Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez RS, Gardner JM. Low grade fibromyxoid sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuelgfibromyxoid.html. Accessed March 31st, 2025.
Definition / general
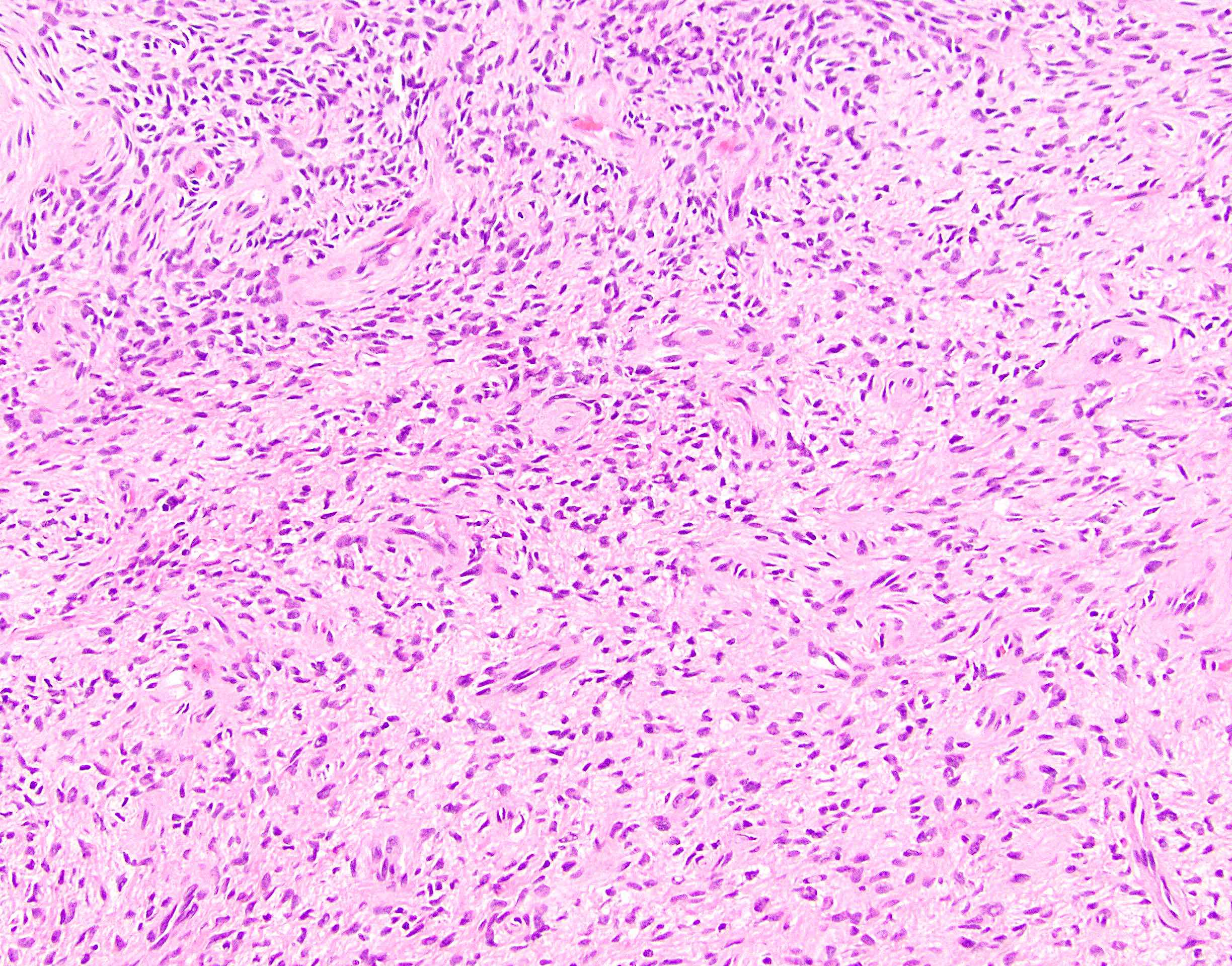
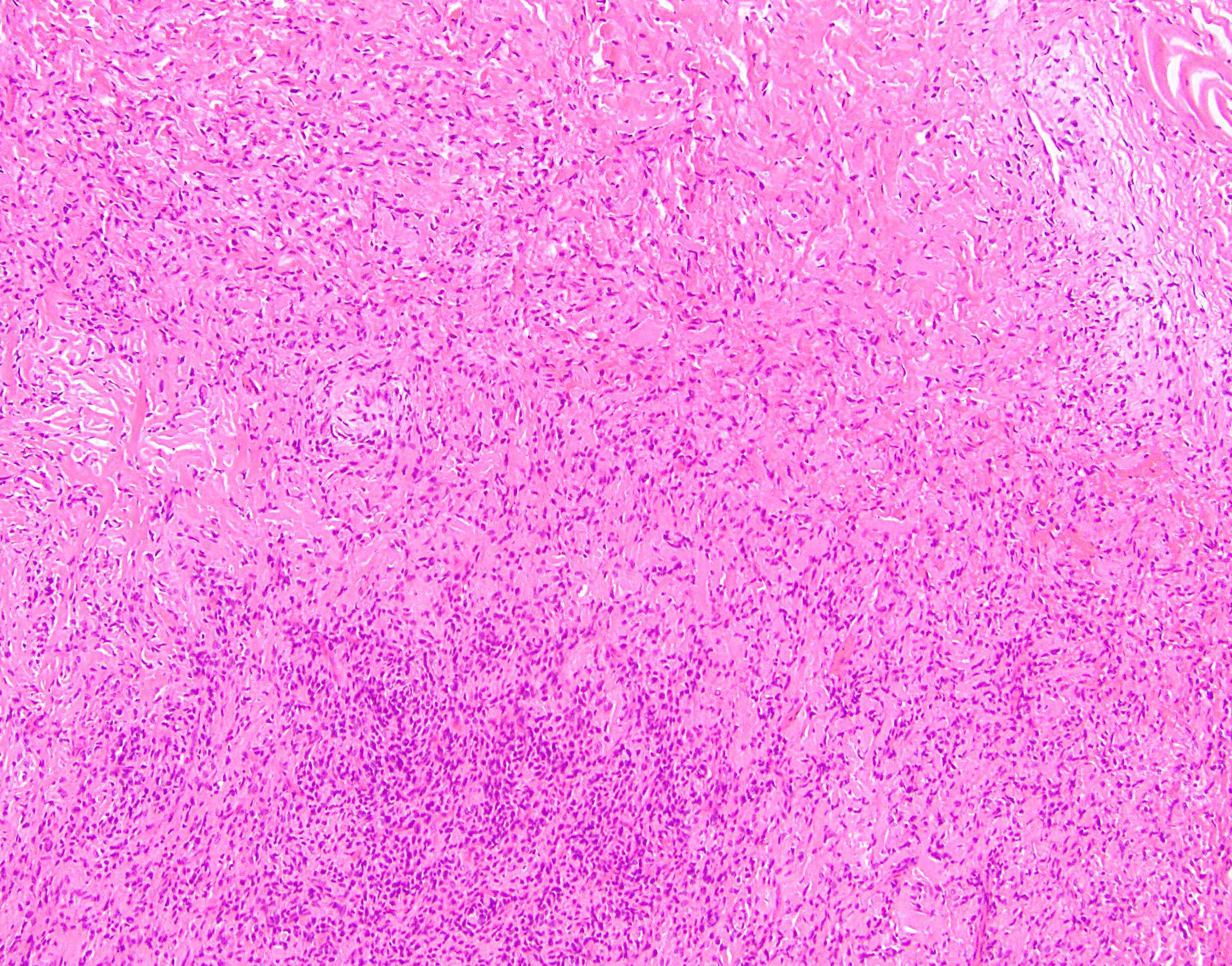
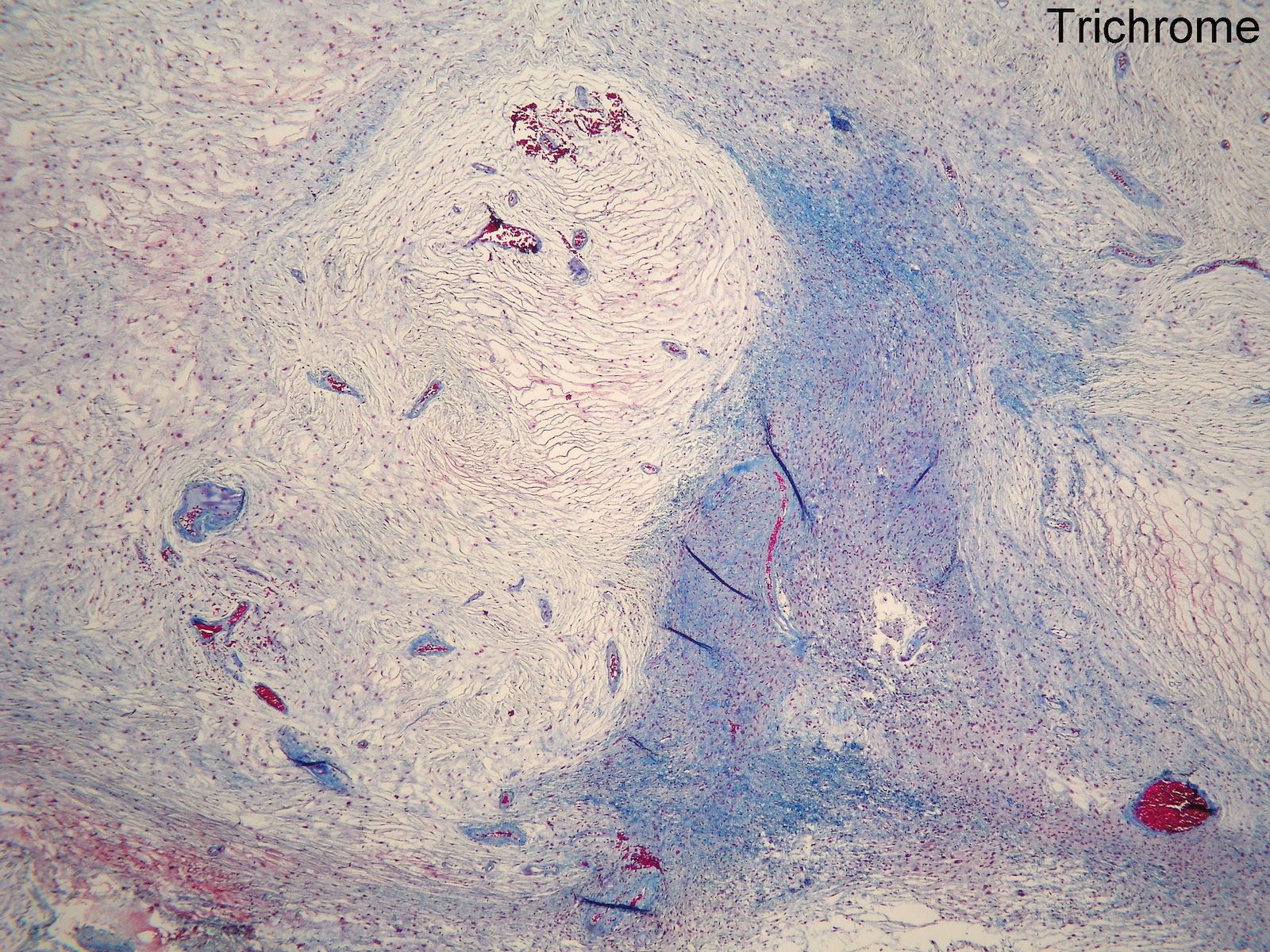
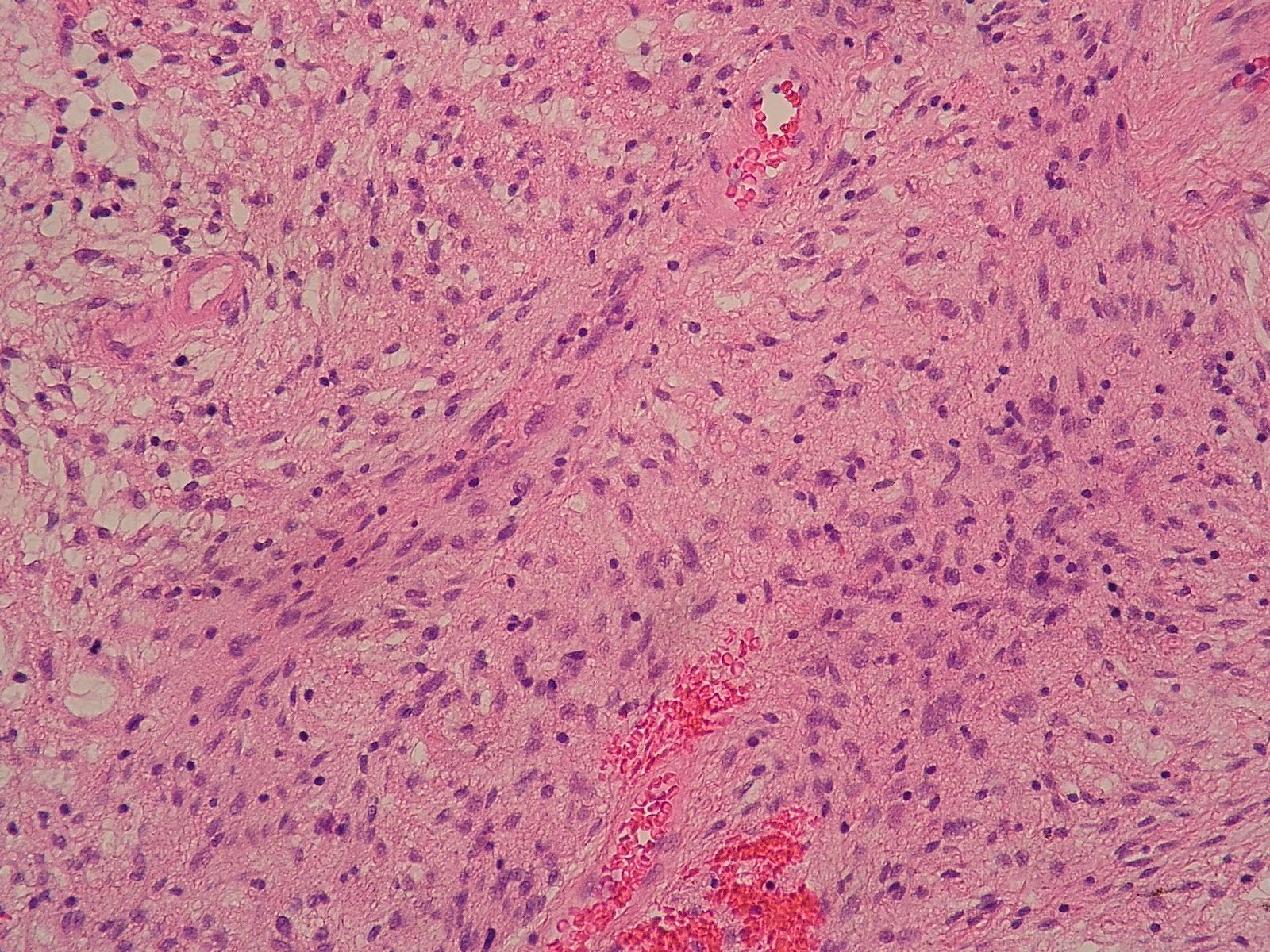
- Low grade sarcoma with fibrous and myxoid areas, whorled growth pattern, low cellularity, bland fibroblastic cells and curvilinear or arcuate vessels
Essential features
- Bland sarcoma that can metastasize after years to decades
- Characteristically expresses MUC4 and has a t(7;16)(q32-34;p11) FUS-CREB3L2 fusion
- Likely closely related to sclerosing epithelioid fibrosarcoma, with case reports of same translocation, cases with intermixed histology and both tumors often express MUC4 immunohistochemically (Am J Surg Pathol 2007;31:1387, Ann Diagn Pathol 2011:15:303, Am J Surg Pathol 2012;36:1444)
