Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3 | Board review style question #4 | Board review style answer #4 | Board review style question #5 | Board review style answer #5Cite this page: Wang J, Cui J. Tenosynovial giant cell tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuegctlocal.html. Accessed December 24th, 2024.
Definition / general
- Tenosynovial giant cell tumor encompasses a group of lesions that most often arise from the synovium of joints, bursae and tendon sheaths and show synovial differentiation
- Malignant tenosynovial giant cell tumor is very uncommon and is defined by the coexistence of a benign tenosynovial giant cell tumor with overtly malignant areas or by recurrence of a typical giant cell tumor as a sarcoma
Essential features
- Localized type
- Second most common tumor of the hand (after ganglion cyst)
- Well circumscribed and lobulated, usually in close association with a tendon
- Composed of variable proportions of large epithelioid mononuclear cells, macrophages and osteoclast-like giant cells
- Diffuse type
- Intra-articular tumors within large joints
- Extra-articular invasive tumors of tendon sheath, bursa or soft tissue origin
- Malignant
- Only ~50 cases were reported
- Contains definite sarcomatous area
- Arises de novo or occurs after multiple recurrences of a conventional tenosynovial giant cell tumor
Terminology
- Acceptable: giant cell tumor of tendon sheath
- Not recommended: pigmented villonodular synovitis
ICD coding
- ICD-O: 9252/0 - tenosynovial giant cell tumor, NOS
- ICD-10: D48.1 - neoplasm of uncertain behavior of connective and other soft tissue
- ICD-11:
- 2F7Z & XH6911 - neoplasms of uncertain behavior of unspecified site & tenosynovial giant cell tumor, localized
- 2F7Z & XH52J9 - neoplasms of uncertain behavior of unspecified site & tenosynovial giant cell tumor, diffuse
- 2D4Y & XH5AQ9 - other specified malignant neoplasms of ill defined or unspecified primary sites & malignant tenosynovial giant cell tumor
Epidemiology
- Localized type
- 40 patients/1 million
- Fourth or fifth decade of life (most frequently)
- F:M = 2:1
- Diffuse type (NIH: SEER Cancer Statistics Review, 1975-2010 [Accessed 24 November 2021])
- Annual incidence rate: 1.8 patients/1 million in United States
- Peaks in the third and fourth decades of life with an average of 35 years
- Female predominance
- Malignant
- Uncommon
- Middle aged to older adults (most are 50 - 60 years)
Sites
- Localized type
- Predominantly occurs in the digits (85%), especially fingers (75%)
- Uncommon around large joints (10%)
- Intra-articular localized tenosynovial giant cell tumors are most frequent in the knee
- Diffuse type (Lancet Oncol 2019;20:877)
- Intra-articular
