Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zada S, Lee BA. Sebaceous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticsebaceouscarcinoma.html. Accessed April 1st, 2025.
Definition / general
- Malignant neoplasm with sebaceous differentiation
- Generally classified into periocular and extraocular
- Mostly occurs sporadically in elderly patients with an equal gender distribution; periocular locations have a female predominance (Curr Treat Options Oncol 2017;18:47, Onco Targets Ther 2018;11:3713)
Essential features
- Periocular versus extraocular
- Atypical sebocytes can be well, moderately or poorly differentiated
- May rarely occur in association with Muir-Torre syndrome, an autosomal dominant syndrome characterized by a sebaceous neoplasm (adenoma, sebaceoma or carcinoma) and occasionally keratoacanthoma associated with a visceral malignancy (Dermatol Surg 2015;41:1)
- Aggressive tumor with 5 year survival rate of 92.7%
- Treatment is primarily surgical excision
Terminology
- Sebaceous gland carcinoma
- Sebaceous cell carcinoma
- Meibomian gland carcinoma (J Korean Med Sci 2017;32:1351)
ICD coding
- ICD-10: C44.1392 - sebaceous cell carcinoma of skin of eyelid, including canthus
Epidemiology
- 0.2 - 4.6 % of all malignant cutaneous tumors and the third most common eyelid malignancy (Curr Treat Options Oncol 2017;18:47)
