Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Dehner C, Dehner L. Inflammatory myofibroblastic tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueinflammyofibro.html. Accessed April 3rd, 2025.
Definition / general
- Histologically distinctive myofibroblastic spindle cell neoplasm of borderline malignancy, classically featuring an intermixture of plasma cells and lymphocytes
Essential features
- Myofibroblastic spindle cell neoplasm of borderline malignancy
- Myofibroblastic spindle cells without overt cytologic atypia, interspersed by more or less prominent lymphoplasmacytic infiltrates
- Up to 60% of cases show ALK rearrangement and will be positive for ALK1 IHC
- Patients may present with constitutional symptoms (fever, night sweats, weight loss)
- Epithelioid inflammatory myofibroblastic sarcoma is a distinct, highly aggressive variant that is predominantly intra-abdominal and is associated with a worse outcome
Terminology
- Inflammatory pseudotumor; inflammatory myofibrohistiocytic proliferation; plasma cell granuloma; inflammatory fibrosarcoma (obsolete terms, not recommended)
ICD coding
- ICD-O: 8825/1 - Inflammatory myofibroblastic tumor
- ICD-10: D48.9 - Neoplasm of uncertain behavior, unspecified
- ICD-11: 2B53.Y & XH66Z0 - Other specified fibroblastic or myofibroblastic tumor, primary site and myofibroblastic tumor, NOS
Epidemiology
- Wide age range but most common in children and young adults
- Extrapulmonary IMTs show predilection for children, with mean age of ~10 years (Semin Diagn Pathol 1998;15:85)
Sites
- Most common extrapulmonary sites are the mesentery and omentum (Semin Diagn Pathol 1998;15:85, Semin Diagn Pathol 1998;15:102)
- Can also occur in lung, GI tract, female genital tract, bladder, etc.
Clinical features
- Site specific symptoms
- Intra-abdominal tumors associated with increased abdominal girth, possibly symptoms of obstruction
- Some patients (~33%) will present with systemic symptoms, such as fever, night sweats, weight loss (thought to be related to cytokine release) (Cytokine 2008;44:293)
Diagnosis
- Tissue sampling and histological examination
Laboratory
- Some patients have laboratory abnormalities (elevated erythrocyte sedimentation rate [ESR], hypochromic, normocytic anemia, thrombocytosis, hypergammaglobulinemia), which resolve soon after surgical resection (Cancer 1993;72:2042, Semin Diagn Pathol 1998;15:85)
Radiology description
- Nonspecific radiology findings; ultrasound may show hypoechoic or hyperechoic mass(es) with ill or well defined borders; increased vascularity on Doppler studies
