Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ly TY. Cutaneous neuroendocrine carcinoma / Merkel cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticmerkelcell.html. Accessed March 30th, 2025.
Definition / general
- Merkel cell carcinoma (MCC) is an uncommon and highly aggressive primary cutaneous neuroendocrine carcinoma
Essential features
- Merkel cell carcinoma is a highly aggressive primary cutaneous neuroendocrine carcinoma primarily affecting elderly and immunosuppressed individuals
- Diagnosis requires microscopic evaluation as the clinical appearance is nonspecific and can mimic a variety of benign and malignant skin lesions
- There is emerging evidence of distinct Merkel cell polyomavirus associated and UV mediated oncogenetic pathways
- Distinction between primary cutaneous Merkel cell carcinoma and metastatic neuroendocrine carcinoma in the skin requires immunohistochemical and clinical pathologic correlation
Terminology
- Originally described as trabecular carcinoma by Toker in 1972
Epidemiology
- Primarily affects elderly Caucasians, seventh decade and older (J Am Acad Dermatol 2018;78:457)
- Rising incidence due to aging population and improved recognition (J Am Acad Dermatol 2018;78:457, Nat Rev Dis Primers 2017;3:17077)
- M > F (J Am Acad Dermatol 2018;78:457)
Sites
- Sun exposed skin: head and neck > extremities > trunk (J Cutan Pathol 2010;37:20)
Pathophysiology
- Emerging evidence of distinct oncogenetic pathways: majority of cases (up to ~80%) are associated with Merkel cell polyomavirus while minority are UV mediated (Eur J Cancer 2017;71:53)
Etiology
- Risk factors: advanced age, chronic sun exposure, fair skin, immune suppression (e.g. organ transplantation, HIV infection, chronic lymphocytic leukemia, autoimmunity) (Head Neck Pathol 2018;12:31)
Clinical features
- Painless and rapidly growing flesh colored or red-violaceous nodule
- AEIOU acronym for clinical characteristics (J Am Acad Dermatol 2008;58:375):
- Asymptomatic / lack of tenderness
- Expanding rapidly
- Immune suppression
- Older than age 50
- UV exposed site
Diagnosis
- Biopsy or surgical excision
- Distinction between primary cutaneous Merkel cell carcinoma and metastatic neuroendocrine carcinoma in the skin is based on the immunohistochemical profile of the tumor and clinical pathologic correlation (i.e. clinically exclude prior malignancy and potential noncutaneous sources of metastases)
Radiology description
- CT: isoattenuating or hyperattenuating areas in soft tissue
- MRI: enhances with contrast
