Table of Contents
Adult type rhabdomyoma | Fetal type rhabdomyoma | Genital type rhabdomyoma | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Youssef R, Dehner C. Rhabdomyoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueadultrhabdomyoma.html. Accessed April 1st, 2025.
Adult type rhabdomyoma
Definition / general
Essential features
ICD coding
Epidemiology
Sites
Clinical features
Diagnosis
Radiology description
Radiology images
Images hosted on other servers:
Prognostic factors
Case reports
Treatment
Clinical images
Images hosted on other servers:
Gross description
Gross images
Contributed by Mark R. Wick, M.D.
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Carina Dehner, M.D., Ph.D.
Cytology description
Cytology images
Images hosted on other servers:
Positive stains
Negative stains
Electron microscopy description
Sample pathology report
Differential diagnosis
- Benign tumor of mature skeletal muscle
- Usually classified into cardiac and extracardiac forms (Am J Dermatopathol 2016;38:154)
- Extracardiac tumors are not associated with tuberous sclerosis
Essential features
- Rare, benign tumor of mature skeletal muscle
- Predominant in men, usually in the head and neck region
- Extracardiac rhabdomyomas are divided into fetal, adult and genital histologic types (50%, 40% and 10% of extracardiac rhabdomyomas, respectively) (Int J Gynecol Pathol 2021;40:97)
ICD coding
- ICD-O: 8900/0 - rhabdomyoma, NOS
- ICD-11
- 2E86.2 & XH8WG9 - rhabdomyoma & rhabdomyoma, NOS
- 2E86.2 & XH4BG5 - rhabdomyoma & adult rhabdomyoma
Epidemiology
- Median age: 60 years (Hum Pathol 1993;24:608)
- M:F = 3:1 (Am J Dermatopathol 2016;38:154)
Sites
- Usually head and neck, particularly the oral cavity, followed by the extremities, esophagus and others (Head Neck Pathol 2021;15:1253)
Clinical features
- Very rare
- Often a solitary mass (70%) but may be multinodular (26%) and rarely multicentric (4%) (Head Neck Pathol 2021;15:1253)
- It has been suggested to have an association with Birt-Hogg-Dubé (BHD) syndrome
- Caused by heterozygous germline mutations in the folliculin gene (FLCN) located on chromosome 17p11.2 (Head Neck Pathol 2019;13:507)
Diagnosis
- Usually requires a surgical specimen
- On biopsy, it is hard to differentiate between rhabdomyoma and well differentiated rhabdomyosarcomas (RMS) that may be extremely well differentiated, hypocellular or have insidiously bland nuclei
Radiology description
- Computed tomography scan (CT): enhancing soft tissue mass with attenuation similar to muscle, with indistinct margins
- Magnetic resonance imaging (MRI): enhancing mass with signal intensity following muscle on T1 and T2 weighted sequences and indistinct margins (Clin Neuroradiol 2022;32:303)
Radiology images
Images hosted on other servers:
Prognostic factors
- Local recurrence may rarely occur
- Malignant transformation to rhabdomyosarcoma has not been reported (Cancer 1980;46:780)
Case reports
- 34 year old man presented with a yellow lesion in the maxillary vestibule (Ear Nose Throat J 2023 May 26 [Epub ahead of print])
- 47 year old man with a diagnosis of adult rhabdomyoma (ARM) in the oral cavity (Head Neck Pathol 2021;15:1253)
- 60 year old man with Birt-Hogg-Dubé syndrome with a diagnosis of adult rhabdomyoma presenting as a thyroid nodule (Diagn Cytopathol 2020;48:576)
- 73 year old man with multifocal adult rhabdomyoma of the head and neck (Int J Oral Maxillofac Surg 2021;50:327)
Treatment
- Excision is curative but may recur if incompletely excised
Clinical images
Images hosted on other servers:
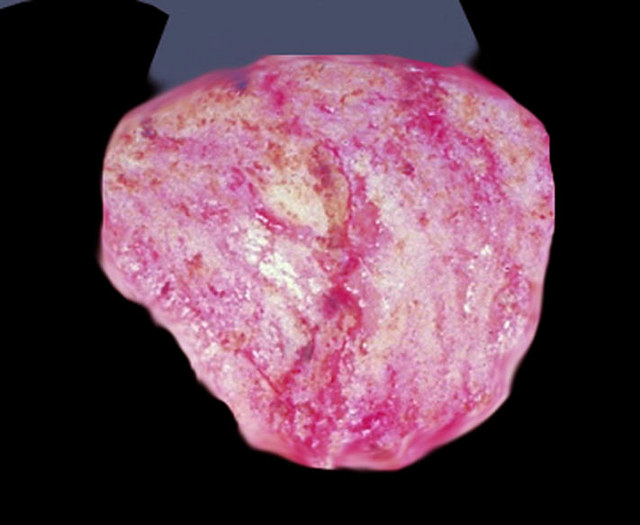
Gross description
- Median: 3 cm
- Circumscribed, soft, tan-red-brown
- Nodular or lobulated
- Multifocal lesions are multilobulated, circumscribed and fleshy tumors (Int J Oral Maxillofac Surg 2021;50:327)
Gross images
Contributed by Mark R. Wick, M.D.