- First described by Evans in 1987; with increasing awareness, less rare than originally believed (Am J Clin Pathol 1987;88:615)
Terminology
- Also called Evans tumor, hyalinizing spindle cell tumor with giant rosettes (a unique morphologic pattern seen in some low grade fibromyxoid sarcomas) (Am J Surg Pathol 2003;27:1229)
Epidemiology
- Usually occurs in young to middle aged adults (median age 34 years, range 3 - 78 years)
- Slight male predominance
Sites
- Trunk and deep extremities (thigh most common site), also intrathoracic (Hum Pathol 2008;39:623)
- Rarely in retroperitoneum and mediastinum
Clinical features
- Prolonged preclinical stage
- Slow growing, painless soft tissue mass (1 - 18 cm)
- Earlier studies suggested only a small subset metastasized but a more recent study with long term follow up reported recurrence in 64%, metastasis in 45%, death from disease in 42%; patients with positive / uncertain margins more likely to have recurrence (up to 15 years later; median 3.5 years); metastases usually to lungs, pleura, chest wall (up to 45 years later; median 5 years) (Am J Surg Pathol 2011;35:1450)
Radiology description
- Multinodular, with alternating strongly and weakly enhancing areas (Skeletal Radiol 2012;41:1263)
Prognostic factors
- Neither the presence of focal intermediate to high grade sarcoma nor histologic features affect prognosis; however, a dedifferentiated recurrence (anaplastic round cell morphology with numerous mitoses) portends short survival (Am J Surg Pathol 2000;24:1353, Am J Surg Pathol 2011;35:1450)
- Superficially located tumors may be more common than previously recognized, may have a better prognosis and may be more common in pediatric patients (Am J Surg Pathol 2005;29:204)
- Small tumors less than 3.5 cm may have better prognosis (Am J Surg Pathol 2011;35:1450)
Case reports
