Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Electron microscopy description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shenoy A, Russo PA. Autoimmune enteropathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelautoimmuneenter.html. Accessed April 3rd, 2025.
Definition / general
- Immune mediated disorder causing small intestinal atrophy and resulting in severe diarrhea
Essential features
- Intractable diarrhea leading to malabsorption and electrolyte imbalances
- Histologic findings include intestinal atrophy with variable inflammation (acute and chronic), crypt apoptosis and absence of goblet / Paneth cells
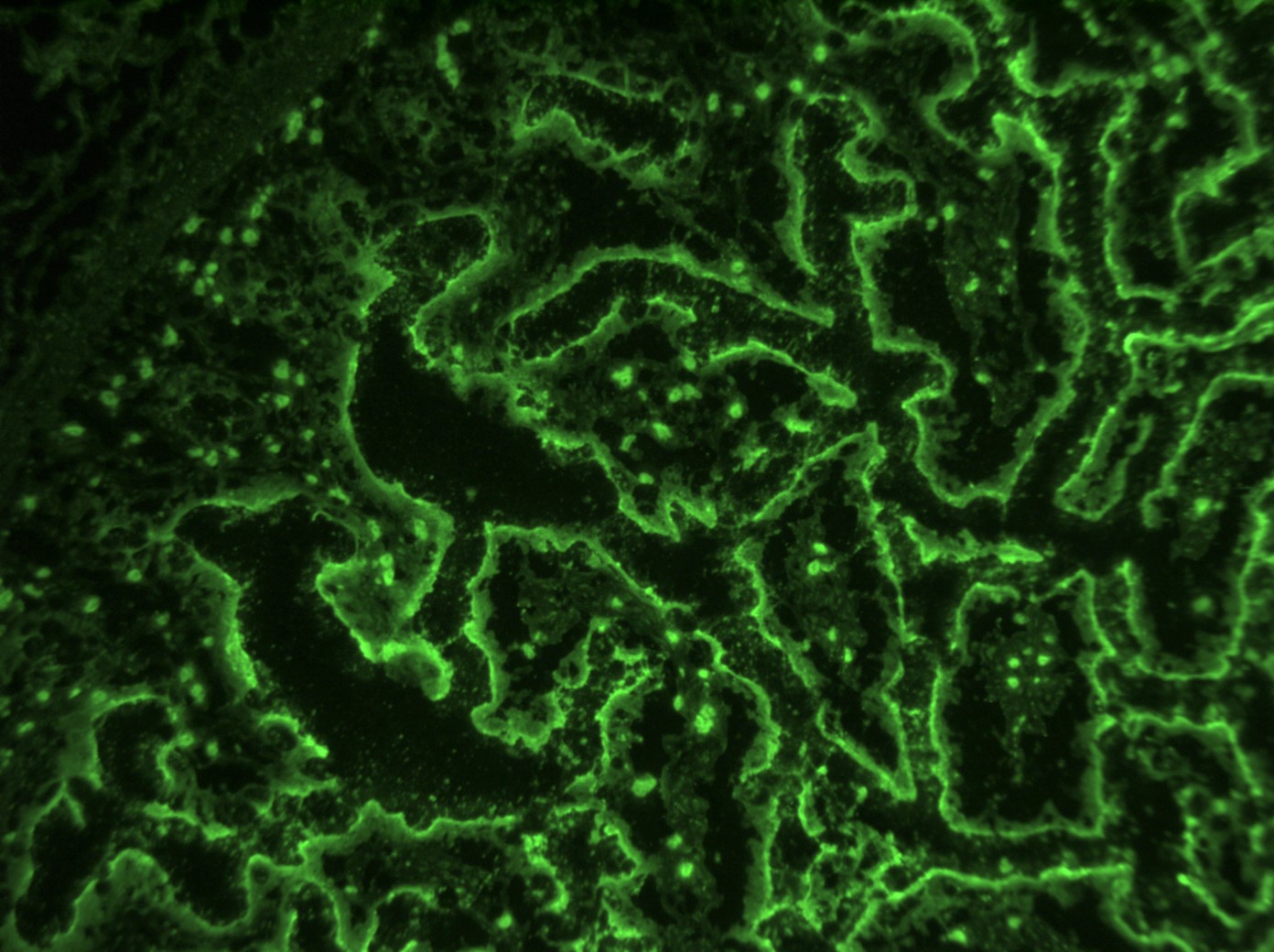
- Indirect immunofluorescence on normal intestinal tissue using patient’s serum is useful in detecting circulating anti-enterocyte and antigoblet cell antibodies
- Extraintestinal autoimmune manifestations are possible
- Prognosis is much improved with immunomodulatory therapy
Terminology
- Autoimmune enteropathy
- Syndromic forms: immune dysregulation, polyendocrinopathy, enteropathy and X linked (IPEX) syndrome; autoimmune polyglandular syndrome (APS 1) also known as autoimmune phenomena, polyendocrinopathy, candidiasis and ectodermal dystrophy (APECED) syndrome
ICD coding
