Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alrohaibani A, Makhoul E, Wong M. Crohn's disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelcrohns.html. Accessed March 31st, 2025.
Definition / general
- Idiopathic chronic inflammatory condition that may involve any part of the upper and lower gastrointestinal tract
- Tends to involve the distal ileum and proximal large intestine
Essential features
- Diagnostic criterion: segmental disease, transmural inflammation, noncaseating granulomas, deep fissuring ulcers, ileal involvement
- Distal ileum is the most commonly involved part of the small intestine
- Risk of colorectal carcinoma increases with duration and extent of disease
Terminology
- Inflammatory bowel disease (IBD), Crohn's disease (CD), Crohn's
ICD coding
- ICD-10: K50 - Crohn's disease of the small intestine
Epidemiology
- Western counties, with the highest reported prevalence in Europe (322 per 100,000 in Germany) and North America (319 per 100,000 in Canada) (Lancet 2017;390:2769)
- Rising incidence in newly industrialized countries in Africa, Asia and South America (Lancet 2017;390:2769)
- Genetic predisposition through population and family based studies showed Crohn's disease with higher incidence among relatives with Crohn's disease, twins and Jewish population from middle European origin (Gastroenterology 2011;140:1704, Gastroenterology 1989;97:900, Med Clin North Am 1990;74:1)
- Bimodal age distribution, first peak between 15 - 30 years, where the majority of patients are diagnosed; the second peak is between 50 - 80 years of age (Am J Gastroenterol 2006;101:1559, Gastroenterology 1991;100:350, Med Clin North Am 1990;74:1)
- Slightly more common in women (F:M = 1.3:1)
Sites
- May occur anywhere in the GI tract, from oral cavity to perianal area
- Terminal ileum is the most commonly affected site (80%), with 33% having ileitis alone
- 50% of patients have ileocolitis (involvement of both terminal ileum and colon)
- About 20% of patients have limited colon disease, of which only half will have rectal sparing
- 33% of patients have perianal disease
- 5 - 15% can have oral gastroduodenal involvement, with significantly fewer patients developing esophageal and proximal small intestinal involvement
- Reference: UpToDate: Clinical Manifestations, Diagnosis, and Prognosis of Crohn Disease in Adults [Accessed 22 October 2021]
Pathophysiology
