Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alexiev B. Leiomyosarcoma-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueleiomyosarcoma.html. Accessed December 22nd, 2024.
Definition / general
- Leiomyosarcoma (LMS) is a malignant mesenchymal tumor showing smooth muscle differentiation (J Clin Oncol 2018;36:144)
Essential features
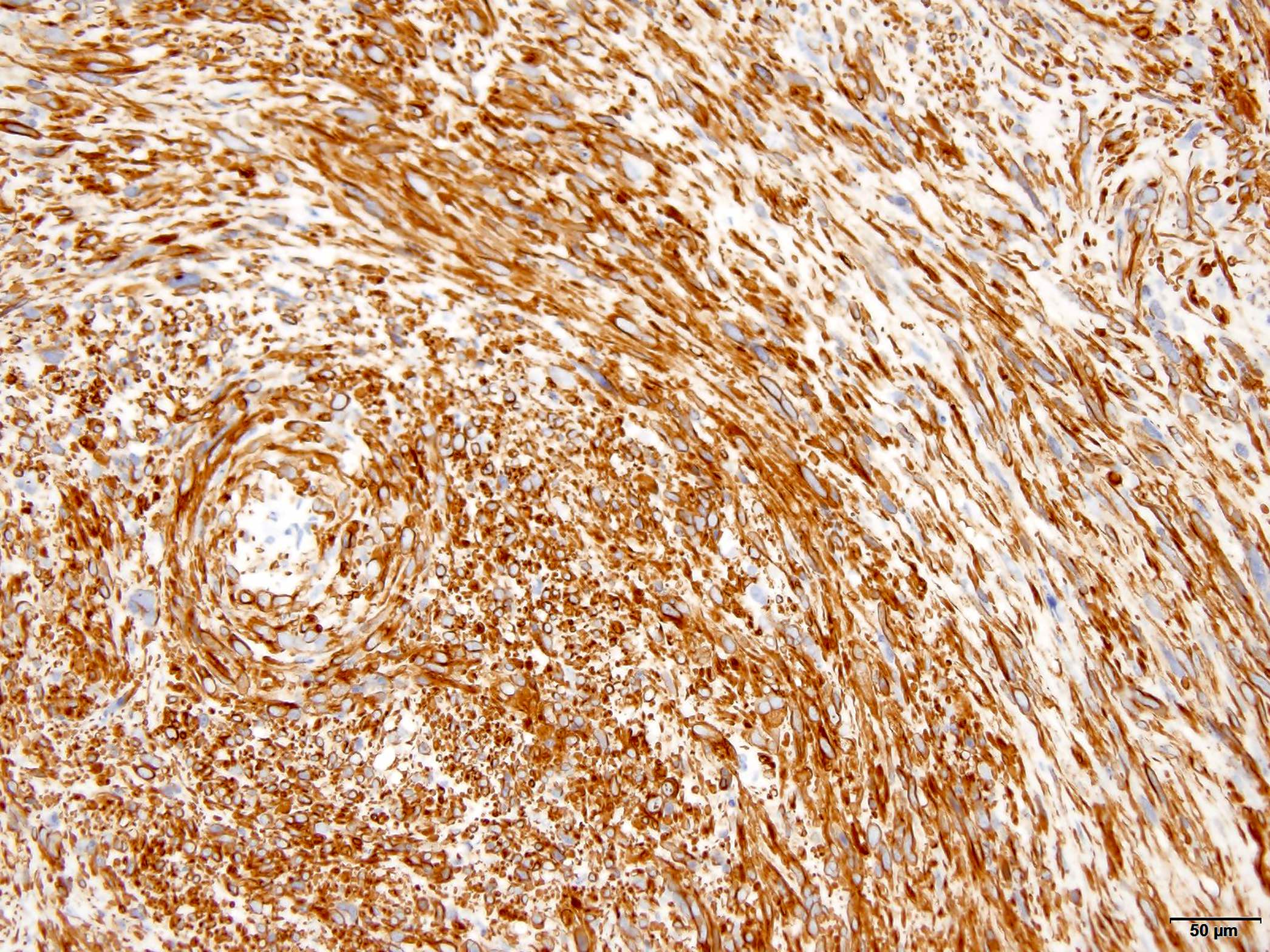
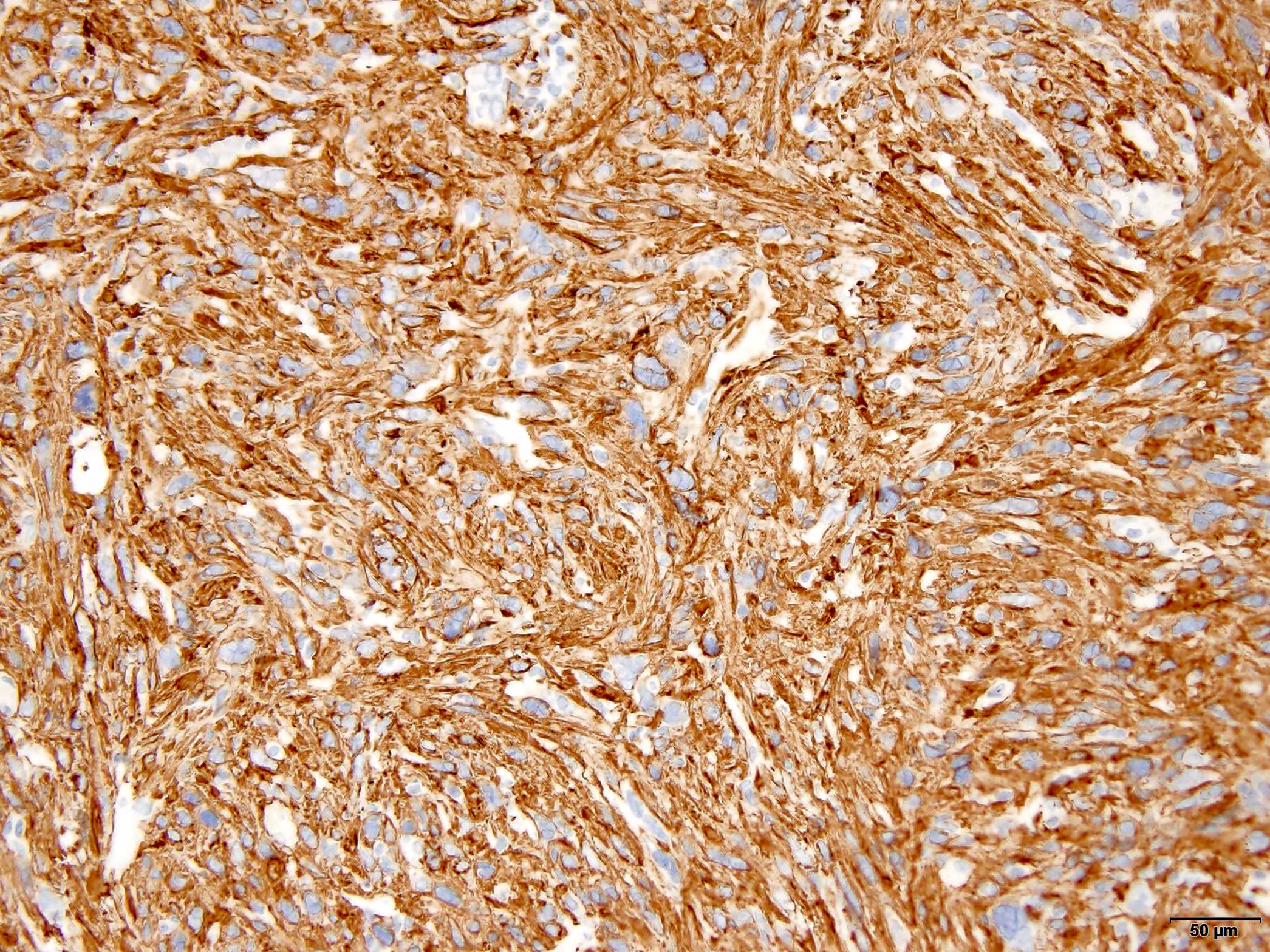
- Fascicles of eosinophilic spindled cells with blunt ended nuclei showing variable pleomorphism (Cancer 1981;48:1022, Am J Surg Pathol 2002;26:14)
- Immunostaining for SMA, MSA, desmin or h-caldesmon
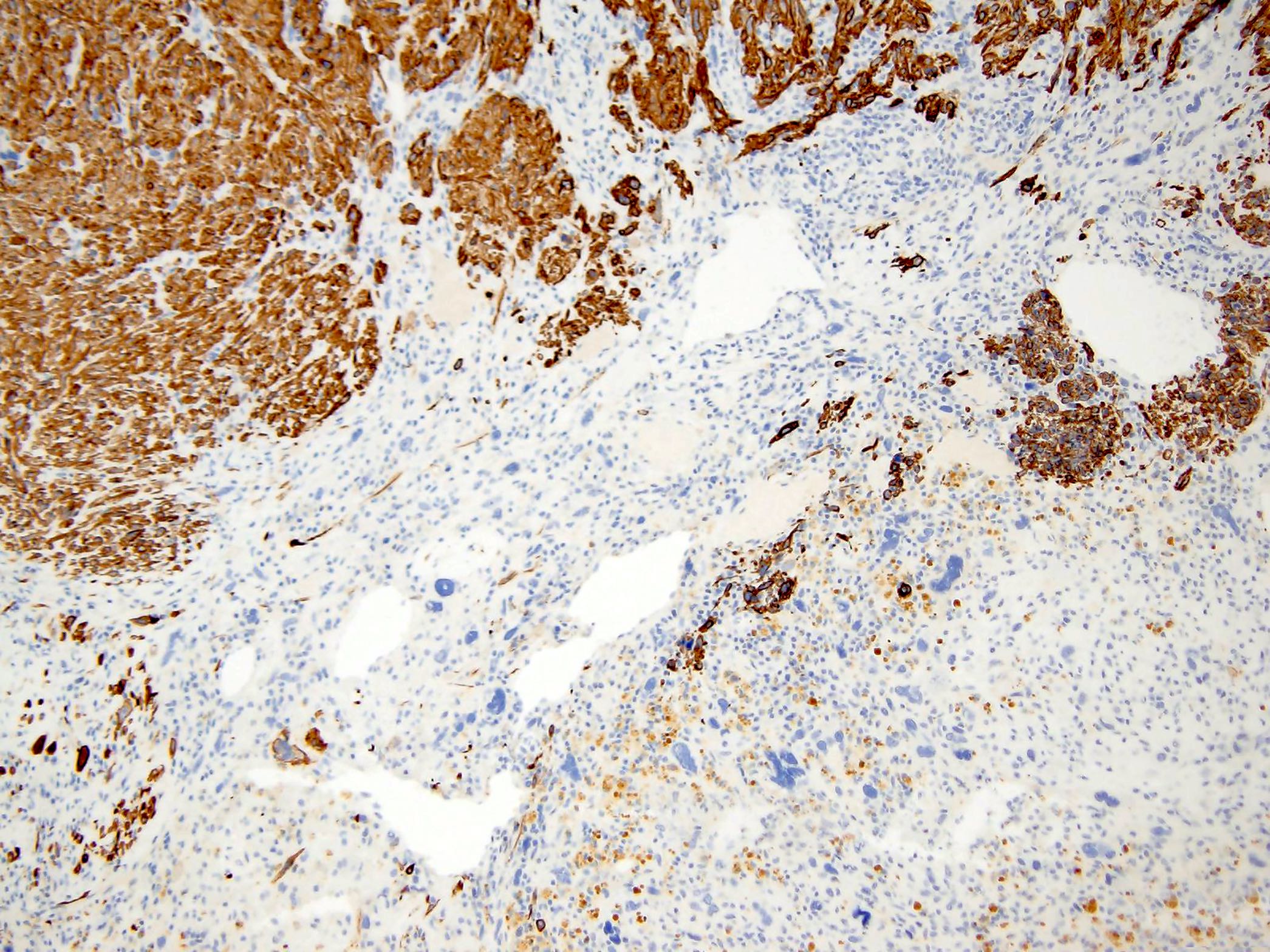
- Dedifferentiated areas lack expression of myogenic markers (Histopathology 2011;59:1135)
- Clinically aggressive neoplasms with frequent local recurrences and distant metastases
ICD coding
- ICD-O: 8890/3 - leiomyosarcoma, NOS
- ICD-11:
- 2B58.0 & XH7ED4 - leiomyosarcoma of retroperitoneum or peritoneum & leiomyosarcoma, NOS
- 2B58.Y & XH7ED4 - leiomyosarcoma, other specified primary site & leiomyosarcoma, NOS
- 2B58.Z & XH7ED4 - leiomyosarcoma, unspecified primary site & leiomyosarcoma, NOS
Epidemiology
- Leiomyosarcoma is one of the most common subtypes of malignant mesenchymal neoplasms and represents ~10 - 20% of all newly diagnosed soft tissue sarcomas (J Clin Oncol 2018;36:144)
- Overall incidence of leiomyosarcoma increases with age and peaks at the seventh decade of life
- Sex predilection greatly depends on tumor location, with women comprising a clear majority of patients with retroperitoneal and inferior vena cava leiomyosarcoma and men showing a slight predominance in noncutaneous soft tissue sites
Sites
- Most commonly arise in the extremities, retroperitoneum, abdomen / pelvis and trunk (Ann Surg Oncol 2013;20:1851, Cancer 1981;48:1022)
- A distinctive subgroup originates in large blood vessels, most commonly the inferior vena cava (Cancer 1986;57:1395, Am J Surg Pathol 2002;26:14)
Pathophysiology
- Leiomyosarcoma belongs to the group of soft tissue sarcomas with complex and unbalanced karyotypes, which results in severe genomic instability (J Clin Oncol 2018;36:144)