Epidemiology
- Age at diagnosis: variable, predominantly infants and young children, median age at presentation ~6 months; adult presentation documented (Mod Pathol 2014;27:543, Dig Dis Sci 2019;64:643)
- < 1/100,000 children (Scand J Gastroenterol 2008;43:1102)
- M > F
Sites
Pathophysiology
- Exact pathogenesis is unclear
- Intestinal epithelial damage from anti-enterocyte antibodies and antigoblet cell antibodies
Etiology
- Complex, multifactorial
- IPEX syndrome: FOXP3 mutation leading to impaired function / number of regulatory T cells, X linked
- APECED syndrome: AIRE mutation resulting in lack of suppression of autoreactive T cells, autosomal recessive
- IPEX-like syndrome: mutations in genes related to regulatory T cell functions such as CD25, STAT5b, STAT1, LRBA and CTLA4 (Front Immunol 2018;9:2411)
Clinical features
- Severe intractable diarrhea, unresponsive to dietary modifications (Dig Dis Sci 2020 Aug 24 [Epub ahead of print])
- Failure to thrive, weight loss, growth restriction
- IPEX and APECED: endocrinopathies and cutaneous manifestations (see Sites)
Diagnosis
- Combination of clinical presentation, histologic findings and laboratory studies
Laboratory
