Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Liang T, Chopra S. GIST. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelGIST.html. Accessed December 20th, 2024.
Definition / general
- Most common mesenchymal tumor of the gastrointestinal (GI) tract
- Derived from interstitial cells of Cajal
Essential features
- Small bowel is second most common site of GISTs (stomach is first)
- NF1 and BRAF mutated GISTs are more common in small bowel versus other sites
- Prognosis depends on size, mitotic rate and location
Terminology
- Gastrointestinal stromal tumor (GIST)
ICD coding
- ICD-10: C49.A3 - gastrointestinal stromal tumor of small intestine
- ICD-11: 2B5B&XH9HQ1 - gastrointestinal stromal tumor
- ICD-O: 8936/3 - gastrointestinal stromal tumor, malignant
Epidemiology
- M:F = 1
- Median age is 60 - 65 years; rare in children and young adults
- May present in younger patients in neurofibromatosis type 1 (NF1) lesions (mean age 49 years), Carney triad (childhood), familial (middle age)
- Annual incidence of GIST is between 11 and 14.5 cases per million (Int J Cancer 2005;117:289, Cancer 2005;103:821)
- GISTs account for 1 - 3% of all GI neoplasms
Sites
- Occurs anywhere in tubular GI tract
- Small bowel is second most common site
- Stomach (60%) > jejunum and ileum (30%) > duodenum (4 - 5%) > rectum (4%) > colon and appendix (1 - 2%) > esophagus (< 1%) (Semin Diagn Pathol 2006;23:70)
- Extraintestinal GISTs occur in mesentery, omentum, retroperitoneum (Am J Surg Pathol 2005;29:52, Mod Pathol 2000;13:577)
- May represent a metastasis from an unrecognized primary or a detached mass from the GI tract
Pathophysiology
- Sporadic - vast majority
- Somatic mutations in KIT (70 - 85%), PDGFRA (5 - 10%, mutually exclusive with KIT mutations), NF1 and BRAF (Science 2003;299:708, Cancer Res 2001;61:8118)
- Sporadic tumor syndrome (nonhereditary)
- Carney triad (GIST, paraganglioma, pulmonary chondroma)
- SDH deficient but lacking SDH germline mutations
- Carney triad (GIST, paraganglioma, pulmonary chondroma)
- Autosomal dominant hereditary syndromes (5 - 10% of all GISTs)
- Neurofibromatosis type 1 (NF1) - commonly small bowel and often multifocal
- Germline KIT mutations
- Germline PDGFRA mutations
- Carney-Stratakis syndrome
- Germline mutations in SDHB, SDHC or SDHD subunit (Arch Pathol Lab Med 2020;144:655)
Etiology
- Unknown, most cases are sporadic
