Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Obeidin F. Lymphangioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuelymphangioma.html. Accessed April 2nd, 2025.
Definition / general
- Benign localized or diffuse vascular proliferation composed of lymphatic vessels
Essential features
- Developmental proliferation composed of lymphatic vessels of varying sizes
- May be either microcystic or macrocystic in nature
- Wide age range but predominant in children and young adults
- Histology: dilated, thin walled lymphatic channels with flat endothelial cells; may show prominent stromal lymphoid tissue and proteinaceous fluid
- IHC: PROX1, CD31, D2-40 and VEGFR3 positive
Terminology
- Updated 2018 ISSVA classification for vascular anomalies recommends using the term lymphatic malformation for all lymphatic anomalies
- Related / previous terminology: cystic hygroma, lymphangioma, lymphangioma circumscriptum, cavernous lymphangioma, intra-abdominal cystic lymphangioma, hemangiolymphangioma
ICD coding
- ICD-10: D18.1 - lymphangioma, any site
Epidemiology
- Wide age range
- Majority are in children and young adults (90% diagnosed by age 2)
- Mean age is 3.3 years (J Pediatr Surg 1999;34:1164)
- Slight male predominance
Sites
- May be superficial or deep (Semin Intervent Radiol 2017;34:225)
- Macrocystic
- Often in skin, subcutaneous tissue or deeper
- Commonly neck and groin in infants with chromosomal abnormalities
- Microcystic
- Most commonly in skin and mucosal sites
Pathophysiology
- Multiple theories suggested for the pathogenesis, including
- Sequestration of lymphoid tissue during development
- Abnormal budding of lymphatic vessels during development
- Lack of fusion of the lymphatic system to the venous system
- Trauma / infection
- Various vascular growth factors are associated with the genesis of lymphangiomas (Virchows Arch 2008;453:1)
Etiology
- Many lymphatic malformations show somatic mutations in PIK3CA (J Pediatr 2015;166:1048)
- Macrocystic lymphatic malformations (cystic hygroma) may be associated with both euploid and aneuploid fetuses, including trisomy 21, trisomy 18, trisomy 13, Turner syndrome and Noonan syndrome (Acta Obstet Gynecol Scand 2007;86:1442)
Diagrams / tables
Table 1: Nomenclature for vascular anomalies
| Vascular tumors | Vascular malformations | |
Benign Locally aggressive or borderline Malignant | Simple | Combined |
| Capillary malformations Lymphatic malformations Venous malformations Arteriovenous malformations Arteriovenous fistula | Combination of capillary, venous, lymphatic or arterial vessels; for example