- 12 year old girl with massive tumor of chest cavity (Pediatr Radiol 2009;39:396)
- 37 year old man with tumor of falciform ligament (BMC Surg 2003 Sep 24;3:7)
- 44 year old woman with tumor on epicardial surface of heart (Hum Pathol 2008;39:623)
Treatment
- Complete excision with wide margins
- Resection of pulmonary metastases (metastasectomy) may be considered
- Long term clinical follow up is prudent, due to potential of very late recurrence or metastasis (decades after initial diagnosis)
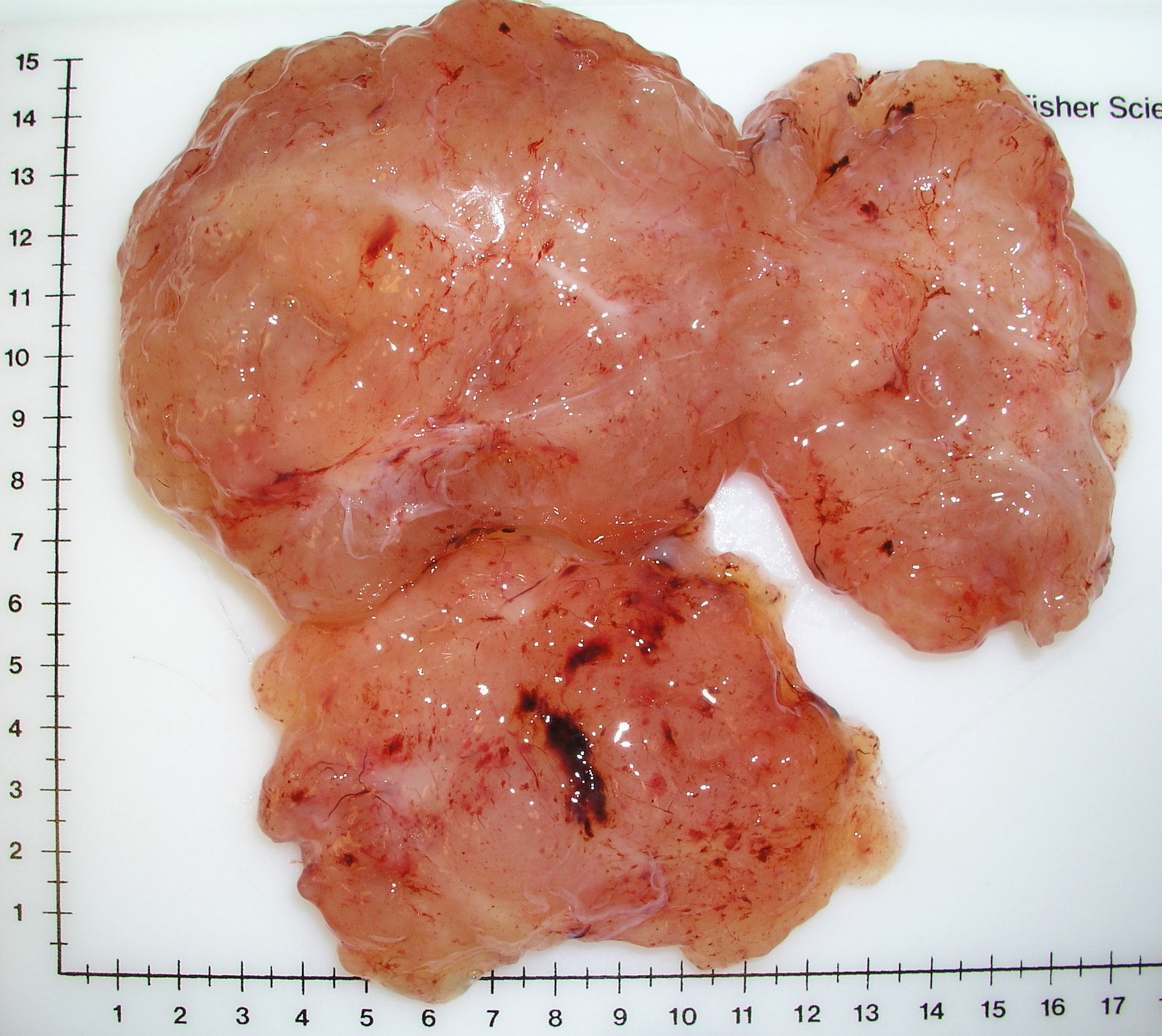
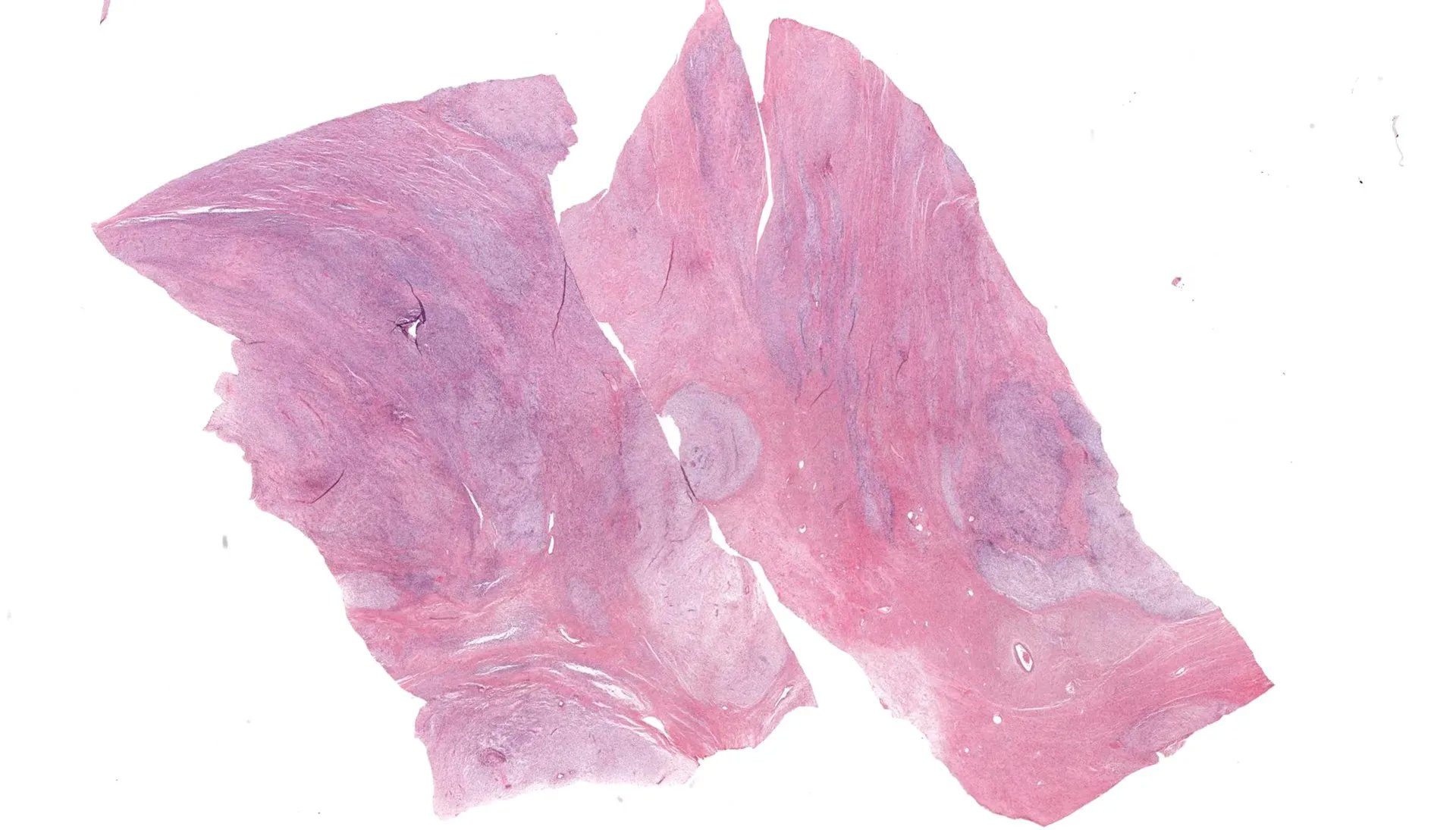
Gross description
- Often large (median ~9 cm), well circumscribed, fibromyxoid cut surface, may be grossly infiltrative
Gross images
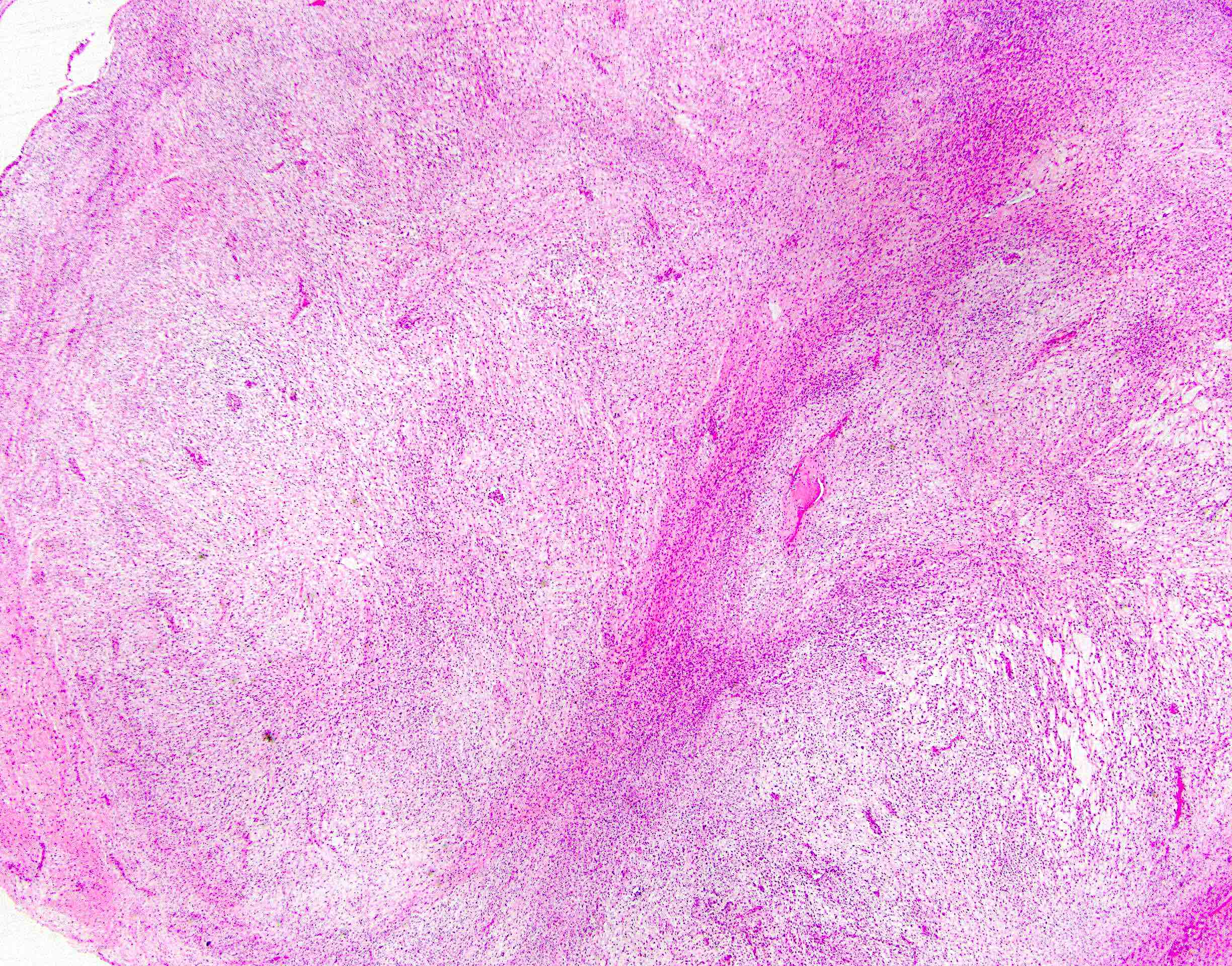
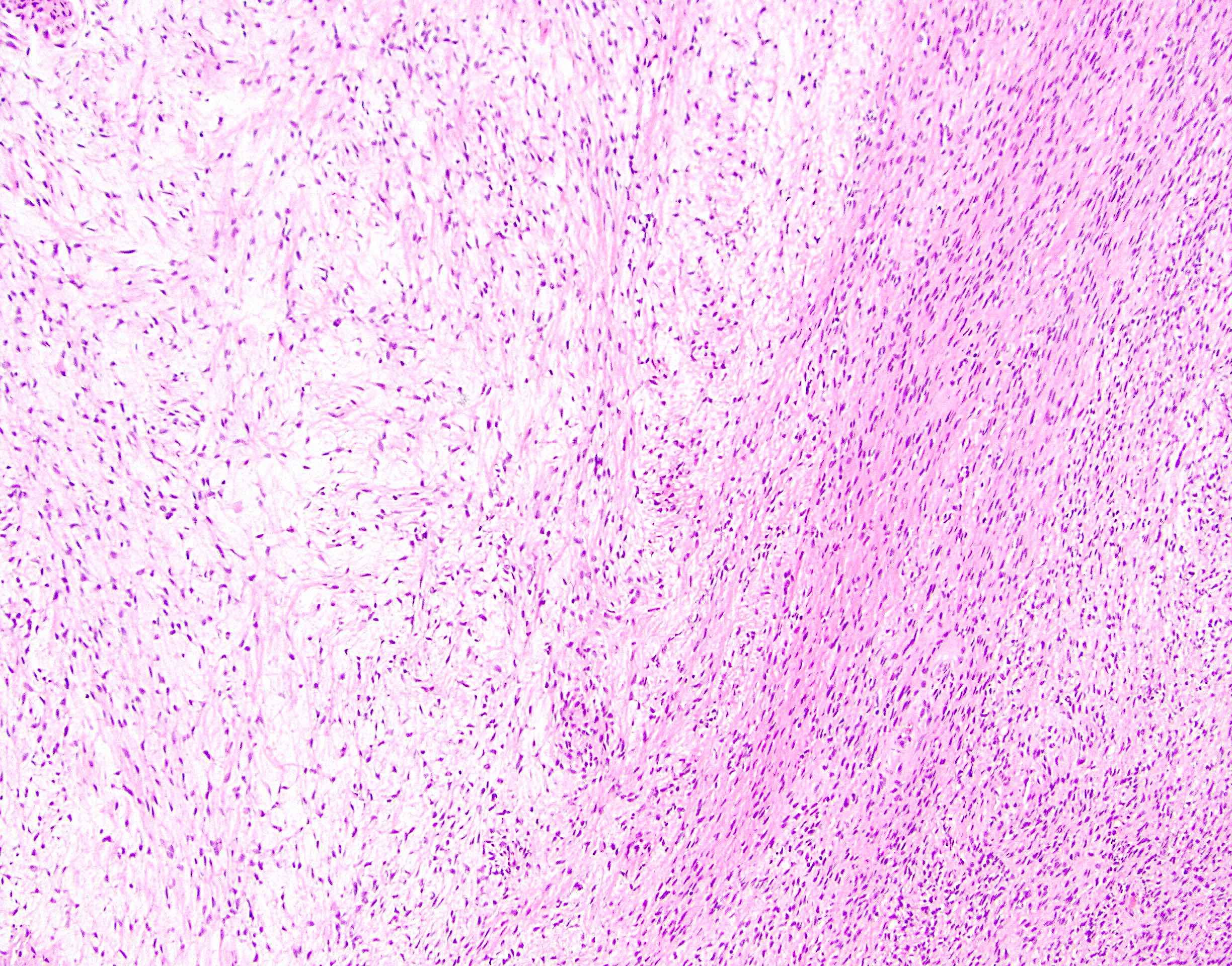
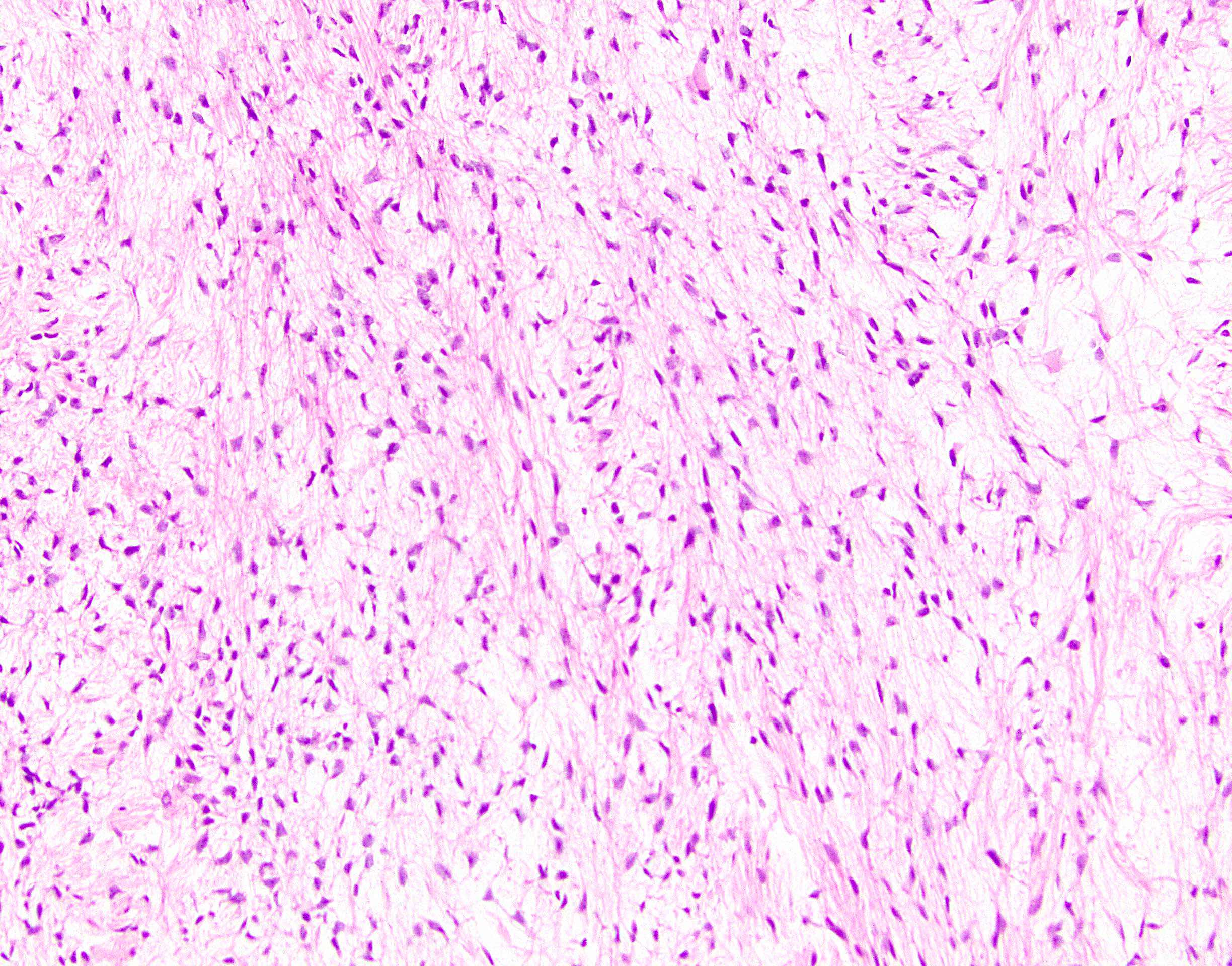
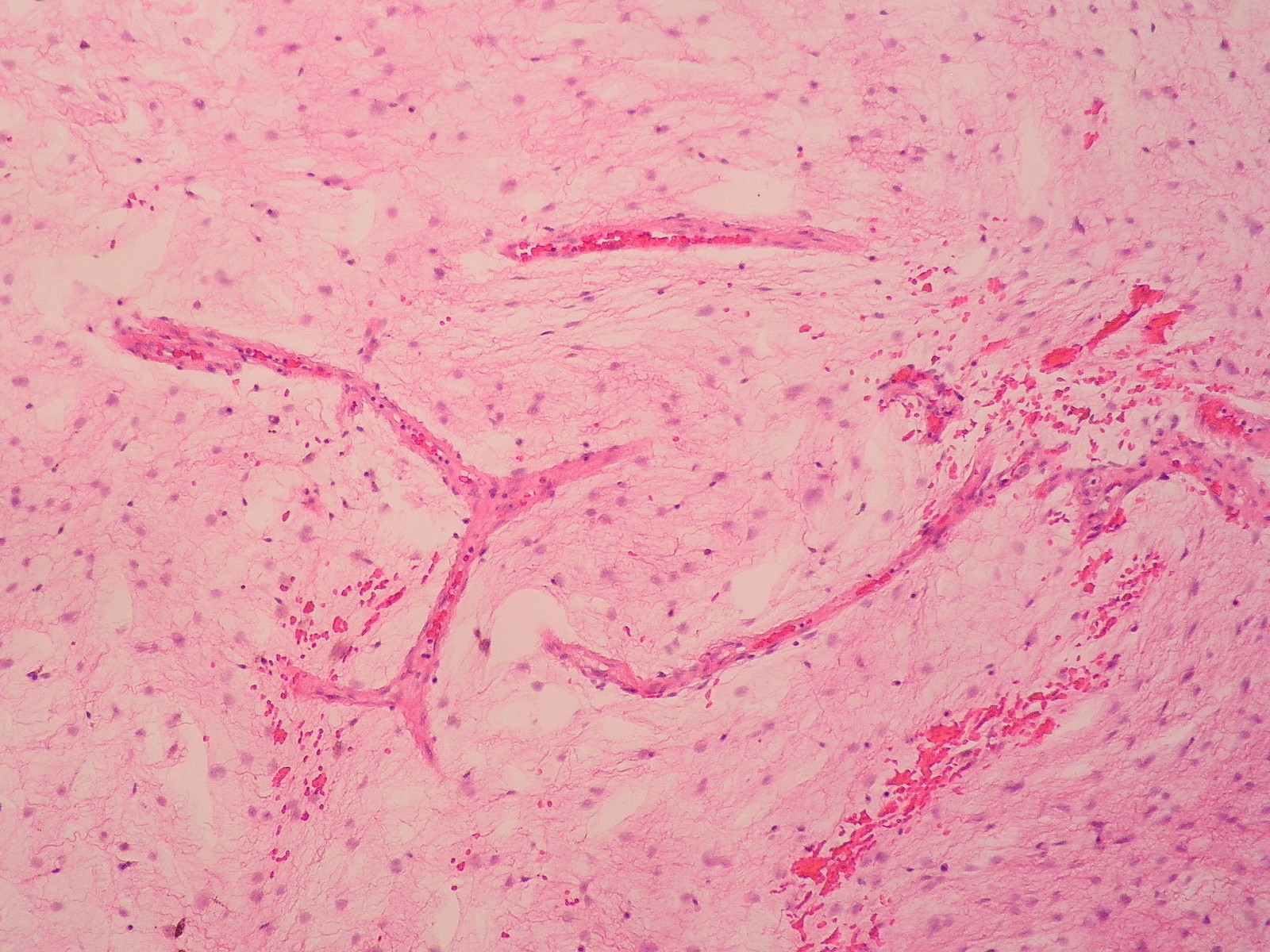
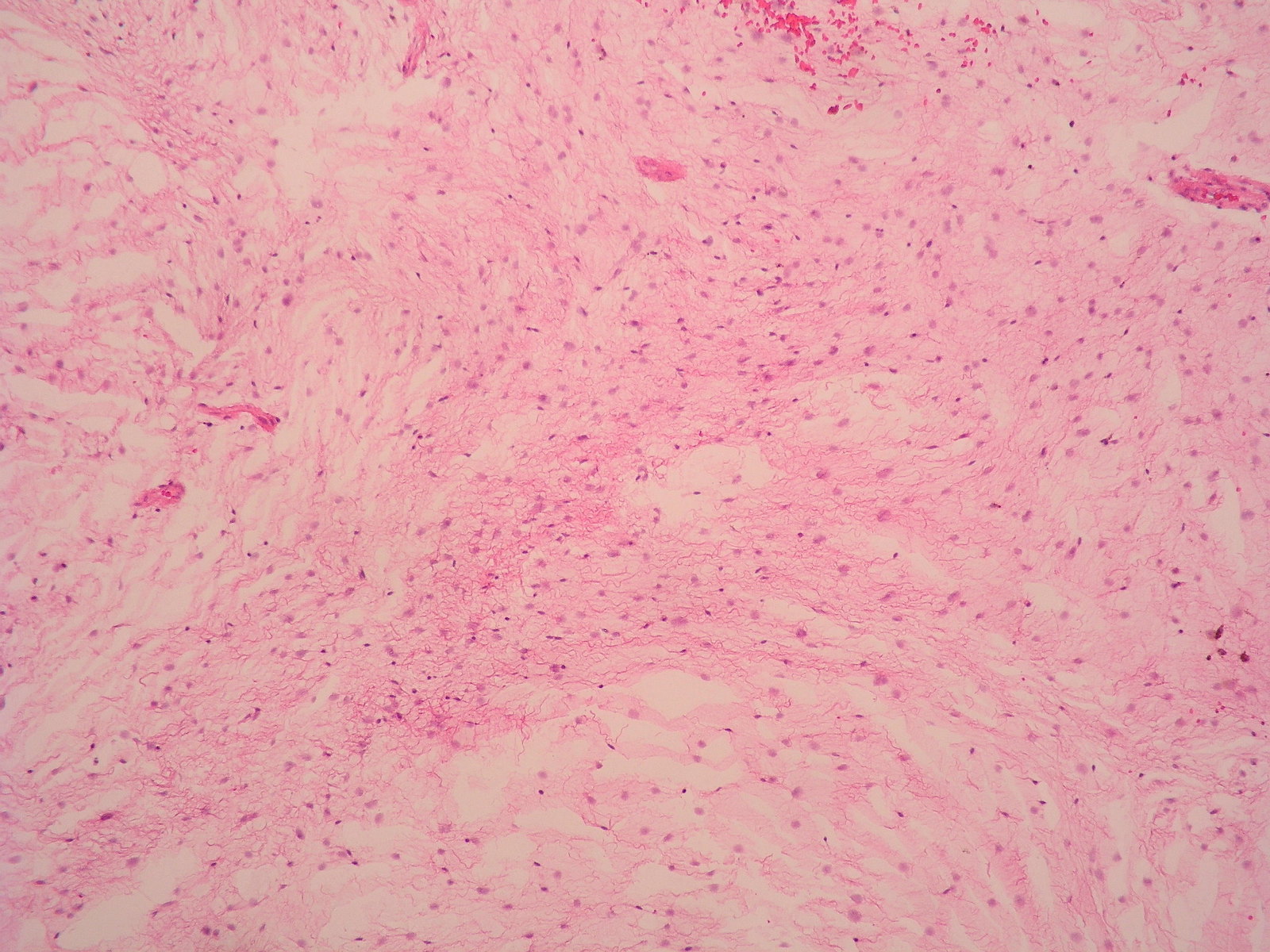
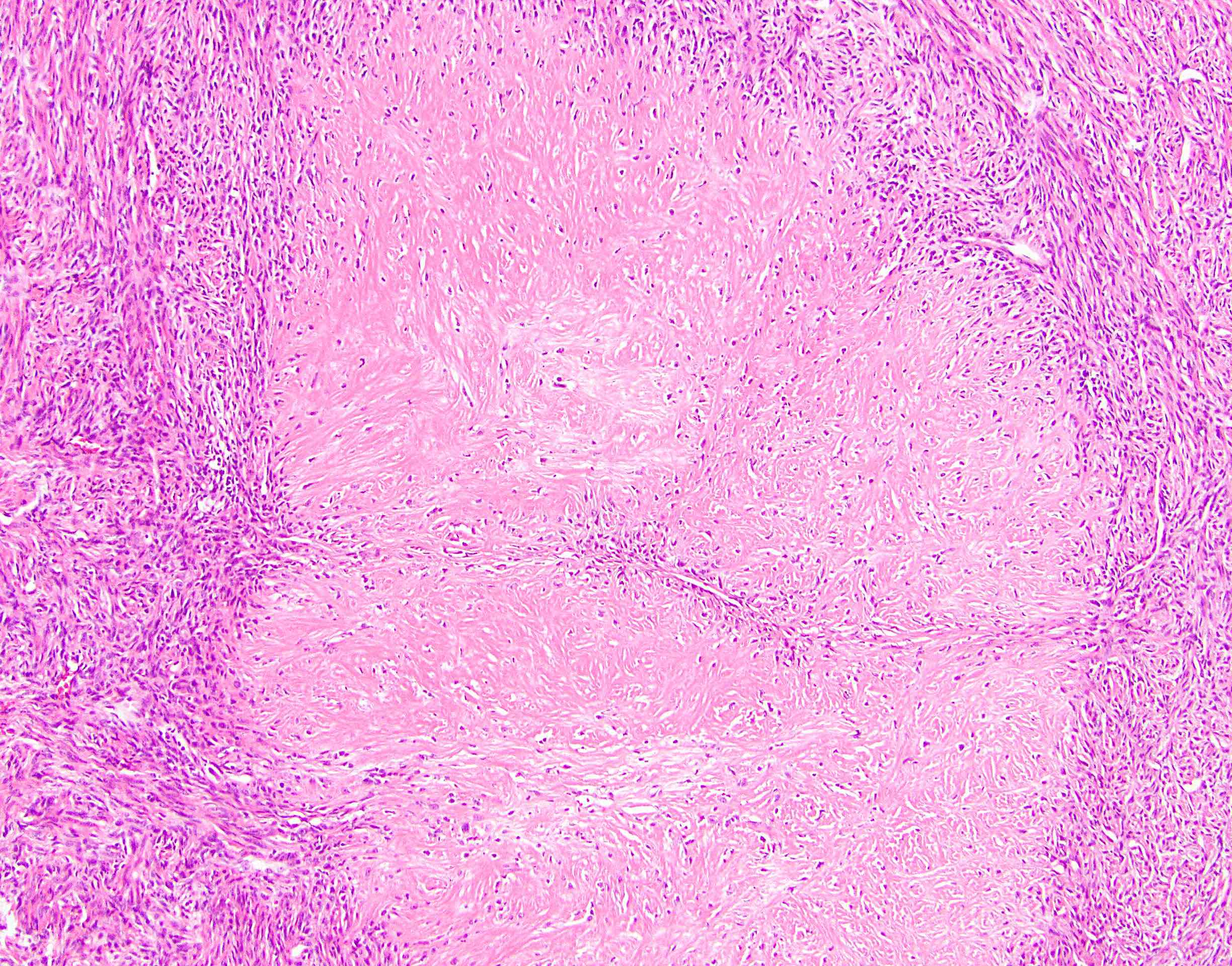
