Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khazaeli M, Motaparthi K. Syringocystadenoma papilliferum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticpapillarysyringadenoma.html. Accessed April 2nd, 2025.
Definition / general
- Benign, hamartomatous, adnexal tumor (J Clin Diagn Res 2014;8:QD03)
- Originates from the apocrine or the eccrine sweat glands (J Clin Diagn Res 2013;7:742)
Essential features
- Benign adnexal tumor, most commonly occurring in the head and neck in early childhood (J Dermatol 2004;31:939)
- Most are solitary papules but variable clinical presentation
- Macroscopic: pink, hairless plaque or nodule
- Microscopic: cystic invaginations of the infundibular epithelium extending into the dermis with a double cell layer of inner columnar and outer cuboidal cells
Terminology
- Syringocystadenoma papilliferum (SCAP), also known as papillary syringadenoma (J Clin Diagn Res 2014;8:QD03)
Epidemiology
- M = F (Indian J Dermatol Venereol Leprol 2009;75:170)
- 50% of cases present at birth or in early childhood (Onco Targets Ther 2013;6:233)
- 15 - 30% of cases develop during puberty (Onco Targets Ther 2013;6:233)
Sites
- 75% of cases are reported in the head and neck region (Indian J Dermatol Venereol Leprol 2009;75:170)
- Unusual locations: buttock, vulva and scrotum, pinna, eyelid, outer ear canal, postoperative scar, scalp, nipple, thigh, axilla, back and right lower abdomen (3 cases) (J Clin Diagn Res 2014;8:QD03)
Pathophysiology
- Benign hamartomatous adnexal tumor (J Clin Diagn Res 2014;8:QD03)
- Origin is uncertain:
- Derived from apocrine glands, eccrine glands or both:
- Immunohistochemical studies support an apocrine origin (J Clin Diagn Res 2014;8:QD03)
- Ultrastructural analysis favors an eccrine derivation (J Clin Diagn Res 2014;8:QD03)
- May arise from pluripotent stem cells (J Clin Diagn Res 2014;8:QD03)
- Derived from apocrine glands, eccrine glands or both:
- During puberty, may increase in size and develop a crusted and papillomatous texture (Br J Dermatol 2000;142:543)
- Although benign, co-occurrence of basal cell carcinoma, verrucous carcinoma metastatic adenocarcinoma and ductal carcinoma may be observed (Onco Targets Ther 2013;6:233, OrphaNet: Syringocystadenoma Papilliferum [Accessed 5 November 2021])
Etiology
- Often observed in association with other benign adnexal neoplasms, such as nevus sebaceus (8 - 19% of patients), apocrine nevus, tubular apocrine adenoma, apocrine hidrocystoma, apocrine cystadenoma and clear cell syringoma (Pathologica 2006;98:178)
Clinical features