- Unclear, as overall pathogenesis remains poorly understood
- Inappropriate immune response has been implicated, with vast literature delineating the role of both host and microbial factors in its pathogenesis (Nat Rev Immunol 2008;8:458)
- Dysregulation in epithelial barriers, immune cells and secreted mediators have been shown to play a role (J Clin Invest 1983;72:142, Gut 2013;62:1734, Gastroenterology 2009;136:1261)
- Microbiota may induce inflammatory bowel disease if a concurrent underlying genetic defect is present (Nature 2012;491:119)
- More than 200 loci have been identified, many of which are shared among both Crohn's disease and ulcerative colitis (UC), indicating the overlap between these 2 entities; these loci lead to modulation of protein expression, rather than amino acid change, which supports that each locus confers an increased risk of developing Crohn's disease (Nature 2012;491:119, Inflamm Bowel Dis 2015;21:1166)
Etiology
- Idiopathic
- Some associations have been demonstrated:
- Smoking, as shown in meta analysis studies (Mayo Clin Proc 2006;81:1462, Am J Gastroenterol 2012;107:1399)
- Physical activity is inversely related to developing Crohn's disease, with some limited data suggesting exercise can even reduce disease activity (BMJ 2013;347:f6633, Prev Med Rep 2016;3:177, Inflamm Bowel Dis 2015;21:1063)
- Sleep deprivation (Inflamm Bowel Dis 2013;19:2440, Sleep Breath 2020;24:971)
- Infection and immune response with Salmonella and Campylobacter gastroenteritis, as shown in population based cohort studies (Nat Rev Immunol 2008;8:458, Gastroenterology 2009;137:495)
- Mycobacterium paratuberculosis (Expert Opin Biol Ther 2019;19:79)
- Unclear medication association (Am J Gastroenterol 2011;106:2133, Am J Gastroenterol 2014;109:1728, Am J Gastroenterol 2010;105:2610, Lancet Gastroenterol Hepatol 2020;5:986)
Clinical features
- Abdominal pain, diarrhea (bloody or nonbloody), fatigue and weight loss are classic symptoms (Am J Gastroenterol 2000;95:3458, Clin Gastroenterol Hepatol 2006;4:614, Am J Gastroenterol 2018;113:481)
- Patients with distal terminal ileal involvement can present with right lower quadrant abdominal pain
- Distal ileum is the most commonly involved site
- Given the transmural inflammation nature in Crohn's disease, some advanced conditions can present with bowel obstruction due to fibrotic stricture formation