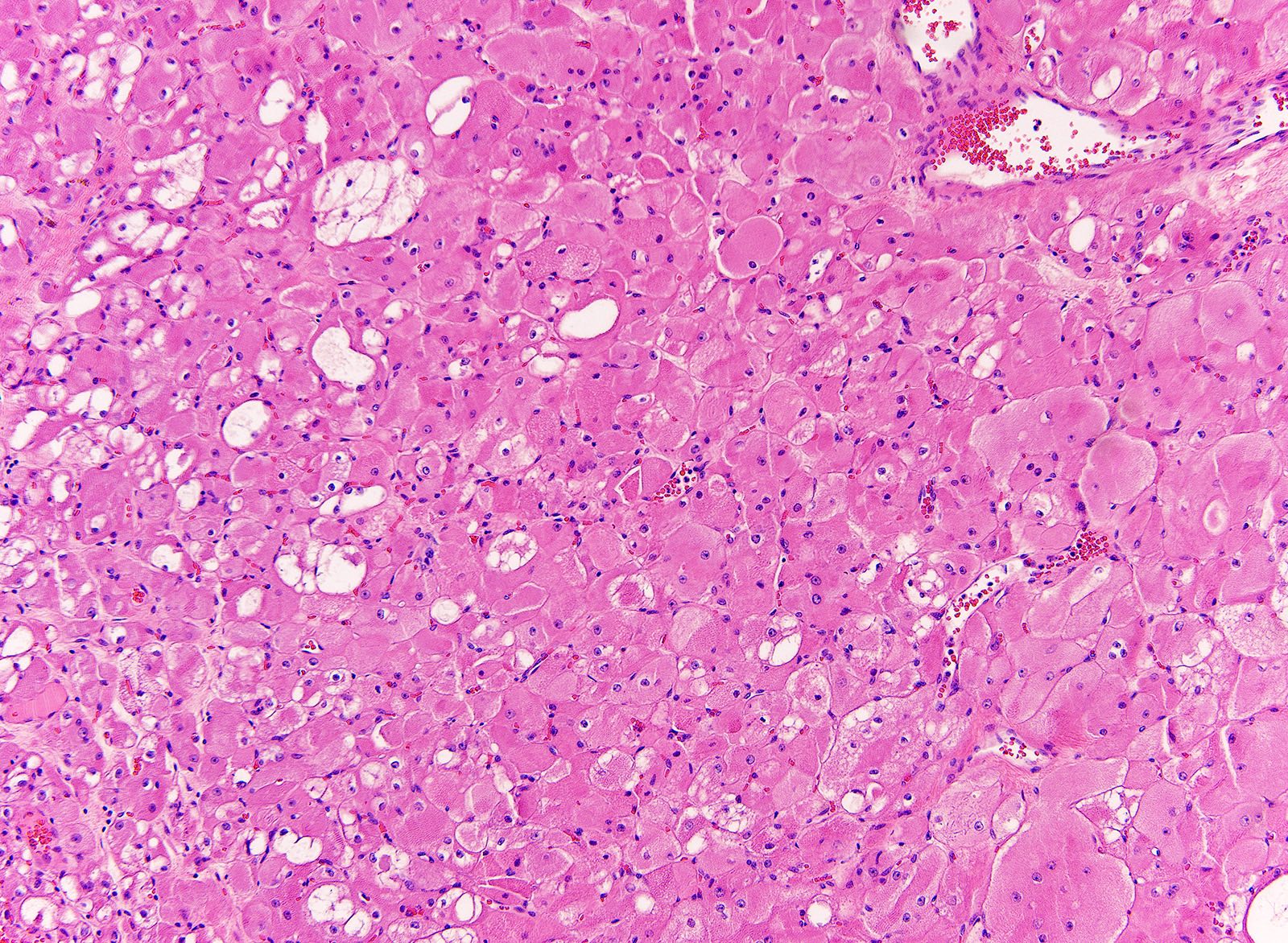
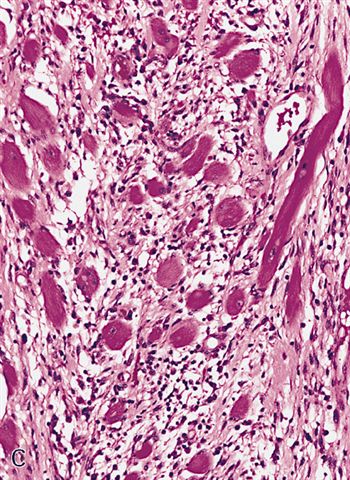
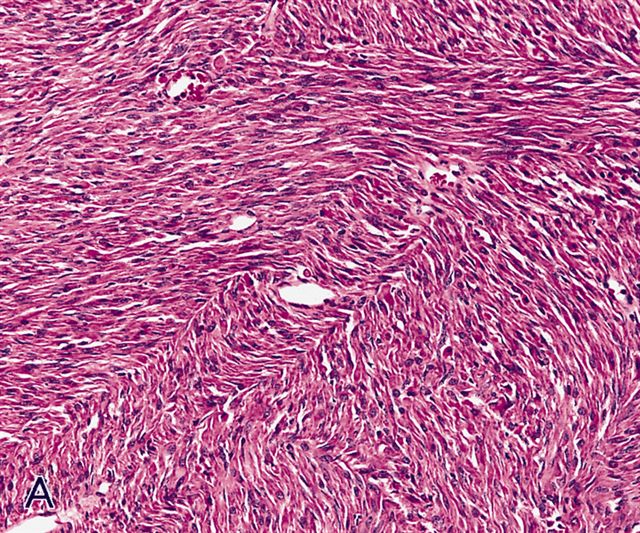
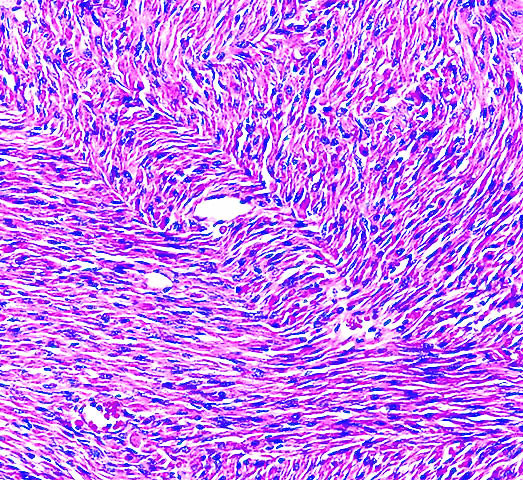
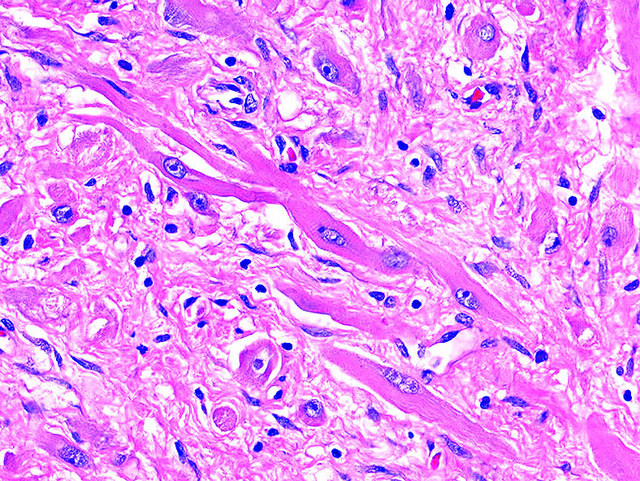
Microscopic (histologic) description
- Well circumscribed, not encapsulated, sheets of large, well differentiated skeletal muscle cells
- Cells are round or polygonal with abundant eosinophilic fibrillar or granular cytoplasm with frequent cross striations and intracytoplasmic rod-like inclusions (Head Neck Pathol 2021;15:1253)
- Nuclei are small, round and vesicular; may have prominent nucleoli
- May have spider cells with vacuolated cytoplasm (cells resemble spider webs) (Cancer 1980;46:780)
- Variable glycogen and lipid
- No mitotic activity, no atypia
Microscopic (histologic) images
Contributed by Carina Dehner, M.D., Ph.D.
Cytology description
- Fragments of tumor cells, large and polygonal cells
- Cells are grouped into large loosely cohesive clusters with scattered individual cells
- Abundant eosinophilic cytoplasm with a small round to oval, peripherally located nuclei
- Round nucleoli and cytoplasmic striation may be seen (Diagn Cytopathol 2011;39:686)
Cytology images
Images hosted on other servers:
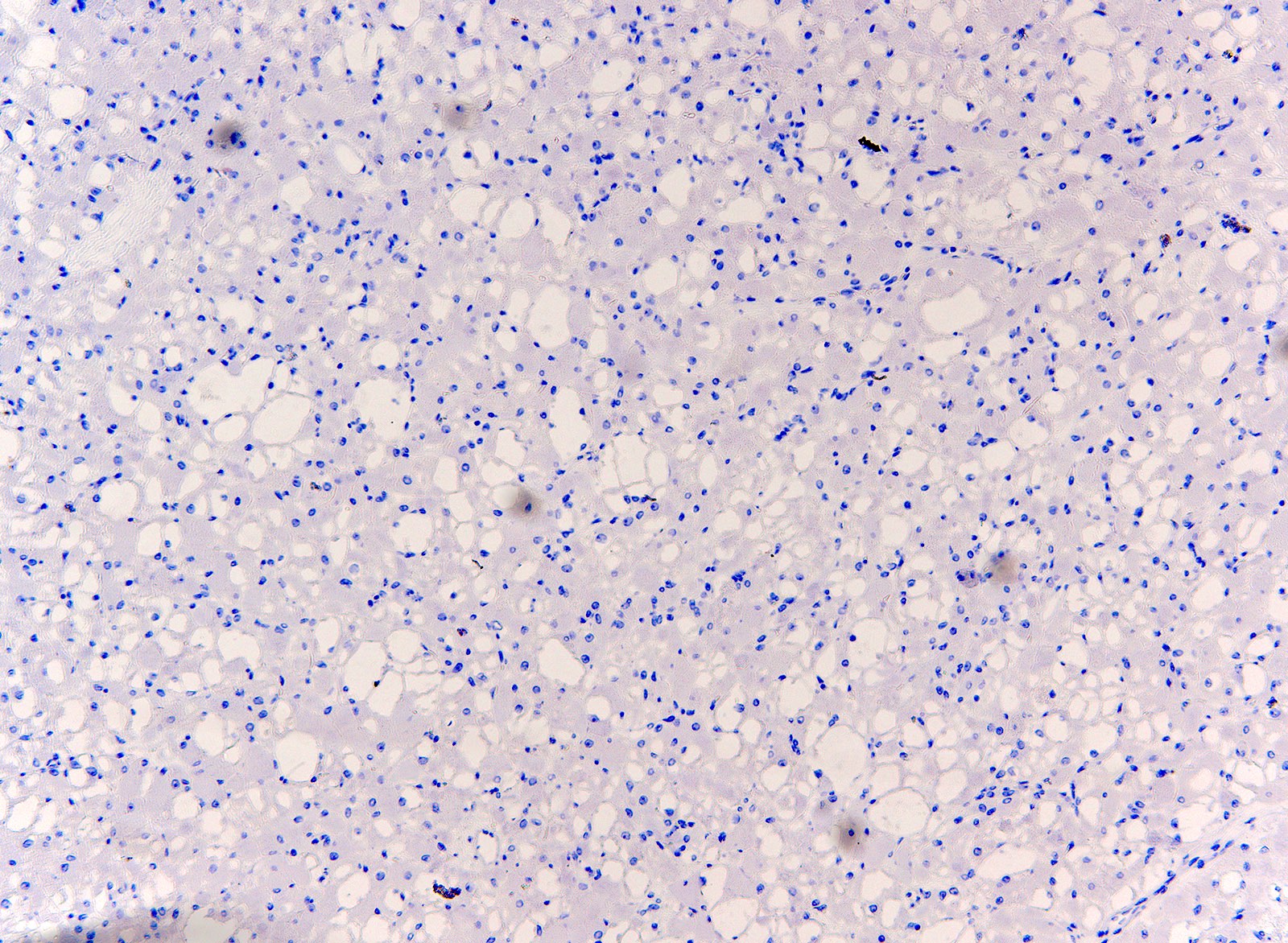
Positive stains
- MyoD1, myogenin, muscle specific actin, desmin and myoglobin (100%) (Case Rep Otolaryngol 2017;2017:7186768)
- PAS+, diastase sensitive (detects glycogen)
- PTAH and Masson trichrome highlight cross striations and rod-like inclusions
Negative stains
- Keratin, EMA, CD68, S100 (or weak) (Case Rep Otolaryngol 2017;2017:7186768)
Electron microscopy description
- Actin and myosin filaments with Z bands, ample mitochondria and cytoplasmic glycogen can be detected (Acta Cytol 2010;54:775)
Sample pathology report
- Soft tissue, mass, excision:
- Rhabdomyoma, adult type (see comment)
- Comment: The H&E sections show a well circumscribed mass composed of sheets of large, well differentiated skeletal muscle cells with abundant eosinophilic fibrillar cytoplasm and frequent cross striations. The nuclei are small, round and vesicular. No mitotic figures or atypia are identified. Immunohistochemistry shows that the tumor cells are diffusely positive for MyoD1, myogenin, muscle specific actin, desmin and negative for keratin AE1 / AE3, CD68 and S100.
Differential diagnosis
- Oncocytoma:
- Benign salivary gland neoplasm
- Positive for epithelial markers, whereas muscular markers are negative (Head Neck Pathol 2021;15:1253)
- Alveolar soft part sarcoma:
- Organoid and nest-like growth pattern
- TFE3 and cathepsin K+