- More frequent:
- Patient age > 40
- Asian (periocular) (StatPearls: Sebaceous Gland Carcinoma [Accessed 30 March 2021])
Sites
- Most common in periocular area, head and neck but can arise from any sebaceous gland of the skin (StatPearls: Sebaceous Gland Carcinoma [Accessed 30 March 2021])
- Periocular (75%) > extraocular (25%) in most studies; however, more recent studies suggest the opposite (Dermatol Surg 2015;41:1, Cancer 2008;113:3372)
- Periocular:
- 1.0 - 3.2% of all malignant eyelid tumors
- Upper eyelid > lower eyelid
- Originates from meibomian glands, Zeiss glands, caruncle or skin of eyebrow (Curr Treat Options Oncol 2017;18:47)
- Extraocular:
- Occurs on the head and neck mostly, then rarely on the trunk, extremities, genitalia, external auditory meatus
- Very rarely can occur in extracutaneous sites, such as lungs, salivary glands and breast (Dermatol Pract Concept 2012;2:39, J Korean Med Sci 2017;32:1351)
- Can rarely occur in a nevus sebaceus of Jadassohn (J Dermatol 2016;43:175)
Pathophysiology
- Unknown
Etiology
- Radiation
- Immunosuppression
- Muir-Torre syndrome: autosomal dominant syndrome with mutation in one or more of the mismatch repair genes (MLH1, MSH2, MSH6 PMS2) and associated microsatellite instability
