Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style question #3Cite this page: Alhalaseh Y, Pradhan D. Sebaceoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticsebaceoma.html. Accessed March 31st, 2025.
Definition / general
- Benign sebaceous neoplasm consisting of an admixture of mature sebocytes and predominantly immature basaloid cells (> 50% of the neoplasm)
- Associated with Muir-Torre syndrome (MTS) but can also be an isolated (sporadic) tumor (Am J Dermatopathol 2000;22:155)
Essential features
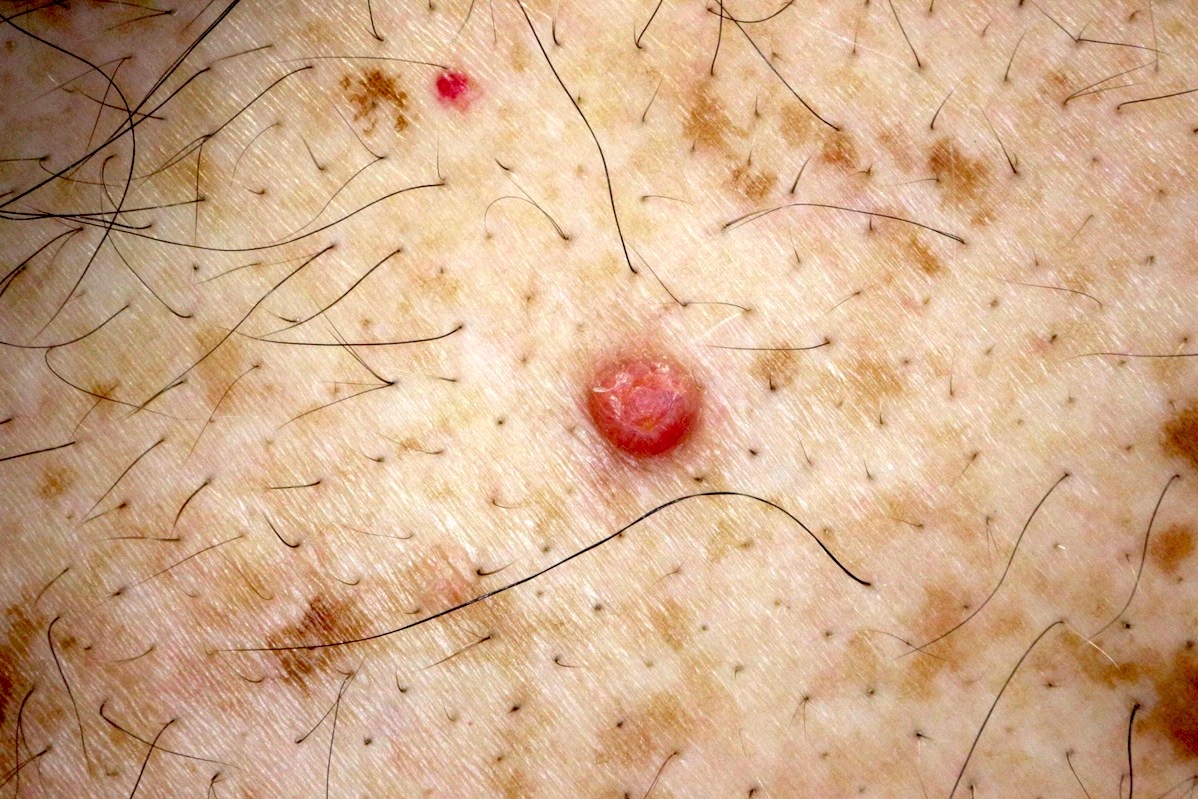
- Benign adnexal neoplasm that clinically presents as a solitary, yellow-tan papule / nodule
- Histologic sections show well circumscribed cellular lobules composed of predominant immature basaloid cells (> 50% of the lesion) with admixed mature sebocytes
- Associated with Muir-Torre syndrome
Terminology
- Sebaceous epithelioma, as a term, is confusing and is best not used
- Sebaceous epithelioma could refer to a low grade form of sebaceous carcinoma, a basal cell carcinoma with sebaceous differentiation or sebaceous proliferations of uncertain potential and thus is not a useful term
ICD coding
- ICD-O: 8410/0 - sebaceoma
- ICD-11: 2F22 & XH0QL4 - benign neoplasms of epidermal appendages & sebaceoma
Epidemiology
- Female predominance (Am J Dermatopathol 2002;24:294, Am J Dermatopathol 1984;6:7)
- Majority in the sixth to ninth decades (Ann Dermatol Venereol 2016;143:814)
- Mean age at diagnosis is 70 years (Am J Dermatopathol 1984;6:7)
Sites
