Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Potterveld S, Clay MR. Dedifferentiated liposarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuededifflipo.html. Accessed December 18th, 2024.
Definition / general
- Well differentiated liposarcoma (WDL) with transition, either in the primary tumor or as a recurrence to a sarcoma that is typically nonlipogenic
- Most cases are intermediate to high grade; the existence of low grade dedifferentiated liposarcoma, although now officially recognized, has been controversial
Essential features
- Nonlipogenic sarcoma (typically) that arises from well differentiated liposarcoma
- Precursor well differentiated liposarcoma may or may not be identifiable in the background
- Both low and high grade classifications are now recognized (see Terminology)
- Molecularly characterized by ring or giant marker / rod chromosomes composed of material from 12q13-15
- Results in localized amplification of several neighboring genes, including MDM2
- Rarely, the high grade component can be lipogenic and resemble pleomorphic liposarcoma (homologous lipoblastic differentiation) (Am J Surg Pathol 2010;34:1122)
- First tumor type to consider in cases of high grade sarcoma of the retroperitoneum in an adult
- Retroperitoneal tumors historically regarded as inflammatory subtype of malignant fibrous histiocytoma (MFH) are now considered to represent a common morphologic pattern of dedifferentiation in dedifferentiated liposarcoma
Terminology
- Although originally these tumors were all considered high grade, low grade dedifferentiation is now a recognized phenomenon
- Low grade dedifferentiation can be histologically indistinguishable from cellular well differentiated liposarcoma; the terminology that is used varies among practicing pathologists