- Knee (65%)
- Hip and ankle (25%)
- Elbow, shoulder, temporomandibular joint, spine
- Extra-articular extension
- Knee
- Foot, wrist, inguinal, elbow region, digits
- Intra-articular
- Malignant
- Often occurs in the lower extremities
Pathophysiology
- Translocation of the CSF gene that encodes colony stimulating factor 1 (CSF1) was frequently involved in this tumor
- It is reported that tumor cells with CSF1 translocation synthesize large amounts of the CSF1 protein
- Actually, only a small subset of cells harbor the translocation
Etiology
- Unknown
Clinical features
- Localized type (Orthop Traumatol Surg Res 2017;103:S91)
- Skin colored nodule without specific features
- Most are slow growing and painless
- Diffuse type (J Rheumatol 2017;44:1476)
- Painful mass, long duration
- Hemorrhagic joint effusion
- Decreased range of motion
- Malignant (Mod Pathol 2019;32:242)
- Similar to their benign counterparts in tumor location
- Recurrence or metastasis to regional lymph nodes and distant locations
Diagnosis
- Localized type (Orthop Traumatol Surg Res 2017;103:S91)
- Usually, diagnosis via ultrasound and pathology
- Diffuse type and malignant (Orthop Traumatol Surg Res 2017;103:S91)
- Diagnosis via radiology and pathology
Laboratory
- Nonspecific
Radiology description
- Localized type
- Xray (Orthop Traumatol Surg Res 2017;103:S91):
- Most commonly demonstrates a soft tissue mass, some of which demonstrate bony erosion
- Ultrasonography (AJR Am J Roentgenol 2004;183:337):
- Lesion does not move with the tendon during flexion / extension
- Solid, not cystic (helps to differentiate from ganglion cyst)
- MRI findings (Skeletal Radiol 2021;50:1585):
- Well demarcated
- Associated with a tendon (and in some instances encasing a tendon)
- May have variability in signal intensity but in general will have foci of low intensity on T1 and T2 weighted images from hemosiderin
- Xray (Orthop Traumatol Surg Res 2017;103:S91):
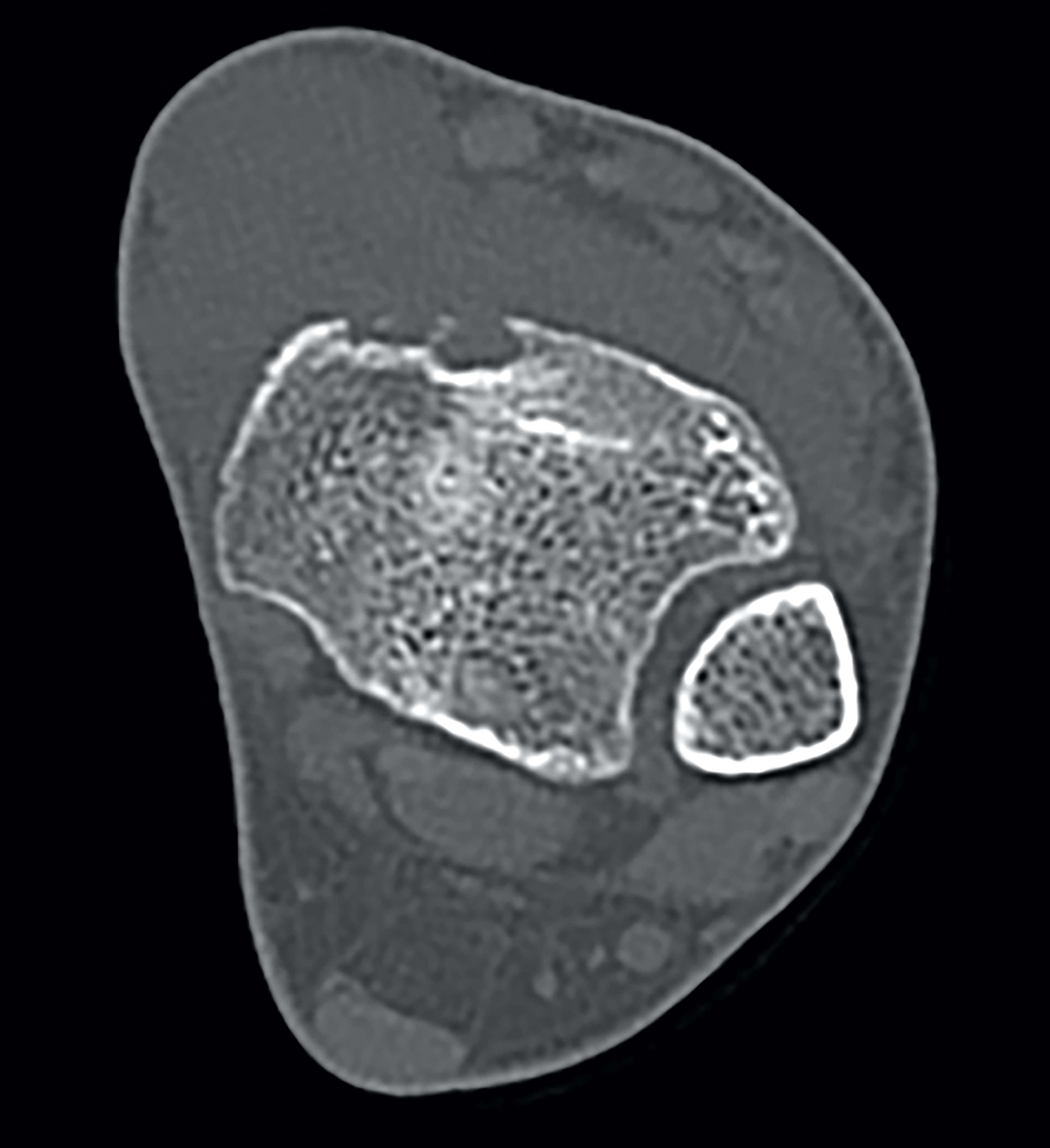
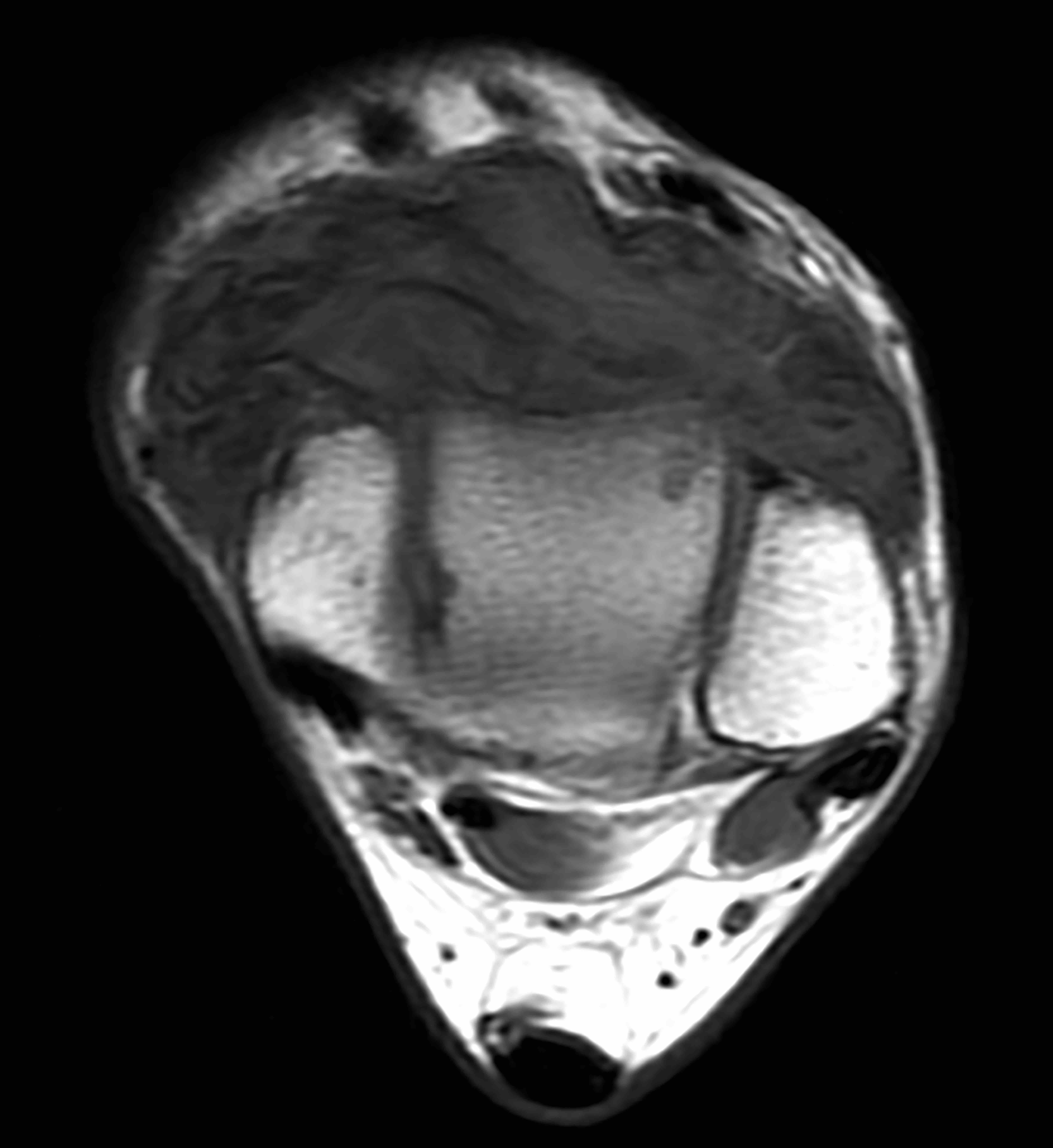
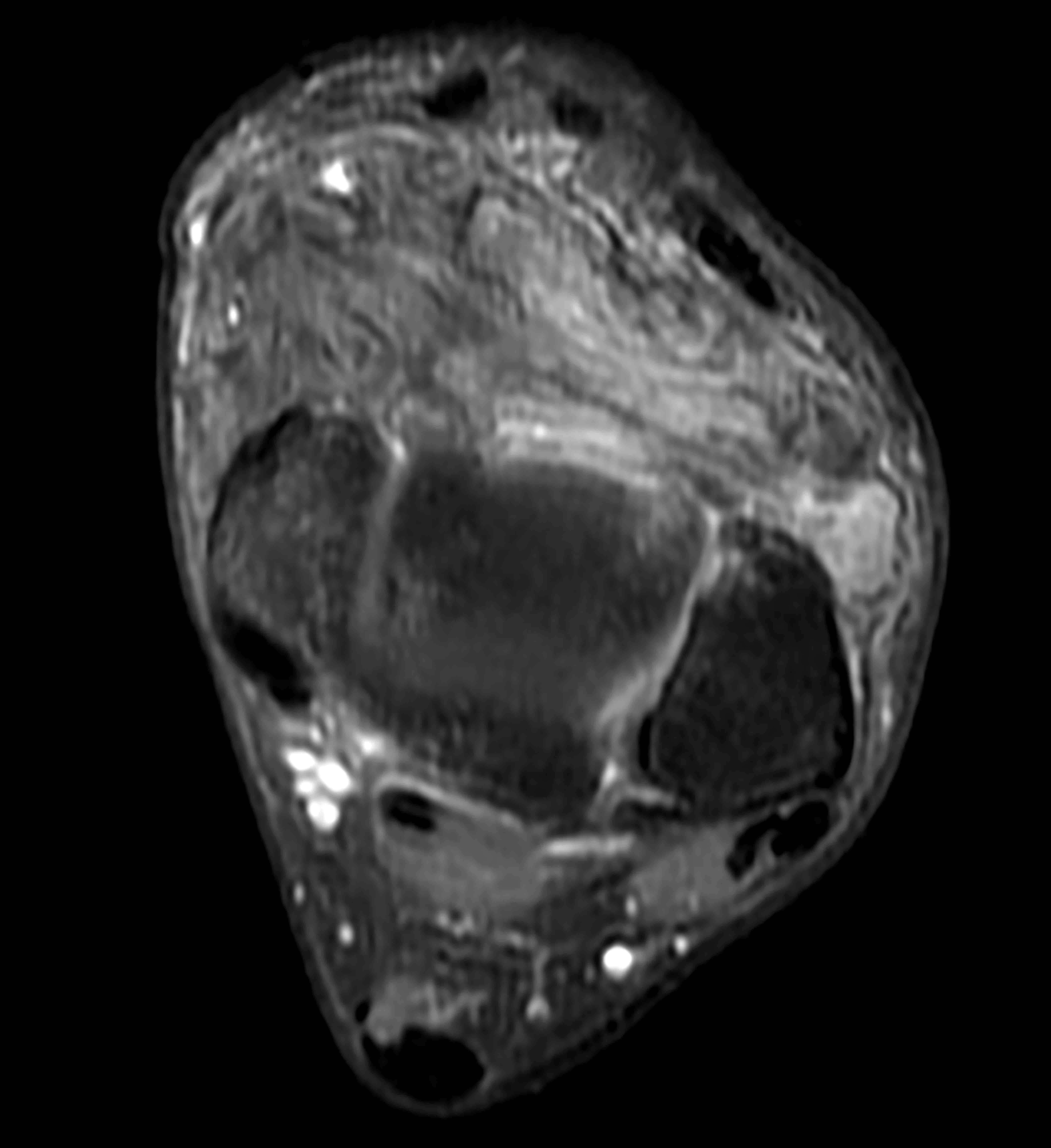
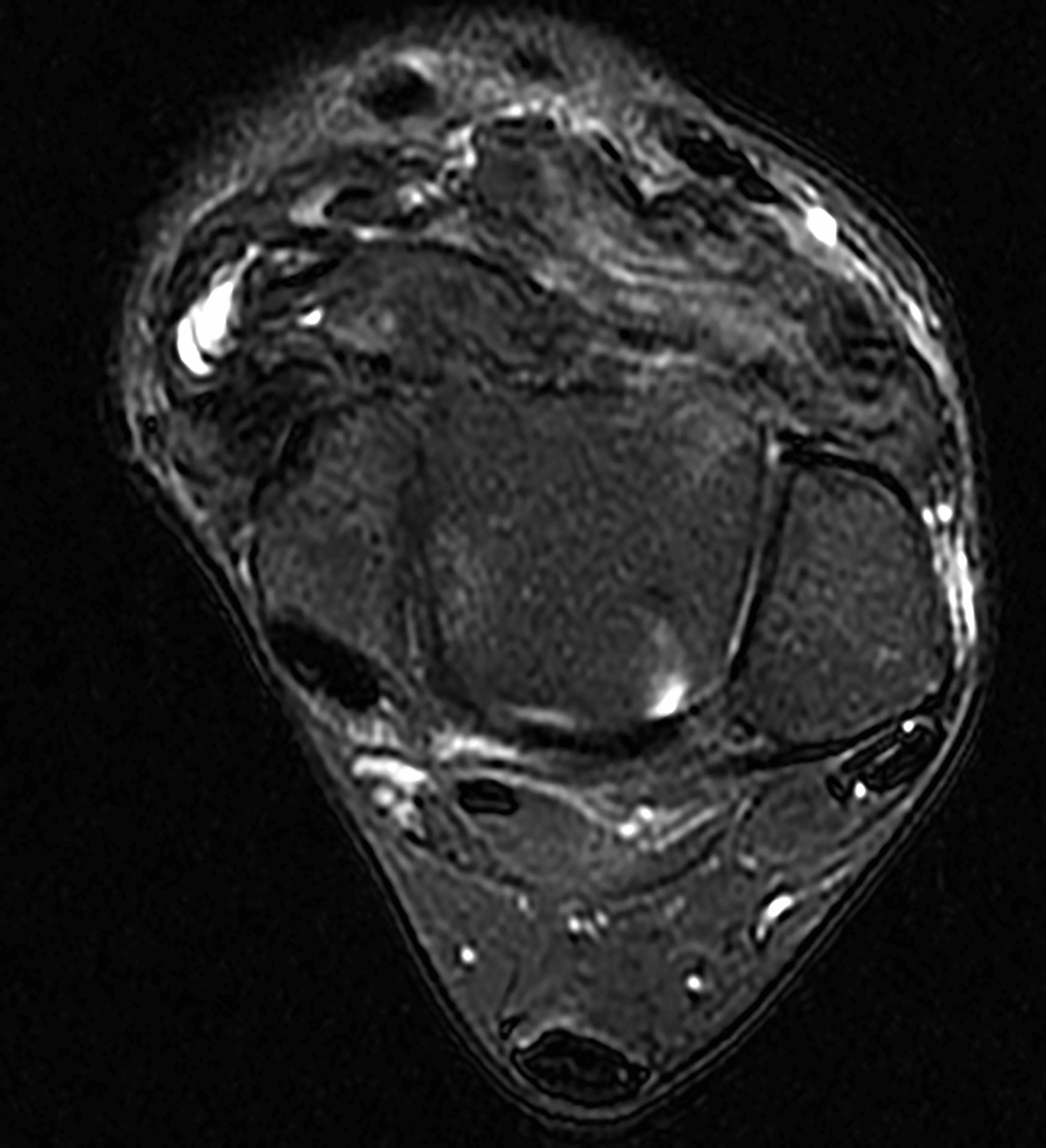
- Diffuse type
- Xray and CT (Orthop Traumatol Surg Res 2017;103:S91):
- Ill defined periarticular soft tissue mass
- Bone erosion is common
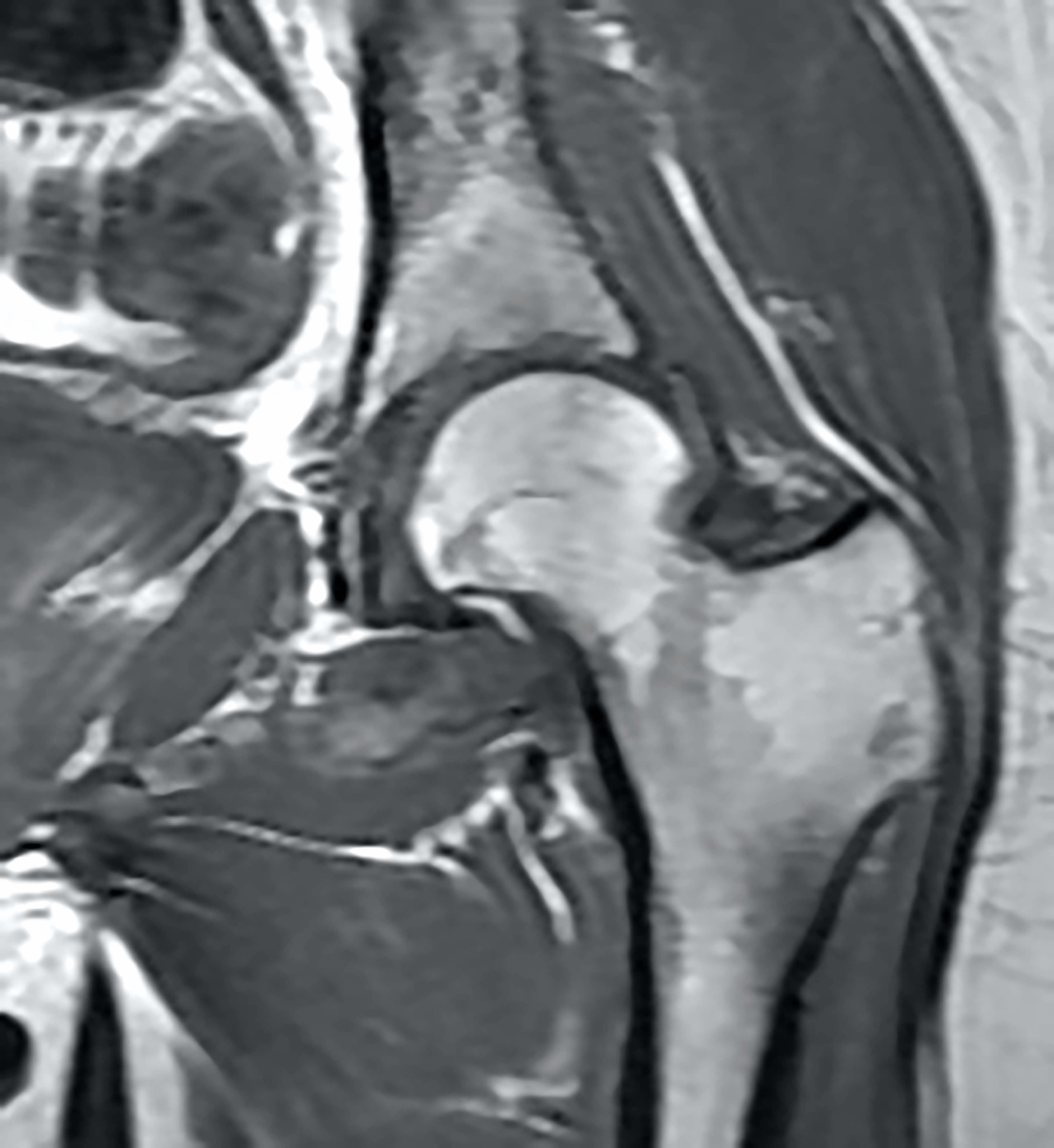
- MRI findings (Skeletal Radiol 2021;50:1585):
- Low signal on T1 and T2
- Enhancement with contrast
- MR signal voids secondary to hemosiderin
- Xray and CT (Orthop Traumatol Surg Res 2017;103:S91):
- Malignant
- Xray and CT (J Clin Imaging Sci 2015;5:13):
- May show extensive bone destruction
- Xray and CT (J Clin Imaging Sci 2015;5:13):
Radiology images
Contributed by Jigang Wang, M.D., Ph.D. and Jiufa Cui, M.D., Ph.D.