- Most common location is the face and scalp
- Less frequently on the trunk or extremities and should prompt consideration of Muir-Torre syndrome (Am J Dermatopathol 2001;23:58, J Am Acad Dermatol 1996;34:47, Am J Dermatopathol 1984;6:7)
Pathophysiology
- Sebaceomas commonly have mutation of RAS family genes (HRAS and KRAS), TP53, CDKN2A, EGFR and CTNNB1 when examined by next generation sequencing
- Abnormalities of TP53 were most frequently found (Pathology 2016;48:454)
Etiology
- Sebaceomas are associated with defective mismatch repair proteins, manifesting as loss of expression of mismatch repair gene products, including MLH1, MSH2, MSH6 and PMS2; a subset of these are related to Muir-Torre syndrome (J Cutan Pathol 2009;36:613, Arch Pathol Lab Med 2014;138:1685, J Am Acad Dermatol 2016;74:558, Am J Dermatopathol 2017;39:239, Mod Pathol 2011;24:1004, Histopathology 2010;56:133, Am J Dermatopathol 2021;43:174)
Clinical features
- Yellow-orange or flesh colored papule, nodule or tumor (Am J Dermatopathol 1984;6:7, Am J Dermatopathol 2002;24:294)
- Usually a single lesion but can be multifocal in association with Muir-Torre syndrome (Am J Dermatopathol 2000;22:155)
- Muir-Torre syndrome is considered a phenotypic variant of hereditary nonpolyposis colorectal carcinoma syndrome (HNPCC, Lynch syndrome) and is caused by germline mutations in one allele of the DNA mismatch repair (MMR) genes, most commonly MLH1, MSH2, MSH6 and PMS2
- Muir-Torre syndrome is associated with sebaceous neoplasia (most commonly sebaceous adenoma), colorectal, genitourinary (GU) and other visceral adenocarcinomas