- Production of nitrosamines (food or medication)
- Retinoblastoma (Onco Targets Ther 2018;11:3713)
Clinical features
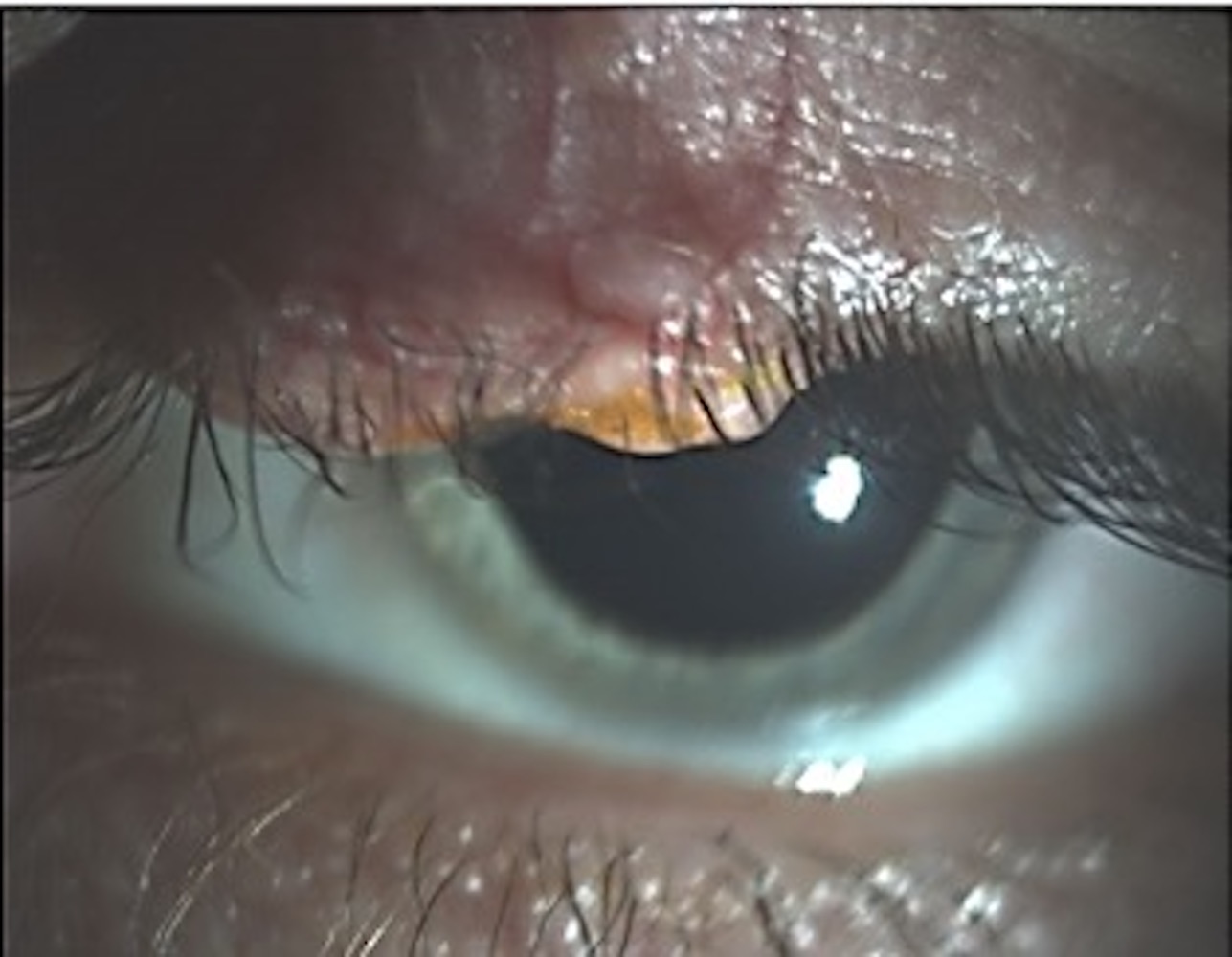
- Periocular: presents as a yellow to pink, painless, rapidly enlarging, firm papule, nodule or cystic lesion (Curr Treat Options Oncol 2017;18:47)
- Extraocular: presents as yellowish nodule, often with ulceration (StatPearls: Sebaceous Gland Carcinoma [Accessed 30 March 2021])
Diagnosis
- Biopsy is essential for the diagnosis (Curr Treat Options Oncol 2017;18:47)
Radiology description
- Radiologic studies may help to reveal bone destruction or soft tissue involvement by the tumor (Curr Treat Options Oncol 2017;18:47)
Prognostic factors
- 5 year relative survival rate: 92.7% (J Am Acad Dermatol 2016;75:1210)
- Overall prognosis for localized disease after complete excision is good
- Most significant predictor of reduced survival is the presence of metastatic disease at the time of diagnosis
- Other factors: multicentricity, pagetoid spread, perineural vascular and lymphatic invasion, poorly differentiated cytology, periocular location, primary site on the ear or lip, tumor size (> 10 mm), black race (Curr Treat Options Oncol 2017;18:47, Dermatol Surg 2015;41:1)