Diffuse type
Images hosted on other servers:
Prognostic factors
- Localized type
- Benign but recurs locally (10 - 20%)
- Risk factors for recurrence include degenerative joint disease and osseous erosion
- Diffuse type (Eur J Cancer 2015;51:210)
- High recurrence rate
- Risk factors for recurrence are still unknown
- It is very rare that tumors progress to malignancy or metastasize
- Malignant
- Risk factors for recurrence are still unknown
Case reports
- Localized type
- 31 year old man presented with a tumor in the right middle finger (J Korean Med Sci 1999;14:682)
- 66 year old woman presented with a painful growth of her right index finger (BMJ Case Rep 2020;13:e231902)
- 71 year old man presented with a 5 year history of a slowly growing, painless mass in the right thumb (Anticancer Res 2020;40:4373)
- 72 year old man presented with a tumor of his left hand (Int J Surg Pathol 2020;28:447)
- 83 year old man presented with a 2 year history of a slowly growing solitary nodule on the distal end of his left middle finger (Arch Dermatol 2009;145:931)
- Diffuse type
- 22 year old woman presented with a palpable posterior neck mass (Skeletal Radiol 2021;50:451)
- 41 year old woman developed multiple metastases from diffuse tenosynovial giant cell tumor with benign histological features (J Orthop Surg (Hong Kong) 2017;25:2309499017690323)
- 74 year old man presented with gradual onset of pain, hemarthrosis and functional impairment of the right shoulder (Eur J Rheumatol 2017;4:142)
- 74 year old woman presented with an enlarging left thigh mass (Int J Surg Pathol 2019;27:59)
- Malignant
- 41 year old woman presented with a progressive increasing mass in the upper left thigh (Anticancer Drugs 2020;31:80)
- 50 year old man presented with a slowly progressing, painless swelling in the right knee (J Cytol 2017;34:174)
- 55 year old woman presented with progressively worsening right posterior calf pain (J Clin Imaging Sci 2015;5:13)
- 57 year old man with pleural metastases arising in the left knee (Hum Pathol 2017;63:144)
- 58 year old woman noticed a small mass on her left buttock (Pathol Int 2012;62:559)
Treatment
- Localized type
- Complete local excision
- Diffuse type (Eur J Cancer 2016;63:34)
- Surgical excision
- Wide local excision
- Total synovectomy
- Prosthetic joint replacement
- Amputation in advanced cases
- External beam radiotherapy
- Radiosynovectomy
