Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chundriger Q, Ud Din N. Hemangioma & variants. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuehemangioma.html. Accessed April 1st, 2025.
Definition / general
- Benign tumor composed of circumscribed proliferation of predominantly small capillary sized blood vessels
- See also these related soft tissue topics: anastomosing hemangioma, cystic / cavernous lymphangioma, epithelioid hemangioma, intramuscular angioma, lymphangioendothelioma, lymphangioma, lymphangiomatosis, venous hemangioma
Essential features
- Most cases arise in children, with equal gender distribution
- Composed of small capillary sized blood vessels with a larger feeding vessel commonly present
- Most cases are treated with topical or systemic beta blockers in isolation or in combination with other modalities like laser therapy, excision, etc.
- Recurrence is uncommon and only exceptional examples show malignant transformation
Terminology
- Hemangioma is commonly used with a qualifier (e.g. congenital hemangioma)
Epidemiology
- Most common tumor of childhood and infancy (Goldblum: Enzinger and Weiss's Soft Tissue Tumors, 7th Edition, 2019)
- M = F; gender predilection is variable for site specific examples, like synovial hemangioma (Eur J Orthop Surg Traumatol 2019;29:1291)
- Common in Klippel-Trenaunay syndrome, PHACE syndrome and LUMBAR syndrome (Surg Neurol Int 2018;9:205, StatPearls: PHACE Syndrome [Acessed 13 October 2021], Med Arch 2021;75:158, Actas Dermosifiliogr 2017;108:475)
Sites
- Most are superficial, commonly in head and neck region
- Hepatic hemangiomas are common in infants
- Deep visceral or skeletal location is rare but well documented (J Cancer Res Ther 2020;16:938, World J Gastroenterol 2020;26:11, BMC Musculoskelet Disord 2021;22:27, J Optom 2017;10:79)
Pathophysiology
- Specific pathogenesis has not been fully understood
- Currently regarded as a multifactorial condition, resulting in endothelial proliferation, with uncontrolled angiogenesis and abnormal function of downstream pathways (notably HIF1α, VEGF and PI3K / Akt) (Biomed Res Int 2021;2021:5695378)
Etiology
- Not known
Clinical features
- Superficial: red to purple papules, nodules or ill defined elevations (Semin Cutan Med Surg 2016;35:108)
- Cavernous hemangiomas present as port wine nevi
- May be associated with von Hippel-Lindau disease (Can Med Assoc J 1969;101:135)
- Visceral: hemoptysis, visual field defects, localized pressure effects, mass effect (Medicine (Baltimore) 2018;97:e11203, J Optom 2017;10:79, Ital J Pediatr 2020;46:157, J Cancer Res Ther 2020;16:938, Ann Thorac Cardiovasc Surg 2019;25:71, J Pak Med Assoc 2018;68:1846, J Int Med Res 2020;48:300060520954718)
- Presence of more than 5 cutaneous lesions has increased chance of visceral involvement (Pediatrics 2008;122:360)
- Hepatic hemangioma: abdominal distension and discomfort when more than 5 cm in size; most are asymptomatic (J Hepatobiliary Pancreat Sci 2017;24:417)
- Skeletal: mostly asymptomatic; rarely present with localized symptoms, such as bone pain and pathological fracture (BMC Musculoskelet Disord 2021;22:27)
- Infantile hemangioma: small at birth; grows up to 6 months of age and involutes after first year of life (Hum Pathol 2000;31:11)
- Congenital hemangioma: maximum size at birth, lacks growth phase, either involutes partially (partially involuting congenital hemangioma [PICH]) or completely (rapidly involuting congenital hemangioma [RICH]) or requires treatment / intervention (noninvoluting congenital hemangioma [NICH]) (Semin Pediatr Surg 2014;23:162, BMJ Paediatr Open 2020;4:e000816)
Diagnosis
- Requires correlation of detailed history and physical examination with microscopic features, as the latter overlaps for various clinical presentations
Laboratory
- Transient mild to moderate thrombocytopenia due to consumption may be seen in rapid growth phase (F1000Res 2019;8:F1000)
Radiology description
- Mostly required for extracutaneous cases
- Skeletal (bone) hemangiomas: radiology is highly nonspecific (BMC Musculoskelet Disord 2021;22:27)
- Ultrasound: highly effective; shows well defined mass with high vascularity
- Contrast enhanced ultrasonography (CEUS): gold standard for hepatic hemangiomas (Korean J Radiol 2000;1:191)
- High flow in proliferative phase of infantile hemangioma; slow flow in involuted phase
- Central high flow for NICH; slow flow for RICH
- Fluttering sign: recently described feature for grayscale ultrasound in hepatic hemangiomas (Ultrasound Med Biol 2021;47:941)
- MRI: useful in deep locations to estimate extent of tissue involvement
- Infantile hemangioma: hyperintense on T2; isointense on T1 with postcontrast enhancement
- Congenital hemangioma: heterogeneous appearance on MRI
- CT scan: hypodense, with postcontrast enhancement of periphery (World J Gastroenterol 2020;26:11)
Radiology images
Prognostic factors
- Most common complications in superficial lesions include ulceration and permanent skin changes, like scarring (Semin Cutan Med Surg 2016;35:108, Semin Pediatr Surg 2014;23:162)
- Recurrence if larger or deep lesions are incompletely excised or inadequately treated (Acta Ophthalmol 2020;98:679, Int J Surg Case Rep 2019;60:319)
- Large lesions may contribute to high output cardiac failure (Interv Neuroradiol 2017;23:102)
- Only exceptional examples show malignant transformation (Am J Surg Pathol 2002;26:1319)
Case reports
- 3 month old girl with facial lesion and intussusception (Oman Med J 2020;35:e204)
- 14 year old boy with right sided hearing loss (Einstein (Sao Paulo) 2018;16:eRC4509)
- 32 year old woman with progressive loss of vision (J Ophthalmic Vis Res 2012;7:244)
- 49 year old woman with lumbar pain (Medicine (Baltimore) 2019;98:e14001)
- 84 year old man with BI RADS III mass in right breast (Am J Case Rep 2018;19:1425)
Treatment
- Aims at stopping the growth of lesion
- Systemic and topical beta blockers, alone or in combination with steroids or surgery, may be useful depending on age, site and size of lesion (Turk J Pediatr 2017;59:254)
- Laser treatments, embolization and sclerotherapy or a combination of different modalities have all been described to be useful depending on individual cases (J Optom 2017;10:79, J Int Med Res 2020;48:300060520977589, Intern Med 2020;59:1727, Am J Case Rep 2021;22:e931042)
- Proanthocyanidins are under research as potential therapeutic options for infantile hemangioma (Biomed Res Int 2021;2021:5695378)
Clinical images
Contributed by Nasir Ud Din, M.B.B.S.
