Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alexiev B. Composite hemangioendothelioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuehemangioendotheliomacomposite.html. Accessed March 30th, 2025.
Definition / general
- Rare vascular neoplasms of intermediate biological potential
- Tumor is characterized by a complex admixture of benign, low grade malignant and malignant vascular components (Am J Surg Pathol 2000;24:352, Adv Anat Pathol 2015;22:254, Am J Dermatopathol 2013;35:517)
Essential features
- Vascular neoplasm which is considered to be of intermediate (rarely metastasizing) malignant potential
- Striking morphologic variation at low power, both within individual tumors and between tumors of different patients
- Distinguishing composite hemangioendothelioma from other vascular neoplasms largely lies in finding different histologic vascular patterns within 1 lesion
ICD coding
- ICD-O:
- ICD-11: 2F72.Y & XH8D24 - other specified neoplasms of uncertain behavior of skin & composite hemangioendothelioma
Epidemiology
- Uncommon vascular neoplasm (Am J Surg Pathol 2000;24:352)
- Tumor mainly occurs in adults but has a wide age distribution ranging from infancy (including congenital cases), children and teenagers, to adults in the eighth decade (J Cutan Pathol 2002;29:226, Adv Anat Pathol 2015;22:254)
Sites
- Most cases occur on the distal extremities, especially the hands and feet (Am J Dermatopathol 2013;35:517)
- Other sites include head and neck, back, mediastinum, bone, inguinal lymph node, kidney and spleen (Head Neck Pathol 2015;9:519, Am J Dermatopathol 2008;30:262, Tumori 2009;95:98, Clin Nucl Med 2014;39:e180, Adv Anat Pathol 2015;22:254, Int J Clin Exp Pathol 2013;6:1935, Jpn J Clin Oncol 2012;42:770)
