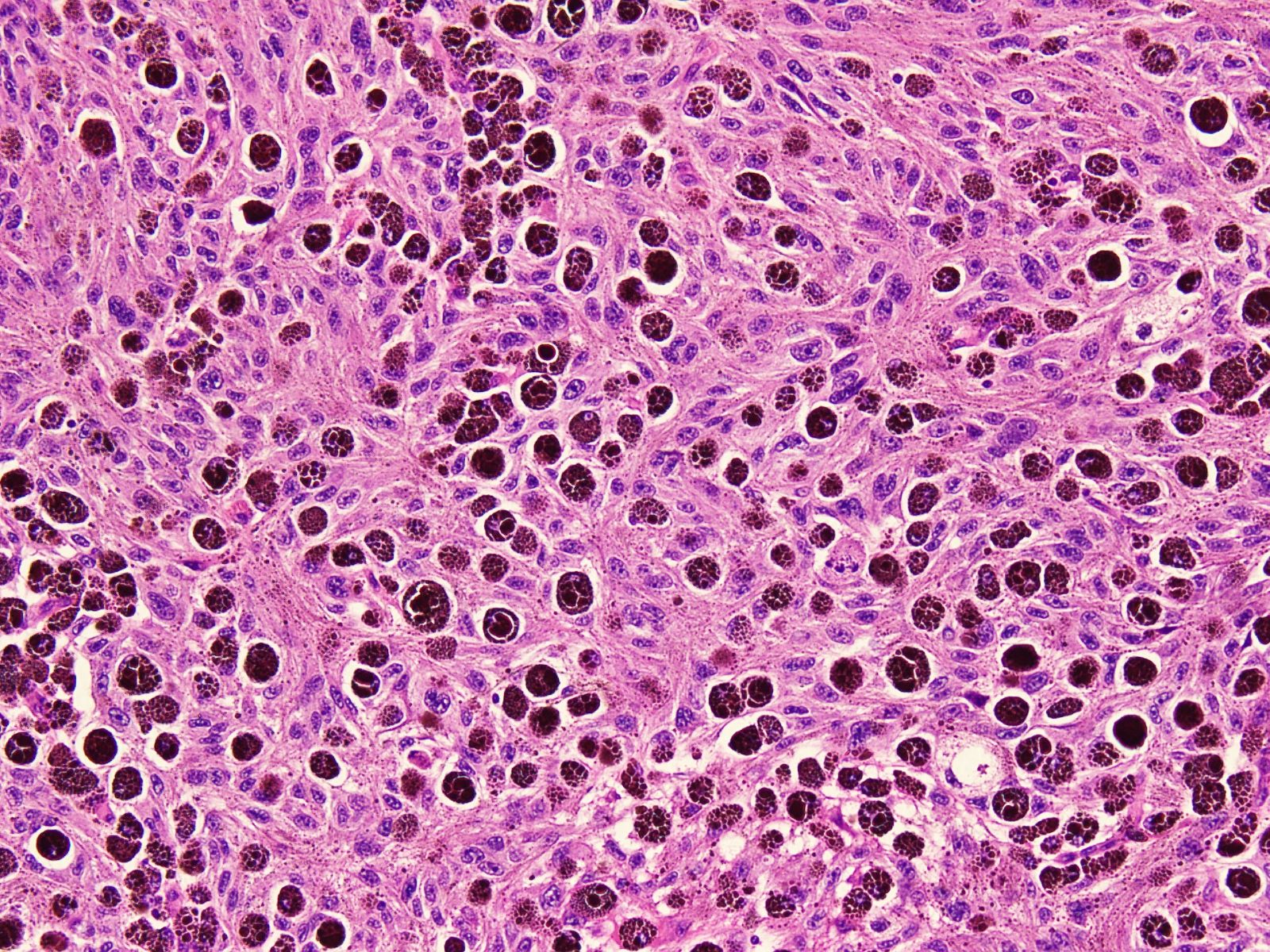
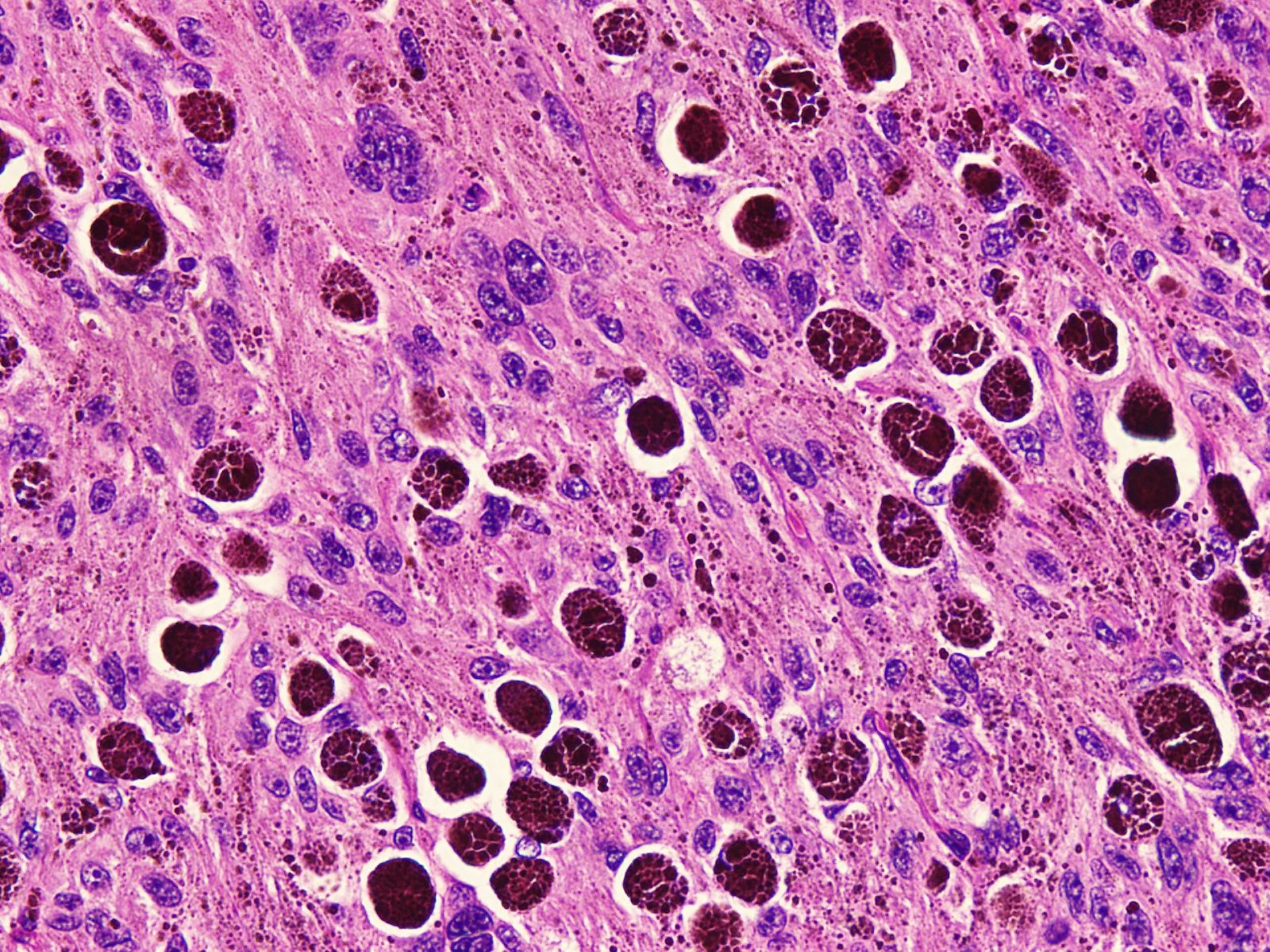
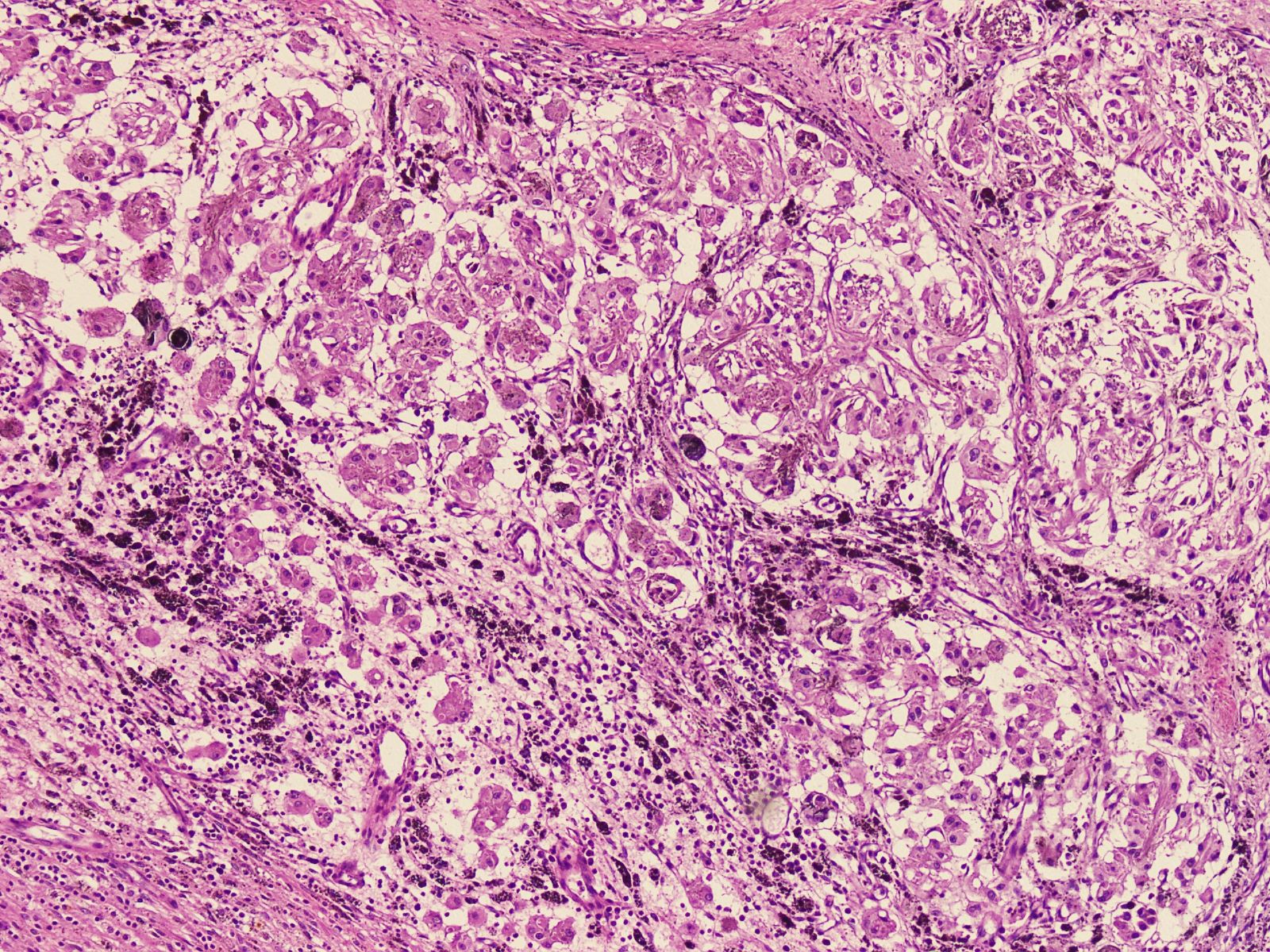
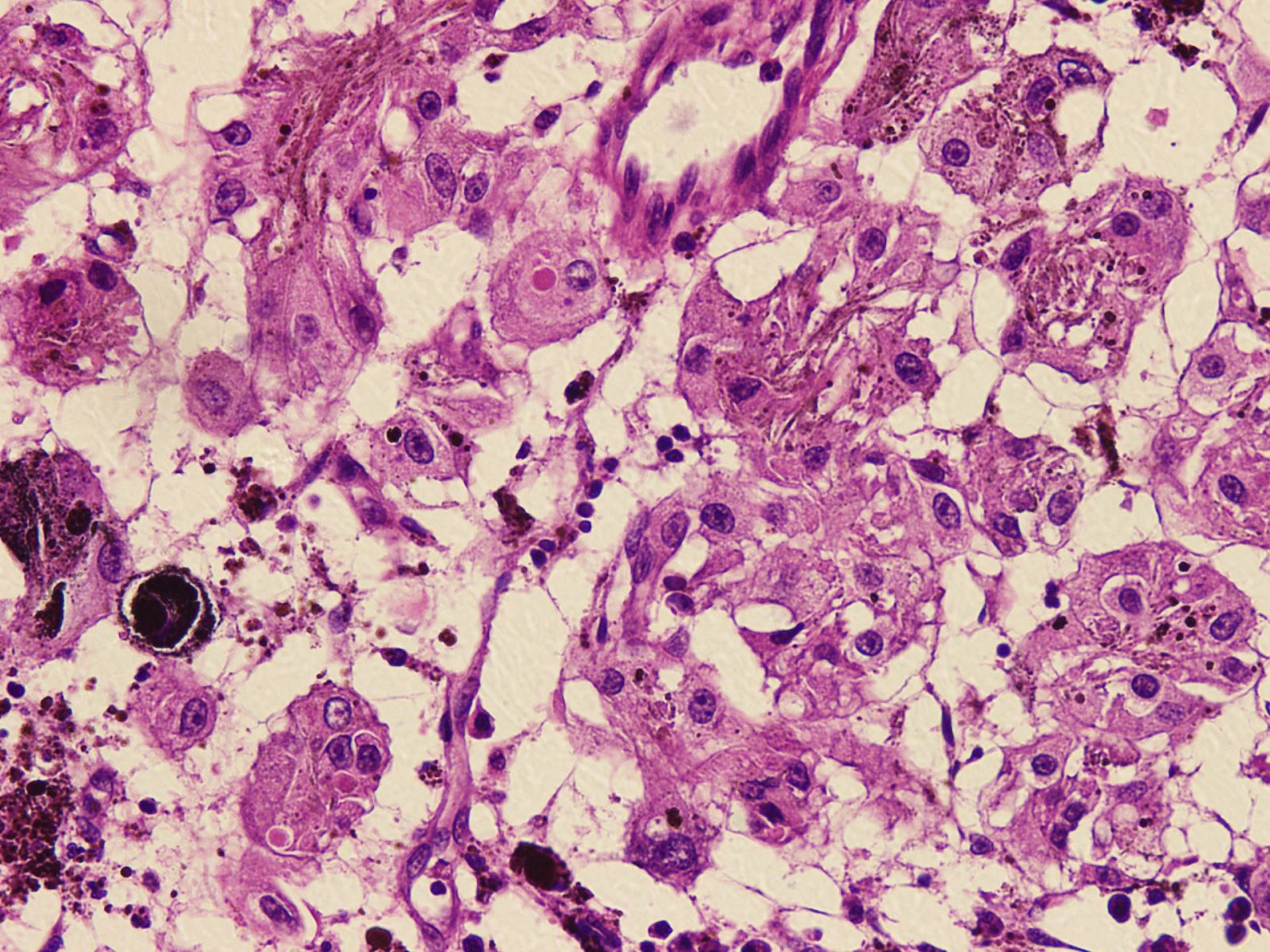
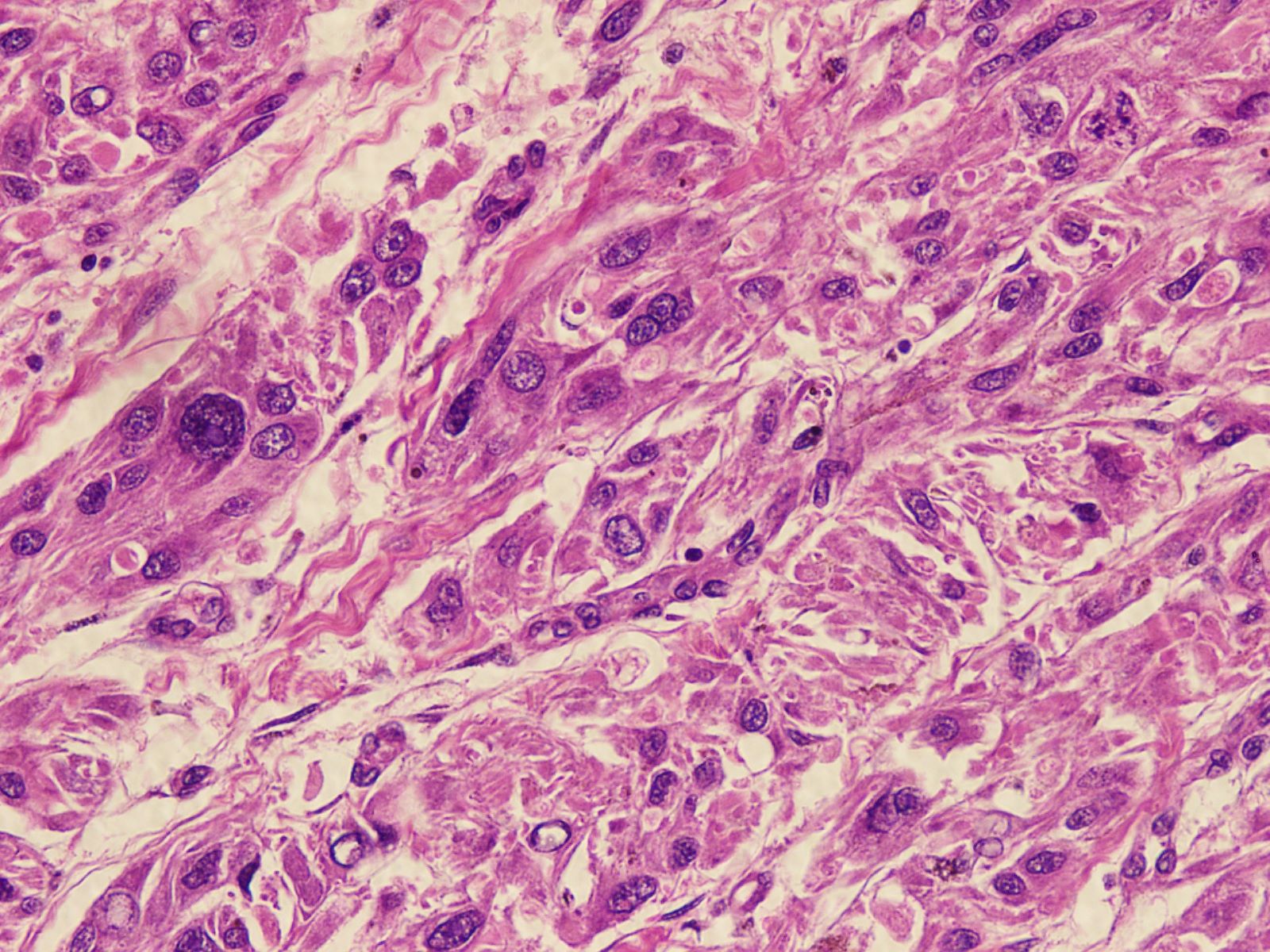
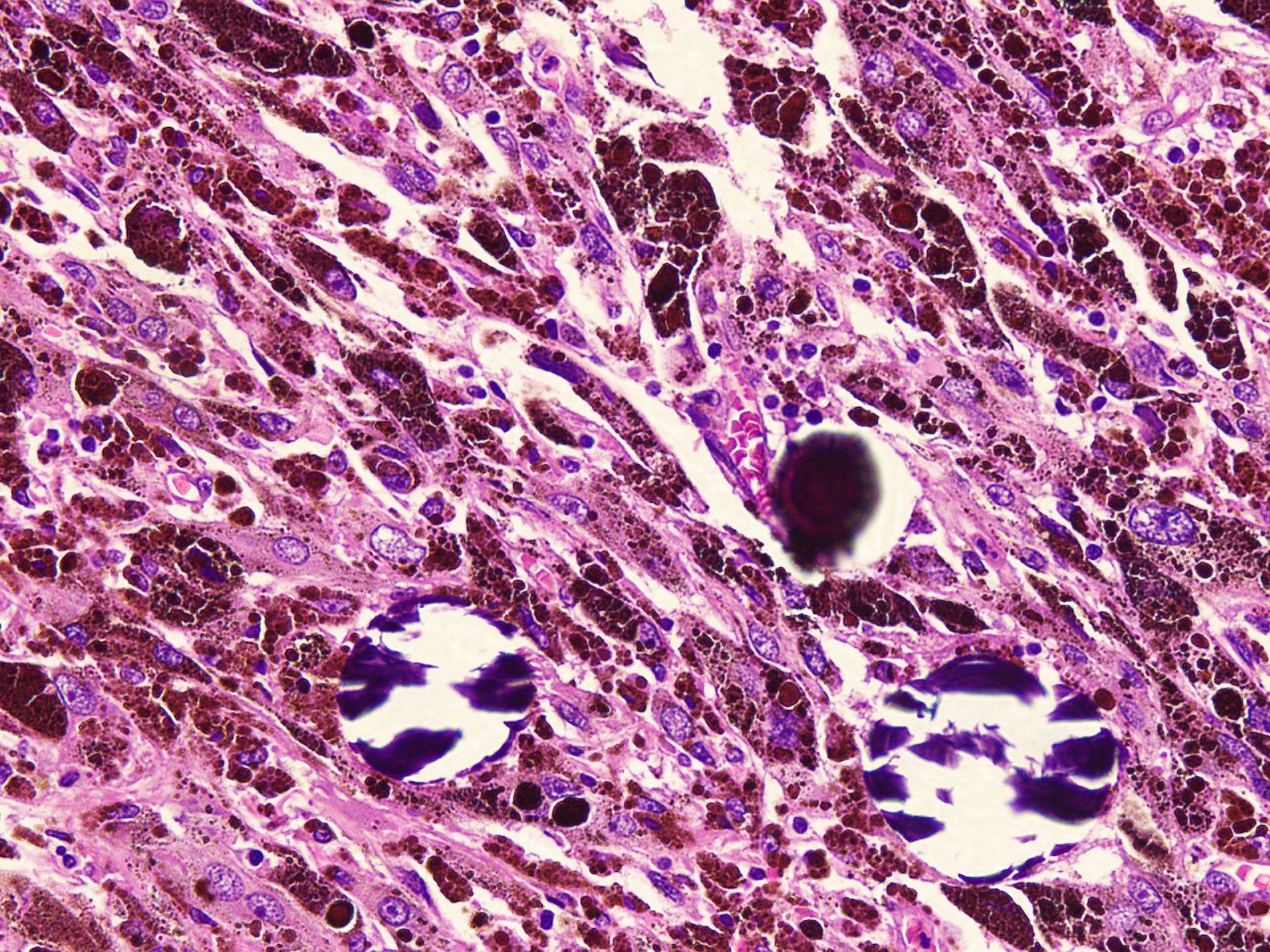
- Circumscribed, unencapsulated lesion with plump spindle and epithelioid cells arranged in interlacing fascicles or nests
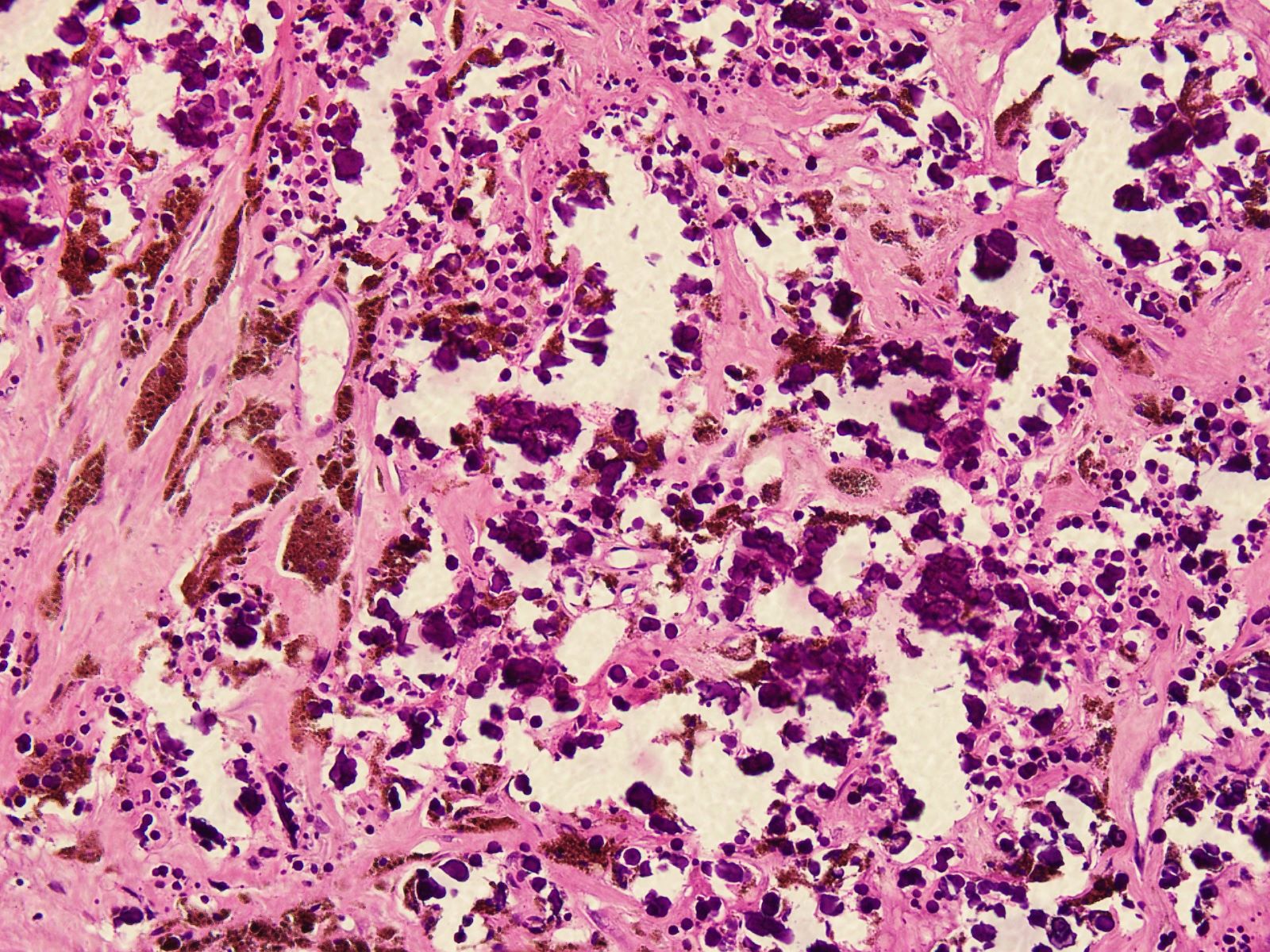
- Accumulation of melanin in neoplastic cells and associated melanophages