- Anti-enterocyte and antigoblet cell antibodies demonstrable by indirect immunofluorescence; predominantly IgG, less commonly IgM and IgA
- Sequencing for known mutations
Prognostic factors
- Can be fatal if untreated; advances in treatment and aggressive nutritional care have improved outcomes
Case reports
- 13 year old girl with autoimmune enteropathy successfully treated with infliximab (J Clin Gastroenterol 2014;48:264)
- 18 year old Caucasian man with APECED (BMJ Case Rep 2013;2013:bcr2012008116)
- 55 year old man with autoimmune enteropathy and bowel transplantation (Transplant Proc 2020;S0041:32669)
Treatment
- Supportive nutrition, enteral and parenteral
- Immunosuppression (steroids, immunomodulatory chemotherapeutic agents, biologic medications)
- Stem cell transplant (IPEX syndrome) (Dig Dis Sci 2019;64:643)
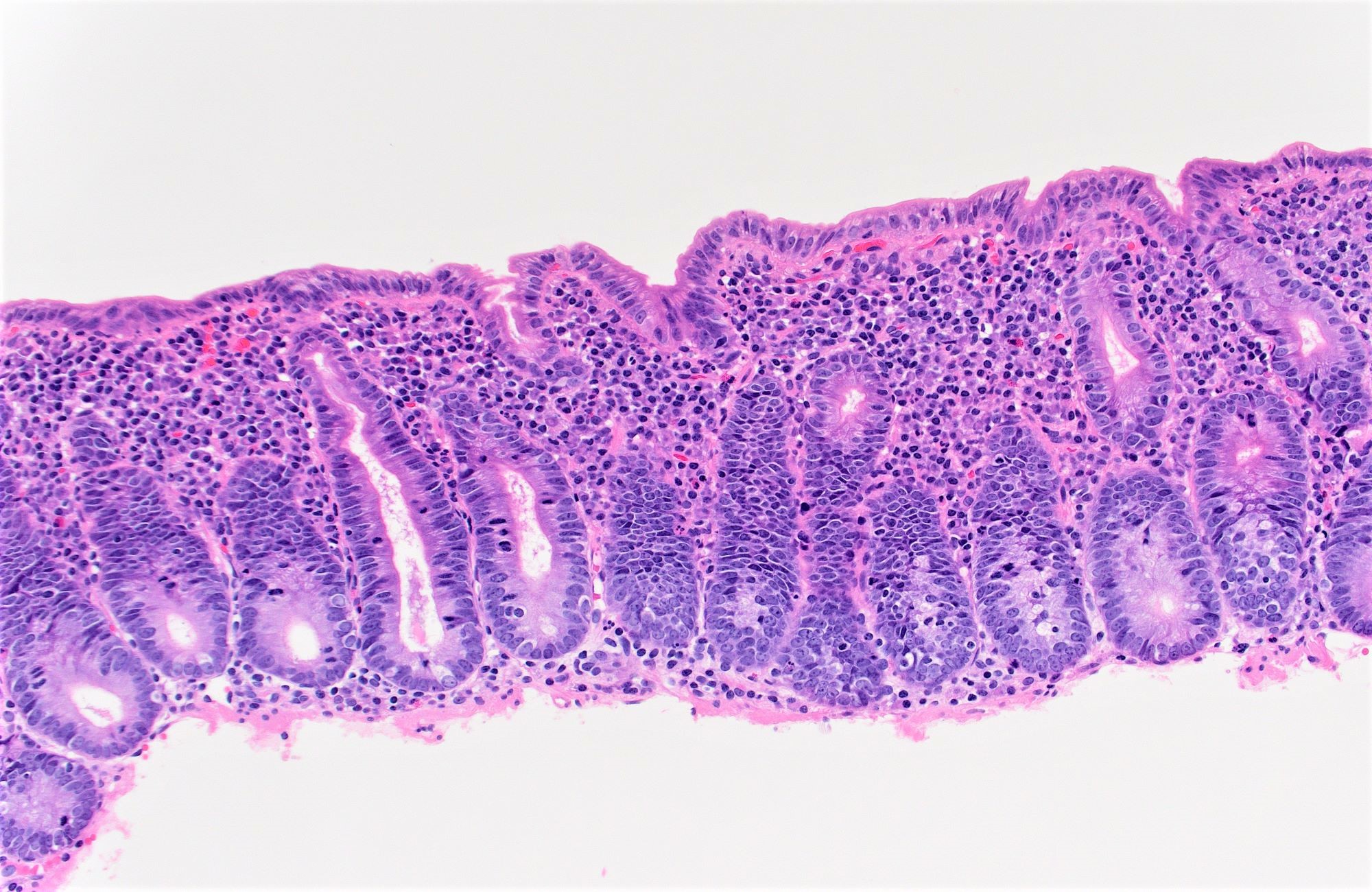
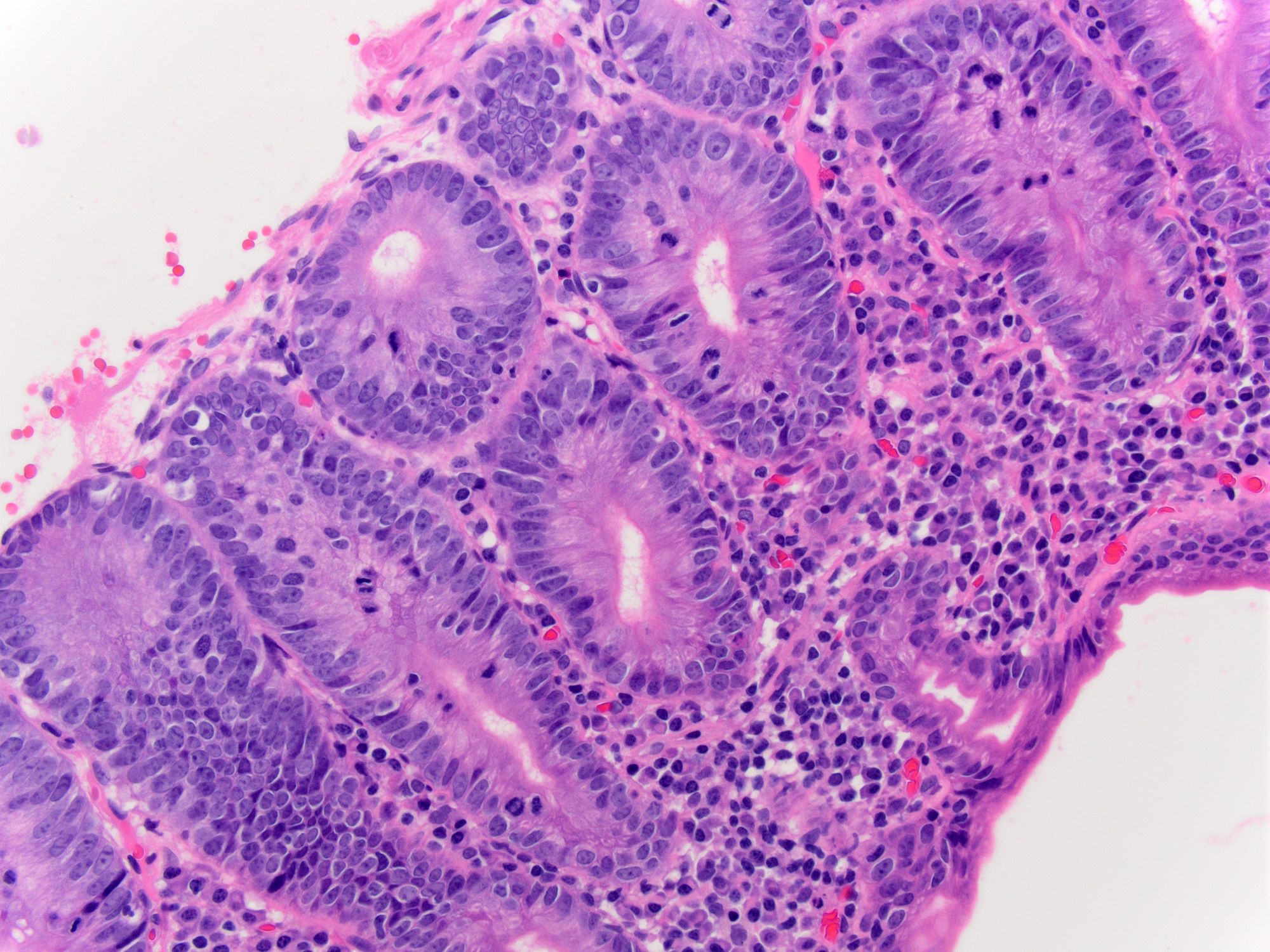
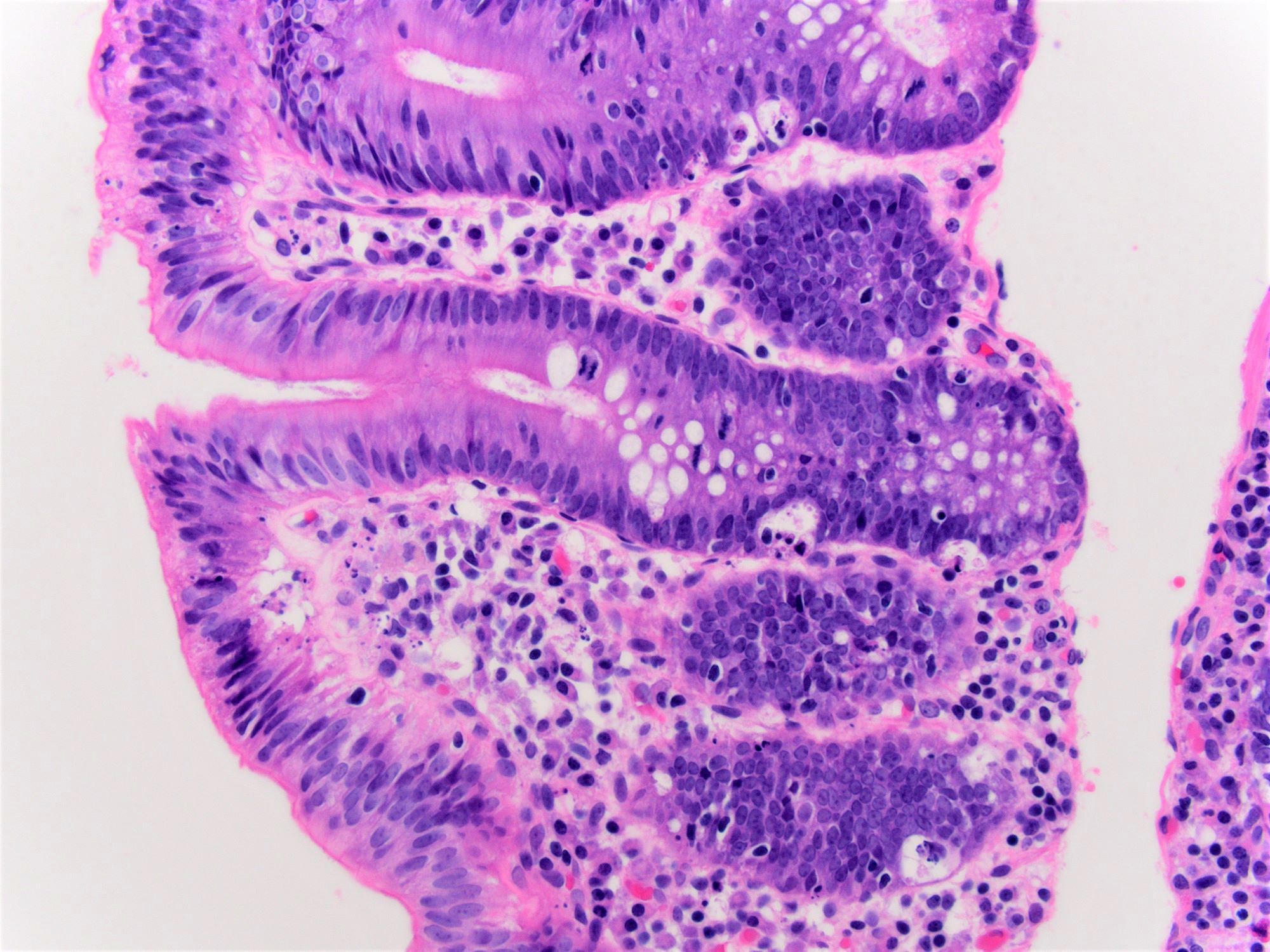
Microscopic (histologic) description
- Villous architectural abnormalities
- Villous blunting, severe villous atrophy and crypt hyperplasia
- Absence of an epithelial cell subtype
- Diminished / absent goblet cells and Paneth cells
- Observed in a subset of cases; not a requisite for diagnosis (Am J Surg Pathol 2014;38:1319, Mod Pathol 2014;27:543)
- Inflammation:
- Increased intraepithelial lymphocytes
- Active (acute) inflammation and cryptitis
- Increased crypt apoptosis resembling graft versus host disease
- Findings pronounced in duodenum / small bowel; variable findings can also be seen in the stomach and colon (Am J Surg Pathol 2014;38:1319)
- Severity of histologic findings variable among individuals and reversible with therapy
Immunofluorescence description
- Indirect immunofluorescence test performed using patient’s serum on normal frozen small intestinal tissue can assist in diagnosis; positive staining of apical and basolateral borders of enterocytes or goblet cell staining indicates the presence of anti-enterocyte and antigoblet cell antibodies (Pediatr Dev Pathol 1999;2:65)
Electron microscopy description
- Not routinely used for diagnosis; if performed, helpful in eliminating congenital diarrheas that are in the differential diagnoses
Sample pathology report
- Duodenum, biopsy:
- Severe villous blunting with absence of goblet cells and Paneth cells, intraepithelial lymphocytosis and increased crypt apoptosis
- Duodenum, biopsy:
- Chronic active duodenitis with increased apoptosis (see comment)
- Comment: The biopsies demonstrate histologic features that raise the possibility of autoimmune enteropathy, in the correct clinical context. If celiac disease is excluded, serologic or molecular testing for autoimmune enteropathy is recommended.
Differential diagnosis
- Celiac disease:
- Intact goblet and Paneth cells
- Typically more pronounced intraepithelial lymphocytes
- Typically responsive to gluten free diet
- Positive serologic tests (antiendomysial antibodies and tissue transglutaminase) for celiac disease
- Very early onset inflammatory bowel disease:
- Intact goblet and Paneth cells
- Granulomas (in Crohn’s disease)
- Infections:
- Stool polymerase chain reaction tests, cultures
- Acute onset of symptoms responsive to antibiotic medications
- Common variable immunodeficiency:
- Paucity of lamina propria plasma cells
- Congenital diarrheas:
- Tufting enteropathy:
- Epithelial tufts, EpCAM mutations, negative EpCAM immunohistochemical stain
- Microvillus inclusion disease:
- Enteroendocrine cell dysgenesis:
- Negative chromogranin, NEUROG 3 mutations
- Tufting enteropathy:
- Graft versus host disease
- History of stem cell transplant
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Mutation in which of the following genes is associated with IPEX syndrome?
- FOXO1
- FOXP3
- SS18
- TFE3
Board review style answer #2