- Although some report a comparable prognosis for well differentiated and low grade dedifferentiated cases, others report an unfavorable outcome with any percentage or degree of dedifferentiation (Am J Surg Pathol 2007;31:1, Am J Surg Pathol 1997;21:271)
- Minimal dedifferentiation
- Although controversial, some require macroscopic evidence of dedifferentiation (> 1.0 cm) to label a tumor as truly dedifferentiated
- Even cases with so called minimal dedifferentiation (< 1.0 cm) can still carry an inferior prognosis when compared with well differentiated liposarcoma; prolonged clinical follow up is recommended regardless of size
ICD coding
- ICD-O: 8858/3 - dedifferentiated liposarcoma
- ICD-11: 2B59 & XH1C03 - liposarcoma, primary site & dedifferentiated liposarcoma
Epidemiology
- Typically occurs in older adults, with a slight predilection for men
- Occurs in up to 10% of well differentiated liposarcomas, with more frequent dedifferentiation noted in retroperitoneal primaries
Sites
- Most common site is the retroperitoneum, followed by the extremities
- Other frequent sites include the spermatic cord
- Rare in the head and neck
- Extremely rare in the subcutis; as a general rule, subcutaneous atypical lipomatous tumors do not dedifferentiate
Diagnosis
- Imaging studies are recommended for initial diagnostic workup and may show both fatty and nonfatty components
- Percutaneous biopsy has low sensitivity for detecting dedifferentiated liposarcoma (Ann Surg Oncol 2015;22:1068)
- Surgical resection is recommended for accurate tumor classification
Radiology description
- Characterized by a nonlipomatous mass contiguous with a well demarcated fatty component
- On MRI, nonfatty regions typically show low signal intensity on T1 weighted images, high signal intensity on T2 weighted images and marked enhancement after IV gadolinium (Eur J Radiol 2004;50:257)
- Other imaging features suggestive of dedifferentiation include central necrosis, contrast enhancement and increased FDG uptake on PET / CT (J Comput Assist Tomogr 2016;40:872, Sarcoma 2020;2020:8363986)