- Round, ovoid or elongated nuclei which contain delicate, evenly distributed chromatin and small distinct nucleoli; some areas may show large and prominent nucleoli
- Rare mitoses
- Tumors associated with Carney complex may show sheets of adipose-like cells and psammoma bodies
- Degenerative nuclear atypia, markedly enlarged, hyperchromatic nuclei, smudgy chromatin and cytoplasmic nuclear inclusions may occasionally be seen
- Psammoma bodies can be seen; these can be isolated foci or innumerable calcified structures (J Int Med Res 2020;48:300060520947919, Am J Surg Pathol 2014;38:94, Arch Pathol Lab Med 2018;142:1517)
- Necrosis, when present, is often geographic in pattern
- Strict criteria of malignancy in MMNST are not well developed, although a combination of worrisome histologic features (large, vesicular nuclei with macronucleoli; brisk, mitotic activity; necrosis) raises concern of aggressive behavior (Arch Pathol Lab Med 2018;142:1517)
Microscopic (histologic) images
Contributed by Nasir Ud Din, M.B.B.S.
Positive stains
- S100, SOX10, MelanA, HMB45, tyrosinase (Medicine (Baltimore) 2021;100:e24803, Neuroradiol J 2019;32:335, J Belg Soc Radiol 2018;102:15)
- Retained SMARCB1 (Am J Surg Pathol 2014;38:94)
- Ki67 index is less than 5% in 92% of cases, 5 - 10% in 8% of cases (Am J Surg Pathol 2014;38:94)
- Antigen Ki67 shows a highly variable mitotic index between 1% and 20%, with an average of 3% (J Belg Soc Radiol 2018;102:15)