- New therapeutic strategies
- Immunotherapy: anti-TNF-α drugs
- Targeted therapy: tyrosine kinase inhibitors, CSF inhibitors
- Surgical excision
- Malignant
- Local treatment
- Radical resection
- Systemic therapy
- Tyrosine kinase inhibitors (TKIs) had very limited activity in malignant tenosynovial giant cell tumor (BMC Cancer 2018;18:1296)
- CSF1R inhibitors
- Cytotoxic chemotherapy
- Local treatment
Clinical images
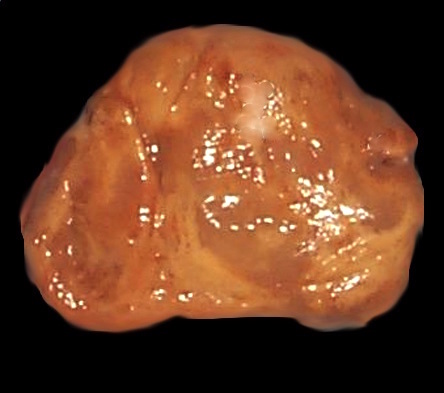
Gross description
- Localized type
- Well circumscribed and partially encapsulated with a lobulated appearance
- Variegated cut surface (yellow, tan, red-brown)
- Diffuse type
- Brown-yellow spongy tissue, firm and nodular, often 5 cm or larger
- Diffusely covers most of synovial surface
- Villous, nodular or villonodular
- Poorly demarcated from adjacent tissues
- Malignant
- Similar to benign but may be larger
- Sarcomatous area showed a solid growth pattern with whitish color, massive hemorrhage and necrosis (Pathol Int 2012;62:559)
Gross images
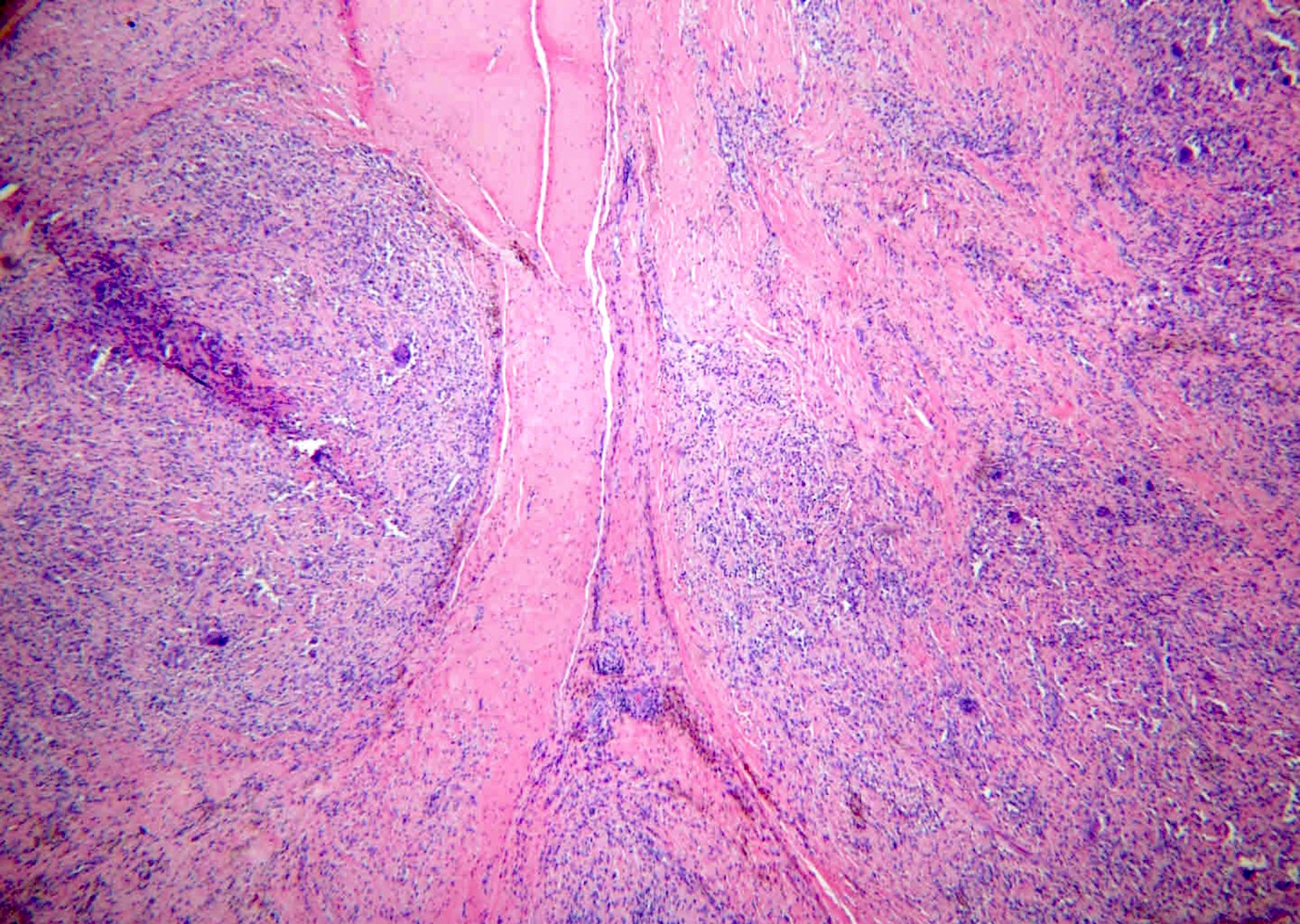
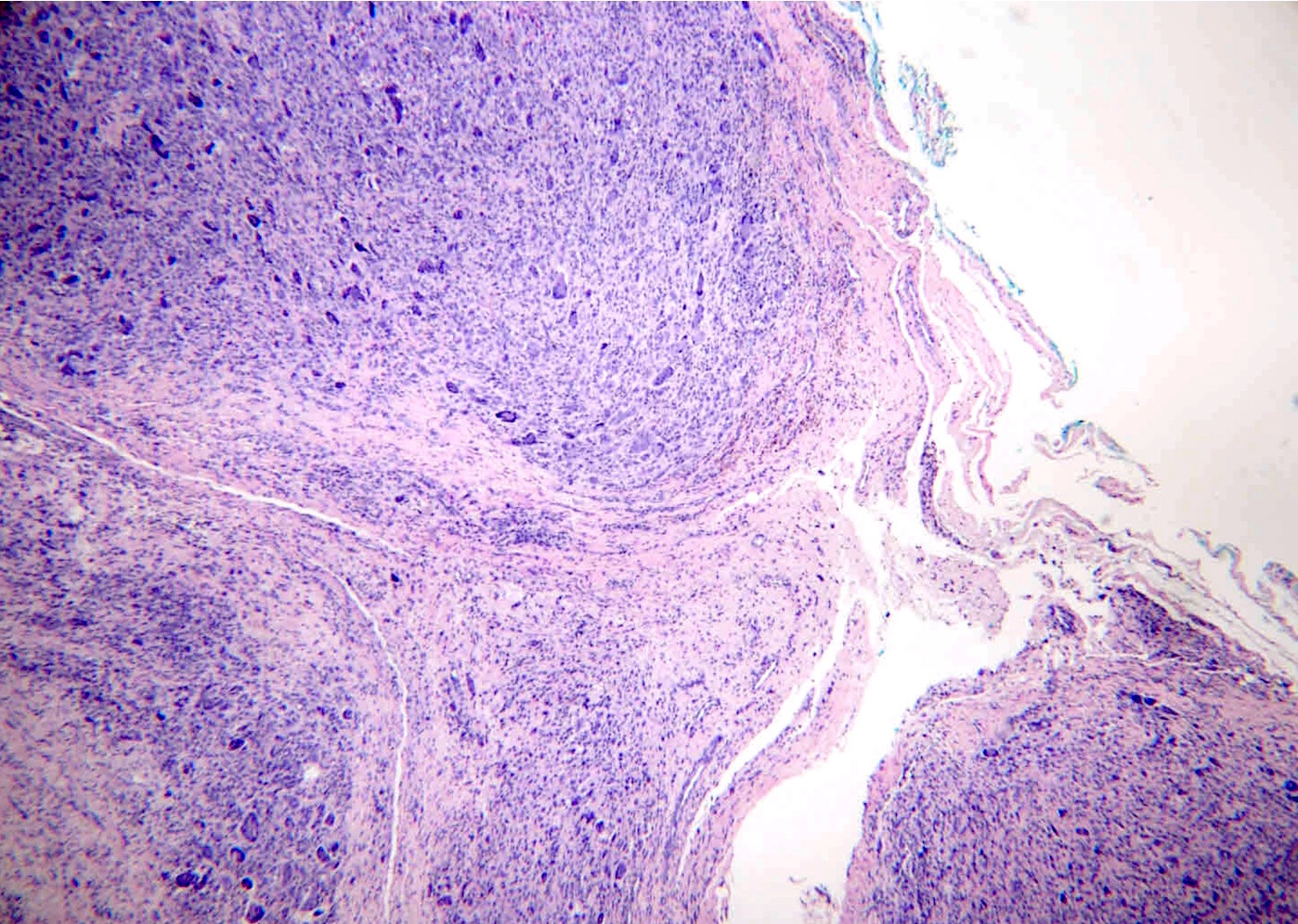
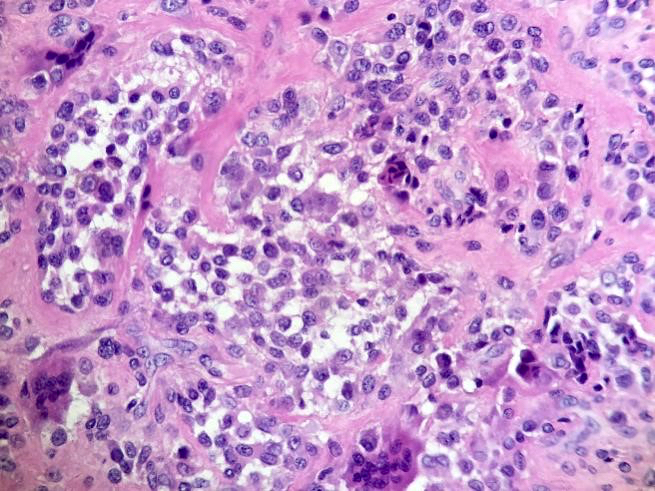
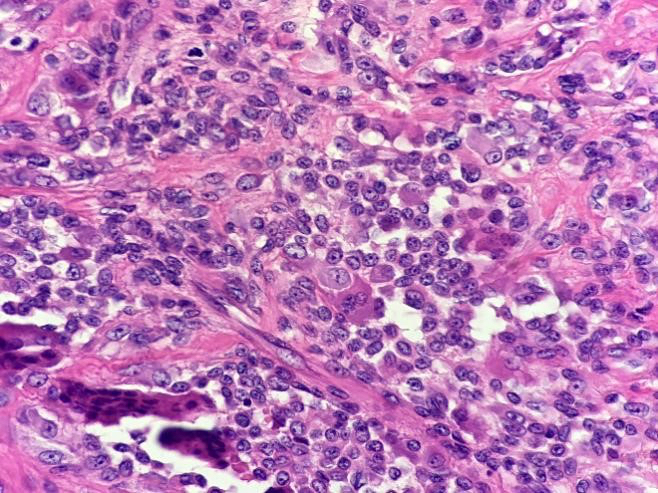
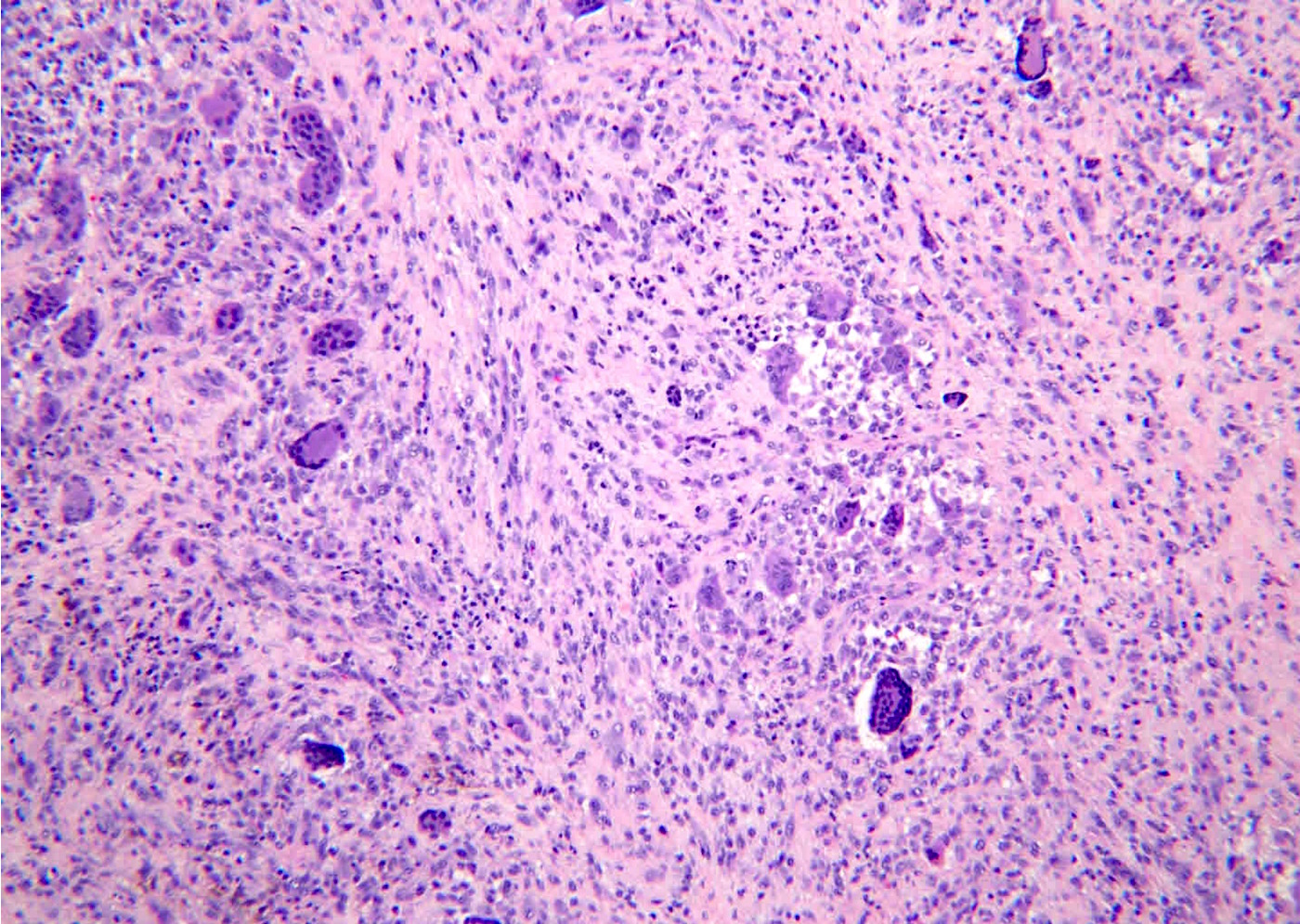
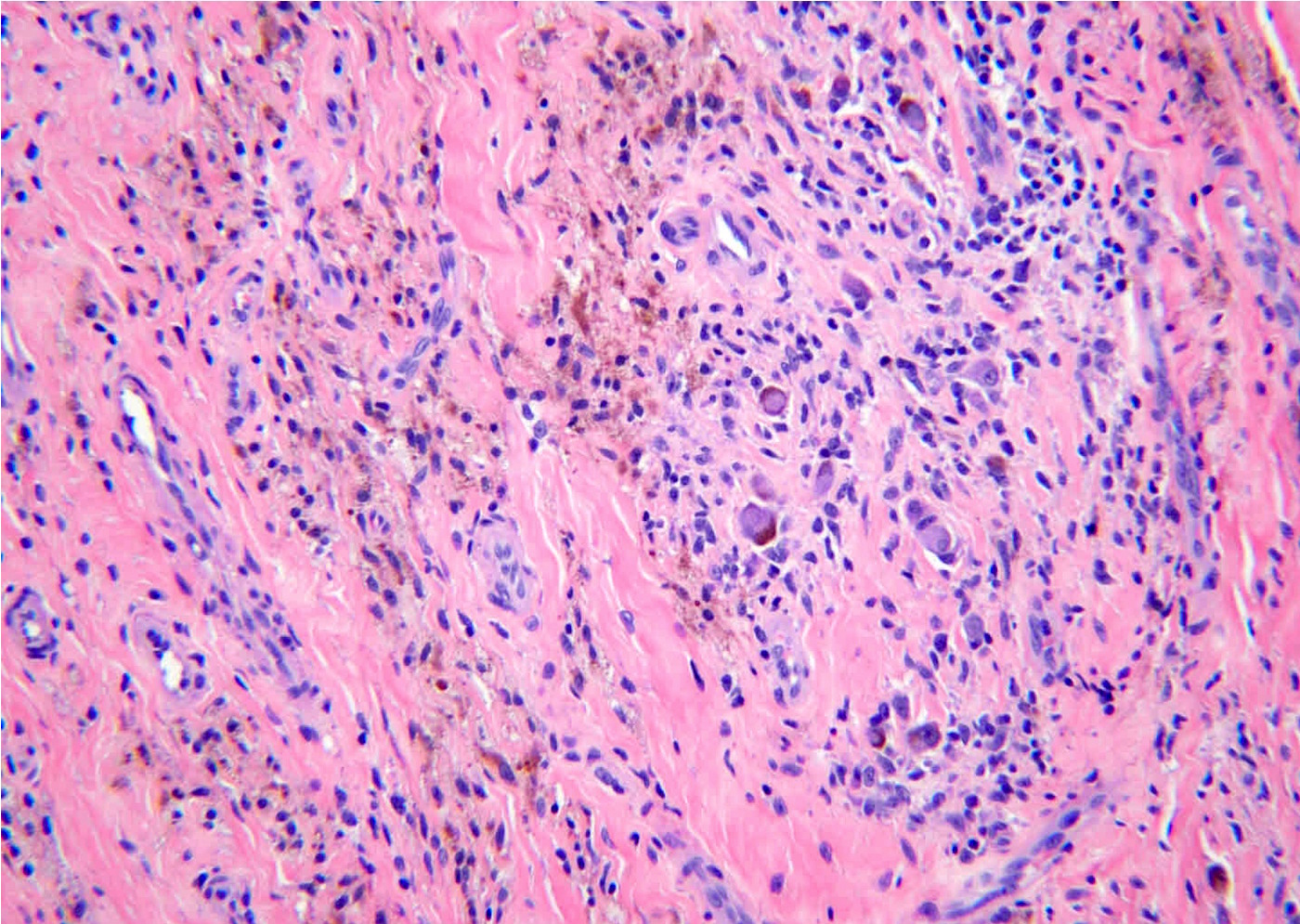
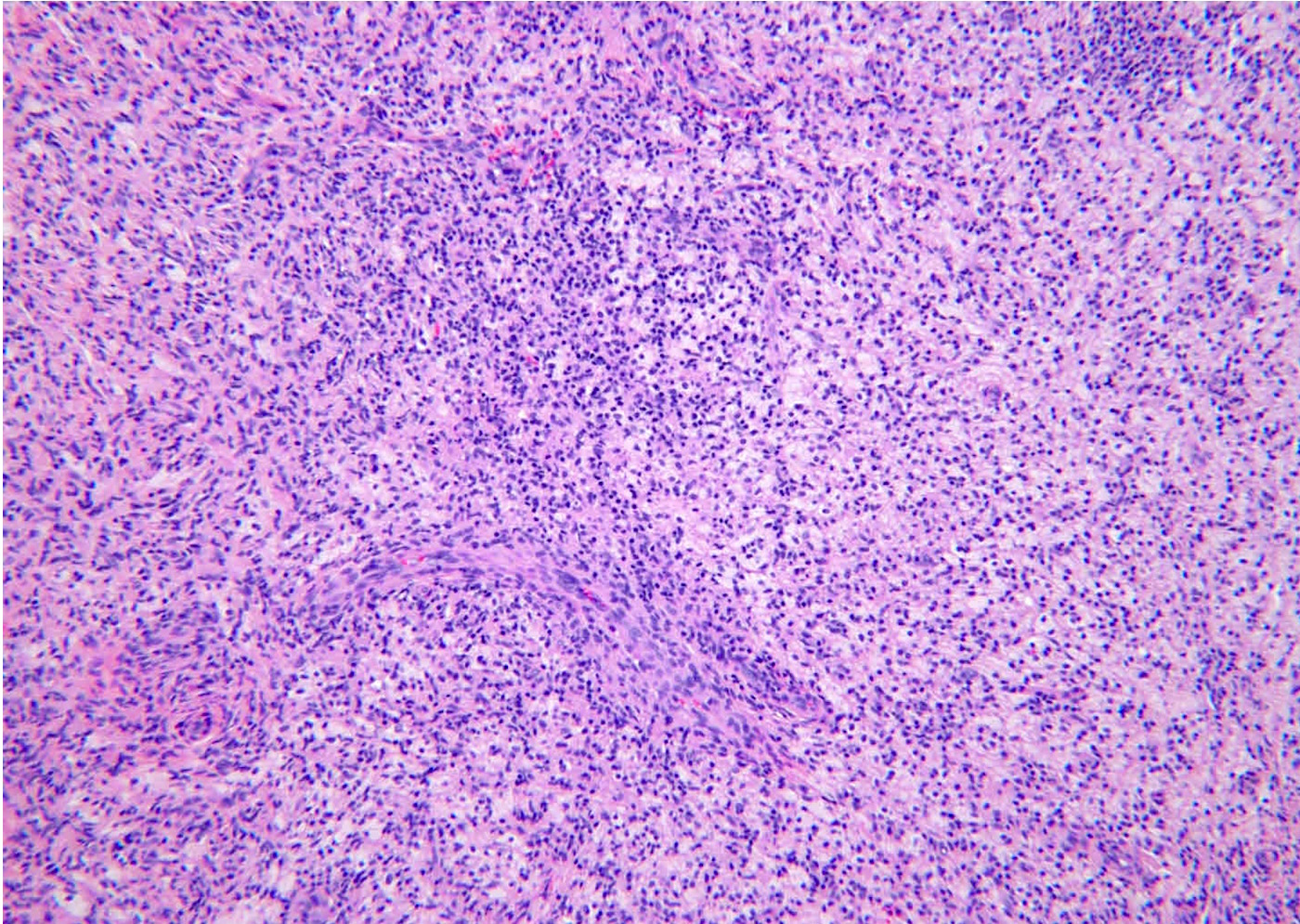
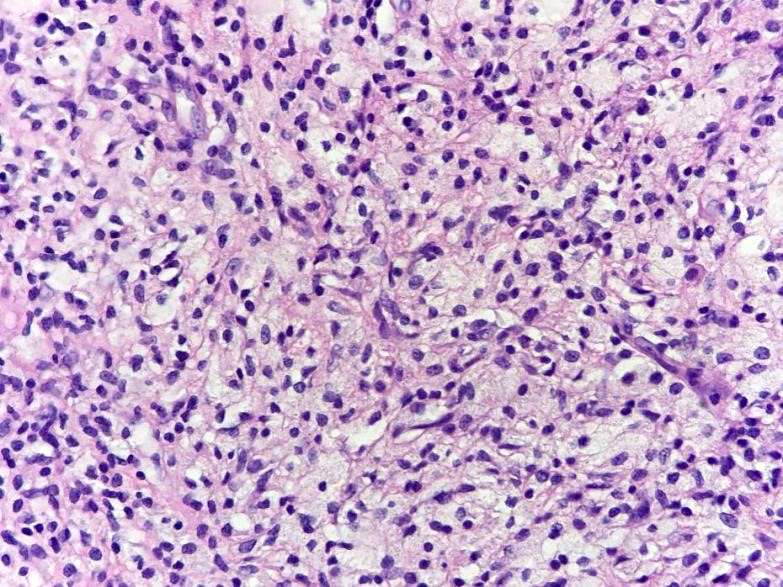
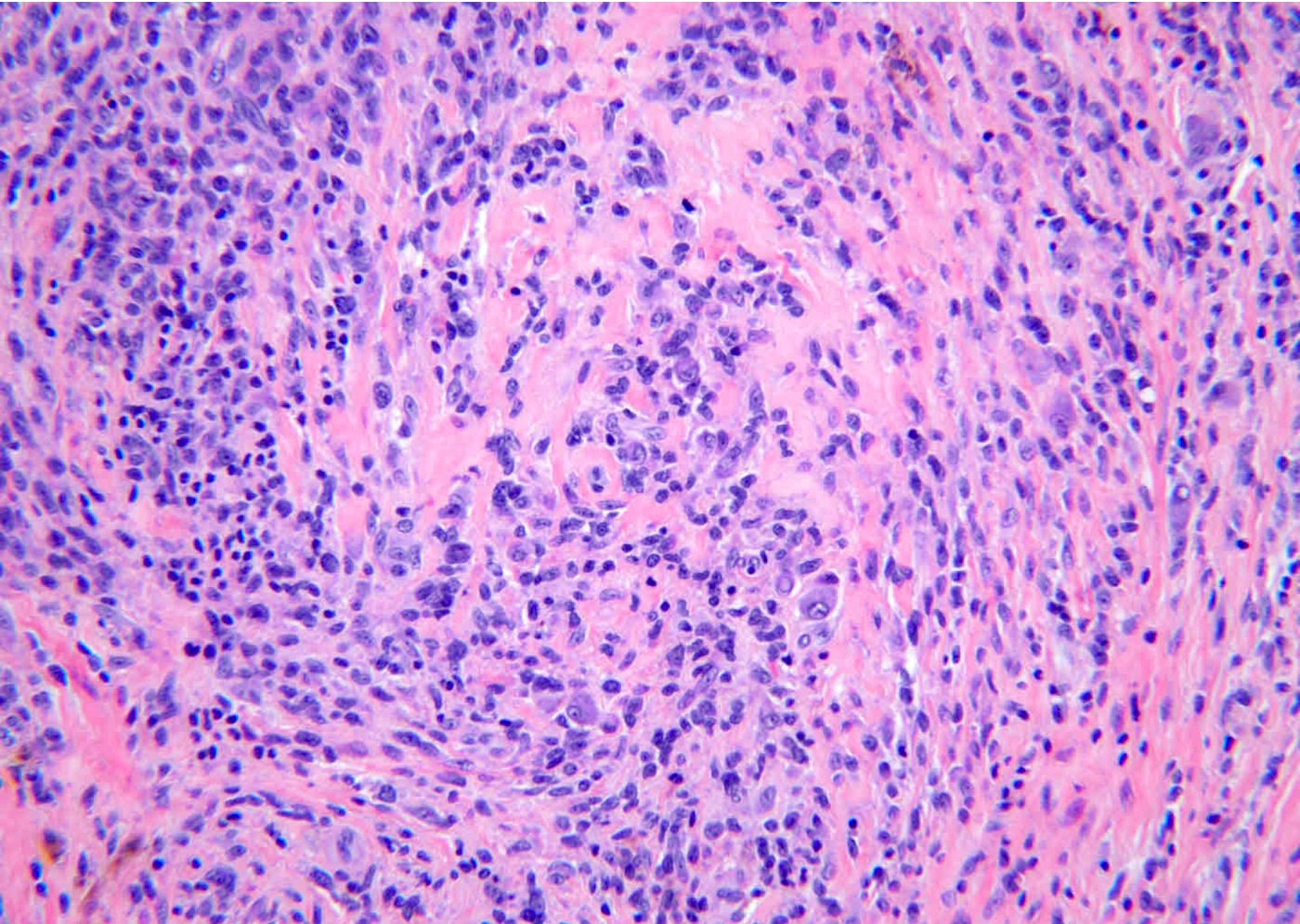
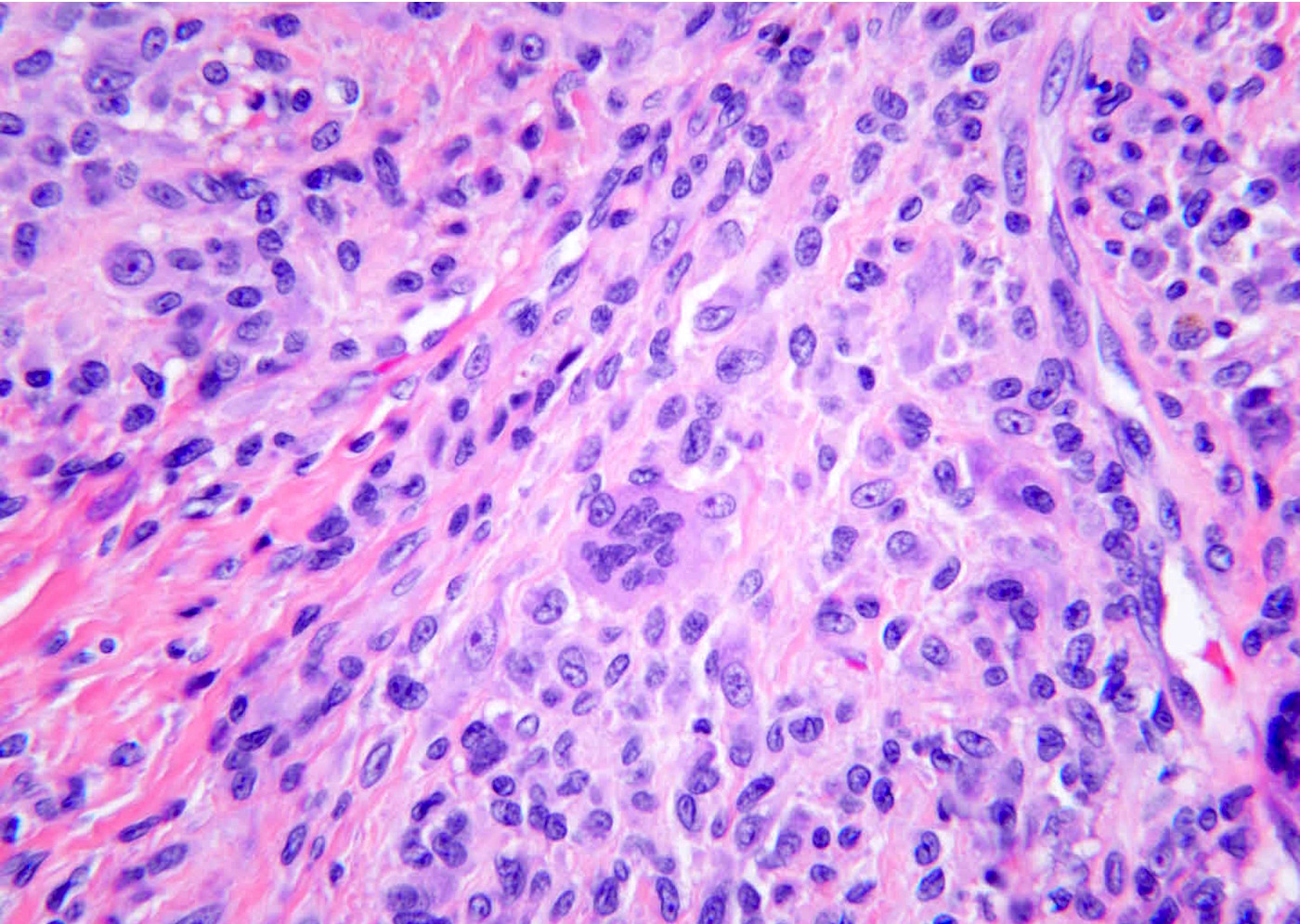
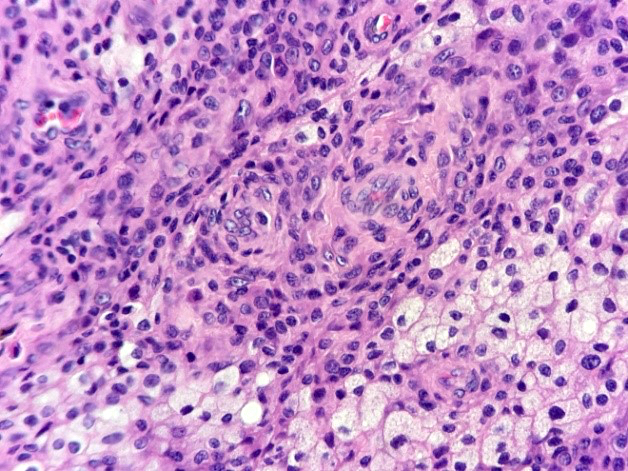
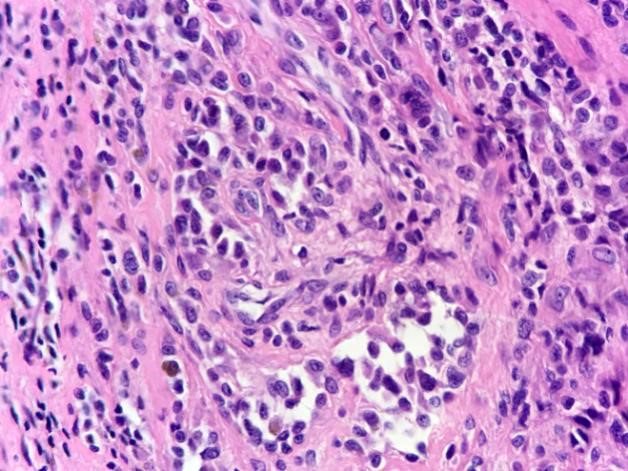
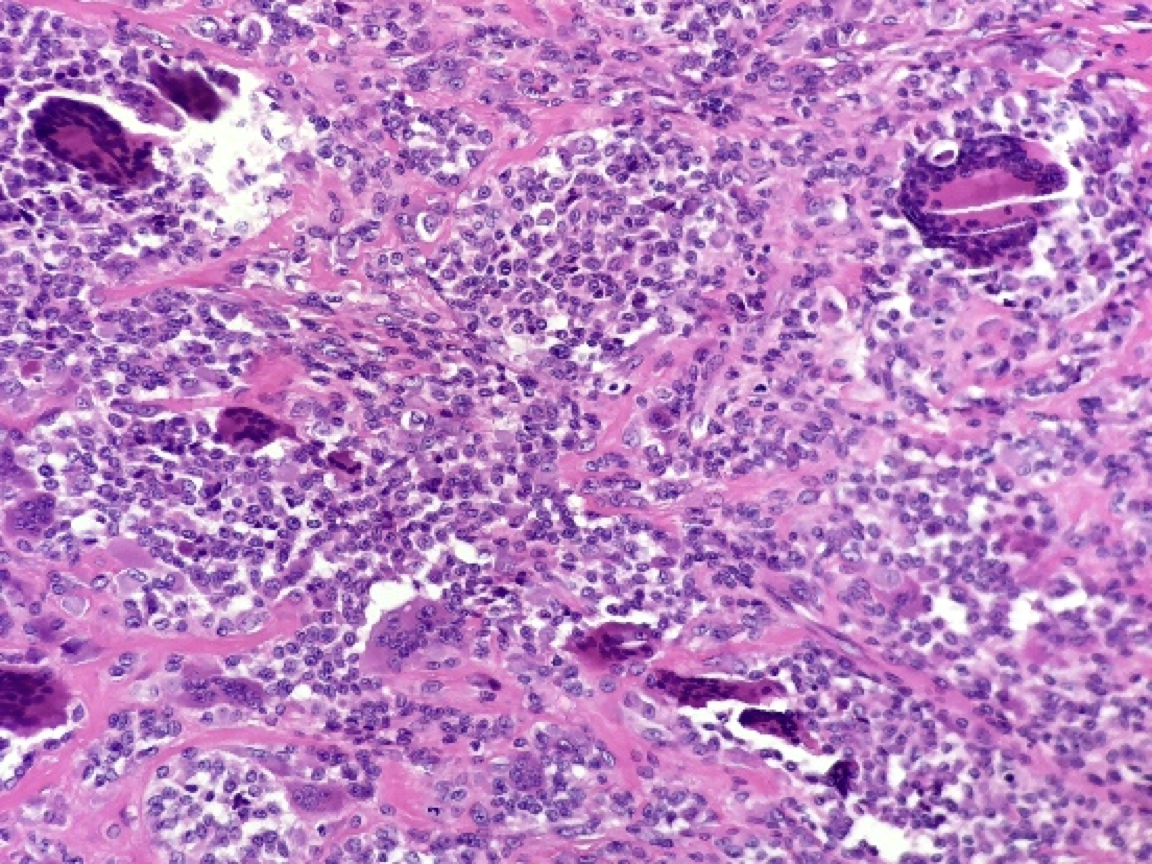
Microscopic (histologic) description
- Composed of mononuclear cells, multinucleated giant cells, foamy macrophages, inflammatory cells and hemosiderin
- 2 principal cell types of the mononuclear components:
- Small histiocyte-like cells: pale cytoplasm and round or reniform nuclei
- Large epithelioid cells: amphophilic cytoplasm and rounded vesicular nuclei, often containing a peripheral rim of hemosiderin granules
- Mitotic activity may be brisk
- Necrosis can be present
- Localized type (J Surg Oncol 1998;68:100)
- Lobulated and well circumscribed
- Osteoclast-like giant cells are usually readily apparent
- Xanthoma cells are frequent, tend to aggregate locally near the periphery of nodules, and may be associated with cholesterol clefts
- Hemosiderin deposits
- Stroma showed variable degrees of hyalinization