- CT may show a homogeneous or heterogenous lesion with variable enhancement on delayed acquisitions due to fibrosis; calcification(s) seen in 15 - 25% of lung lesions in children, while rare in adult patients (Insights Imaging 2015;6:85, Radiology 1998;206:511)
- MRI shows low signal intensity on T1 and T2 weighted sequences (Insights Imaging 2015;6:85)
Radiology images
Prognostic factors
- Variable; generally good prognosis but up to 35% may recur and rare cases of distant metastasis have been reported
- Adverse factors: intra-abdominal location, epithelioid variant
- No established correlation of tumor size, mitotic rate, cellularity, necrosis and atypia with outcome in conventional IMT; however, ALK positive IMTs are less likely to recur and may have less aggressive behavior (Am J Surg Pathol 2007;31:509)
Case reports
- 8 month old girl with orbital mass (Ophthalmic Plast Reconstr Surg 2020;36:e65)
- 7 year old child presenting with intussusception (J Surg Case Rep 2020;2020:rjaa322)
- 42 year old woman with hematuria (Urol Case Rep 2019;27:100997)
- 60 year old man with breast lesion (Ochsner J 2017;17:277)
Treatment
- Surgical resection (re-excision of recurrences)
- Treatment with specific tyrosine kinase inhibitors, such as crizotinib (N Engl J Med 2010;363:1727)
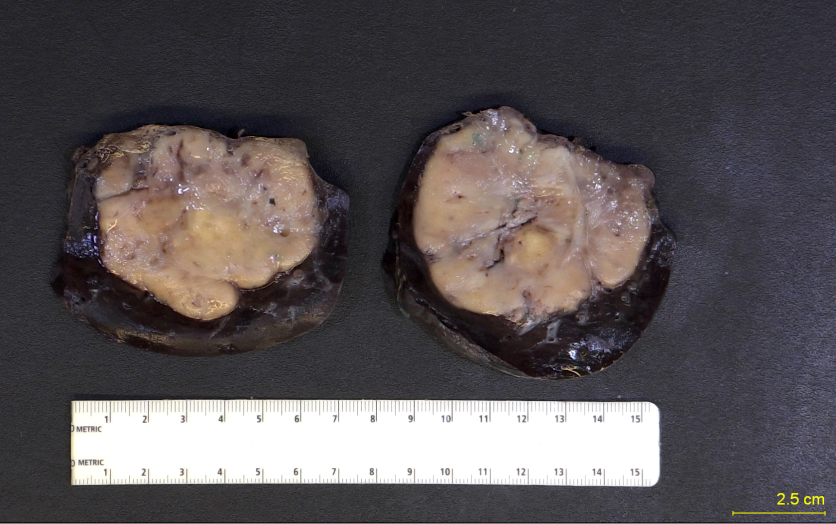
Gross description
- Circumscribed, solid mass with rubbery cut surface
- May present with calcifications
- May present as multiple nodules (same anatomic site) in 33% of cases
- Size ranges from 1 to 20 cm (median: 5 - 6 cm)
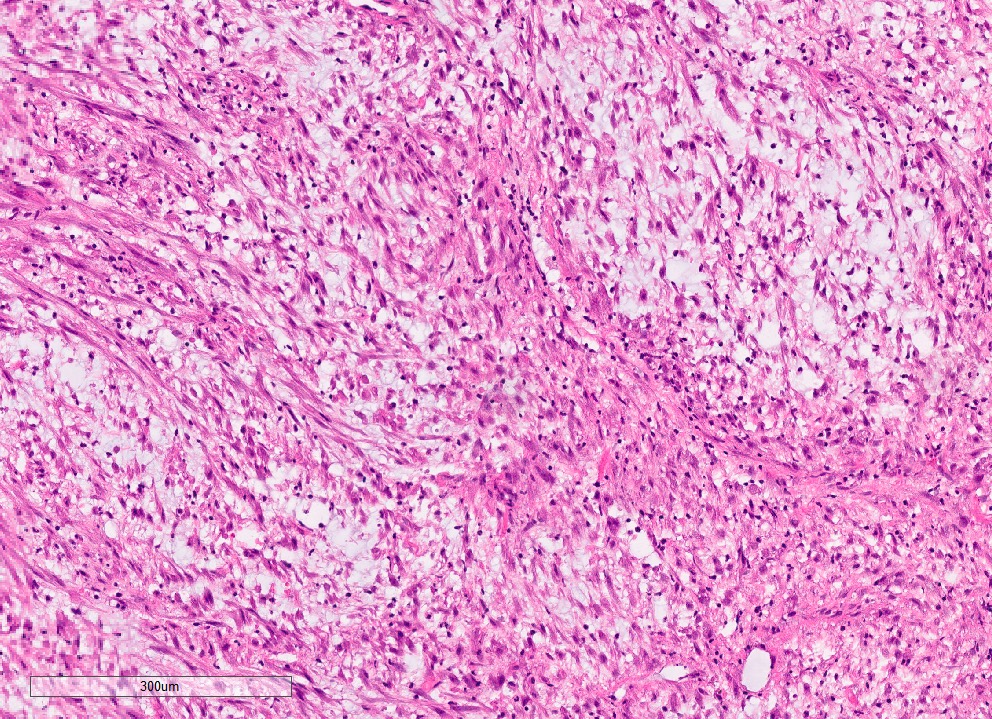
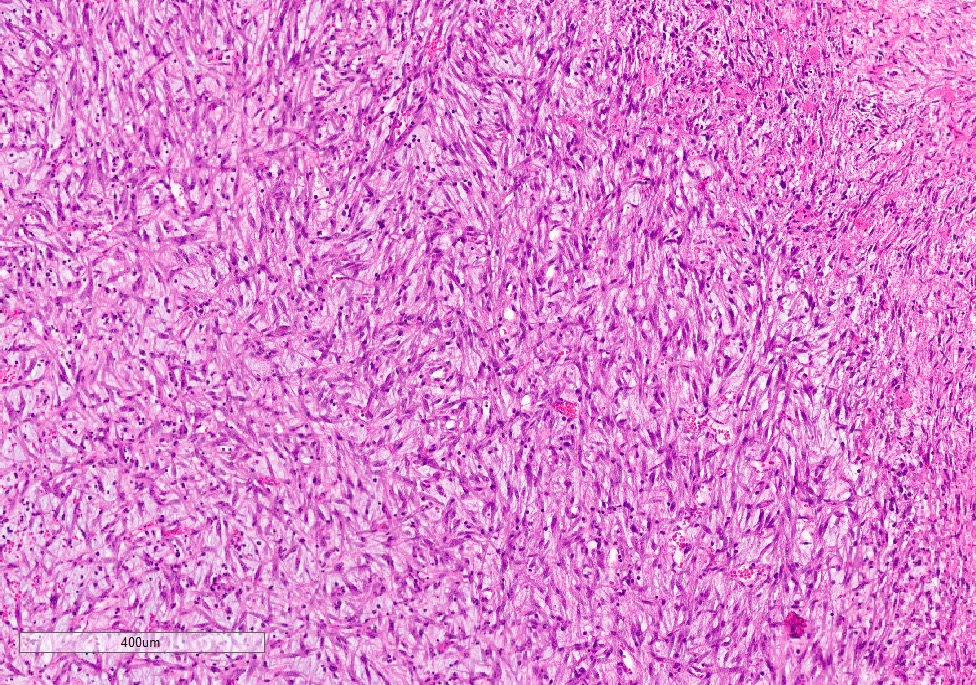
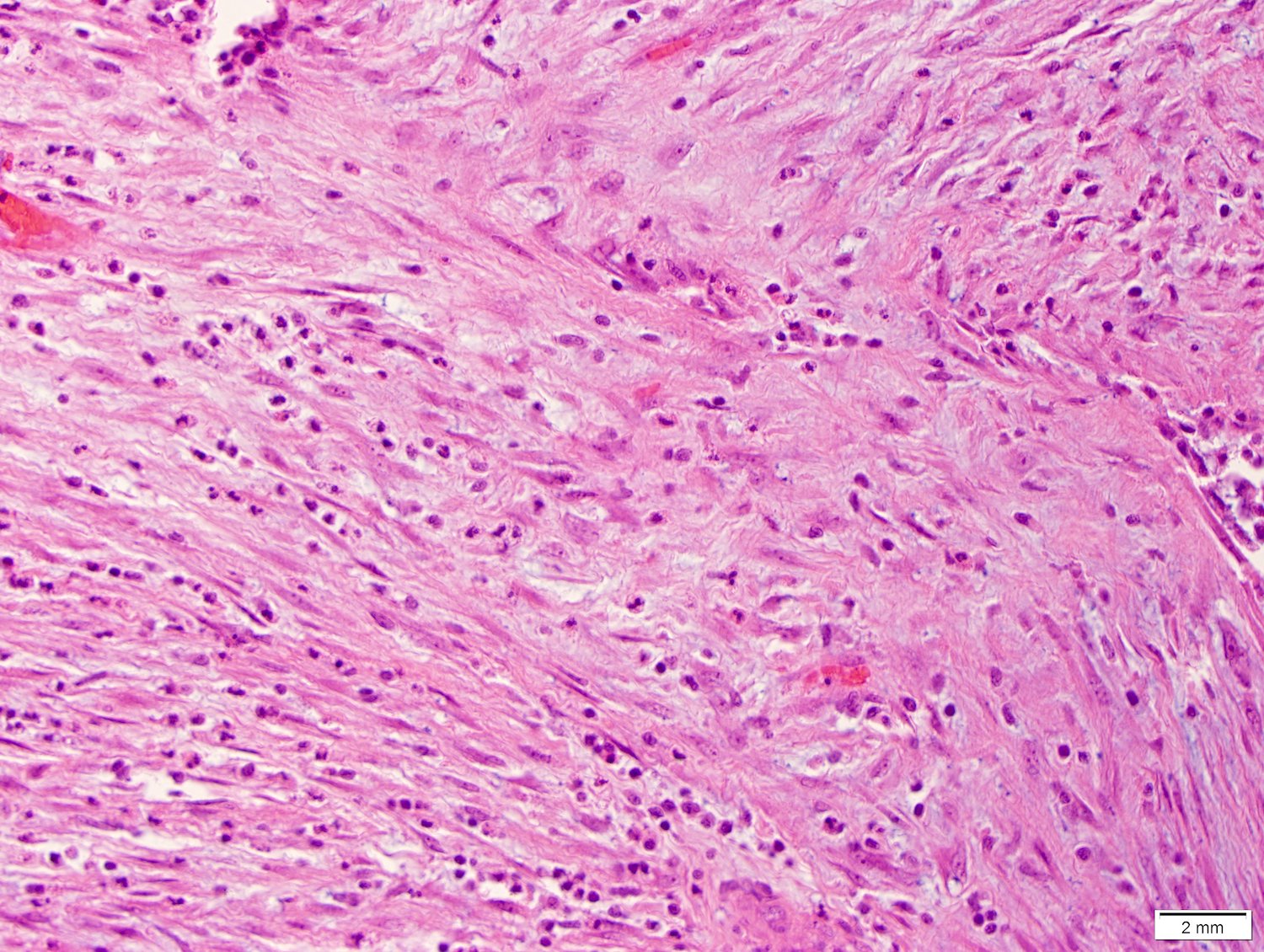
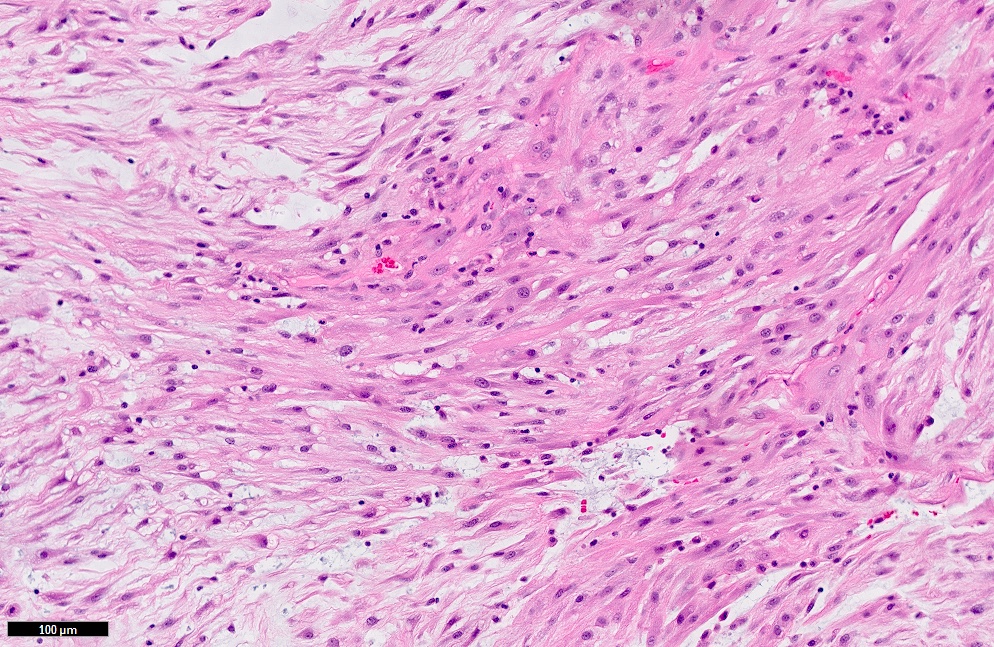
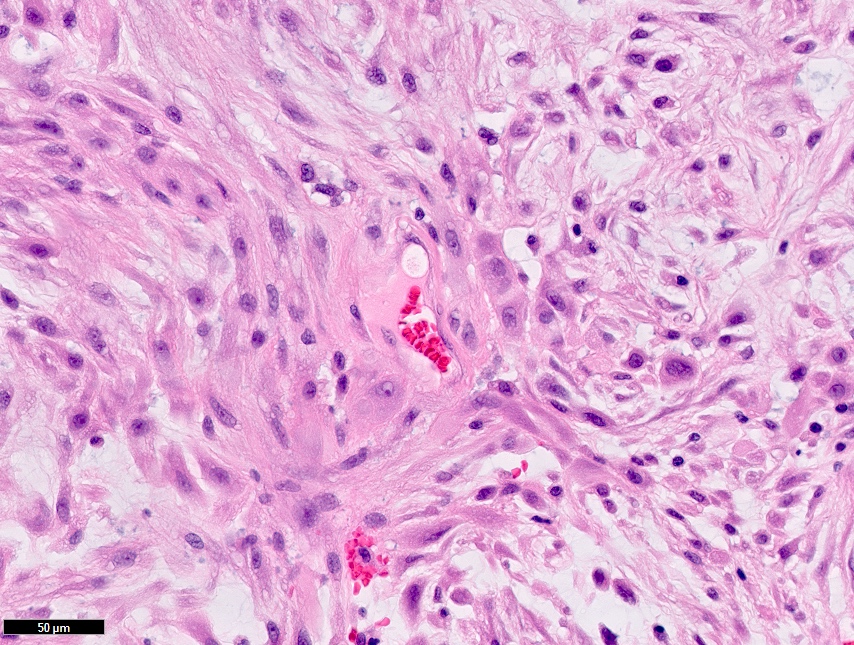
Microscopic (histologic) description
- Myofibroblastic spindle cell proliferation with mixed inflammation (lymphocytes, plasma cells and eosinophils)
- Number of mitotic figures varies, atypical figures can be seen
- Significant pleomorphism should be viewed with concern, may not fit with diagnosis of IMT
- Variety of histologic patterns sometimes seen
- Loosely arranged myxoid or hyaline stroma, spindle to stellate cells and admixed inflammatory cells (nodular fasciitis-like)
- Storiform or fascicular growing elongated spindle cells without overt hyperchromasia or cytologic atypia, associated with prominent lymphoplasmacytic infiltrate
- Hypocellular, scar-like pattern with occasional metaplastic bone or associated calcifications