- Defective MMR gene products have been observed in association with sebaceoma, including MLH1, MSH2, MSH6 and PMS2; a subset of these are related to Muir-Torre syndrome (J Cutan Pathol 2009;36:613, Arch Pathol Lab Med 2014;138:1685, J Am Acad Dermatol 2016;74:558, Am J Dermatopathol 2017;39:239, Mod Pathol 2011;24:1004, Histopathology 2010;56:133, Am J Dermatopathol 2021;43:174)
- MSH2 is the gene most commonly mutated in Muir-Torre syndrome
- If there is concern for Muir-Torre syndrome (personal or family history of colorectal, GU or breast cancer; an older patient with numerous sebaceous neoplasms, especially not on the head and neck), further testing for MMR IHC or microsatellite instability (MSI) can be performed
- IHC cannot differentiate between loss of MLH1 expression caused by a germline mutation versus a somatic hypermethylation; some germline missense mutations may be erroneously interpreted as normal by IHC because they may result in an antigenically intact but nonfunctional protein
- MSI analysis, performed on formalin fixed tissue, is more sensitive at detecting patients with germline MMR defects than IHC
- Results are either MSI-H (high degree of MSI) or MSI-L (low degree of MSI)
- Germline mutation analysis: blood leukocyte genomic sequencing is preferred to identify germline mutations in the MLH1, MSH2, MSH6 and PMS2 genes; if there are no germline mutations but the tumor shows MMR deficiency, there may be involvement of other MMR proteins, somatic mutations or hypermethylation of the promoter region