- Calcification on imaging may suggest heterologous osteosarcomatous dedifferentiation (AJR Am J Roentgenol 2011;197:W37)
Radiology images
Prognostic factors
- Better prognosis than other high grade pleomorphic sarcomas but still recurs in 40 - 75% of cases, metastasizes in 10 - 15% of cases and is associated with a 28% mortality rate (Am J Surg Pathol 1994;18:1213, Am J Surg Pathol 1997;21:271)
- Higher Fédération Nationale des Centres de Lutte Contre le Cancer (FNCLCC) grade and myogenic differentiation are associated with a worse clinical outcome (Am J Surg Pathol 2015;39:383)
- A modified FNCLCC grade, which assigns a tumor differentiation score (1 - 3) according to the dedifferentiated component of the tumor (in contrast to the standard FNCLCC grading system, which assigns a tumor differentiation score of 3 to all dedifferentiated liposarcomas) has been shown to predict local recurrence, supporting the hypothesis that tumor behavior is influenced by the degree of differentiation within the dedifferentiated component (Mod Pathol 2015;28:37)
- Metastasis can occur in cases with low and high grade dedifferentiation and there is no minimal amount of dedifferentiation that mitigates this risk (Am J Surg Pathol 1997;21:271)
- Cases with myxofibrosarcoma-like features are particularly aggressive (Mod Pathol 2005;18:976)
- Retroperitoneal dedifferentiated liposarcoma has higher rates of local recurrence and disease specific death (Curr Opin Oncol 2011;23:373)
- If followed long enough, nearly all retroperitoneal tumors will recur
- Must rule out dedifferentiated liposarcoma in any retroperitoneal sarcoma; this can be aided by
- Adequate sampling, particularly of peripheral areas
- Cytogenetics
- Immunostaining for MDM2 and CDK4 or molecular testing for 12q13-15 amplification
Case reports