- Myogenin and MyoD1-
- Crystal storing histiocytosis:
- Absence of cross striations or glycogen
- Granular cell tumor:
- Finely granular cytoplasm
- Devoid of cross striations and defined borders (Head Neck Pathol 2021;15:1253)
- No skeletal muscle differentiation, no glycogen; smaller cells have poorly defined cell borders
- Often overlying pseudoepitheliomatous hyperplasia
- S100+, myogenin-
- Hibernoma:
- No skeletal muscle differentiation, no glycogen
- Intracytoplasmic lipid droplets, centrally placed nuclei (Head Neck Pathol 2021;15:1253)
- S100+
- Paraganglioma:
- NSE+, synaptophysin+, chromogranin+
- Rhabdomyosarcoma:
- Rhabdomyosarcomas show nuclear atypia and pleomorphism (Head Neck Pathol 2021;15:1253)
- Ill circumscribed and infiltrative tumor
- Subtypes: embryonal, alveolar, spindle cell / sclerosing, pleomorphic
Fetal type rhabdomyoma
Definition / general
Essential features
Terminology
ICD coding
Epidemiology
Sites
Clinical features
Diagnosis
Radiology description
Radiology images
Images hosted on other servers:
Case reports
Prognostic factors
Treatment
Clinical images
Images hosted on other servers:
Gross description
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D. and AFIP
Cytology description
Cytology images
Images hosted on other servers:
Positive stains
Negative stains
Electron microscopy description
Molecular / cytogenetics description
Sample pathology report
Differential diagnosis
- Rare, benign tumor of immature skeletal muscle differentiation, usually in the head and neck
Essential features
- Rare, benign skeletal muscle tumor
- More common in male patients, in the head and neck
- Distinguished from adult rhabdomyoma by the presence of elongated immature rhabdomyocytes in varying stages of differentiation (Cancer 1972;30:160)
- Often detected at birth or even during pregnancy (Cureus 2021;13:e18096)
Terminology
- Myxoid type is called the classic type
- Cellular type is also called juvenile or intermediate rhabdomyoma
ICD coding
- ICD-O: 8900/0 - rhabdomyoma, NOS
- ICD-11
- 2E86.2 & XH8WG9 - rhabdomyoma & rhabdomyoma, NOS
- 2E86.2 & XH4729 - rhabdomyoma & fetal rhabdomyoma
Epidemiology
- 70% male; median age is 4.5 years with a range between 3 and 58 years old (Hum Pathol 1993;24:754)
- Less common than the adult type (Am J Dermatopathol 2014;36:e93)
- M > F (M:F = 2.3:1) (Hum Pathol 1993;24:754)
- Myxoid type occurs only in infants as subcutaneous lesions in the head and neck
- Cellular type tends to present in older individuals (adolescents or adults) (Int J Pediatr Otorhinolaryngol 2006;70:1115)
Sites