- Head and neck sebaceomas tend to be MMR stable as compared to sebaceomas outside the head and neck regions, which tend to be MMR deficient (Am J Surg Pathol 2008;32:936, Am J Dermatopathol 2021;43:174)
- Other mutations have been identified in sebaceoma with next generation sequencing studies, including TP53 (most common), RAS family genes (HRAS and KRAS), CDKN2A, EGFR and CTNNB1 (Pathology 2016;48:454)
- Sebaceoma can arise in a pre-existing sebaceous nevus (Pathology 2016;48:454)
Diagnosis
- Solitary, yellow-tan papules / nodule (Am J Dermatopathol 1984;6:7)
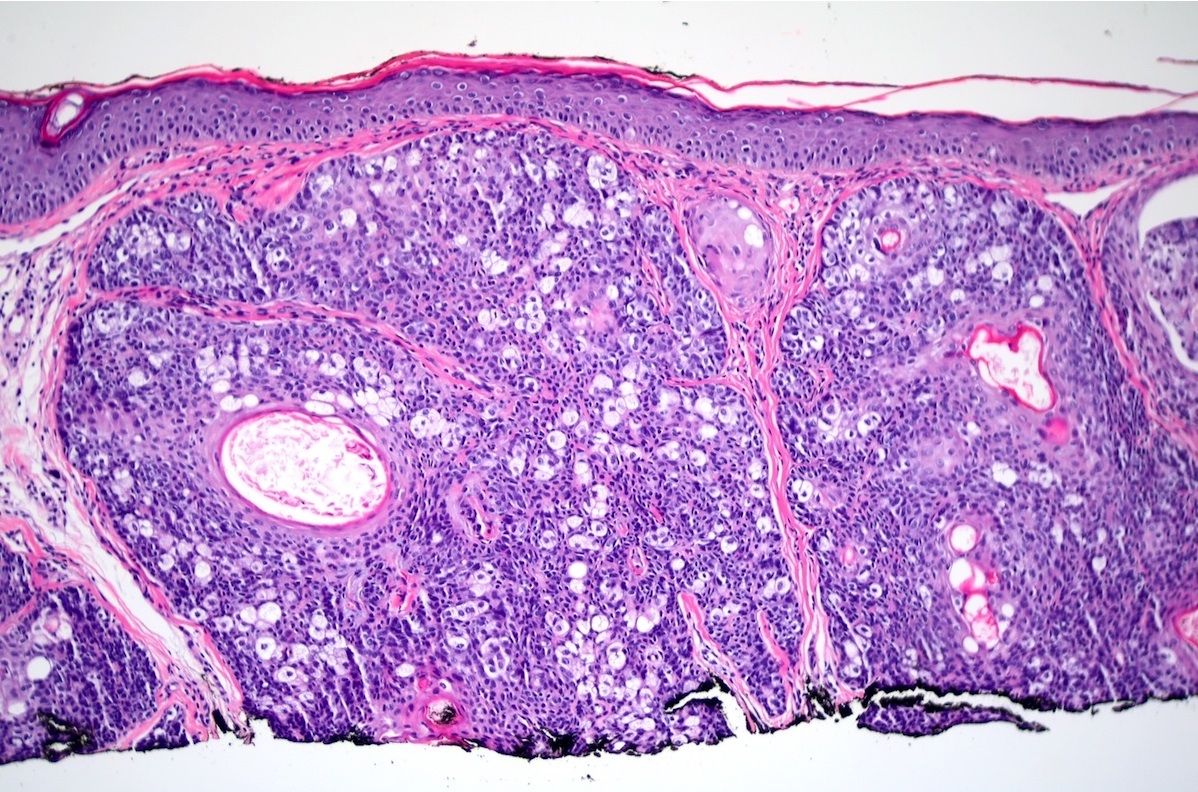
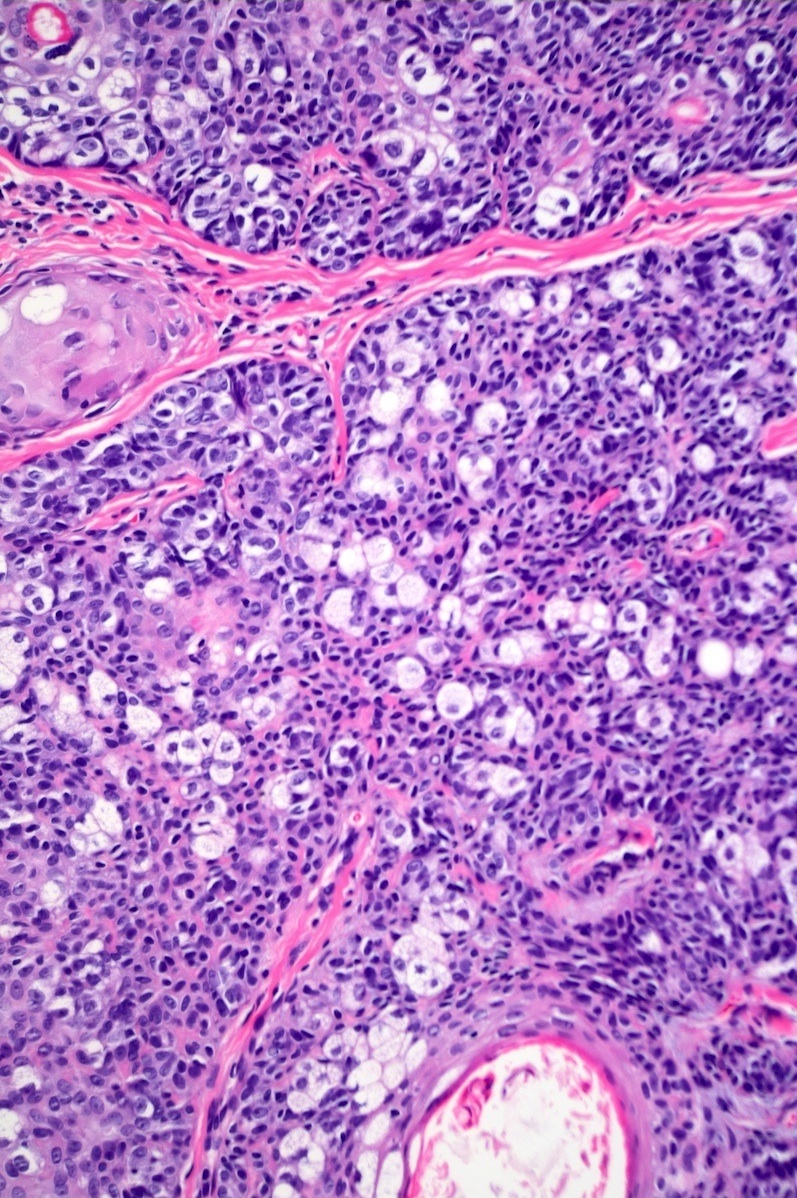
- Well circumscribed cellular lobules comprised mostly of small monomorphic immature but cytologically benign basaloid cells admixed with fewer mature sebocytes (< 50%), haphazardly distributed throughout the tumor (Histopathology 2010;56:133)
Prognostic factors
- Sebaceomas have excellent prognosis and can be treated with conservative excision (Histopathology 2010;56:133)
- Loss of nuclear staining for MLH1, MSH2, MSH6 or PMS2 suggests MSI, supports a diagnosis of Muir-Torre syndrome and increases the risk of associated visceral malignancies (J Cutan Pathol 2009;36:613, J Am Acad Dermatol 2016;74:558, Arch Pathol Lab Med 2014;138:1685)
- Transformation to sebaceous carcinoma is rare (J Cutan Pathol 2016;43:64, J Cutan Pathol 2013;40:676)
Case reports