- Measures between 1 - 3 cm and < 4 cm in diameter (J Clin Diagn Res 2013;7:742)
- Variable clinical presentation:
- Solitary papule
- Linear arrangement of several papules (Onco Targets Ther 2013;6:233)
- Most patients present with solitary lesions in the head and neck region at birth or in early childhood (J Clin Diagn Res 2014;8:QD03)
- Variable presentations:
- Warty plaques on the head and neck (J Clin Diagn Res 2014;8:QD03)
- Papule or a smooth hairless plaque on the scalp and forehead (Indian J Dermatol Venereol Leprol 2009;75:170)
- Often in the setting of nevus sebaceus (J Clin Diagn Res 2014;8:QD03)
- Nodular or verrucous transformation is noted at puberty (Indian J Dermatol Venereol Leprol 2009;75:170)
- Multiple lesions are rarely seen and those that arise outside the head and neck region are even more uncommon (J Clin Diagn Res 2014;8:QD03)
- With increasing size:
- More prominent papillary configuration develops (Onco Targets Ther 2013;6:233)
- Surface can develop hemorrhagic crust (Onco Targets Ther 2013;6:233)
Diagnosis
- Skin biopsy
Case reports
- 6 year old boy with progressive growth lesion on left flank (An Bras Dermatol 2020;95:112)
- 25 year old man with a 10 year history of an asymptomatic, slowly growing skin lesion on face (Case Rep Dermatol 2019;11:36)
- 45 year old woman with a right supraclavicular lesion since childhood (J Nippon Med Sch 2017;84:79)
- 56 year old woman with a swelling lesion on right temporal scalp (Malays J Pathol 2019;41:47)
- 64 year old man with a growing mass on left occipital scalp (Case Rep Pathol 2019;2019:1783758)
Treatment
- Surgical excision (J Cutan Aesthet Surg 2016;9:204)
Clinical images
Gross description
- Macroscopic:
- Skin colored to pink, hairless, firm plaque of grouped nodules or as a solitary nodule
- Verrucous, papillary, hyperkeratotic, moist or fleshy excrescences have also been described (Onco Targets Ther 2013;6:233)
- Some tumors may show central umbilication through which small fistulae may discharge fluid (Onco Targets Ther 2013;6:233)
- Mature lesions:
- Clusters of pinkish brown nodules (Onco Targets Ther 2013;6:233)
- 2 - 10 mm in diameter (Onco Targets Ther 2013;6:233)
- Occasional central opening (Onco Targets Ther 2013;6:233)
- Skin colored to pink, hairless, firm plaque of grouped nodules or as a solitary nodule
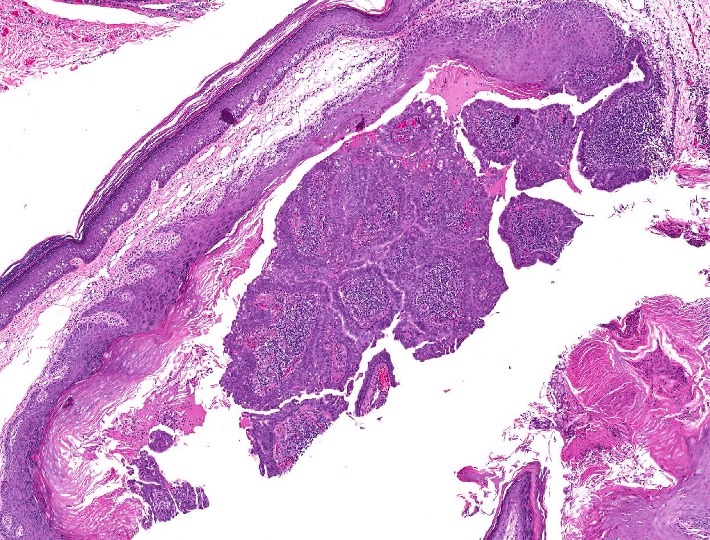
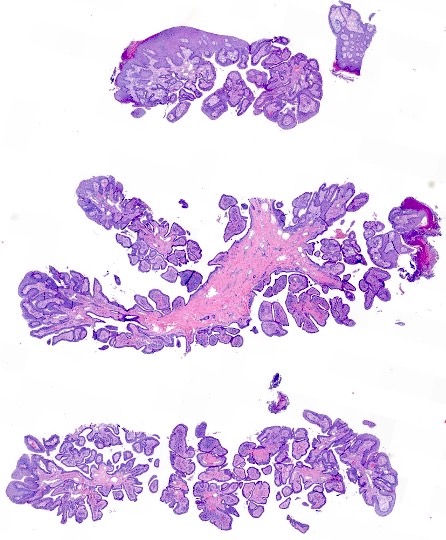
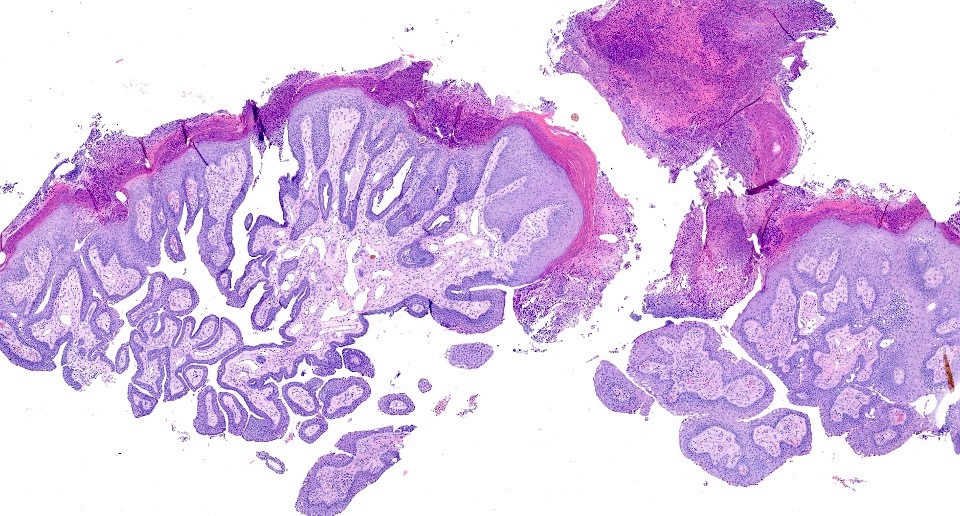
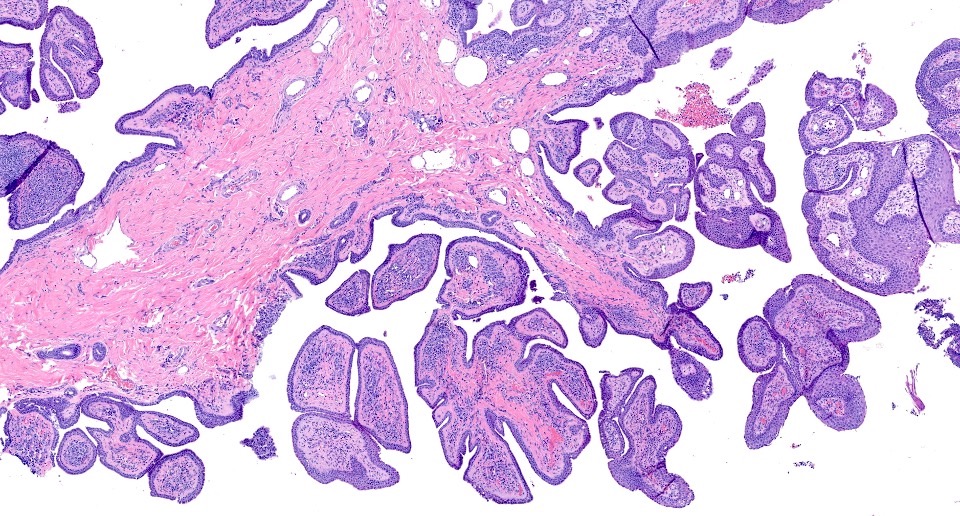
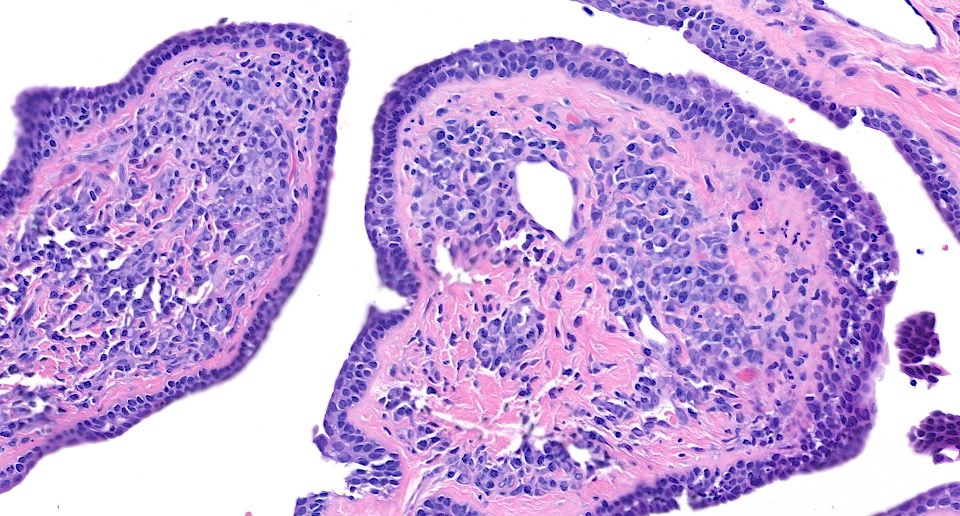
Microscopic (histologic) description