- Some tumors may show ganglion-like cells
- Epithelioid variant predominantly composed of plump round to epithelioid cells with vesicular chromatin, large, prominent nucleoli and amphiphilic to eosinophilic cytoplasm; a prominent neutrophilic component and abundant myxoid stroma are common (Am J Surg Pathol 2011;35:135)
- Reference: Goldblum: Enzinger and Weiss's Soft Tissue Tumors: Expert Consult, 7th Edition, 2019
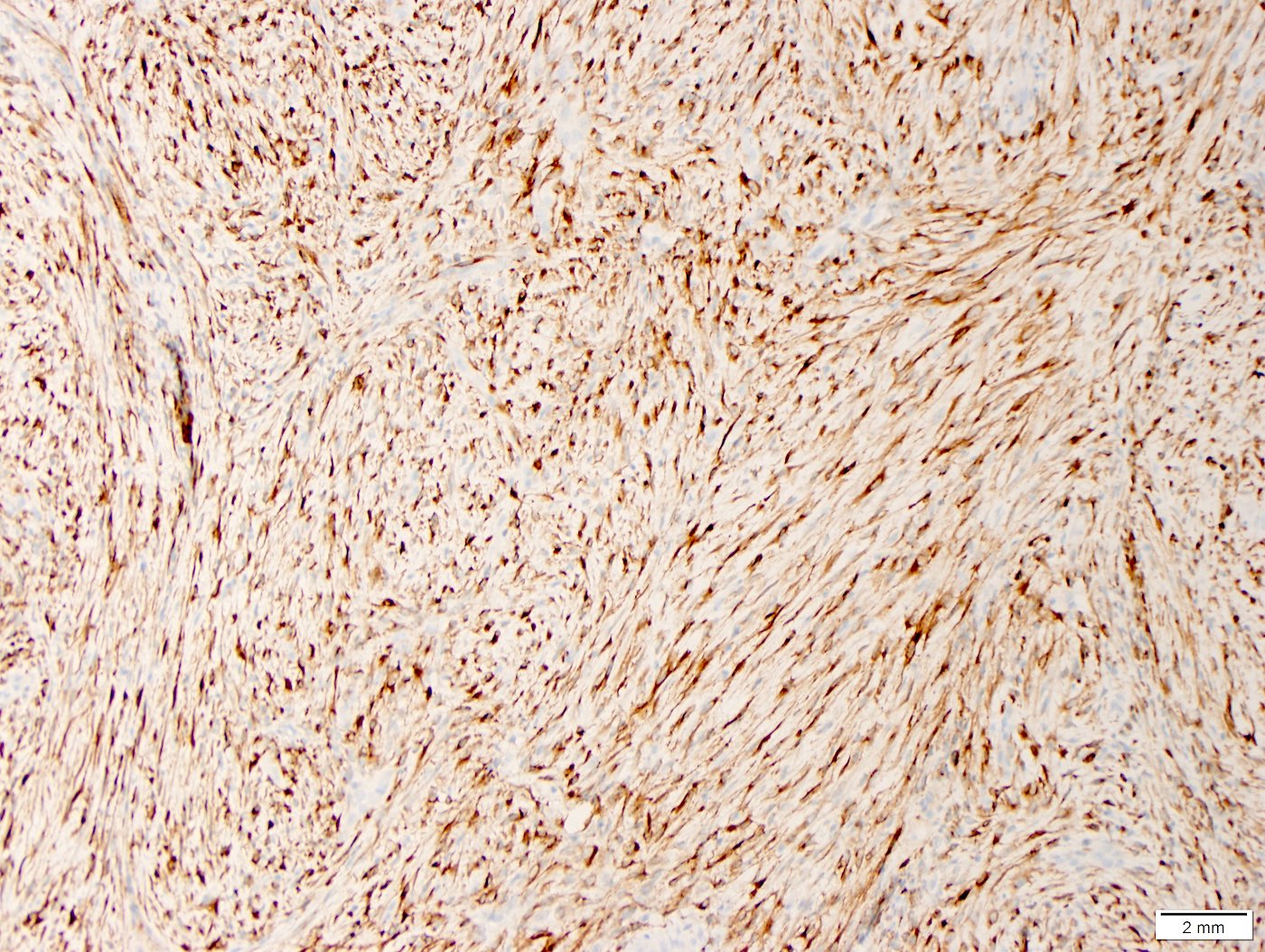
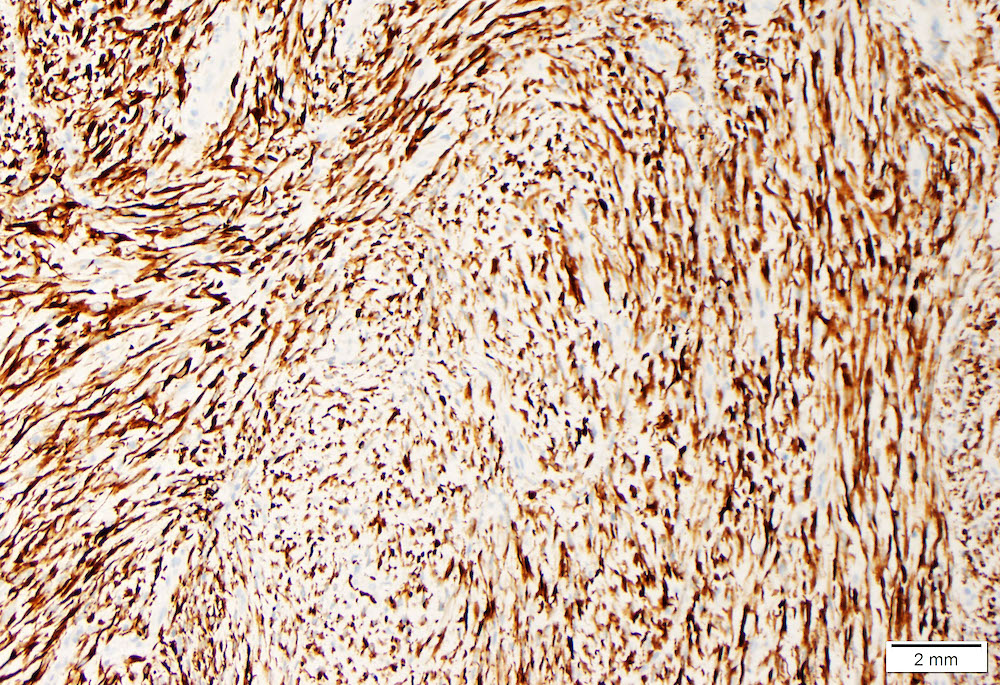
Microscopic (histologic) images
Positive stains
- Vimentin (diffuse, strong), smooth muscle actin, muscle specific actin, calponin, desmin (variable)
- Keratin in 40 - 70%
- ALK1 (diffuse cytoplasmic) in 40 - 60% (Am J Surg Pathol 2001;25:1364, Mod Pathol 2002;15:931)
- ALK negative cases can be diagnosed in the presence of typical clinicopathologic findings; molecular studies may be very helpful in these cases
- Epithelioid variant has a distinct pattern of ALK staining: nuclear membrane or perinuclear pattern (Am J Surg Pathol 2011;35:135)
Electron microscopy description
- Myofibroblasts and fibroblasts
Molecular / cytogenetics description
- Rearrangement of 2p23 (ALK) in 50 - 70% (Cancer Res 1999;59:2776, Curr Opin Oncol 2012;24:409)