- 48 year old man presented with a pea sized growth in his left arm (Indian J Pathol Microbiol 2022;65:465)
- 71 year old woman had a dome shaped, slightly erythematous nodule on the anterior scalp (Am J Dermatopathol 2001;23:437)
- 76 year old woman with a 3 mm solitary pink papule on the nose (Skin Res Technol 2022;28:886)
Treatment
- Once the diagnosis is established, no further treatment is needed if the biopsy margins are negative
- However, complete excision should be considered if the tumor is only partially biopsied or there is concern for basal cell carcinoma with sebaceous differentiation or sebaceous carcinoma
Clinical images
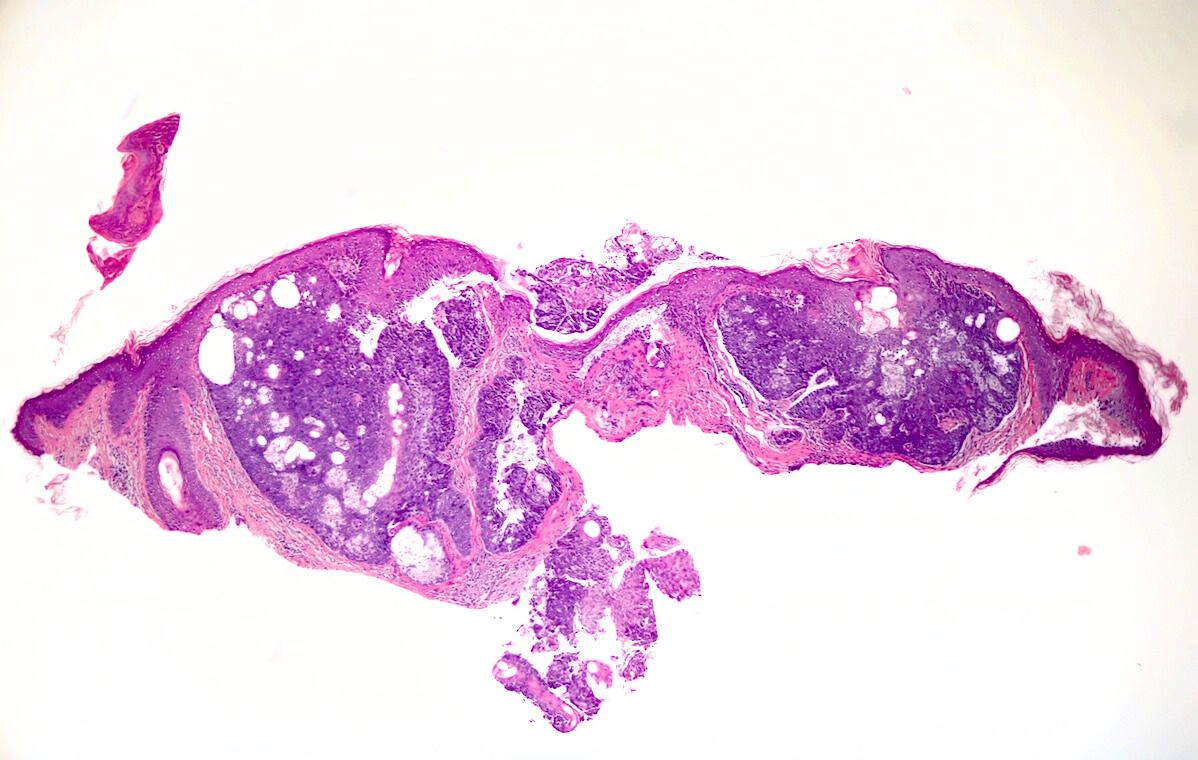
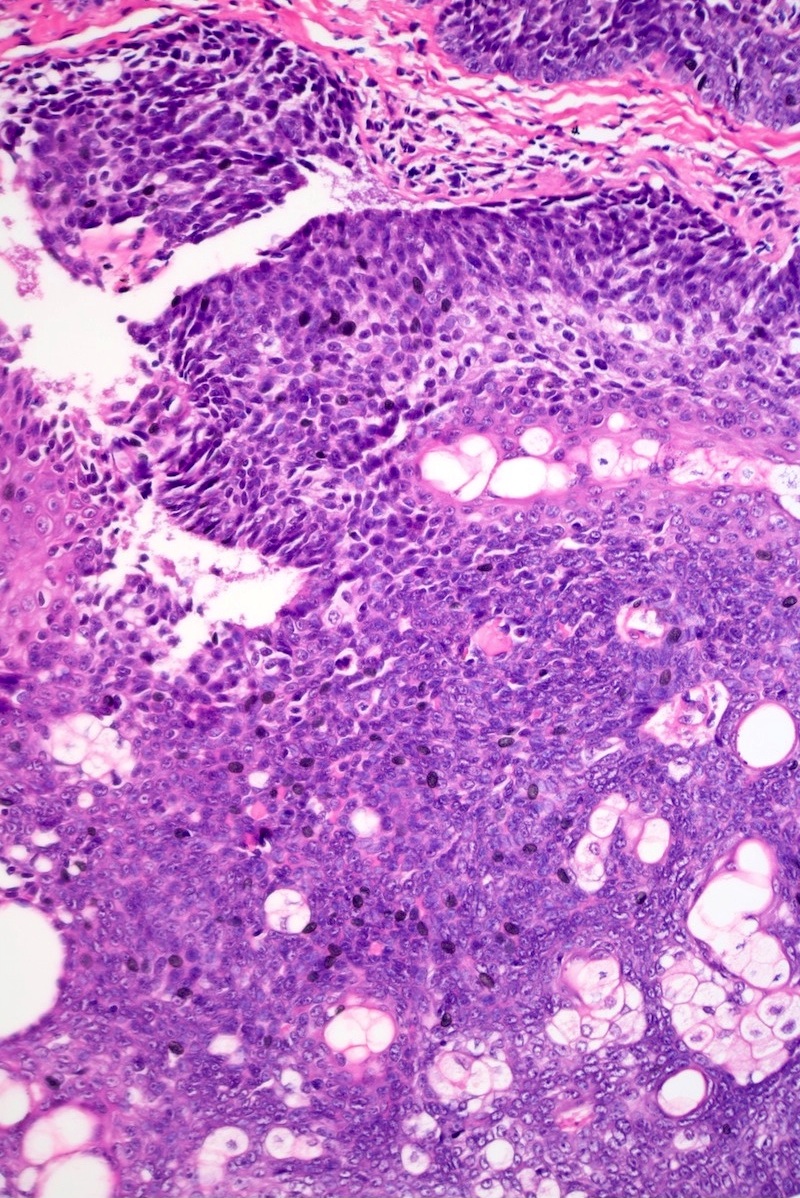
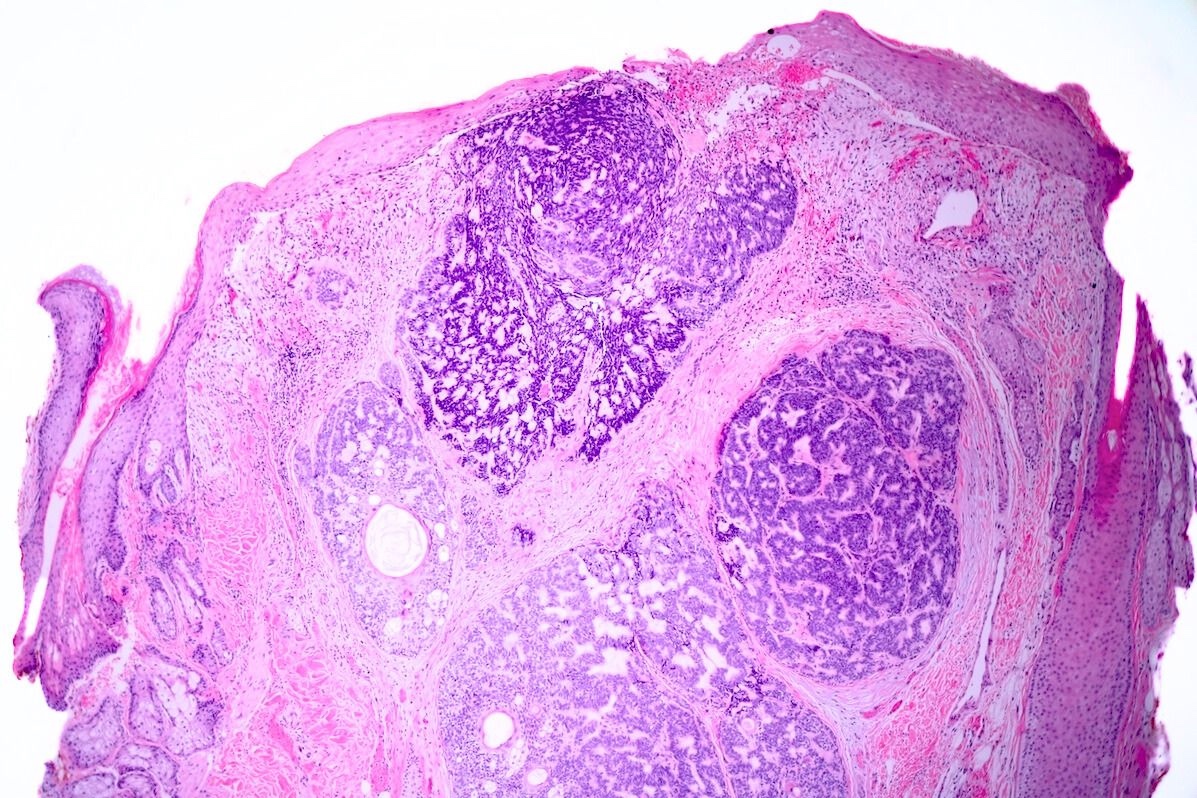
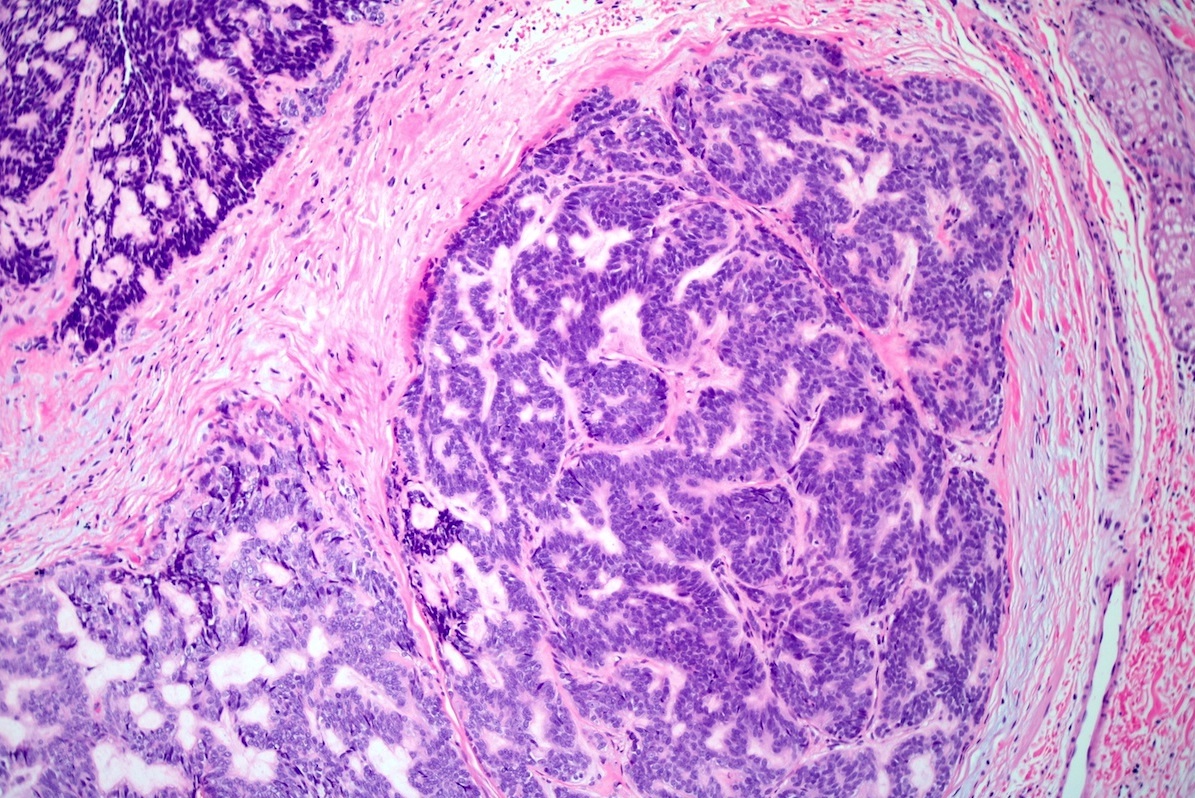
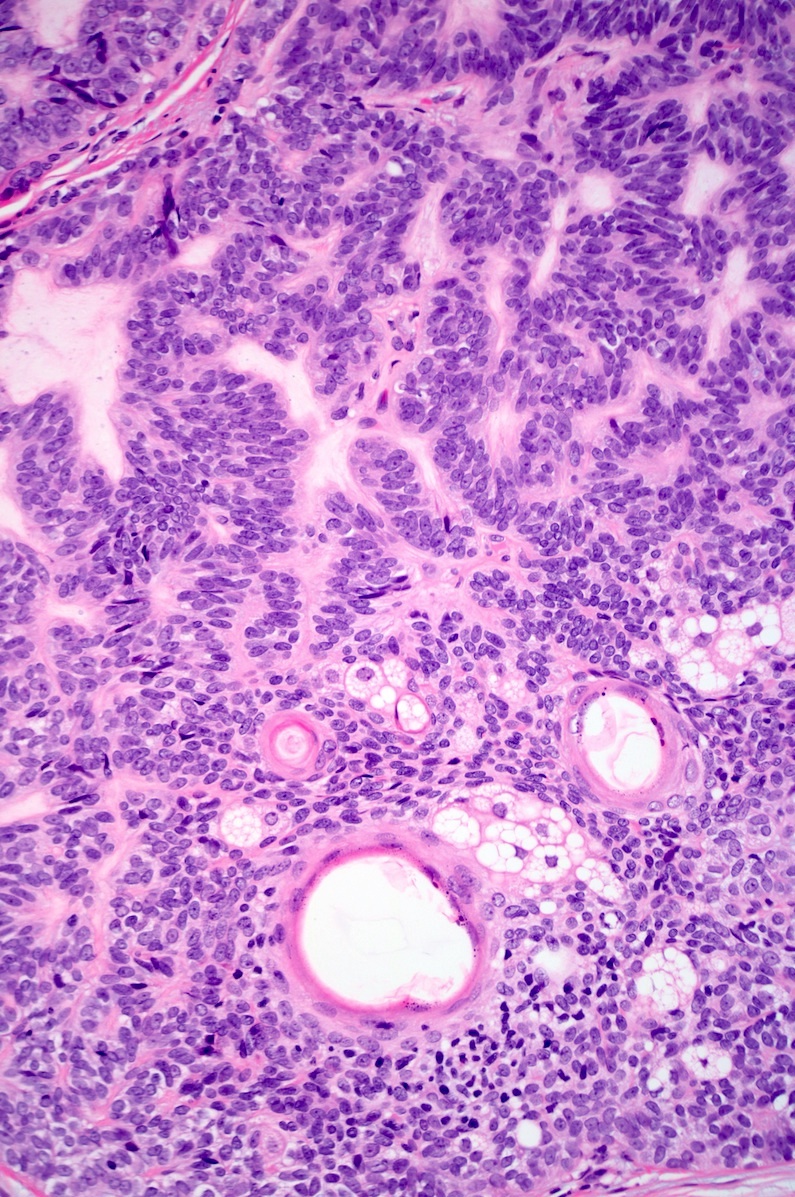
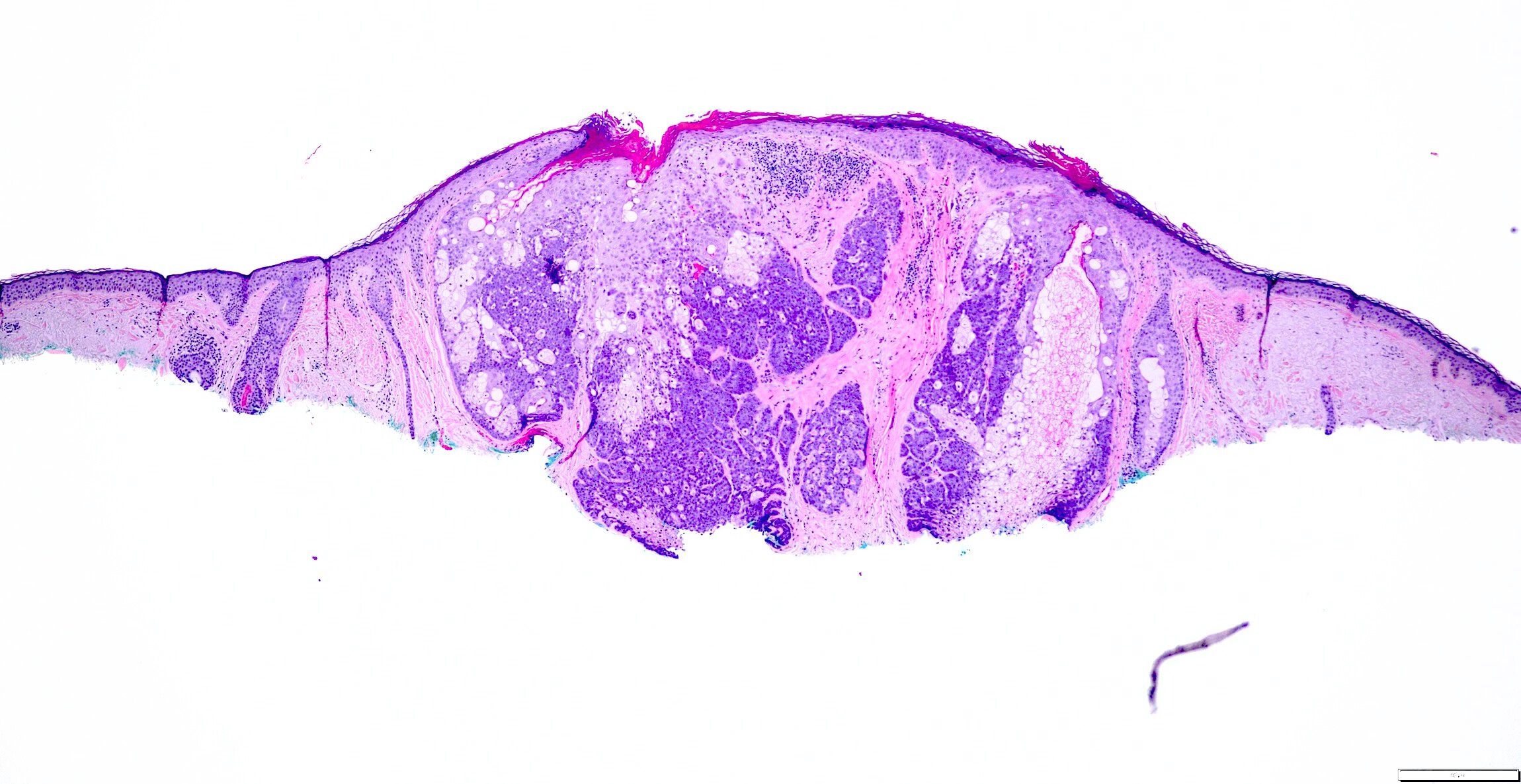
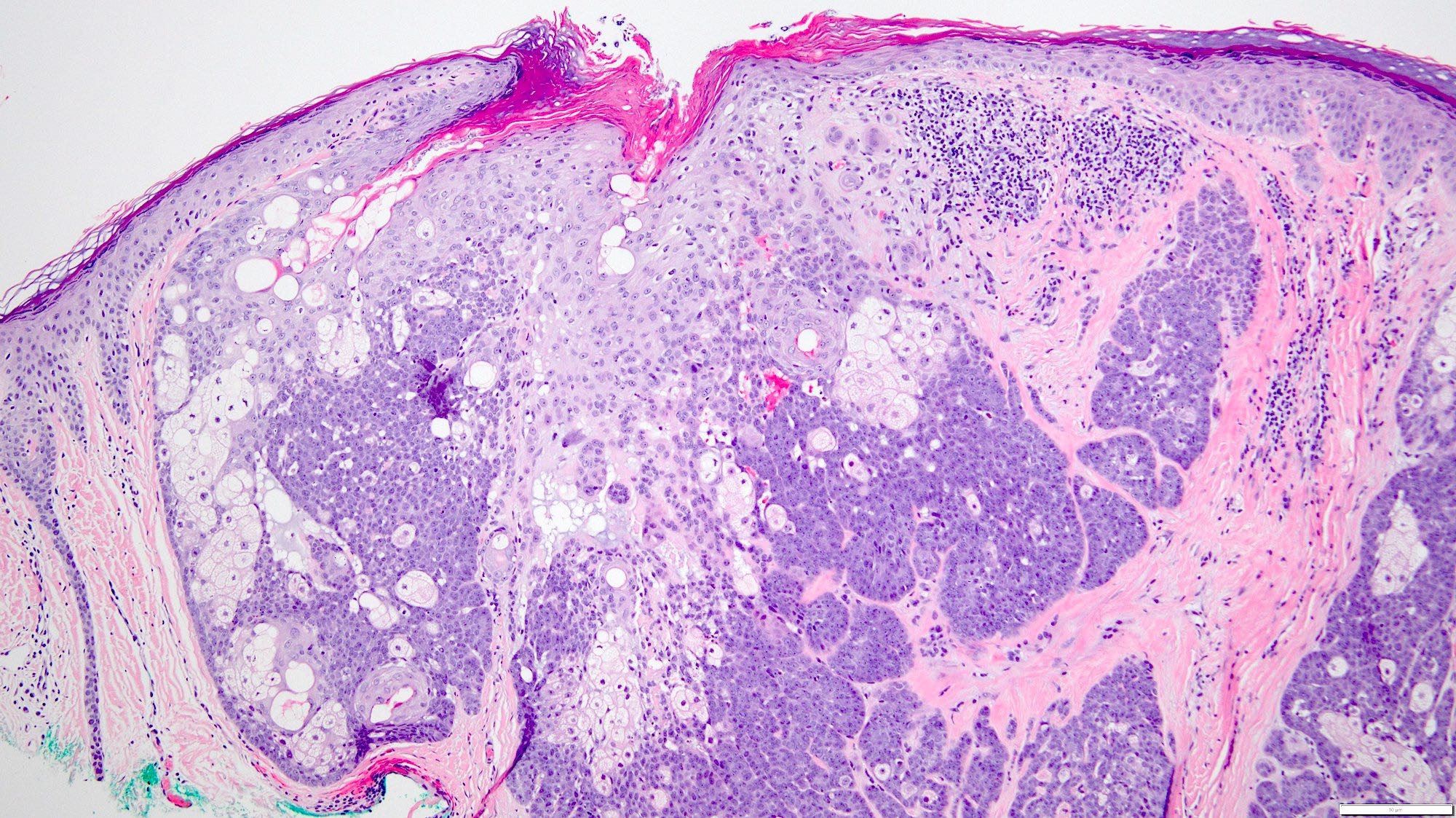
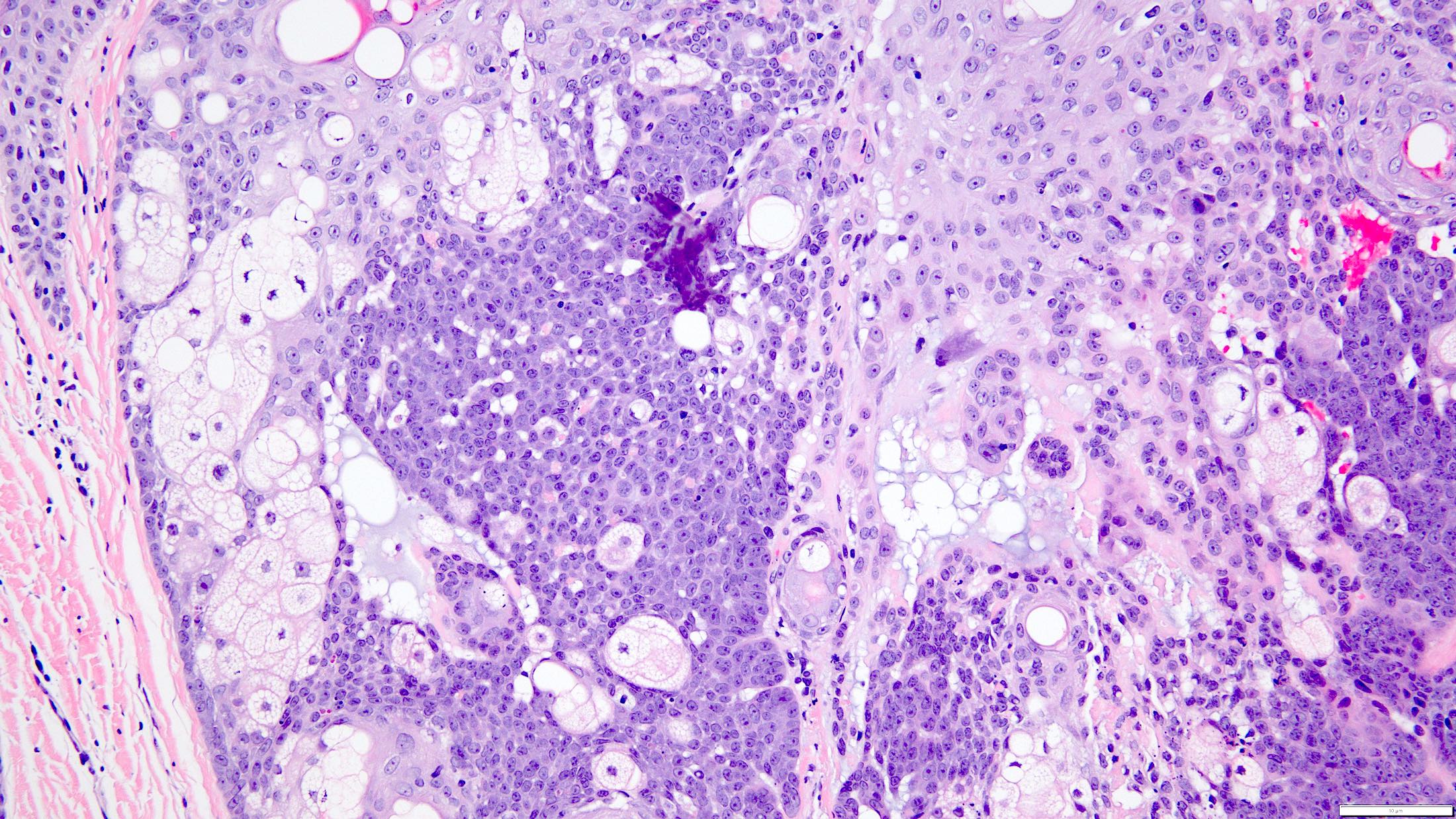
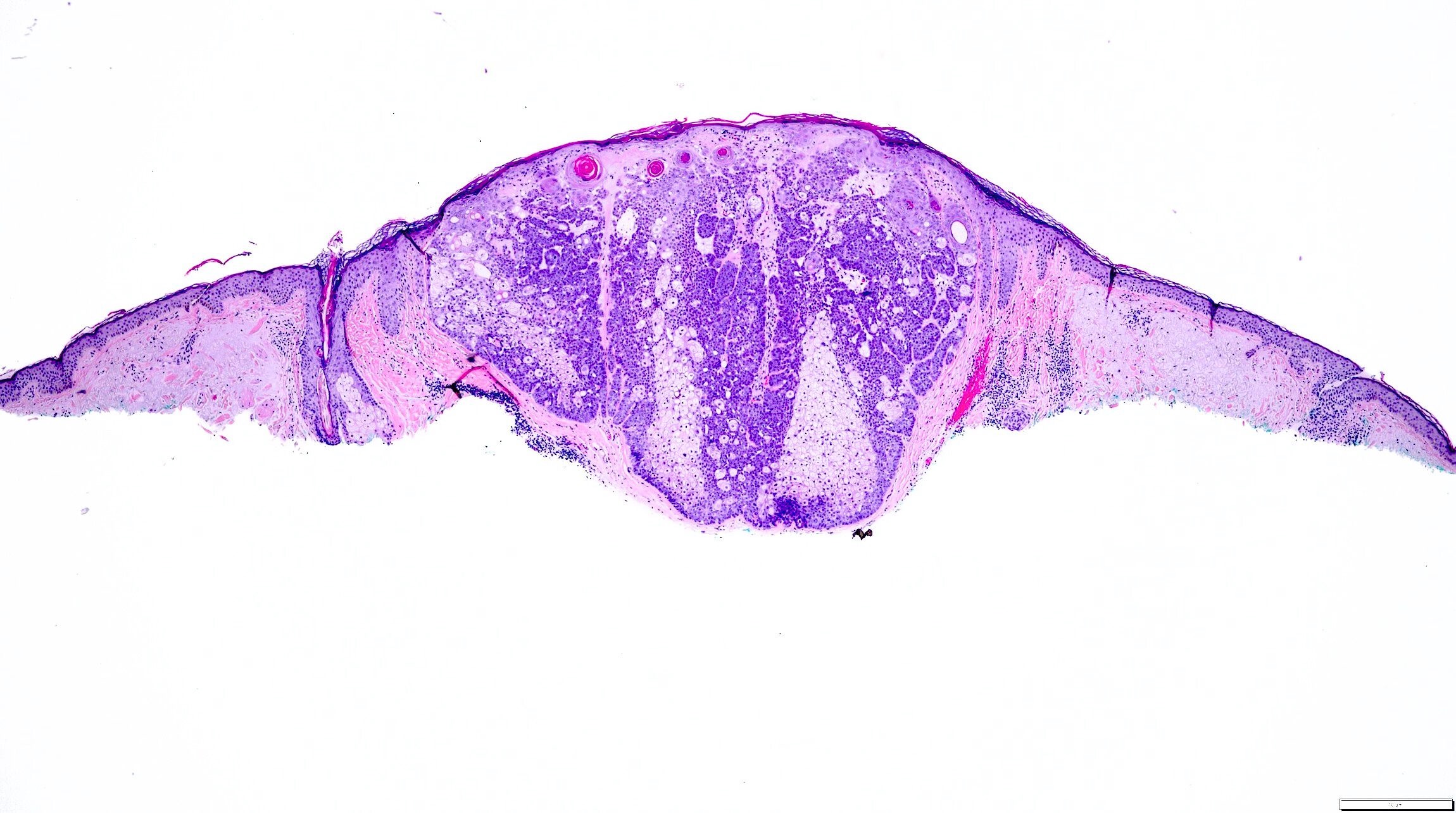
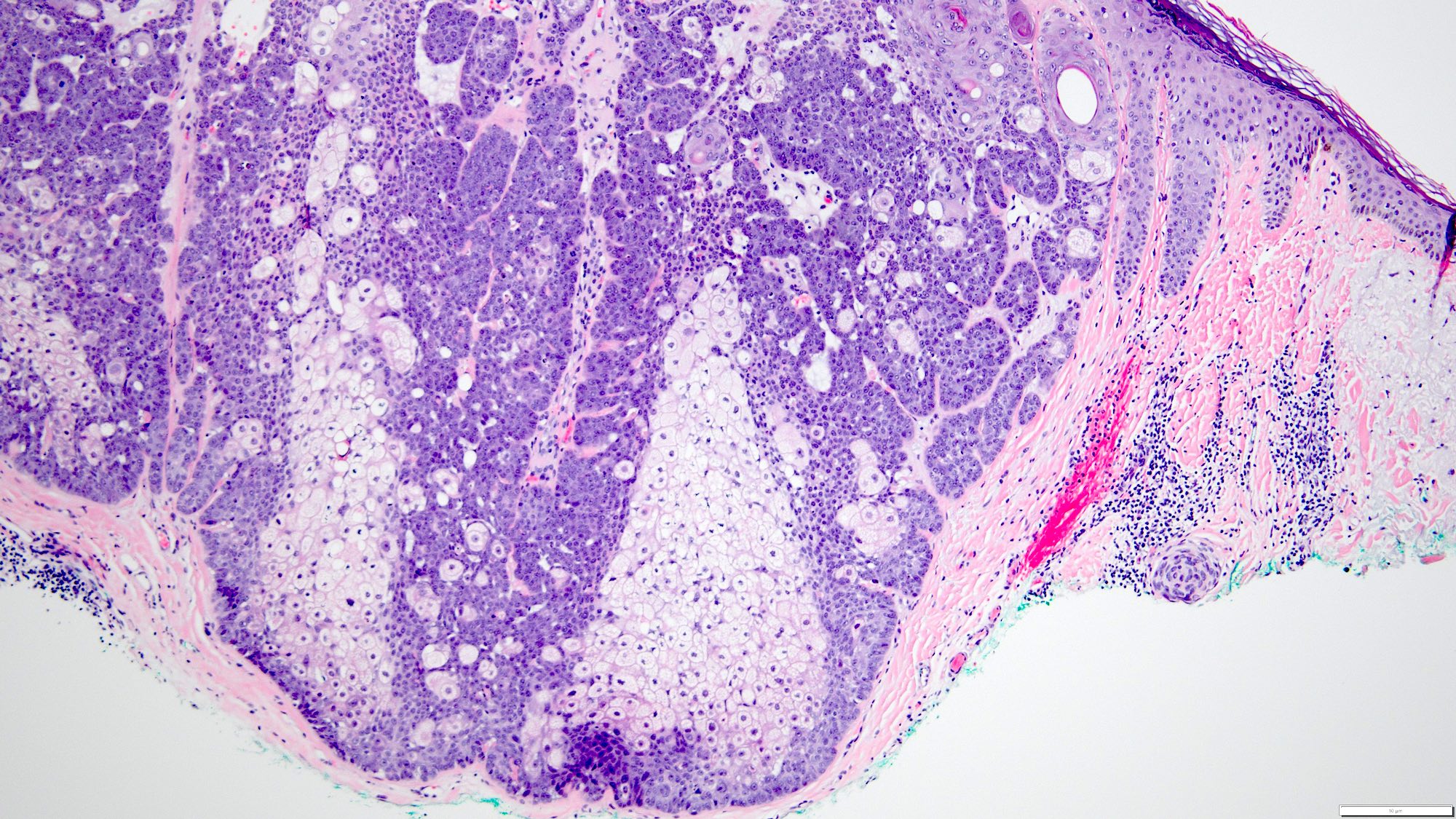
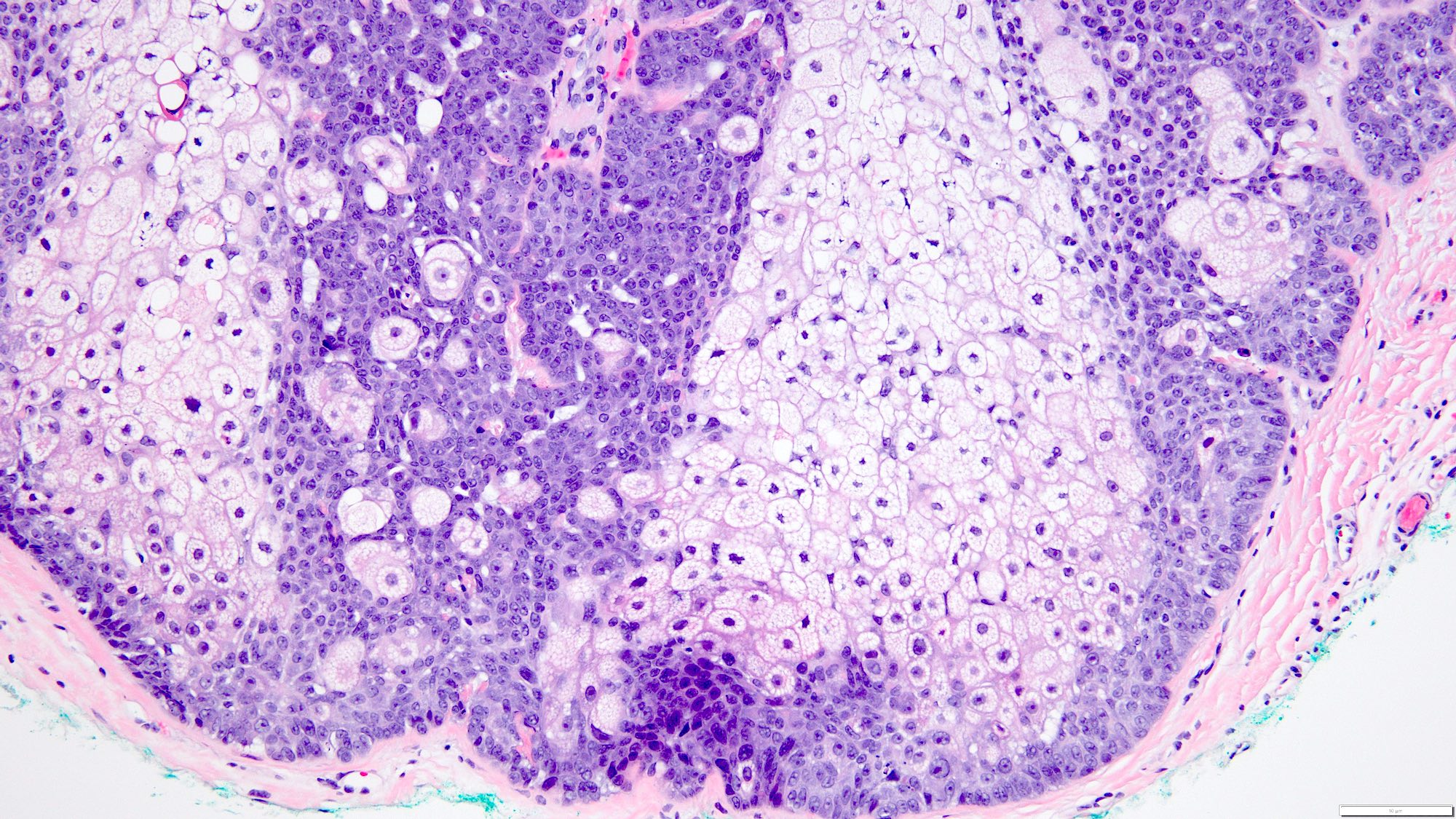
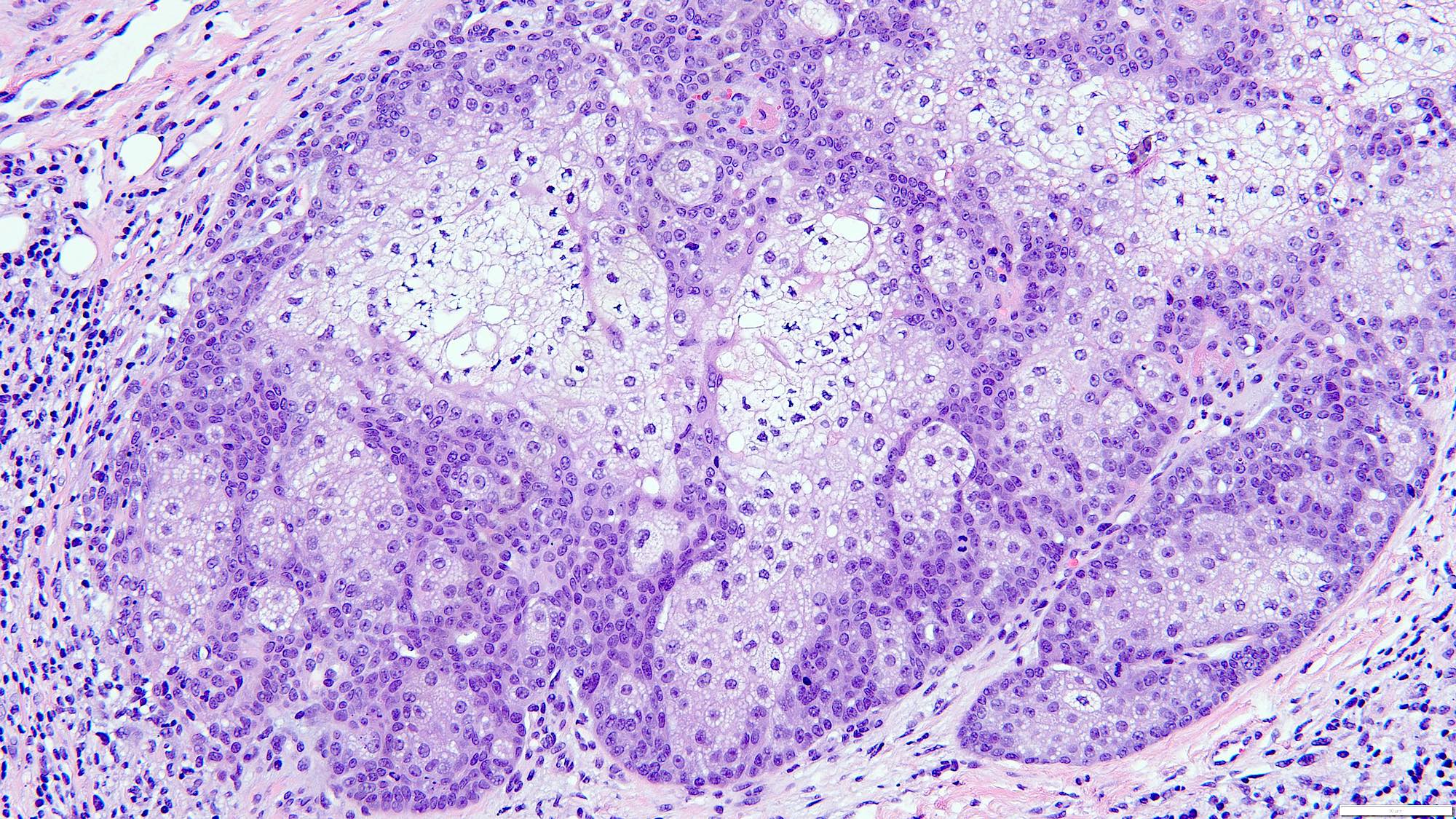
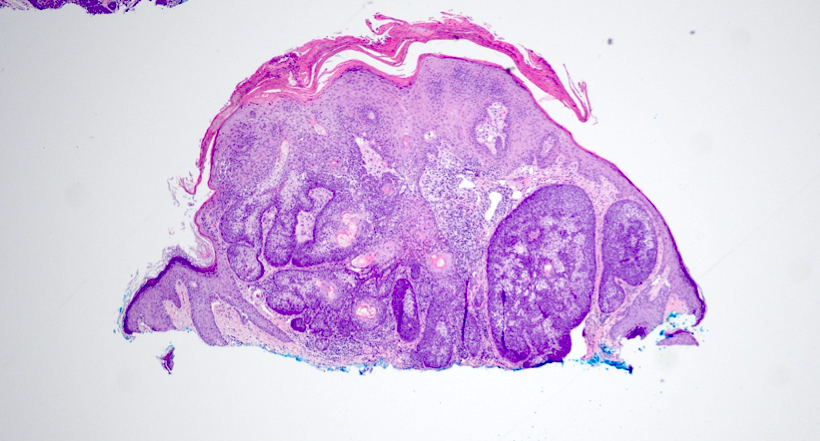
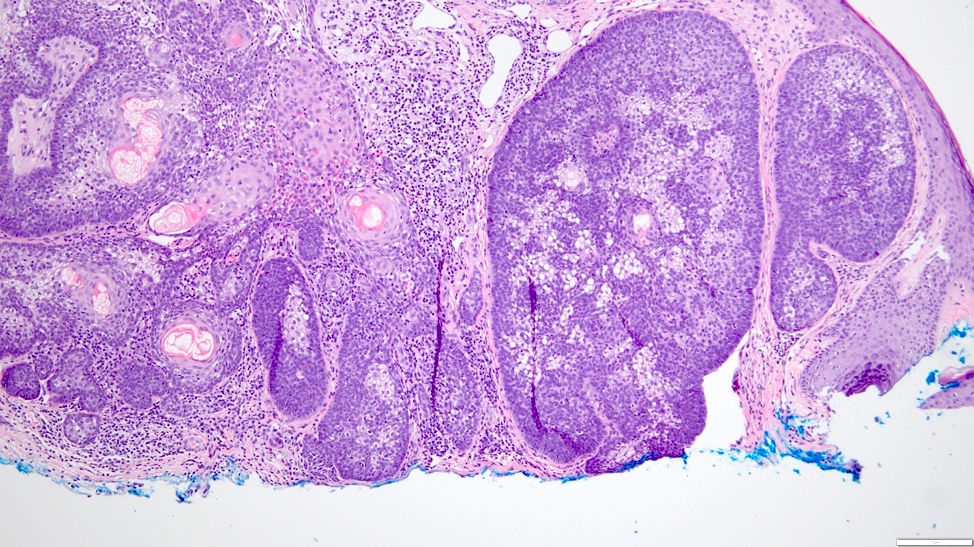
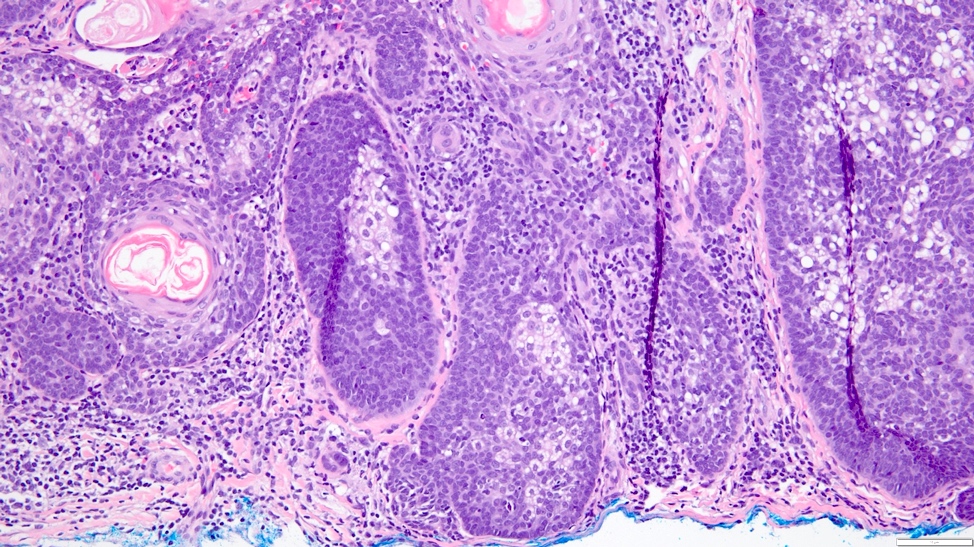
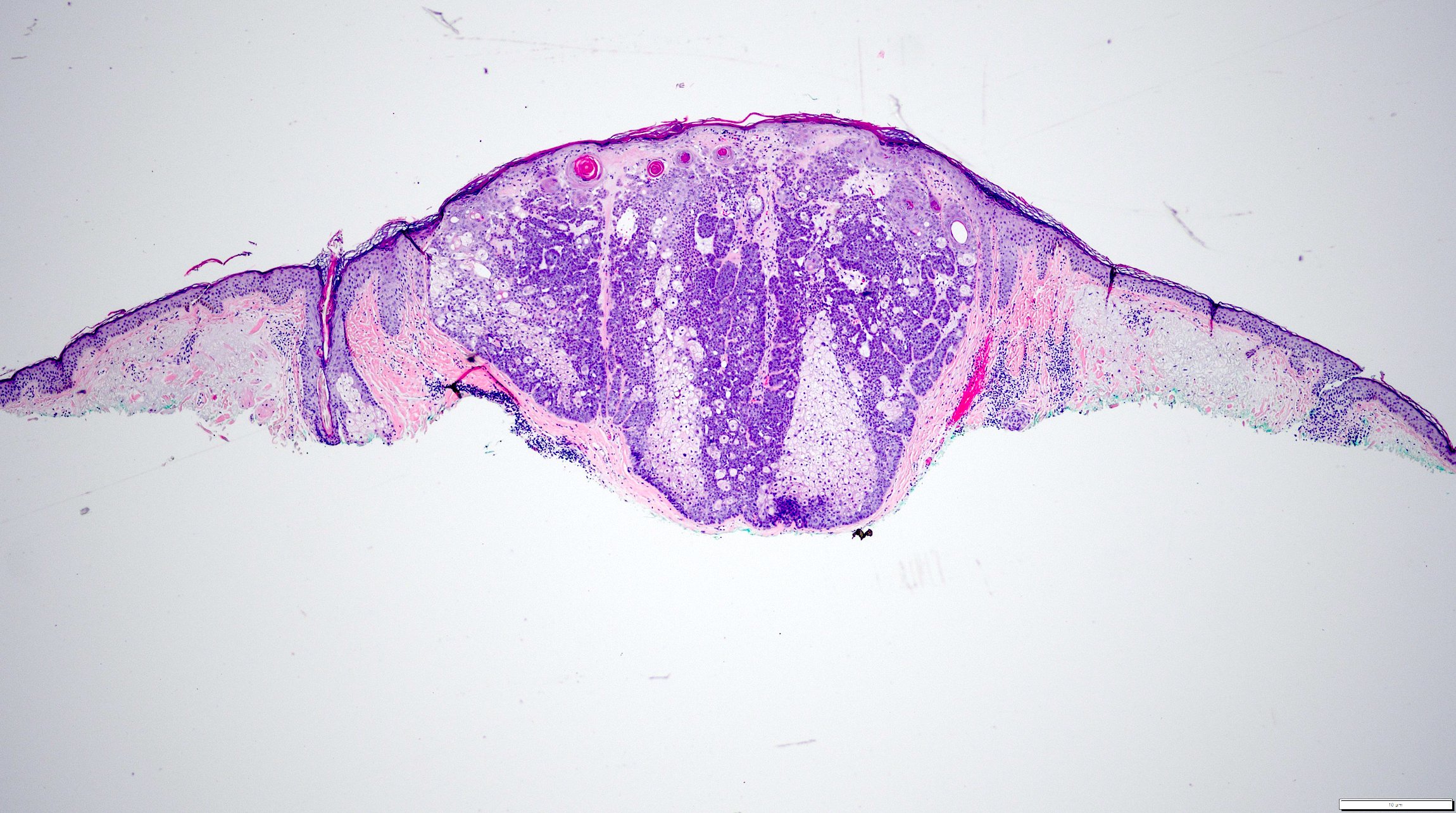
Microscopic (histologic) description
- Dermal based tumor with rare epidermal attachments
- Consists of variably sized, discrete nodules that lack lobular organization architecture (Am J Dermatopathol 1984;6:7, Am J Dermatopathol 2002;24:294, Am J Dermatopathol 2001;23:58, J Am Acad Dermatol 1990;22:533)