Images hosted on other servers:
Gross description
- Deep lesions are well circumscribed and solid to cystic, with dilated vessels and with or without thrombus formation (Pediatr Radiol 2010;40:S63)
- May be polypoid with a stalk (Ann Thorac Cardiovasc Surg 2019;25:71)
Gross images
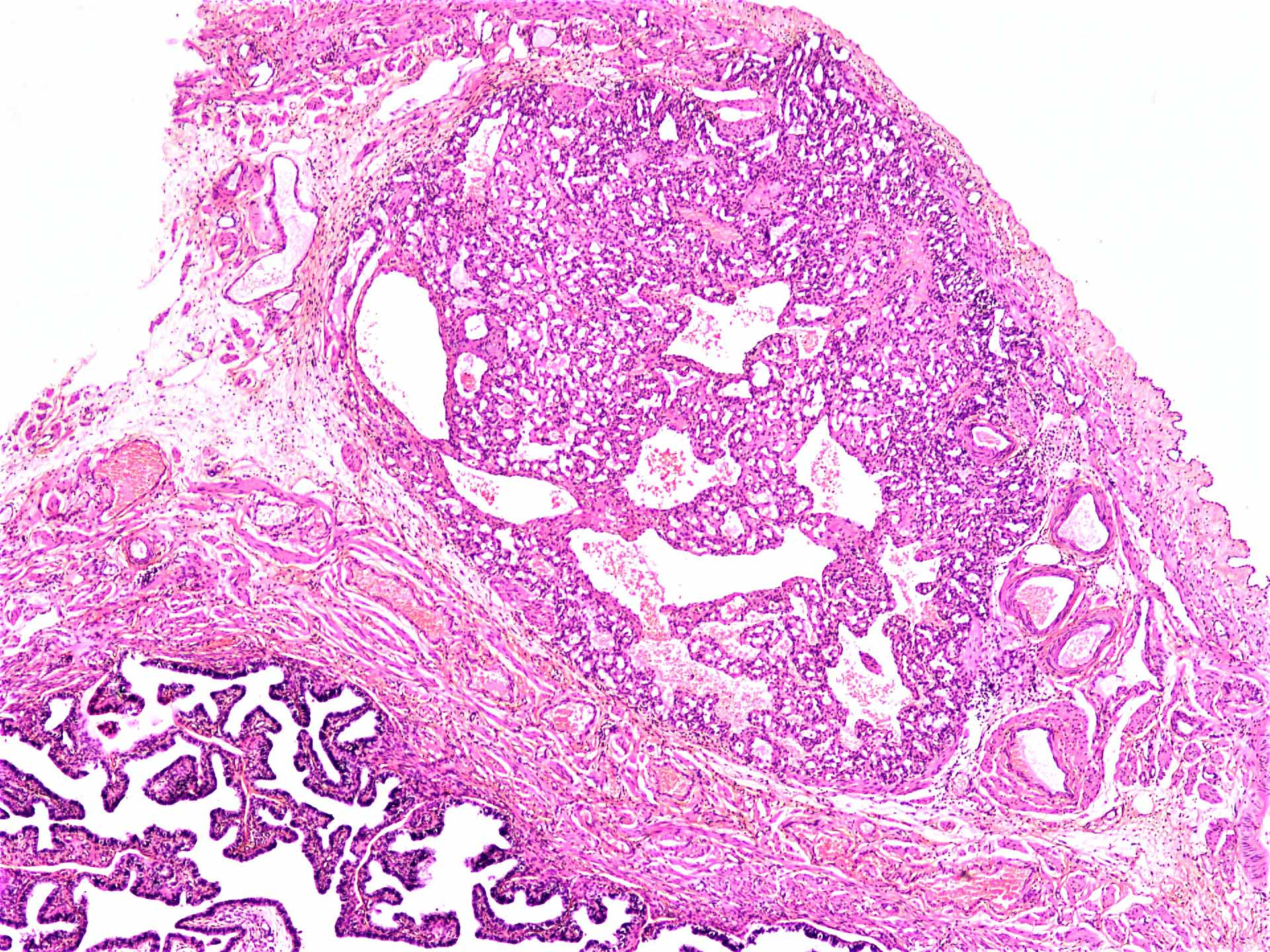