- Multiple fusion partners (EML4, TPM3, TPM4, CARS, RANBP2, IGFBP5, etc.) (Mod Pathol 2017;30:1489, Am J Surg Pathol 2017;41:773, Am J Pathol 2000;157:377, Lab Invest 2003;83:1255)
- ALK negative IMTs may show ROS1 and PDGFRB alterations (Am J Surg Pathol 2015;39:957, Cancer Discov 2014;4:889, Mod Pathol 2015;28:732)
- ETV6::NTRK3 fusion found in a subset (may be on a spectrum with congenital / infantile fibrosarcoma)
Videos
Inflammatory myofibroblastic tumor
Sample pathology report
- Lung, right upper lobe, pneumonectomy:
- Inflammatory myofibroblastic tumor, ALK positive, present at bronchial and vascular margins (see comment)
- Comment: Sections of the right lobe show a circumscribed spindle cell neoplasm with a prominent inflammatory component. The tumor has replaced the lung parenchyma and is continuous with the right upper lobe bronchus with partial destruction of the bronchial cartilage. The bronchial and vascular margins are involved by tumor. Immunohistochemical stains show that tumor cells are diffusely positive for vimentin, SMA and ALK, while negative for IgG and IgG4. In summary, the morphological and immunohistochemical features support the diagnosis of inflammatory myofibroblastic tumor.
Differential diagnosis
- Nodular fasciitis:
- Most commonly in extremities, ALK negative, MYH9::USP6 fusion