- Small subset of cases can be familial (see Pathophysiology)
Clinical features
- Vague abdominal pain
- Symptoms related to mucosal ulceration, including bleeding (47%) (Ther Clin Risk Manag 2018;14:1467)
- Abdominal mass
- Smaller GISTs are discovered incidentally
- NF1 associated GISTs (Am J Surg Pathol 2006;30:90)
- Patients are more likely to develop multiple independent GISTs
- NF1 tumors have a strong predilection to arise in small bowel
- While NF1 associated GISTs have been estimated to account for only about 1 - 2% of tumors from all anatomic sites, they make up ~4 - 6% of small intestinal GISTs
Diagnosis
- Double balloon enteroscopy (89%), CT angiography (71%) and CT (55%) are best imaging modalities (Ther Clin Risk Manag 2018;14:1467)
- Endoscopy with biopsy or fine needle aspiration
Radiology description
- Radiologic findings are variable, depending on size and time of presentation
- CT usually shows a solid, heterogeneous mass (reflecting the presence of hemorrhage or cystic degeneration)
- Endoscopic ultrasound reveals a hypoechoic solid mass
- References: Front Oncol 2021;11:582847, Front Oncol 2021;11:631927
Radiology images
Prognostic factors
- Prognosis depends on site, size, mitotic activity, molecular profile (Semin Diagn Pathol 2006;23:70)
- Small bowel GISTs are more likely to be malignant (35 - 40%) compared with gastric GISTs (25%) (Am J Surg Pathol 2006;30:477, Am J Surg Pathol 2005;29:52)
- NF1 mutated GISTs are usually grossly small and mitotically inactive, much like spontaneous low grade GISTs of the small intestine
- Their histologically benign appearance is reflected in their commonly nonaggressive clinical behavior
- NF1 associated tumors that do manifest as clinically malignant disease are generally bigger (> 5 cm in greatest dimension) and more proliferative (> 5 mitoses/5 mm2), adhering to the risk stratification provided by standard staging criteria
Case reports
- 58 year old woman with small bowel GIST presenting as intussusception (GE Port J Gastroenterol 2016;23:279)
- 68 year old woman with small bowel GIST with diffuse omental and mesenteric implants (J Surg Case Rep 2020;2020:rjaa341)
- 74 year old man with small bowel GIST presenting as strangulated inguinal hernia (BMJ Case Rep 2017;2017:bcr2016217273)
- 75 year old woman with NF1 jejunal GIST ( J Surg Case Rep 2018;2018:rjy017)
Treatment