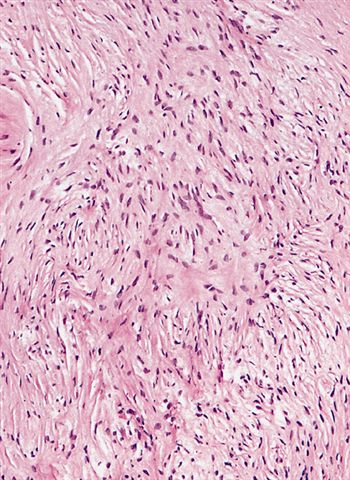
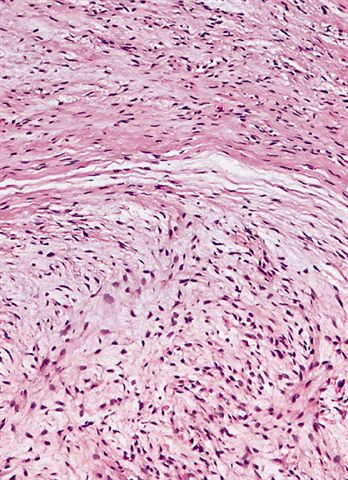
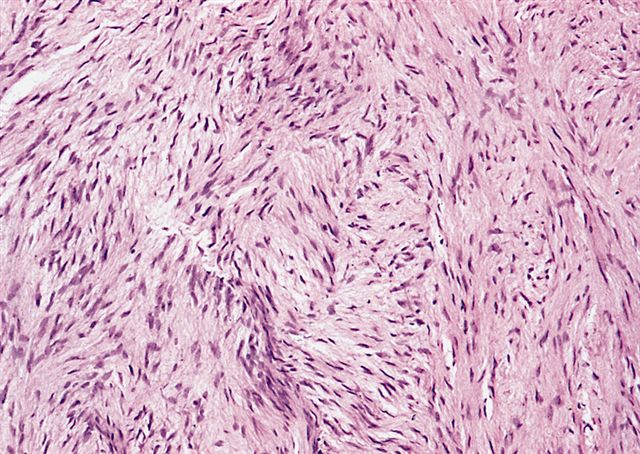
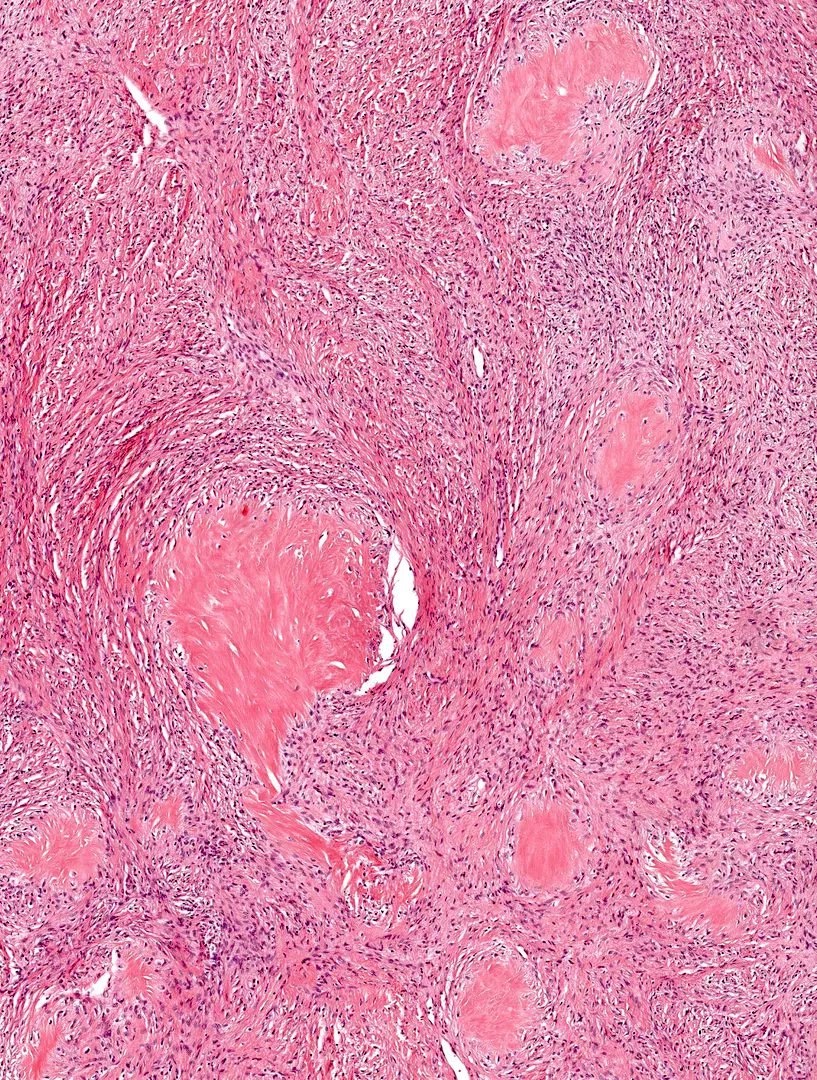
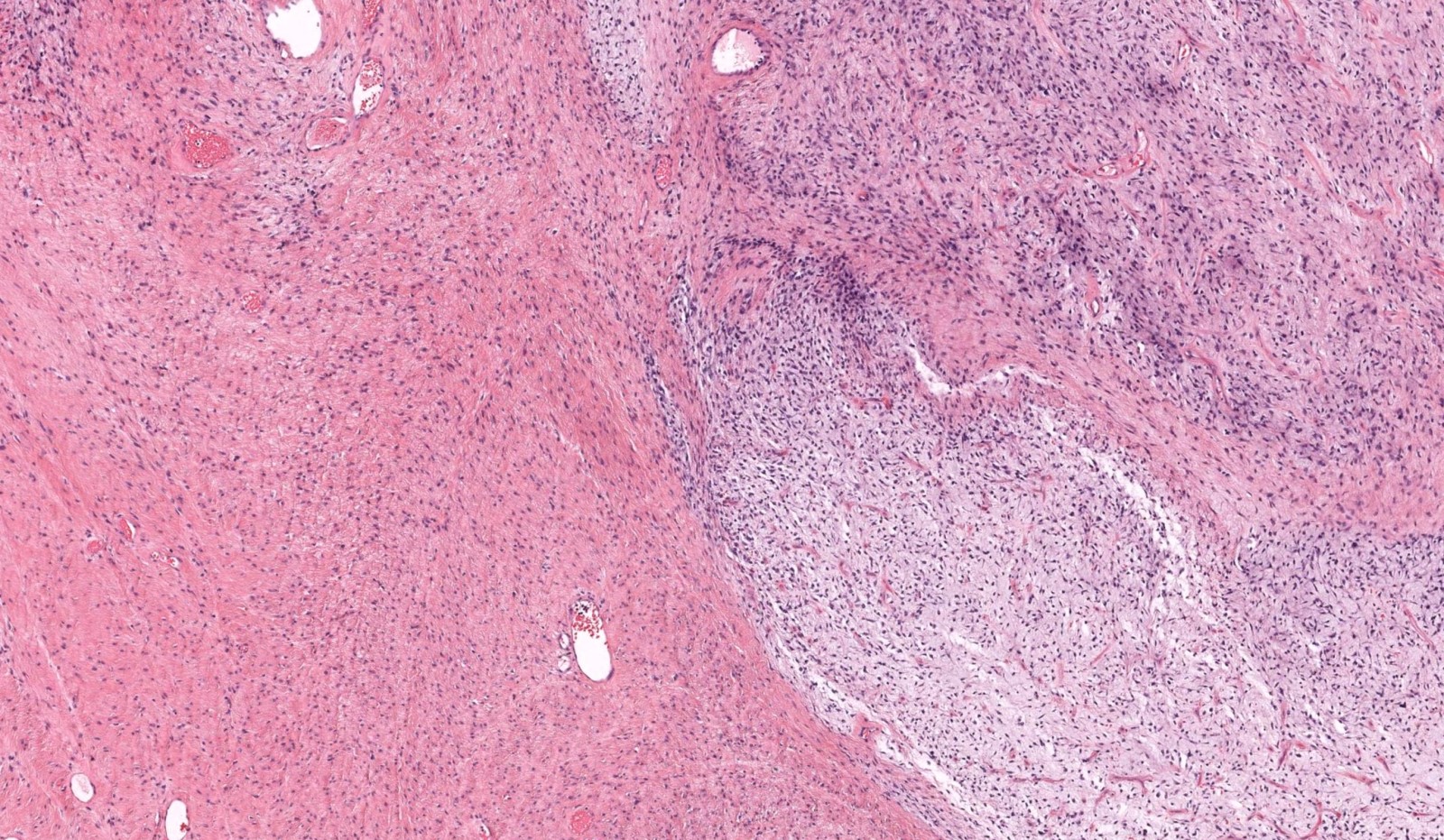
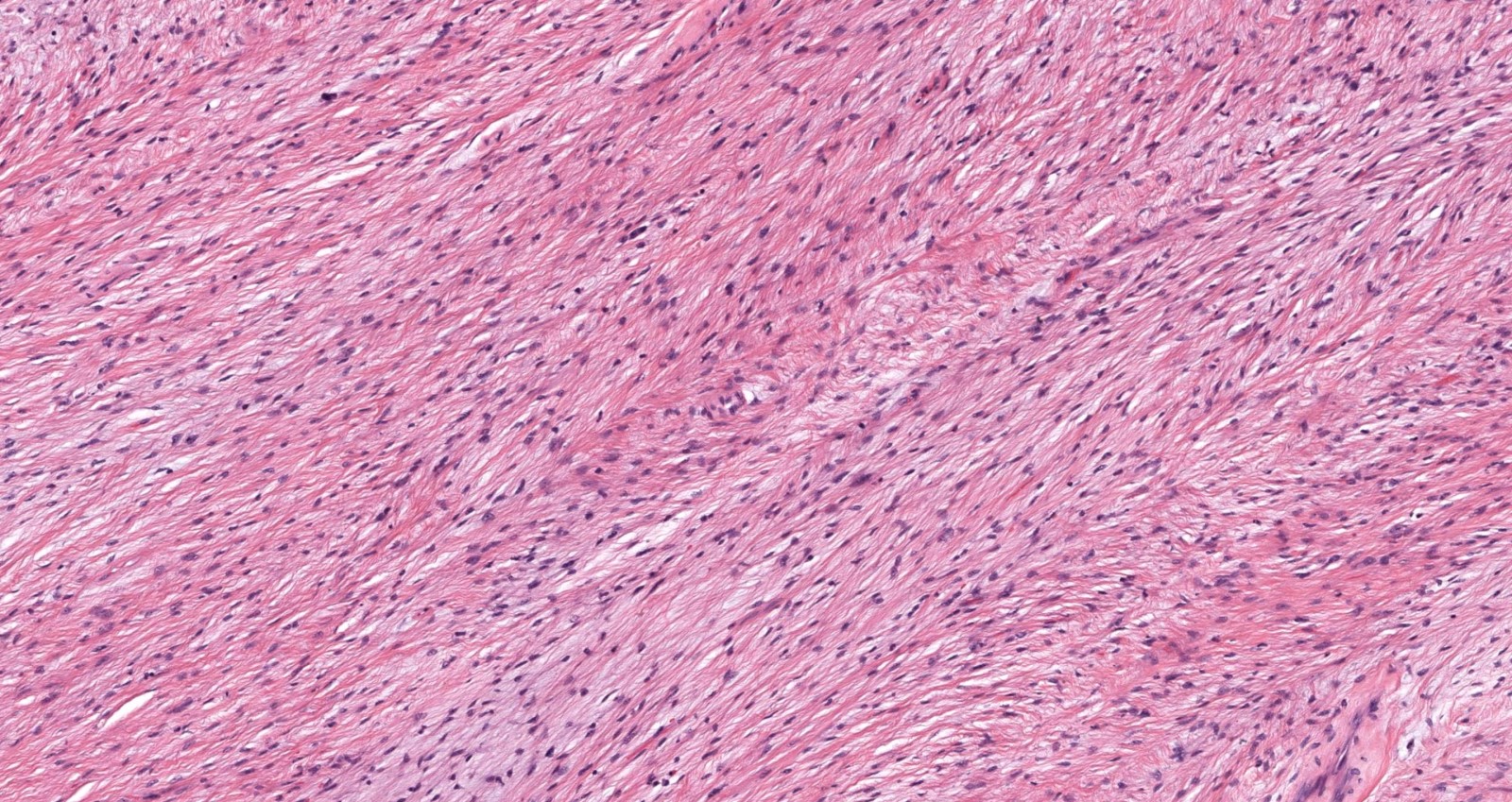
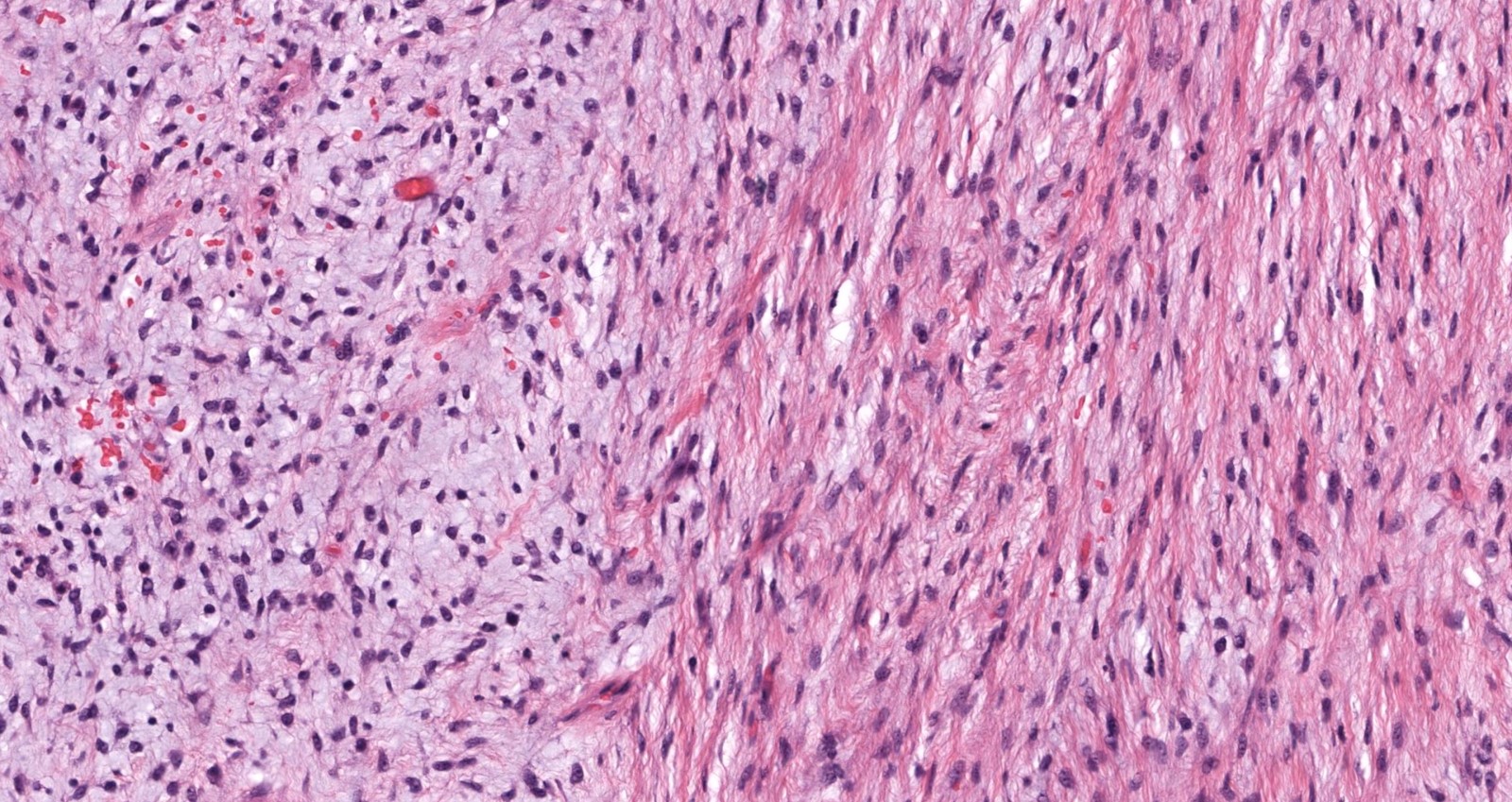
Microscopic (histologic) description
- Low to moderately cellular, bland fusiform or spindled cells with focal to diffuse whirling in heavily collagenized stroma with abrupt transition to myxoid areas
- 45% have epithelioid areas
- 40% contain poorly formed but large collagen rosettes
- Often infiltrates adjacent skeletal muscle
- Occasionally has areas of increased cellularity, atypia, necrosis or mitotic activity characteristic of intermediate to high grade sarcoma
- Recurrences may show increased cellularity and mitotic activity
Microscopic (histologic) images
Cytology description