Negative stains
- GFAP, EMA, AE1 / AE3 (Medicine (Baltimore) 2021;100:e24803)
- Loss of PRKAR1A expression (Am J Surg Pathol 2014;38:94, Genes Chromosomes Cancer 2015;54:463)
Electron microscopy description
- Epithelial Schwann cells and pigmented spindle cells are bundle shaped, interleaved and wheel shaped, with round and oval nuclei, obvious nucleoli and rare nuclear division (Medicine (Baltimore) 2021;100:e24803)
- Numerous elongated tumor cell processes, duplicated basement membrane and melanosomes are observed in all developmental stages (Arch Pathol Lab Med 2018;142:1517)
Molecular / cytogenetics description
- Loss of PRKAR1A expression corresponding to mutations of the gene (Am J Surg Pathol 2014;38:94, Genes Chromosomes Cancer 2015;54:463)
Videos
MMNST by Dr. Jerad Gardner
Sample pathology report
- Lumbar spine mass, excision:
- Malignant melanotic nerve sheath tumor (see comment)
- Comment: Histology showed a circumscribed, unencapsulated lesion containing plump spindle to epithelioid cells arranged in interlacing fascicles. Individual cells are round to ovoid with regular nuclei and evenly distributed chromatin. No significant mitotic activity or necrosis is identified. These cells exhibit melanin pigment. These tumors can be sporadic or part Carney complex or neurofibromatosis type 1. Clinical correlation is suggested.