- 23 year old woman with an orbital tumor (Int J Ophthalmol 2011;4:452)
- 53, 57 and 69 year old men with rhabdomyoblastic dedifferentiation (Virchows Arch 2005;447:835)
- 53 year old man with a retroperitoneal tumor exhibiting a paraganglioma-like histologic pattern (Arch Pathol Lab Med 2004;128:788)
- 66 and 84 year old men with challenging cases of dedifferentiated liposarcoma resolved with molecular testing (BMC Clin Pathol 2014;14:36)
- 67 year old woman with a retroperitoneal tumor with leiomyosarcomatous differentiation and human chorionic gonadotropin (hCG) production (Sarcoma 2008;2008:658090)
- 71 year old man whose relapse had an extensive lymphoid component (Pathol Res Pract 2005;201:347)
- 71 year old woman with a thigh mass exhibiting osteosarcomatous dedifferentiation (Radiographics 2005;25:1082)
- 72 year old man with an arm tumor, elevated serum granulocyte colony stimulating factor (GCSF) and leukocytosis (World J Surg Oncol 2007;5:131)
- 72 year old man with a retroperitoneal tumor producing alpha fetoprotein (Virchows Arch 2006;448:517)
- 76 year old woman with an abdominal mass (World J Gastrointest Oncol 2011;3:116)
- 85 year old woman with a soft tissue mass of buttock; dedifferentiated liposarcoma diagnosed by fine needle aspiration (Cytojournal 2010;7:5)
Treatment
- Resectable disease is treated with surgery to obtain negative margins (NCCN Guidelines: Neuroendocrine and Adrenal Tumors [Accessed 28 March 2023])
- Neoadjuvant radiation therapy can be considered in selected patients at high risk for local recurrence but adjuvant radiation therapy is discouraged for retroperitoneal / intra-abdominal sarcoma
- Palbociclib (CDK4 inhibitor) may be useful as single agent therapy for the treatment of unresectable tumors
Gross description
- Large firm mass (may resemble fish flesh) with coarse lobulation that can be surrounded by the more grossly fatty appearing well differentiated component