- Fluorodeoxyglucose PET / CT: avid hypermetabolic activity (AJR Am J Roentgenol 2013;200:1186)
Prognostic factors
- Factors relevant to staging for Merkel cell carcinoma include tumor size, depth of invasion, locoregional nodal involvement and disseminated metastasis
- Negative clinical prognostic indicators: advanced disease stage at diagnosis (most important), age > 60, male gender, head and neck site, immunosuppression, Merkel cell polyomavirus negative subtype (Curr Opin Oncol 2019;31:72)
- ~60% present with local disease, ~30% with nodal disease and ~10% with distant disease (Ann Surg Oncol 2016;23:3564)
- High mortality
- Rarely, complete spontaneous regression of the tumor can occur (J Cutan Pathol 2016;43:1150)
Case reports
- 51 year old man with concurrent metastatic Merkel cell carcinoma and cutaneous squamous cell carcinoma in the same lymph node (Am J Dermatopathol 2019;41:e61)
- 54 year old man with primary retroperitoneal Merkel cell carcinoma (Int J Surg Case Rep 2016;19:21)
- 64 and 68 year old men, organ transplant recipients, with Merkel cell carcinoma (JAAD Case Rep 2015;1:S29)
- 65 year old man with primary Merkel cell carcinoma of the parotid gland diagnosed on cytopathology (Cytopathology 2017;28:552)
- 96 year old woman with spontaneous regression (Cutis 2018;101:301)