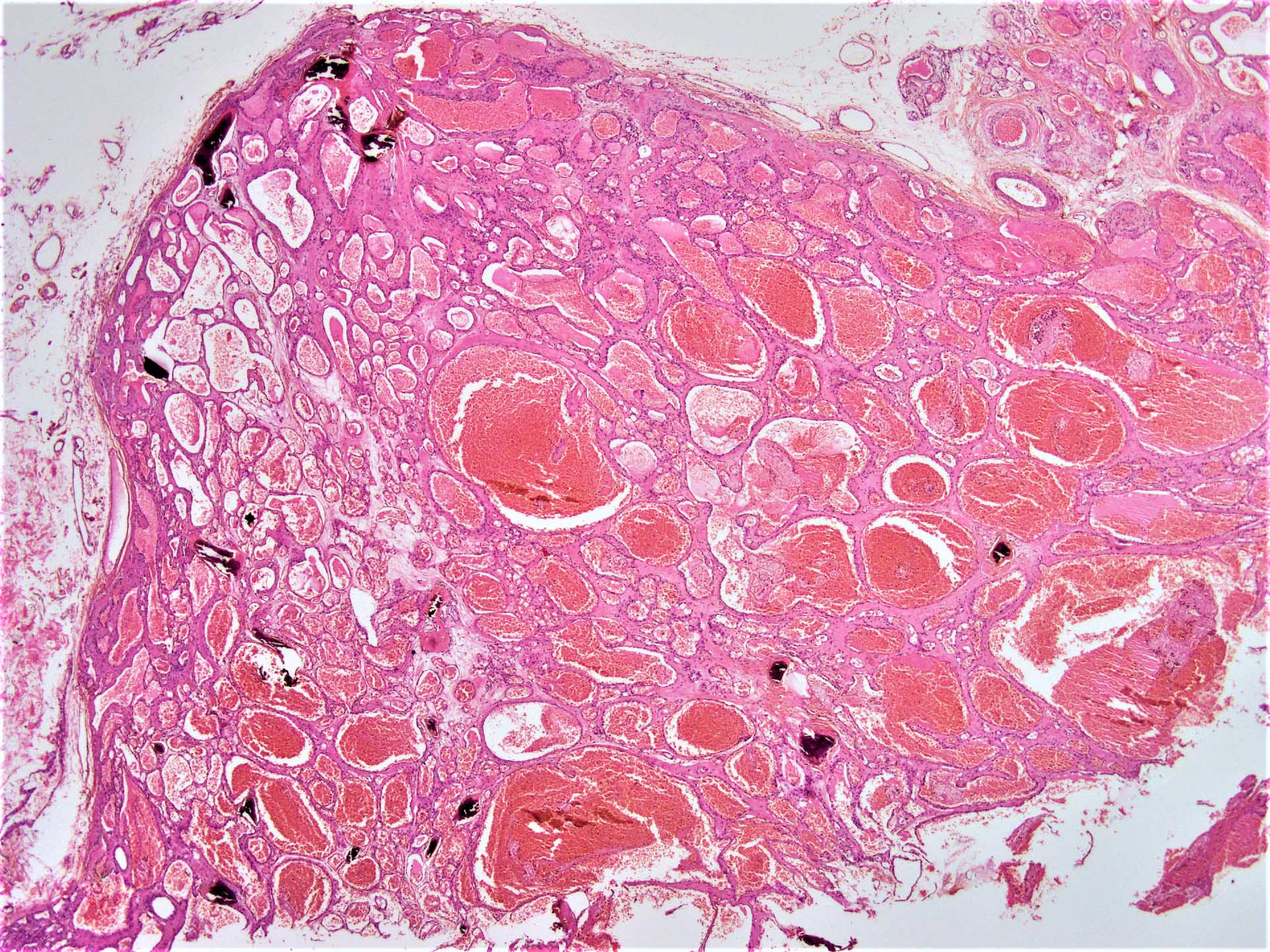
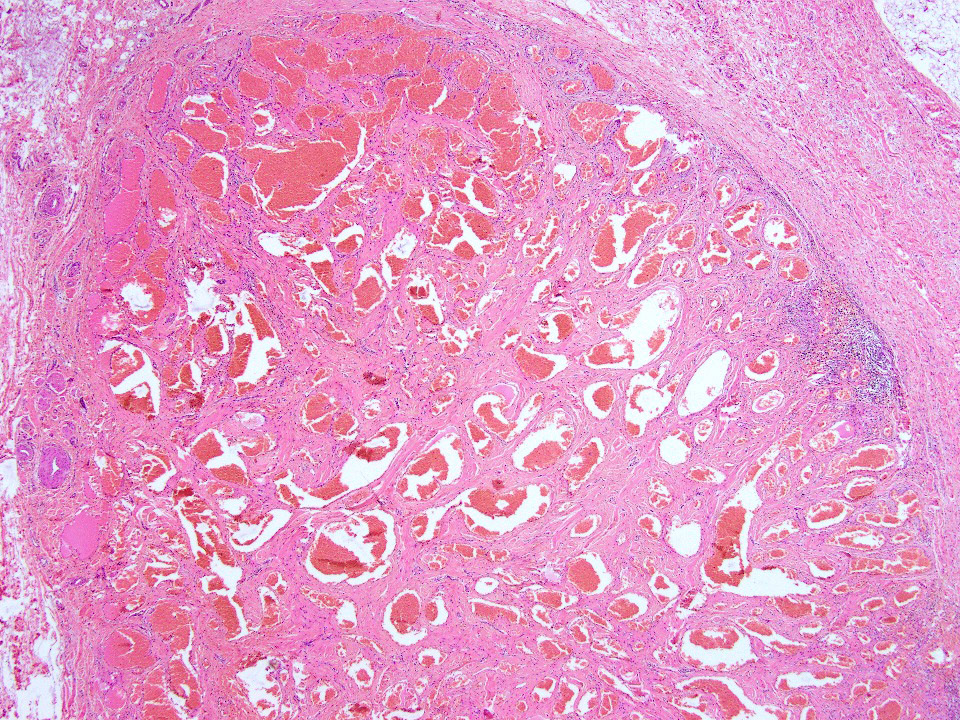