- Sebaceous carcinoma may metastasize in 2.4% of the cases; the majority of metastases occur within the first 2 years after initial treatment (Head Neck 2012;34:1765)
Case reports
- 37 year old woman with Muir-Torre syndrome associated sebaceous carcinoma occurring in the setting of lipedematous scalp (Case Reports Plast Surg Hand Surg 2020;7:124)
- 55 year old woman presenting with asymptomatic nodular ulcerating lesions on the right side of the vulva (Indian J Dermatol Venereol Leprol 2017;83:221)
- 59 year old woman with disseminated subcutaneous nodules with history of previously treated sebaceous cell carcinoma (Am J Case Rep 2018;19:1192)
- 67 year old woman with longstanding history of an ovarian dermoid cyst (Gynecol Oncol Rep 2018;26:37)
Treatment
- Wide local excision or Mohs micrographic surgery are the best initial treatment options
- Sentinel lymph node biopsy for periorbital sebaceous carcinoma > 10 mm in diameter
- Radiation therapy and systemic chemotherapy are only used for patients who are poor surgical candidates or those with recurrent or metastatic disease
- Immunohistochemistry to evaluate for microsatellite instability (MSH2, MSH6, MLH1, PMS2) should be offered on sebaceous carcinoma specimens, especially extraocular ones, to screen for Muir-Torre syndrome
- Evidence of orbital invasion on imaging necessitates exenteration (Dermatol Surg 2015;41:1)