- Most GISTs are treated with surgical resection
- Imatinib mesylate (Gleevec): tyrosine kinase inhibitor of KIT and PDGFRα
- Metastatic / recurrent / high risk GIST
- Sunitinib malate (Sutent): a tyrosine kinase inhibitor of KIT, PDGFRα, VEGFR
- Used in imatinib resistant GIST
- NF1 mutated GISTs - surgery is treatment of choice as these tumors do not respond to imatinib
- BRAF mutated GISTs do not respond to imatinib and BRAF inhibitors are used for therapy if indicated
- References: Am J Surg Pathol 2015;39:922, Surg Clin North Am 2017;97:437
Gross description
- Well circumscribed masses of various sizes
- Cut surface may show hemorrhage, cystic change or necrosis
- Usually centered in the muscularis propria
- Small bowel GISTs more frequently present as external masses
- Reference: Am J Surg Pathol 2009;33:1267
Frozen section description
- Spindle cell neoplasm
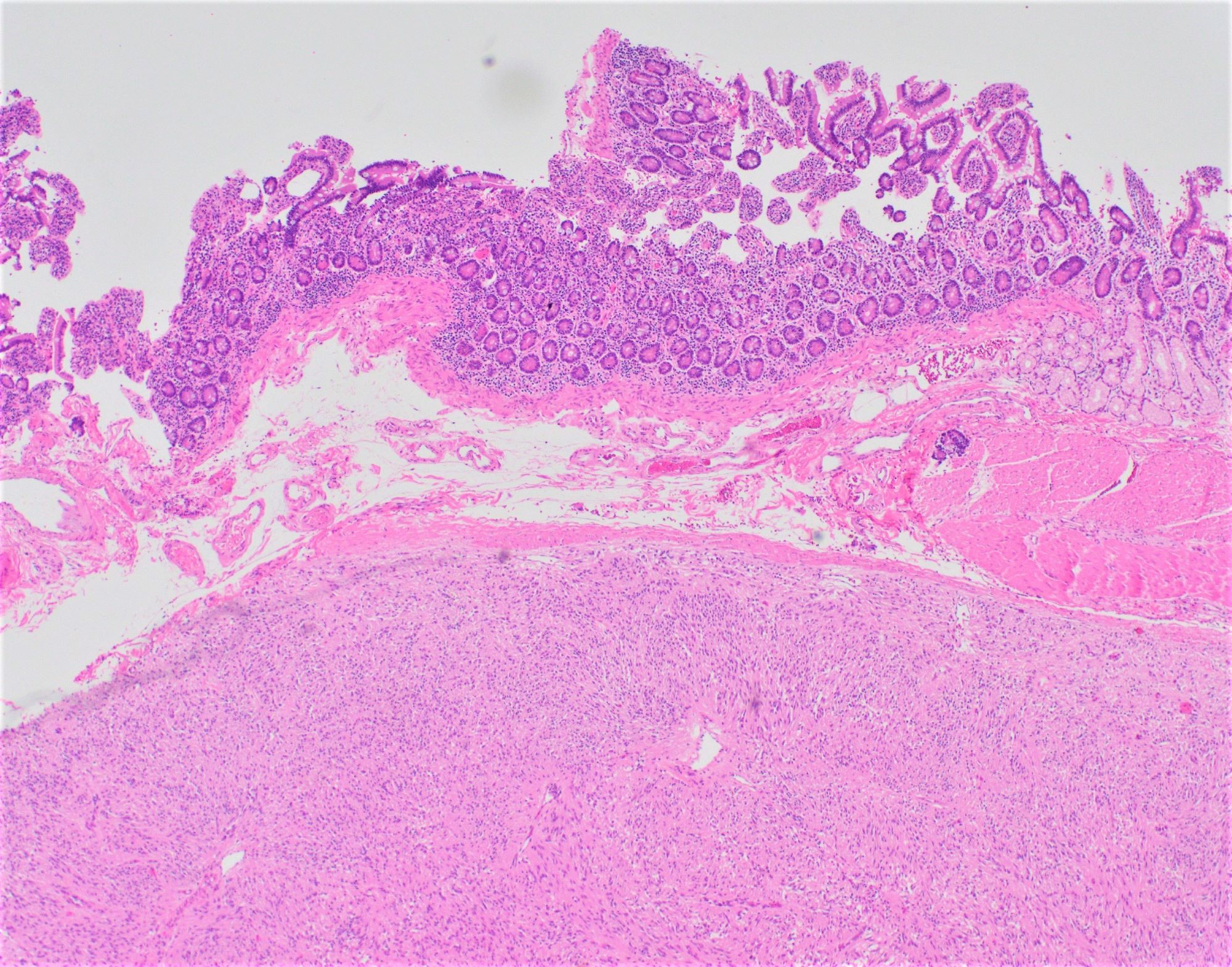
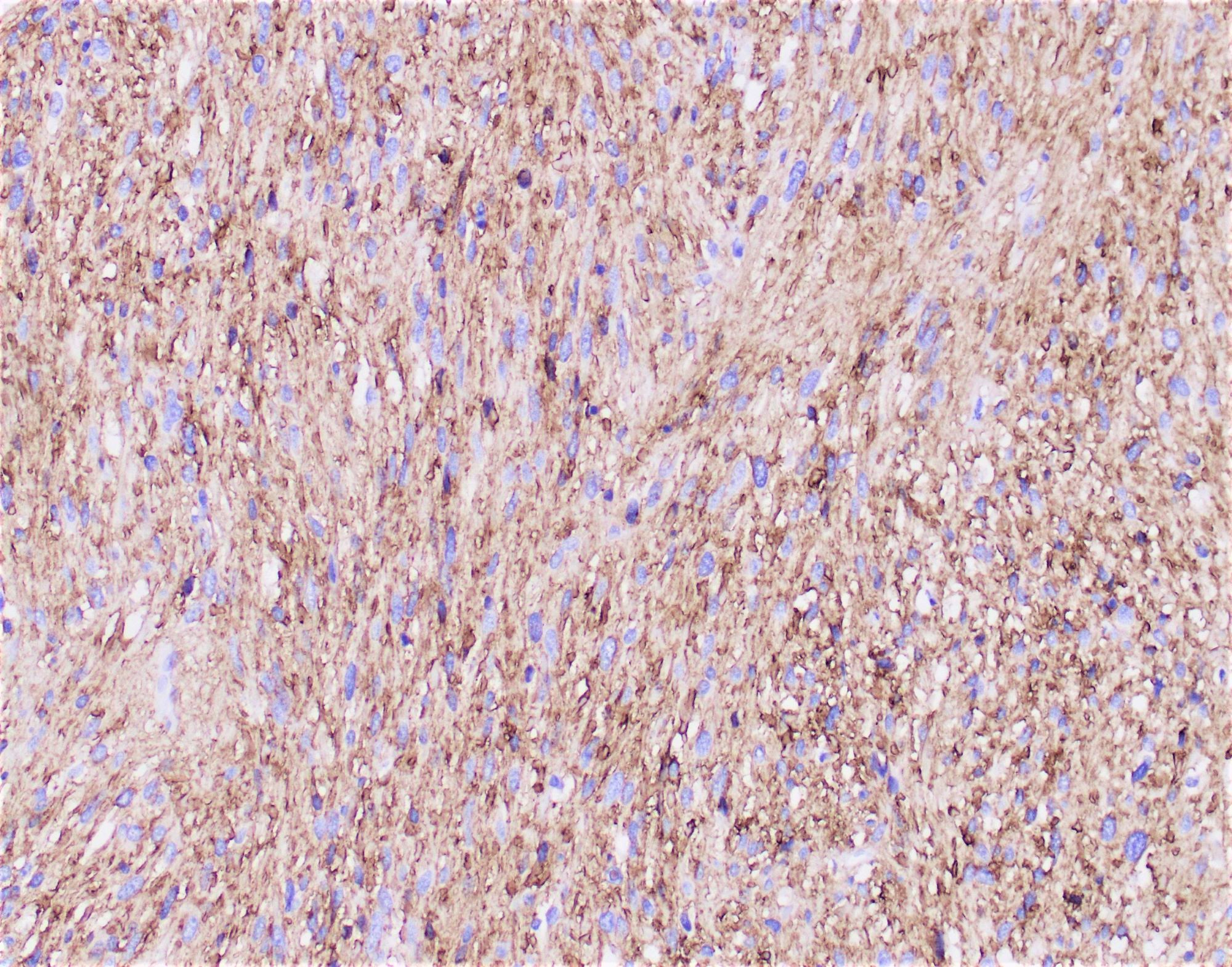
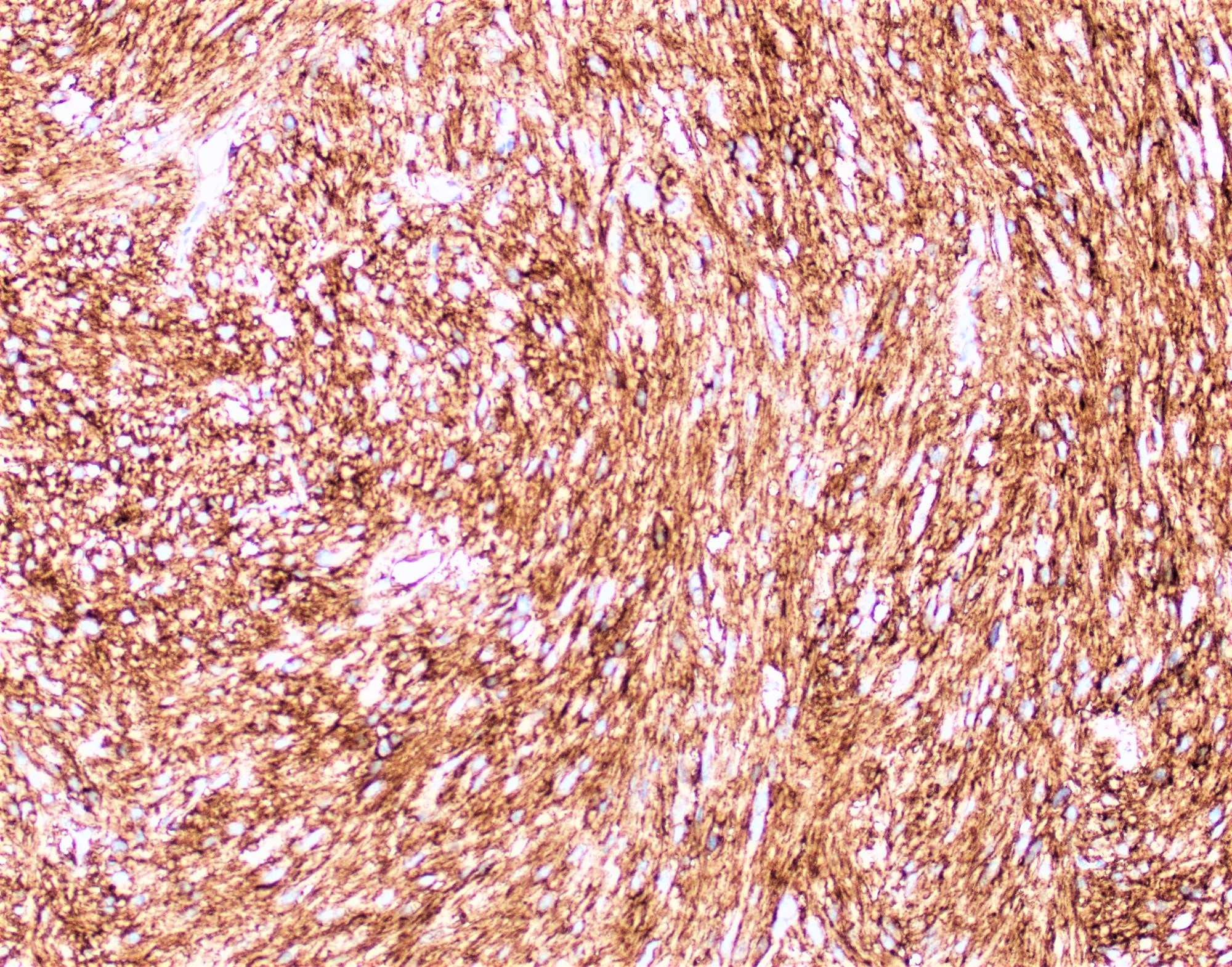
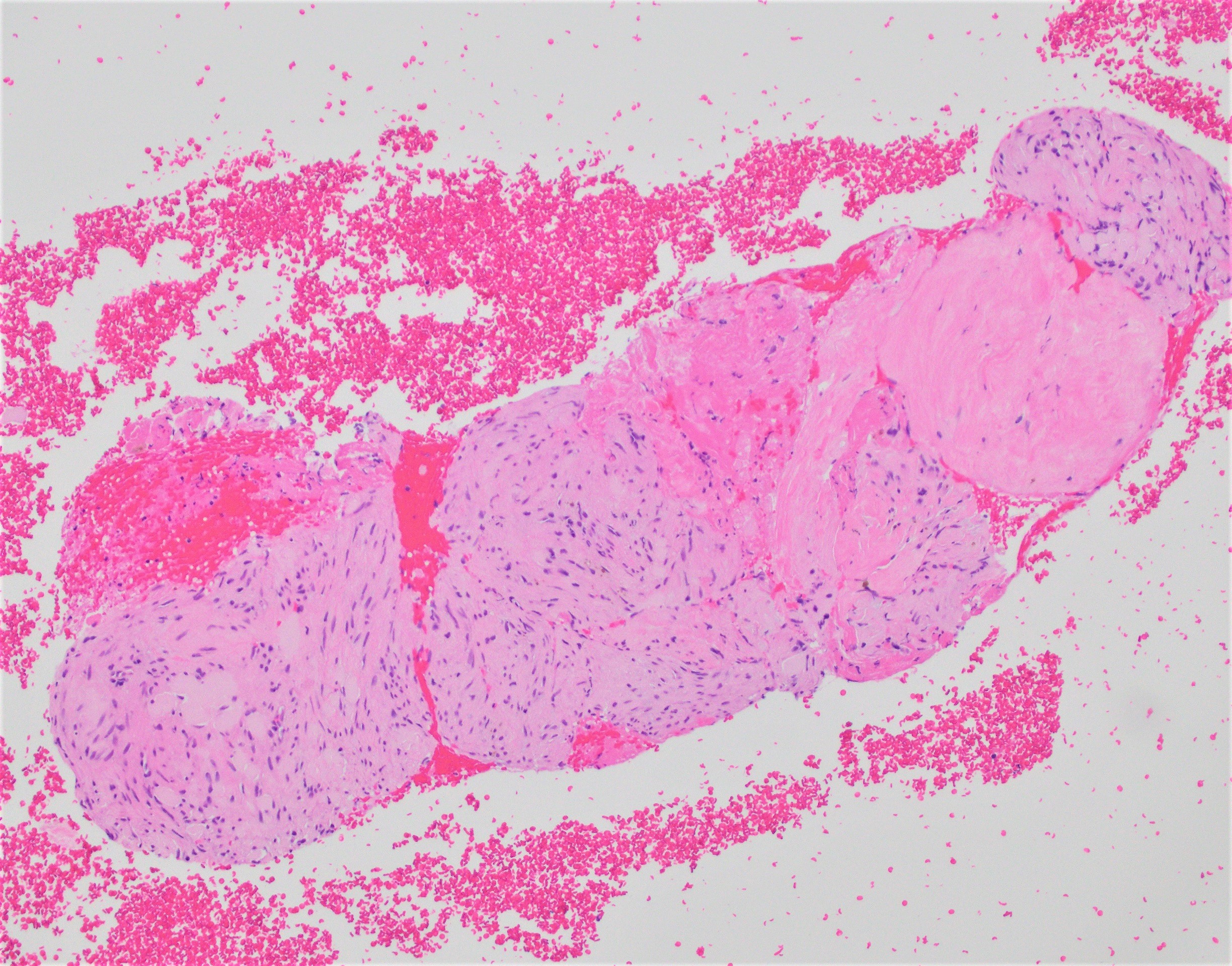
Microscopic (histologic) description
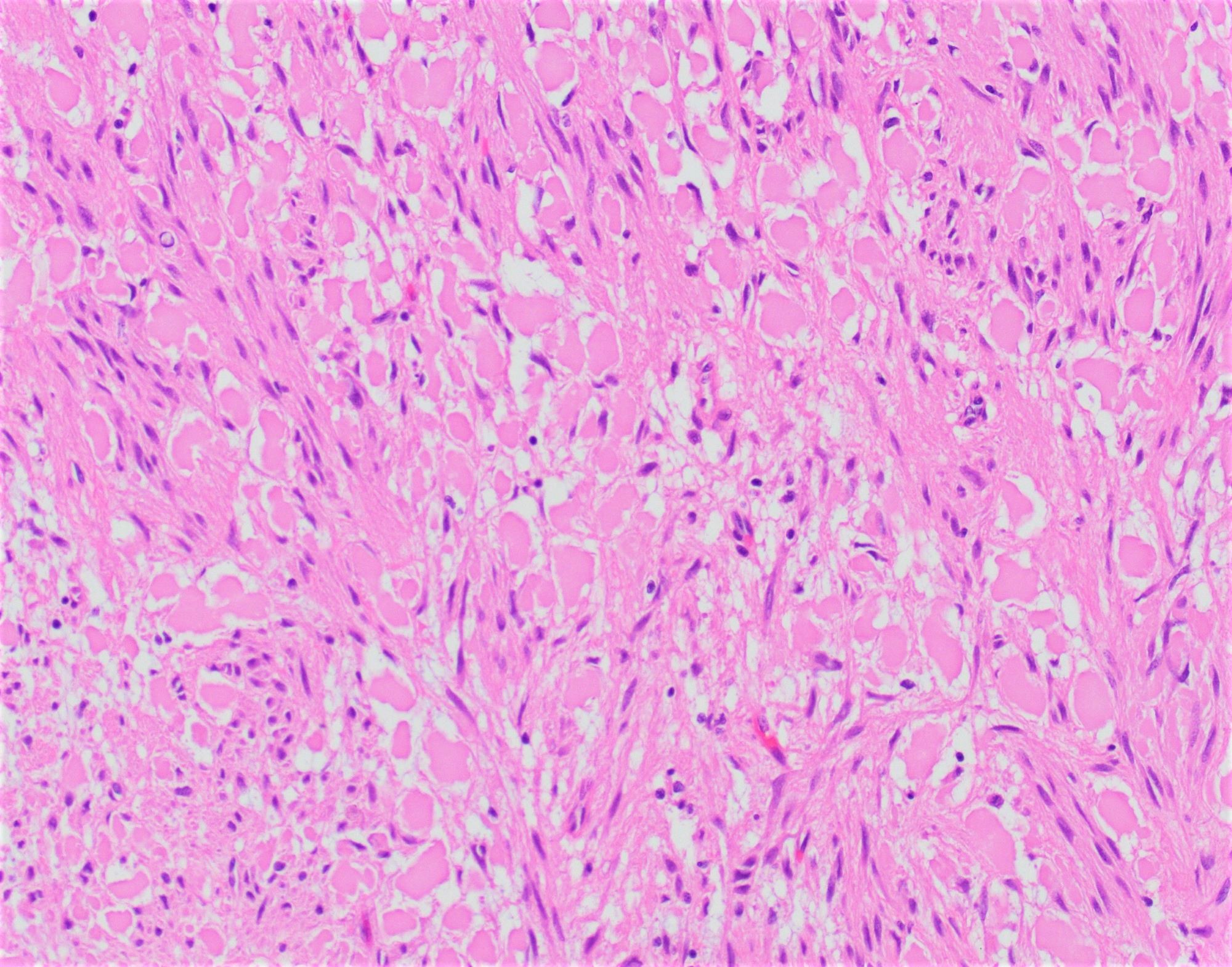
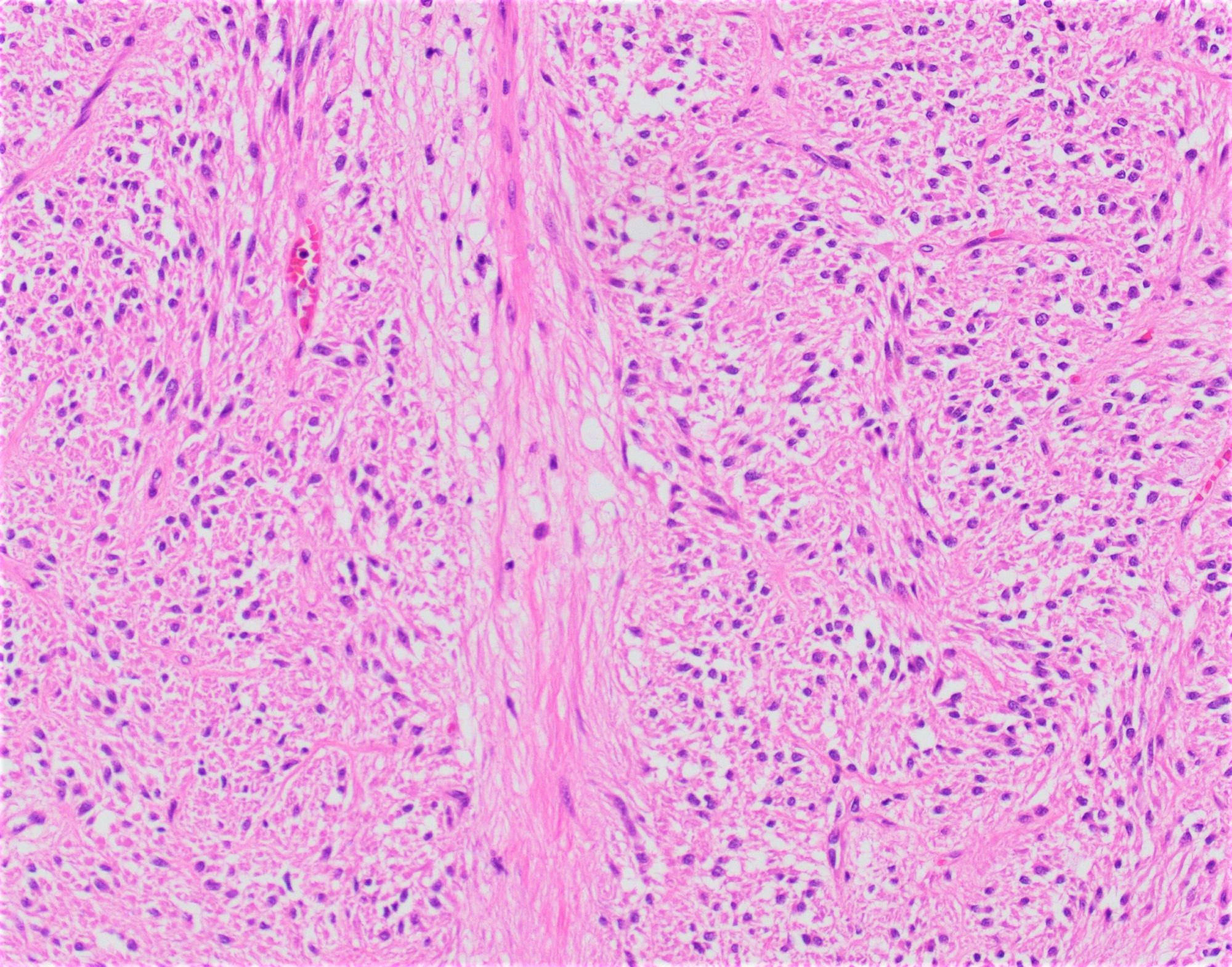
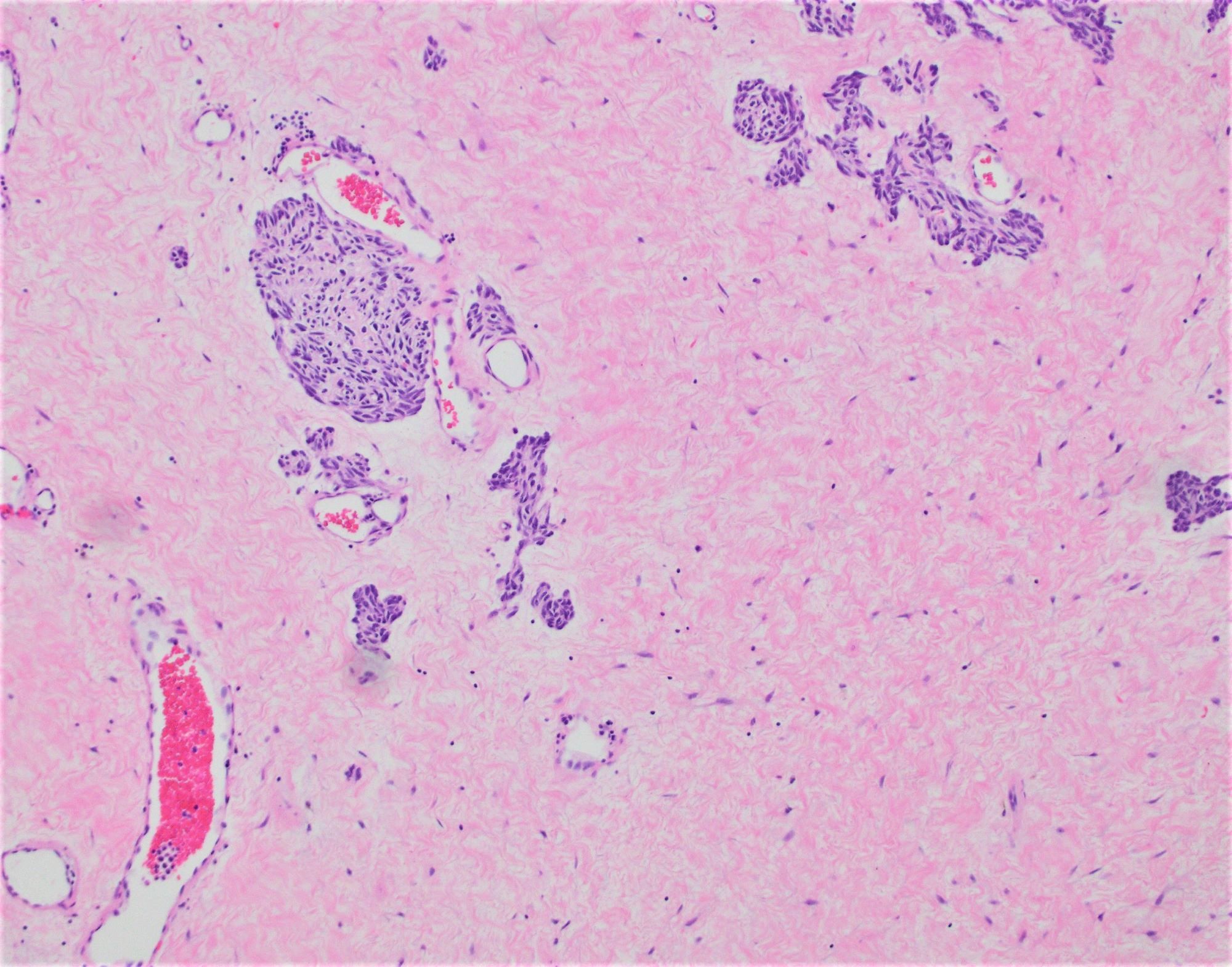