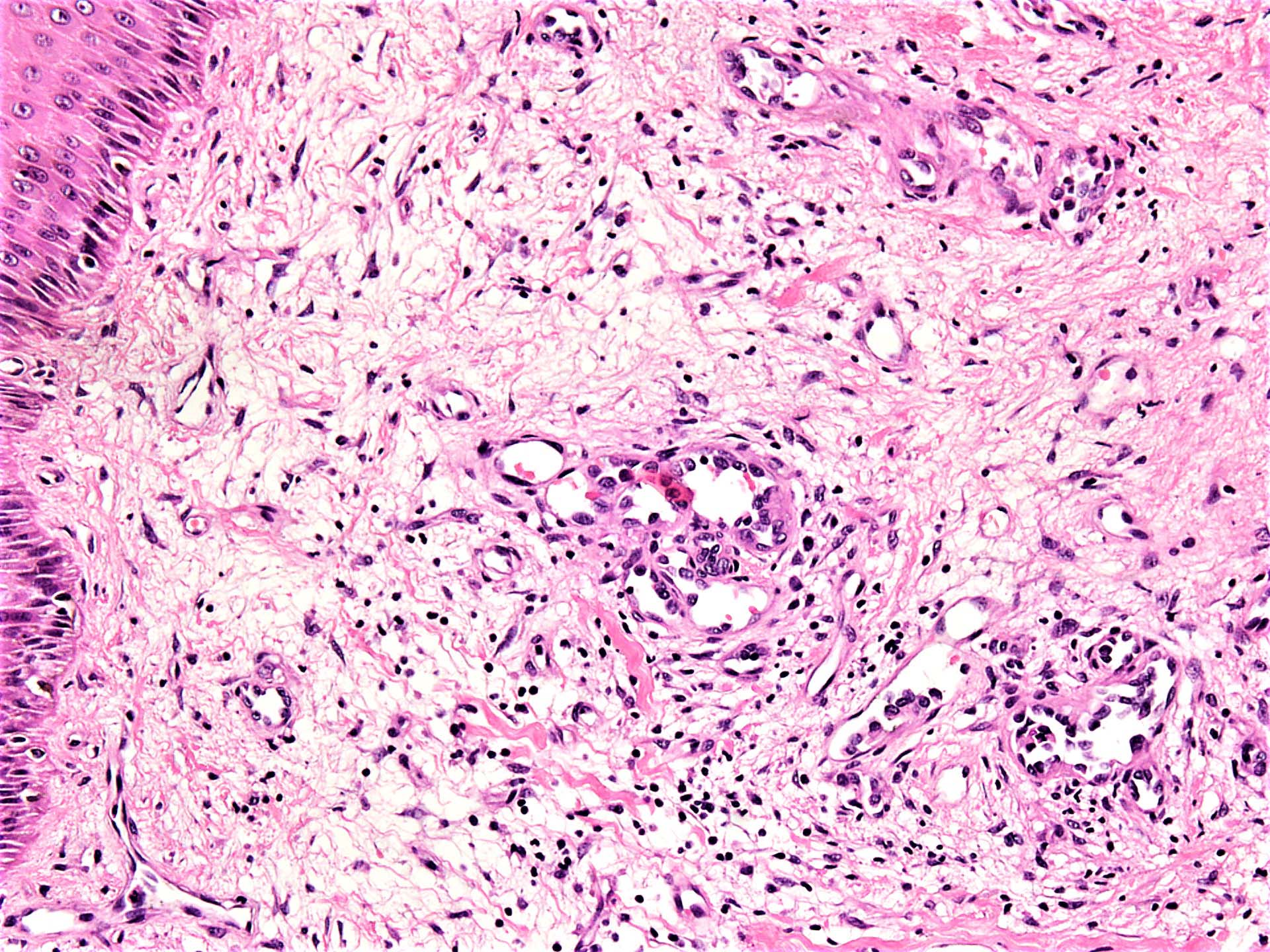
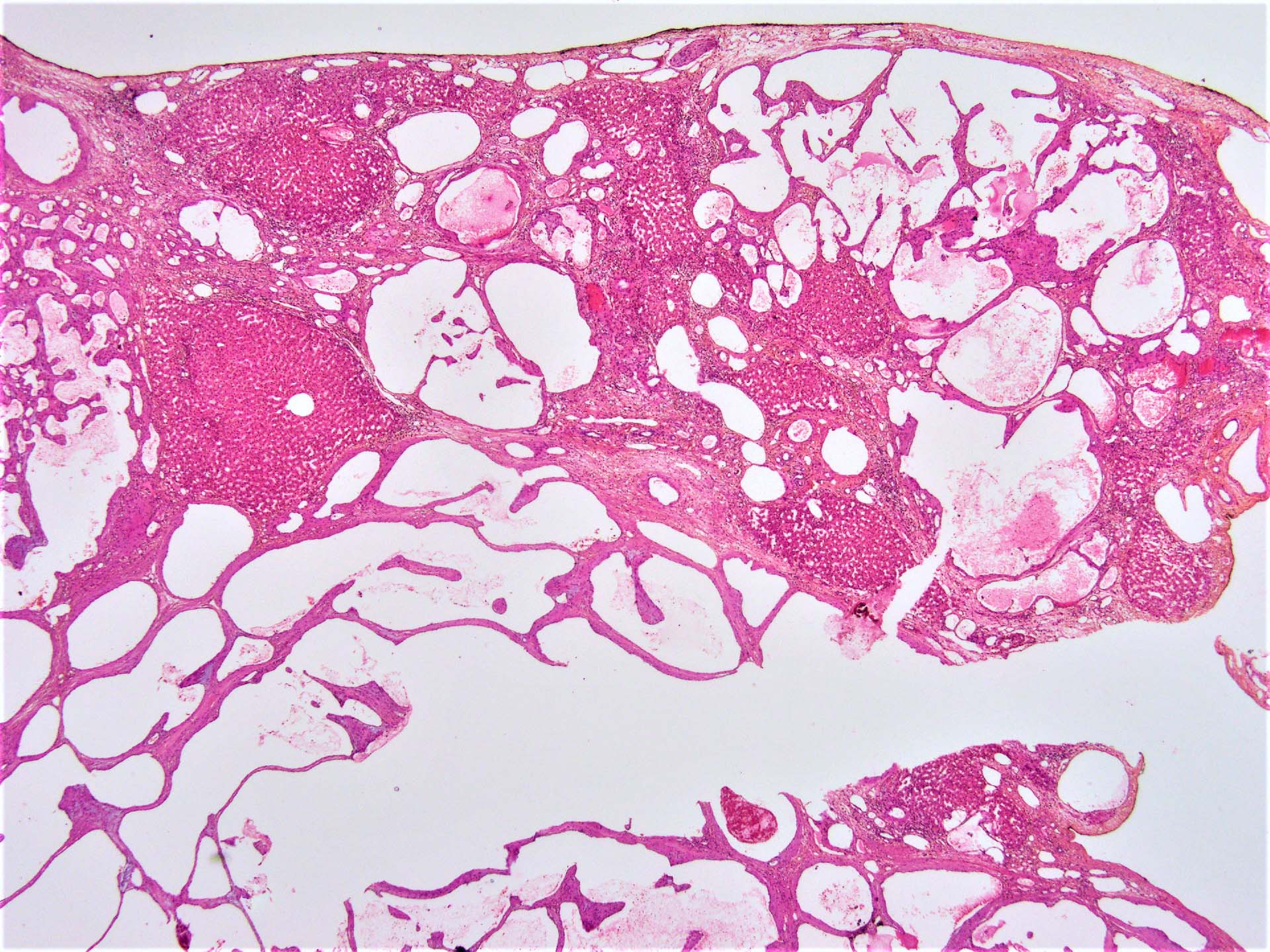
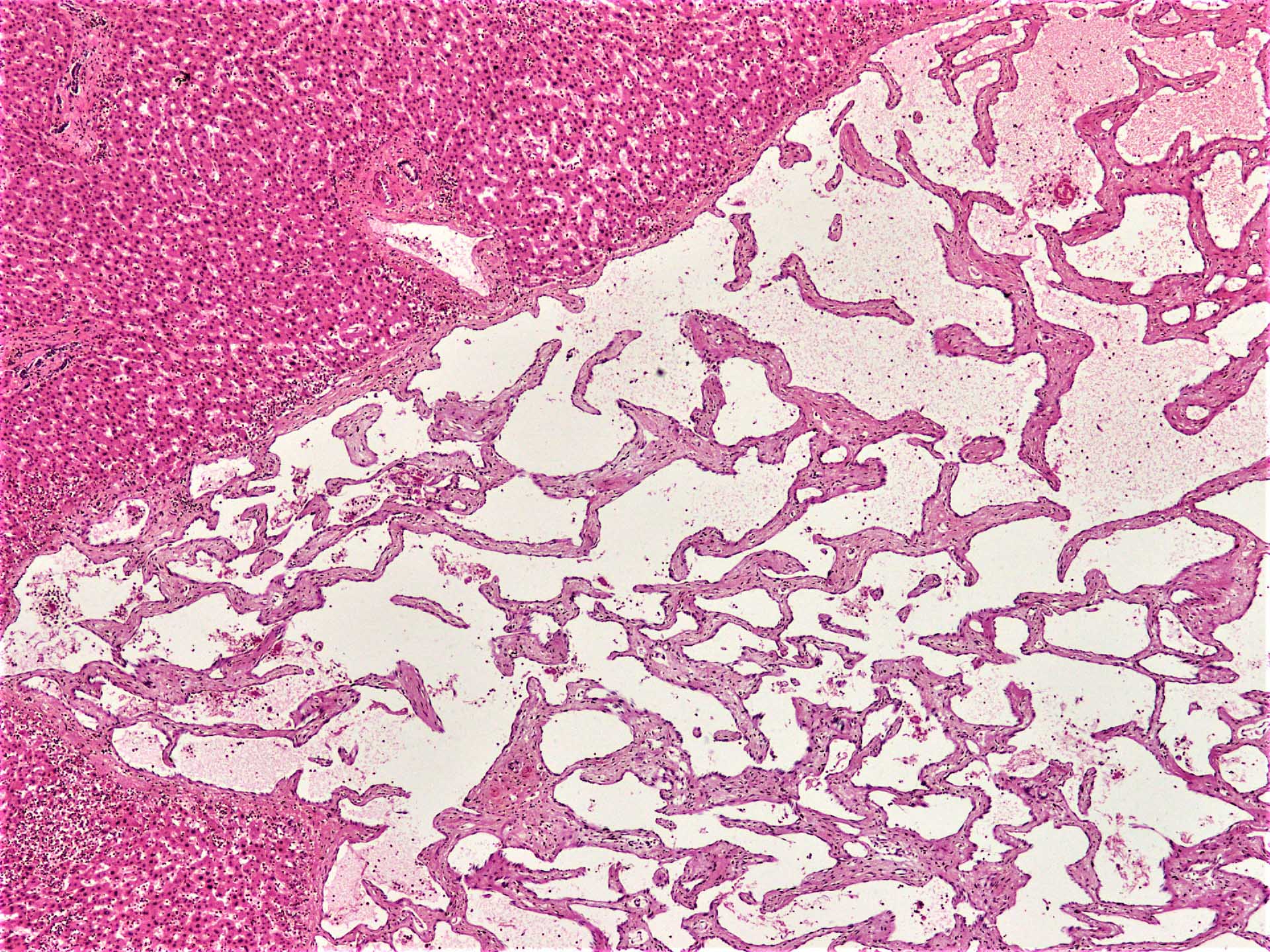