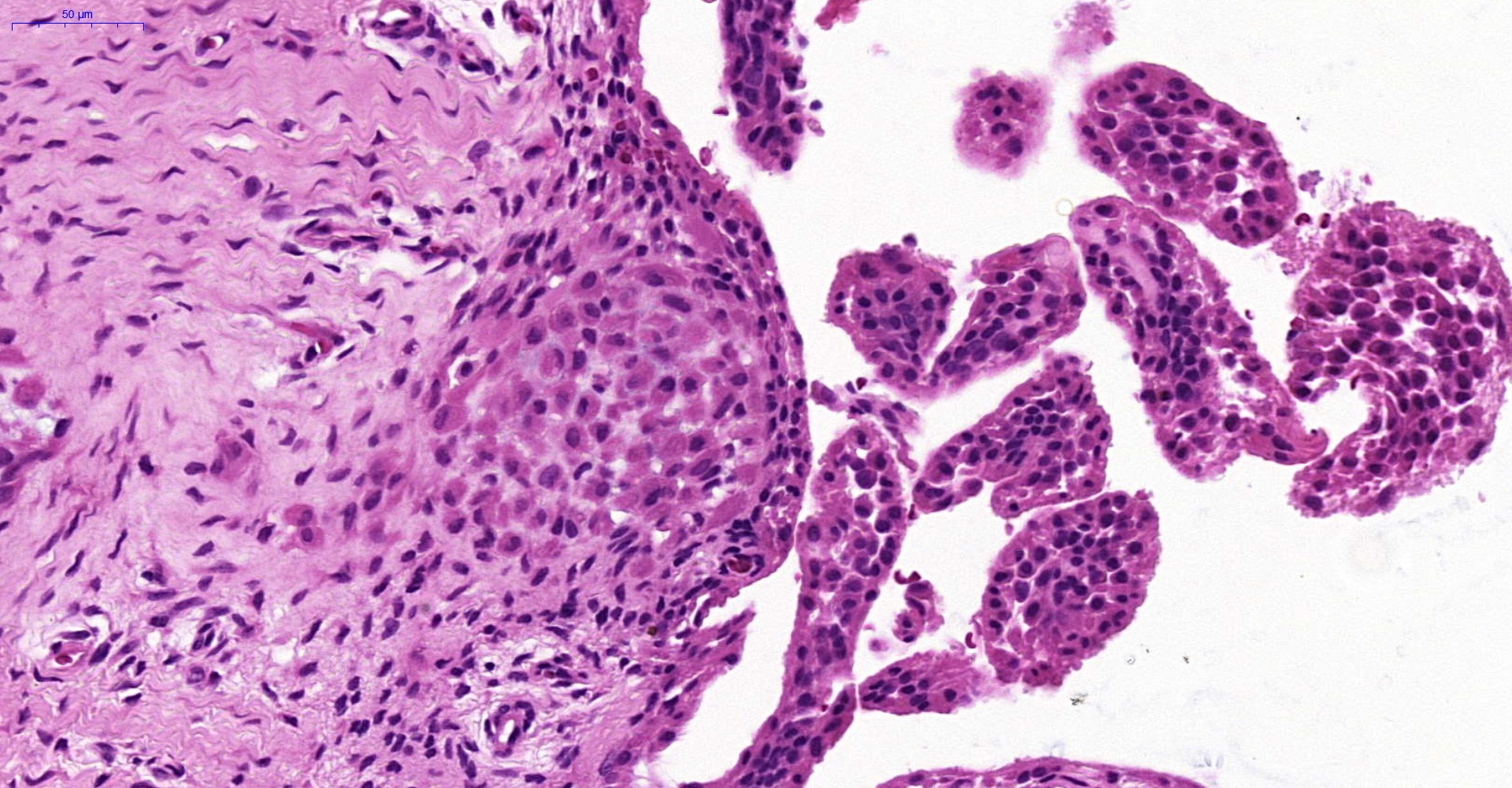
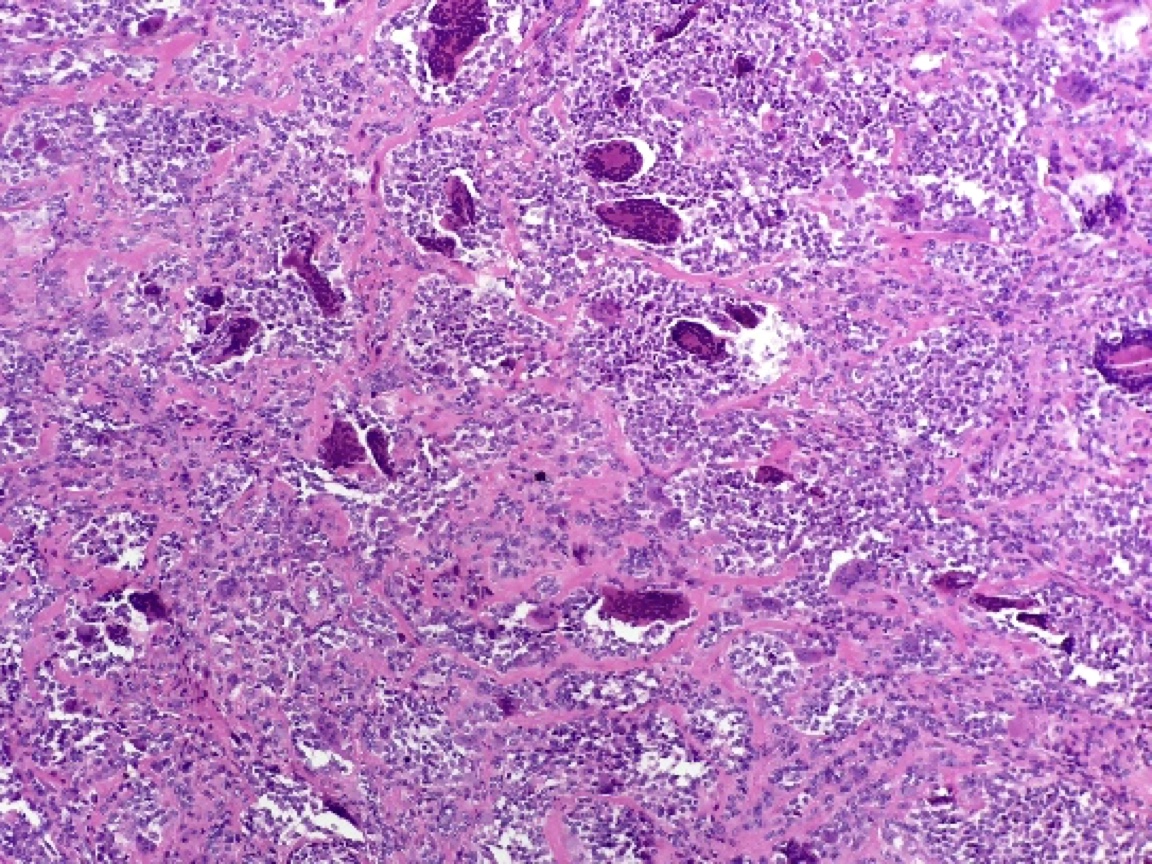
- Diffuse type (J Surg Oncol 1998;68:100, J Oral Maxillofac Surg 2019;77:1022.e1)
- Infiltrative, and grow as diffuse, expansile sheets
- Osteoclast-like giant cells are less common in the diffuse form than the localized form and may be absent or extremely rare in as many as 20% of cases
- Cleft-like spaces are common and appear either as artifactual tears or as synovial lined spaces
- Stromal hyalinization is common and may mimic osteoid
- Blood filled pseudoalveolar spaces are seen in approximately 10% of cases
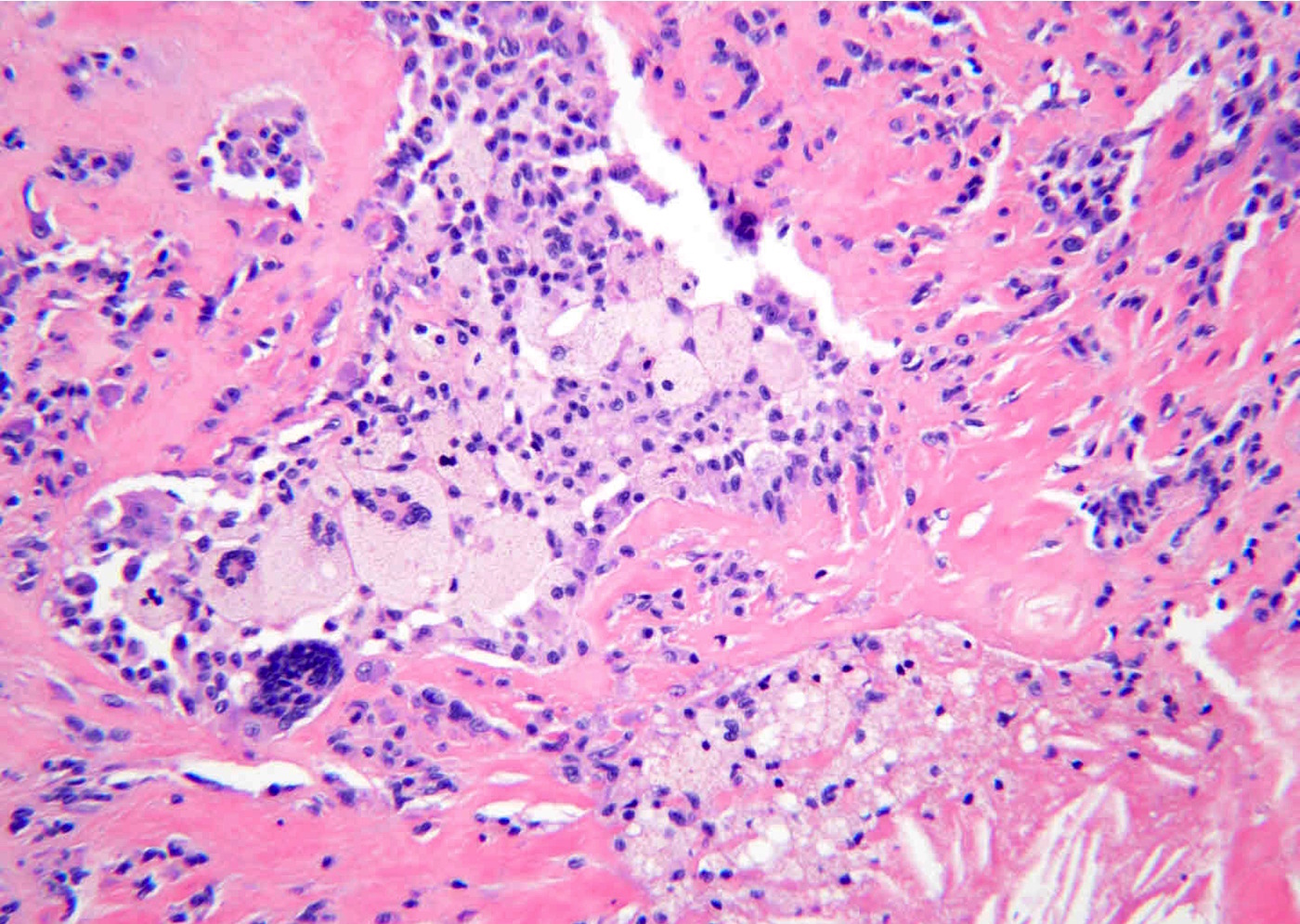
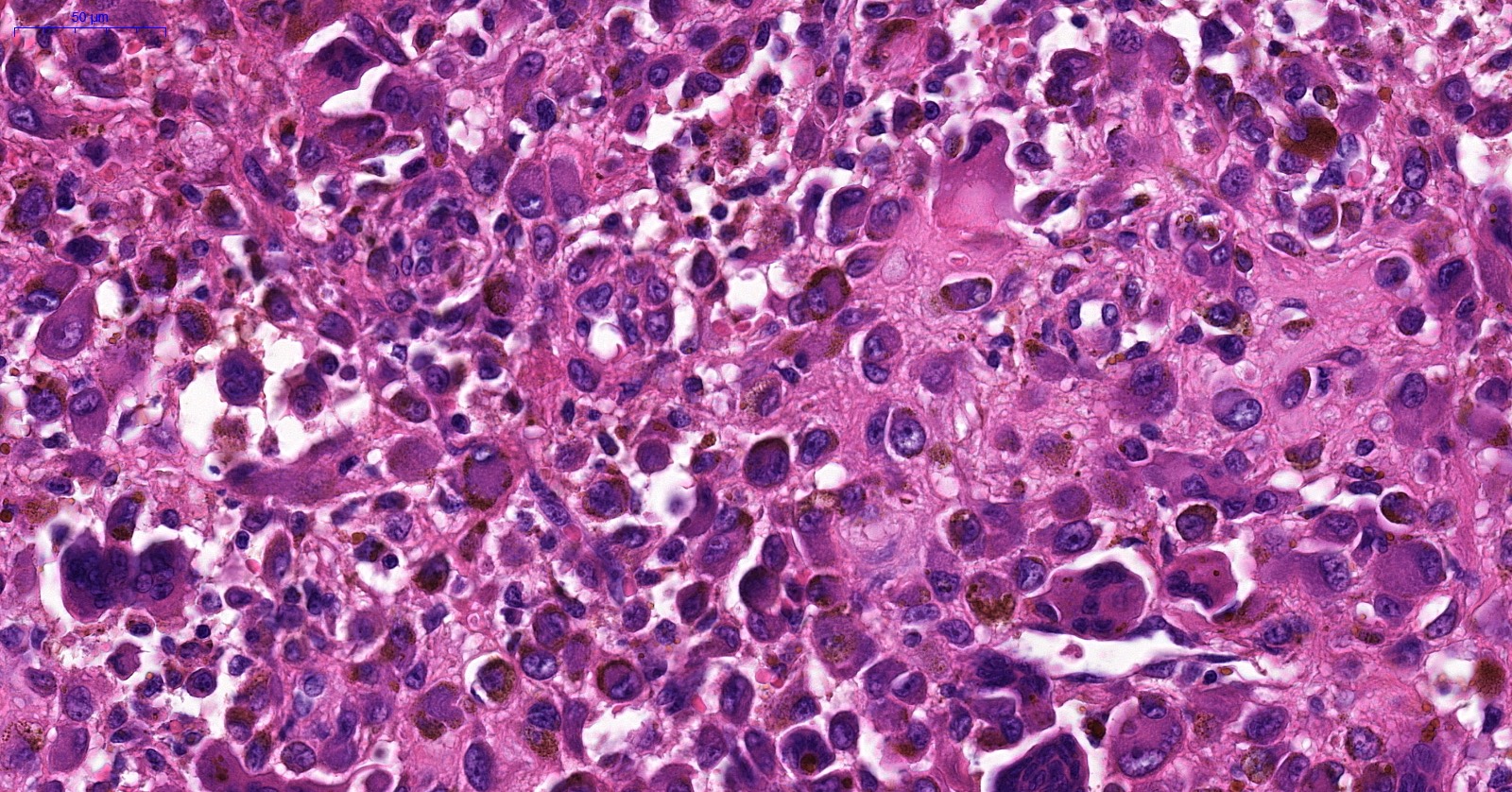
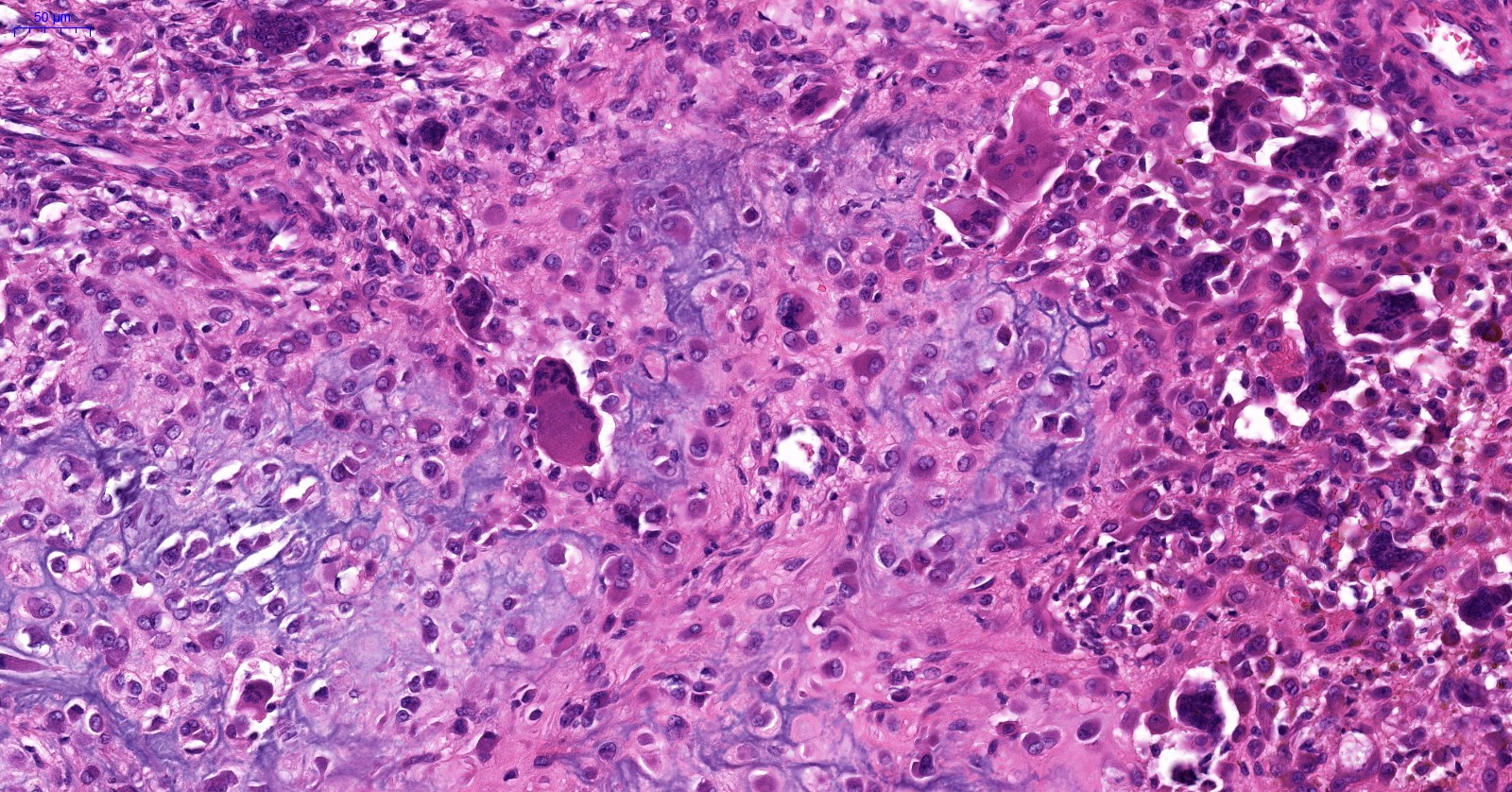
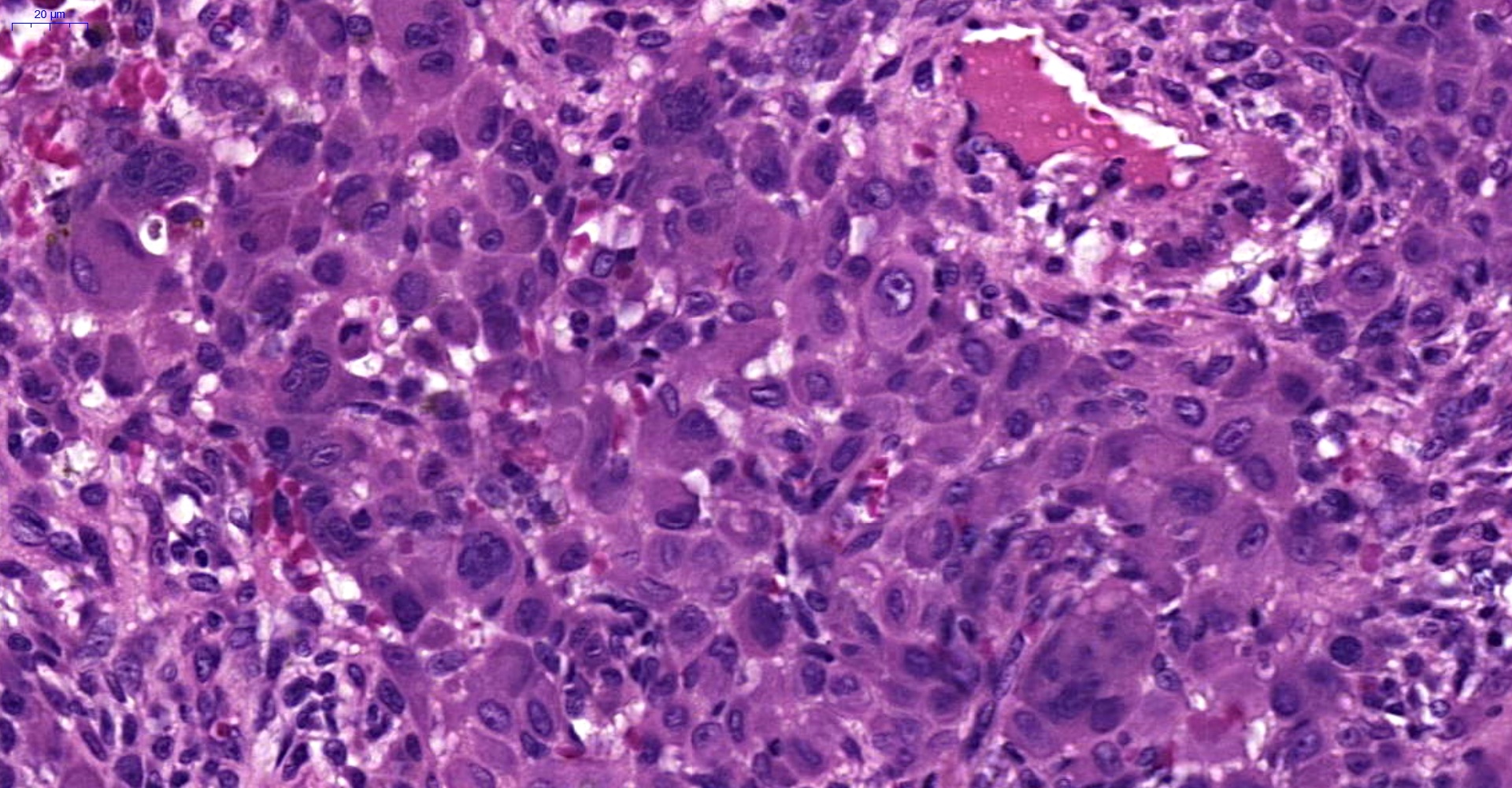
- Malignant (Hum Pathol 2017;63:144, Am J Surg Pathol 1997;21:153)
- Composed of sheets and nodules of enlarged mononuclear cells
- Significantly increased mitotic count, including atypical mitoses, necrosis, enlarged nuclei with nucleoli, spindling of mononucleated cells and myxoid changes
- May contain areas that resemble undifferentiated pleomorphic sarcoma or myxofibrosarcoma
Microscopic (histologic) images
Contributed by Jigang Wang, M.D., Ph.D., Jiufa Cui, M.D., Ph.D. and Michella Whisman, M.D.
Localized type
Diffuse type
Cytology description
- Localized type (Rare Tumors 2015;7:5814)
- Moderately cellular smears with a variable admixture of cell populations:
- Polygonal to spindled mononuclear cells in loose clusters or individually dispersed with moderate cytoplasm and round to oval nuclei
- Scattered osteoclast-like multinucleated giant cells
- Foamy histiocytes
- Hemosiderin laden histiocytes
- Relatively scant background inflammation in most cases
- Moderately cellular smears with a variable admixture of cell populations:
- Diffuse type (Acta Cytol 2017;61:160)
- Heterogeneous cell populations:
- Large epithelioid mononuclear cells
- Abundant eosinophilic cytoplasm, usually containing ring-like hemosiderin pigment
- Vesicular, round to oval, eccentric nuclei with prominent nucleoli
- Macrophages with smaller, oval or reniform nuclei
- Osteoclast-like giant cells
- Large epithelioid mononuclear cells
- Frequent mitotic figures
- Chondroid metaplasia is common in the temporomandibular joint
- Heterogeneous cell populations:
- Malignant (J Cytol 2017;34:174)
Cytology images
Immunofluorescence description