- Desmoid type fibromatosis:
- Spindle cells with interspersed collagen with scant to no inflammation, ALK1 negative, mutation in CTNNB1 (beta catenin)
- (Inflammatory) leiomyosarcoma:
- Cigar shaped nuclei, more organized fascicular growth
- IgG4 related sclerosing disease:
- Ratio of IgG4+/IgG much higher than in IMT, negative for ALK1 by IHC
- Hodgkin lymphoma:
- Inflammatory fibroid polyp:
- Myxoid stroma with eosinophils and lymphocytes
- Negative for ALK1, commonly has PDGFRA mutations
- Gastrointestinal stromal tumor (GIST):
Additional references
Board review style question #1
Board review style answer #1
E. Its aggressive variant (epithelioid inflammatory myofibroblastic tumor) shows distinct, perinuclear or nuclear membrane staining for ALK.
Comment Here
Reference: Inflammatory myofibroblastic tumor
Comment Here
Reference: Inflammatory myofibroblastic tumor
Board review style question #2
Which of the following genes may show a molecular abnormality in inflammatory myofibroblastic tumor?
- CTNNB1
- MYC
- NOTCH3
- ROS1
- USP6
Board review style answer #2
D. ROS1. ALK negative IMTs may show ROS1 alterations.
Comment Here
Reference: Inflammatory myofibroblastic tumor
Comment Here
Reference: Inflammatory myofibroblastic tumor