| |
- Adapted from the 2018 ISSVA classification for vascular anomalies (ISSVA: Classification for Vascular Anomalies [Accessed 6 December 2022])
- Nomenclature may also include the name of major vessels or syndromes when associated with other anomalies
Clinical features
- In the skin, pale and pink vesicles
- Deep lesions are circumscribed, soft, fluctuant and painless swellings
- Large cystic lesions may cause compression of adjacent structures
Diagnosis
- Clinical history and imaging studies can suggest a lymphangioma
- Usually diagnosed on simple excision or incidentally on biopsy
Radiology description
- Considered a low flow vascular malformation
- Usually cystic in appearance but hemorrhage or infection may give a more solid appearance
- Ultrasound (AJR Am J Roentgenol 2004;182:1485)
- Multilocular cystic masses with anechoic cyst contents or echogenic debris
- Can have wide variation
- CT
- Homogenous and cystic with low attenuation
- Often does not show the intrinsic septations
- MRI (AJR Am J Roentgenol 2004;182:1485)
- Septated, lobulated mass with fluid-fluid levels; may infiltrate tissue planes
- Low signal intensity on T1, high signal intensity on T2
- Macrocystic tumors may have rim and septal enhancement that are not seen in microcystic tumors
Radiology images
Prognostic factors
- Benign with a generally excellent prognosis in adults
- Locally recurrent potential (~20% of tumors); younger age and presence of associated symptoms of infection, dyspnea, dysphagia or hemorrhage are associated with higher rates of recurrence (Arch Otolaryngol Head Neck Surg 1997;123:1061)
- Neonatal / congenital and macrocystic tumors have a poor prognosis depending on the associated genetic and clinical anomalies (Arch Gynecol Obstet 2007;276:491, Eur J Obstet Gynecol Reprod Biol 2005;118:40)
Case reports
- Neonate with giant abdominal lymphatic malformation diagnosed at 18 weeks gestation (J Surg Case Rep 2020;2020:rjaa252)
- 3 year old boy with a right upper lip swelling (Pediatr Dermatol 2019;36:967)
- 16 year old boy with generalized subcutaneous swelling over the lower back (Radiol Case Rep 2020;16:66)
- 18 year old man with multiple verrucous lesions of the right hand (Pediatr Dermatol 2013;30:e78)
- 21 year old pregnant woman with difficulty breathing and a mass found in the nasopharynx (Am J Case Rep 2019;20:868)
- 24 year old woman with a dorsal tongue mass (Head Neck Pathol 2020;14:512)