- Cytologically, the sebocytes have multiple cytoplasmic vacuoles and scalloped nuclei; the immature basaloid component features frequent mitotic activity but lacks atypical forms or necrosis
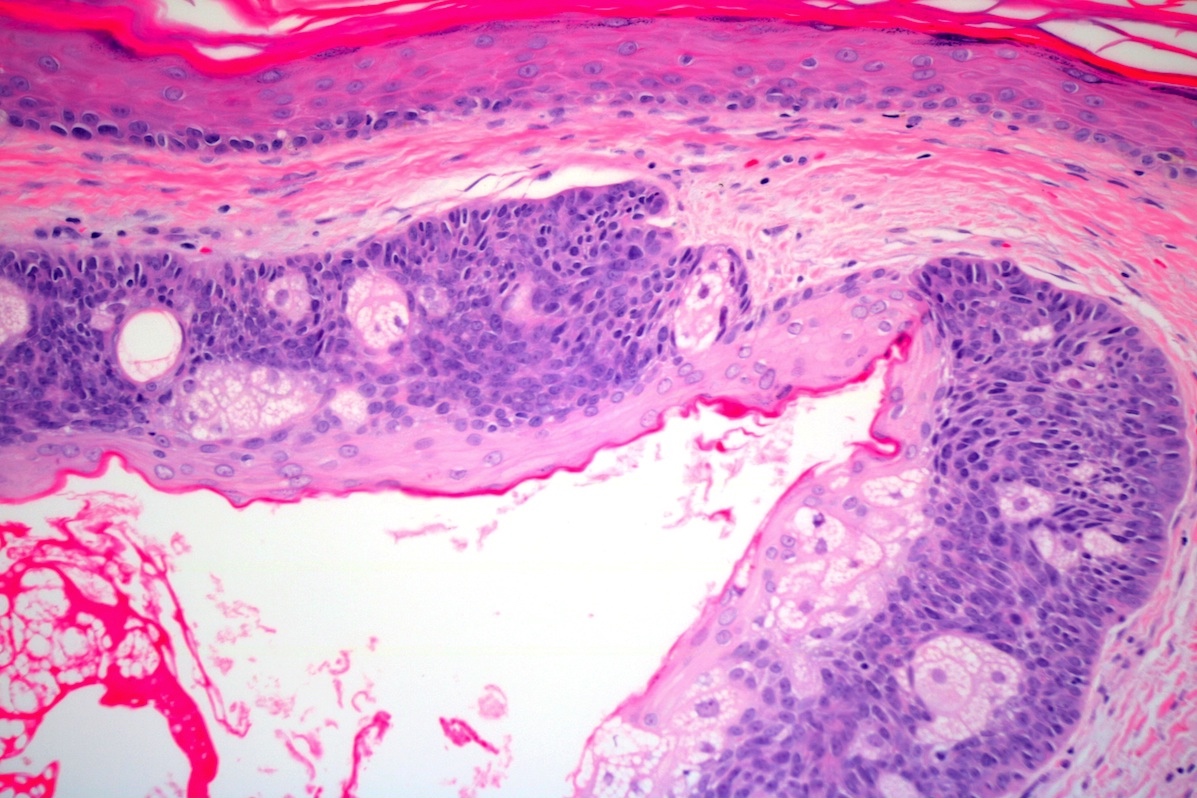
- Cystic spaces and duct-like structures are often present, displaying an eosinophilic cuticle and occasional holocrine secretions (Surg Pathol Clin 2017;10:367, Ann Dermatol Venereol 2016;143:814, Am J Dermatopathol 1984;6:7)
- Moreover, apocrine differentiation, infundibulocystic structures and squamous metaplasia can also be seen (Am J Dermatopathol 2016;38:678)
- Based on the growth patterns, sebaceoma variants can be described as follows: reticulated (rippled), cribriform, sinusoidal / labyrinthine, carcinoid-like and glandular (Dermatol Online J 2016;22:13030, Am J Dermatopathol 2009;31:364, Ann Dermatol Venereol 2016;143:814, Am J Dermatopathol 2005;27:195, Am J Dermatopathol 2018;40:479)
- > 1 configuration may be present within the same neoplasm
- MMR deficient sebaceous neoplasms more often show cystic change, intratumoral mucin, squamous metaplasia, ulceration, a lymphocytic infiltrate and intertumoral heterogeneity compared to MMR stable sebaceous neoplasms (Am J Dermatopathol 2021;43:174)
Microscopic (histologic) images
Contributed by Jerad Gardner, M.D., Jennifer Kaley, M.D., Yazan Alhalaseh, M.D. and Dinesh Pradhan, M.D.
Virtual slides
Positive stains
Negative stains
- BerEP4 is negative in sebaceoma (as compared to basal cell carcinoma [BCC], which has positive BerEP4) (Histopathology 2007;51:80)