- 3 morphologic types: spindle (70%), epithelioid (20%), mixed (10%)
- Monotonous, bland cells with spindled or epithelioid cytoarchitecture, lightly eosinophilic to pale cytoplasm and vesicular chromatin residing within uniformly ovoid or round nuclei
- In spindle cell GISTs, the pink cytoplasm often has a fibrillary texture with indistinct cell borders
- Can show a degree of nuclear palisading reminiscent of schwannoma
- Small intestinal GISTs are most often spindled
- Epithelioid morphology in small intestinal GIST portends malignant behavior, in contrast to the stomach, where epithelioid morphology is not a significant prognostic feature
- Small intestine GISTs more commonly feature skeinoid fibers, stromal PAS positive globules of curved collagen fibrils, which, when present in a small intestinal tumor, correlate with less malignant clinical behavior
- Treated tumors can display a widely variable histomorphology that may significantly differ from treatment naive tumors
- Tumor may be necrotic or hypocellular; the stromal component, which may be hyalinized or calcified, becomes prominent
- Cytomorphology of the tumor cells can change, usually adopting a more epithelioid and even anaplastic or sarcomatoid appearance
- Histologic grade
- G1: low grade, mitoses < 5/5 mm2
- G2: High grade, mitoses > 5/5 mm2
- References: Am J Surg Pathol 2017;41:577, Arch Pathol Lab Med 2020;144:655
Microscopic (histologic) images
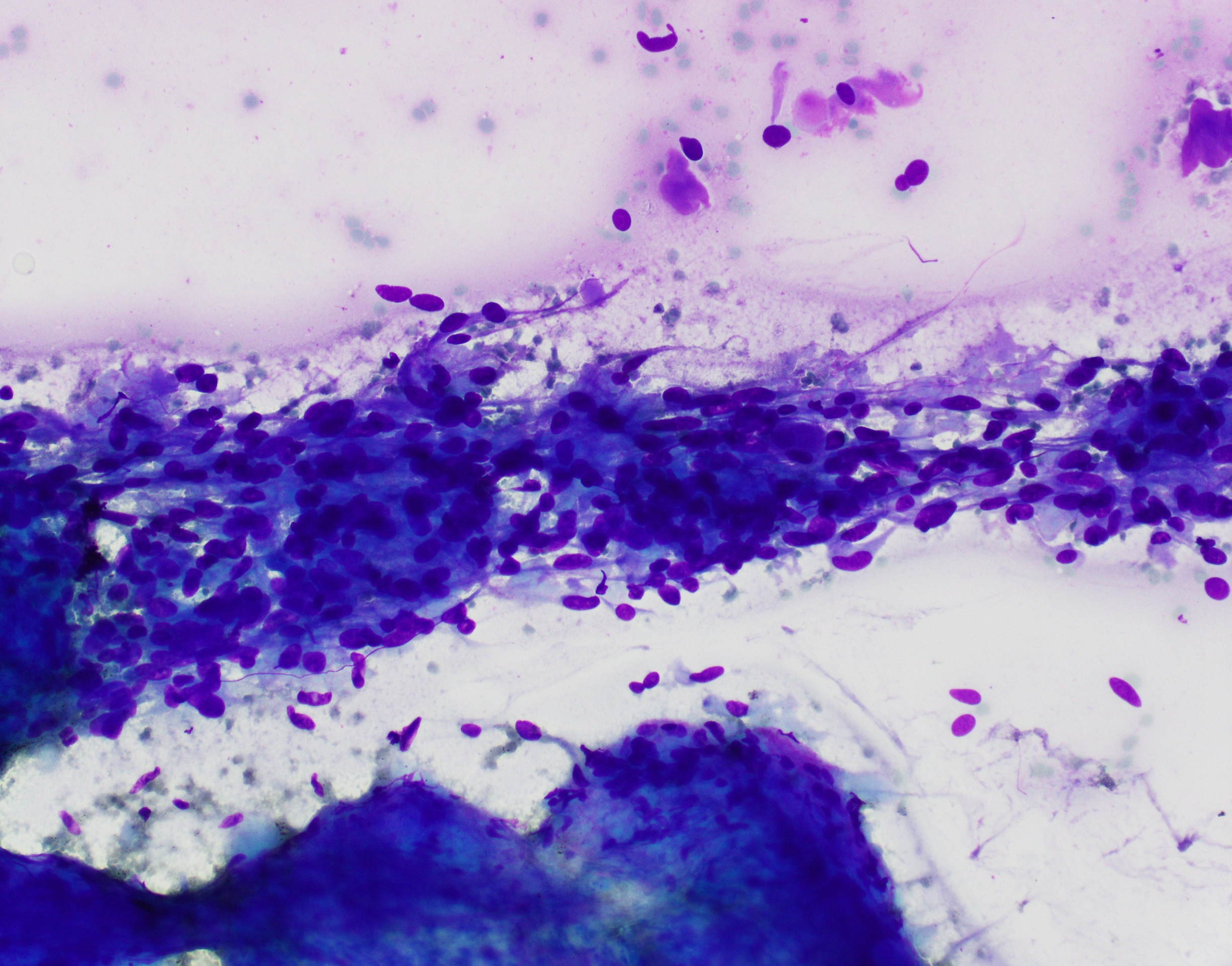
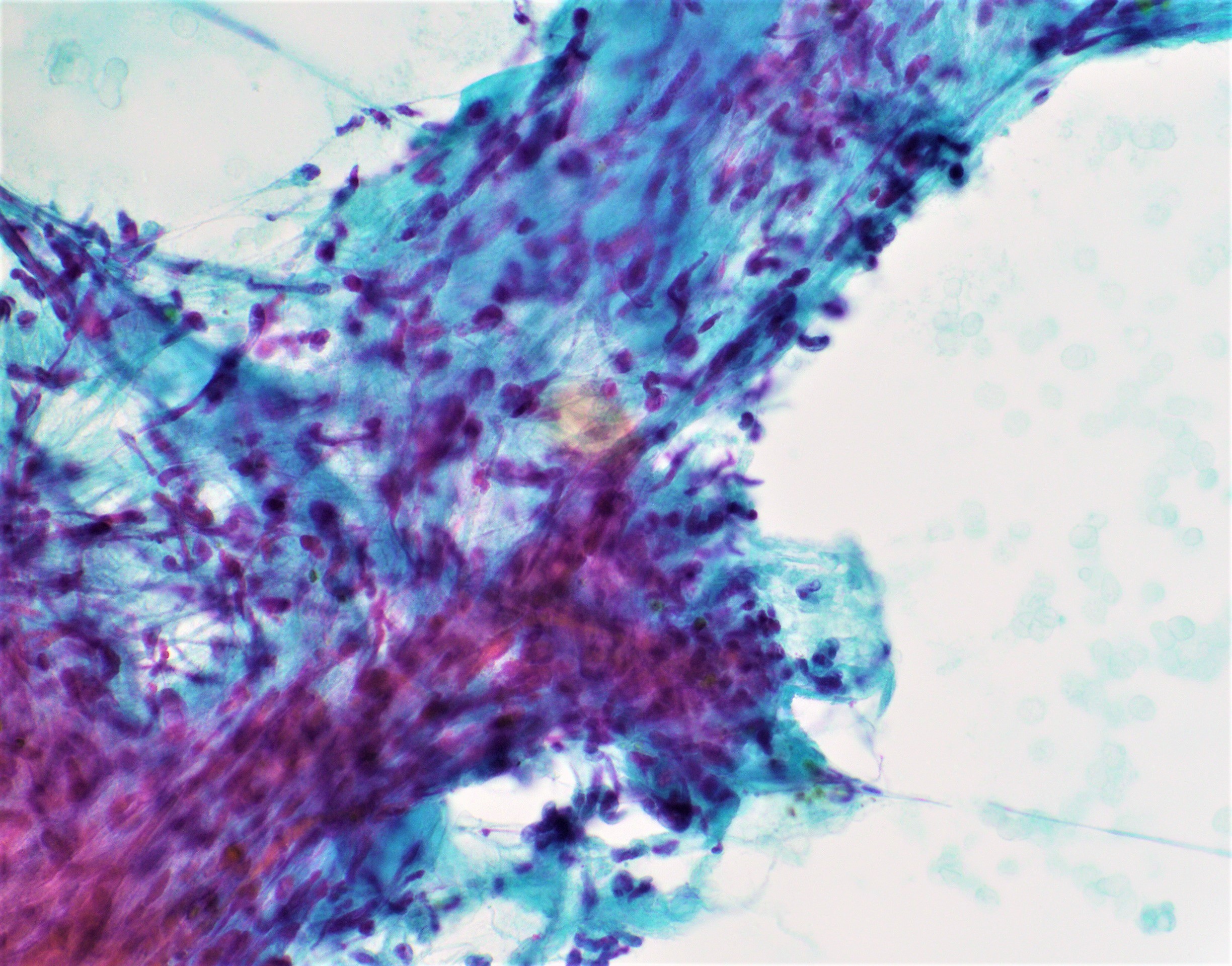
Cytology description
- Bland spindle and sometimes epithelioid cells
- EUS-FNA with IHC staining of cell block can lead to diagnosis
- If not enough material and large tumor size, there might not be enough for genotyping to guide neoadjuvant therapy
- Without enough tissue to perform immunohistochemical stains, it might be hard to get to a definitive diagnosis
- Reference: Diagn Cytopathol 2021 May 18 [Epub ahead of print]
Cytology images
Positive stains
Negative stains
- S100
- Desmin
- CK AE1 / AE3
- SMA - 34% in small bowel GISTs (Am J Surg Pathol 2006;30:477)
- NF1 (loss of expression of NF1; antibody specific to C terminus) - may help in identifying NF1 associated GISTs (Mod Pathol 2018;31:160)
Molecular / cytogenetics description
- See Pathophysiology
Videos
Small bowel GIST
Sample pathology report
- Duodenum, resection:
- Gastrointestinal stromal tumor (GIST), spindle cell type, 3.0 cm, grade 1 (see synoptic report for risk stratification as well as biomarker report)
Differential diagnosis
- Low grade spindle GISTs
- High grade spindle GISTs
- Leiomyosarcoma:
- Dedifferentiated liposarcoma:
- Spindle cell carcinoma:
- Positive for pancytokeratin and negative for CD117 and DOG1
Additional references
Board review style question #1
Which of the following is true regarding gastrointestinal stromal tumors in NF1 patients?
- Always associated with KIT mutation
- Epithelioid in morphology with loss of SDHB immunostaining by immunohistochemistry
- More aggressive than sporadic GISTs and present with metastasis
- Tumor can be multiple, is spindle cell in morphology, located in small intestine and indolent in behavior
Board review style answer #1
D. Tumor can be multiple, is spindle cell in morphology, located in small intestine and indolent
in behavior
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Comment Here
Reference: Gastrointestinal stromal tumor (GIST)
Board review style question #2
Besides KIT and PDGFRa mutations, what other mutations can be seen more commonly in small intestinal GISTs?
- BRAF
- IDH
- KRAS
- SDH
Board review style answer #2