- 29 year old woman with a large intra-abdominal / retroperitoneal mass (Radiol Case Rep 2020;16:123)
Treatment
- Depends heavily on the clinical presentation, size and location
- Small or localized lesions are generally amenable to surgical resection
- Large lesions involving multiple deep structures or tissue planes are often not surgically resectable
- Sclerotherapy has been used to some success; particularly in macrocystic lymphatic malformations (Semin Pediatr Surg 2014;23:178)
- Sirolimus may be used to improve prognosis in lymphatic malformations that are life threatening or refractory to other therapies (J Vasc Surg 2020;71:318)
Clinical images
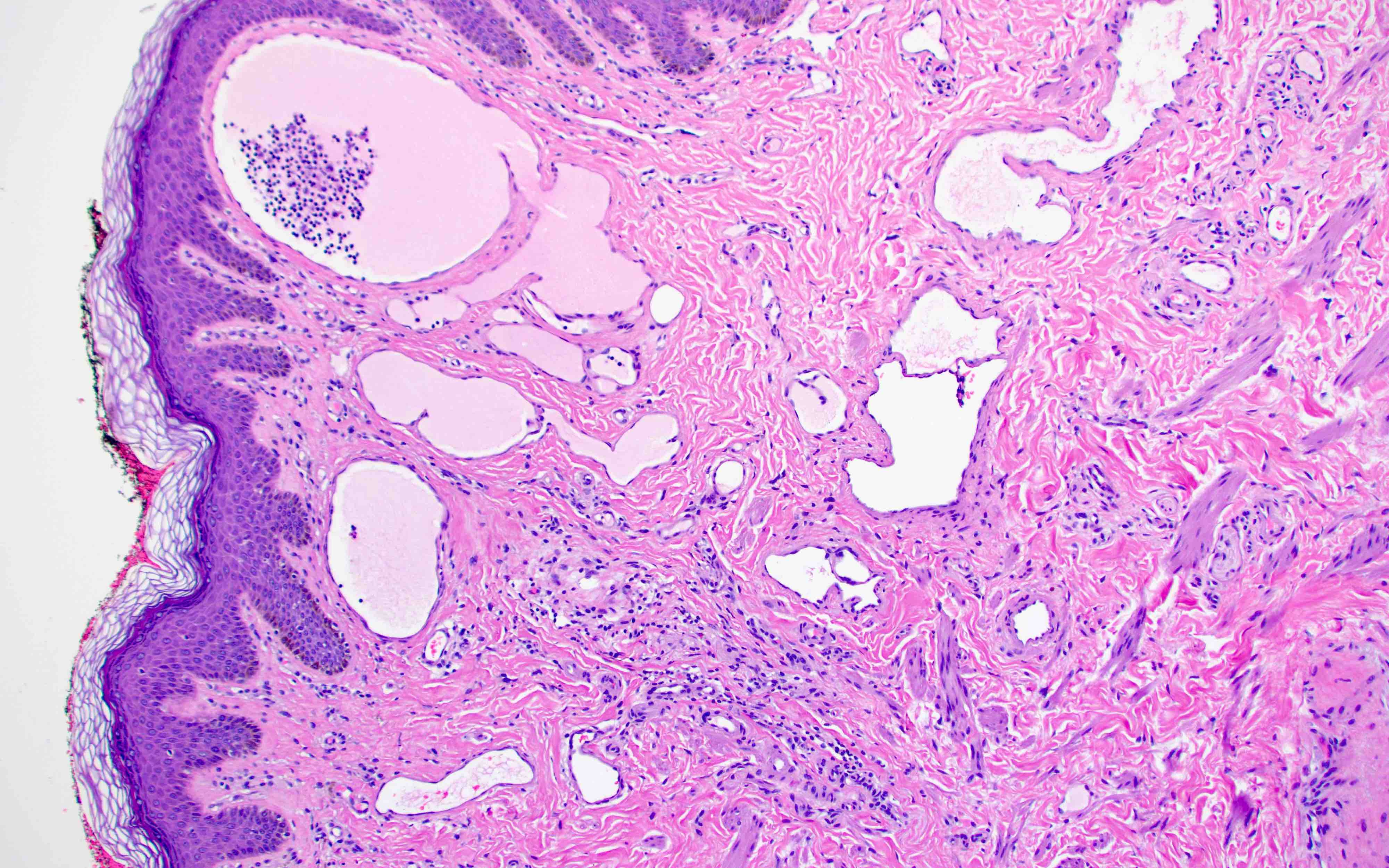
Gross description
- Multicystic and spongy, containing watery / milky chylous fluid
Gross images
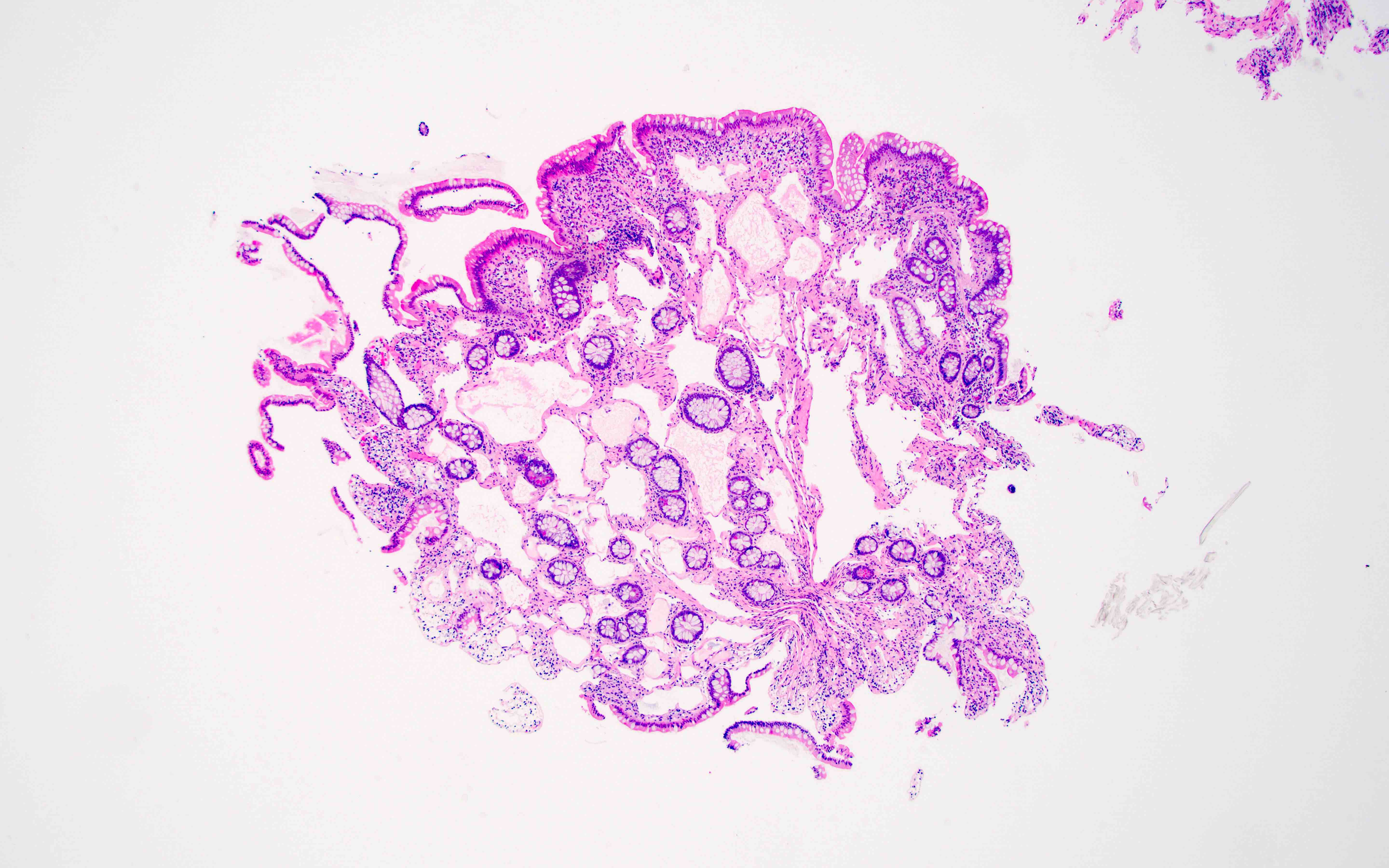
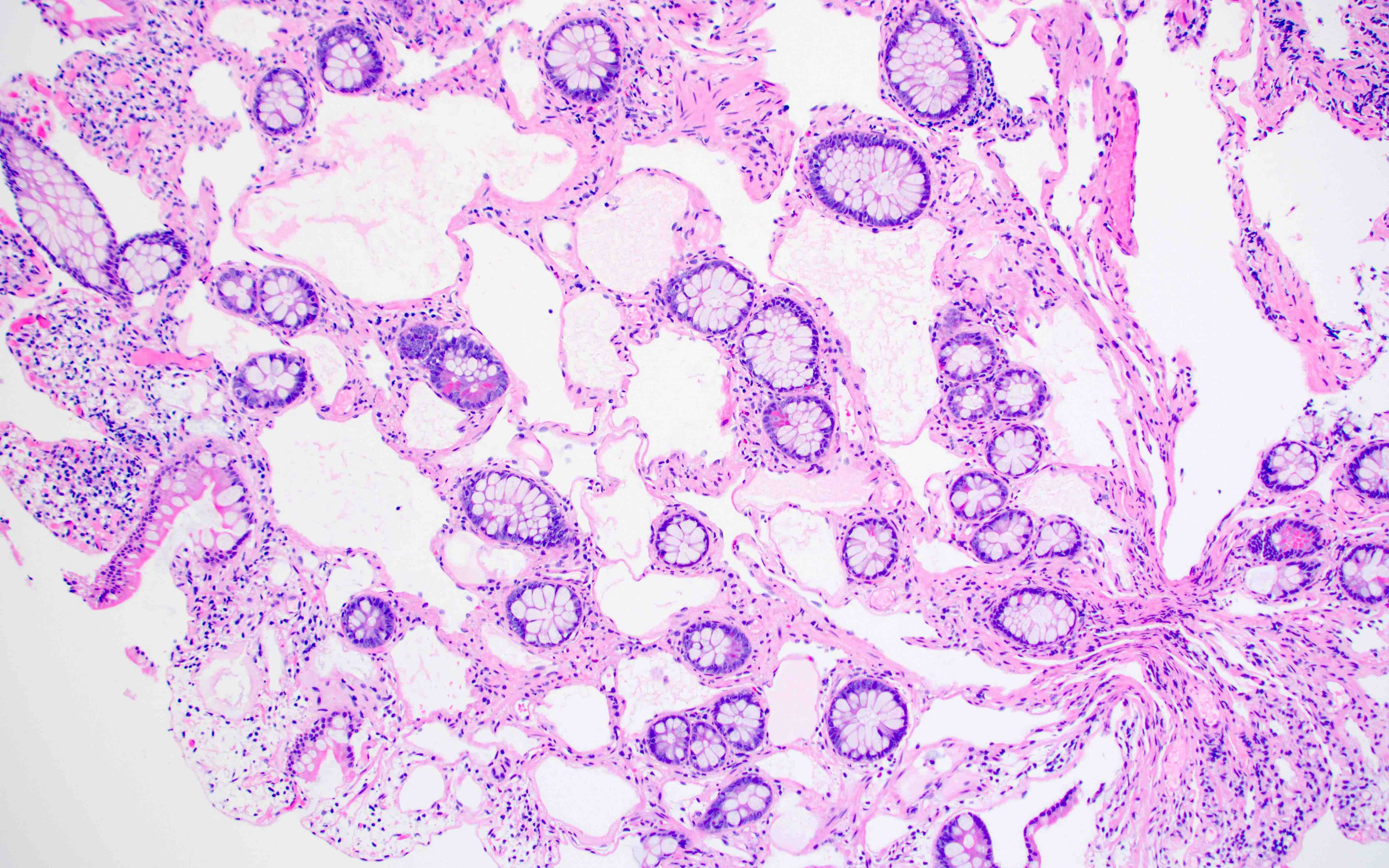
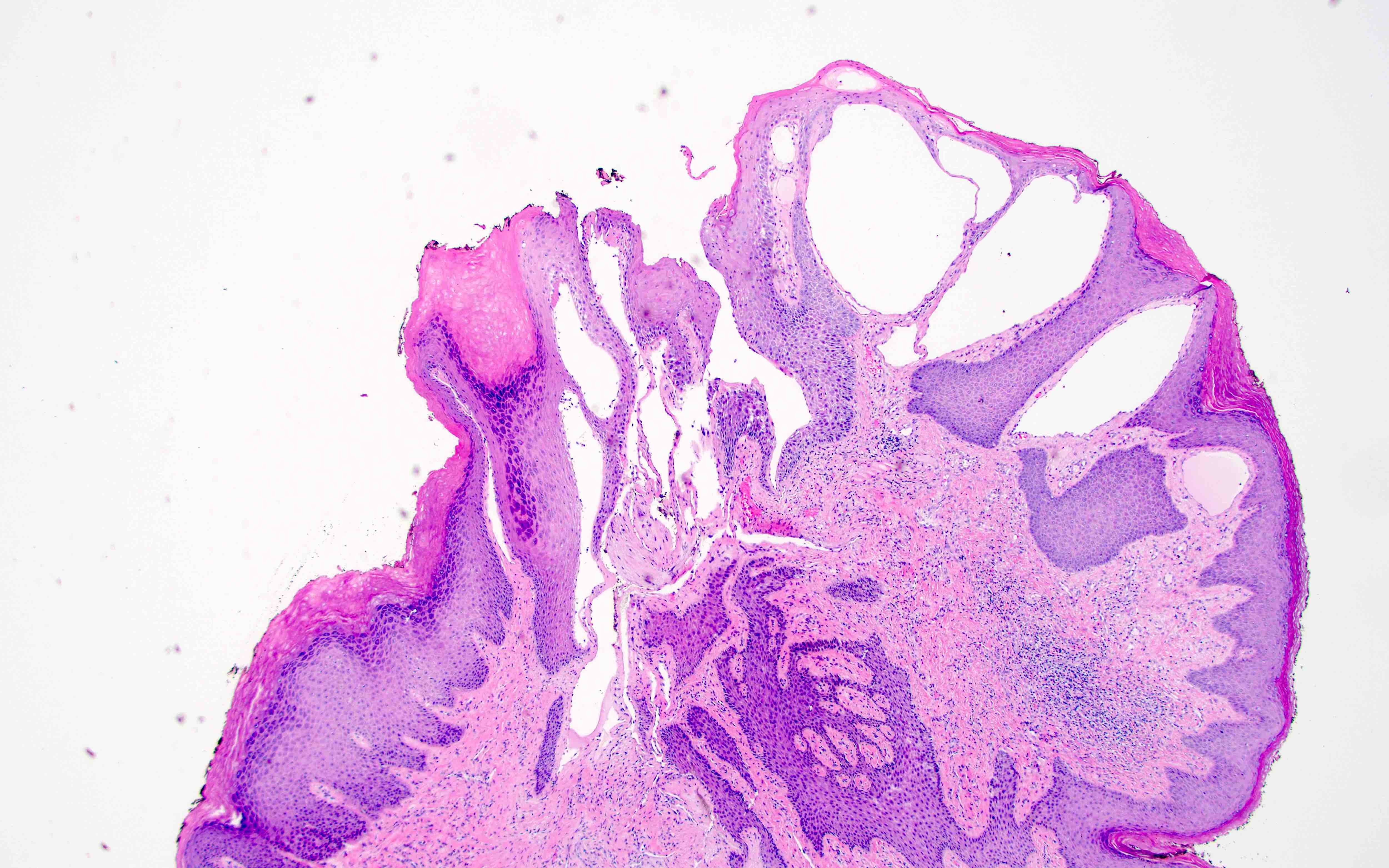
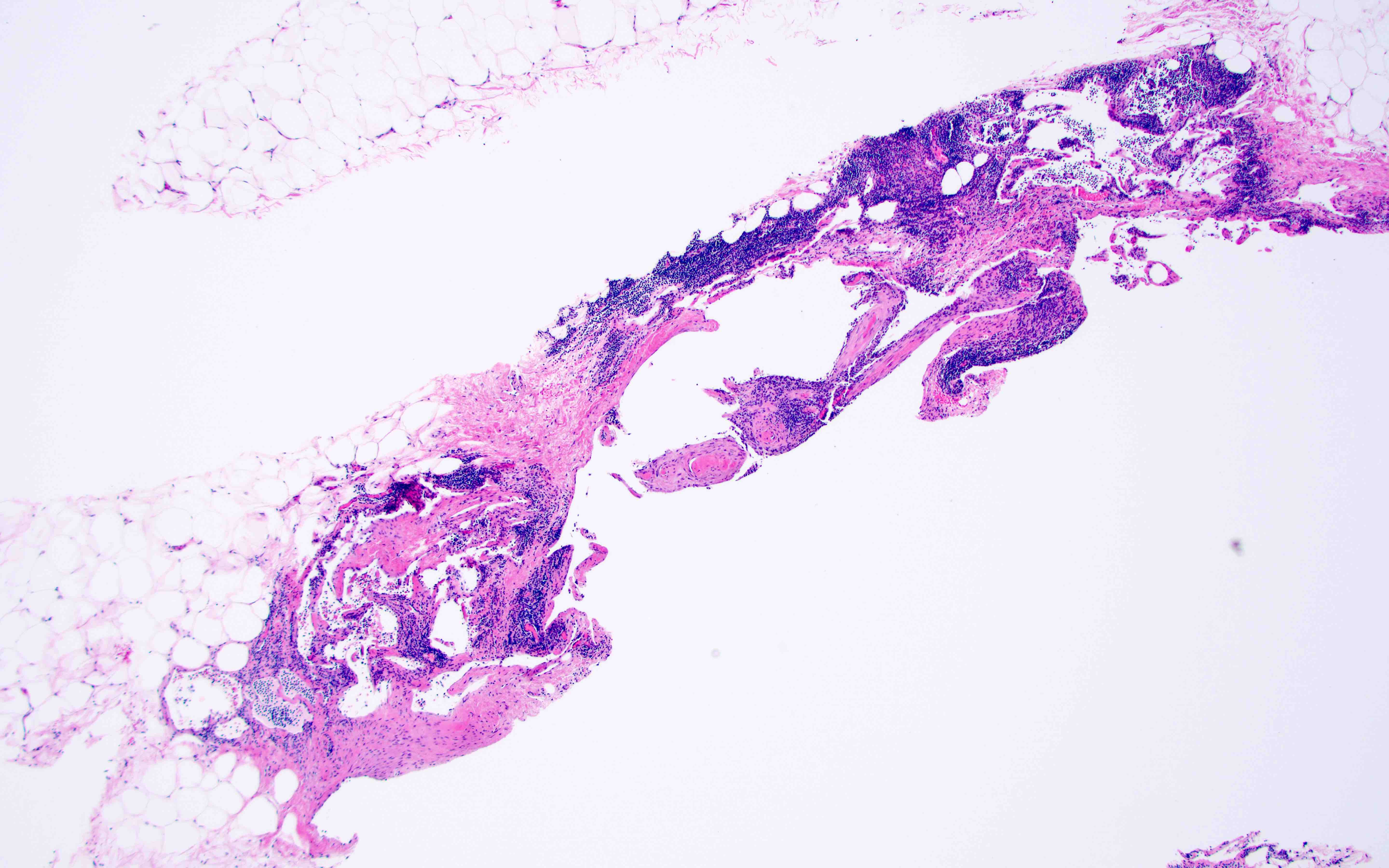
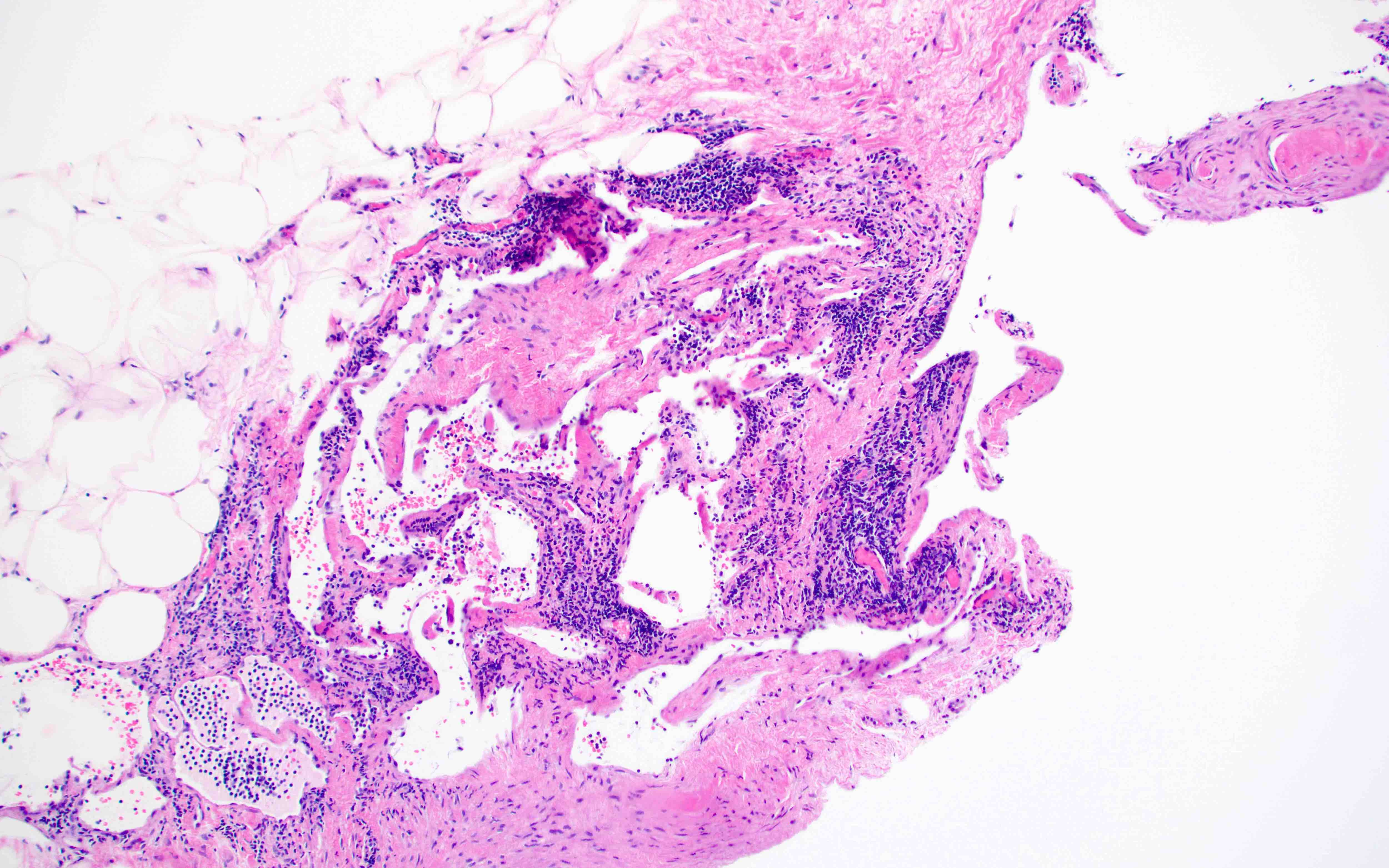
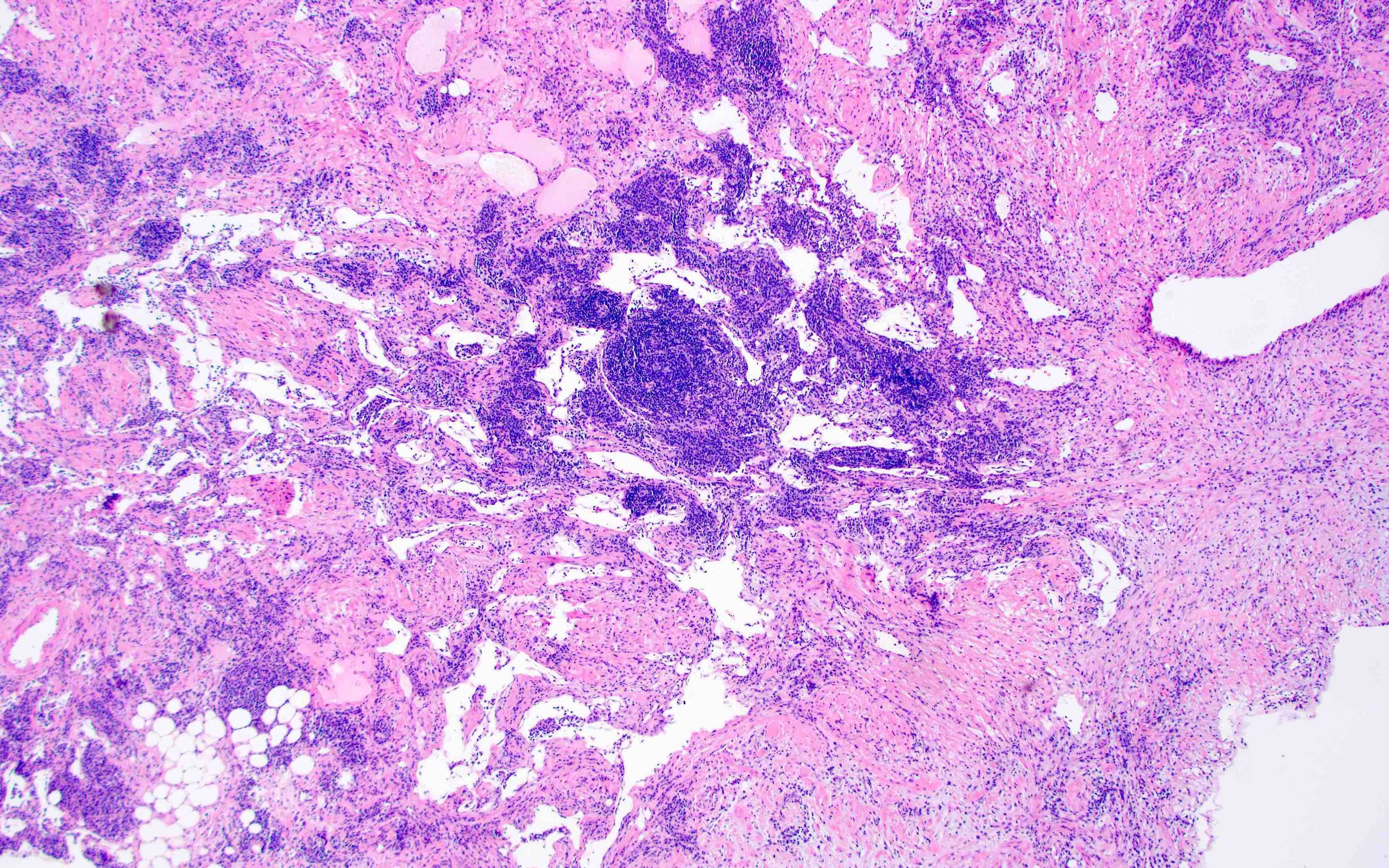
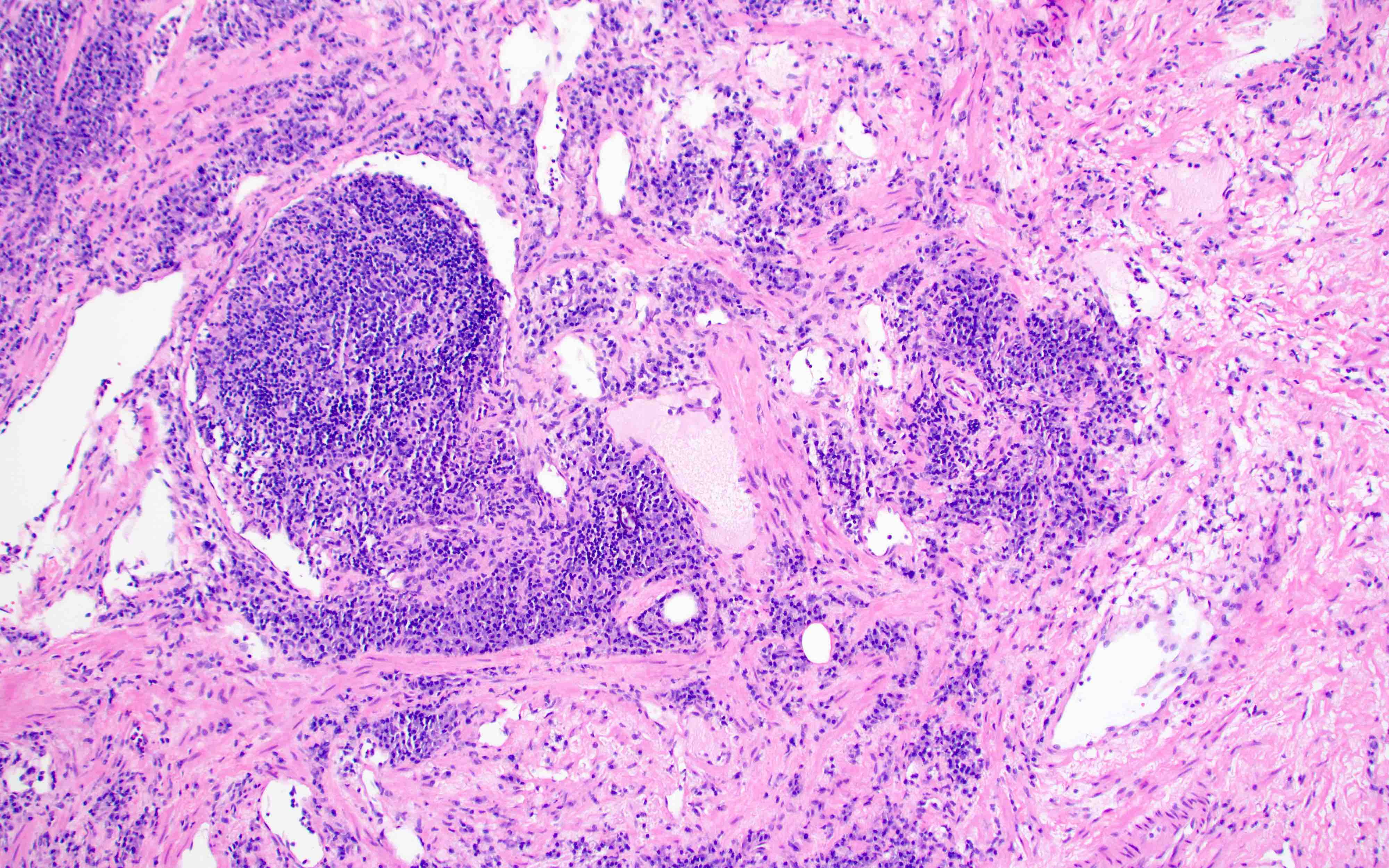
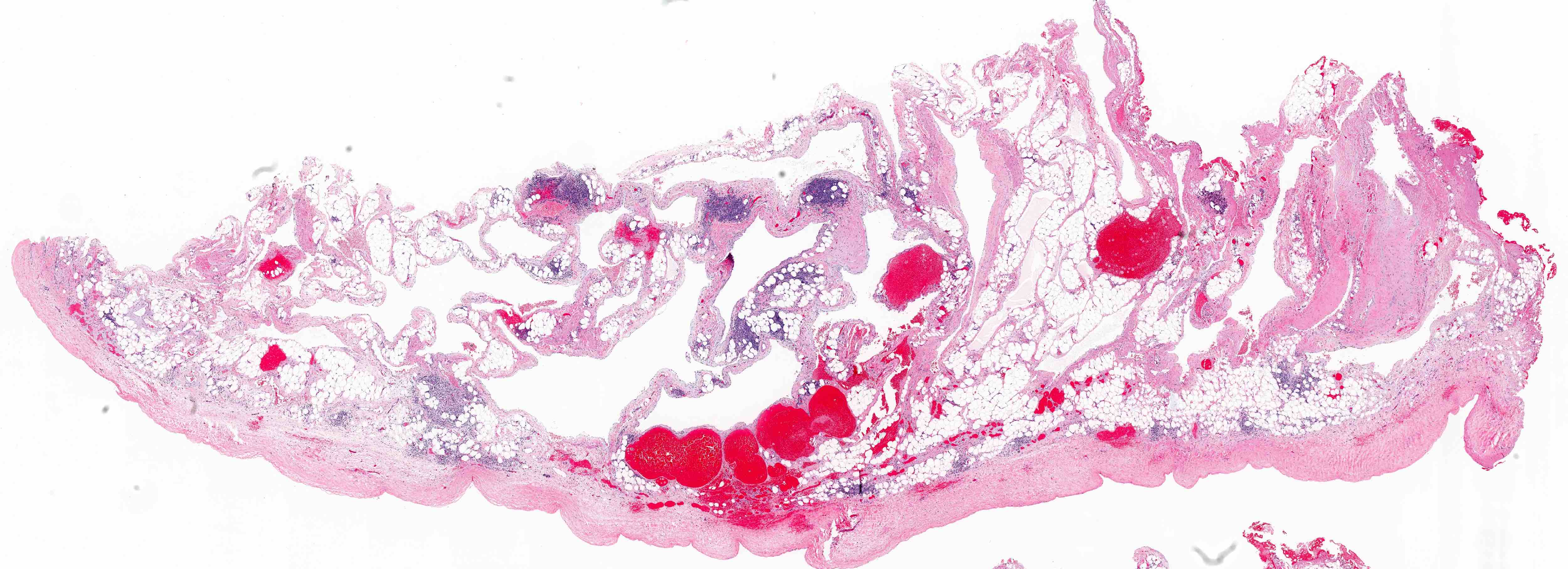
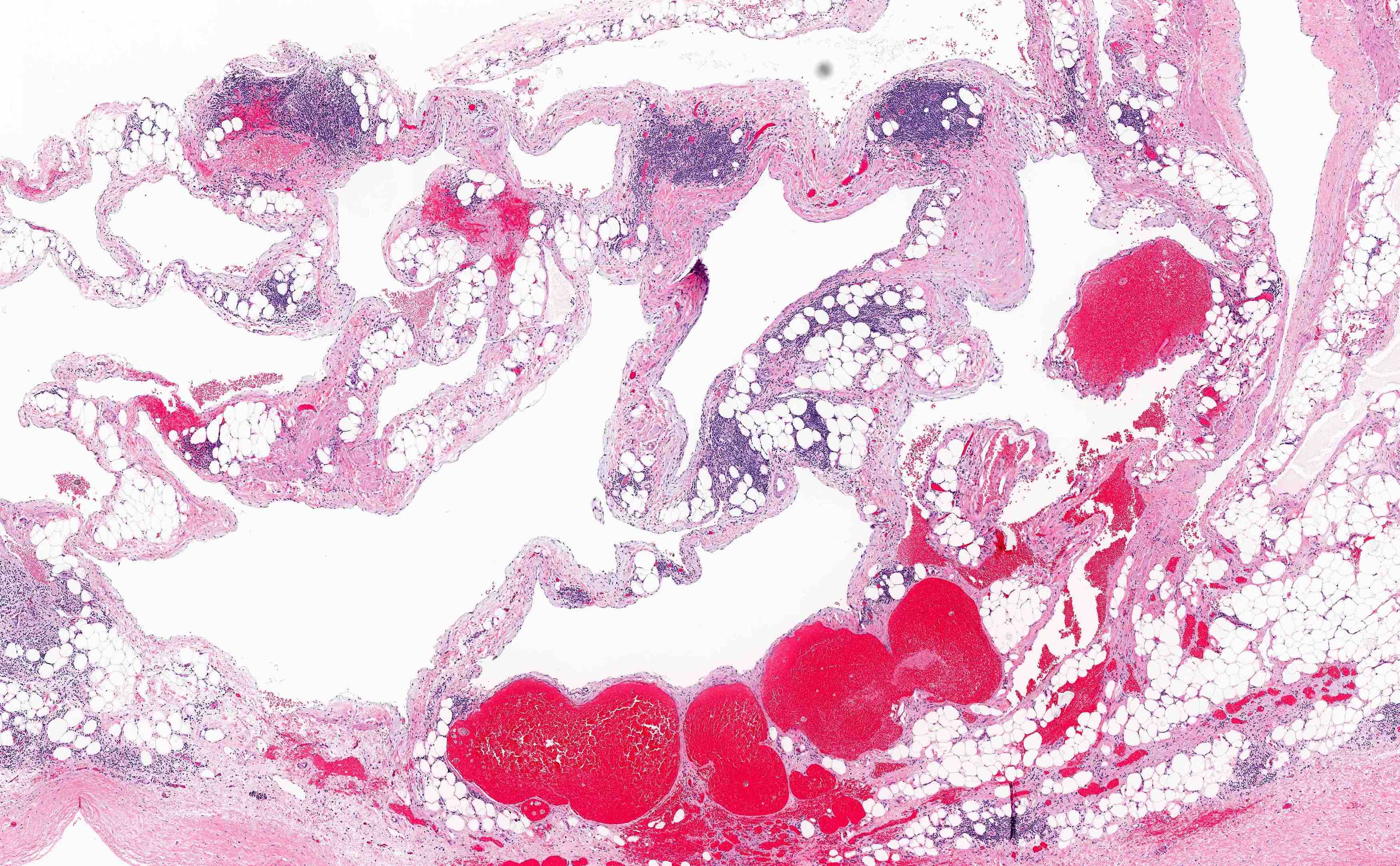
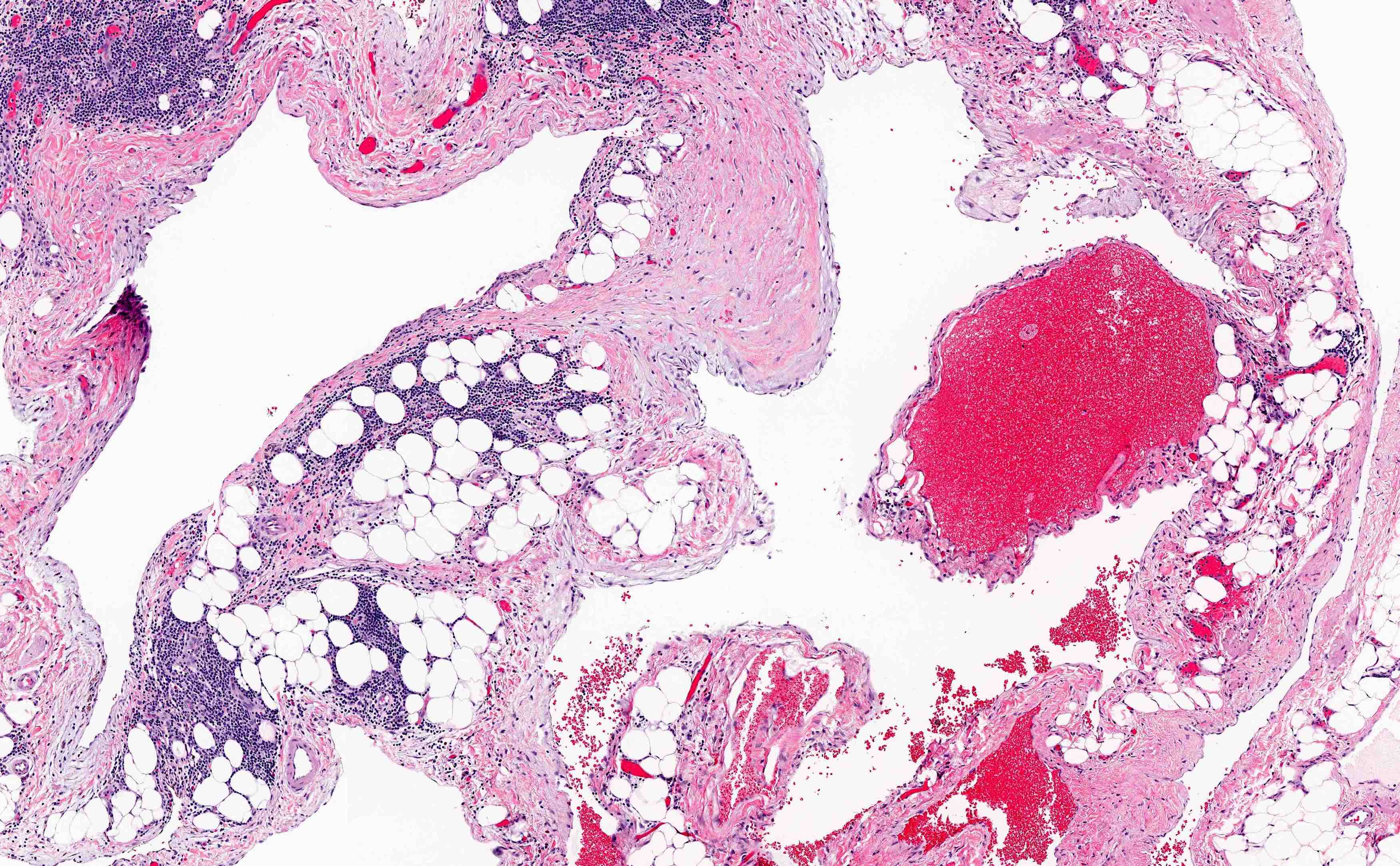
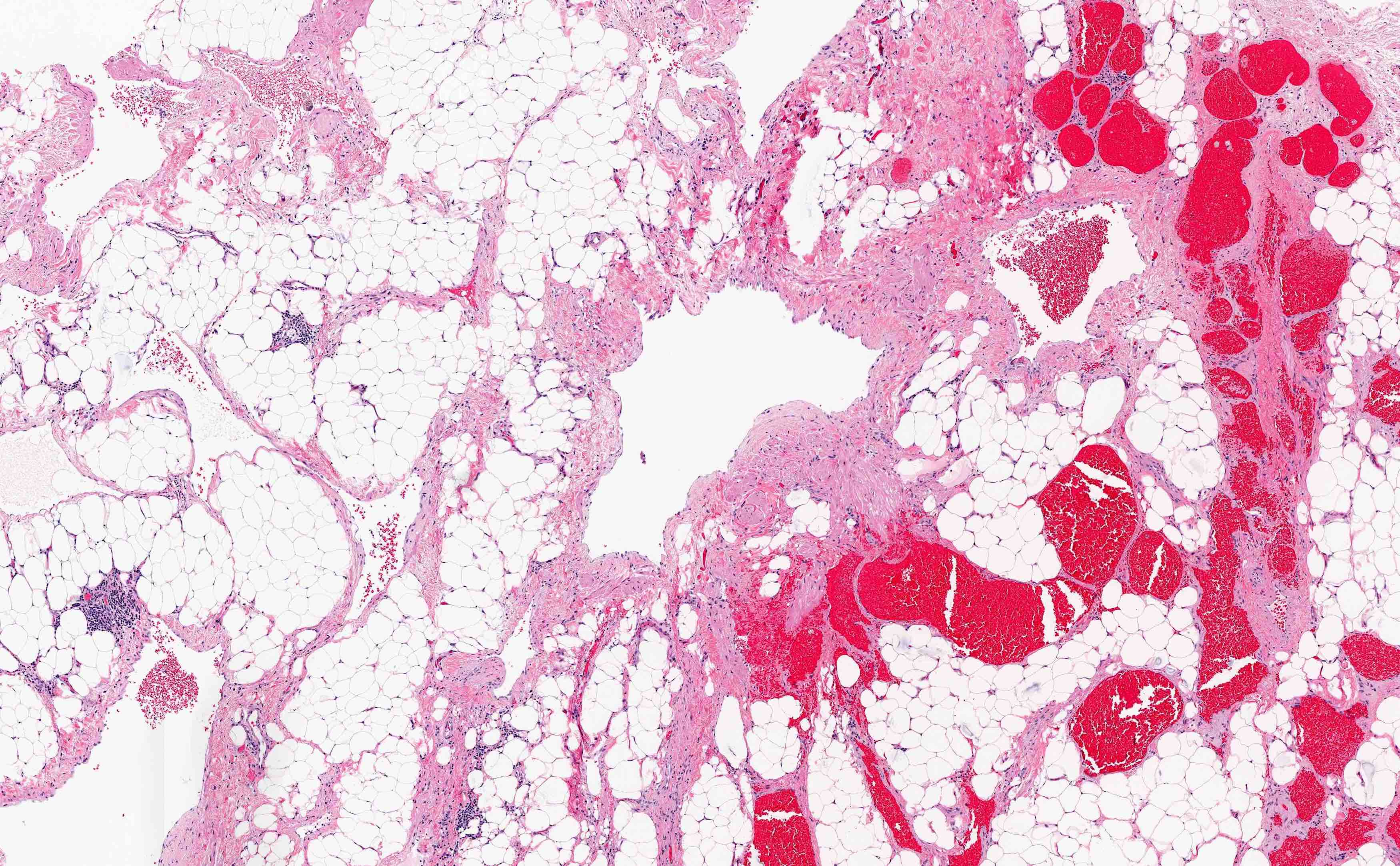
