Table of Contents
Definition / general | Essential features | Terminology | Physiology | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ojukwu K, Hutchings D. Histology-small intestine. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelnormalhistology.html. Accessed March 31st, 2025.
Definition / general
- Extends from gastric pylorus to ileocecal valve
- Layers include mucosa, submucosa, muscularis propria (externa), subserosa and serosa (described luminal to external)
- Functions relies on the structure of mucosal villi and crypts, lined by columnar cells
Essential features
- Extends from gastric pylorus to ileocecal valve
- Composed of duodenum, jejunum and ileum
- Layers include mucosa, submucosa, muscularis propria (externa), subserosa and serosa (described luminal to external)
- Villi lined by columnar absorptive cells and goblet cells
- Crypts comprise the lower portion of mucosa and contain Paneth cells, endocrine cells and undifferentiated (immature) crypt cells
Terminology
- Small bowel
- Duodenum, jejunum, ileum
Physiology
- Villi are the location for digestion and absorption of food into the columnar cells (Gastrointest Endosc Clin N Am 2017;27:1)
- Crypts secrete ions and water and deliver IgA and antimicrobial peptides to the lumen
- Cell division and renewal occur in crypts
- Mucous cells generate adherent mucous layer that protects the epithelium and allows uptake of nutrients
- Terminal ileum absorbs intrinsic factor vitamin B12 complexes
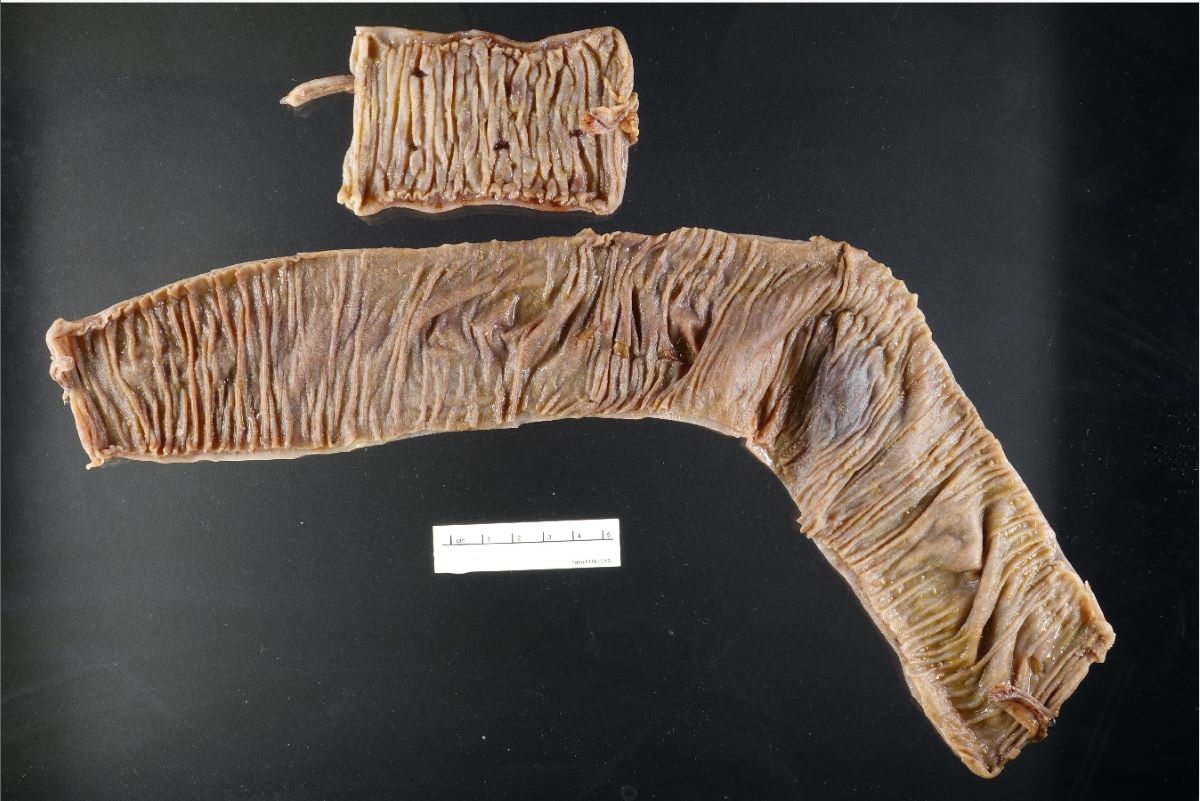
Gross description
- Small intestine is approximately 6 - 7 m in length (Gastrointest Endosc Clin N Am 2017;27:1)
- Duodenum:
- Retroperitoneal, except for first part
- Common bile duct and pancreatic duct enter the second part of the duodenum at the ampulla of Vater
- Suspensory duodenal ligament (ligament of Treitz) divides duodenum from jejunum
- Jejunum and ileum:
- Intraperitoneal
- Transition between the jejunum and ileum is not clearly defined
- Wall of jejunum is thicker due to prominent circular mucosal folds (folds of Kerckring / plicae circulares) (Gastrointest Endosc Clin N Am 2017;27:1)
- Small intestine ends at the ileocecal valve