Treatment
- Multidisciplinary approach with wide local excision and sentinel lymph node biopsy in clinically node negative patients with or without adjuvant radiotherapy
- Emergence of immune checkpoint blockade therapy, targeting PDL1 / PD1 pathway, for advanced disease (N Engl J Med 2016;374:2542, Lancet Oncol 2016;17:1374)
- Chemotherapy generally ineffective and reserved for palliation
- Single modality radiotherapy for inoperable tumors
Gross description
- Fleshy to tan-brown lesion with nodular or ill defined silhouette
- Variable ulceration
Gross images
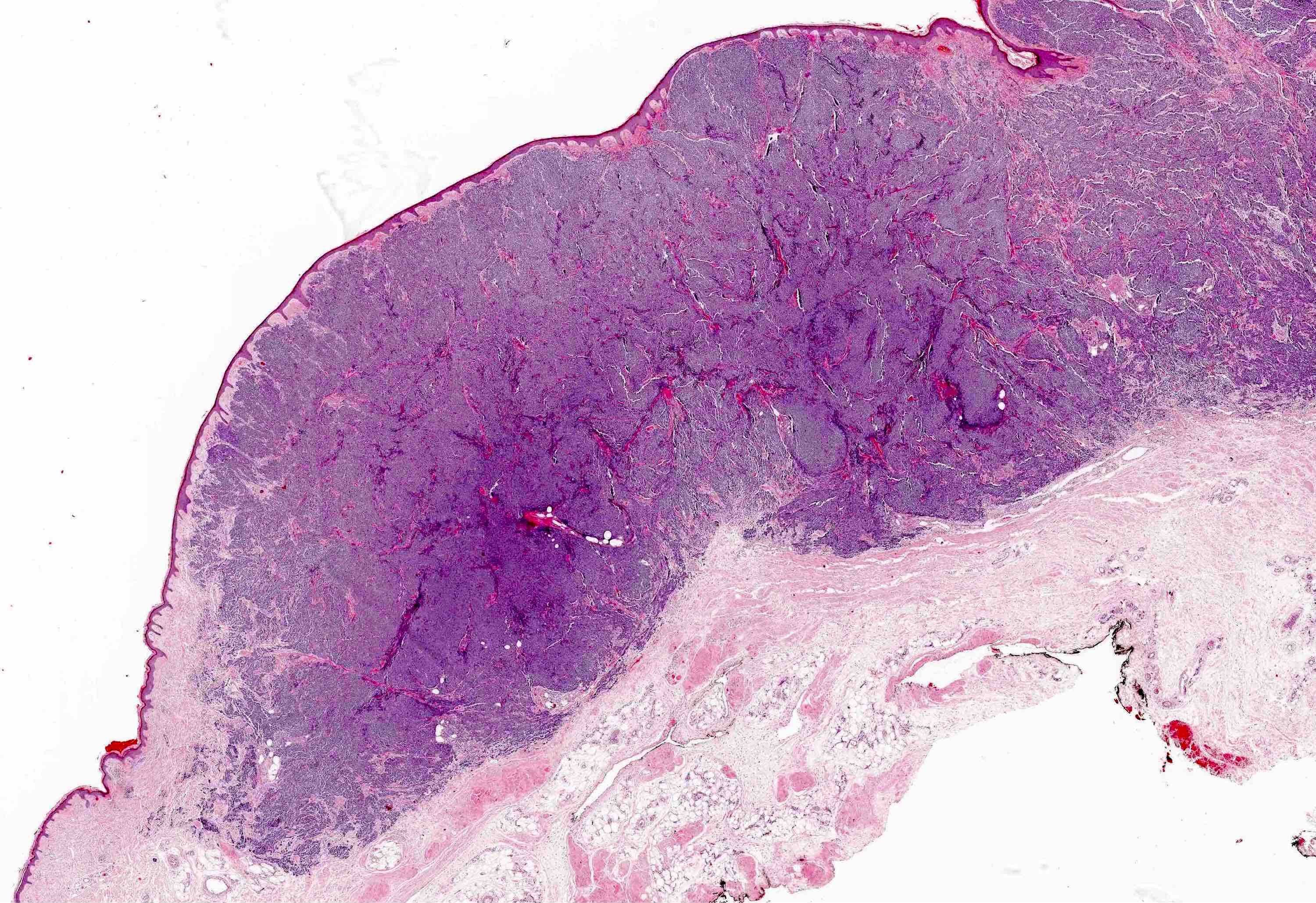
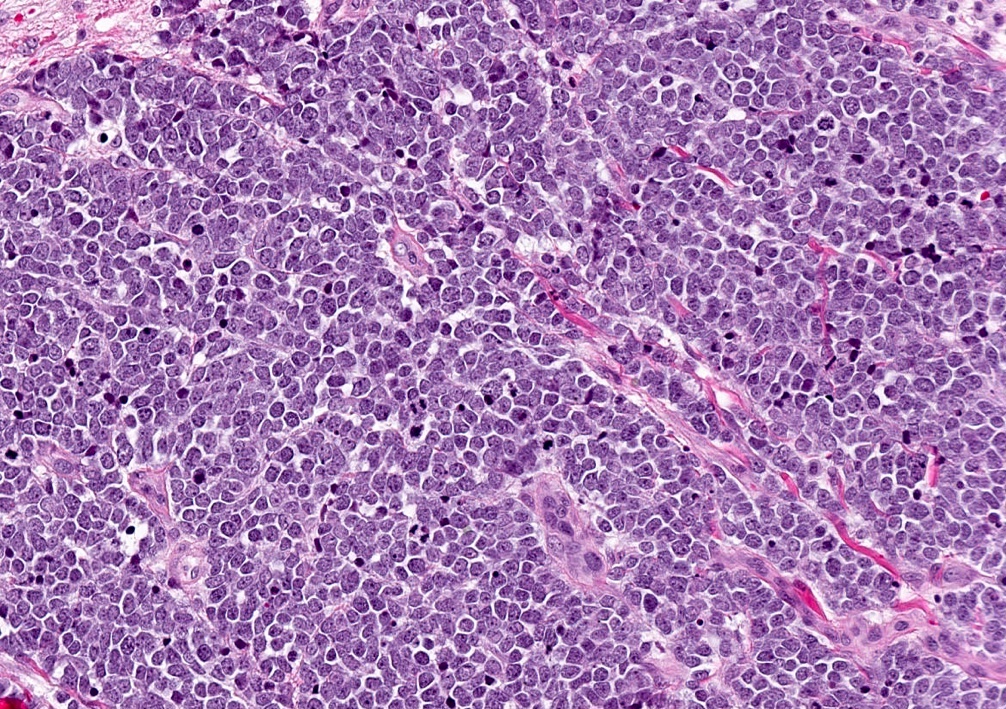
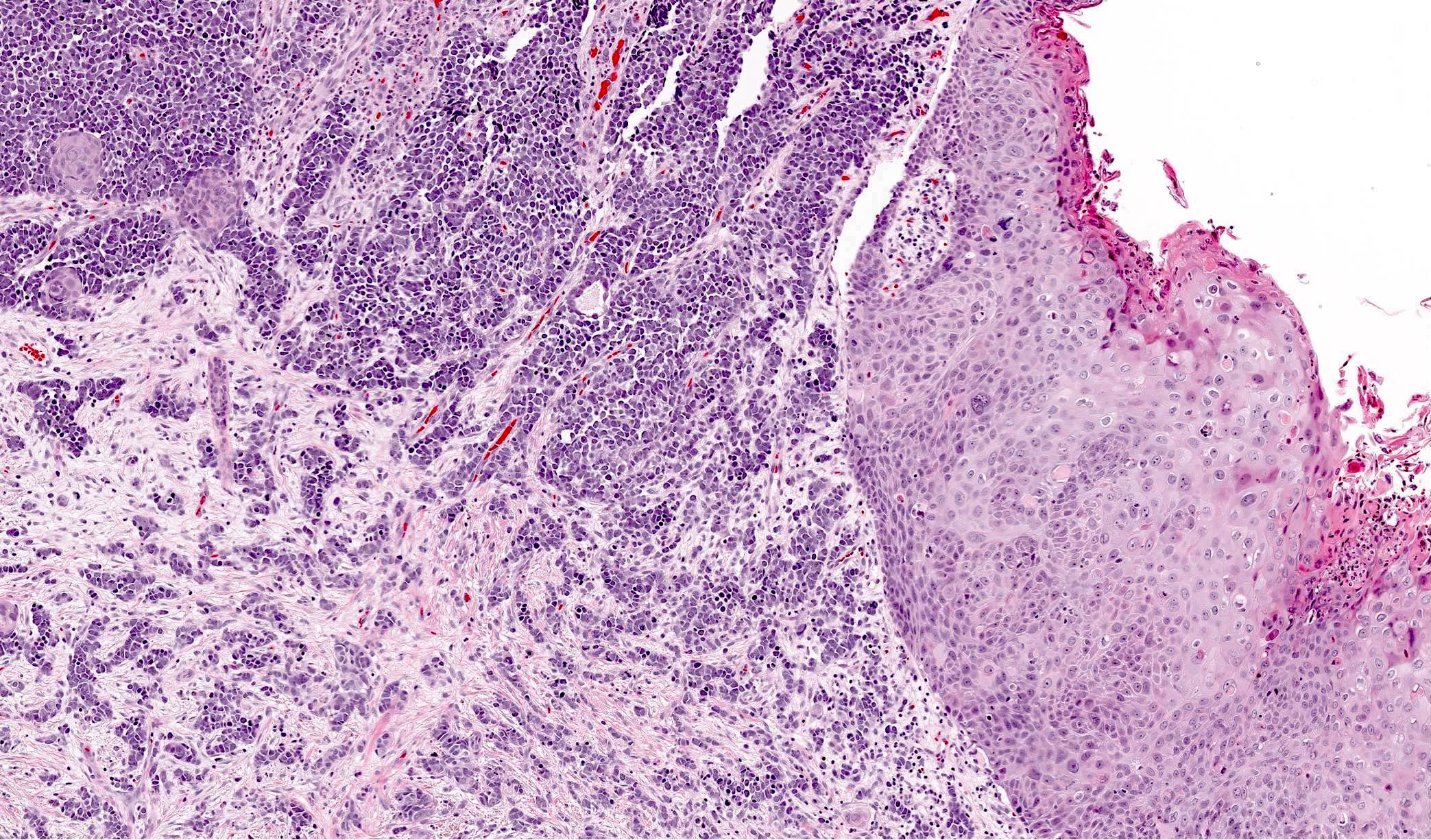
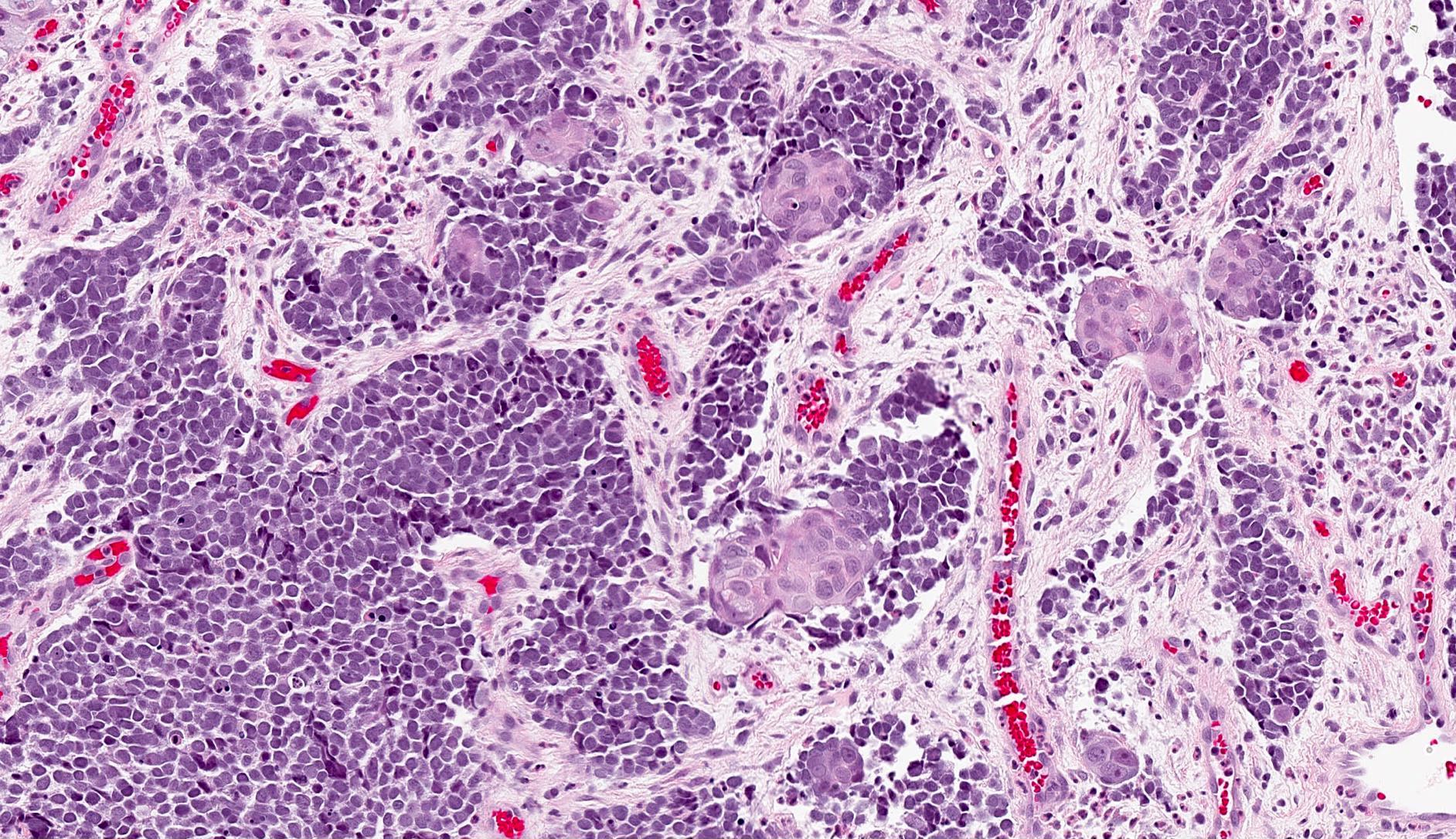
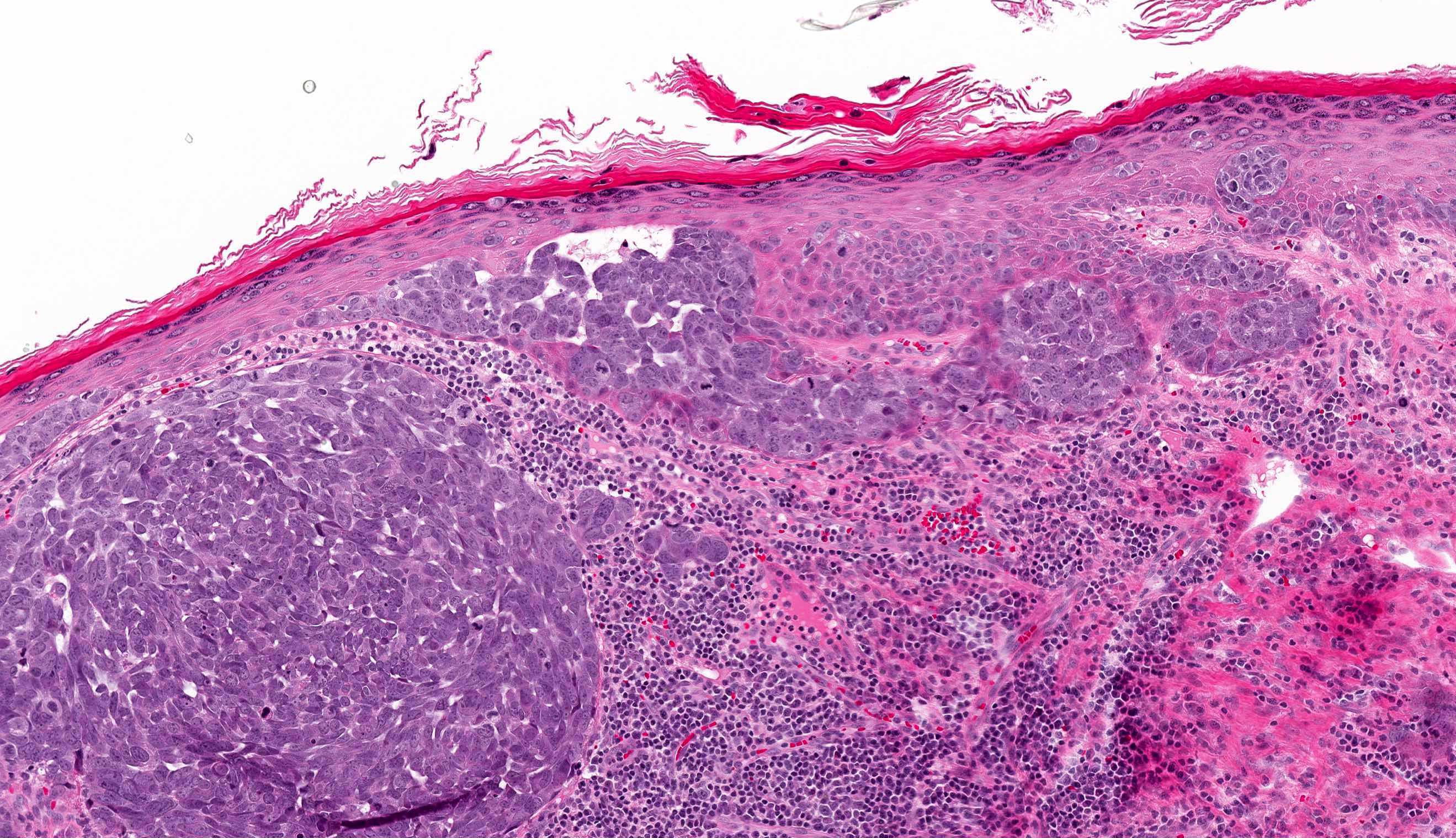
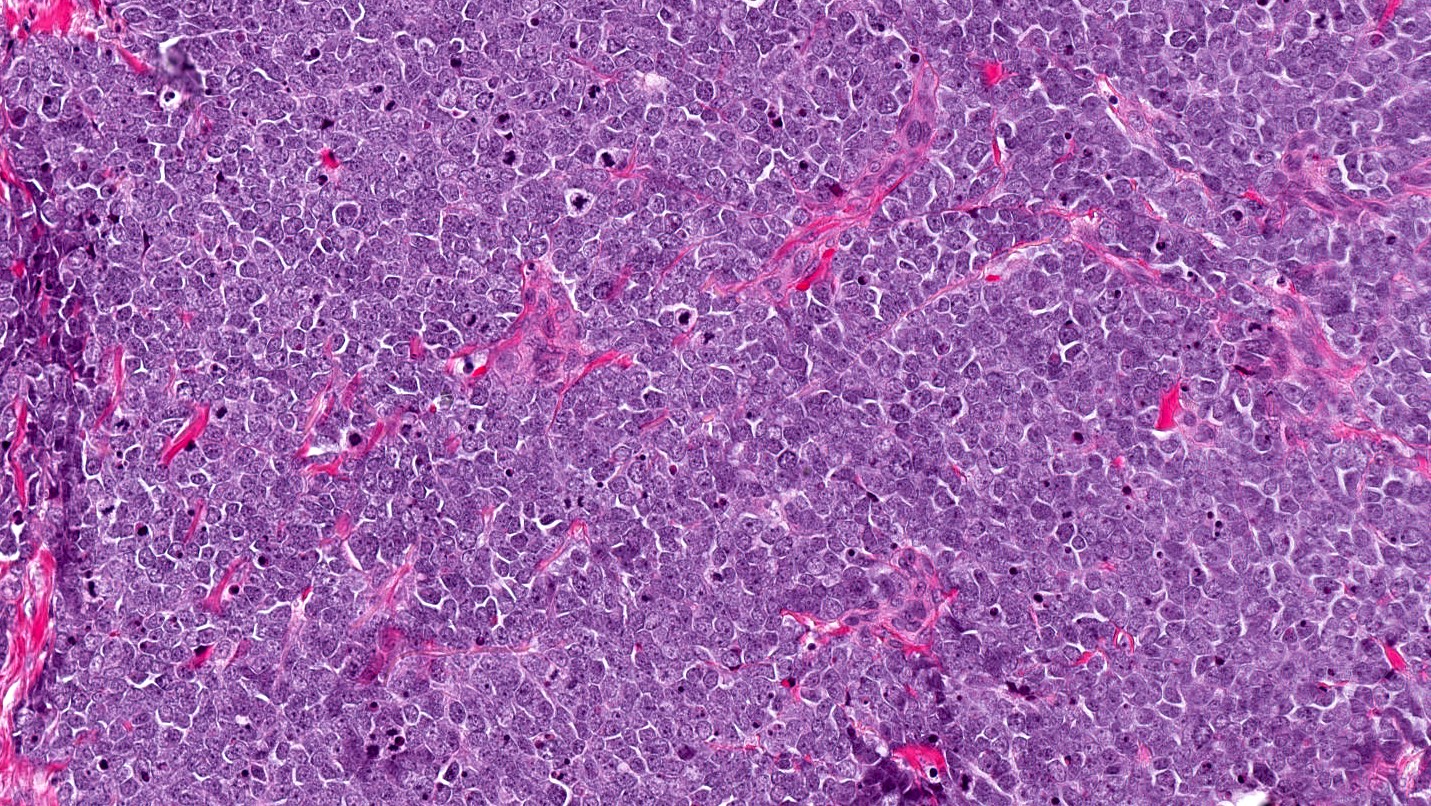
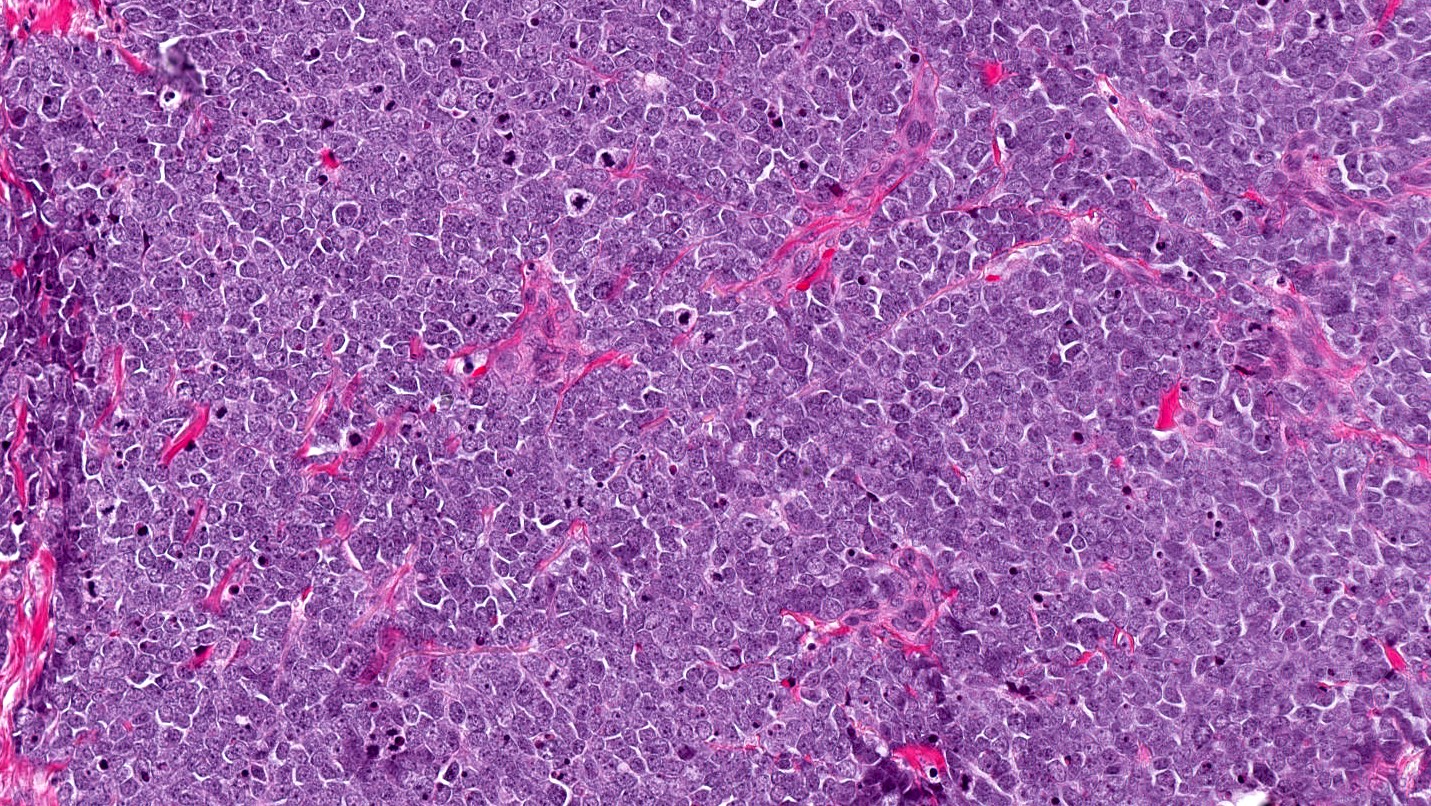
Microscopic (histologic) description
- Expansile, nodular or diffusely infiltrative tumor within the dermis, variably in subcutis
- Variable mixture of nodules, sheets, nests and trabeculae of neoplastic cells
- Intraepidermal tumor (or component) is occasionally present
- Generally, small round blue cell tumor with high N:C ratio, round / oval nuclei, finely dispersed chromatin (salt and pepper), indistinct nucleoli and scant cytoplasm