- Extraintestinal manifestations and associations include (Inflamm Bowel Dis 2011;17:471, J Crohns Colitis 2016;10:239, J Crohns Colitis 2019;13:541):
- Joint and bones: arthropathies and osteoporosis
- Eye: iritis, uveitis and episcleritis
- Skin: erythema nodosum, pyoderma gangerosum, Sweet syndrome
- Liver: primary sclerosing cholangitis, cholelithiasis
- Kidney: nephrolithiasis
- Lung: asthma, bronchiectasis, chronic bronchitis, interstitial lung disease, bronchiolitis obliterans with organizing pneumonia, sarcoidosis, necrobiotic lung nodules and pulmonary infiltrates
Diagnosis
- Multimodality approach with clinicopathologic correlation and exclusion of other differential diagnoses
- Colonoscopy with ileoscopy, esophagogastroduodenoscopy (EGD) and endoscopic ultrasound are helpful in evaluating Crohn's disease as well as differentiating Crohn's disease from ulcerative colitis (Aliment Pharmacol Ther 2014;39:823)
- Endoscopy also plays a pivotal role in evaluating the severity of the disease and surveillance of neoplasms
- Characteristic endoscopic findings of Crohn's disease include (Med Clin North Am 1990;74:51, Gastrointest Endosc 1977;23:150, Gastrointest Endosc 1984;30:167):
- Aphthous ulcers
- Linear and serpiginous ulcers (giving a cobblestone appearance)
- Skip lesions
- Fistulas and strictures
- Isolated terminal ileum involvement, uninvolved rectum
Laboratory
- May be normal
- High white blood cells, anemia, elevated C reactive protein, electrolyte abnormalities, vitamin D deficiency and vitamin B12 deficiency may be found
- Elevated fecal calprotectin or lactoferrin (stool inflammatory markers), which can be used as a screening tool and determine the need for endoscopy (BMJ 2010;341:c3369)
Radiology description
- Not used as a primary diagnostic tool due to the wide availability of colonoscopy
- Magnetic resonance imaging (MRI), computed tomography (CT) and ultrasonography have shown good diagnostic accuracy by prospective meta analysis studies (Arch Dis Child 1996;74:22, Eur J Radiol 2006;58:140, Gut 2005;54:257)
Prognostic factors
- Disease course and severity may vary but is usually chronic and intermittent
- 50% of patients experience intestinal complications (strictures, fistula and abscess) 20 years after diagnosis (Intest Res 2015;13:19)
- Involvement of terminal ileum, ileocolonic and upper GI have higher risk of developing complications (Gastroenterology 2010;139:1147)