Etiology
- Etiology is unknown (Adv Anat Pathol 2015;22:254)
- Several patients had a history of lymphedema (Am J Dermatopathol 2013;35:517)
- Association with Kasabach-Merritt or Maffucci syndrome has been reported (Am J Surg Pathol 2007;31:1567)
Clinical features
- Lesions are usually longstanding and have a reddish-blue, multinodular appearance (Am J Clin Pathol 2014;141:732)
Diagnosis
- Tissue sampling is the gold standard for a definitive diagnosis
- Because of the wide morphologic spectrum, can be difficult to recognize in small tissue samples (Adv Anat Pathol 2015;22:254)
Prognostic factors
- Local recurrence, which can be aggressive, has been described in up to 57% of cases, ranging from 18 months to 10 years after initial excision
- Low rate of metastasis (Am J Clin Pathol 2014;141:732)
- Recurrence or metastasis seem to occur irrespective of angiosarcoma-like foci (Am J Dermatopathol 2013;35:517)
- No difference in biologic behavior among cases with various combinations of histology (Am J Surg Pathol 2007;31:1567)
- Accurate diagnosis is crucial for correct treatment and prognostication (Adv Anat Pathol 2015;22:254)
Case reports
- 31 year old man with painless slow growing swelling on upper back (J Clin Diagn Res 2016;10:ED01)
- 43 year old man with submandibular mass (Head Neck Pathol 2015;9:519)
- 56 year old man with a mass of the manubrium sterni (Clin Nucl Med 2014;39:e180)
- 68 year old man with growing nodule on the vertex of his scalp (Am J Clin Pathol 2014;141:732)
- 78 year old woman with forehead and right eye mass (BMC Dermatol 2017;17:15)
Treatment
- Because of the rarity of these tumors, the best therapeutic approach has not been established