- Low p53 and Ki67 profile as compared to sebaceous carcinoma, which has diffuse p53 expression and high Ki67 proliferation rate (N Am J Med Sci 2015;7:275)
- MLH1, MSH2 and MSH6 may be lost in patients with Muir-Torre syndrome
Videos
Muir-Torre syndrome
Sample pathology report
- Skin, scalp nodule, biopsy:
- Sebaceoma
Differential diagnosis
- Basal cell carcinoma with sebaceous differentiation:
- Predominantly shows peripheral palisading, mucinous stroma and retraction artifact with incidental sebaceous differentiation
- BerEP4 staining is positive in basal cell carcinoma and negative in sebaceoma (Histopathology 2007;51:80)
- EMA and D2-40 are negative in BCC
- Sebaceous adenoma:
- Preserved lobular architecture with distinct and regular maturation (similar to the normal sebaceous gland)
- Tumor with < 50% basaloid cells, as opposed to a sebaceoma, which has > 50% basaloid cells
- Sebaceous carcinoma:
- Has more nuclear pleomorphism, nucleolar prominence, mitotic activity and infiltrative growth pattern, as compared to sebaceoma
- Diffuse p53 expression and high Ki67 proliferation rate (N Am J Med Sci 2015;7:275)
- Trichoblastoma with sebaceous differentiation:
- Look for focal hair differentiation and papillary mesenchymal bodies
Additional references
Board review style question #1
Which immunohistochemical stain favors a diagnosis of basal cell carcinoma (BCC) with sebaceous differentiation over sebaceoma?
- BerEP4
- D2-40
- EMA
- Factor XIIIa