- Usually head and neck; postauricular region is the most common site (Hum Pathol 1993;24:754)
Clinical features
- Very rare
- Symptoms differ according to location; usually a painless mass
- Multiple cases of fetal rhabdomyoma have been reported in patients with nevoid basal cell carcinoma syndrome (Gorlin syndrome) (Virchows Arch 2011;459:235)
Diagnosis
Radiology description
- MRI: localized soft tissue thickening with equal T1 and T2 signals or slightly shorter T1 and T2 signals (Ear Nose Throat J 2024 Oct 7 [Epub ahead of print])
Radiology images
Images hosted on other servers:
Case reports
- 2 month old boy with an asymptomatic mass over the left masseter (Children (Basel) 2023;10:1818)
- 25 year old man presented with a 6 month history of liquid and solid dysphagia (Cureus 2021;13:e18096)
- 59 year old man presented with cough and breathing difficulties (Pathologica 2021;113:436)
Prognostic factors
- Local recurrence may rarely occur (incomplete resection) (Int J Pediatr Otorhinolaryngol 2006;70:1115)
- Malignant transformation is very rare (Cancer 1991;67:2907)
Treatment
- Complete excision
Clinical images
Images hosted on other servers:
Gross description
- Median: 3 - 5 cm
- Solitary, well circumscribed mass of soft tissue or mucosa
- Gray-white / tan-pink, soft with glistening mucoid cut surface (Hum Pathol 1993;24:754)
- Rare cases are multifocal
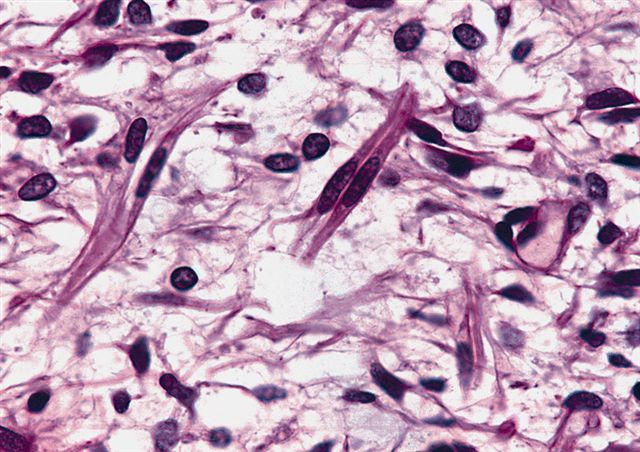
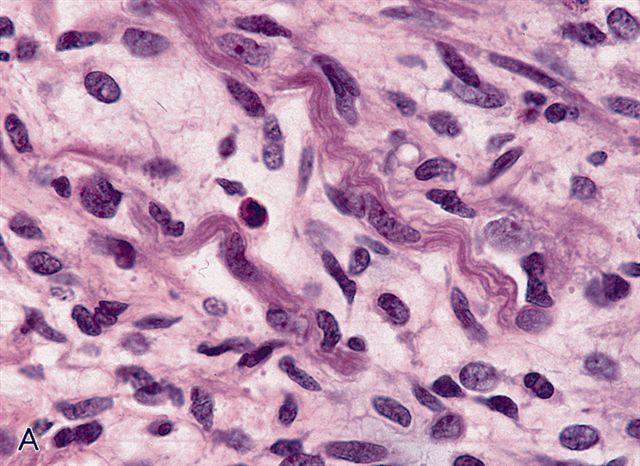
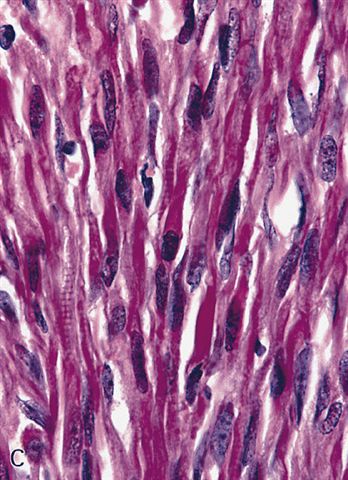
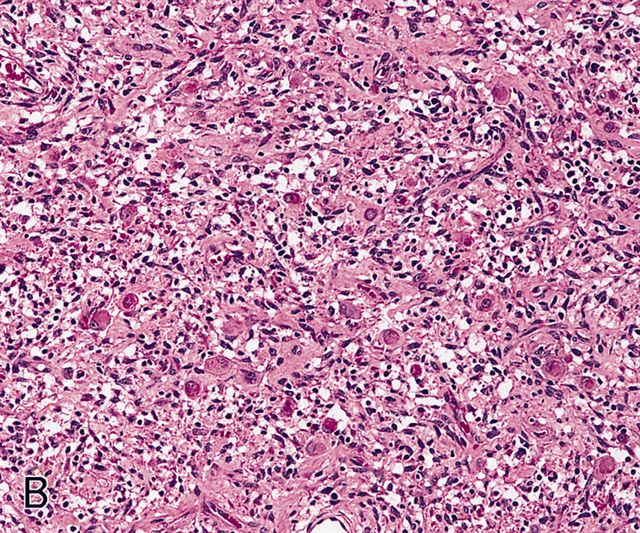
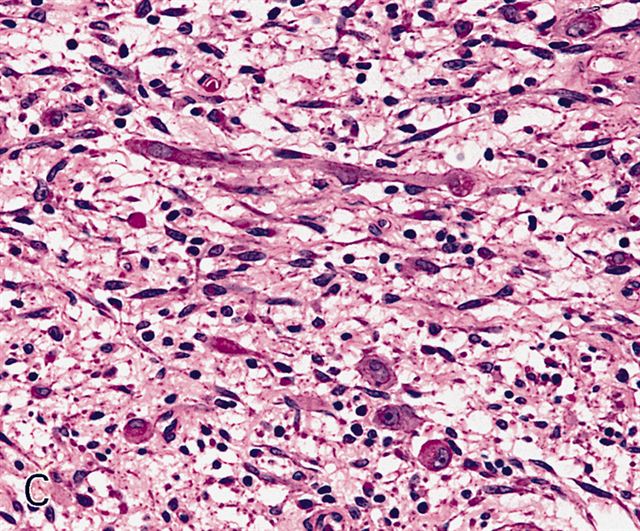
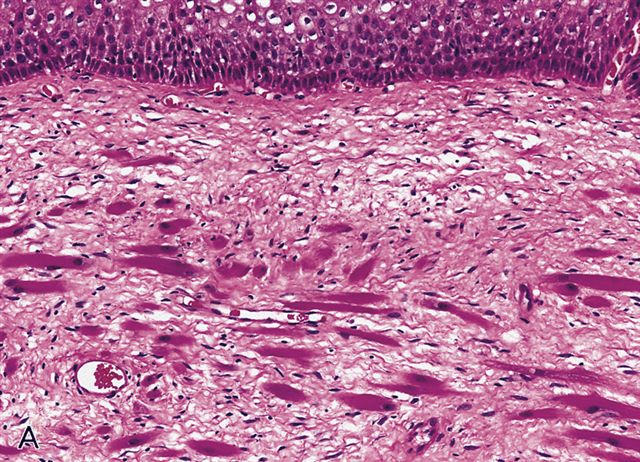
Microscopic (histologic) description
- Circumscribed but not encapsulated
- Myxoid
- Mild to moderately cellular
- Bundles or fascicles of immature muscle fibers haphazardly arranged
- Admixed with undifferentiated round / oval or spindled mesenchymal cells
- Myofibrils and cross striation may be identified in scattered strap and ribbon shaped cells
- Undifferentiated cell components are in the center and skeletal muscle cells mature towards the periphery (Cancer 1972;30:160)
- Stroma is myxoid or fibromyxoid
- Cellular
- Bundles or fascicles of cells in interlacing patterns
- Sparse collagenous or myxoid stroma
- Cells have variable skeletal muscle differentiation ranging from immature cells of myxoid pattern to ganglion cell-like rhabdomyoblasts with prominent nucleoli or strap cells with abundant basophilic or eosinophilic cytoplasm and prominent cross striations
- Infiltration of skeletal muscle may make margins difficult to determine
- Usually no or rare mitosis