- Surgical excision is often curative (Adv Anat Pathol 2015;22:254)
- Local radiotherapy and chemotherapy for recurrent and metastatic disease have been used with some success
Gross description
- Bluish-purple or reddish blue infiltrative, uninodular or multinodular mass (Am J Surg Pathol 2000;24:352, J Cutan Pathol 2008;35:225)
Microscopic (histologic) description
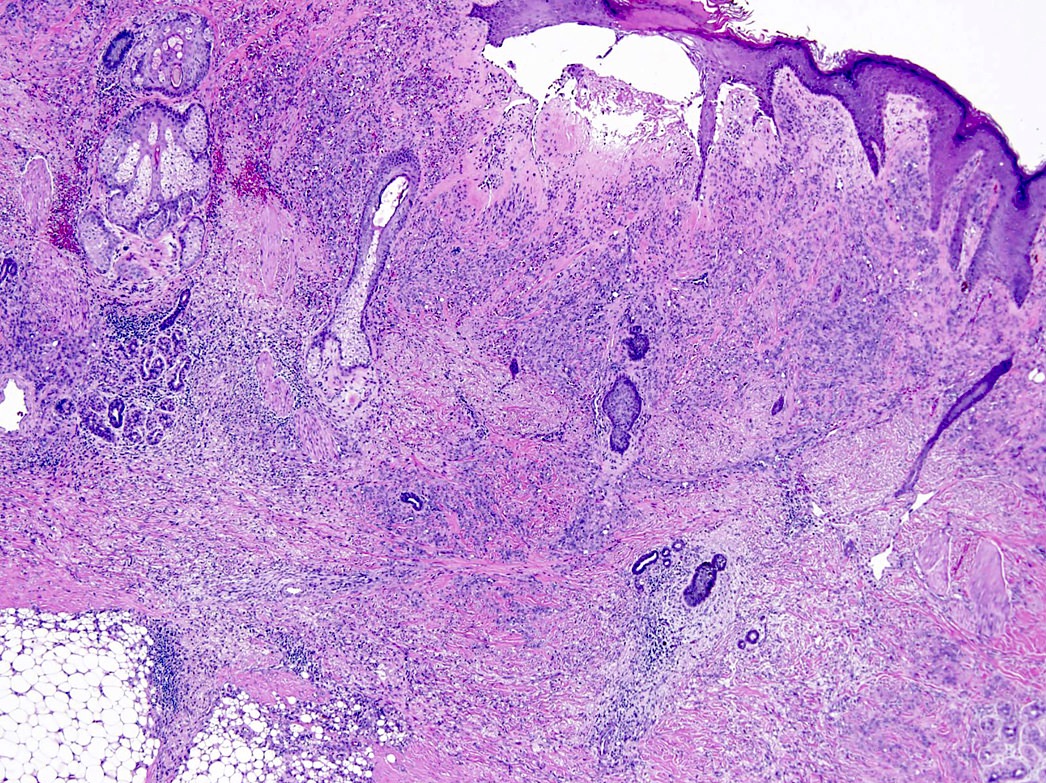
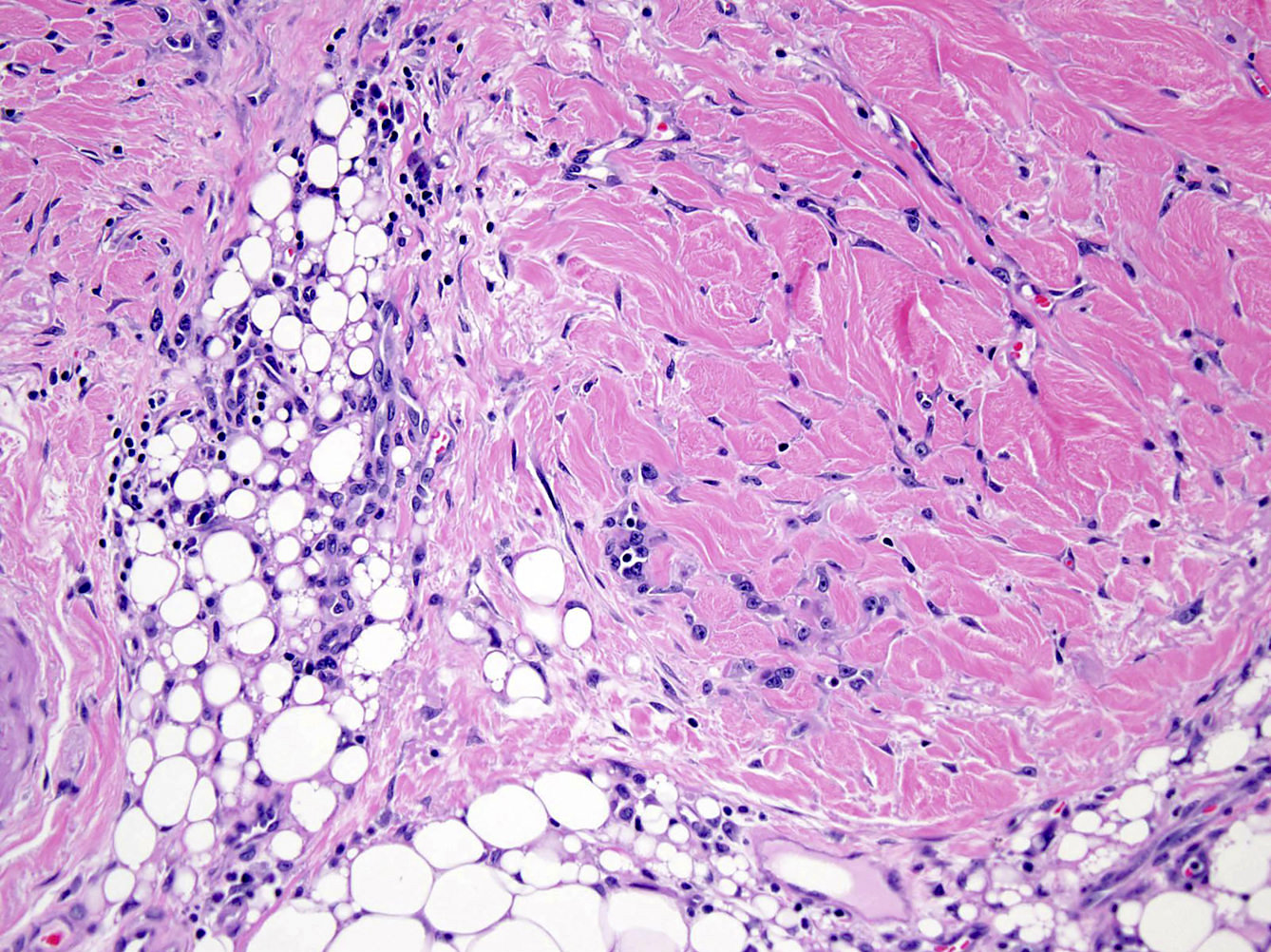
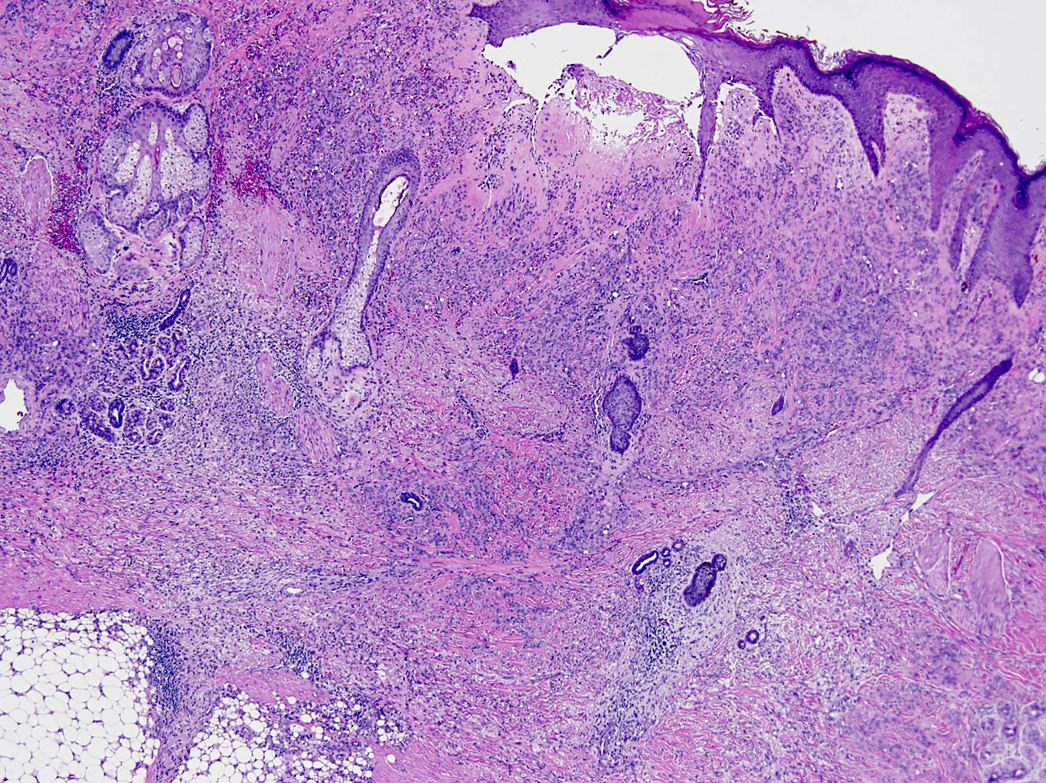
- Poorly circumscribed lesion with infiltrative borders, centered in the deep dermis and subcutis
- The most striking feature at low power is the variability in appearance from area to area
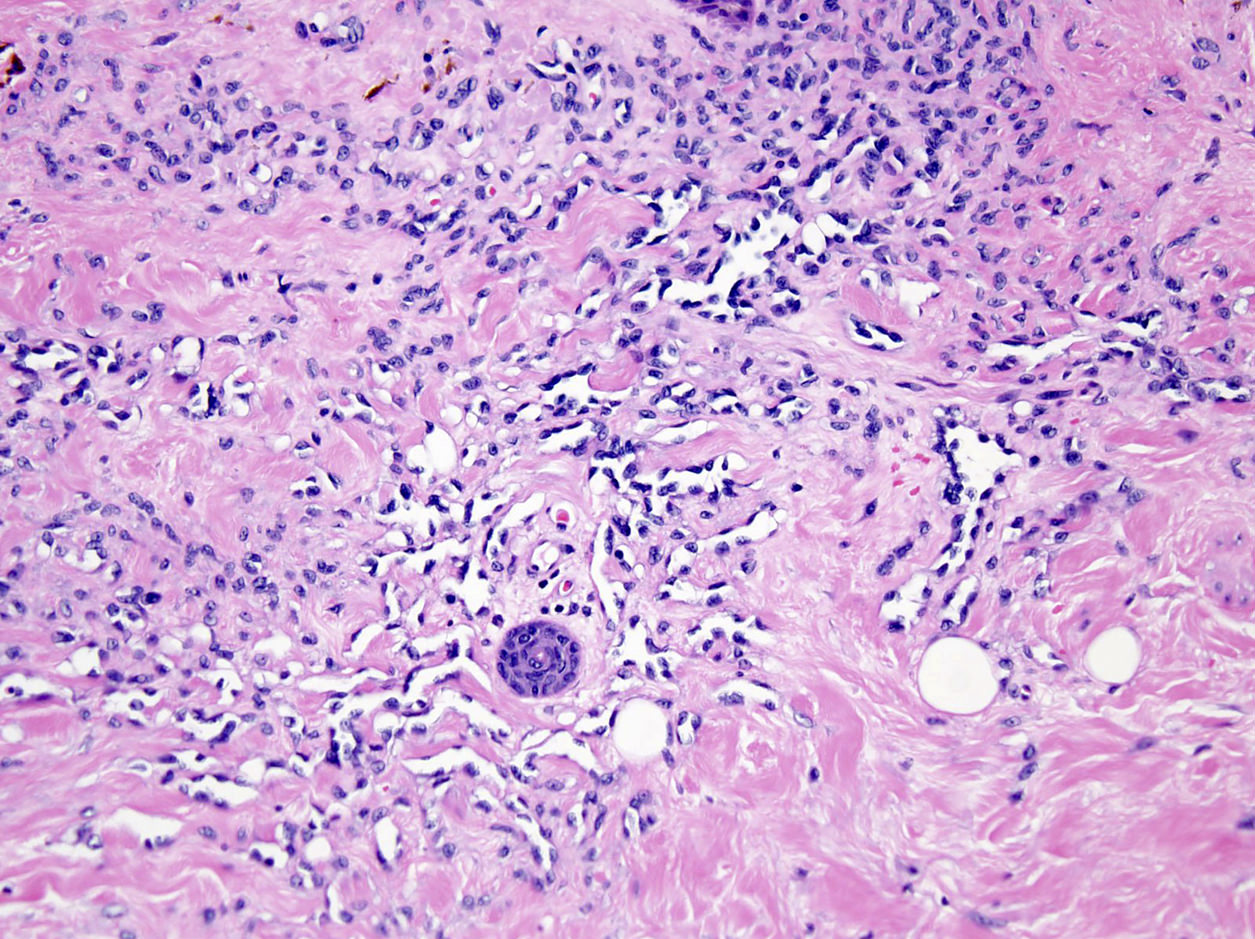
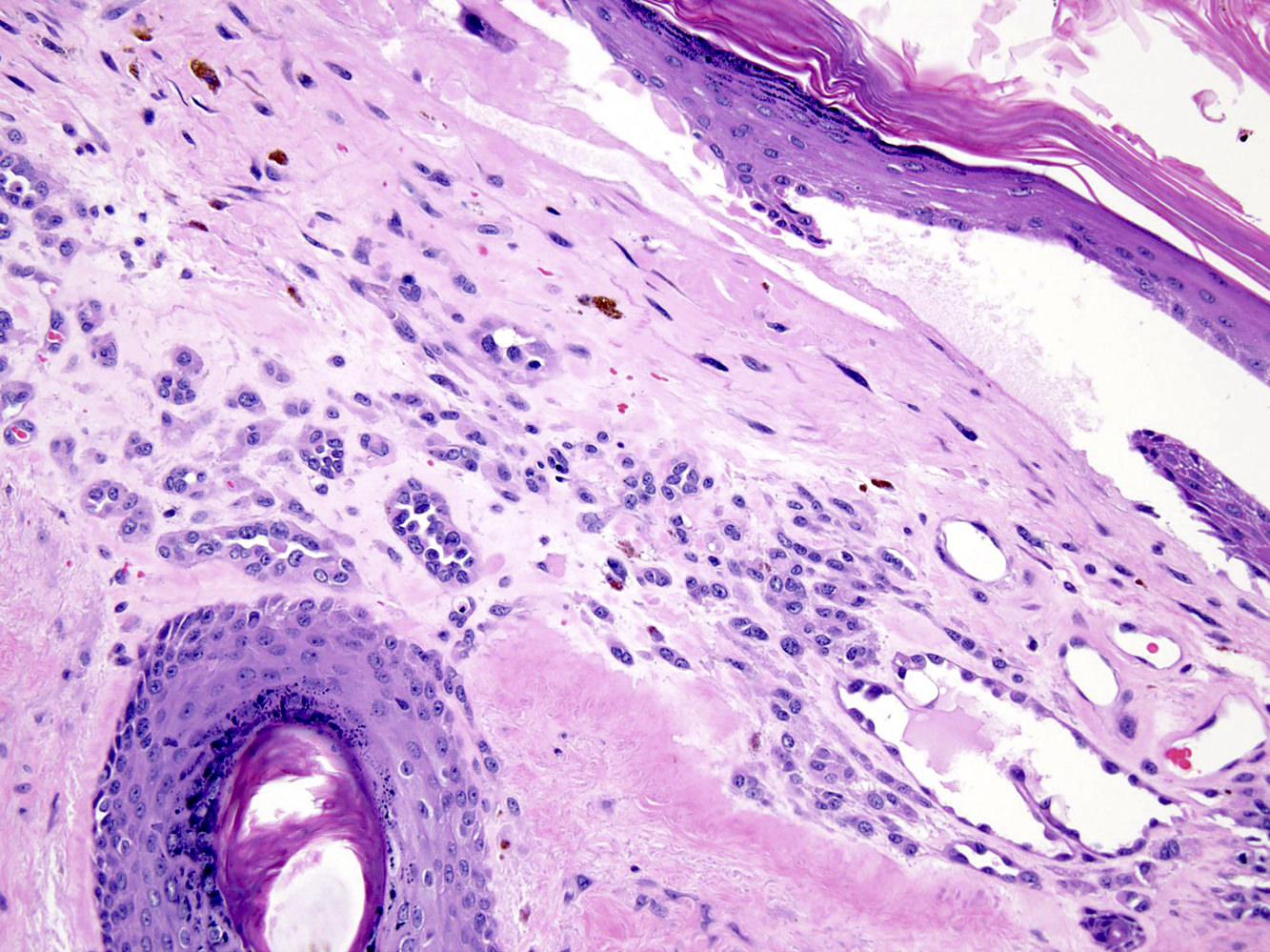
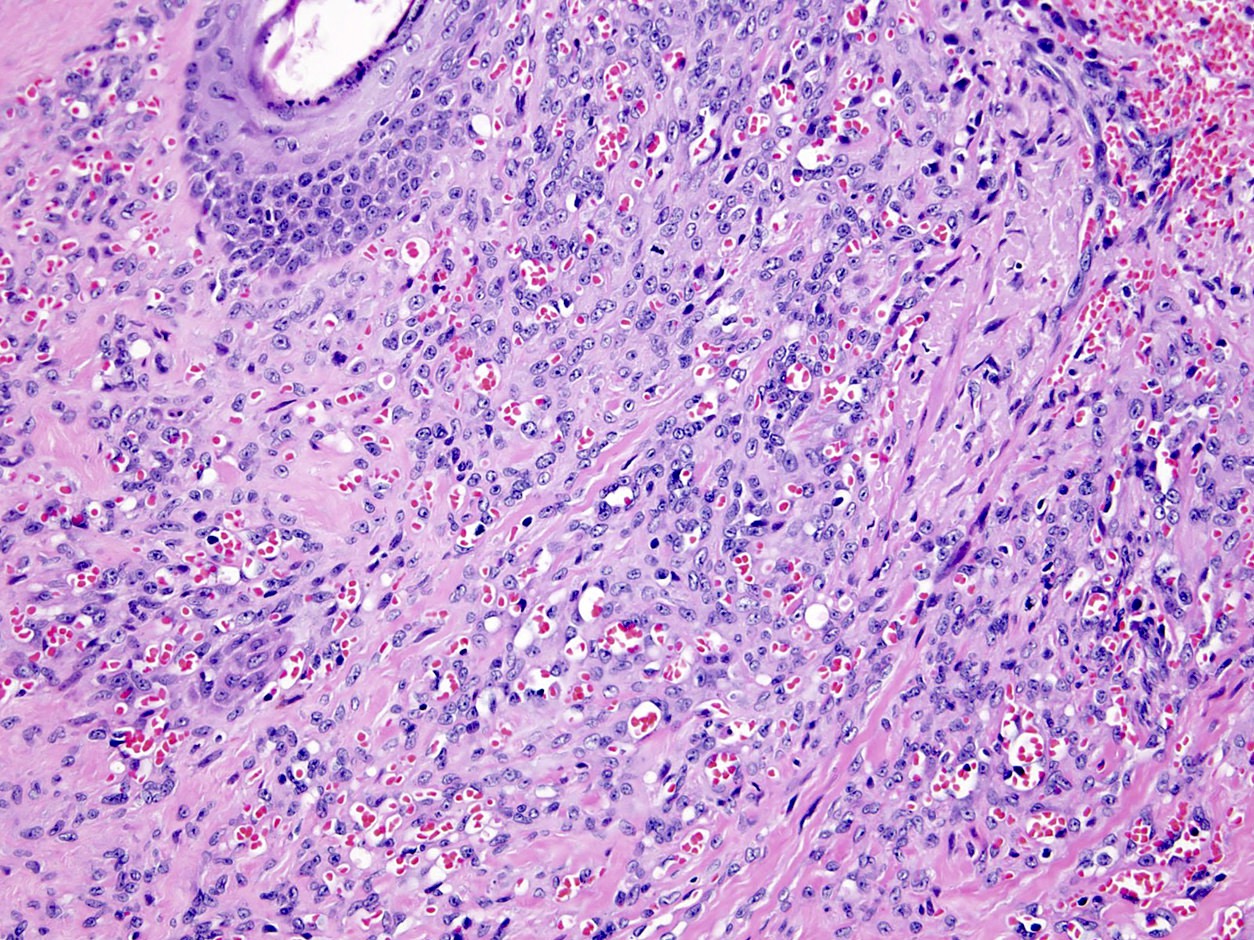