- Conspicuous mitoses and apoptotic bodies
- Variable nuclear molding and crush artifact
- Majority of cases display pure neuroendocrine morphology (pure Merkel cell carcinoma)
- Minority of cases feature neuroendocrine and other elements (combined Merkel cell carcinoma) such as divergent differentiation (e.g. squamous, sarcomatoid) or intimate association with other cutaneous neoplasms (most commonly in situ or invasive squamous cell carcinoma)
Microscopic (histologic) images
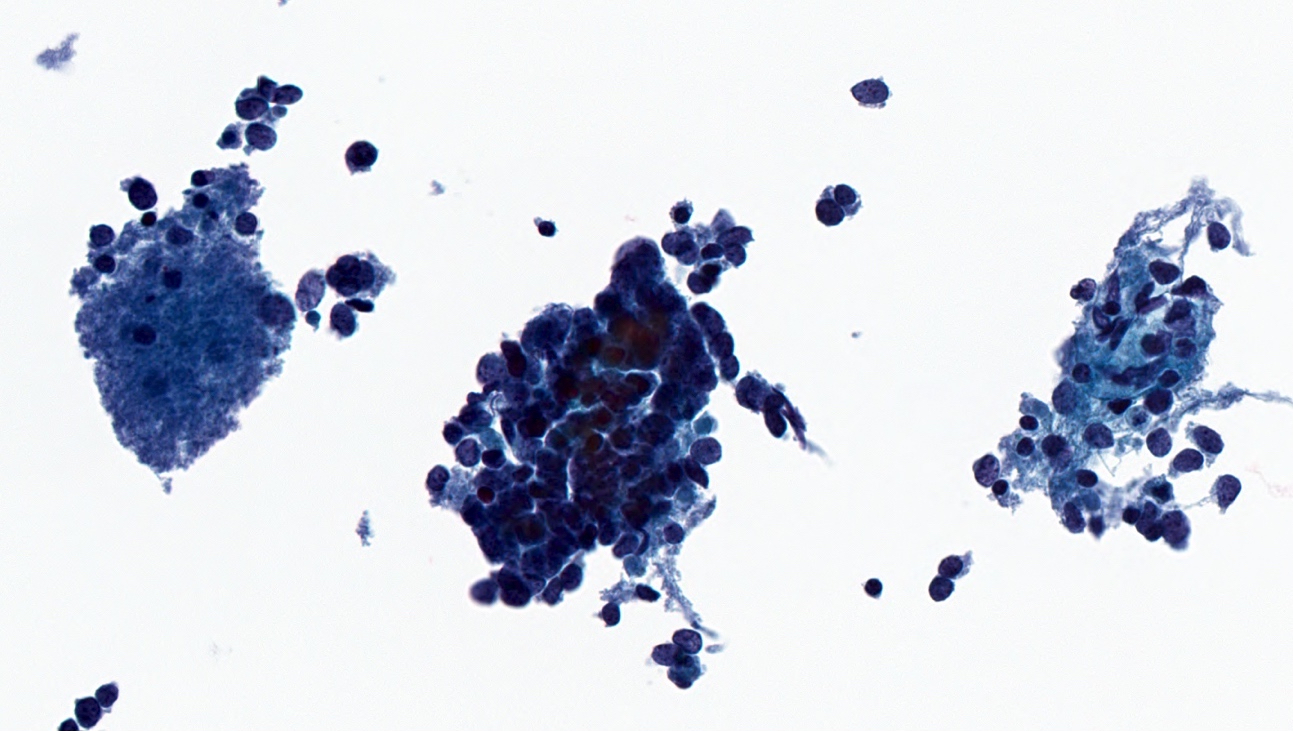
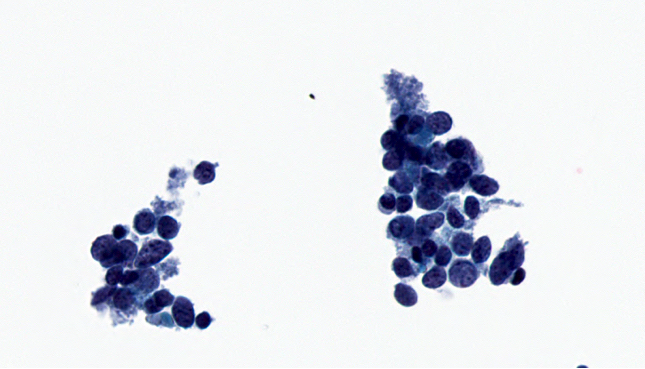
Cytology description
- Hypercellular specimen featuring small to medium sized neoplastic cells, dispersed and arranged in cohesive, disorganized groups with nuclear molding
- Neoplastic cells display uniform, round / oval nuclei with fine stippled chromatin, inconspicuous nucleoli, scant cytoplasm and high N:C ratio
- Apoptotic bodies, necrotic debris and mitoses are frequent
Cytology images
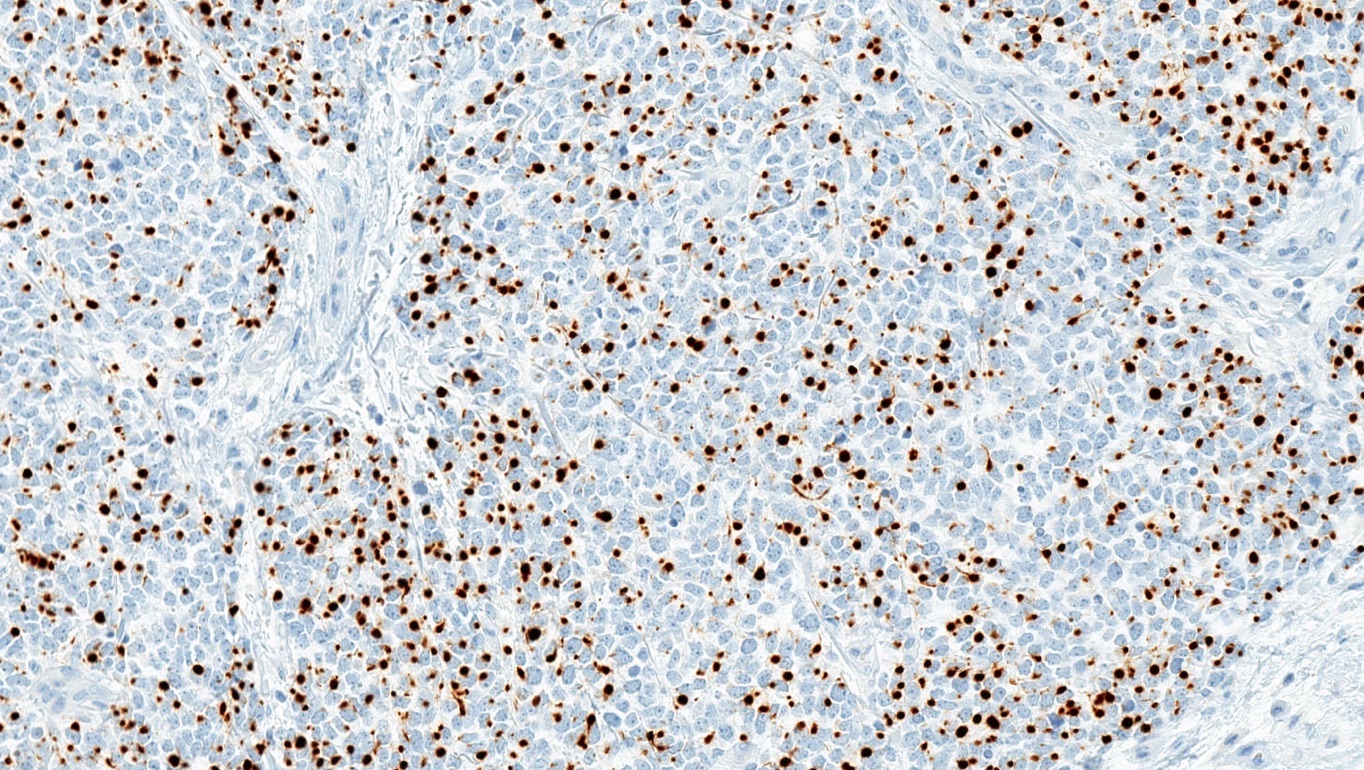
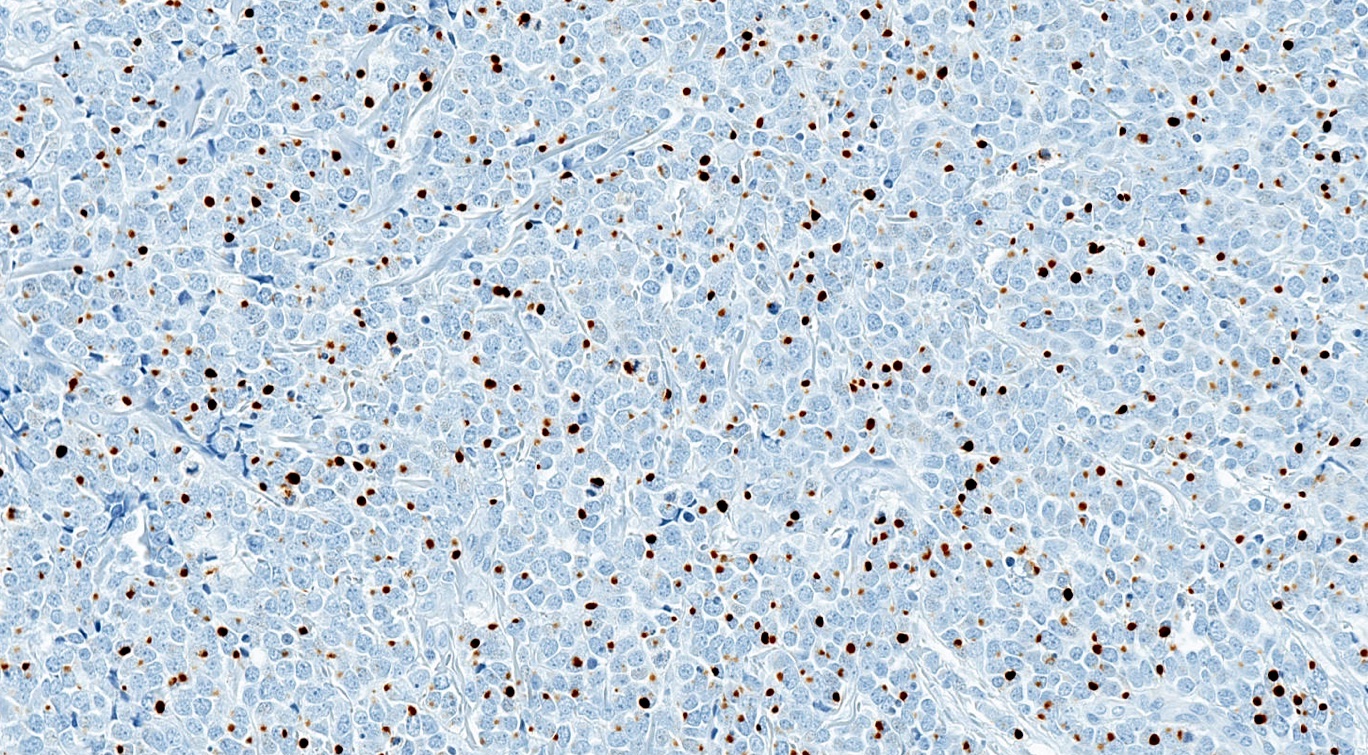
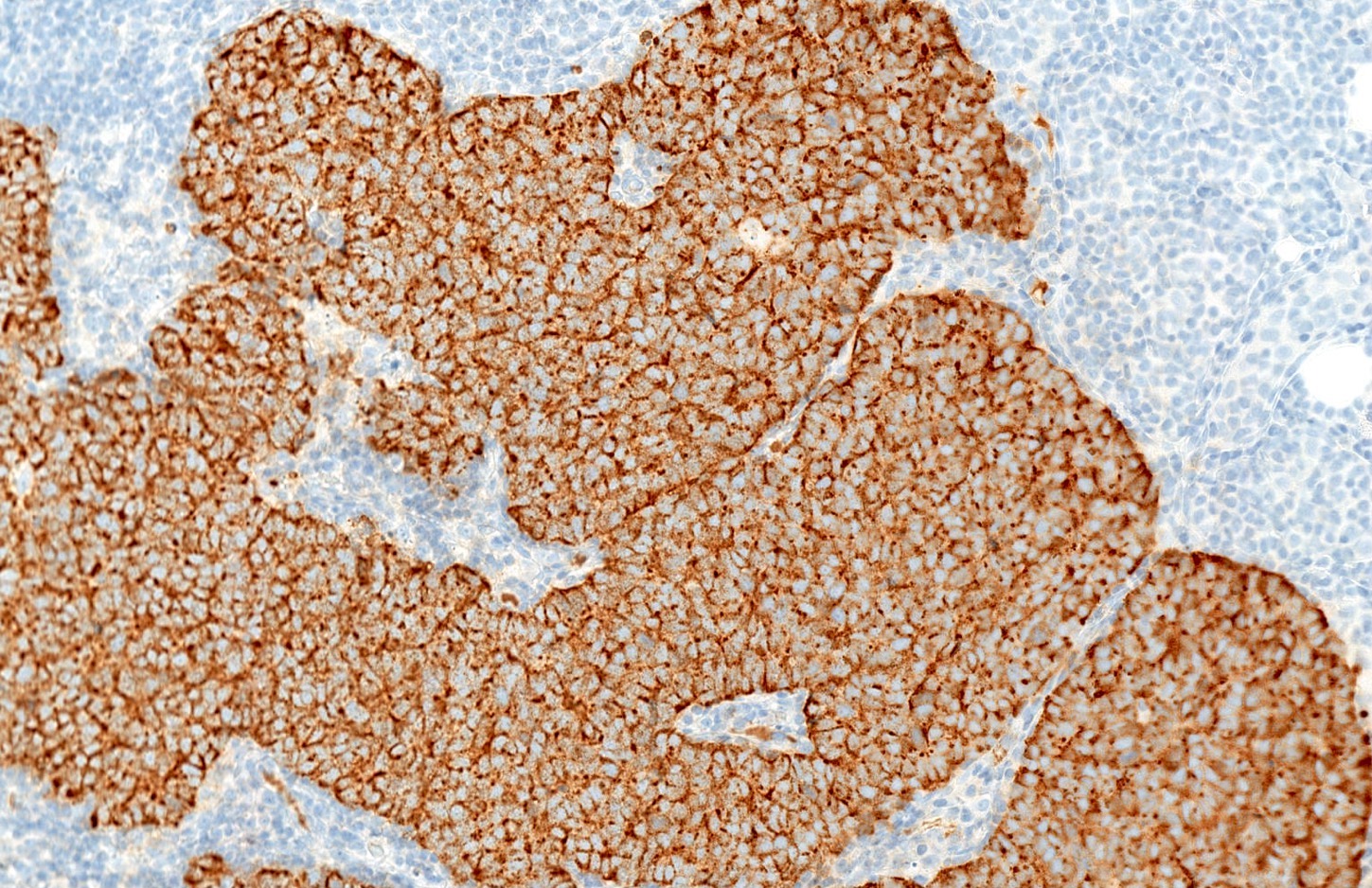
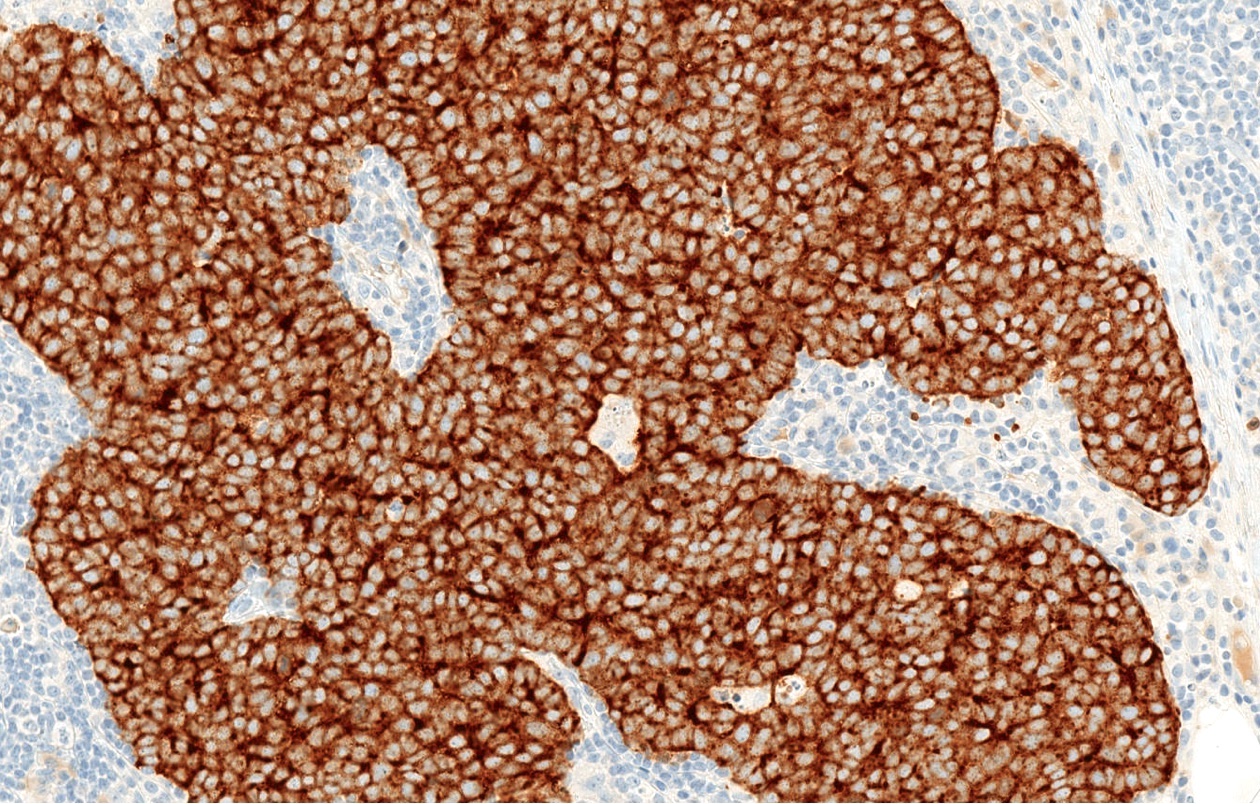
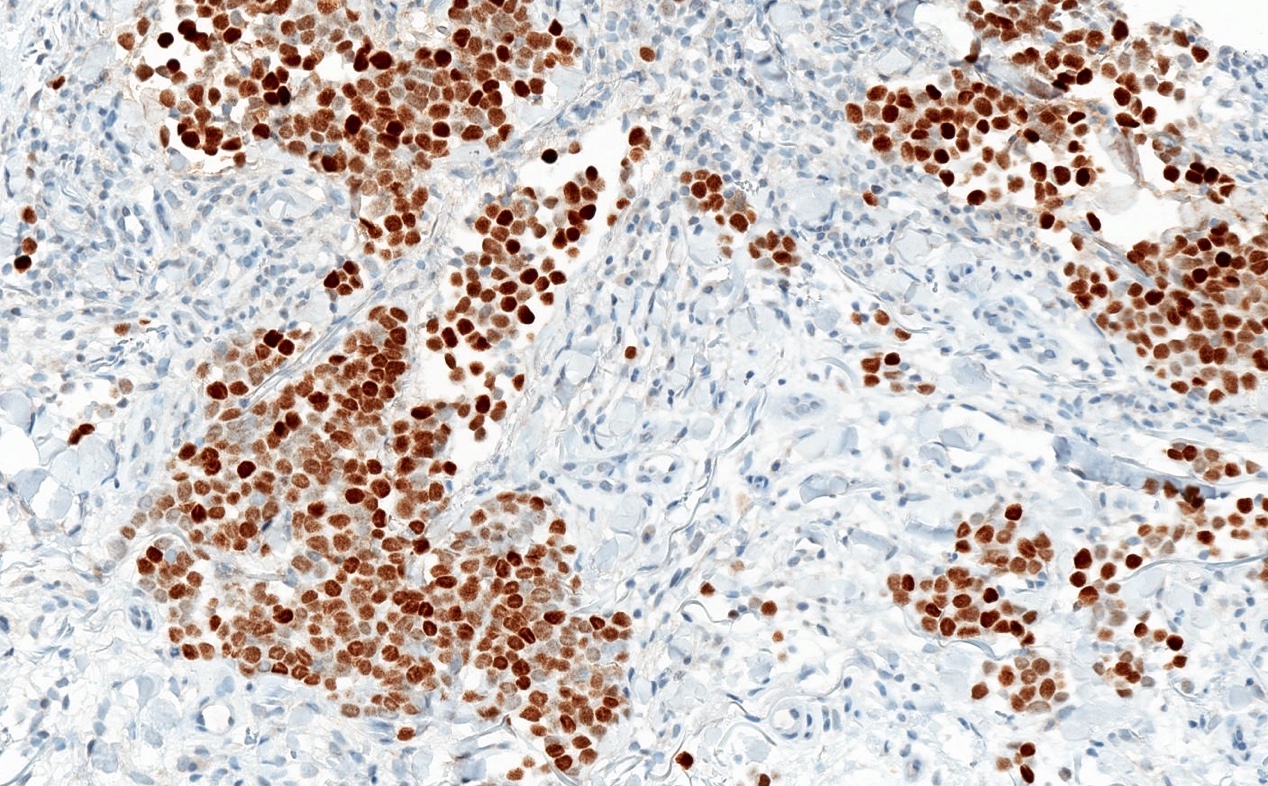
Positive stains
- Broad spectrum keratins: CAM 5.2, AE1 / AE3 (paranuclear, cytoplasmic or mixed pattern)