Board review style answer #1
A. BerEP4. BerEP4 is the only choice that is positive in BCC with sebaceous differentiation. Answers B, C and D are incorrect because EMA, D2-40 and factor XIII are negative in BCC with sebaceous differentiation and positive in sebaceoma.
Comment Here
Reference: Sebaceoma
Comment Here
Reference: Sebaceoma
Board review style question #2
Which immunohistochemical stain is helpful in distinguishing sebaceoma from sebaceous carcinoma?
- Adipophilin
- Androgen receptor
- CK7
- EMA
- p53 and Ki67
Board review style answer #2
E. p53 and Ki67. Diffuse p53 expression and a high Ki67 support a diagnosis of sebaceous carcinoma whereas low p53 expression and low Ki67 favor a diagnosis of sebaceoma. Answers A - D are incorrect because these stains are positive in both sebaceoma and sebaceous carcinoma.
Comment Here
Reference: Sebaceoma
Comment Here
Reference: Sebaceoma
Board review style question #3
Board review style question #3
B. Sebaceoma. The histologic sections show well circumscribed cellular lobules composed of predominant immature basaloid cells (> 50% of the lesion) with admixed mature sebocytes. Answer A is incorrect because the clear cell component displays features of sebaceous differentiation. Answer C is incorrect because sebaceous adenoma has > 50% mature sebocytes and < 50% basaloid components. Answer D (sebaceous carcinoma) is incorrect because the tumor cells lack atypia and necrosis and have low mitotic activity.
Comment Here
Reference: Sebaceoma
Comment Here
Reference: Sebaceoma