Differential diagnosis
- Malignant melanoma:
- Occurs in older patients
- Predilection for cutaneous, mucosal and extracutaneous sites
- Composed of epithelioid or spindle shaped cells with nuclear pleomorphism, hyperchromasia, coarse irregular chromatin and prominent eosinophilic nucleoli
- Variable dusty pigmented cytoplasm, frequent mitosis
- Lacks psammoma bodies, adipose-like cells and pericellular basement membrane synthesis
- Overlapping positive stains (S100 [nuclear and cytoplasmic], SOX10 [nuclear], MelanA / MART1 [cytoplasmic], HMB45 [cytoplasmic], tyrosinase [cytoplasmic]), Ki67 / MIB1 > 10%
- Molecular testing for BRAF V600E is positive
- Pigmented neurofibroma:
- Occurs in 2 - 61 year old patients (median age of 28 years) (Am J Surg Pathol 2000;24:331)
- Localized neurofibromas are superficial and evenly distributed over the body surface
- Diffuse neurofibromas are usually in the head and neck
- Plexiform neurofibromas are localized to a major nerve trunk
- Histologically cells are short and spindle shaped, with wavy scant cytoplasm and occasionally granular, dark brown pigment, small elongated nuclei
- Intratumoral fat in the form of scattered adipocytes may be seen
- Lacks psammoma bodies
- Positive for melanocytic / Schwannian cell markers and CD34
- Pigmented dermatofibrosarcoma protuberans:
- Occurs over a wide age range but most commonly in early to mid adulthood
- Can involve any area of skin but the trunk and extremities are the most common location
- Histologically plump spindle cells in a storiform pattern, diffuse infiltration of the dermal stroma and subcutis with pigmented dendritic cells dispersed among neoplastic cells
- Positive for CD34
- Negative for S100 and other melanocytic markers
- Dendritic pigmented cells show positivity for Fontana-Masson stain; express S100 protein, MelanA and HMB45; contain premelanosomes and mature melanosomes
- Characterized by a t(17;22) translocation resulting in the fusion of exon 2 of PDGFB to COL1A1 gene
- Pigmented epithelioid melanocytoma:
- Age: median age of 20 - 27 years (Surg Pathol Clin 2021;14:285)
- Site: extremities (38.3%), head and neck (30.8%) and trunk (30.8%) (Surg Pathol Clin 2021;14:285)
- Melanocytoma are benign lesions, intermediate grade tumors
- Histologically heavily pigmented, elongated or polygonal cells with vesicular nuclei and distinct nucleoli
- Lacks psammoma bodies and pericellular basement membrane and adipose-like cells
- Often associated with Carney complex or other banal nevi
- Immunoprofile is similar to MMNST: positive for S100, SOX10, HMB45, MelanA
- Negative stain: loss of cytoplasmic PRKAR1A
- Fusions in protein kinase C alpha (PRKCA) or inactivating alterations in protein kinase A regulatory subunit R1 alpha gene (PRKAR1A) with a preceding mutation of BRAF or less frequently, NRAS (J Cutan Pathol 2019;46:878)
- Reference: Arch Pathol Lab Med 2018;142:1517
Additional references
Board review style question #1
Board review style answer #1
C. Malignant melanotic nerve sheath tumor
Comment Here
Reference: Malignant melanotic nerve sheath tumor
Comment Here
Reference: Malignant melanotic nerve sheath tumor
Board review style question #2
Malignant melanotic nerve sheath tumor is associated with which of the following?
- Carney syndrome
- McCune-Albright syndrome
- Neurofibromatosis type 2 (NF2)
- Peutz-Jeghers syndrome
- Tuberous sclerosis
Board review style answer #2