- Some of the most common changes in leiomyosarcoma occur in the form of loss in chromosomes 10q(PTEN) and 13q (RB1) and gain at 17p (TP53)
Etiology
- There is no definite, identifiable, causative factor for leiomyosarcoma
- Prior history of radiotherapy, which is one of the most significant risk factors for development of soft tissue sarcomas, can also lead to the development of leiomyosarcoma (J Natl Cancer Inst 1988;80:233)
- Patients with genetic syndromes like hereditary retinoblastoma (RB1 gene deletion) and Li-Fraumeni syndrome (mutation in the TP53 gene) can develop leiomyosarcoma, amongst other soft tissue sarcomas (J Clin Oncol 2018;36:144)
Clinical features
- Clinical presentation of leiomyosarcoma, as with other soft tissue sarcomas, is often associated with nonspecific symptoms caused by the displacement of structures, rather than invasion, in specific anatomic locations of the primary tumor and its metastases (J Clin Oncol 2018;36:144)
Diagnosis
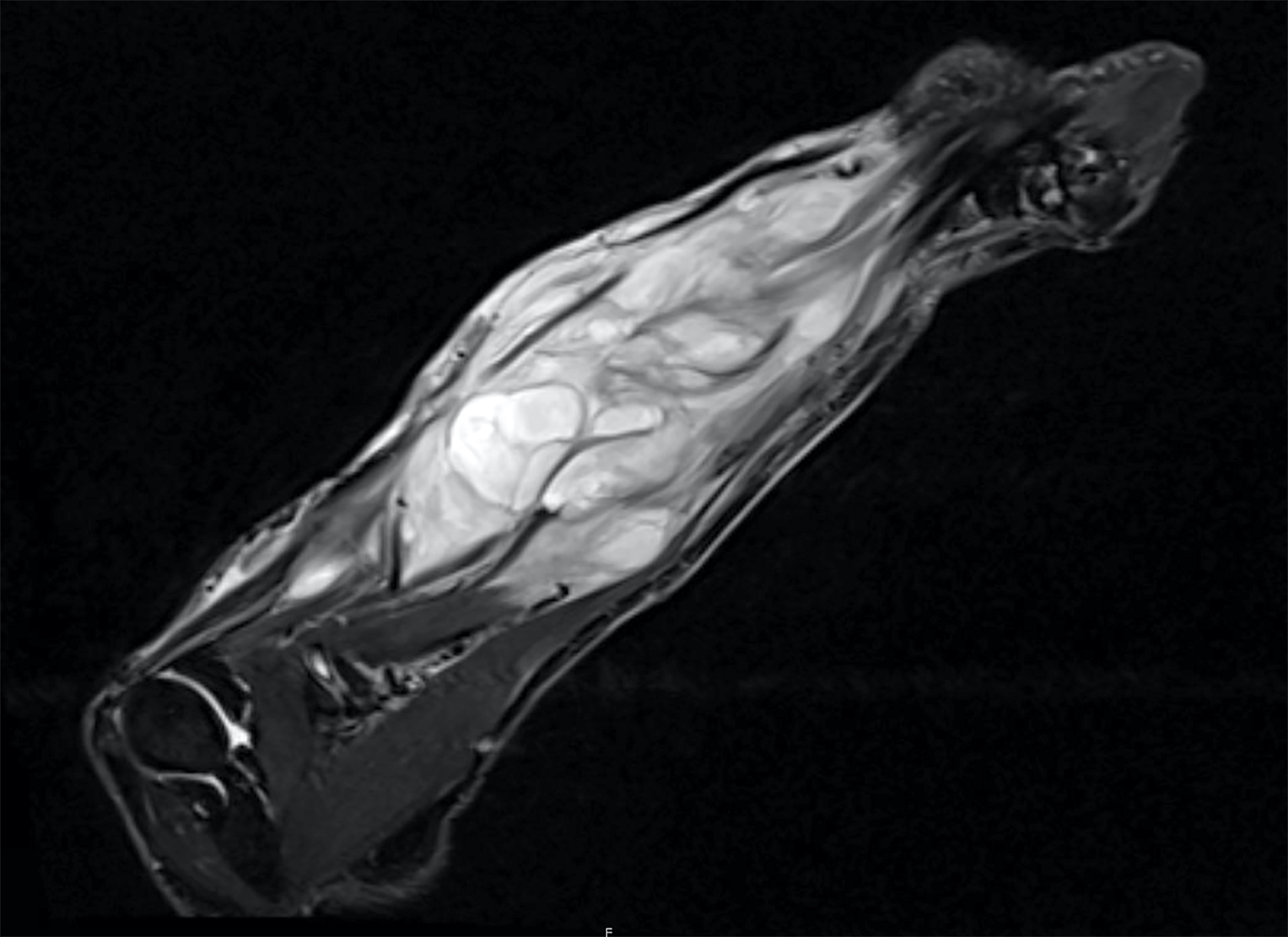
- Imaging approaches include magnetic resonance imaging (MRI) in soft tissue extremity / truncal tumors and contrast enhanced computed tomography (CT) scan for retroperitoneal lesions
- Chest and abdominal CT scans are required in the initial workup, as hematogenous spread is a frequent event in leiomyosarcoma, with the lung and liver as 2 common sites of metastases (AJR Am J Roentgenol 1988;150:615)
- Pretreatment biopsy is mandatory in extrauterine sites, with core biopsy as the preferred technique (J Clin Oncol 2018;36:144)
- Detailed pathologic evaluation is typically performed after complete resection
- Fine needle aspiration is inadequate to establish a diagnosis (J Surg Oncol 2010;102:523)
Laboratory
- There is no laboratory test that is diagnostic of leiomyosarcoma (J Clin Oncol 2018;36:144)
Radiology description
- CT findings (Radiology 1984;152:133)
- Generally heterogeneous
- Commonly demonstrate central low attenuation representing necrosis
- Calcification exceedingly rare
- MRI findings (Diagn Interv Radiol 2015;21:4)
- T1: isointense to muscle
- T2 non-fat suppressed: intermediate to hypointense to neighboring fat