Clinical images
Gross description
- Papule, nodule or cystic lesion
Frozen section description
- Lipid and fat staining with frozen sections have been used in the past
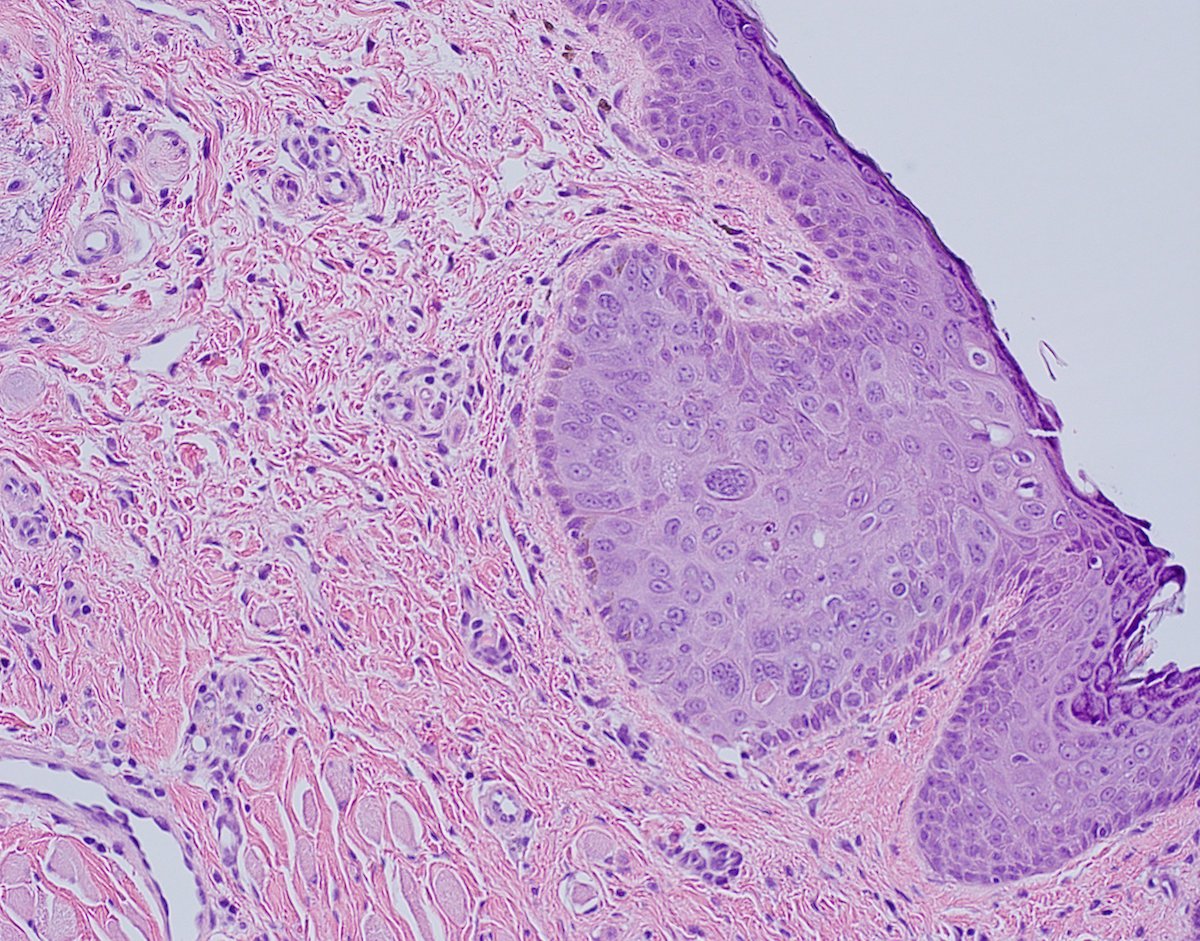
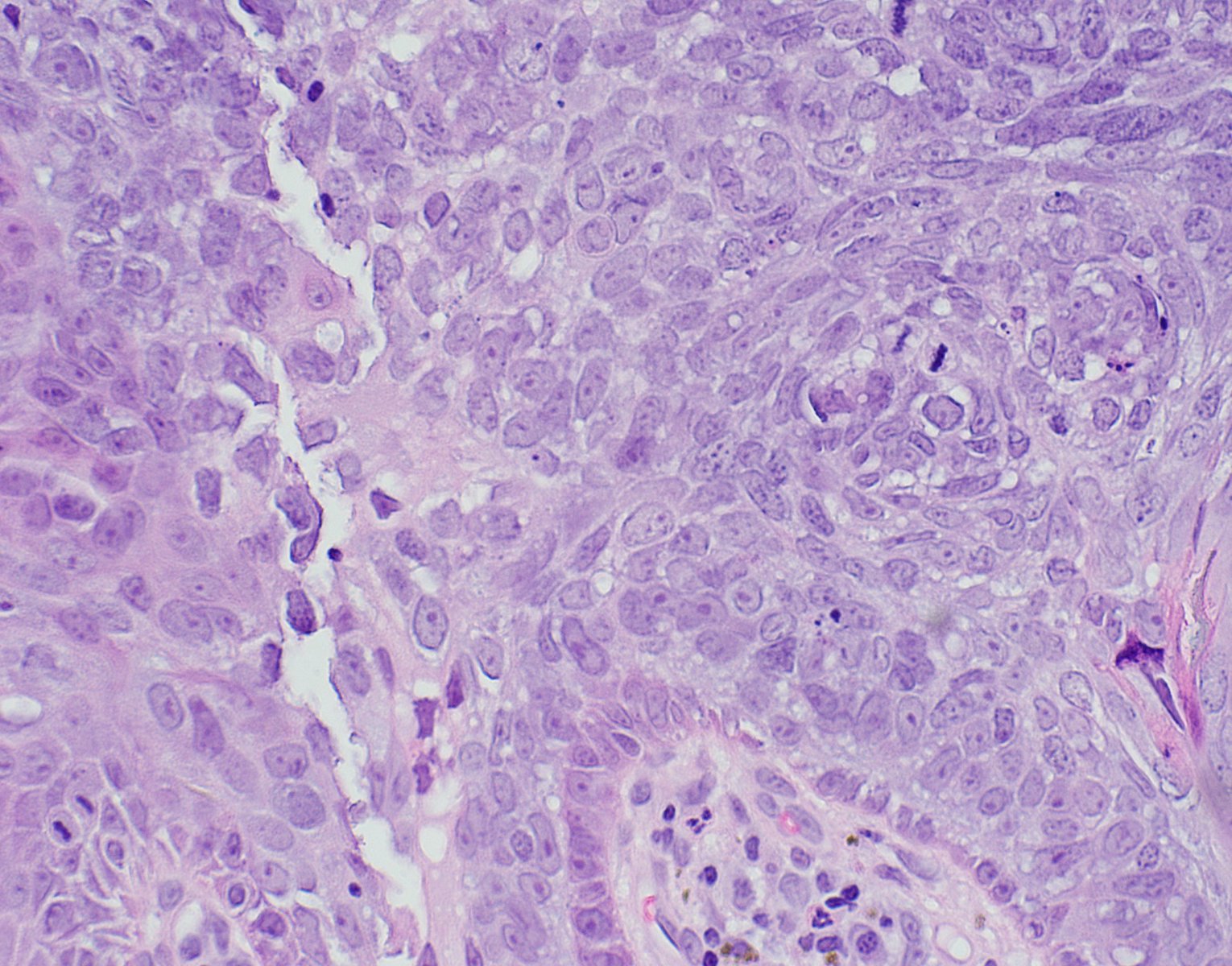
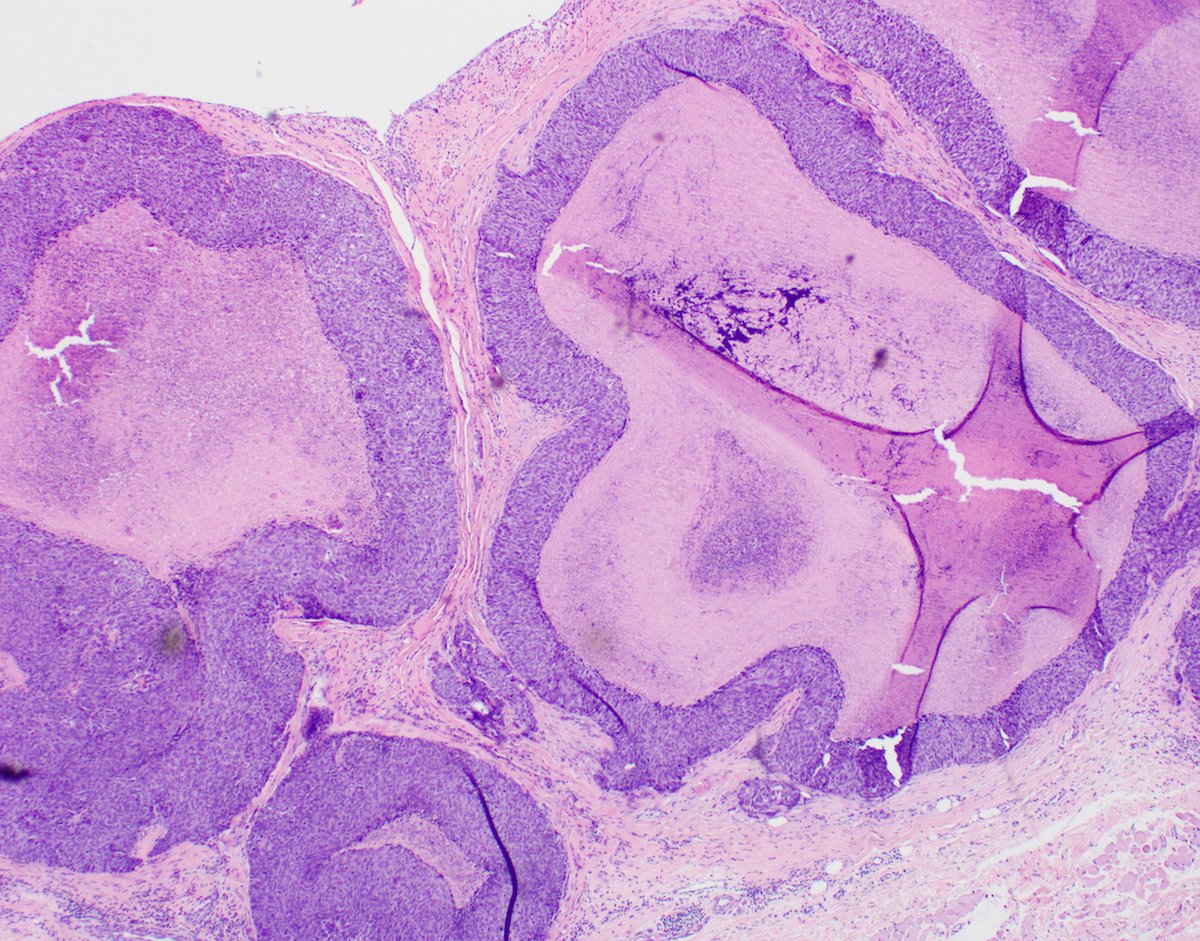
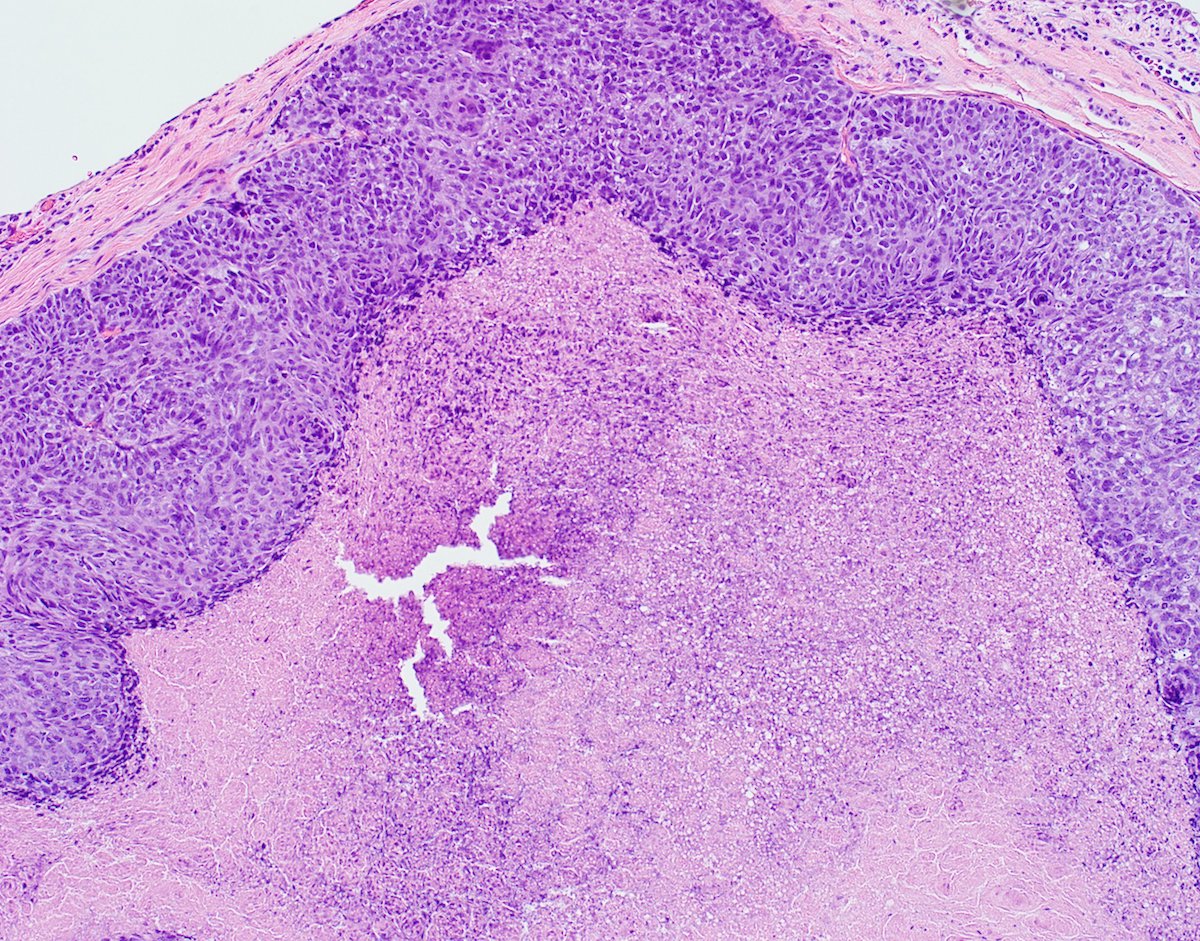
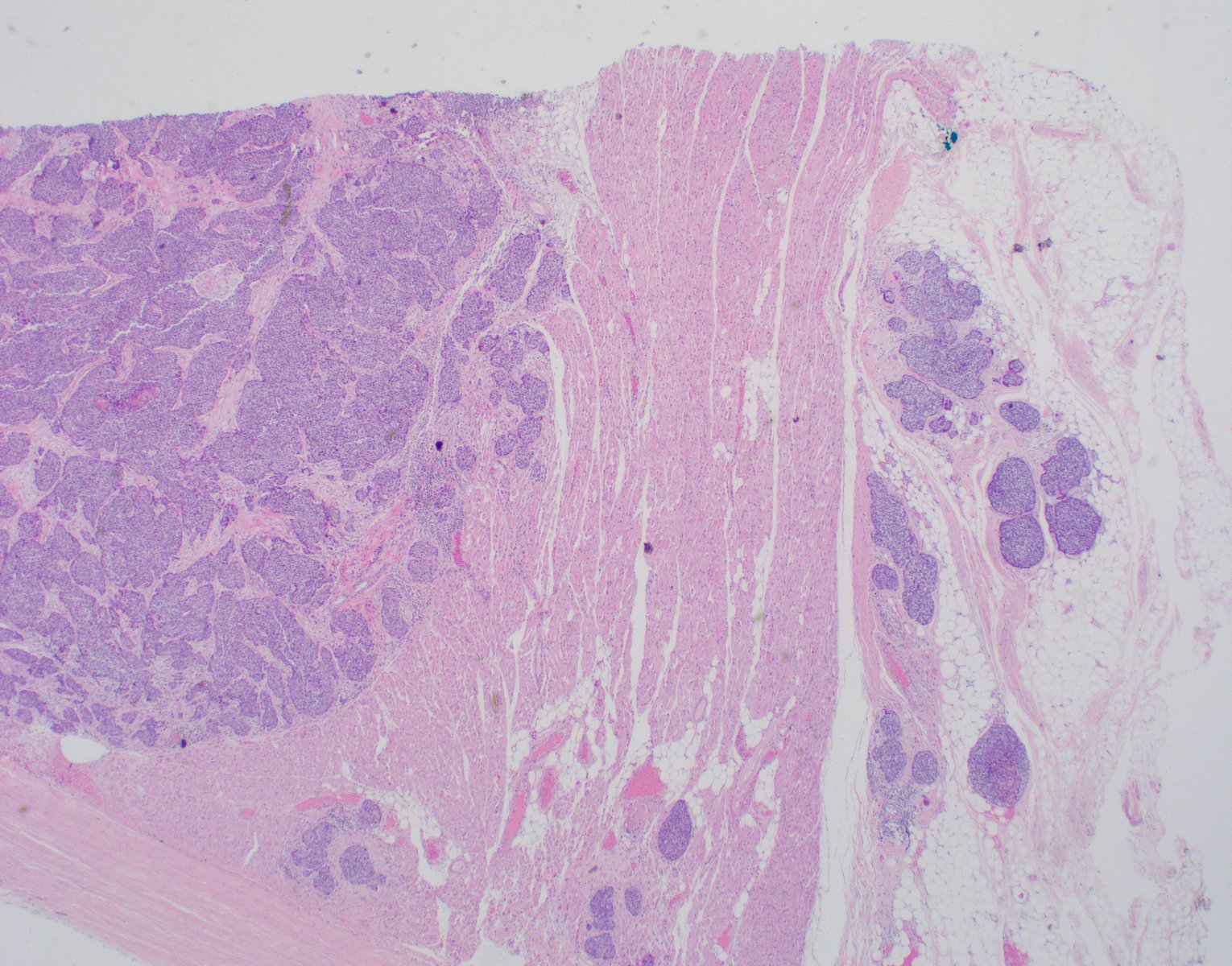
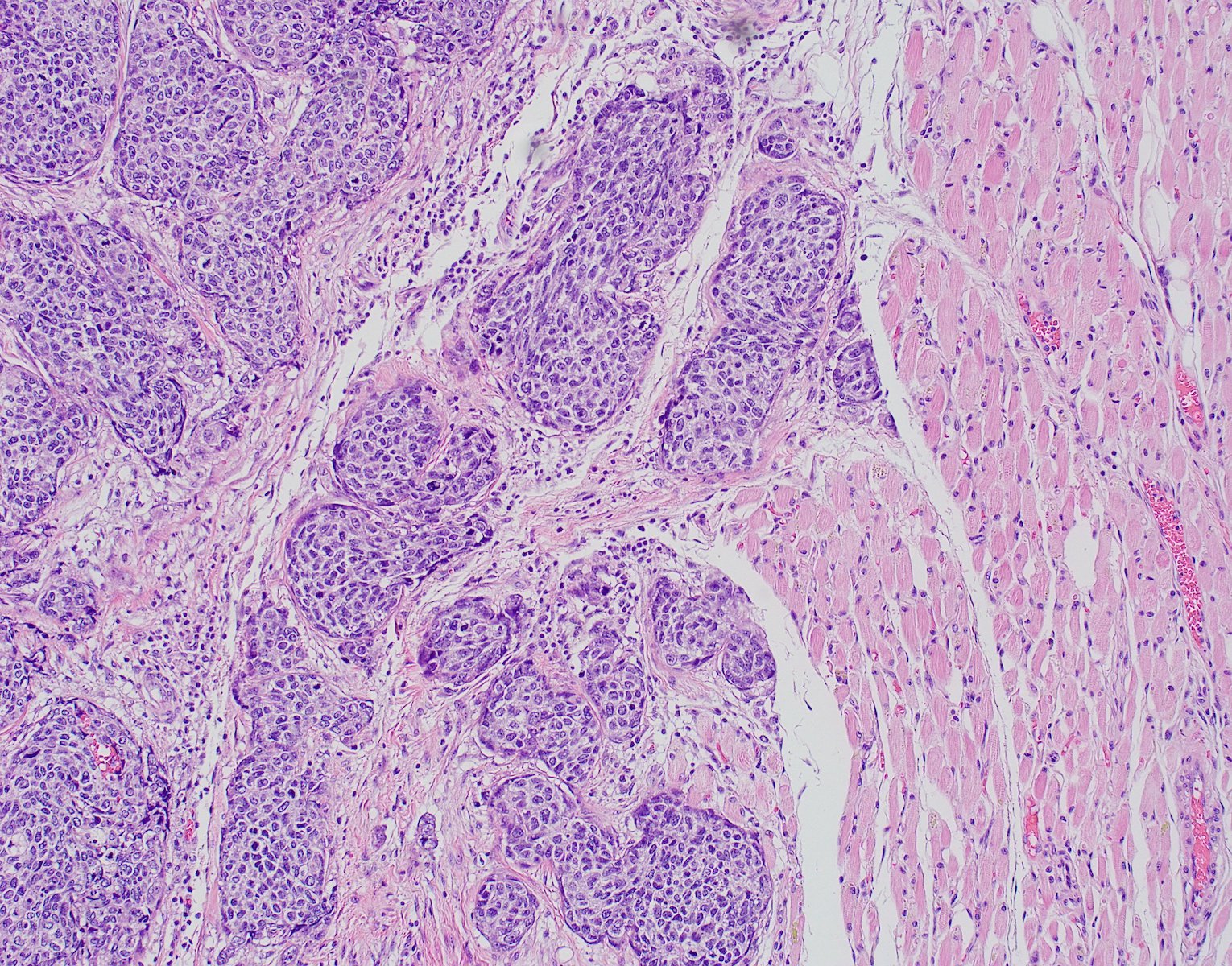
Microscopic (histologic) description
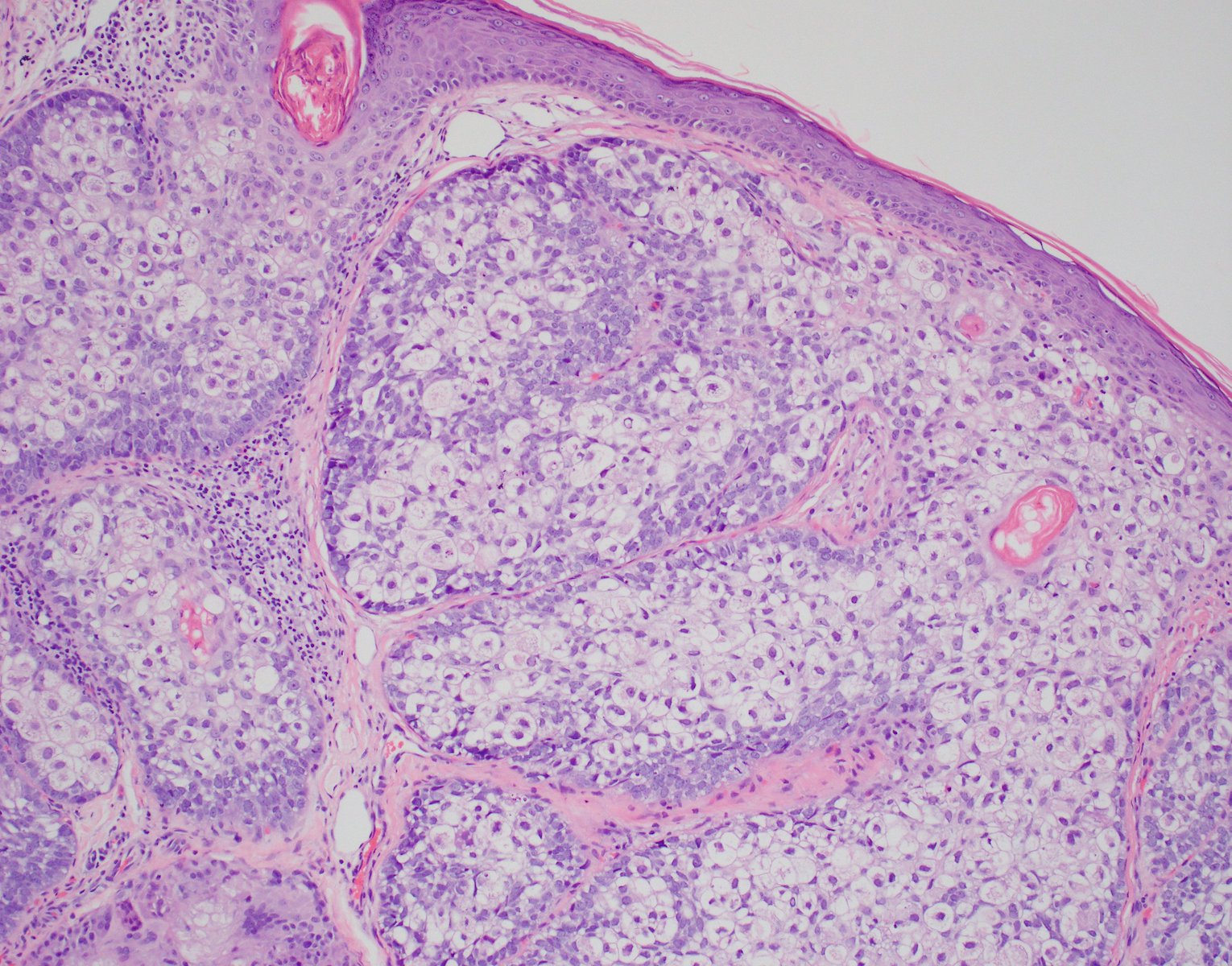
- Architecture: usually sheets or lobules separated by fibrovascular stroma
- Dermal based tumor with focal connection to the epidermis or follicular epithelium
- Can be rounded nodular aggregates or angulated infiltrative aggregates
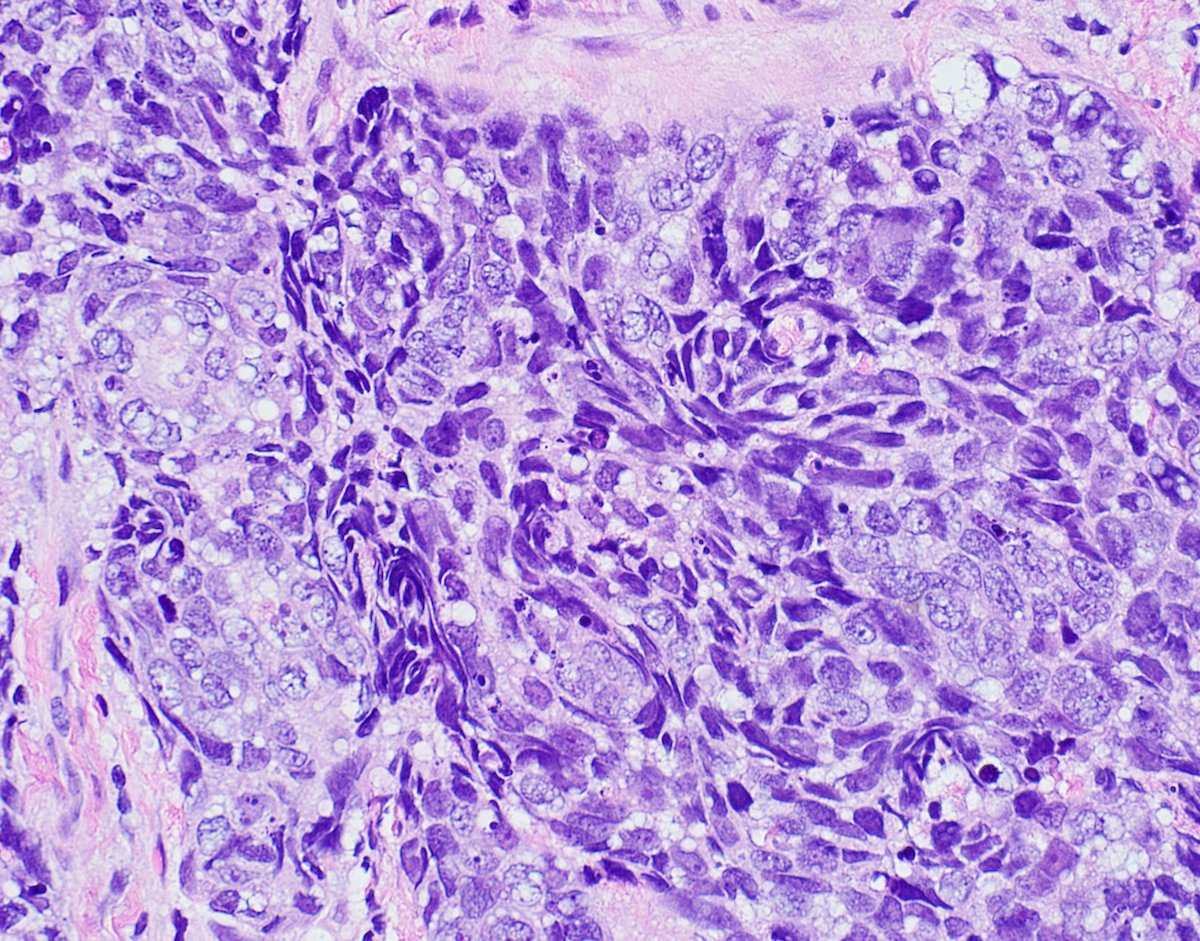
- Can appear cystic with central comedo type necrosis
- Less commonly, can have a broad superficial intraepidermal pattern
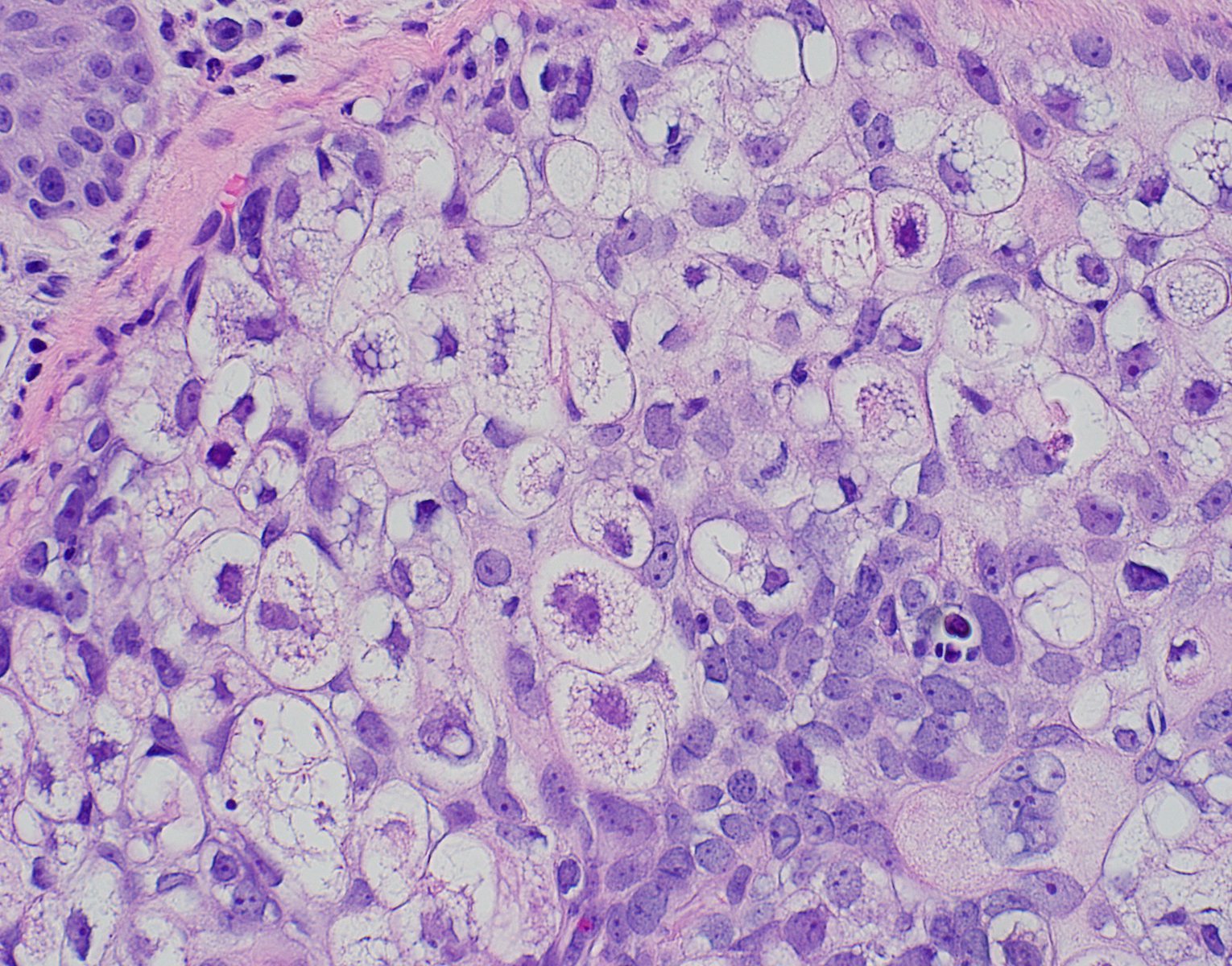
- Cytology: classified as poorly, moderately or well differentiated
- Well differentiated: increased proportion of mature appearing sebocytes (multivacuolated cells) with nuclear indentation relative to basaloid undifferentiated cells
- Mild pleomorphism, minimal mitoses and necrosis