Microscopic (histologic) description
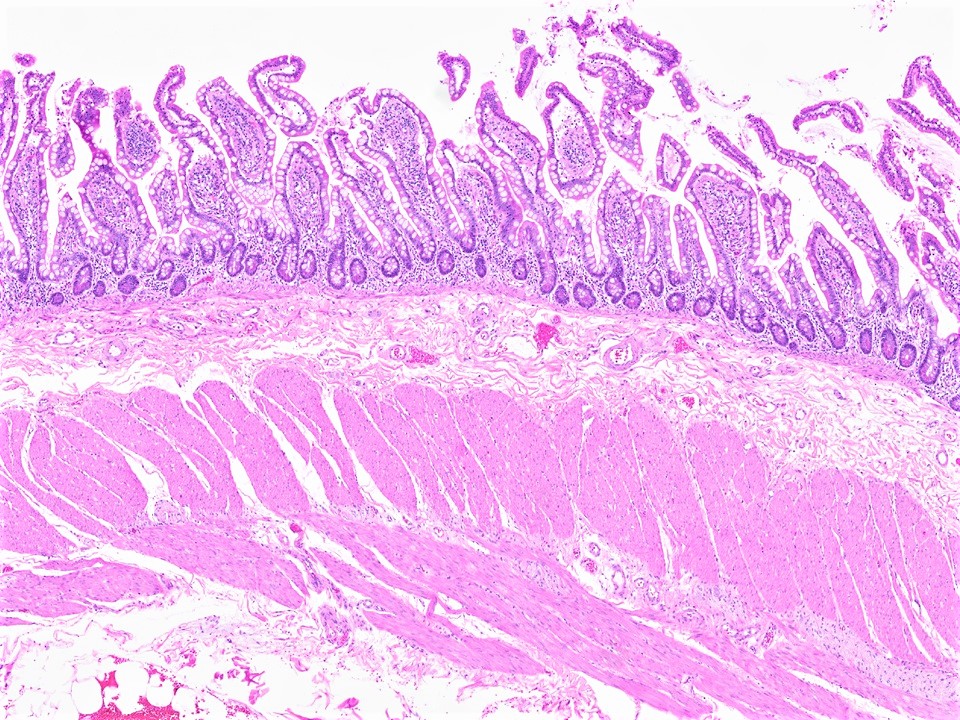
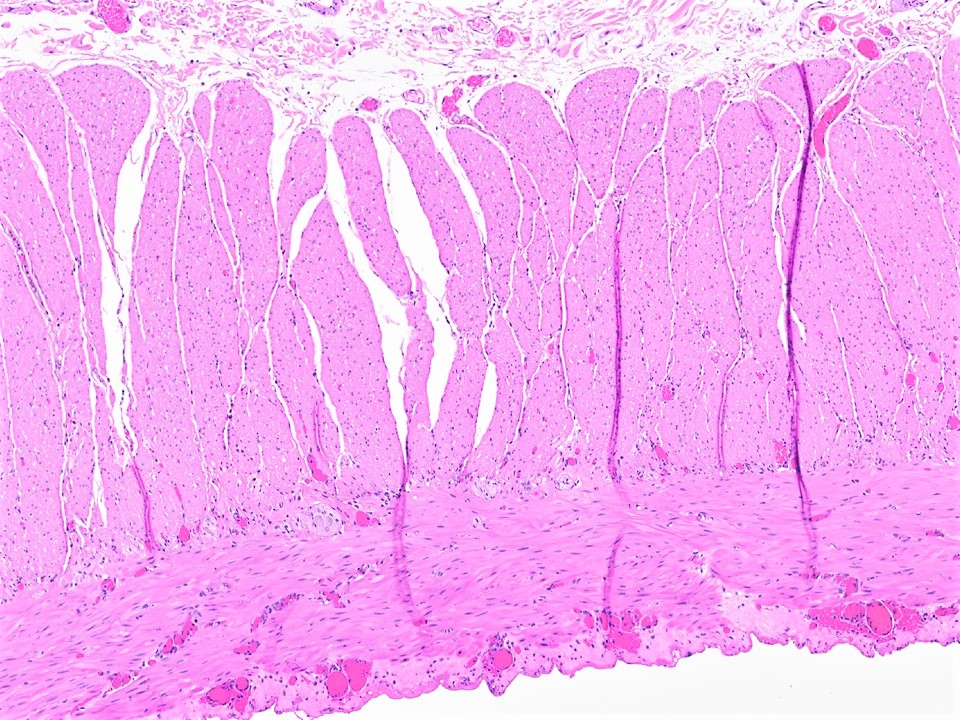
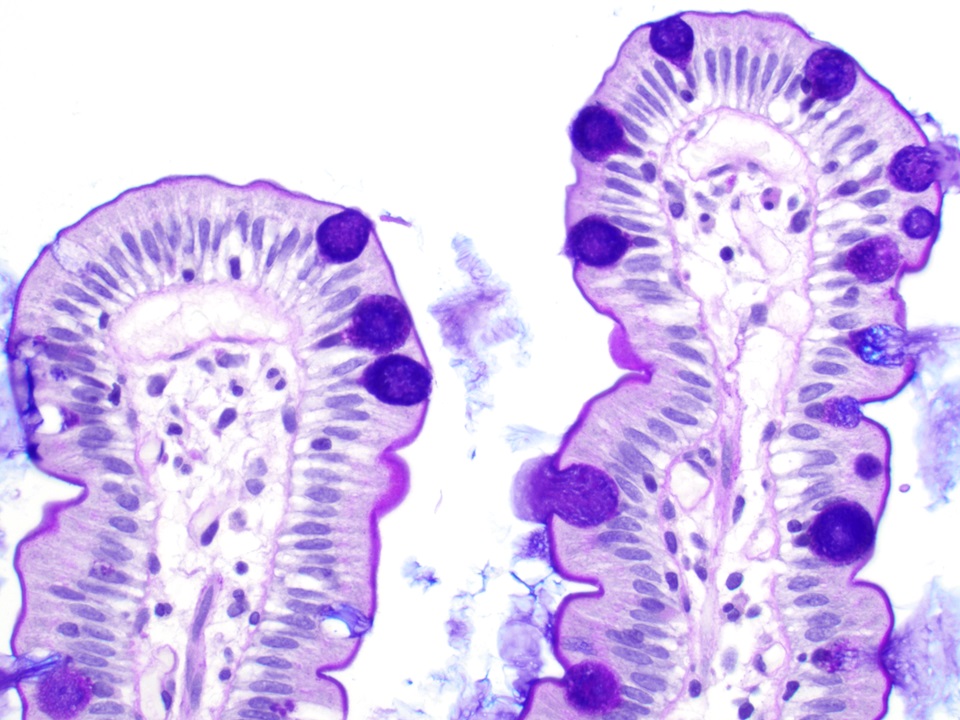
- Mucosa:
- Contains villi (finger-like projections) with central blood vessels, lymphatics
- Layers are epithelium, lamina propria and muscularis mucosa
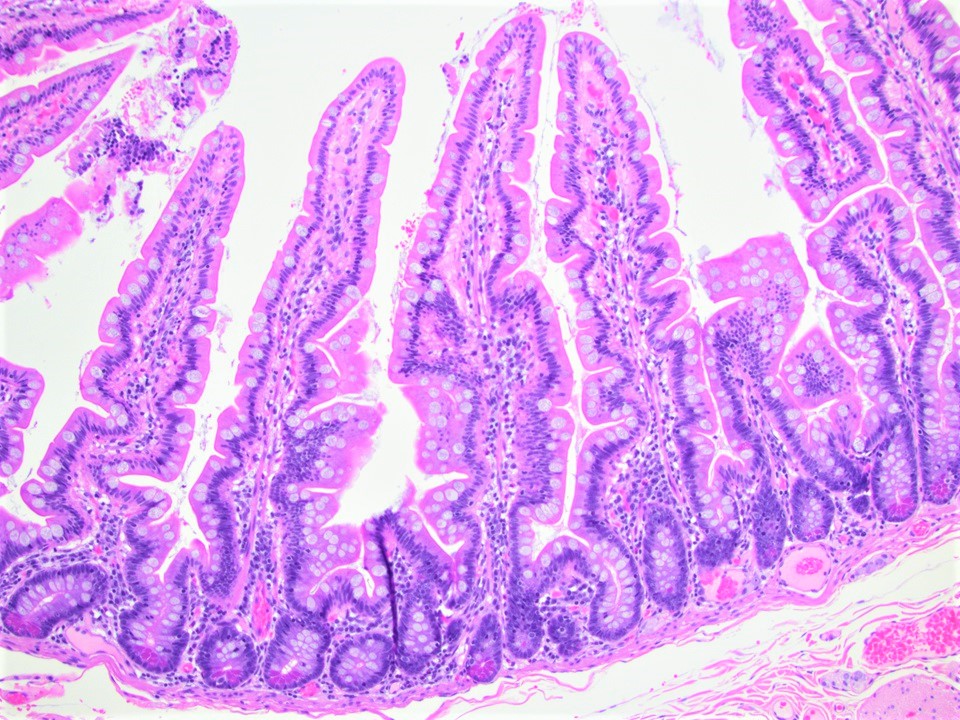
- Villi:
- Tallest in the jejunum, may be shorter or show more variability in height in duodenum
- Surface lined by microvilli
- Villus to crypt length ratio is 3 - 5:1
- Lined by primarily columnar absorptive cells and goblet cells
- Scattered intraepithelial lymphocytes (T cells), usually 1 lymphocyte per 5 enterocytes
- Villi may be shorter and distorted next to lymphoid aggregates
- In a biopsy, 4 normal villi in a row suggests normal villous architecture
- Each villus contains an arteriole with capillary network, veins and a central lymphatic with numerous nerve fibers
- Absorptive cells:
- Enterocytes
- Microvilli on luminal surface (brush border) and underlying mat of microfilaments (terminal web)