- Cellular with spindle cells containing scant wispy cytoplasm, uniform elongated nuclei, small inconspicuous nucleoli
- Prominent myxoid background
- No significant nuclear pleomorphism or mitoses (Acta Cytol 2006;50:208, Cancer 1999;87:75)
- Cannot diagnose based only on cytomorphology (Cytopathology 2009;20:304)
Cytology images
Positive stains
- MUC4 highly sensitive (100%) and specific (Am J Surg Pathol 2011;35:733)
- CD99 (90%), BCL2 (90%), EMA, vimentin (very nonspecific) (Am J Surg Pathol 2007;31:1387)
Negative stains
- S100, desmin, keratin, CD34, MDM2, smooth muscle actin, h-caldesmon, CD117, nuclear beta catenin, DOG1
Electron microscopy description
- Fibroblastic differentiation
Molecular / cytogenetics description
- t(7;16)(q32-34;p11) FUS-CREB3L2 fusion in 90% or more, alternate translocation t(11;16)(p11;p11) FUS-CREB3L1 fusion by RT-PCR or FISH (Lab Invest 2005;85:408, Am J Surg Pathol 2006;30:1077, Am J Surg Pathol 2007;31:1387, Diagn Mol Pathol 2008;17:237, Am J Surg Pathol 2008;32:8, Am J Dermatopathol 2011;33:140)