- CK20 (classic dot-like paranuclear pattern)
- Chromogranin, synaptophysin, CD56, neuron specific enolase
- Neurofilament (dot-like pattern)
- Variable MCPyV (nuclear pattern)
- Can express PAX5, TdT, BCL2, CD99, FLI1
Negative stains
Electron microscopy description
- Intracytoplasmic membrane bound, dense core neurosecretory granules
- Paranuclear aggregates of keratin filaments
Molecular / cytogenetics description
- Divergent genetic profiles for MCPyV+ and MCPyV- tumors
- MCPyV- tumors harbor TP53 and RB1 gene mutations, UV signature mutations and overall higher mutational burden (Oncotarget 2016;7:3403, Cancer Res 2015;75:5228)
Sample pathology report
- Left temple skin, lesion, shave excision:
- Merkel cell carcinoma (see relevant parameters below)
- Tumor size: ___ cm (maximum clinical tumor diameter; if unavailable use maximum gross or microscopic measurement)
- Depth of involvement (dermis only, involvement of fascia, muscle, cartilage or bone or unclear, due to superficial sampling)
- Morphology (pure or combined)
- MCPyV status (positive or negative)
- Lymphovascular involvement (present or absent)
- Margin status (involved or uninvolved)
- Merkel cell carcinoma (see relevant parameters below)