- T2 FS: predominantly hyperintense
Prognostic factors
- Histologic grade, tumor size and tumor depth are the 3 major clinicopathologic prognostic factors for soft tissue sarcomas, including leiomyosarcoma (Cancer 2001;91:1914, J Clin Oncol 1996;14:1679)
- Leiomyosarcoma should be staged using the TNM staging for soft tissue tumors of the AJCC and UICC (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017, Brierley: TNM Classification of Malignant Tumours, 8th Edition, 2017)
- Leiomyosarcoma has substantial intrinsic aggressiveness and is one of the sarcoma subtypes with the highest risk of distant recurrence and decreased disease specific survival (Cancer 2001;91:1914)
- Retroperitoneal leiomyosarcoma and leiomyosarcoma of large vessels tend to have a poor prognosis
- Metastases most commonly occur in lung, liver and soft tissue (Ann Surg Oncol 2013;20:1851, Cancer 1981;48:1022)
- Leiomyosarcoma is the most common sarcoma to produce skin metastases (Cancer 2012;118:2900)
- Overall 5 year survival: 68% (J Surg Orthop Adv 2012;21:96)
Case reports
- 41 year old woman with leiomyosarcoma originating from the mesenteric vein (Surg Case Rep 2022;8:147)
- 65 year old woman with leiomyosarcoma of the peritoneal cavity (Rare Tumors 2014;6:5165)
- 68 year old woman with leiomyosarcoma of the mesentery (Cureus 2020;12:e10777)
- 73 year old man with leiomyosarcoma of the tonsil (J Laryngol Otol 2011;125:869)
- 78 year old man with leiomyosarcoma of external deep soft tissue (Arch Pathol Lab Med 2002;126:481)
Treatment
- Staging of soft tissue sarcomas, including leiomyosarcoma, is important in guiding treatment
- Leiomyosarcoma should be staged using the TNM staging for soft tissue tumors of the AJCC and UICC (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017, Brierley: TNM Classification of Malignant Tumours, 8th Edition, 2017)
- Treatment is best carried out in a specialized center with expertise in sarcoma care (Surg Oncol Clin N Am 2022;31:527)
- Treatment planning begins with a multidisciplinary review of the patient’s history, all available radiographic images and the pathologic results from biopsy