- Unknown at this time
Positive stains
Negative stains
Electron microscopy description
- Localized and diffuse types
- Features of histiocytes and fibroblasts (Ultrastruct Pathol 2002;26:15)
- Malignant
- Unknown at this time
Molecular / cytogenetics description
- Localized type
- Translocations involving CSF1 gene at 1p13 are most common
- Multiple partners have been described
- Diffuse type
- Clonal with neoplastic and reactive features
- Neoplastic due to CSF1 overexpression or 1p13 (CSF1) rearrangements, often with COL6A3 at 2q35 (Am J Surg Pathol 2007;31:970, Proc Natl Acad Sci U S A 2006;103:690)
- Also with reactive features (Hum Pathol 2003;34:65)
- Translocations, t(2;3) and der(8) t(8;12) (Ultrastruct Pathol 2002;26:15)
- Some show trisomy of chromosome 5 and 7
- Malignant
- Loss of the CDKN2A/B gene (Hum Pathol 2017;63:144)
Molecular / cytogenetics images
Sample pathology report
- Right finger, index, excision:
- Tenosynovial giant cell tumor, localized type (giant cell tumor of tendon sheath), 1.6 cm (see comment)
- Comment: Surgery is the main treatment. Localized type rarely recurs after complete removal while diffuse type often recurs.
- Right hip, index, excision:
- Tenosynovial giant cell tumor, diffuse type (pigmented villonodular synovitis)
- Right hip, excision:
- Malignant diffuse tenosynovial giant cell tumor
Differential diagnosis
- Localized type
- Diffuse type tenosynovial giant cell tumor:
- Essentially identical appearance to localized form at high magnification
- Distinguished from localized form by large size, infiltrative growth or anatomic site (often intra-articular and in larger joints)
- Villonodular architecture when intra-articular
- Giant cell tumor of soft tissue:
- More uniform background of mononuclear cells
- Typically have sheets of osteoclastic giant cells similar to giant cell tumor of bone
- Less association with a tendon
- Fibroma of tendon sheath:
- Slit-like vascular spaces at the periphery
- Cracking artifact in collagenous background
- Spindled to stellate fibroblasts / myofibroblasts
- Lacks giant cells, large histiocytoid cells with eccentric nucleus, hemosiderin laden histiocytes and foamy histiocytes
- Diffuse type tenosynovial giant cell tumor:
- Diffuse type
- Localized type tenosynovial giant cell tumor:
- Well circumscribed and encapsulated
- Lacks villi
- Localized to digits, uncommon in large joint