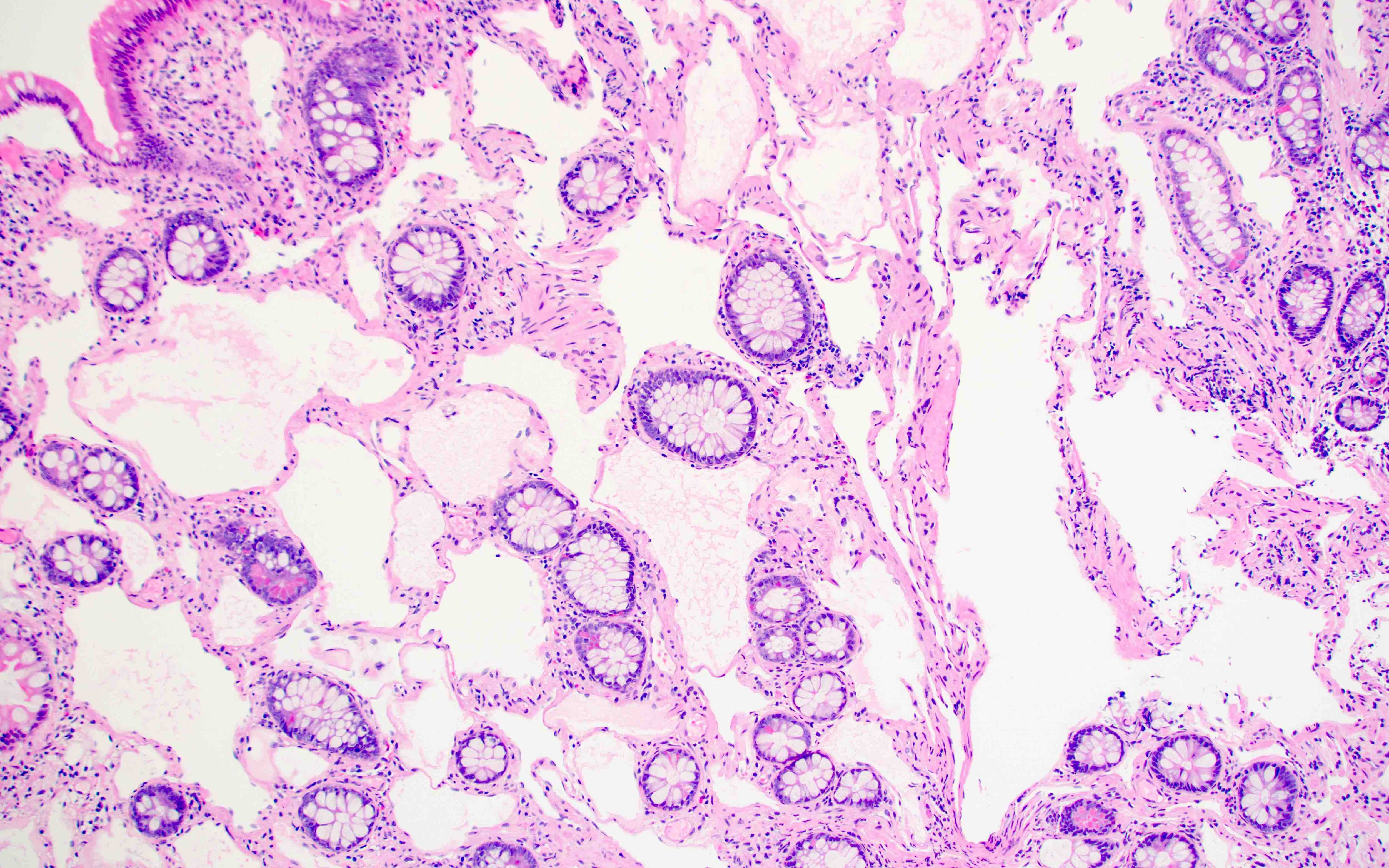
Microscopic (histologic) description
- Divided into categories of macrocystic, microcystic or combined based on the size of the lymphatic channels
- Macrocystic includes cystic hygroma / cystic lymphangioma
- Microcystic includes lymphangioma circumscriptum, cutaneous and small mucosal lymphatic malformations
- Thin walled, dilated lymphatic channels with or without intraluminal proteinaceous material and lymphocytes
- Composed of bland, flat endothelial cells
- Stroma / lymphatic walls may show aggregates of lymphocytes
- Cutaneous tumors may have overlying epidermal hyperplasia
- Larger lymphatic channels can have smooth muscle in the walls
- Longstanding lesions have stromal inflammation, fibrosis, xanthogranulomatous inflammation and myofibroblastic proliferation, particularly in mesenteric and retroperitoneal locations (Hum Pathol 2005;36:426)
- Can cross tissue planes, dissect around normal structures and have anastomosing growth pattern (lymphangiomatosis)
Microscopic (histologic) images
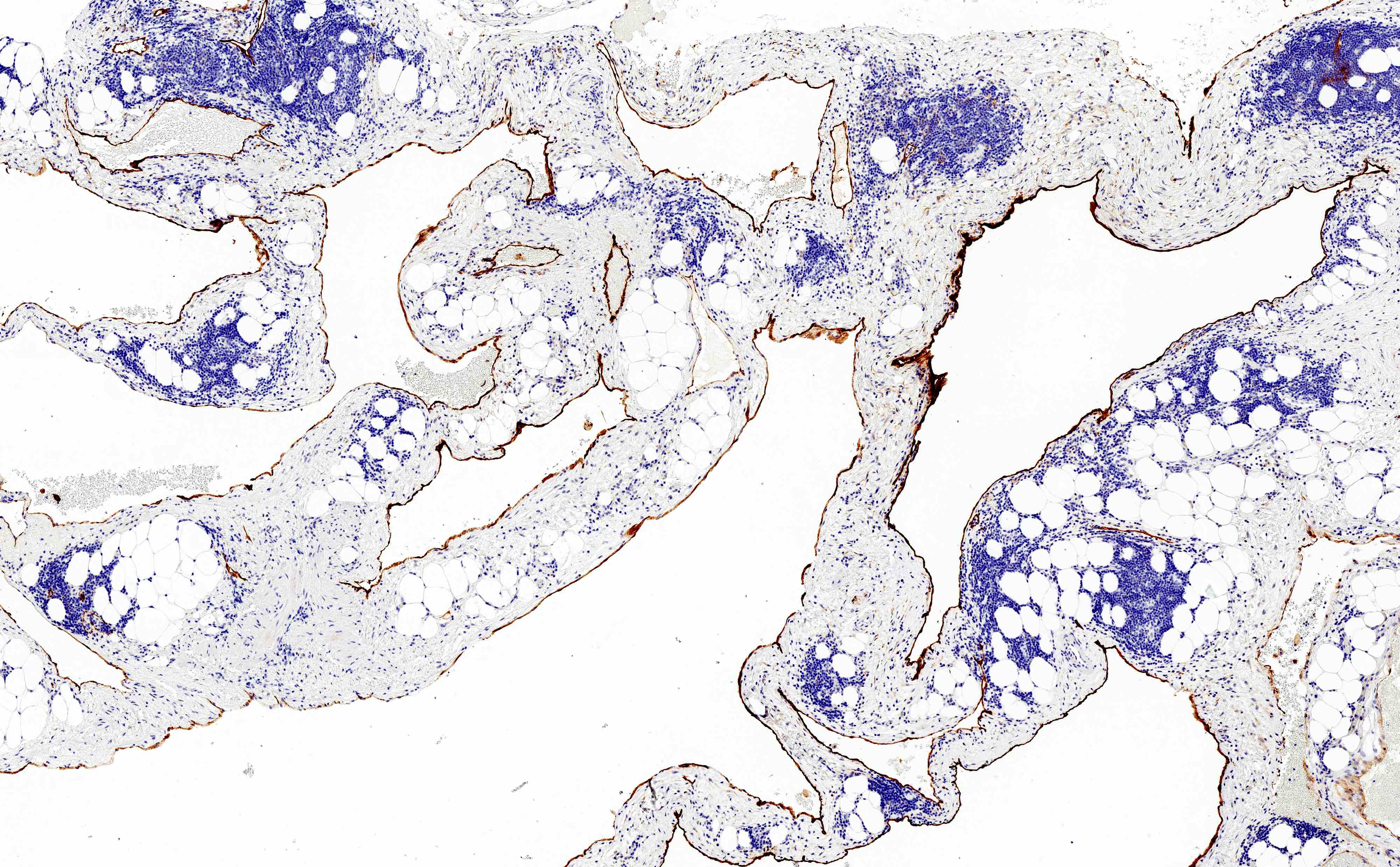
Positive stains
- PROX1, VEGFR3 and CD31 (consistently in small and large vessels); D2-40 / podoplanin (consistent in small vessels but may be lost in large vessels) (Pediatr Dev Pathol 2009;12:187)