- Smoking, age < 40 years, perianal or rectal involvement and steroid requiring conditions are risk factors for disease progression (Gastroenterology 2006;130:650, Gut 2012;61:1140)
- Carcinoma may develop in longstanding disease with cumulative risk of 2.9% at 10 years, 5.6% at 20 years and 8.3% at 30 years after Crohn's disease diagnosis (World J Gastroenterol 2014;20:9872)
- 2 most important risk factors: duration and extent of disease
Case reports
- 24 year old woman with Crohn's terminal ileitis in remission and recurrent ileal invagination (Dtsch Arztebl Int 2020;117:146)
- 41 year old man with Crohn's disease and mesenteric artery thrombosis (Ann Vasc Surg 2019;58:382.e15)
- 62 year old man with duodenal Crohn's disease with associated ampullary stenosis (Dig Dis Sci 2005;50:1118)
- 77 year old man with unusual initial presentation of elderly onset Crohn's disease (Cureus 2020;12:e10173)
Treatment
- Multidisciplinary approach is recommended, including medications, surgery, nutritional, psychosocial support and cancer screening
- Assessing disease severity using Crohn's Disease Activity Index (CDAI) is helpful in guiding treatment approach (Gastroenterology 1979;77:829, J Pediatr Gastroenterol Nutr 1991;12:439, Gastroenterology 1999;116:527)
- Mild to moderately severe disease / low risk disease: sulfasalazine (colonic CD), budesonide (ileocecal CD) (Am J Gastroenterol 2018;113:481)
- Moderate to severe disease / moderate to high risk disease: corticosteroids, immunomodulators (e.g. azathioprine, 6-mercaptourin, methotrexate), anti-TNF agents (e.g. infliximab, adalimumab, certolizumab pegol), agents targeting leukocyte trafficking, agents targeting IL12 / 23 (anti-p40 antibody) (Am J Gastroenterol 2018;113:481)
- Severe / fulminant disease: intravenous corticosteroids, anti-TNF agents (Am J Gastroenterol 2018;113:481)
- Surgery is reserved for patients with limited disease, failure to response to treatment and complications of Crohn's disease (fistula, stricture, perforation) (Gastroenterology 1999;116:527, J Pediatr Surg 1997;32:1063, J Pediatr Gastroenterol Nutr 2015;60:347, Inflamm Bowel Dis 2013;19:7, Am J Gastroenterol 2018;113:481)
- Surveillance colonoscopy for dysplasia and colorectal carcinoma at 8 - 10 years after onset of symptoms with subsequent surveillance intervals of 1 - 2 years (Gastroenterol Hepatol (N Y) 2017;13:357)