- Moderately to poorly differentiated: higher proportion of atypical basaloid (undifferentiated) cells with minimal differentiation toward multivacuolated cells
- Prominent pleomorphism and atypia, frequent mitoses and necrosis
- Well differentiated: increased proportion of mature appearing sebocytes (multivacuolated cells) with nuclear indentation relative to basaloid undifferentiated cells
- Pagetoid (or intraepidermal sebaceous carcinoma, sebaceous carcinoma in situ) tumor growth is much more commonly observed in periocular than in extraocular locations, where it is rare
- Can exhibit squamous metaplasia or focal apocrine differentiation
- References: Dermatol Surg 2015;41:1, Curr Treat Options Oncol 2017;18:47, Int J Surg Pathol 2019;27:432, J Korean Med Sci 2017;32:1351
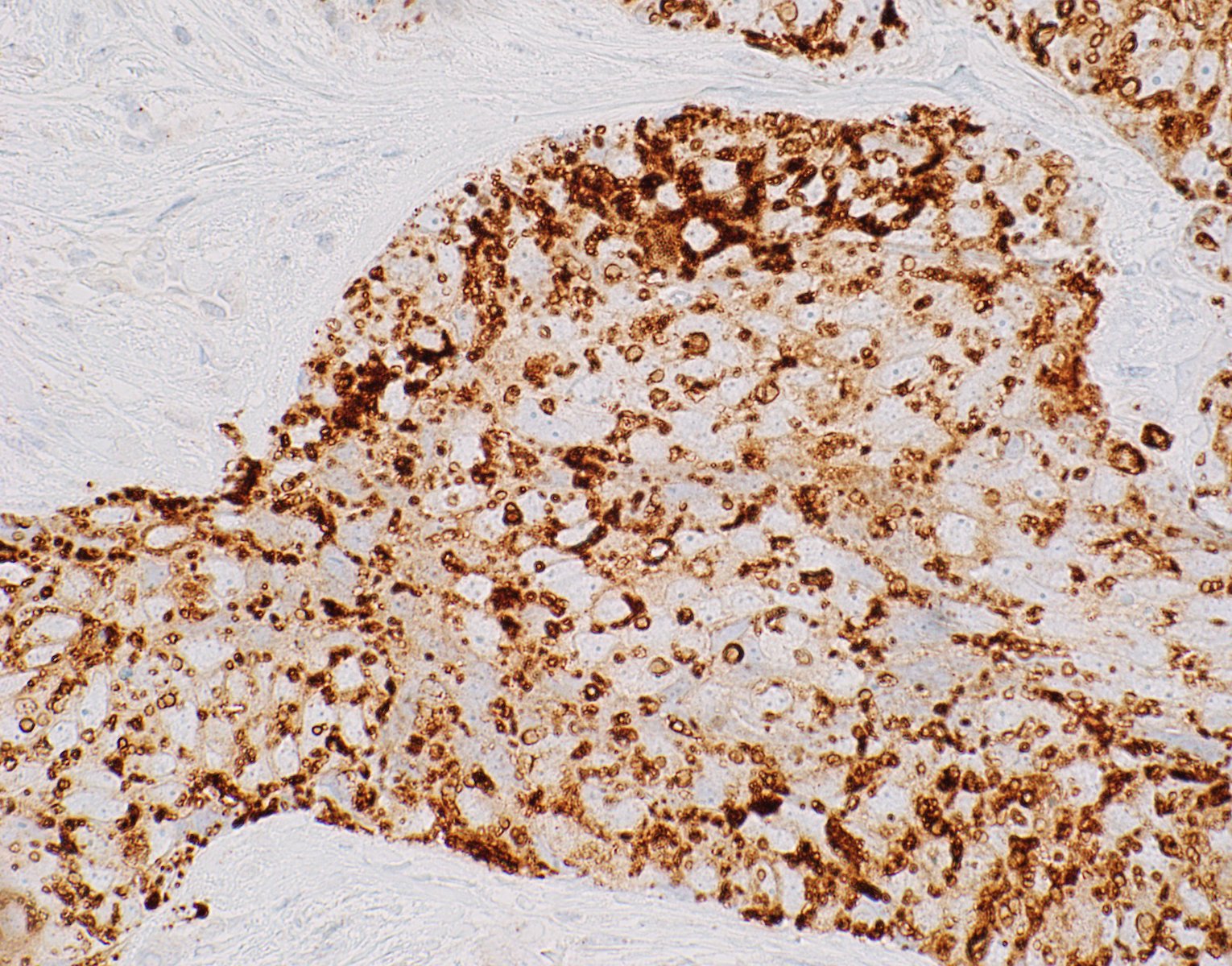
Microscopic (histologic) images
Contributed by Bonnie Lee, M.D. and Maria Del Valle Estopinal, M.D.
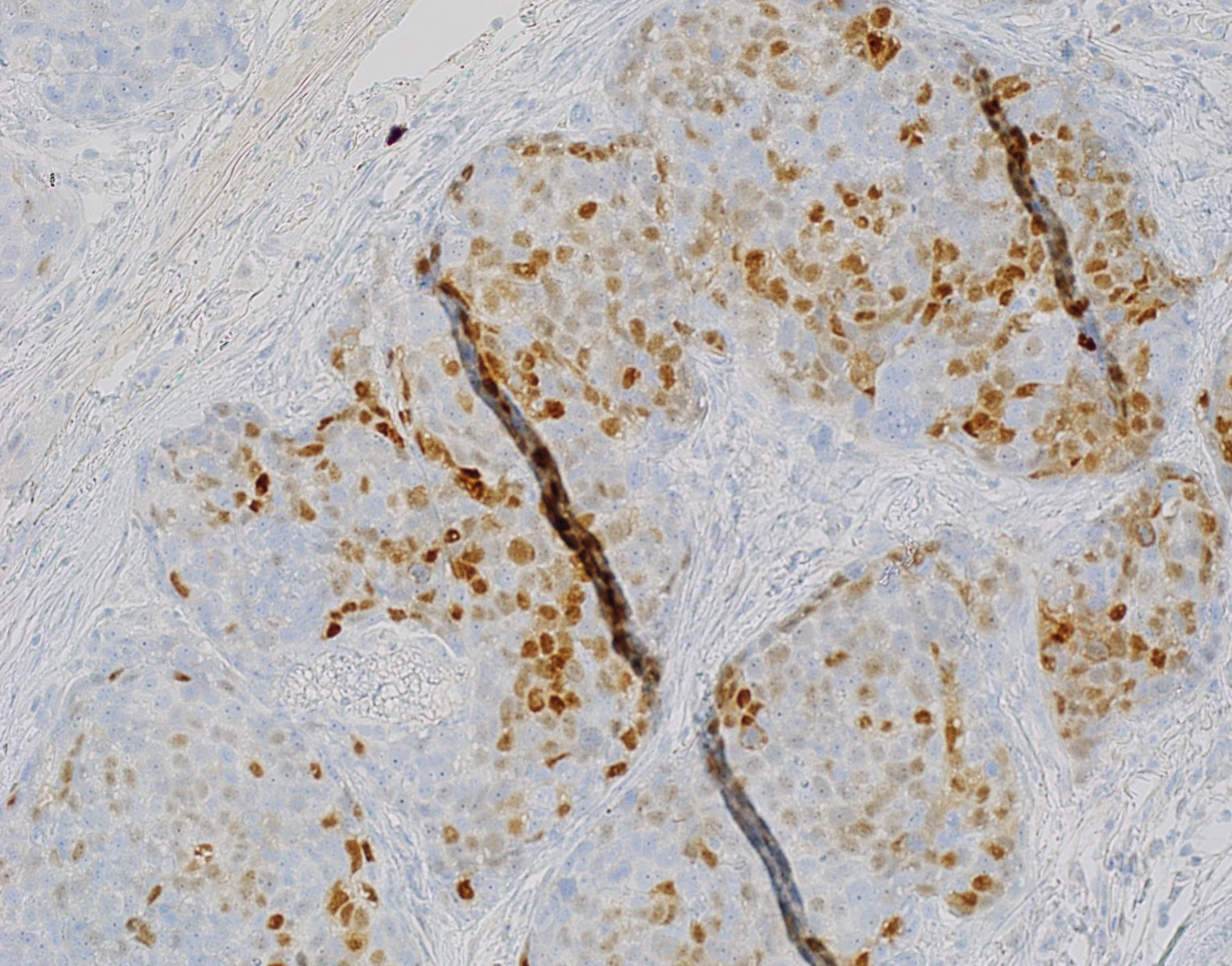
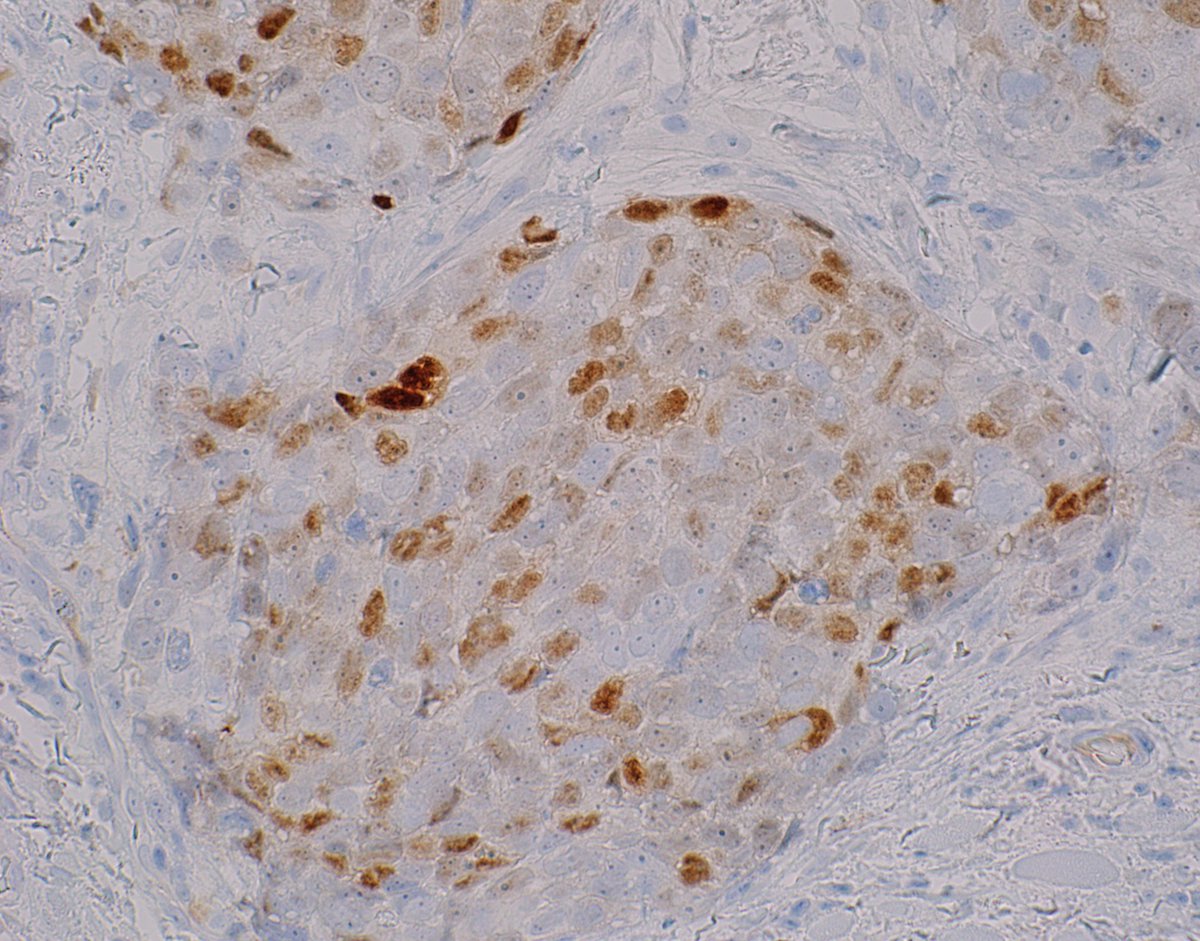
Positive stains
- Androgen receptor
- Adipophilin - membranous vesicular pattern (a granular pattern is considered negative)
- Keratin
- EMA
- LeUM1
- Ki67 - increased relative to sebaceous adenoma and sebaceoma
- p53 - increased relative to sebaceous adenoma and sebaceoma
- BerEP4
- References: Onco Targets Ther 2018;11:3713, Curr Opin Ophthalmol 2018;29:445