- Few cases showed mitotic activity ranging from 1 to 14/50 high power fields (HPF) (Hum Pathol 1993;24:754)
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D. and AFIP
Cytology description
- Spindle cells and rhabdomyoblasts with abundant eosinophilic cytoplasm (Singapore Med J 2009;50:e138)
Cytology images
Images hosted on other servers:
Positive stains
Negative stains
- Keratin, EMA, CD68
- S100 (can be rarely expressed in primitive mesenchymal cells) (Ear Nose Throat J 2024 Oct 7 [Epub ahead of print], Int J Pediatr Otorhinolaryngol 2006;70:1115)
Electron microscopy description
- Thick and thin myofilaments with Z bands and glycogen within the cytoplasm of the rhabdomyoblasts
Molecular / cytogenetics description
- Aberrations at the PTCH1 locus has been identified in some cases (PTCH1 frameshift and homozygous deletions) (J Pathol 2013;231:44)
Sample pathology report
- Soft tissue, mass, excision:
- Rhabdomyoma, fetal type (see comment)
- Comment: The H&E sections show bundles of immature muscle fibers arranged haphazardly, admixed with undifferentiated round spindled mesenchymal cells and myxoid stroma. The undifferentiated cell components are in the center, while the skeletal muscle cells mature toward the periphery. Immunohistochemistry shows the tumor cells are diffusely positive for MyoD1, myogenin, muscle specific actin, desmin and negative for keratin AE1 / AE3, CD68 and S100.
Differential diagnosis
- Botryoid variant of embryonal rhabdomyosarcoma:
- Resembles myxoid variant of fetal rhabdomyoma but has a deep location
- True cambium layer, atypia, numerous mitotic figures, tumor cell necrosis, infiltrative margins
- No maturation of cells at the periphery
- Leiomyoma with trapped skeletal muscle elements:
- Scattered polygonal cells with cross striations (entrapped skeletal muscle) and spindled cells with cross striations (reactive myoblasts)
- Caldesmon is positive in leiomyoma and negative in rhabdomyoma (Am J Dermatopathol 2014;36:e93)
- Rhabdomyomatous mesenchymal hamartoma:
- Mature skeletal muscle elements admixed with adipose tissue, neural and adnexal elements and collagen fibers (Am J Dermatopathol 2014;36:e93)
- S100+
- Neuromuscular hamartoma:
- Benign tumor composed of well differentiated skeletal muscle and nerve fibers; arises in the major peripheral nerves
- Nerve fibers are either myelinated or nonmyelinated and present within and between the muscle bundles
- Nerve fibers are S100+ (J Surg Oncol 1984;26:158)
- Spindle cell variant of embryonal rhabdomyosarcoma:
- Resembles the cellular variant of fetal rhabdomyoma but has cellular pleomorphism and necrosis (Arch Pathol Lab Med 2013;137:1155)
Genital type rhabdomyoma
Definition / general
Essential features
Terminology
ICD coding
Epidemiology
Sites
Clinical features
Diagnosis
Radiology description
Prognostic factors
Case reports
Treatment
Gross description
Gross images
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
AFIP images
Positive stains
Negative stains
Electron microscopy description
Molecular / cytogenetics description
Sample pathology report
Differential diagnosis
- Rare, benign tumor with skeletal muscle differentiation in the vagina, vulva, cervix and rarely urethra
- Paratesticular rhabdomyoma often has distinctive morphologic features and is considered to be a distinct histologic subtype, referred to as sclerosing rhabdomyoma (SRM) (Am J Surg Pathol 2013;37:1737)
Essential features
- Rare, benign tumor with skeletal muscle differentiation
- Usually in middle aged women
- Vagina is the most common site
Terminology
- Historically classified as fetal rhabdomyoma
ICD coding
- ICD-O: 8900/0 - rhabdomyoma, NOS
- ICD-11
- 2E86.2 & XH8WG9 - rhabdomyoma & rhabdomyoma, NOS
- 2E86.2 & XH5AF2 - rhabdomyoma & genital rhabdomyoma
Epidemiology
- Usually seen in the lower genital tract of middle aged women
- 30 - 50 years of age (mean age: 42 years) (Hum Pathol 2012;43:597)
- Rarely occurs in men
Sites
- Uterine cervix, vagina, vulva and rarely ovary and urethra (Hum Pathol 2012;43:597)
- Vagina is the most common site (Int J Gynecol Pathol 2018;37:349)
- Rarely occurs in men in the paratesticular region, epididymis or in the tunica vaginalis of the testis or prostate
Clinical features
- Usually present as slow growing, solitary, asymptomatic masses and are found incidentally
- May be symptomatic according to the location, presenting with vaginal bleeding or dyspareunia (Hum Pathol 2012;43:597)
Diagnosis
Radiology description
- MRI: enhancing mass with signal intensity following muscle on T1 and T2 weighted sequences
Prognostic factors
- Very low risk of local recurrence (Hum Pathol 1993;24:608)
Case reports
- 30 year old woman with a fetal rhabdomyoma presenting as a vaginal mass (Int Urogynecol J 2021;32:3095)
- 32 year old woman presented with secondary sterility and a suspected uterine fibroid (Int J Gynecol Pathol 2021;40:97)
- 35 year old woman presented with a polypoidal mass arising from ectocervix (Indian J Pathol Microbiol 2020;63:467)
Treatment
- Local excision is curative
Gross description
- Well circumscribed, solitary, polypoid mass up to 3 cm (Hum Pathol 2012;43:597)
- Covered by smooth mucosa
Gross images