- CD34 (variable)
- LYVE1
- SMA highlights the smooth muscle in the walls of the vessels (Mod Pathol 2000;13:1128)
Molecular / cytogenetics description
- Can show somatic mutations in PIK3CA or association with PIK3CA related overgrowth syndromes (J Pediatr 2015;166:1048)
Sample pathology report
- Abdominal mass, excision:
- Lymphatic malformation, mixed macrocystic and microcystic (see comment)
- Comment: Microscopic sections demonstrate small to large caliber vascular spaces filled with proteinaceous fluid and are surrounded by extensive lymphocytic inflammation. The endothelial cells are flat without nuclear atypia and are highlighted with a D2-40 immunostain, supporting the diagnosis.
Differential diagnosis
- Benign vascular neoplasms / malformations:
- Papillary intralymphatic angioendothelioma:
- Typically arises in a background of lymphatic malformation
- Defined by tufting and hobnailing endothelial cell proliferation into the lymphatic channels
- Retiform hemangioendothelioma:
- Angiosarcoma:
- Cytologic atypia with anastomosing, infiltrative architecture and mitotic activity
Additional references
Board review style question #1
A 55 year old woman is undergoing a routine screening colonoscopy, which demonstrates a 0.3 cm sessile nodule in the ascending colon. A biopsy is taken and the histology is represented by the picture above. Which of the following immunohistochemical panels would be expected to stain the lesional cells?
- D2-40, PROX1, CD31
- ERG, FLI1, CD34
- HHV8
- p53, AE1 / AE3
Board review style answer #1
A. D2-40, PROX1, CD31. The picture represents a benign lymphatic malformation / lymphangiomatosis in a colon polyp. These tumors may be infiltrative throughout the lamina propria but overall have a benign cytology and stain with lymphatic endothelial cell markers (D2-40, PROX1, CD31, LYVE1).
Comment Here
Reference: Lymphangioma
Comment Here
Reference: Lymphangioma
Board review style question #2
Macrocystic lymphatic malformations (cystic hygroma) are commonly seen in neonates with which of the following syndromes?
- Beckwith-Wiedemann syndrome
- Fragile X syndrome
- Meckel-Gruber syndrome
- Noonan syndrome
Board review style answer #2
D. Noonan syndrome. Cystic hygromas are commonly seen in aneuploidy syndromes like trisomies and Turner syndrome; however, they may also commonly be seen in some euploid fetuses, particularly those with Noonan syndrome.
Comment Here
Reference: Lymphangioma
Comment Here
Reference: Lymphangioma