- Cystic invaginations of the infundibular epithelium projecting into the dermis, covered by a double cell layer (An Bras Dermatol 2017;92:721, J Clin Diagn Res 2014;8:QD03):
- Innermost layer is composed of columnar cells with decapitation secretion
- Outermost layer is composed of cuboidal cells with papillary projections
- Verrucous (papillomatous) epidermal hyperplasia with hyperkeratosis and hypergranulosis (Pathologica 2006;98:178)
- Exoendophytic configuration with a gradual transition from stratified squamous epithelium at the epidermal surface to a bilayered ductal epithelium (Pathologica 2006;98:178)
- Papillary fronds extend upward from the base and plasma cells are common in the stroma of each frond (Pathologica 2006;98:178)
- Many irregular duct-like structures and cystic spaces (Pathologica 2006;98:178)
- Ducts, containing papillary processes and lined by 2 epithelial cell layers, connect to the surface (Indian J Dermatol Venereol Leprol 2009;75:170)
- Exoendophytic architecture, verrucous epidermal hyperplasia, sometimes pseudoepitheliomatous hyperplasia and connection of glands to epidermis (An Bras Dermatol 2017;92:721)
- Background features of nevus sebaceus may be observed (An Bras Dermatol 2017;92:721)
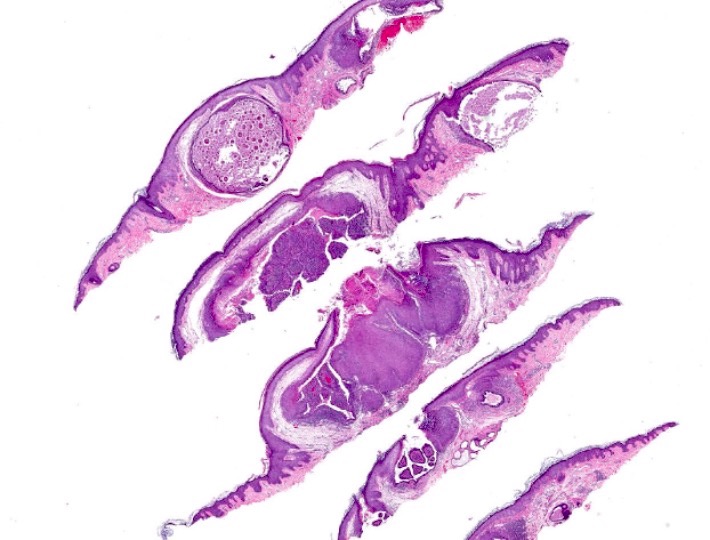
Microscopic (histologic) images
Positive stains
- IHC may help in favoring eccrine or apocrine lineage but is not required for diagnosis (Indian J Dermatol 2013;58:409)
- Positive stains:
- CEA, AE1 / AE3 and EMA highlight ductal epithelium (Indian J Dermatol 2013;58:409)
- Luminal columnar cells:
- Positive for CK7 (Br J Dermatol 2002;147:936)
- > 70% positive for CK19 (Br J Dermatol 2002;147:936)
- CK1, CK5, CK8, CK10, CK14: heterogeneous expression (Br J Dermatol 2002;147:936)
- Basal cuboidal cells:
- Almost constantly express CK1, CK5, CK7, CK8, CK10, CK14 (Br J Dermatol 2002;147:936)
- Basal tumor cells express CK19 and vimentin heterogeneously and alpha smooth muscle actin focally (Br J Dermatol 2002;147:936)
- Positive for SMA, CK5/6 and p63, consistent with myoepithelial differentiation
Molecular / cytogenetics description
- Some cases have mutations in:
- Patched gene (PTCH) (Indian J Dermatol 2013;58:409)
- p16 tumor suppressor gene (Indian J Dermatol 2013;58:409)
Sample pathology report
- Scalp, biopsy:
- Syringocystadenoma papilliferum (see comment)