- Treatment plan is formulated upon the input from orthopedic and general surgeons, musculoskeletal radiologists, pathologists, medical oncologists and radiation oncologists
- Goal of treatment is to control the symptoms, decrease tumor bulk and prolong survival (J Clin Oncol 2018;36:144)
- Surgery (Adv Surg 2015;49:107)
- Local control of soft tissue leiomyosarcoma is usually achieved with surgical resection
- Achieving wide surgical margins is important in preventing local recurrence
- Radiation therapy
- Radiation therapy is an important additional treatment for improving rates of local control
- Many tumors involve or are directly adjacent to vital structures and in these cases achieving a wide surgical margin is impossible
- Radiation therapy can be delivered either preoperatively (neoadjuvant) or postoperatively (adjuvant)
- Perioperative radiation therapy for soft tissue sarcoma is the gold standard of treatment for localized disease in extremities, trunk and head / neck region (J Clin Oncol 2018;36:144)
- At this point, no consensus exists on the timing or benefit of perioperative radiation therapy for patients diagnosed with retroperitoneal soft tissue sarcoma
- Radiation therapy can also be utilized as a means of palliative local control when extensive metastases have already occurred
- Chemotherapy
- Leiomyosarcoma is characterized by severe genomic instability, which results in multiple genetic aberrations; as a result, leiomyosarcoma is considered moderately sensitive to chemotherapy (Sarcoma 2010;2010:506182)
- Neoadjuvant chemotherapy can help shrink the tumor, hence improving resectability, achieving negative margins and earlier control of metastatic disease
- Adjuvant chemotherapy after surgery significantly improves the time to local and distant recurrence and overall recurrence free survival (Lancet 1997;350:1647)
- Chemotherapy is the first line treatment in metastatic or unresectable leiomyosarcoma
Clinical images
Gross description
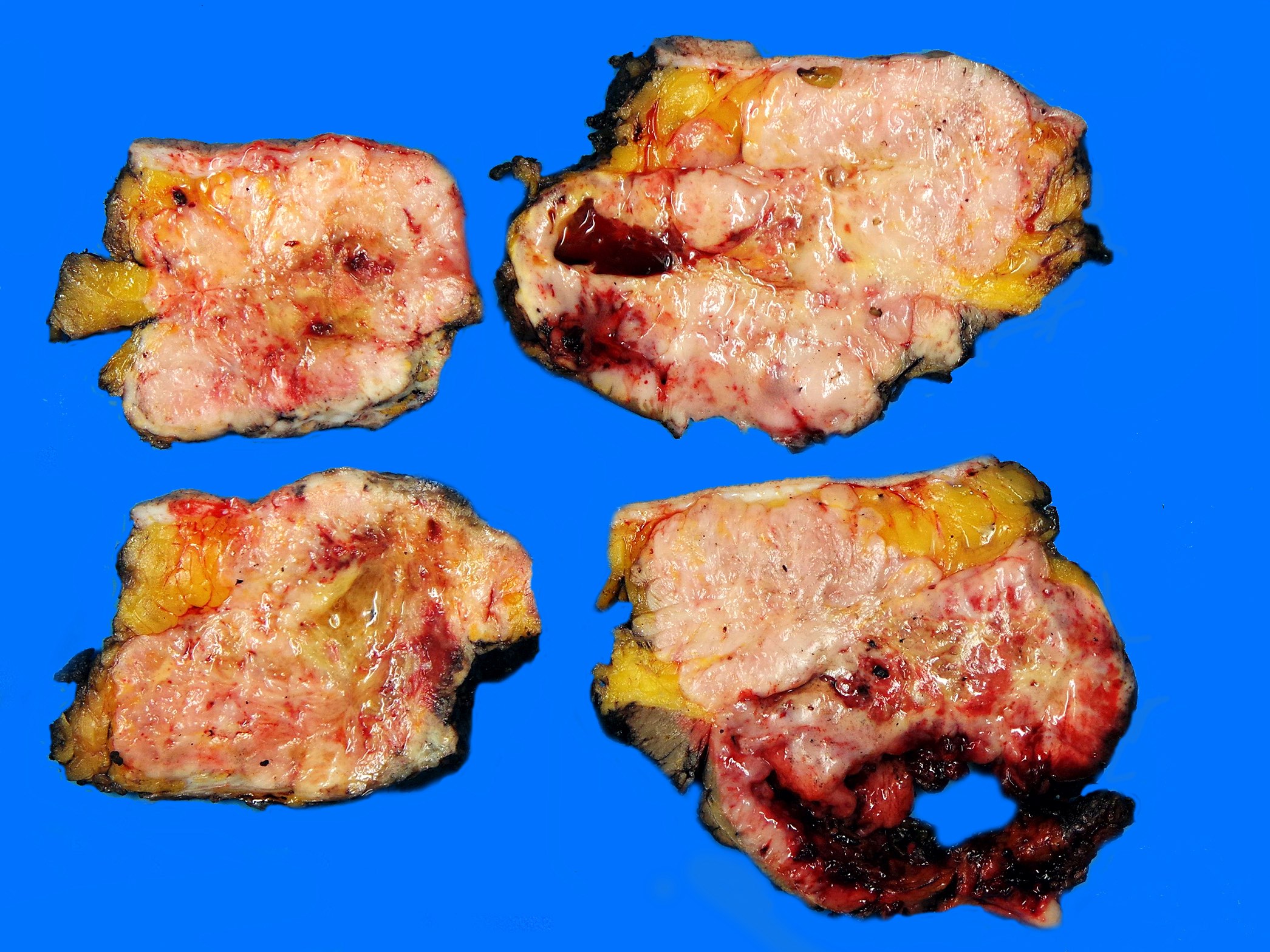
- Typically forms a fleshy, gray to white to tan mass
- Whorled appearance may be evident
- Large tumors often display hemorrhage, necrosis and cystic change