- Admixture of different vascular components, including but not limited to:
- Epithelioid hemangioendothelioma
- Retiform hemangioendothelioma
- Low grade angiosarcoma
- Lymphangioma
- Hemangioma (spindle cell, capillary, cavernous, hobnail, epithelioid)
- Different components merge imperceptibly, making it difficult to identify the pure components
- Vacuolated epithelioid endothelial cells with pseudo lipoblastic appearance
- Few mitotic figures
Microscopic (histologic) images
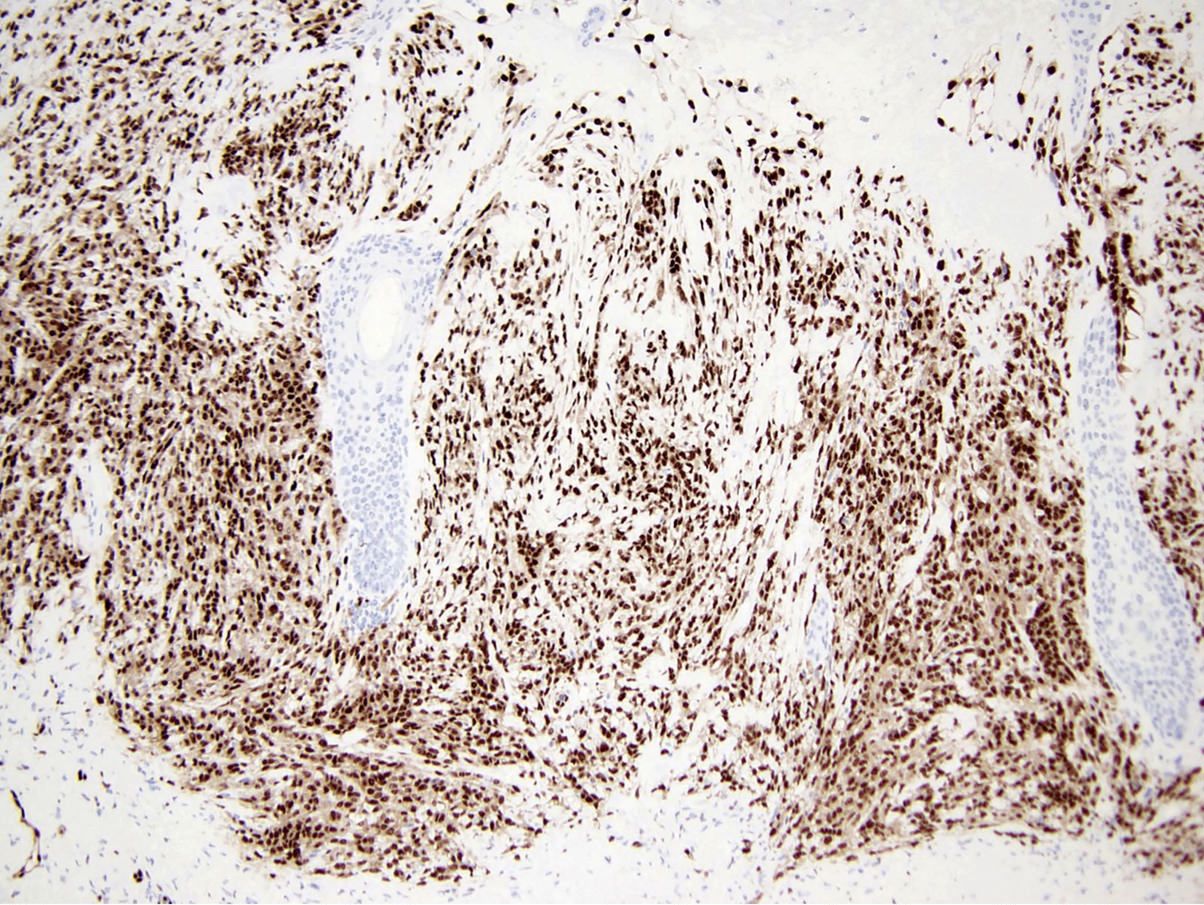
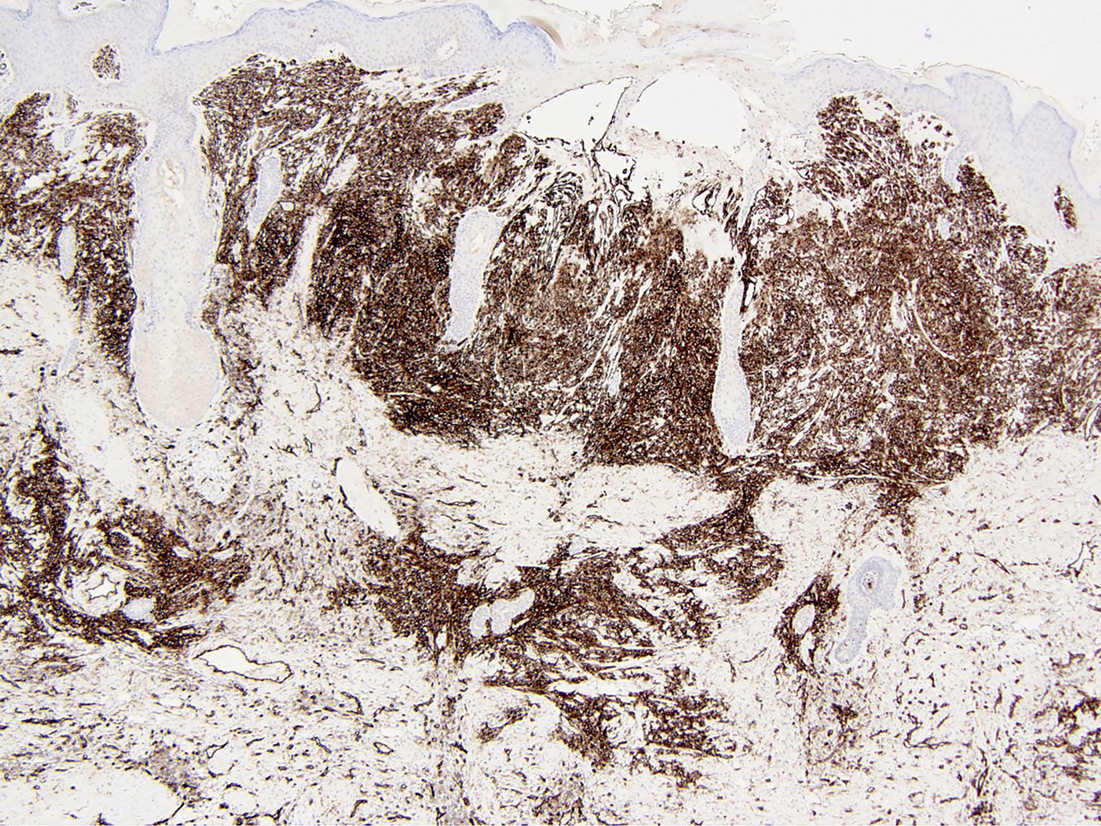
Positive stains
Negative stains
Sample pathology report
- Scalp, excision:
- Composite hemangioendothelioma (see comment)
- Tumor is closest at less than 0.1 cm from the specimen margin
- Comment: There is a poorly circumscribed, infiltrative lesion, which is centered in the dermis and subcutis. It comprises a complex admixture of vascular components, which include arborizing channels simulating the rete testis, chains and cord of eosinophilic epithelioid cells intermixed with large adipocyte-like cells, capillary sized vessels lined by epithelioid endothelial cells and superficial dilated vessels lined by small endothelial cells protruding into the lumina. Irregular anastomosing channels lined by mildly atypical endothelial cells are also noted. No coagulative tumor necrosis is seen. Immunohistochemically the lesional cells have strong expression of ERG and CD31 while are negative for HHV8. This constellation of morphological and immunohistochemical features strongly supports the diagnosis of composite hemangioendothelioma. It is vascular neoplasm prone to local recurrence unless completely excised, with intermediate (rarely metastasizing) malignant potential.