- Microvillus:
- 1.5 - 2 µm in length and 100 nm in diameter
- PAS positive, actin myosin complexes
- Goblet cells:
- Occur in crypts and surface absorptive cells
- Decrease towards villus tip, increase in frequency along small intestine (most numerous in lower ileum)
- Columnar in shape, mucus droplet in supranuclear area, secretes mucus, ions and water
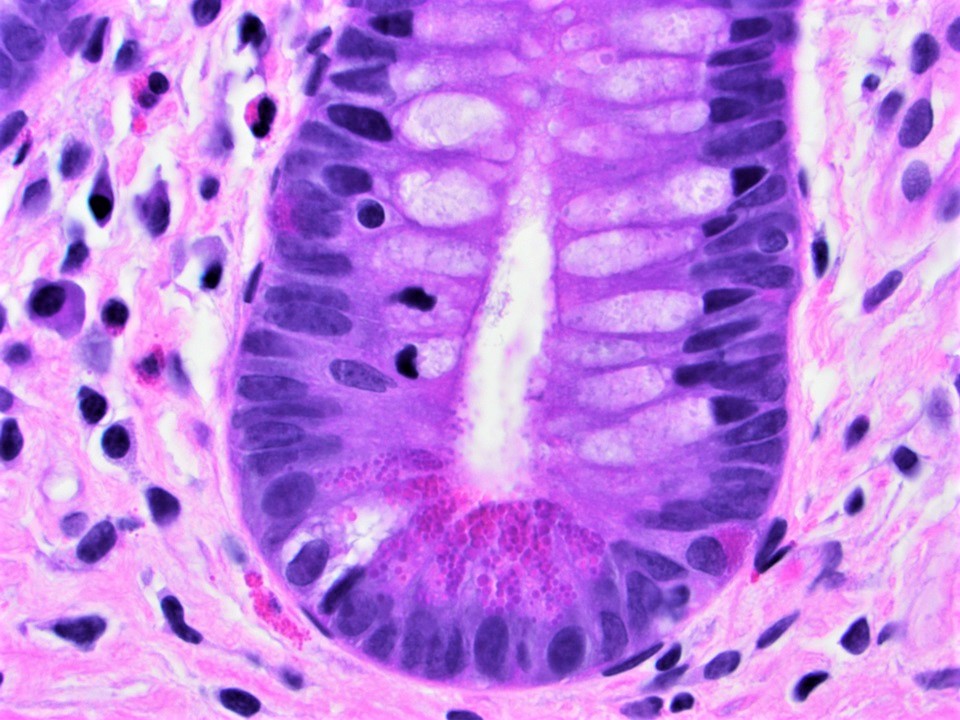
- Paneth cells:
- Populate crypt bases and increase in number from proximal to distal intestine
- Strongly eosinophilic, pyramidal cells with zymogenic or secretory cell characteristics
- Supranuclear Golgi complex contains large, chunky apical membrane bound eosinophilic granules
- Granules contain various proteins involved in host defenses including lysozyme, secretory phospholipase A2 and alpha defensins / cryptdins (World J Gastrointest Pathophysiol 2017;8:150)
- Crypts of Lieberkühn:
- Lower 20% of epithelium, contain undifferentiated (immature) crypt cells, Paneth cells, scattered goblet cells and endocrine cells
- Surrounded by pericrypt fibroblast sheath