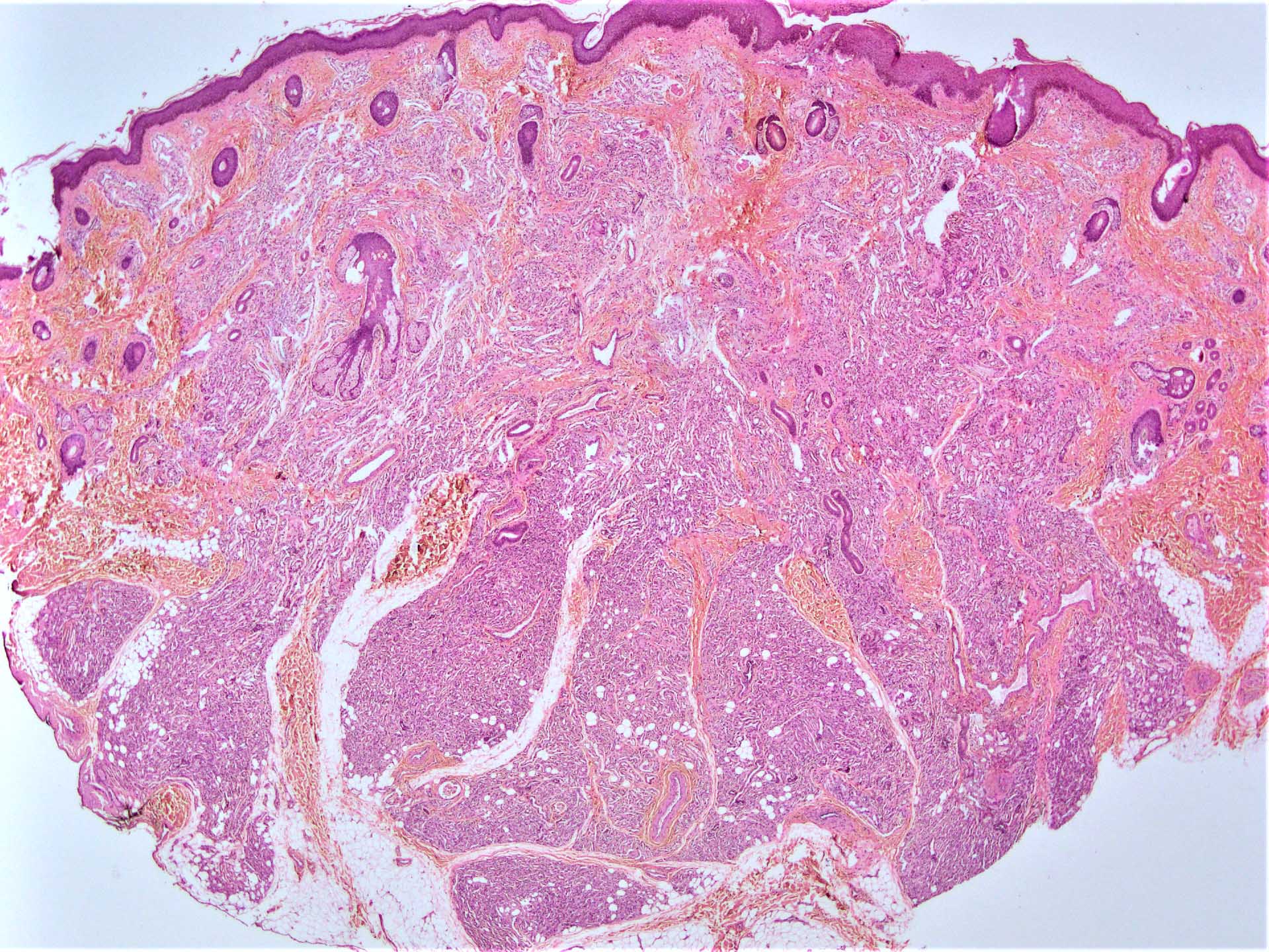
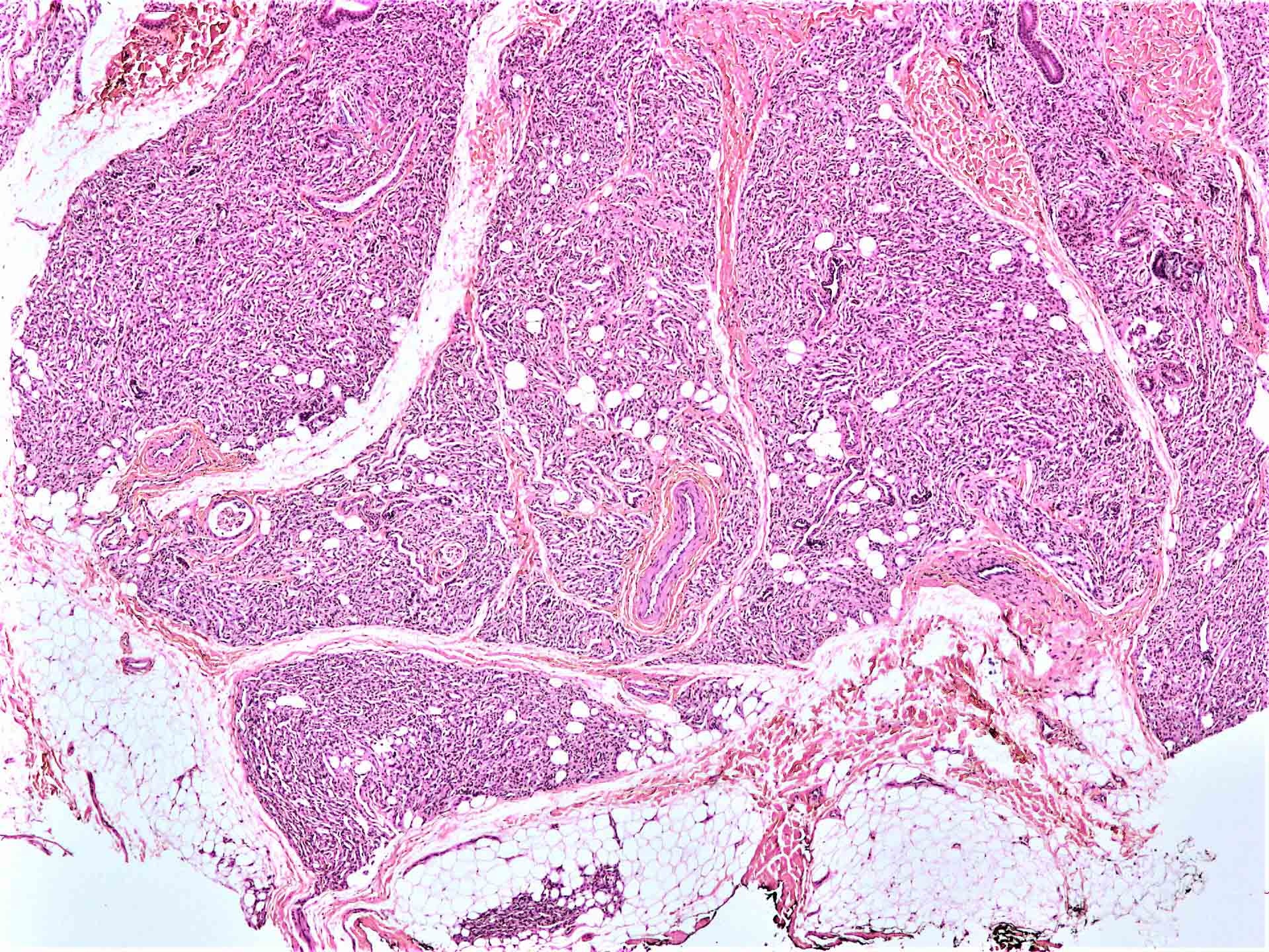