Sample pathology report
- Soft tissue, left thigh, resection:
- Low grade fibromyxoid sarcoma (8.3 cm) (see comment)
- Margins of resection unremarkable.
- Comment: This uncommon soft tissue tumor requires long follow up, as it sometimes metastasizes many years after initial presentation. An immunohistochemical stain for MUC4 is positive.
Differential diagnosis
- Desmoid type fibromatosis:
- Usually lacks myxoid areas (sometimes can be myxoid, though), fibrous cells are aligned in broad sweeping fascicles, straighter, cells appear more like reactive fibroblasts, distinct ectatic vessels present, diffuse or occasionally focal nuclear beta catenin staining (Am J Surg Pathol 2005;29:653)
- Fibrosarcoma:
- No myxoid component; herringbone fascicular pattern, a diagnosis of exclusion that should be made with much hesitation (Histopathology 2006;49:152)
- Myxofibrosarcoma:
- More myxoid and less fibrous, more nuclear pleomorphism and hyperchromatism (in contrast to low grade fibromyxoid sarcoma, which is almost always bland and monomorphic with little to no pleomorphism), more developed vascular network, tumor cells aggregate around vessels (Histopathology 2004;45:29)
- Myxoid neurofibroma:
- Wavy nuclei, background of thick collagen bundles, S100+
- Nodular fasciitis:
- Tissue culture histology, extravasated erythrocytes, myxoid cystic degeneration
Additional references
Board review style question #1
Board review style answer #1
B. It has a characteristic gene fusion - t(7;16)(q32-34;p11) FUS-CREB3L2
Comment Here
Reference: Low grade fibromyxoid sarcoma
Comment Here
Reference: Low grade fibromyxoid sarcoma
Board review style question #2
Which of the following immunohistochemical stains is considered sensitive and specific for low grade fibromyxoid sarcoma?
- h-caldesmon
- MNF116
- MUC4
- TLE1
Board review style answer #2