- Secrete ions, water, IgA, antimicrobial peptides into lumen
- Crypt cells take 3 - 8 days to migrate to surface
- Allows for rapid repair but also causes these cells to be sensitive to radiation therapy and chemotherapy
- Lamina propria:
- Contains loose connective tissue, lymphocytes, plasma cells, occasional eosinophils, macrophages and mast cells
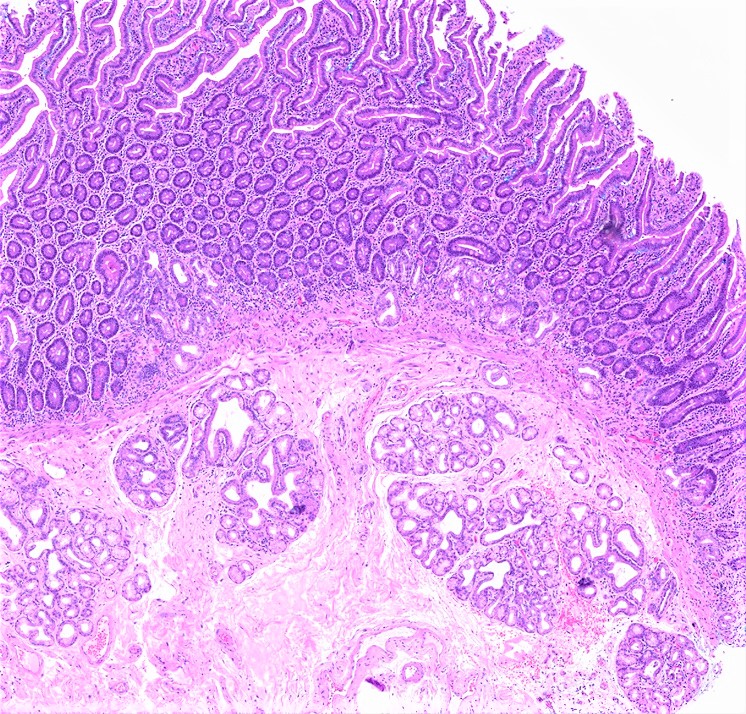
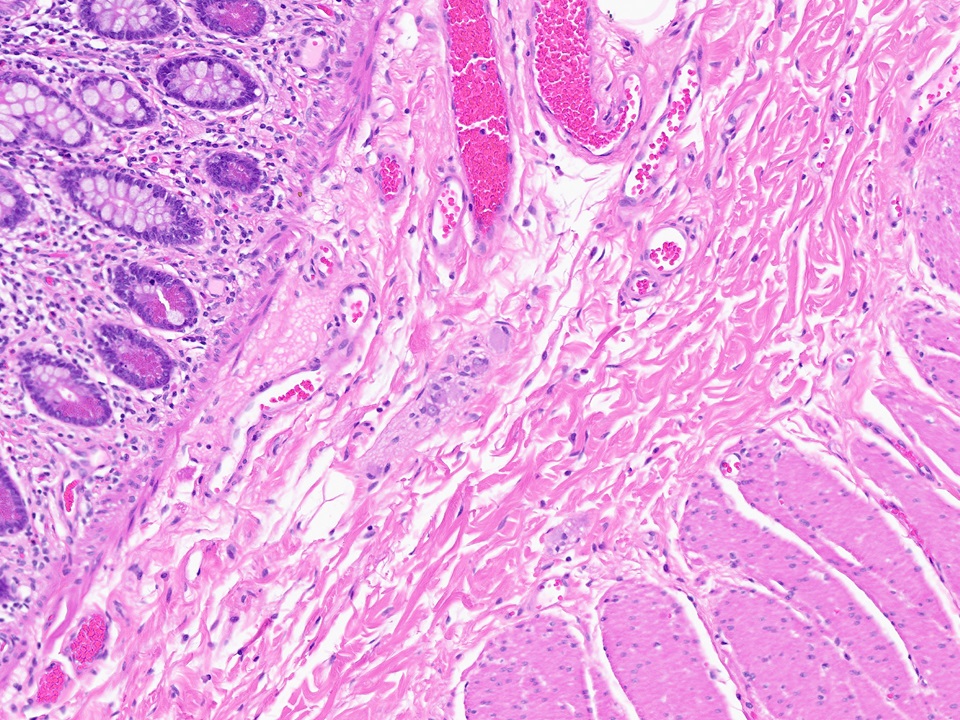
- Submucosa:
- Contains connective tissue, blood vessels, lymphatics, submucosal (Meissner) plexus
- Brunner glands in duodenum
- Brunner glands:
- Submucosal mucous glands in duodenum
- Secrete bicarbonate ions, glycoproteins, pepsinogen II
- Resemble gastric pylorus mucous glands
- Muscularis propria (externa):
- Inner circular and outer longitudinal layer, with myenteric (Auerbach) plexus between these layers
- Plexus also contains interstitial cells of Cajal, ganglion cells, fibroblasts (Am J Surg Pathol 2003;27:228)
- Serosa:
- Contains mesothelial lining, loose connective tissue
- Endocrine cells:
- Contain fine eosinophilic granules with secretory proteins