- Dedifferentiation can be discrete and nodular or more gradual (Semin Diagn Pathol 2019;36:112)
- Look for foci of necrosis in the high grade component
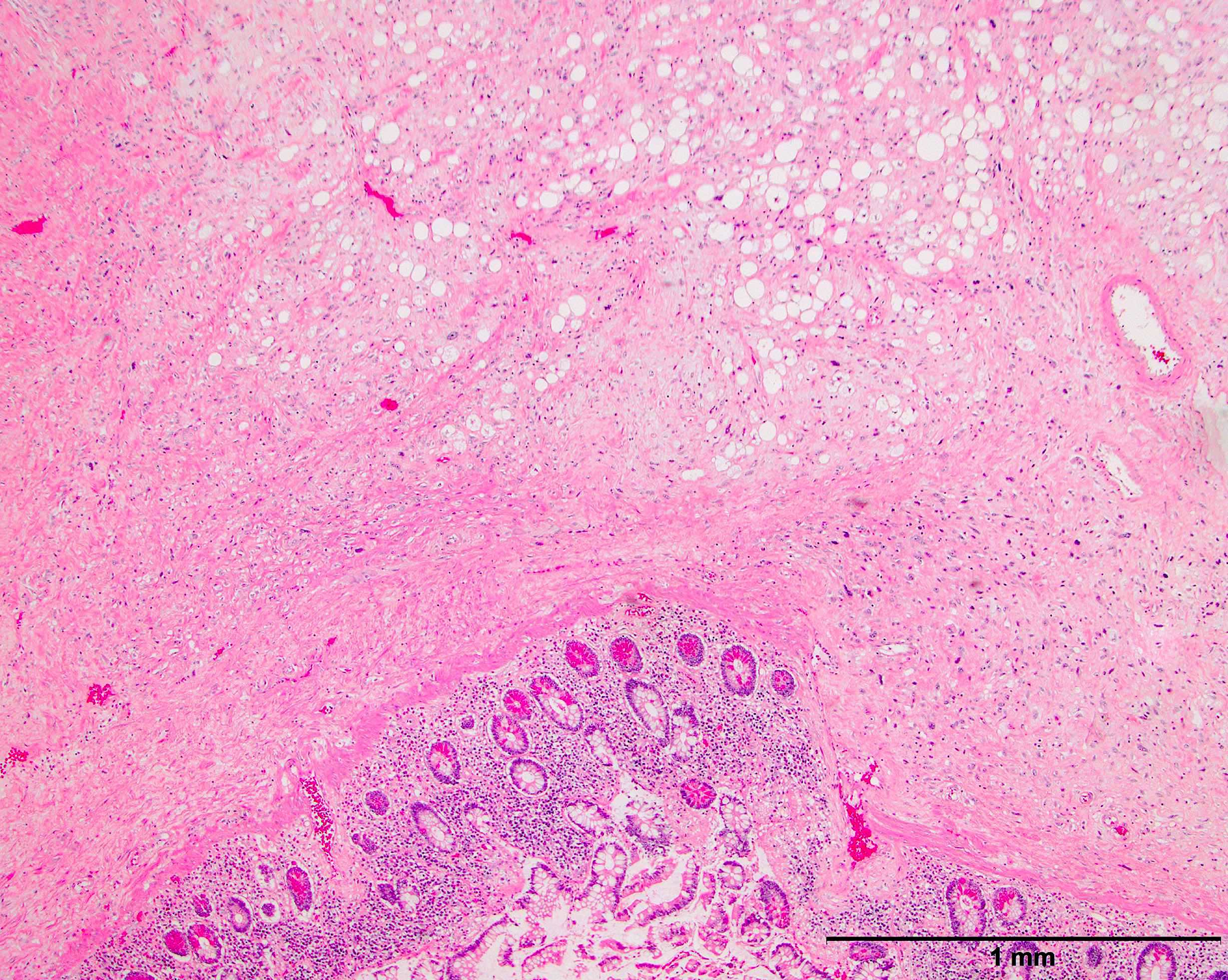
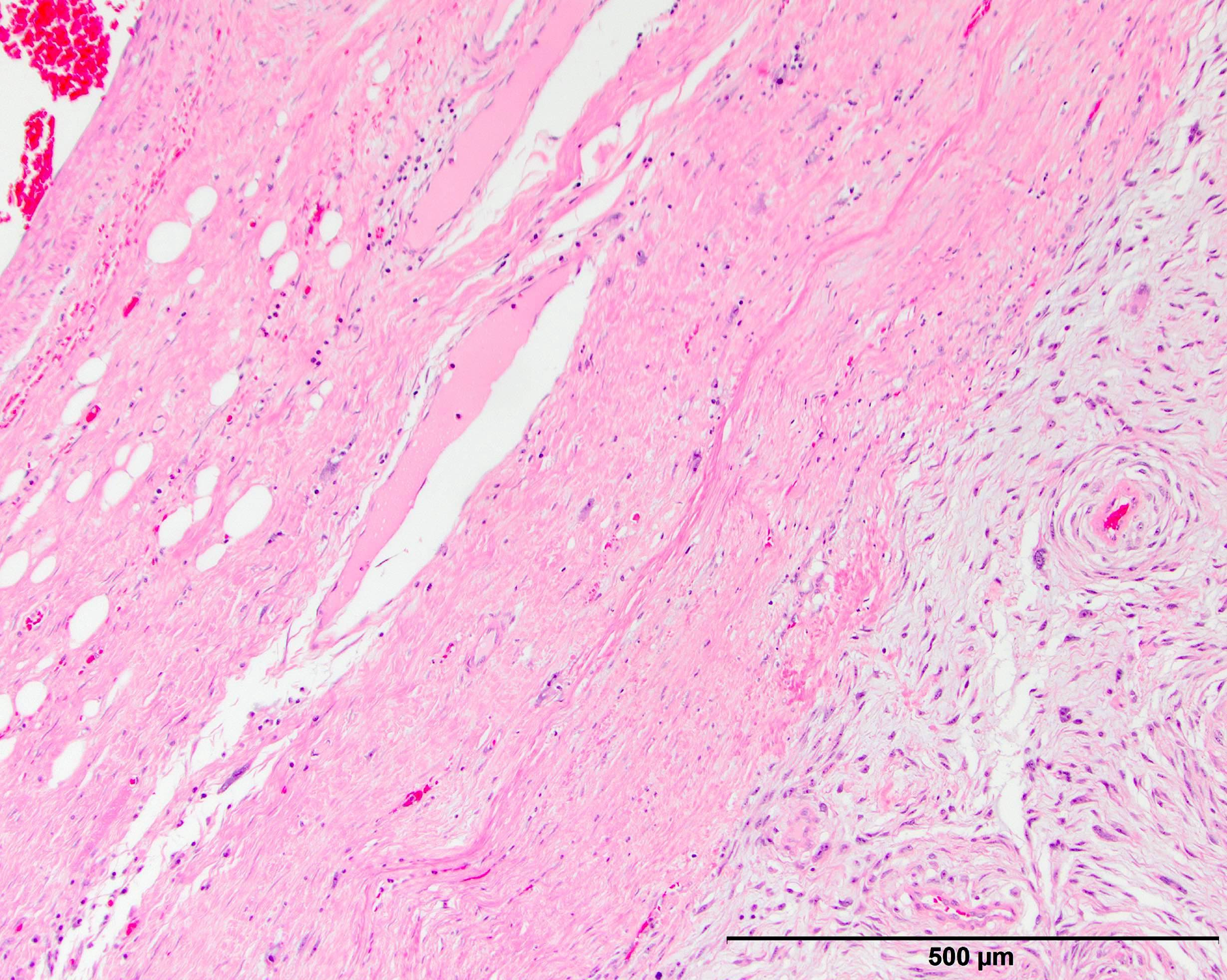
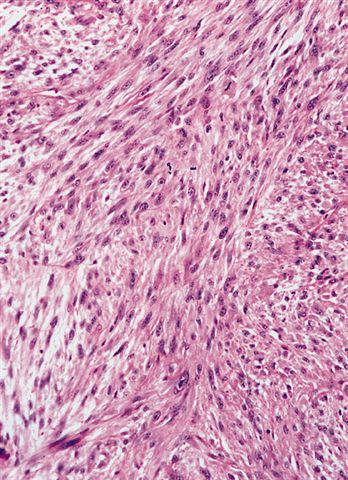
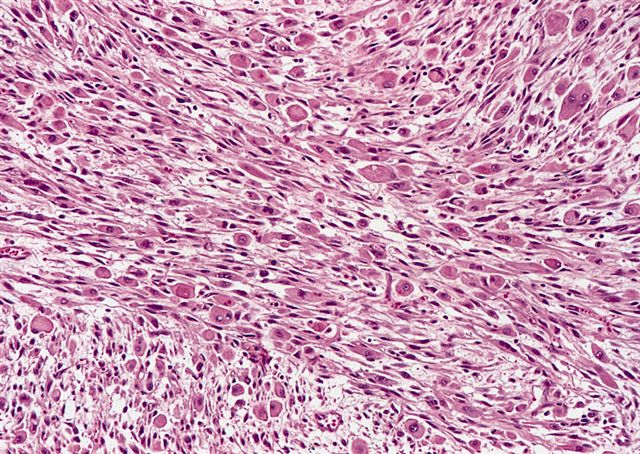
Microscopic (histologic) description
- High grade dedifferentiated liposarcoma
- Well differentiated and dedifferentiated components are often both present and can have abrupt or gradual transitions
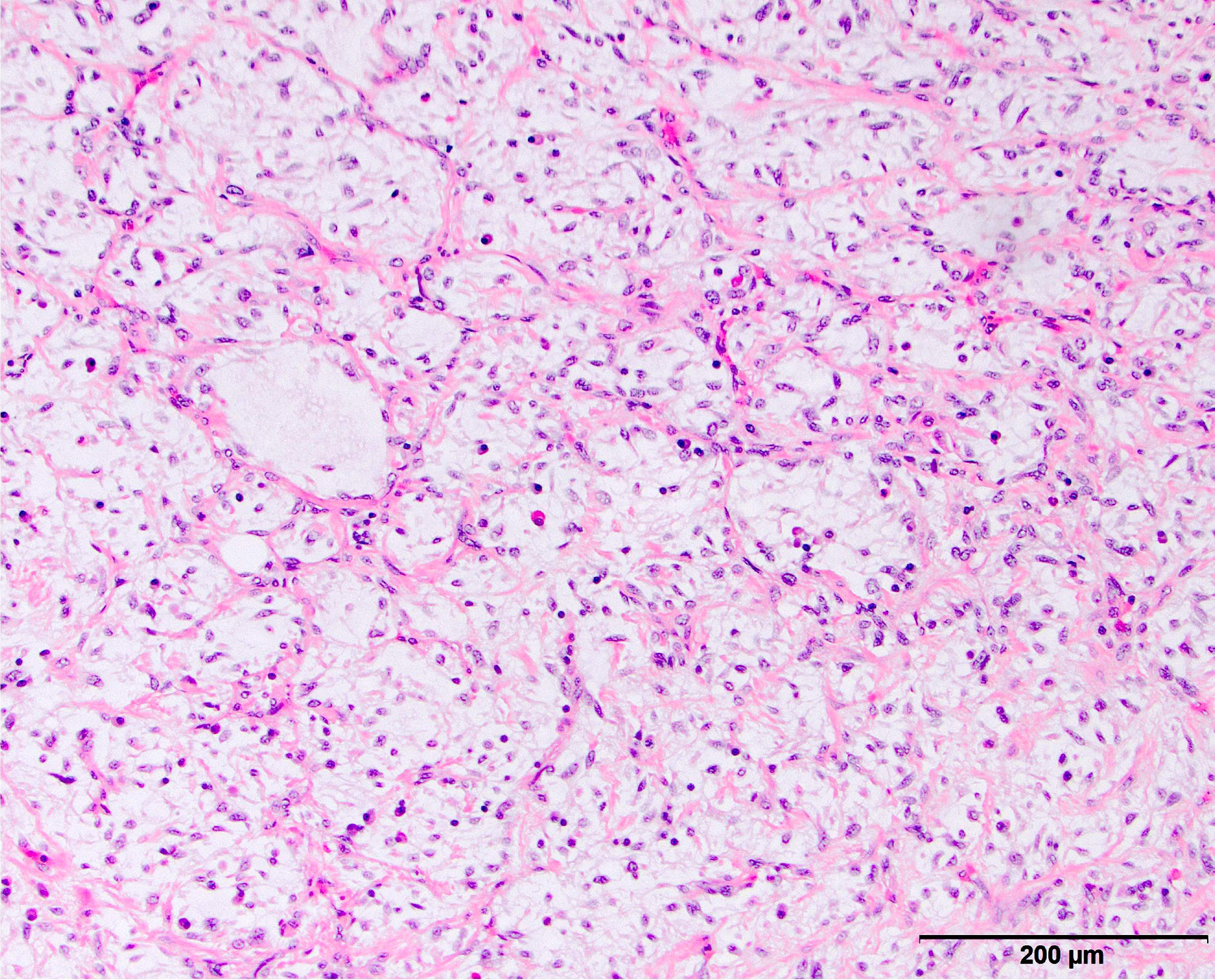
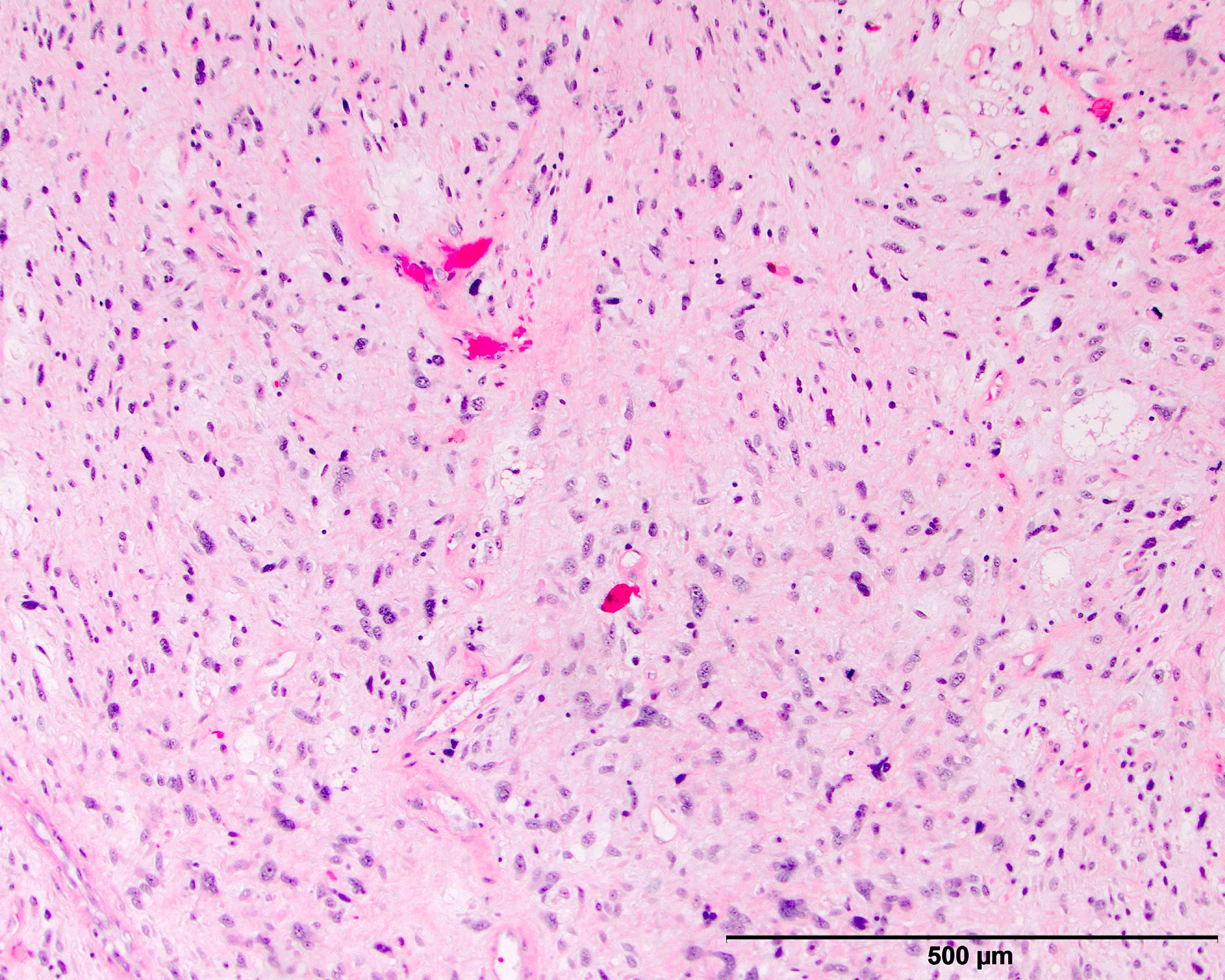
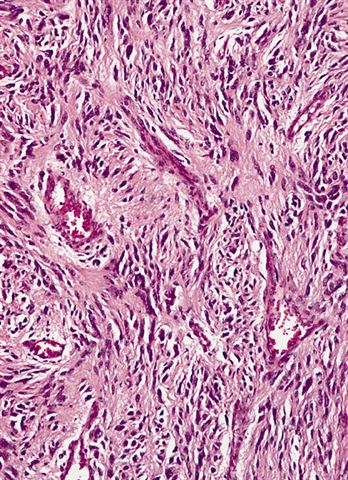
- Dedifferentiated component is a cellular and typically a nonlipogenic sarcoma with significant pleomorphism
- Although some propose a mitotic rate of > 5 mitoses/10 high power fields, this is not uniformly adopted (Am J Surg Pathol 2023;47:649)
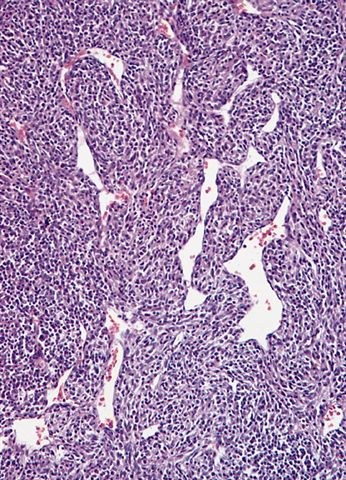
- Often resembles malignant fibrous histiocytoma (MFH), now referred to as undifferentiated pleomorphic sarcoma (UPS), with short fascicles of pleomorphic spindle cells associated with mixed inflammatory infiltrate
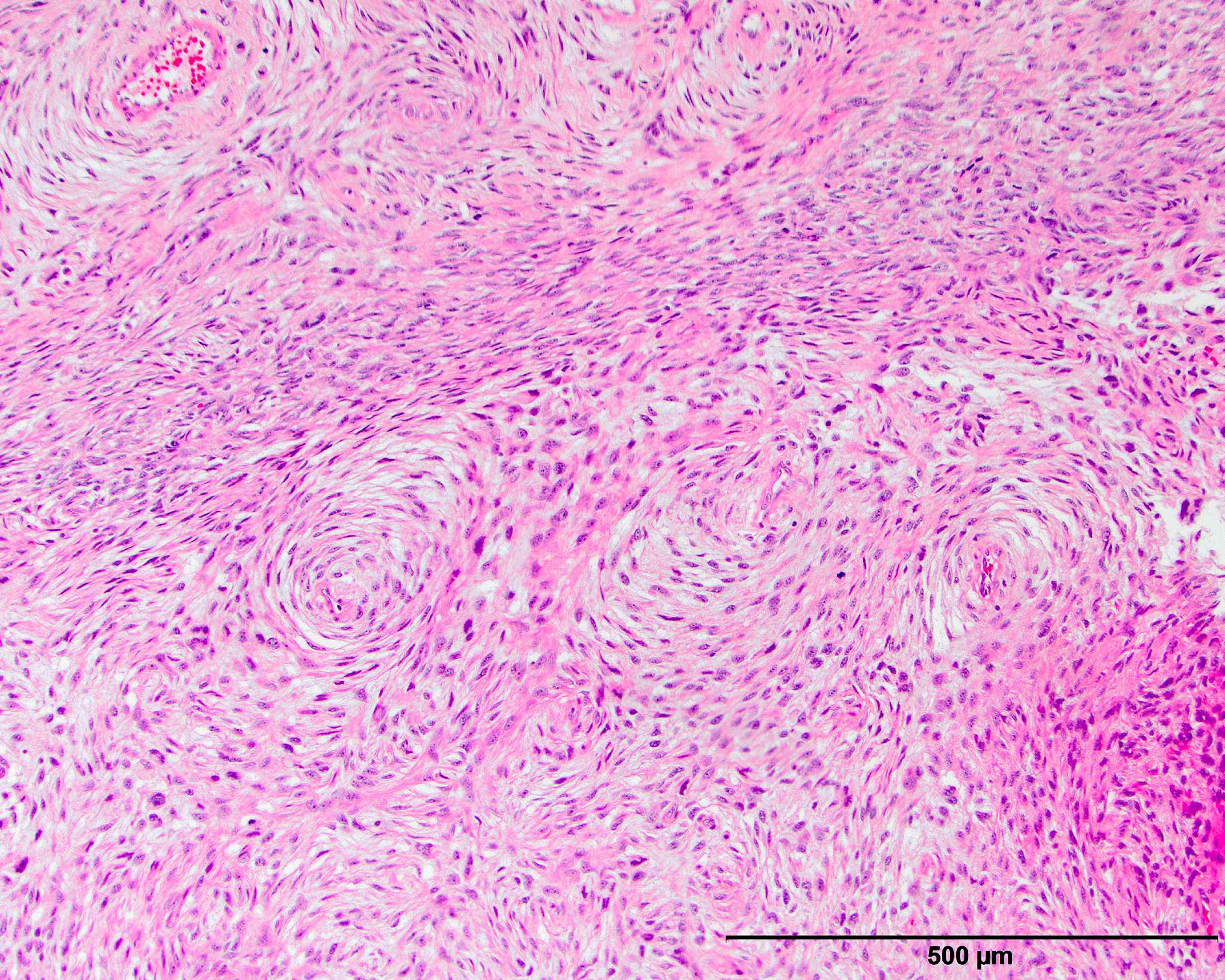
- Can show a peculiar whirling pattern reminiscent of meningothelial structures (Histopathology 1998;33:414, Am J Surg Pathol 1998;22:945)
- Heterologous elements in 5 - 10% of cases
- Heterologous elements can easily mislead pathologists in poorly sampled cases, especially in metastatic sites
- Can manifest as neural differentiation, leiomyosarcoma, osteosarcoma / chondrosarcoma, rhabdomyosarcoma or pleomorphic liposarcoma (homologous lipoblastic dedifferentiation)
- Rhabdomyoblastic differentiation has been associated with worse outcomes
- Angiosarcomatous differentiation has been reported (Virchows Arch 2005;446:456)