Images hosted on other servers:
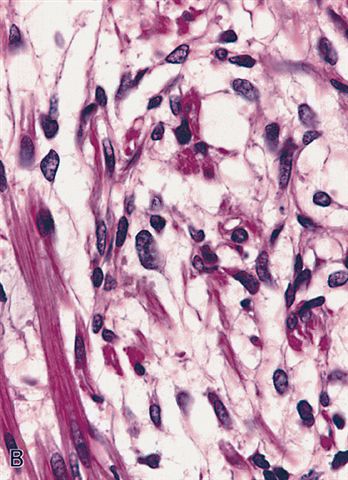
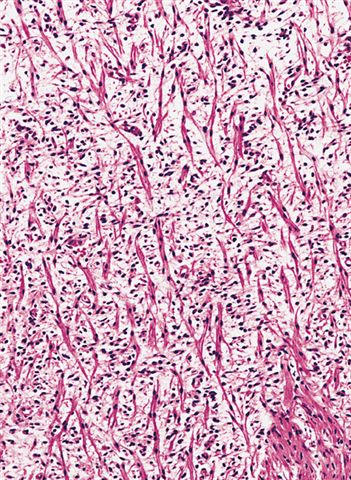
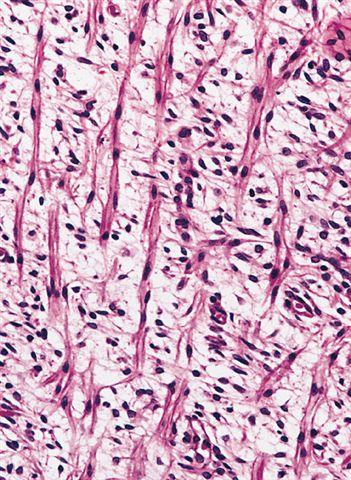
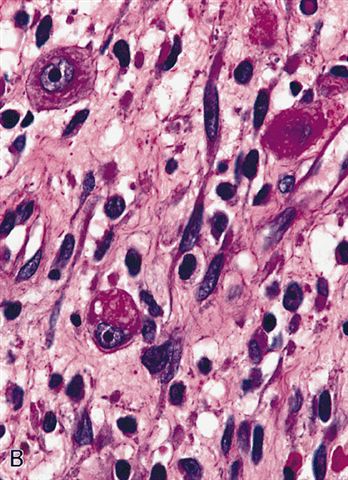
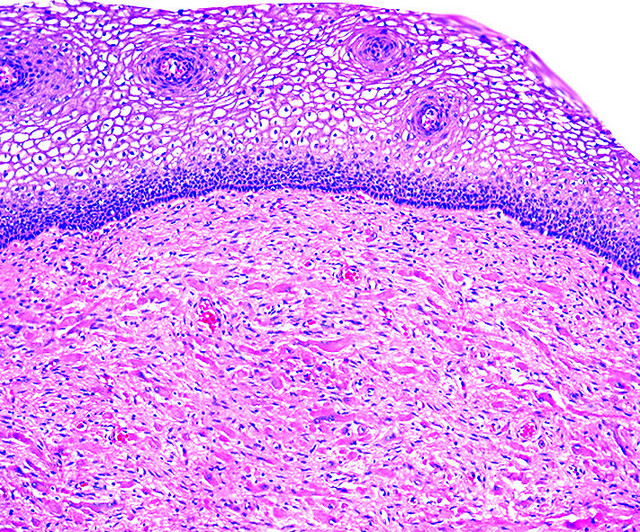
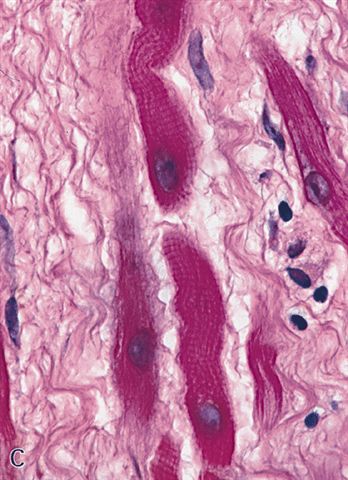
Microscopic (histologic) description
- Submucosal, polypoid, well circumscribed, no capsule
- Scattered and haphazardly arranged rhabdomyoblasts, intermixed in a loose fibrous stroma with dilated vessels
- Cells have abundant eosinophilic cytoplasm with glycogen, cross striations and longitudinal myofibrils
- Nuclei are round, vesicular, central and uniform
- May have binucleated or multinucleated cells
- No / rare mitotic figures, no cambium layer, no spider cells, no spindle cells or rhabdomyoblasts, no necrosis, no nuclear pleomorphism
- Unusual forms
- Resembles cellular type fetal rhabdomyoma with minimal intervening stroma (Int J Gynecol Pathol 2018;37:349)
- Few tumors are paucicellular
Microscopic (histologic) images
AFIP images
Positive stains
- Myogenin, MyoD1, muscle specific actin and desmin highlight rod-like structures; myoglobin (100%) (Hum Pathol 2012;43:597)
- Ki67 (< 1%) (Diagn Pathol 2012;7:47)
Negative stains
Electron microscopy description
- Similar to adult rhabdomyoma
- Small foci of Z band material can be identified; they do not form the rod inclusions noted in the adult type
- Differs from adult type rhabdomyoma by cytoplasmic bodies, peripheral couplings and specialized cell to cell attachments (Cancer 1976;37:2283)
Molecular / cytogenetics description
- Paratesticular rhabdomyoma with sclerosing rhabdomyoma morphology harbors a recurrent H3C2 p.K37I mutation (Am J Surg Pathol 2013;37:1737)
Sample pathology report
- Soft tissue, mass, excision:
- Rhabdomyoma, genital type (see comment)
- Comment: The H&E sections show a submucosal, well circumscribed mass formed of scattered and haphazardly arranged rhabdomyoblasts, intermixed in a loose fibrous stroma with dilated vessels. The cells have abundant eosinophilic cytoplasm with cross striations and small bland nuclei. No atypia, mitosis or necrosis was identified. Immunohistochemistry shows the tumor cells are diffusely positive for MyoD1, myogenin, muscle specific actin, desmin and negative for keratin AE1 / AE3, CD68 and S100.
Differential diagnosis
- Botryoid variant of embryonal rhabdomyosarcoma:
- Grape-like vesicles, often with ulceration of the overlying epithelium (Hum Pathol 2012;43:597)
- Patients are usually < 25 years old and present with a rapidly growing mass with a cambium layer, atypia and mitotic activity