- Tumor border frequently appears well circumscribed
- References: Int J Surg Case Rep 2016;19:109, Arch Pathol Lab Med 2002;126:468, Cancer 1994;74:2251
Frozen section description
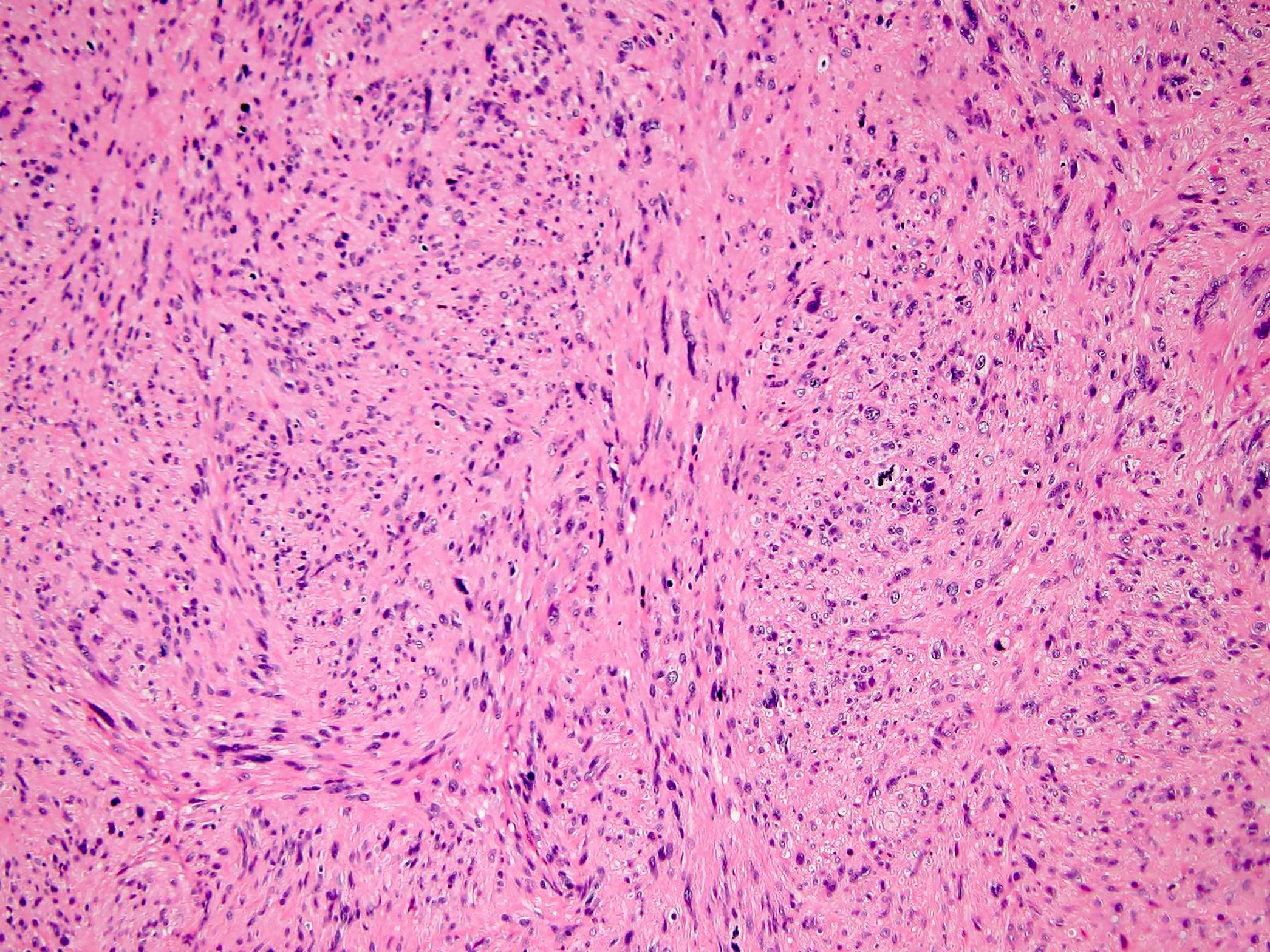
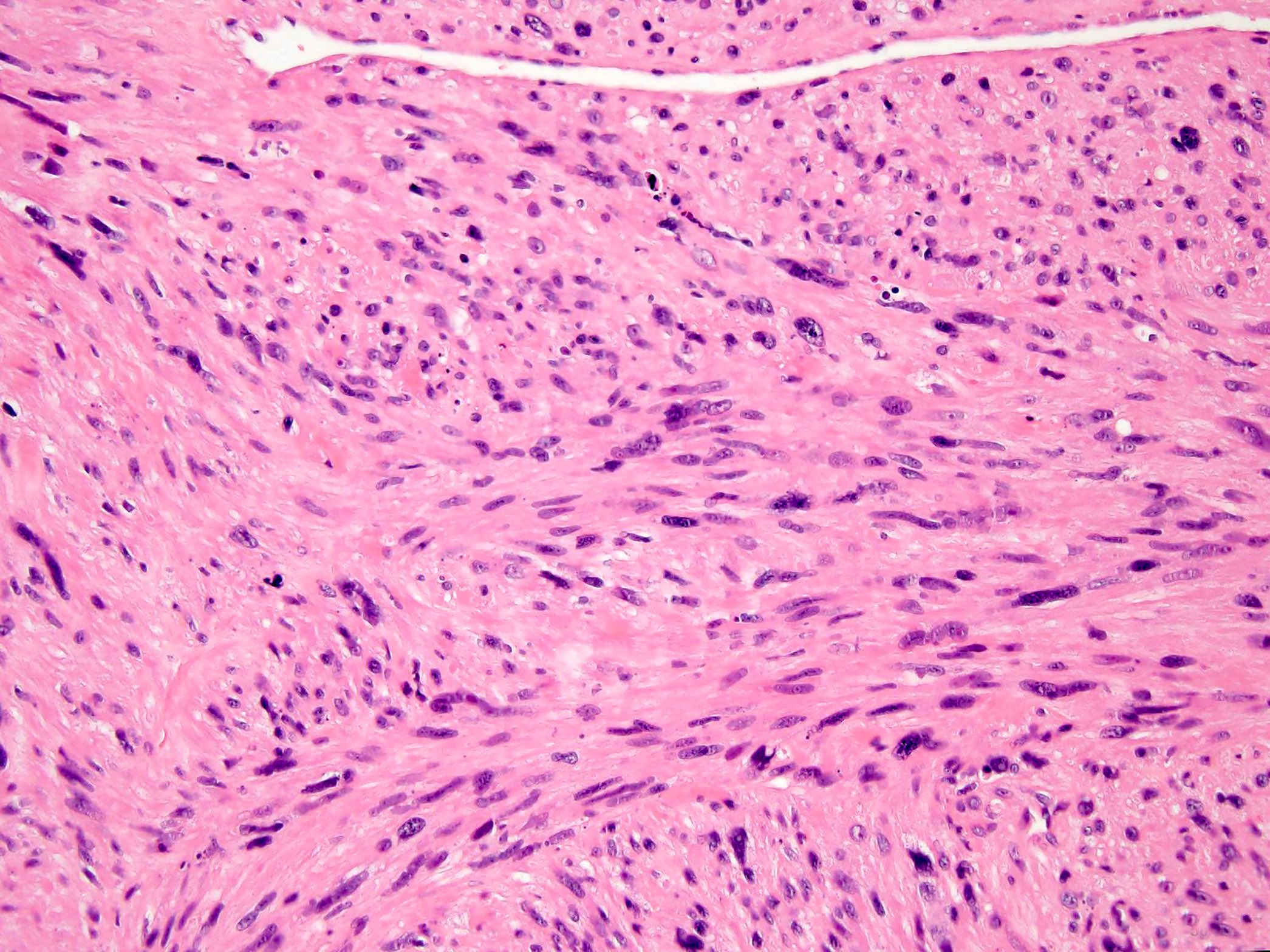
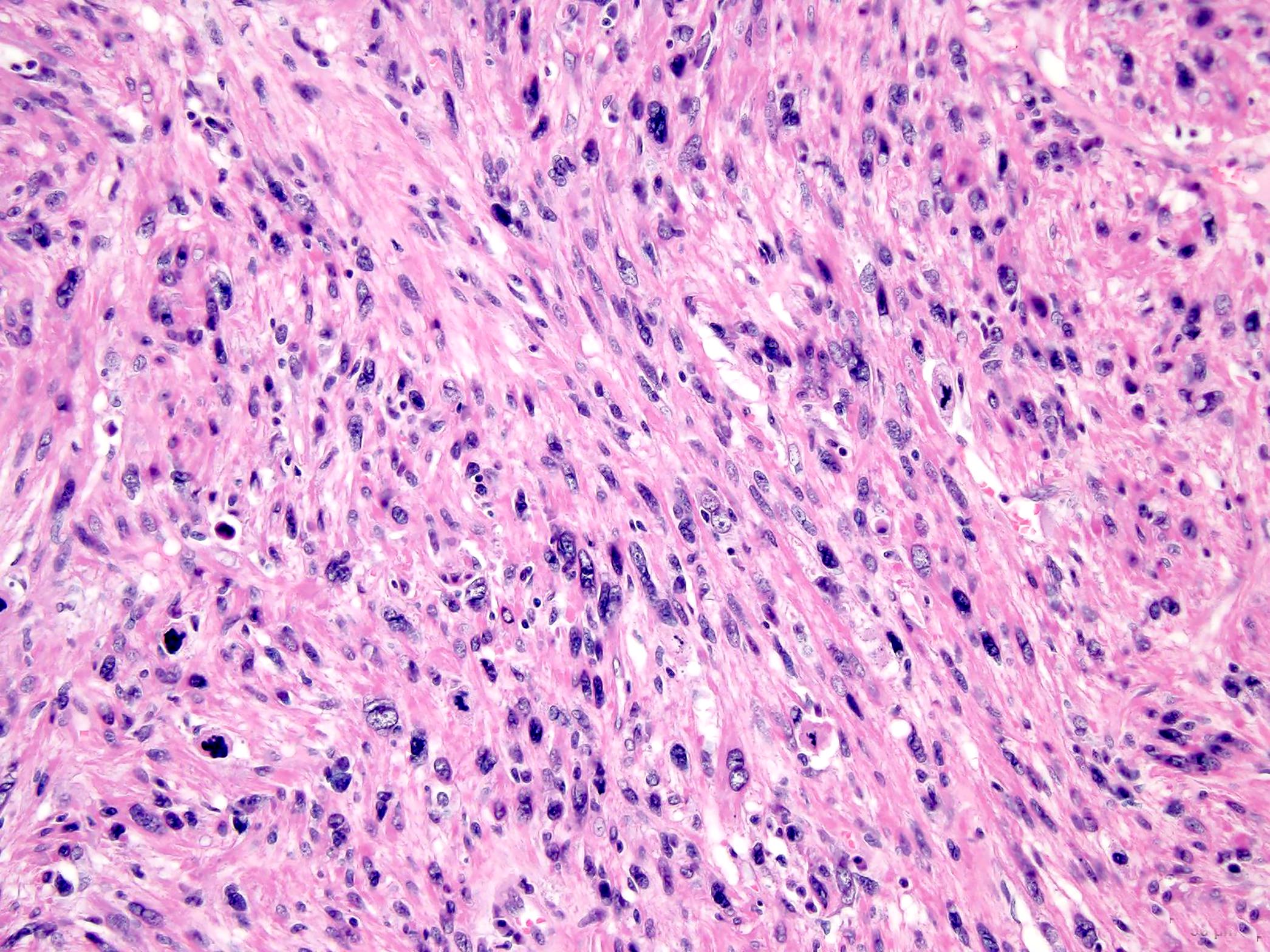
- Cellular neoplasm that is composed of intersecting fascicles of spindle cells with bright eosinophilic cytoplasm and elongated, blunt ended (cigar shaped) nuclei (Eur J Cancer 2002;38:1218, Am J Clin Pathol 2006;125:555)
- Nuclear pleomorphism, tumor necrosis and mitotic activity
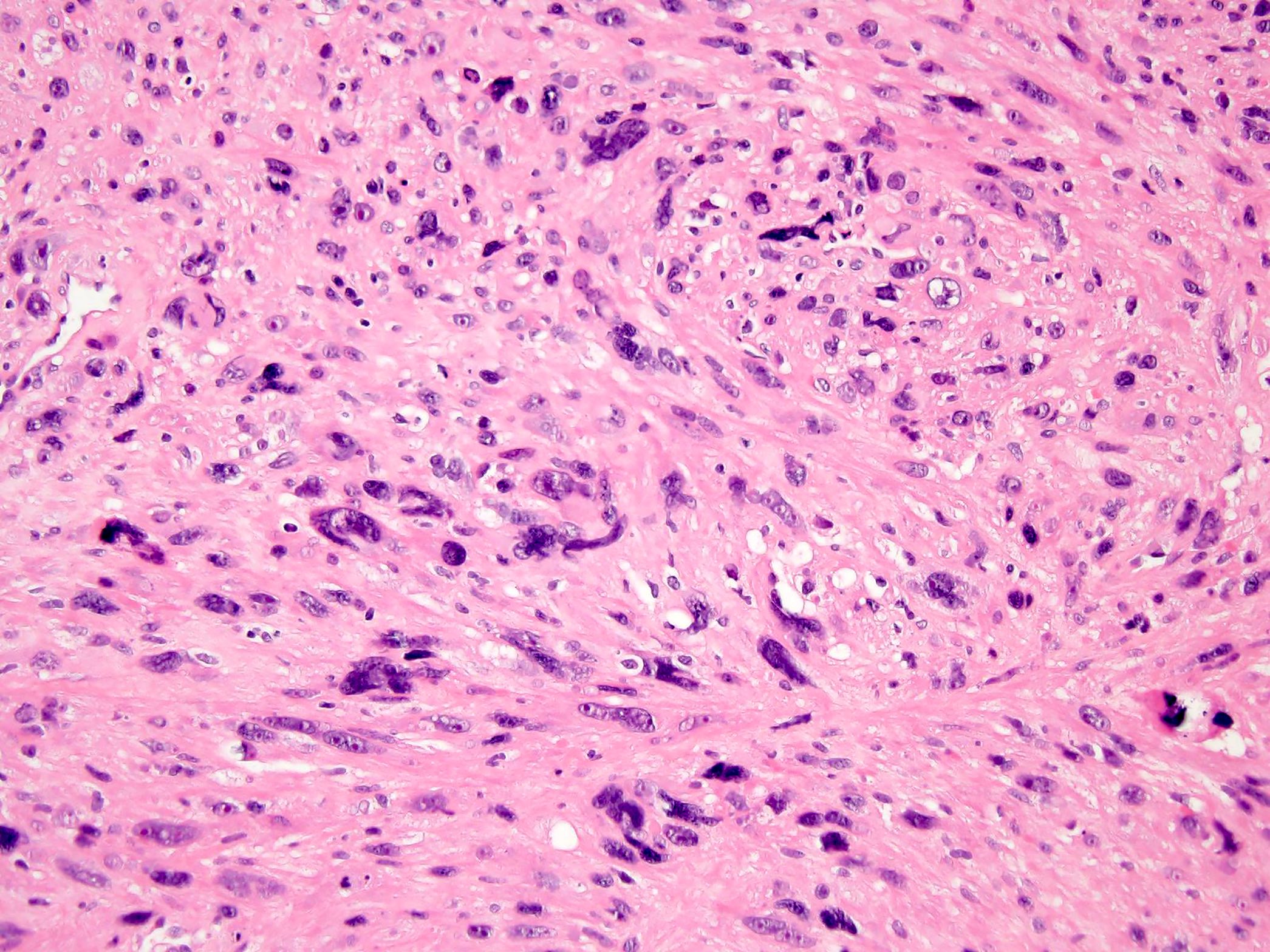
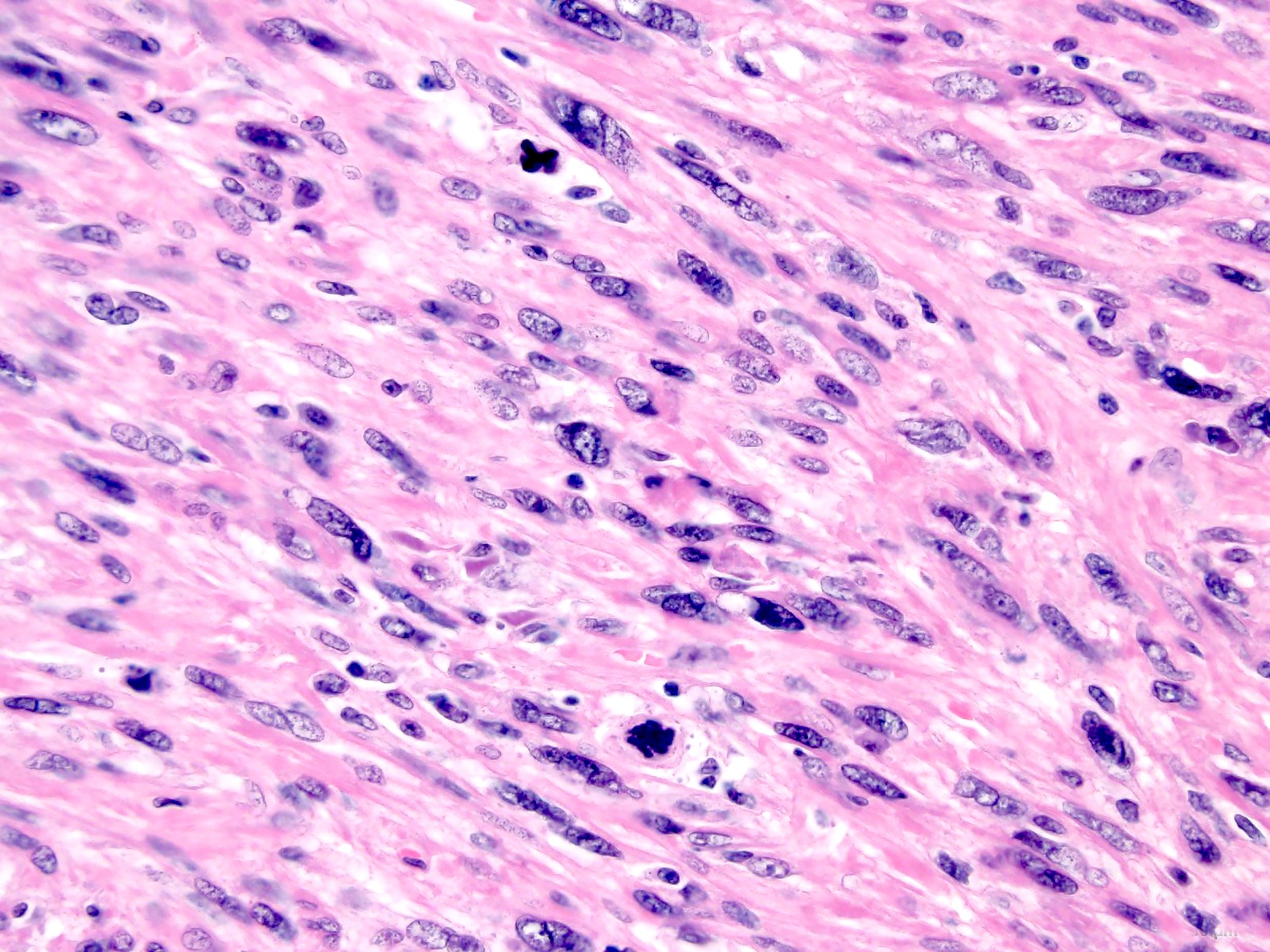
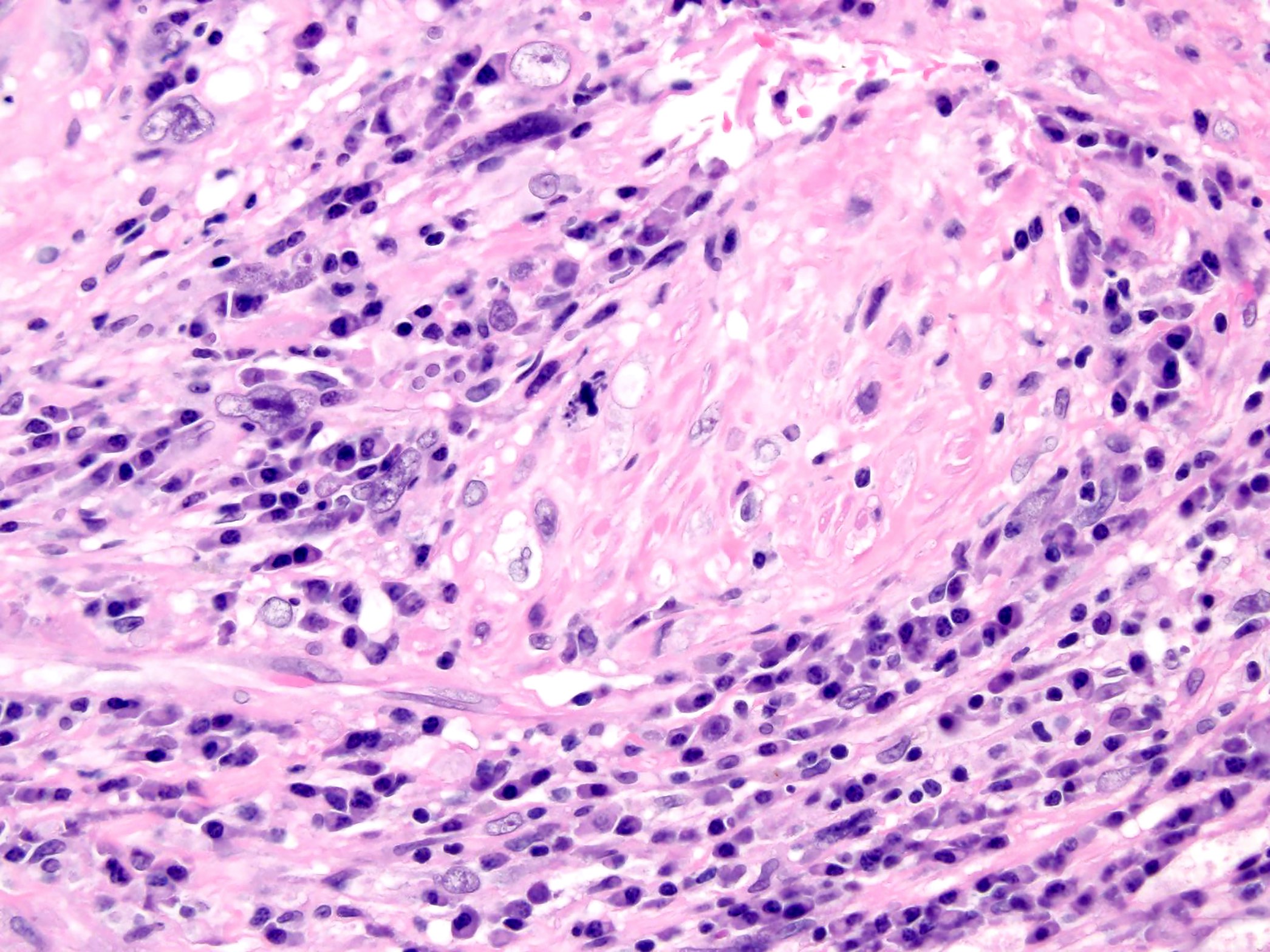
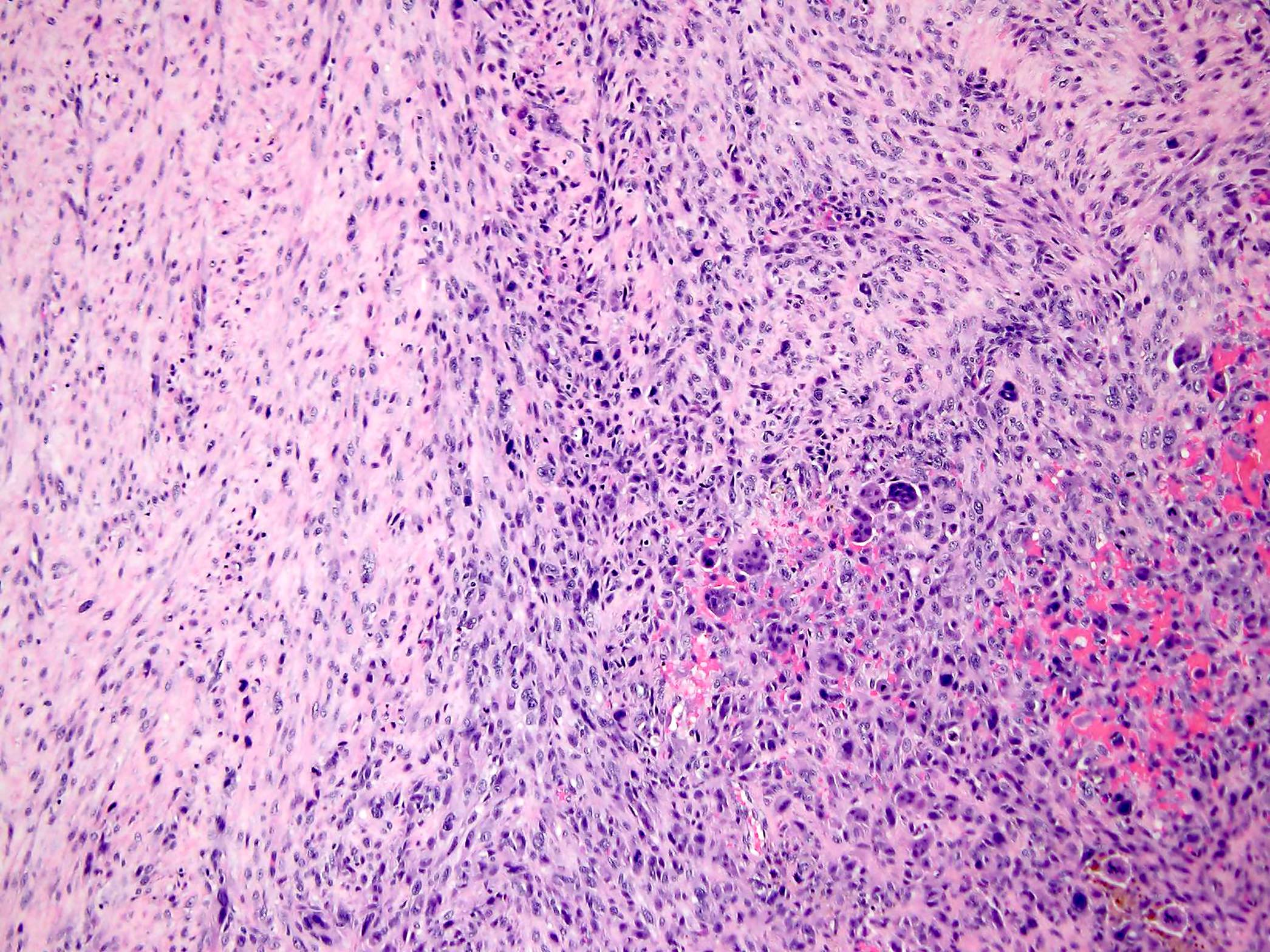
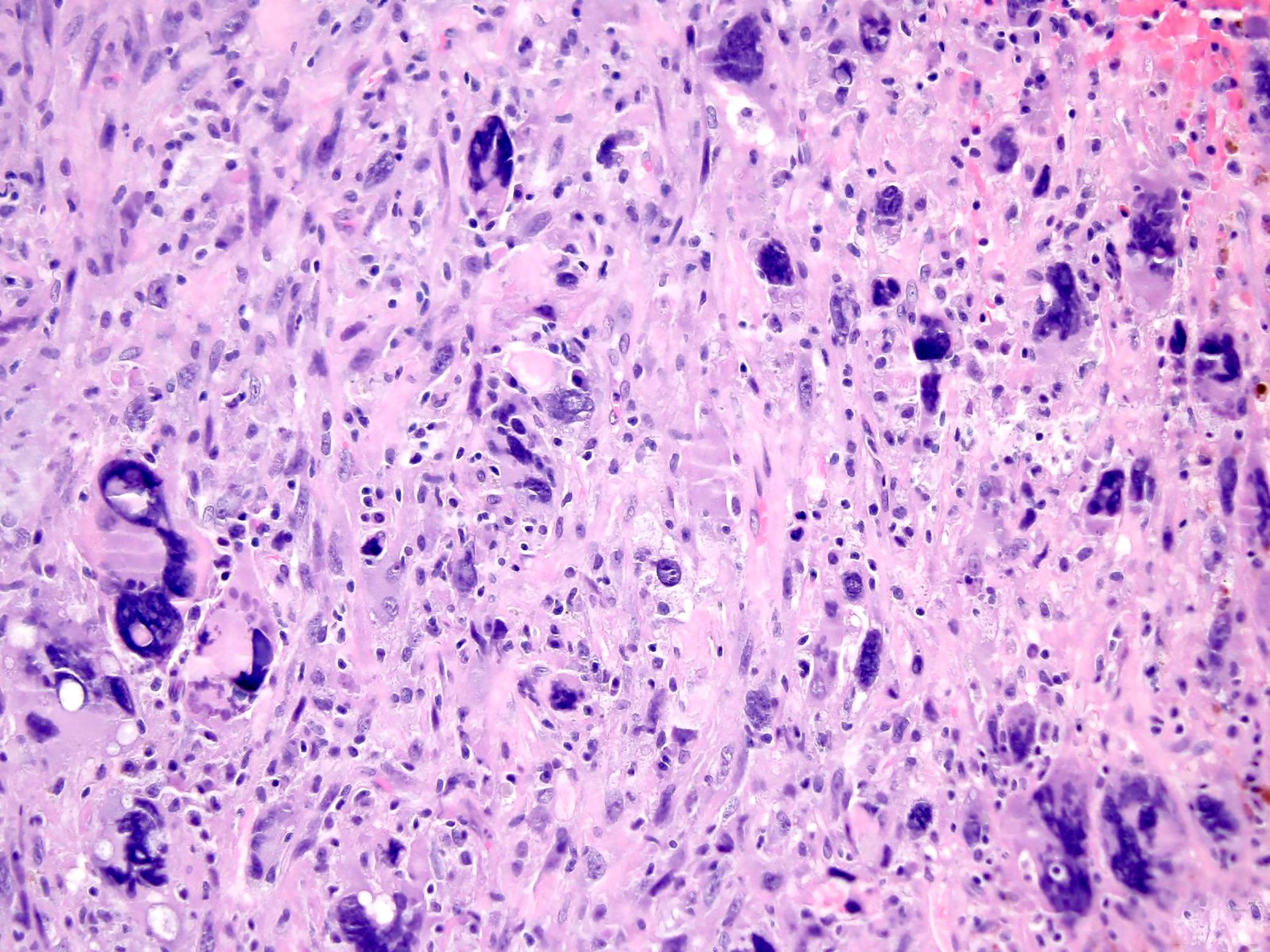
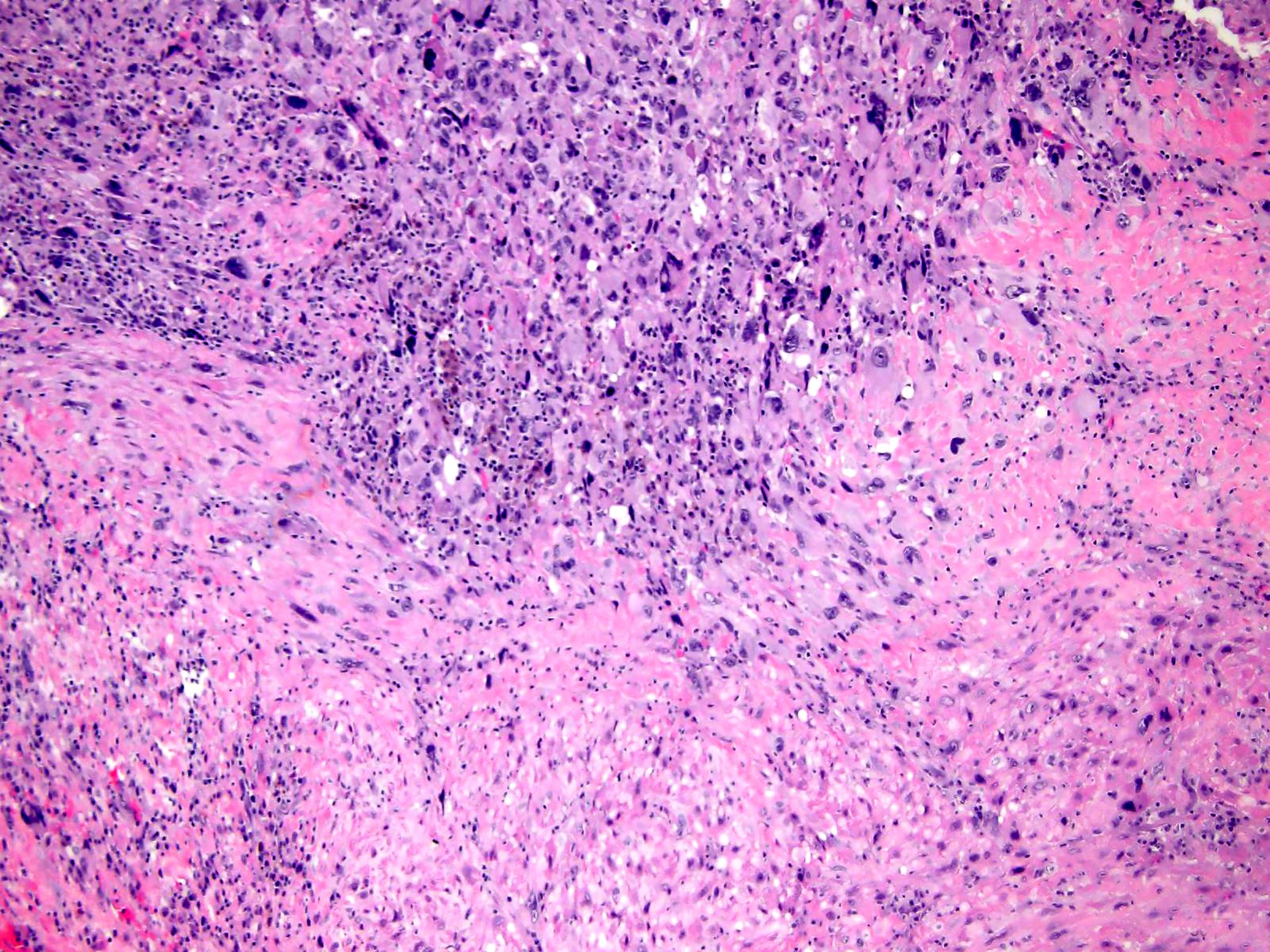
Microscopic (histologic) description
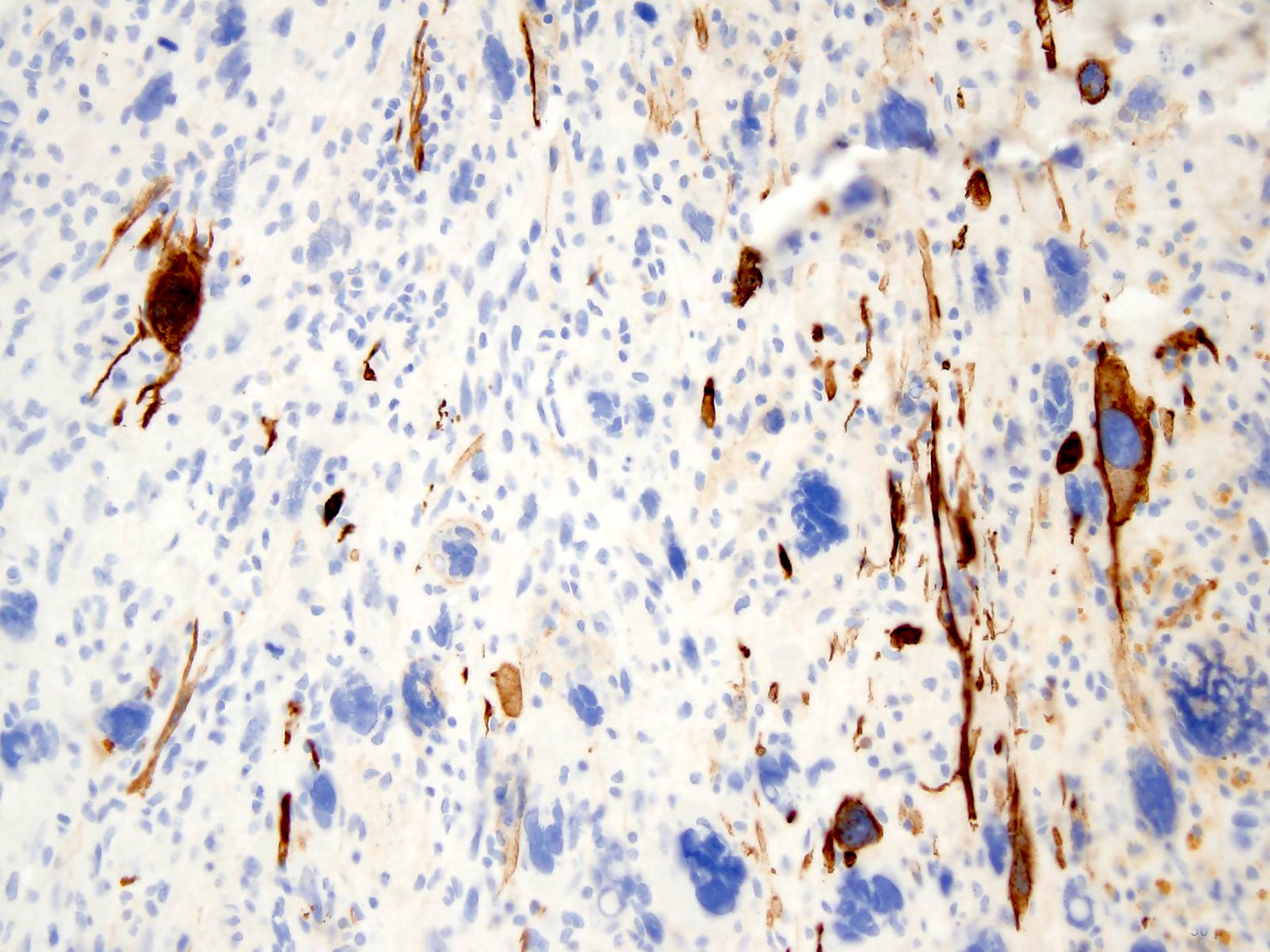
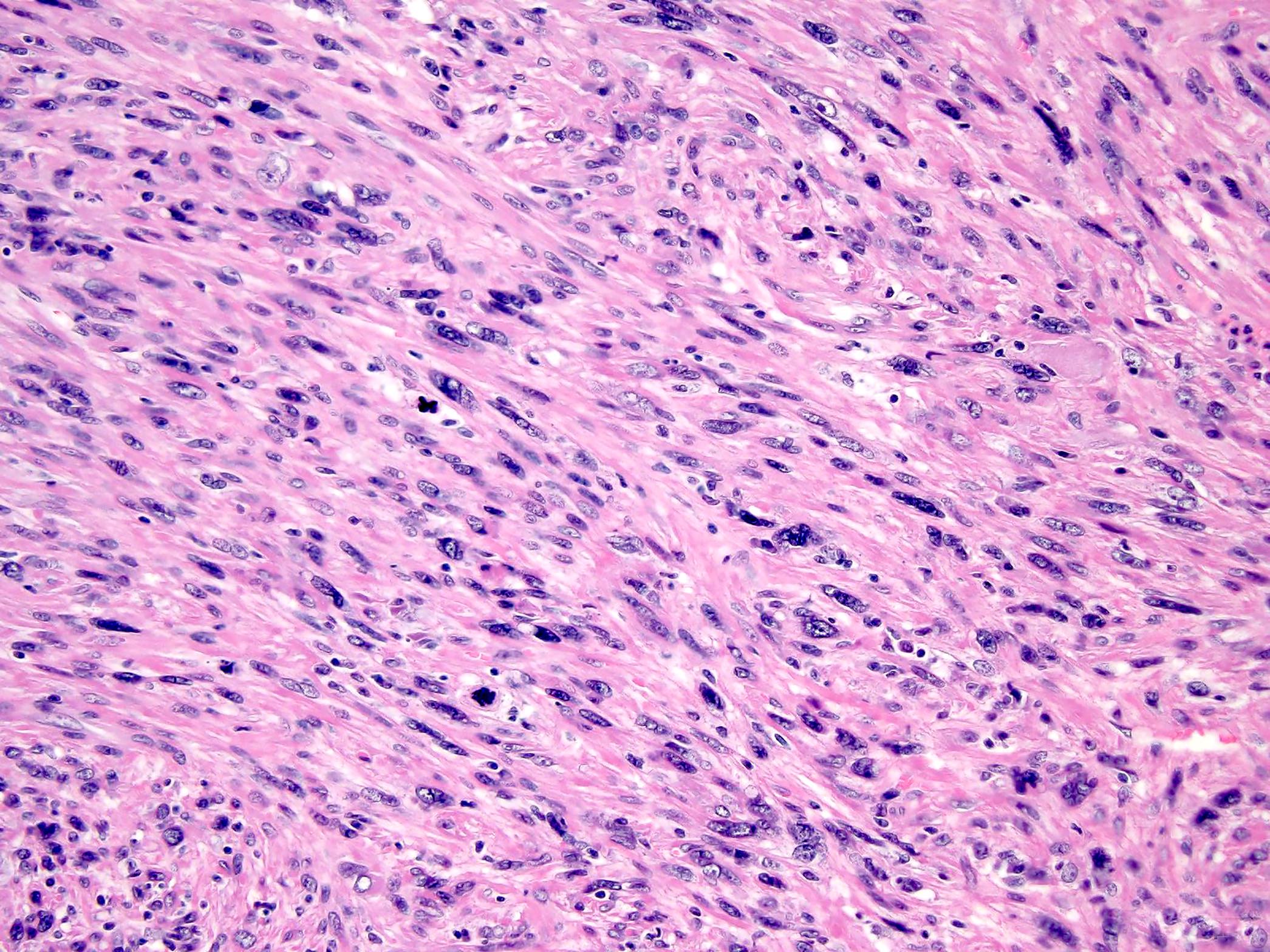
- Classic leiomyosarcoma (Eur J Cancer 2002;38:1218, Am J Clin Pathol 2006;125:555)
- Spindle shaped cells with plump, blunt ended nuclei and moderate to abundant, pale to brightly eosinophilic fibrillary cytoplasm
- Cells are set in long intersecting fascicles parallel and perpendicular to the plane of section
- Some tumors show areas with storiform or palisaded patterns
- Moderate nuclear pleomorphism is usually noted, although pleomorphism may be focal
- Mitotic figures, including atypical ones, are easy to find
- Tumors usually show diffuse hypercellularity
- Focal fibrosis, myxoid change and hyalinized hypocellular areas can be seen
- Tumor cell necrosis is often present
- Unusual features in soft tissue leiomyosarcoma include multinucleated osteoclast-like giant cells, granular cytoplasmic change and epithelioid morphology
- Pleomorphic leiomyosarcoma (Am J Surg Pathol 2001;25:1030)
- Composed of pleomorphic cells with or without abundant eosinophilic or fibrillary cytoplasm in > 66% of the maximum cut surface of the tumor, accompanied by an ordinary leiomyosarcoma fascicular area covering < 33%
- Storiform pattern in > 50% of cases
- Stromal hyalinization