- Myxoid liposarcoma-like morphologic features may exist in a subset of cases (often with coexisting amplification of DDIT3) and are important to recognize as a unique histologic pattern of dedifferentiated liposarcoma to avoid misclassification as myxoid liposarcoma (Mod Pathol 2019;32:585)
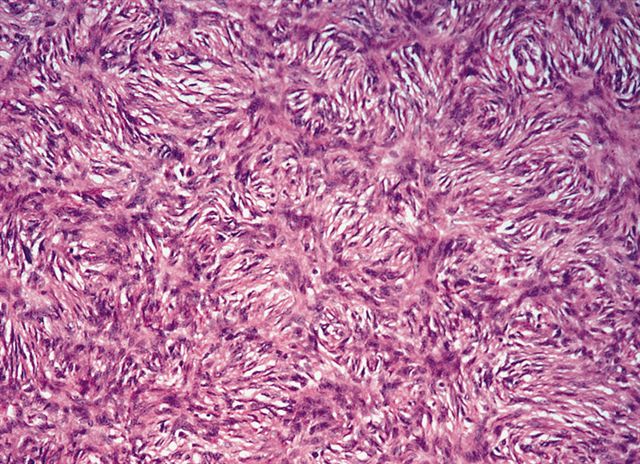
- Low grade dedifferentiated liposarcoma
- Less common low grade tumor resembling fibromatosis or well differentiated fibrosarcoma
- Nonlipogenic (in contrast to well differentiated spindle cell liposarcoma, which contains atypical fat / lipoblasts)
- Considered by some to be the same as cellular atypical lipomatous tumor, although there is evidence that even low grade dedifferentiation is associated with a poorer prognosis when compared with conventional atypical lipomatous tumor
- Now a recognized WHO classification
- Pitfalls and tips
- Look at the edges of dedifferentiated liposarcoma to identify a rim of background well differentiated liposarcoma that may mimic compressed background fat with reactive change
- Dedifferentiated liposarcoma often shows a significant amount of heterogeneity (multiple patterns of differentiation and growth) and the confusing nature of the tumor can be a clue to the correct diagnosis
- Imaging may show both a fatty and solid nonfatty component
- Metastases often contain only the dedifferentiated component
- When in doubt use ancillary testing to confirm either protein overexpression or gene amplification
Microscopic (histologic) images
Contributed by Michael R. Clay, M.D. and AFIP
Cytology description
- Hypercellular with multinucleated, pleomorphic giant cells with abundant cytoplasm, small clusters of cells with high N:C ratio, spindled cells with elongated nuclei (Acta Cytol 2001;45:641)
- Occasional osteoclast type giant cells (Cytojournal 2010;7:5)
- Most samples are suitable for molecular confirmation
Positive stains