- Primitive small and basophilic cells with scant cytoplasm and spindled cells
- Alternating hypercellular and hypocellular zones (Int J Gynecol Pathol 2018;37:349)
- Fibroepithelial stromal polyp:
- Fibromatous stroma covered with benign squamous epithelium
- No rhabdomyoblasts
- Myogenin and MyoD1 are usually negative (Int J Gynecol Pathol 2018;37:349)
- Dedifferentiated liposarcoma with heterologous rhabdomyoblastic differentiation:
- Atypia, mitotic activity
- MDM2+
Board review style question #1
A 30 year old woman presented with a 2 cm vaginal polyp. Histologic details are shown in the image above. Regarding this entity, which of the following statements is true?
- Cells are positive for myogenin
- Ki67 proliferative index is very high (> 50%) in this tumor
- Often associated with overlying pseudoepitheliomatous hyperplasia
- S100 is always positive
- Shows cellular pleomorphism and necrosis
Board review style answer #1
A. Cells are positive for myogenin. The image shows genital type rhabdomyoma, which most commonly presents in the vagina as a polyp. Histologically, rhabdomyoma is formed of scattered and haphazardly arranged rhabdomyoblasts, intermixed in a loose fibrous stroma with dilated vessels. Cells have abundant eosinophilic cytoplasm with glycogen, cross striations and longitudinal myofibrils and are positive for myogenin, MyoD1, muscle specific actin and desmin.
Answer C is incorrect because pseudoepitheliomatous hyperplasia is usually associated with granular cell tumors.
Answer B is incorrect because Ki67 proliferative index is usually very low (< 1%).
Answer D is incorrect because S100 is positive in granular cell tumor and nerves.
Answer E is incorrect because rhabdomyosarcoma shows cellular pleomorphism and necrosis, not rhabdomyoma.
Comment Here
Reference: Rhabdomyoma
Comment Here
Reference: Rhabdomyoma
Board review style question #2
Regarding adult type rhabdomyoma, which of the following statements is true?
- Cells are positive for synaptophysin
- May arise in the context of Gardner syndrome
- More common in female patients
- Mostly found in the head and neck
Board review style answer #2
D. Mostly found in the head and neck. Answer A is incorrect because paraganglioma is positive for synaptophysin while rhabdomyoma is negative. Answer C is incorrect because adult type rhabdomyoma is more common in male patients. Answer B is incorrect because adult type rhabdomyoma can be associated with Birt-Hogg-Dubé (BHD) syndrome, not Gardner syndrome.
Comment Here
Reference: Rhabdomyoma
Comment Here
Reference: Rhabdomyoma