- Chronic inflammatory infiltrate
- Myxofibrosarcoma-like (myxoid malignant fibrous histiocytoma-like) areas
- Myxoid leiomyosarcoma (Am J Surg Pathol 2000;24:927)
- Extensively myxoid stroma (> 50% of the tissue examined)
- Tumor cells are predominantly spindled
- 3 major histologic architectures: fascicular, reticular / microcystic and myxofibrosarcoma-like
- Areas of conventional leiomyosarcoma are usually present at least focally
- Dedifferentiated leiomyosarcoma (Histopathology 2011;59:1135)
- Tumor showing features of low grade leiomyosarcoma associated with a discrete undifferentiated component lacking morphological or immunophenotypic features of myogenic differentiation
- Diagnostic threshold for diagnosing low grade leiomyosarcoma is much lower outside the uterus than in the uterus
- Diagnosis requires nuclear atypia and essentially any level of mitotic activity (Adv Anat Pathol 2002;9:351)
- Some authors recommend expert review by sarcoma pathologists for diagnosis of leiomyosarcoma at any site (J Clin Oncol 2018;36:144)
- Histologic grade (French Federation of Cancer Centers Sarcoma Group [FNCLCC]) (J Clin Oncol 1997;15:350)
- The majority of soft tissue leiomyosarcomas are high grade
- See Soft tissue - Grading
Microscopic (histologic) images
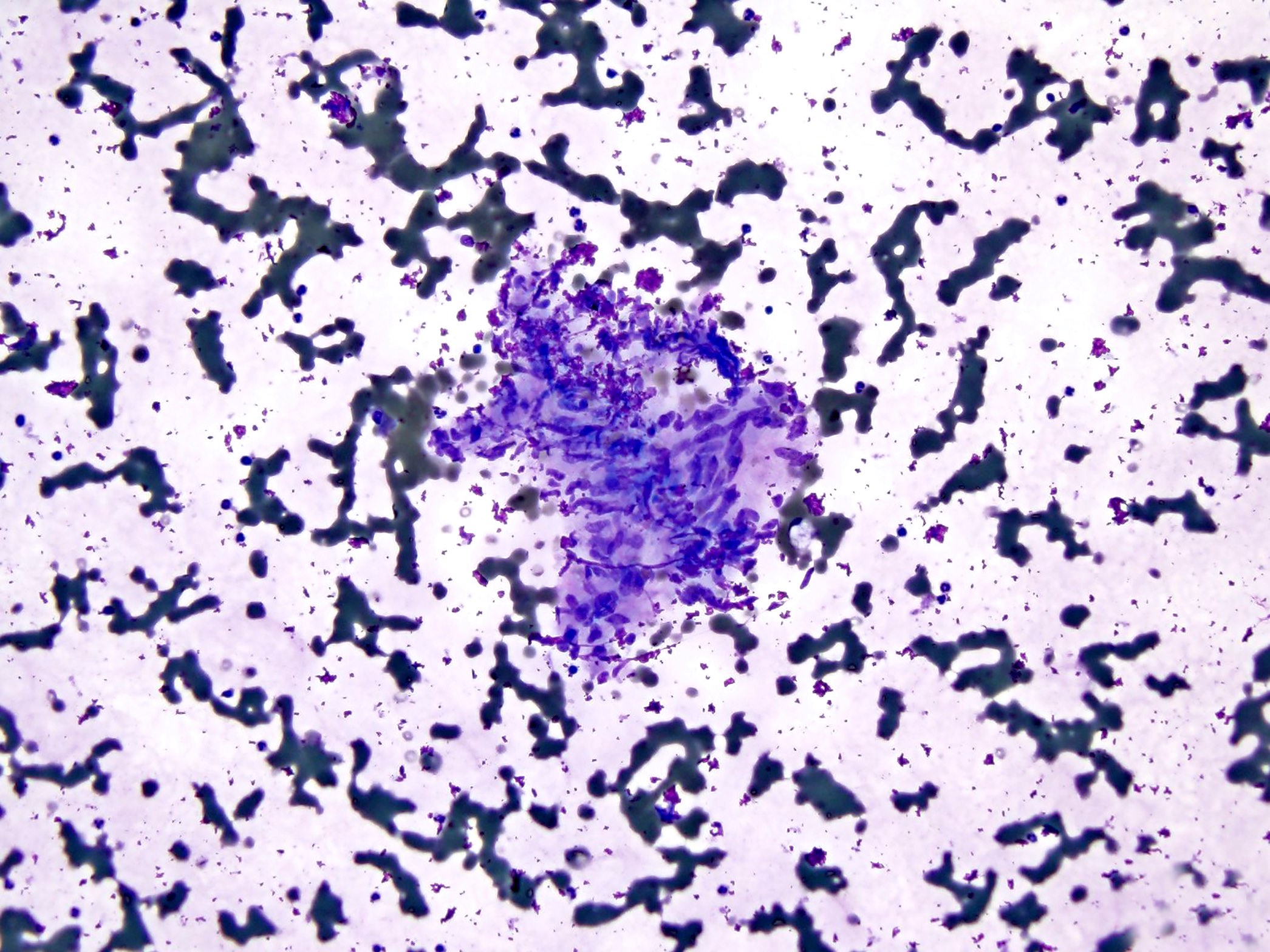
Cytology description
- Leiomyosarcoma, classical variant (Diagn Cytopathol 2003;28:119)
- Various proportions of spindle shaped, cohesive, small or large sized cells arranged in parallel alignment
- Blunt ended nuclei
- Cytoplasm varies from fibrillary to granular to vacuolar
- Leiomyosarcoma, epithelioid variant
- Round or polygonal cells
- Eccentrically located nuclei (Diagn Cytopathol 1994;11:321)
- Granular or clear cytoplasm
- Leiomyosarcoma, pleomorphic variant
- Variably sized and shaped cells, often including multinucleated giant cells with atypical nuclei
- Leiomyosarcoma, myxoid variant
- Large amounts of background myxoid matrix containing large spindle shaped and giant cells
- Intranuclear inclusions and mitotic figures are occasionally seen, as well as stromal fragments
Positive stains
Negative stains