- Left ear, tumor, wide excision:
- Merkel cell carcinoma (see synoptic report)
- Refer to the International Collaboration on Cancer Reporting (ICCR) Histopathology Reporting Guide (1st Edition, 2019) and CAP reporting guidelines for Merkel cell carcinoma and Merkel cell carcinoma staging
Differential diagnosis
- Basal cell carcinoma:
- Displays budding from epidermal base, peripheral palisading of nuclei, myxoid stroma and peritumoral stromal retraction
- Negative: CK20, MCPyV, neurofilament
- Metastatic neuroendocrine carcinoma:
- May be morphologically indistinguishable
- Positive: variable TTF1, CK7, CDX2, MASH1, PAX8, calcitonin
- Negative: CK20, MCPyV, neurofilament
- Lymphoma / leukemia:
- Small cell melanoma:
- Ewing sarcoma:
- Rare, small round blue cell tumor
- Characteristic EWSR1 translocation
- Negative: CK20, MCPyV
- Caveat: both can express CD99, FLI1, neuron specific enolase
Additional references
Board review style question #1
This is a tumor from a 65 year old man with a history of a cutaneous malignancy. The tumor expresses paranuclear AE1 / AE3, neuroendocrine markers and MCPyV. Which is true about the lesion?
- Clinical course is indolent
- Middle aged females are primarily affected
- Morphological features alone cannot distinguish between primary cutaneous disease and metastasis from a noncutaneous source
- Nuclear pattern of CK20 expression is classic
- Site of predilection is the trunk
Board review style answer #1
C. This is Merkel cell carcinoma. Morphological features alone cannot distinguish between primary cutaneous disease and metastasis from a noncutaneous source. Accurate diagnosis requires immunohistochemistry, clinical investigation and clinical-pathologic correlation. Merkel cell carcinoma primarily affects the sun exposed skin of elderly males and preferentially the head and neck region. The classic pattern of CK20 expression is dot-like and paranuclear. Merkel cell carcinoma is aggressive and associated with high mortality.
Comment Here
Reference: Merkel cell carcinoma
Comment Here
Reference: Merkel cell carcinoma
Board review style question #2
Which of the following is typically expressed in Merkel cell carcinoma?
- CD45
- CK7
- CK20
- S100
- TTF1
Board review style answer #2
C. CK20. The classic pattern of CK20 expression is dot-like and paranuclear. Lack of expression for CK7, TTF1, S100 and CD45 help exclude other entities such as pulmonary neuroendocrine carcinoma, melanoma and lymphoma.
Comment Here
Reference: Merkel cell carcinoma
Comment Here
Reference: Merkel cell carcinoma