- Cytoplasmic granules are subnuclear (versus supranuclear granules in Paneth cells)
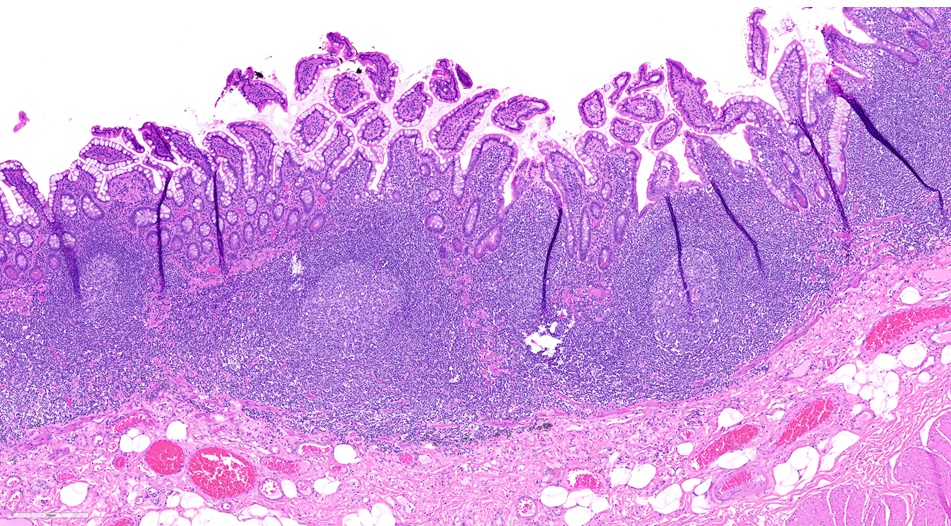
- Peyer patch:
- Lymphoid aggregates randomly distributed around circumference of the small intestine (partially mucosal, partially submucosal) with central germinal center
- Peyer patch germinal centers are more common in children than adults
- Increase in number distally in the small bowel and become confluent in the ileum
- Exogenous dark brown granular pigment may be present within macrophages (Hum Pathol 1987;18:50, Gut 1996;38:390)
Microscopic (histologic) images
Positive stains
- Epithelium: CK20, CDX2 (Am J Surg Pathol 2004;28:1352, Int J Dev Biol 2005;49:867)
Negative stains
Electron microscopy description
- Each microvillus contains a core bundle of vertically oriented, polarized actin filaments extending from the tip of the microvillus to the base of the terminal web
Videos
Small intestine: histology
Additional references
Board review style question #1
What is the location and function of the submucosal mucous glands shown above?
- Duodenum, secrete bicarbonate ions, glycoproteins, pepsinogen II
- Duodenum, secrete proteins involved in host defense (e.g. alpha defensins / cryptdins)
- Ileum, secrete proteins involved in host defense (e.g. alpha defensins / cryptdins)
- Jejunum, secrete bicarbonate ions, glycoproteins, pepsinogen II
Board review style answer #1
A. Duodenum, secrete bicarbonate ions, glycoproteins, pepsinogen II. Brunner glands are located in the duodenum and secrete bicarbonate ions, glycoproteins and pepsinogen II.
Comment Here
Reference: Histology - small intestine
Comment Here
Reference: Histology - small intestine
Board review style question #2
Resection of what segment of the small intestine puts the patient at risk for vitamin B12 malabsorption?
- First part of the duodenum
- Ileum
- Jejunum
- Second part of the duodenum
Board review style answer #2
B. Ileum. In the ileum, surface epithelial cells, specific receptors are present to uptake intrinsic factor vitamin B12 complexes.
Comment Here
Reference: Histology - small intestine
Comment Here
Reference: Histology - small intestine