Clinical images
Gross description
- Discontinuous pattern of inflammation (segmental disease, skip lesions)
- Cobblestone appearance (areas of nonulcerated mucosa separated by deep ulcers)
- Adhesions, creeping fat / fat wrapping, strictures and fistulas
- References: Histopathology 2012;60:1034, Virchows Arch 2014;464:511, Virchows Arch 2018;472:81
Gross images
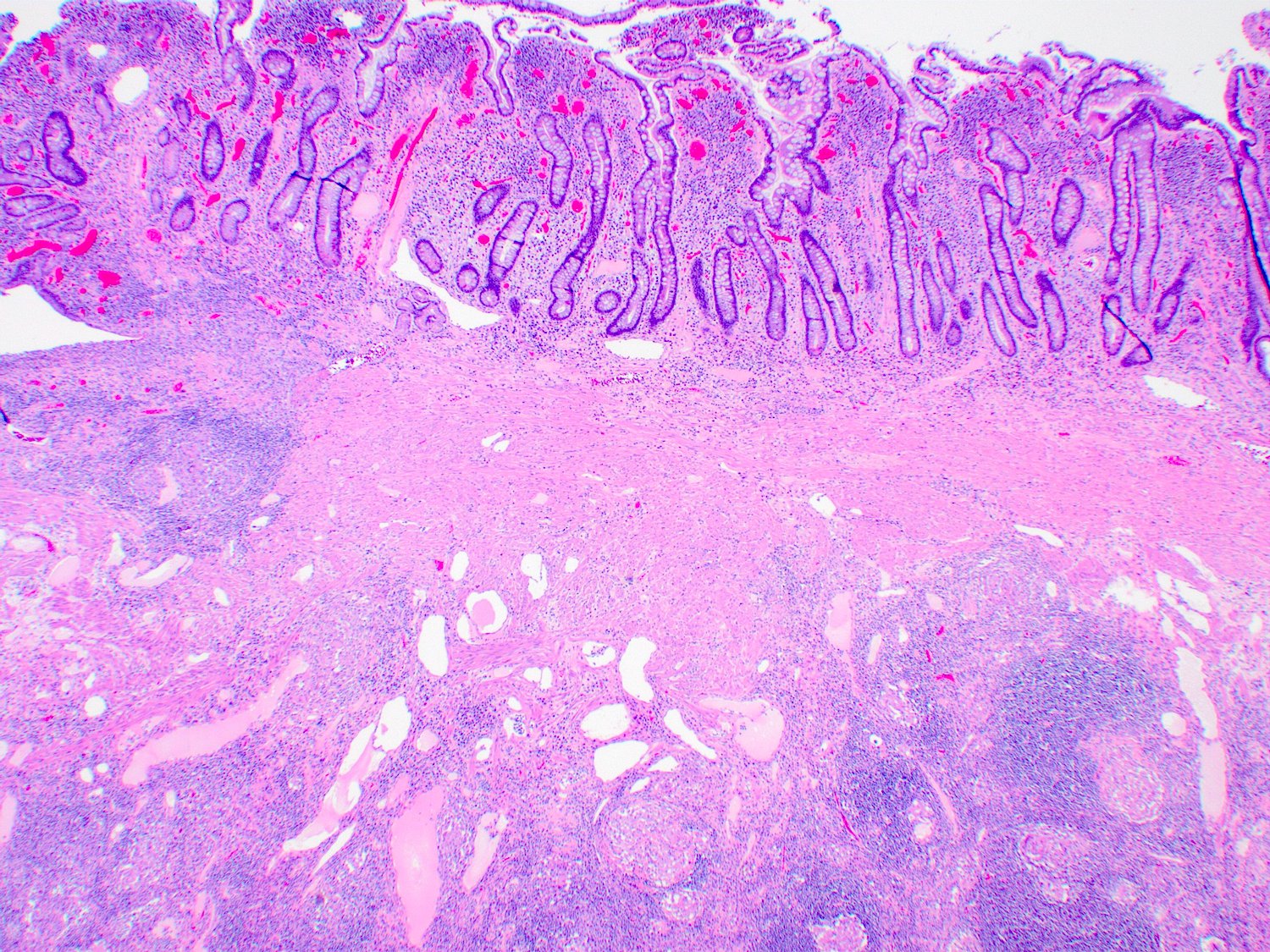
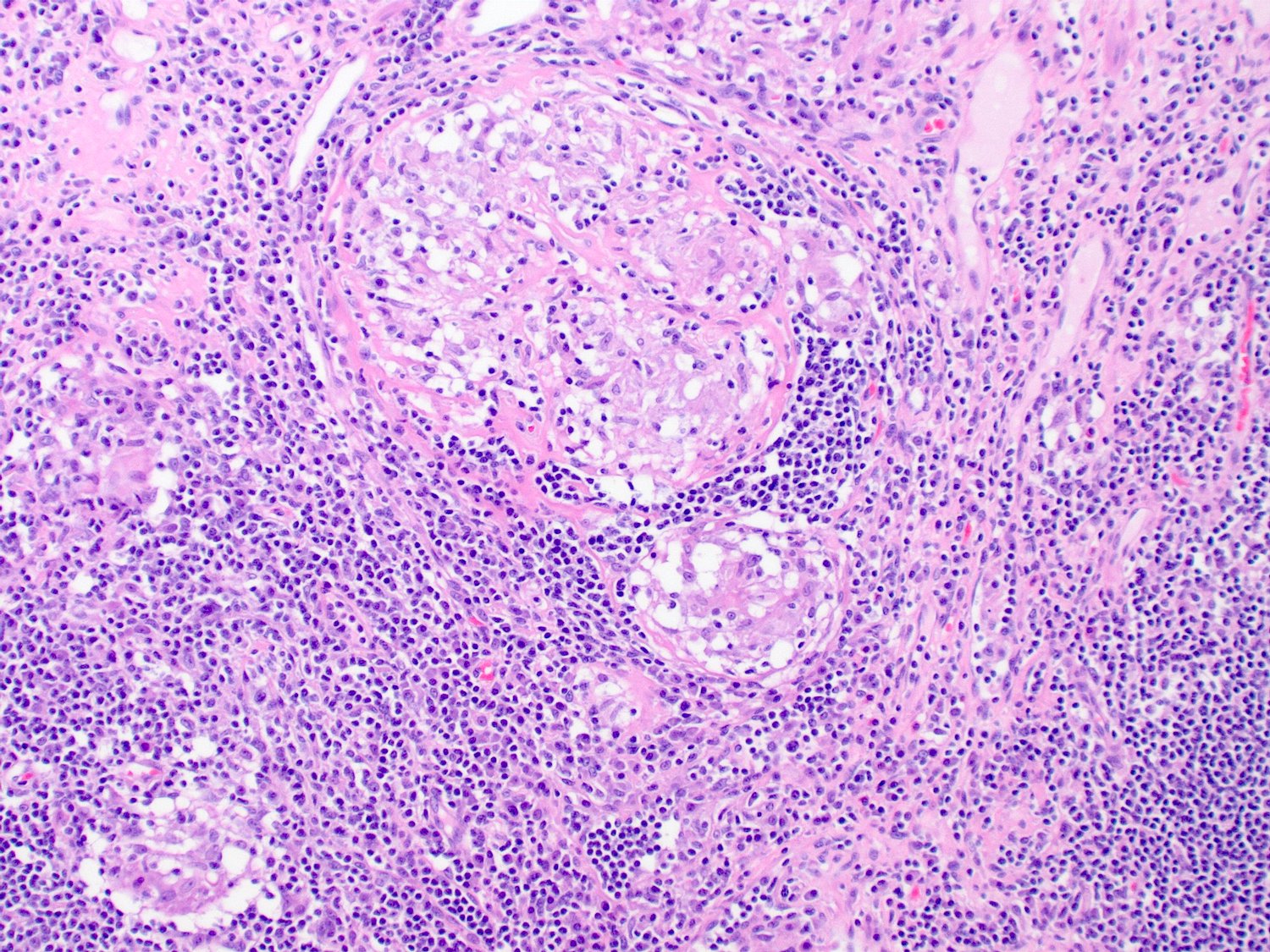
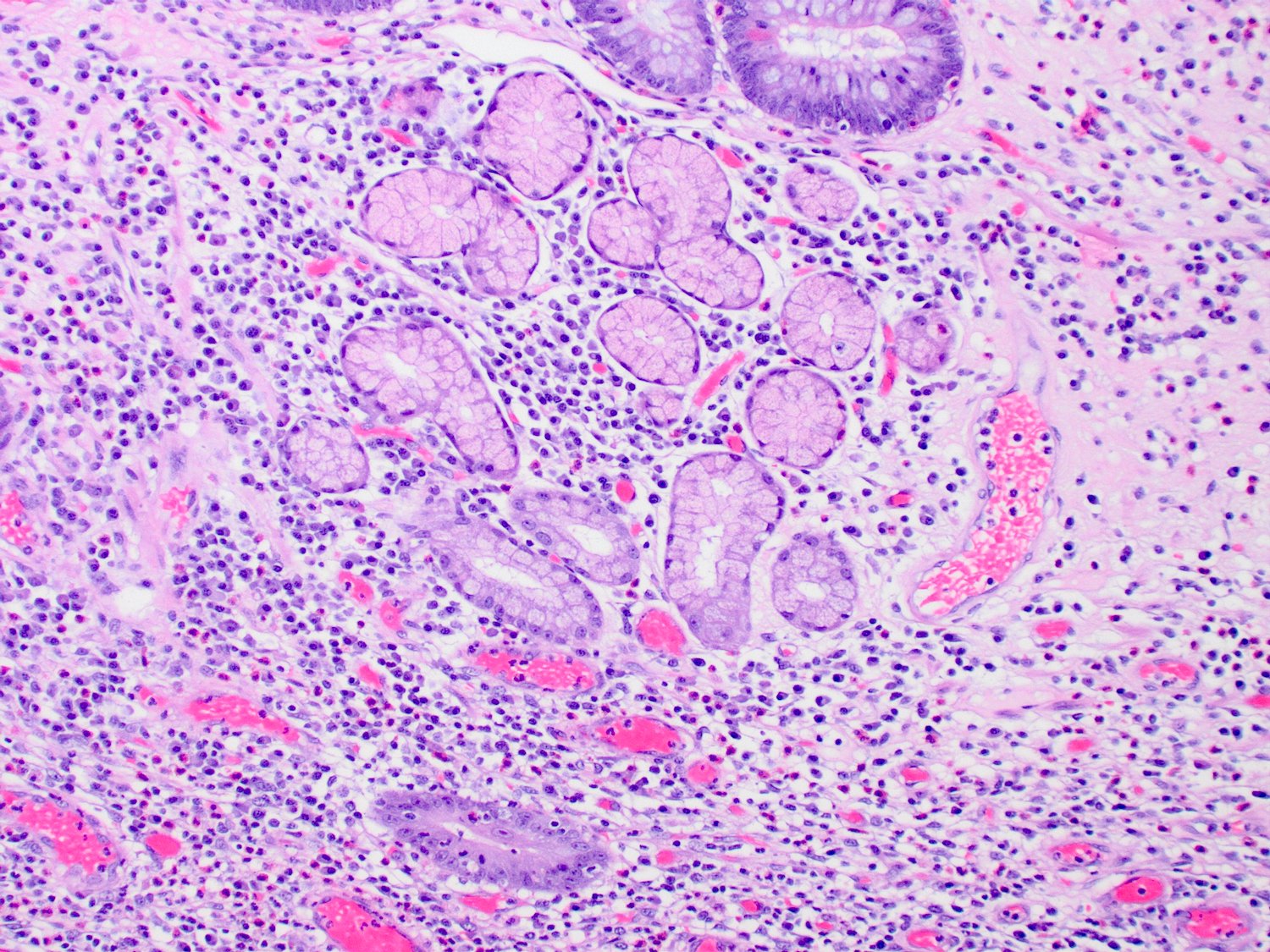
Microscopic (histologic) description
- Features of activity: active inflammation with cryptitis, crypt abscess and ulceration
- Features of chronicity: pyloric gland metaplasia, architectural distortion, crypt loss, crypt atrophy, basal lymphoplasmacytosis, fibrosis and stromal hypertrophy
- Skip lesions (portions of normal appearing small intestine with scattered areas of disease)
- Transmural lymphoid aggregates (beading or rosary pattern)
- Noncaseating granulomas (not related to crypt injury)
- Deep fissuring ulcers
- Aphthous ulcers (small ulcers occurring over lymphoid aggregates)
- Obliterative muscularization of submucosa (Arch Pathol Lab Med 2001;125:1331)
- Dysplasia (low or high grade) and carcinoma may be present in patients with longstanding disease
- Note: Some features of Crohn’s disease may also be seen in fulminant, untreated ulcerative colitis, such as aphthous ulcers, deep ulceration with transmural inflammation and superficial fissuring ulcers
- References: Circulation 1965;32:332, Histopathology 2012;60:1034, Virchows Arch 2014;464:511, Virchows Arch 2018;472:81, Mod Pathol 2015;28:S30
Microscopic (histologic) images
Molecular / cytogenetics description
- 71 susceptibility loci on 17 chromosomes (Nat Genet 2010;42:1118)
- Nucleotide binding oligodimerization domain 2 (NOD2) or caspase recruitment domain 15 (CARD15) on chromosome 16 (Nature 1996;379:821, Hum Mol Genet 1996;5:1679, Gastroenterology 2000;119:1483, Ann N Y Acad Sci 2006;1072:9)
- Autophagy related 16-like 1 (ATG16L1) and immunity related guanosine triphosphatase family member M (IRGM) gene on chromosome 5 (Nat Genet 2007;39:596, Gut 2008;57:717)
- Genetic polymorphisms in tumor necrosis factor receptors (TNFRSF1A / 1B) with differential treatment response to TNFα inhibitors (BMJ Open Gastroenterol 2019;6:e000246)
Sample pathology report
- Terminal ileum and cecum, ileocecectomy:
- Segment of terminal ileum with features consistent with history of Crohn's disease, including:
- Moderately to markedly active chronic ileitis with patchy ulcerations
- Fibromuscular stricture with decreased luminal circumference
- Scattered noncaseating granulomas
- No dysplasia identified
- Immunostain for CMV is negative
- Segment of terminal ileum with features consistent with history of Crohn's disease, including:
Differential diagnosis
- Ulcerative colitis:
- Small bowel typically not involved except in case of backwash ileitis
- Absence of granulomas and segmental disease (these features are more specific for CD)
- Typically superficial inflammation with lack of transmural lymphoid aggregates
- Deep or serosal based lymphoid aggregates may be seen adjacent to ulceration in both UC and CD
- Absence of deep fissuring ulceration
- Superficial fissures may be seen in fulminant disease
- Infectious enteritis:
- May show overlapping features of inflammatory bowel disease
- Correlation with microbiologic studies is necessary for exclusion
- Drug associated enteritis (e.g. NSAIDs):
- Patchy active inflammation
- Tends to lack significant features of chronicity
- Behçet disease:
- Form of vasculitis
- Recurrent aphthous stomatitis and genital ulcers may be present
- Ischemia:
- Withering crypts and hyalinization of lamina propria
- References: Ann Gastroenterol 2011;24:271, Curr Gastroenterol Rep 2010;12:249
Additional references
Board review style question #1
A 30 year old woman presents with abdominal pain and bloody diarrhea. The patient is refractory to medical management and a resection of the small intestine is performed. What diagnosis is most consistent with the histological findings?
- Backwash ileitis
- Crohn’s disease
- Drug associated enteritis
- Infections enteritis
Board review style answer #1
Board review style question #2
In fulminant disease, sometimes it is difficult to differentiate between Crohn's disease and ulcerative colitis. Which one of the following features can be seen in both fulminant, untreated Crohn's disease and ulcerative colitis?
- Deep fissuring ulceration
- Deep or serosal based lymphoid aggregates adjacent to ulceration
- Granulomas
- Segmental disease
Board review style answer #2
B. Deep or serosal based lymphoid aggregates adjacent to ulceration
Comment Here
Reference: Crohn's disease
Comment Here
Reference: Crohn's disease