- Comment: Several cystic invaginations arise from a papillomatous epidermis. These invaginations demonstrate papillae lined by 2 rows of cuboidal to columnar epithelial cells, with oval nuclei and a pale eosinophilic cytoplasm. The deep dermis contains tubular glands with apocrine decapitation secretion. The stroma contains a dense mononuclear infiltrate, which is comprised predominantly of plasma cells.
Differential diagnosis
- Hidradenoma papilliferum:
- Almost exclusively occurs in the anogenital region of women; diagnosis outside of this site should be exceptional (J Clin Diagn Res 2014;8:QD03)
- Unlike syringocystadenoma papilliferum, there is no epidermal connection (it hides in the dermis) (J Clin Diagn Res 2014;8:QD03)
- Dermal nodule that consists of arborizing ducts that produce maze-like patterns (J Clin Diagn Res 2014;8:QD03)
- Papillary eccrine adenoma:
- Composed of multiple, dermal, dilated, duct-like spaces containing papillary projections (J Clin Diagn Res 2014;8:QD03)
- No exoendophytic architecture, glands appear cystic, no epidermal connection and lacks plasmacellular stroma
- Warty dyskeratoma:
- Exoendophytic architecture and verrucous epidermal hyperplasia but lacks ductal epithelium
- Lined by elongated dermal papillae with suprabasilar acantholysis of keratinocytes, some of which are dyskeratotic (J Clin Diagn Res 2014;8:QD03)
- Tubular apocrine adenoma:
- Predominantly cuboidal and columnar cells with or without secretions (J Cytol 2015;32:130)
- No epidermal connection
- Glands contain papillary projections and form cysts
- Syringocystadenocarcinoma papilliferum (J Korean Med Sci 2007;22:762):
- Nipple adenoma (and variant erosive adenomatosis of the nipple):
- Anatomic site permits differentiation
Board review style question #1
A 38 year old man presents with a verrucous nodule on the scalp, present for the past 12 years. Representative histopathology is shown in the above image. Which of the following statements is correct?
- More common in adulthood
- Represents a malignant adnexal tumor
- Subset of tumors have loss of heterozygosity for PTCH or p16
- Usually does not communicate with surface epithelium
Board review style answer #1
C. Subset of tumors have loss of heterozygosity for PTCH or p16
Comment Here
Reference: Syringocystadenoma papilliferum
Comment Here
Reference: Syringocystadenoma papilliferum
Board review style question #2
An 8 year old girl presents with a slowly growing, 3 cm, erythematous nodule with smooth surface on the left labium majus, present since birth. A biopsy is performed (see above image). Which of the following is most associated with this tumor?
- Basal cell carcinoma
- Merkel cell carcinoma
- Nevus sebaceus
- Squamous cell carcinoma
Board review style answer #2