- ER, PR, WT1 (Am J Surg Pathol 2016;40:1557)
- CD117, S100, HMB45 (Am J Surg Pathol 2001;25:1355)
- Positive staining for cytokeratin and EMA in 38% and 44% of cases, respectively (Pathol Int 2000;50:7)
Molecular / cytogenetics description
- Complex karyotypes with numerous chromosomal gains and losses (JCO Precis Oncol 2020;4:PO.20.00040)
- Losses involving tumor suppressors TP53 (17p13.1), RB1 (13q14.2) and PTEN (10q23.31) (Am J Pathol 2010;177:2080)
- TP53 is mutated in as many as 50% of sporadic leiomyosarcomas
- Homozygous copy loss of CDKN2C at chromosome 1p32.3b (JCO Precis Oncol 2020;4:PO.20.00040)
- CDKN2C null leiomyosarcoma defines a genomically distinct tumor that may have prognostic or therapeutic clinical implications, including the possible use of specific cyclin dependent kinase inhibitors
Sample pathology report
- Right thigh mass, core biopsy:
- Leiomyosarcoma, FNCLCC grade 2 (see comment)
- Comment: The neoplasm is composed of cellular, intersecting fascicles of spindle cells with bright eosinophilic cytoplasm and elongated blunt ended (cigar shaped) nuclei. Moderate nuclear pleomorphism and mitotic activity (up to 13 mitoses/10 high power fields) are noted. There is focal tumor necrosis (< 5%). Immunohistochemical stains for SMA, desmin and h-caldesmon are positive in tumor cells. These pathologic findings support the diagnosis above.
- Leiomyosarcomas of soft tissue are aggressive neoplasms with frequent local recurrence and distant metastases. The most important prognostic factors are histologic grade, tumor location and size.
Differential diagnosis
- Leiomyoma (Am J Surg Pathol 1994;18:576, Am J Surg Pathol 2001;25:1355):
- Well circumscribed
- Lacks significant nuclear atypia
- Mitoses are rare to absent
- Retroperitoneal leiomyomas resemble uterine leiomyomas by histology and are positive for hormone receptors
- Malignant peripheral nerve sheath tumor (Mod Pathol 2016;29:582):
- May demonstrate clinical and histologic origin from nerve
- Can arise in association with benign nerve sheath tumor
- Fascicles of spindle shaped cells, often with a hemangiopericytoma-like vascular pattern
- Alternating hypercellular and hypocellular areas (tapestry appearance)