- MDM2 and CDK4 are more sensitive in dedifferentiated liposarcoma than in well differentiated tumors given how cellular they are (Am J Surg Pathol 2005;29:1340)
- These stains are most useful in ruling out differential diagnoses that should be negative
- Addition of p16 to the stains above may increase sensitivity and specificity (Am J Surg Pathol 2012;36:462)
- Also vimentin, p53, Rb (66%), PPAR gamma (Mod Pathol 2008;21:517)
- Focal positivity for smooth muscle actin
- Subset positivity for most antibodies is not too shocking given the nature of this entity
Molecular / cytogenetics description
- 12q14 amplification, often due to supernumerary ring or giant chromosome derived from 12q13-15 region
- Degree of copy number change has been correlated with progression to higher grade tumors (Am J Clin Pathol 2014;141:334)
- Pitfalls
- Beware of other tumors that have MDM2 gene amplification, including
- Intimal sarcoma (majority) (Cancer Genet Cytogenet 2007;179:146)
- Parosteal osteosarcoma, low grade central osteosarcoma (Arch Pathol Lab Med 2014;138:694)
- Malignant peripheral nerve sheath tumor (MPNST) (20%) (Arch Pathol Lab Med 2012;136:95)
- Endometrial stromal sarcoma (5%) (Int J Gynecol Pathol 2015;34:576)
- Sclerosing rhabdomyosarcoma (Sarcoma 2013;2013:520858)
- Beware of other tumors that have MDM2 gene amplification, including
Molecular / cytogenetics images
Videos
Dedifferentiated liposarcoma with heterologous osteosarcoma component
Dedifferentiated liposarcoma
Sample pathology report
- Retroperitoneal mass, resection:
- Dedifferentiated liposarcoma (10.0 cm) (see comment)
- Resection margins are negative for tumor
- Comment: Histologic sections of this retroperitoneal mass show a malignant spindle cell lesion with prominent scattered pleomorphic cells and well differentiated adipose tissue at the periphery. The malignant cells show strong nuclear expression of MDM2 by immunohistochemistry, supporting the diagnosis.