- Hemarthrosis:
- Villiform synovial hyperplasia with hemosiderosis
- Solid cellular areas are rare
- History is important: repetitive hemarthrosis (e.g., trauma or hemophilia)
- Malignant tenosynovial giant cell tumor:
- Often with past history of radiation therapy
- Pleomorphic spindle cells and high mitotic rate and necrosis
- Epithelioid cells with prominent nucleoli
- Localized type tenosynovial giant cell tumor:
- Malignant
- Benign diffuse tenosynovial giant cell tumor:
- Lacks sarcomatous area
- Other soft tissue sarcoma:
- Lacks typical area of diffuse tenosynovial giant cell tumor
- Lacks medical history of diffuse tenosynovial giant cell tumor
- Benign diffuse tenosynovial giant cell tumor:
- Dermatofibroma:
- Dermal lesions
- Rare in digits
- Lacks large epithelioid cells and osteoclast-like giant cells
- Lacks CSF1 rearrangement
- Plexiform fibrohistiocytic tumor:
- Usually involves dermis and subcutis
- Nodules or clusters are interconnected in characteristic plexiform arrangement
- Plump fibroblastic cells and histiocyte-like cells within a finely granular myxoid background
- Large epithelioid mononulear cells are absent
Additional references
Board review style question #1
Which of the following features must be identified to the make the diagnosis of tenosynovial giant cell tumor?
- Epithelioid mononuclear cells
- Foamy macrophages
- Hemosiderin laden macrophages
- Inflammatory cells
- Multinucleated giant cells
Board review style answer #1
A. Epithelioid mononuclear cells. The lesion is a tenosynovial giant cell tumor, localized type (also called giant cell tumor of tendon sheath). Although all the listed cell types can be seen in varying proportions within the tumor, the histiocytoid mononuclear cells are the neoplastic component and should always be present.
Comment Here
Reference: Tenosynovial giant cell tumor
Comment Here
Reference: Tenosynovial giant cell tumor
Board review style question #2
Which of the following is true regarding tenosynovial giant cell tumor, localized type?
- Both genders are affected equally
- Diagnosis can be made even in the absence of osteoclast-like giant cells
- Highly infiltrative lesion, which leads to recurrence in the majority of cases
- It is the most common tumor of the hand
- The patient always reports a history of trauma
Board review style answer #2