Sample pathology report
- Skin, right elbow, shave biopsy:
- Well differentiated sebaceous neoplasm with severe nuclear atypia, consistent with sebaceous carcinoma (G1)
- Tumor measures at least 5.5 mm in greatest dimension
- Margins cannot be evaluated in the plane of sections examined
- No definite lymphovascular or perineural invasion identified
- American Joint Committee on Cancer pathologic staging (8th edition): pT1 pNx (Amin: AJJC Cancer Staging Manual, 8th edition, 2017)
- Left lower eyelid, wedge excision:
- Recurrent, sebaceous cell carcinoma in situ, moderately differentiated involving the skin of the left lower eyelid
- Tumor size: 0.7 mm
- Lymphovascular space invasion: not identified
- Perineural invasion: not identified
- Mitotic rate: 5 mitoses per square mm
- Surgical margins: nasal, temporal, inferior and deep margins are negative for sebaceous carcinoma
- Microsatellite instability markers for sebaceous carcinoma: positive (retained) nuclear staining for MLH1, PMS2, MSH2 and MSH6
- Pathologic staging: pTIs
- IHC stains: androgen receptor - positive in tumor cells; adipophilin - positive in tumor cells; BerEP4: negative in tumor cells
Differential diagnosis
- Basal cell carcinoma with sebaceous differentiation:
- Clear cell squamous cell carcinoma:
- Balloon cell melanoma:
- Metastatic clear cell carcinoma (renal):
- Clear cell sarcoma:
Additional references
Board review style question #1
A 75 year old woman had an excisional biopsy for a rapidly growing mass in her upper eyelid. Histologic details are shown in the image above. Which of the following is true regarding this entity?
- Pagetoid spread is more common in periocular location
- Radiation therapy is the first line treatment
- Surgical excision is not helpful
- This tumor is S100 positive
Board review style answer #1
A. Pagetoid spread is more common in periocular location. The pagetoid pattern of sebaceous carcinomas is seen much more in the periocular area. This tumor is characteristically S100 negative. First line treatment is surgical excision. Radiation therapy is helpful in metastatic disease and in poor surgical candidates.
Comment Here
Reference: Sebaceous carcinoma
Comment Here
Reference: Sebaceous carcinoma
Board review style question #2
Which immunostain is negative in sebaceous carcinoma?
- Adipophilin
- Androgen receptor
- CEA
- EMA
Board review style answer #2
C. CEA. Sebaceous carcinoma stains positive for EMA, adipophilin, androgen receptor. It is usually negative for CEA.
Comment Here
Reference: Sebaceous carcinoma
Comment Here
Reference: Sebaceous carcinoma