Differential diagnosis
- Leiomyosarcoma:
- Even in pleomorphic cases there are usually areas with morphology distinctive of well differentiated leiomyosarcoma
- There is no background well differentiated liposarcomatous component and no 12q13-15 amplification
- Immunostaining can be supportive but beware of desmin / actin expression in dedifferentiated liposarcoma
- Malignant peripheral nerve sheath tumor (MPNST):
- No well differentiated liposarcomatous component
- History of neurofibromatosis can be helpful
- Be wary of molecular / immunohistochemical testing as 20% of MPNST can have MDM2 gene amplification and protein overexpression
- More commonly located in the deep soft tissues of the extremities than in the retroperitoneum
- Typically more uniform in growth pattern than dedifferentiated liposarcoma, although the distinction may be very difficult
- Melanoma:
- Pleomorphic liposarcoma (PLS):
- Has lipoblasts set in the background of a pleomorphic sarcoma
- Only way to distinguish PLS from dedifferentiated liposarcoma with secondary homologous differentiation is to either identify background well differentiated liposarcoma or verify MDM2 overexpression or amplification by ancillary studies (Cancer Cytopathol 2014;122:128)
- This is an important distinction as pleomorphic liposarcoma has a significantly worse prognosis
- Rhabdomyosarcoma:
- No well differentiated liposarcomatous component, no 12q13-15 amplification or MDM2 protein overexpression
- Rhabdomyoblastic stains can be unreliable given heterologous differentiation in dedifferentiated liposarcoma
- Other sarcoma subtype infiltrating background adipose tissue:
- Try to look in areas outside of the main tumor bulk to identify a well differentiated liposarcoma component; imaging can be particularly useful in showing a well differentiated fatty component associated with the higher grade sarcoma
- Molecular and immunohistochemical studies are helpful
- This may be particularly necessary when the background entrapped fat takes on a reactive appearance with fat necrosis, as this can closely mimic an underlying well differentiated liposarcoma
- Sarcomatoid carcinoma:
- Look for epithelial markers (EMA / cytokeratin) and clinical history indicative of a primary epithelial malignancy
- No well differentiated liposarcomatous component, no 12q13-15 amplification
- Sarcomatoid mesothelioma:
- Similar age group but often have a clinical history of asbestos exposure, even in peritoneal disease (Am J Surg Pathol 2015;39:1568)
- Variably positive for mesothelial markers (cytokeratin in 93%, calretinin in only 31%) (Mod Pathol 2010;23:470)
- There is no well differentiated liposarcomatous component and no 12q13-15 amplification
- Undifferentiated pleomorphic sarcoma (UPS) / malignant fibrous histiocytoma (MFH):
- Retroperitoneal tumors are dedifferentiated liposarcoma until proven otherwise
- Be very wary of this diagnosis in that location
- Although UPS may have a complex karyotype, MDM2 gene amplification would indicate the diagnosis of dedifferentiated liposarcoma (Mod Pathol 2003;16:256)
- Retroperitoneal tumors are dedifferentiated liposarcoma until proven otherwise
Additional references
Board review style question #1
A 10 cm retroperitoneal mass was surgically resected with the histologic appearance shown in the image above. Which one of the following ancillary tests would best help support the diagnostic impression?
- FISH positive for DDIT3 gene rearrangement
- FISH positive for EWSR1 gene rearrangement
- FISH positive for FOXO1 gene rearrangement
- FISH positive for MDM2 gene amplification
- FISH positive for MDM2 gene rearrangement
Board review style answer #1
D. FISH positive for MDM2 gene amplification. The microscopic image demonstrates a proliferation of variably sized adipocytes admixed with scattered enlarged, hyperchromatic tumor cells that abruptly transitions to a cellular, spindle cell component with significant pleomorphism. These are the key histologic features of dedifferentiated liposarcoma. Detection of MDM2 amplification by FISH is a useful ancillary tool to confirm the diagnosis of both well differentiated and dedifferentiated liposarcoma. It is important to recognize, however, that MDM2 gene amplification is not entirely specific for well differentiated and dedifferentiated liposarcoma as it can also be found in other tumors, including intimal sarcoma, parosteal osteosarcoma, low grade central osteosarcoma, malignant peripheral nerve sheath tumor, endometrial stromal sarcoma and sclerosing rhabdomyosarcoma.
Comment Here
Reference: Dedifferentiated liposarcoma
Comment Here
Reference: Dedifferentiated liposarcoma
Board review style question #2
Which of the following is associated with an adverse prognosis in patients with dedifferentiated liposarcoma?
- Age > 65 years old
- Amount of the dedifferentiated component
- Heterologous differentiation into rhabdomyosarcoma
- Located in the extremity
- Lower FNCLCC grade
Board review style answer #2
C. Heterologous differentiation into rhabdomyosarcoma. Rhabdomyoblastic differentiation and a higher FNCLCC grade have been associated with worse clinical outcomes, whereas the amount and grade of the dedifferentiated component have not. Overall, anatomic location is the most important prognostic factor in dedifferentiated liposarcomas, with retroperitoneal tumors behaving the most aggressively.
Comment Here
Reference: Dedifferentiated liposarcoma
Comment Here
Reference: Dedifferentiated liposarcoma