B. The diagnosis can be made even in the absence of osteoclast-like giant cells. Some cases show a paucity of giant cells, which is why it is best to know the constellation of histologic features aside from the presence of giant cells in order to make the diagnosis in giant cell poor cases. Tenosynovial giant cell tumor, localized type, is the second most common tumor of the hand (ganglion cyst is most common). It shows a predilection for females (F:M = 2:1). The tumors are usually well circumscribed. They may recur but simple excision is curative most of the time. Some patients report a history of trauma but not all.
Comment Here
Reference: Tenosynovial giant cell tumor
Comment Here
Reference: Tenosynovial giant cell tumor
Board review style question #3
Which of the following is true regarding the location of diffuse tenosynovial giant cell tumor?
- Knee is the most frequent, followed by hip and ankle
- Often in foot and hand
- Often occurs in small joint
- Only intra-articular
Board review style answer #3
A. Knee is the most frequent, followed by hip and ankle. Diffuse tenosynovial giant cell tumor often involves large joint and can be extra-articular. Localized tenosynovial giant cell tumor often occurs in small joint, such as foot and hand.
Comment Here
Reference: Tenosynovial giant cell tumor
Comment Here
Reference: Tenosynovial giant cell tumor
Board review style question #4
Board review style answer #4
E. Tenosynovial giant cell tumor. The pictured lesion is a tenosynovial giant cell tumor, localized type (also called giant cell tumor of tendon sheath). The tumor usually occurs in small joint and is attached to tendon sheath. Microscopically, the tumor was a giant cell rich tumor with prominent epithelioid mononuclear cells that can be observed.
Comment Here
Reference: Tenosynovial giant cell tumor
Comment Here
Reference: Tenosynovial giant cell tumor
Board review style question #5
Which of the following is true regarding malignant tenosynovial giant cell tumor?
- Malignant tumor from the location around large joint
- May have a previous history or typical morphological area of tenosynovial giant cell tumor
- Often occurs in upper extremities
- Usually affects young people
Board review style answer #5
B. May have a previous history or typical morphological area of tenosynovial giant cell tumor
Comment Here
Reference: Tenosynovial giant cell tumor
Comment Here
Reference: Tenosynovial giant cell tumor