- S100 and SOX10 expression (often focal)
- Loss of H3K27me3
- Negative for muscle markers
- Desmin expression seen in rhabdomyoblastic elements in malignant Triton tumor
- PEComa (Am J Surg Pathol 2005;29:1558, Int J Clin Exp Pathol 2019;12:4380):
- May show morphologic overlap with leiomyosarcoma
- Nested architecture or sheet-like growth pattern
- Spindled to epithelioid cells with abundant clear to granular eosinophilic cytoplasm
- Distinctive perivascular pattern of growth, with tumor cells radially arranged around vessels
- Characteristic myomelanocytic immunophenotype
- Synovial sarcoma (monophasic) (Am J Clin Pathol 2011;135:839, Cancer Res 2002;62:135):
- Monomorphic blue spindle cells arranged in dense cellular sheets or vague fascicles
- May contain strands of wiry or hyalinized collagen and calcifications
- Many tumors focally display a staghorn shaped vascular pattern
- Expression of EMA, keratins, BCL2, CD99 and TLE1
- Negative for muscle markers
- Synovial sarcoma harbors a unique t(X;18)(p11;q11) translocation
- Undifferentiated pleomorphic sarcoma (Ann Diagn Pathol 2018;37:118):
Additional references
Board review style question #1
A 57 year old woman presented with a mass in the soft tissue of the left thigh. H&E stains show a tumor composed of spindle shaped cells with plump, blunt ended hyperchromatic nuclei and moderate pale to brightly eosinophilic fibrillary cytoplasm. The cells are set in long intersecting fascicles parallel and perpendicular to the plane of the section. Mitotic figures, including atypical ones, are present.
Immunohistochemical stains for h-caldesmon, SMA and desmin are positive in tumor cells, while all of the following are negative: TLE1, CD99, HMB45, MelanA, S100, SOX10, EMA and AE1 / AE3.
Which of the following is most likely the correct diagnosis?
- Leiomyoma
- Leiomyosarcoma
- Malignant peripheral nerve sheath tumor
- PEComa
- Synovial sarcoma (monophasic)
Board review style answer #1
Board review style question #2
What is the most common gene mutation in soft tissue leiomyosarcoma?
- EWSR1
- FUS
- NF1
- PLAG1
- TP53
Board review style answer #2