Differential diagnosis
- Distinguishing composite hemangioendothelioma from other vascular neoplasms largely lies in finding different histologic vascular patterns within 1 lesion
- Retiform hemangioendothelioma (Am J Surg Pathol 1994;18:115):
- Long arborizing blood vessels arranged in a retiform pattern (reminiscent of normal rete testis)
- Blood vessels lined by monomorphic hobnail endothelial cells with scant cytoplasm
- Very prominent lymphocytic infiltrate in most cases
- Focal presence of papillae with hyaline collagenous cores, similar to those seen in papillary intralymphatic angioendothelioma (Dabska tumor)
- Absence of endothelial atypia or mitotic activity
- Lymphatic marker PROX1 is positive (Am J Surg Pathol 2012;36:351)
- Other lymphatic markers, including podoplanin (D2-40) are usually but not always negative (J Cutan Pathol. 2009 Sep;36(9):987)
- CD31+, CD34+, ERG+
- Dabska type hemangioendothelioma (Cancer 1969 Sep;24:503):
- More common in infants and children
- Poorly delineated dermal or subcutaneous proliferation of lymphatic channels
- Distinctive intravascular growth of well differentiated columnar / matchstick-like / hobnail endothelial cells with eosinophilic cytoplasm and indistinct nucleoli (Am J Surg Pathol 1999;23:1004)
- Intraluminal papillary tufts with hyaline cores
- Varying degrees of stromal or intraluminal lymphocytes
- Minimal cytologic atypia and rare to absent mitotic activity
- D2-40+, VEGFR3+, CD31+, CD34 variable
- Kaposiform hemangioendothelioma:
- Tumor occurs nearly exclusively in children
- Often associated with Kasabach-Merritt phenomenon
- Typically seen in the retroperitoneum or deep soft tissues, although can occur in the skin and superficial soft tissues
- Features reminiscent of both capillary hemangioma and Kaposi sarcoma (Am J Surg Pathol 2004;28:559)
- Tumor nodules composed of fascicles of spindle shaped endothelial cells and slit-like or crescentic vascular channels (Int J Clin Exp Pathol 2015;8:13711)
- Tumor infiltrates soft tissue in a cannonball fashion
- Signature feature of the lesion is glomeruloid structures, which comprise tightly coiled capillary vessels invested with pericytes
- Glomeruloid structures are ERG+, CD31+ and CD34+
- Lymphatic markers (PROX1, D2-40, VEGFR3) are highly expressed in the slit-like vessels, whereas the glomeruloid structures lack these antigens (Am J Surg Pathol 2010;34:1563)
- HHV8-
- GLUT1-
- No tendency to regress
- Epithelioid hemangioendothelioma:
- Histologic hallmark of these tumors is the presence of chains and cords of round or slightly spindled eosinophilic endothelial cells with primitive lumen formation by single cells (Cancer 1982;50:970, Adv Anat Pathol 2014;21:254)
- Presence of focal vascular channels
- Distinct lack of mitotic activity or significant pleomorphism in most cases
- Myxohyaline stroma
- Recurrent translocations involving chromosomal regions 1p36.3 and 3q25, resulting in the formation of a WWTR1-CAMTA1 fusion gene in approximately 90% of cases
- A small subset (< 5%) have a YAP1-TFE3 fusion gene
- CAMTA1+, ERG+, CD31+, CD34+
- Most of CAMTA1 - tumor express TFE3 (Am J Surg Pathol 2016;40:94)
- Kaposi sarcoma:
- The disease is uniformly associated with human herpesvirus (HHV8) infection (Science 1994;266:1865, N Engl J Med 2019;380:1181)
- Patch stage:
- Abnormal vessels lined by thin endothelial cells dissecting the dermis
- Ramifying proliferating vessels often surround larger ectatic vessels, producing the so called promontory sign (not pathognomonic for Kaposi sarcoma)
- Plaque stage:
- All characteristic of the patch stage are exaggerated
- Vascular spaces show jagged outlines
- Nodular stage:
- Well circumscribed, cellular nodules of intersecting fascicles of spindle cells and numerous slit-like spaces containing erythrocytes
- Variable chronic inflammatory infiltrate composed of lymphocytes, plasma cells, and dendritic cells
- Several histologic variants of Kaposi sarcoma have been described, including anaplastic Kaposi sarcoma (Arch Pathol Lab Med 2013;137:289)
- ERG+, CD31+, D2-40+, HHV8+
- Angiosarcoma (J Clin Pathol 2017;70:917):
- Wide range of morphological appearances ranging from areas of well formed, anastomosing vessels to solid sheets of epithelioid or spindled cells without clear vasoformation
- Multiple patterns may be present in the same tumor
- Vast majority are high grade neoplasms with brisk mitotic activity, significant nuclear atypia and coagulative necrosis
- Amplification of MYC in 8q24 is a consistent hallmark of radiation induced and chronic lymphedema associated angiosarcoma (Genes Chromosomes Cancer 2011;50:25, Am J Pathol 2010;176:34)
- ERG+, CD31+, CD34+, FLI1+, AE1 / AE3 variable, CAM5.2 variable
Additional references
Board review style question #1
Board review style answer #1
E. Distinguishing composite hemangioendothelioma from other vascular neoplasms largely lies in finding different histologic vascular patterns within 1 lesion
Comment here
Reference: Composite hemangioendothelioma
Comment here
Reference: Composite hemangioendothelioma
Board review style question #2
A 65 year old man presents with a poorly circumscribed, infiltrative lesion of the scalp, which is centered in the dermis and subcutis. H&E stained tissue sections demonstrate a complex admixture of vascular components, which include arborizing channels simulating the rete testis, chains and cord of eosinophilic epithelioid cells intermixed with large adipocyte-like cells, capillary sized vessels lined by epithelioid endothelial cells and superficial dilated vessels lined by small endothelial cells protruding into the lumina. Irregular anastomosing channels lined by mildly atypical endothelial cells are also noted. Rare mitoses are seen (up to 2 mitoses/10 high power fields). Immunohistochemically the lesional cells have strong expression of ERG and CD31 while are negative for HHV8. Which of the following is most likely the correct diagnosis?
- Angiosarcoma
- Composite hemangioendothelioma
- Epithelioid hemangioendothelioma
- Kaposi sarcoma
- Pseudomyogenic hemangioendothelioma
Board review style answer #2