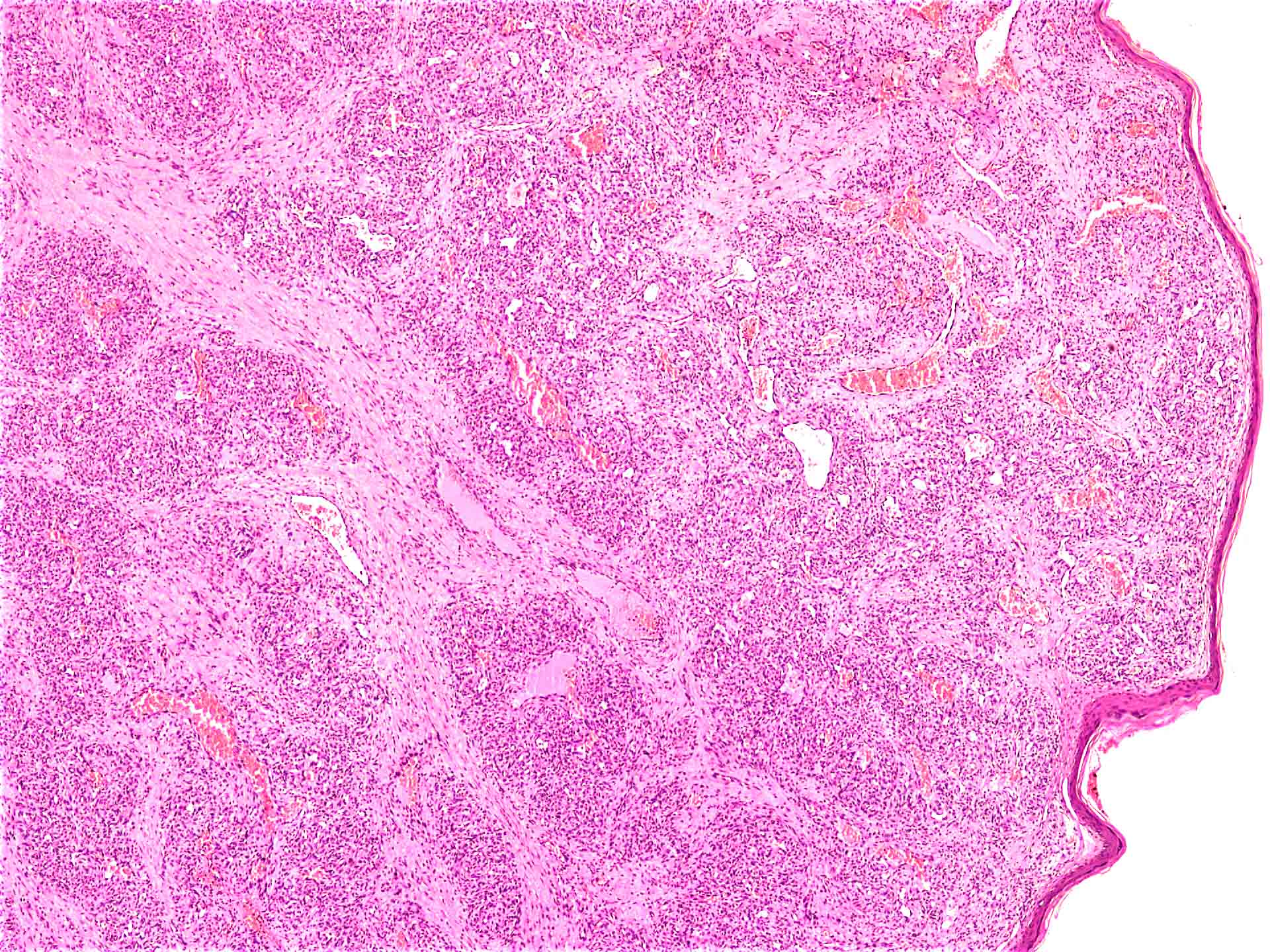
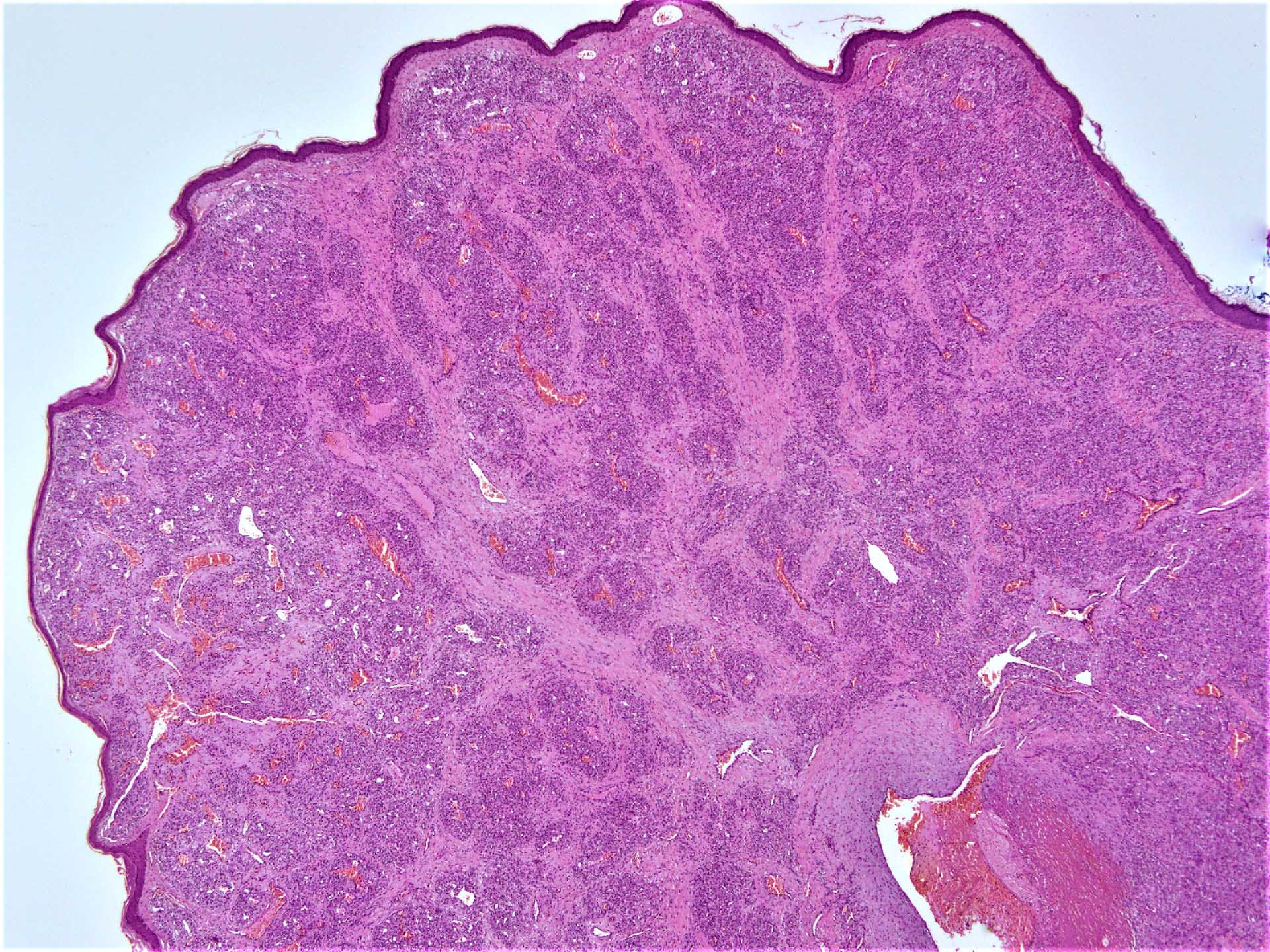
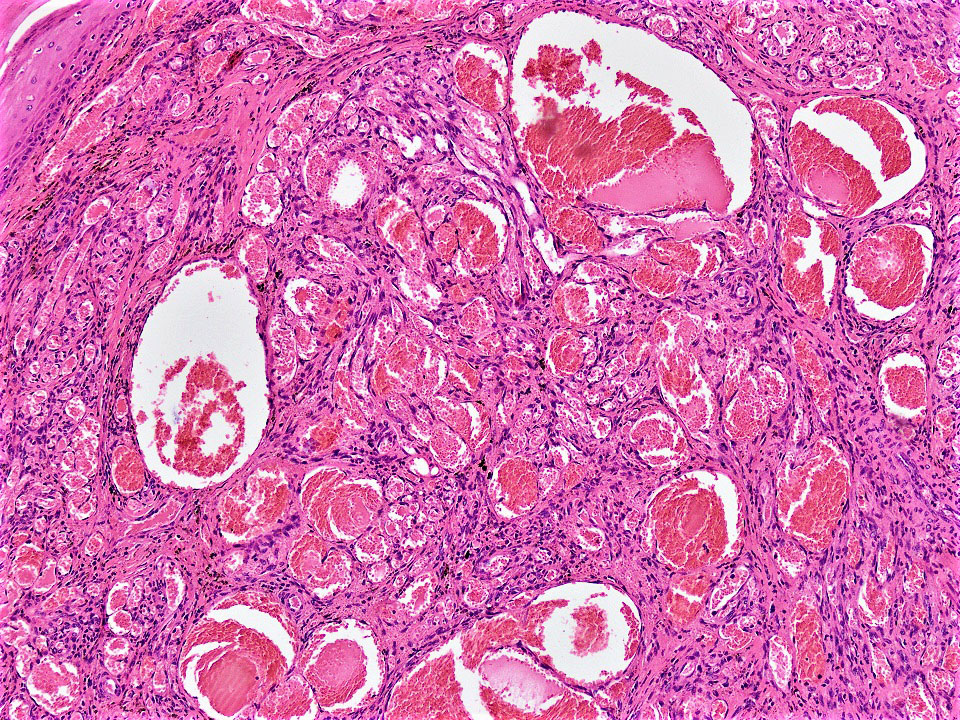
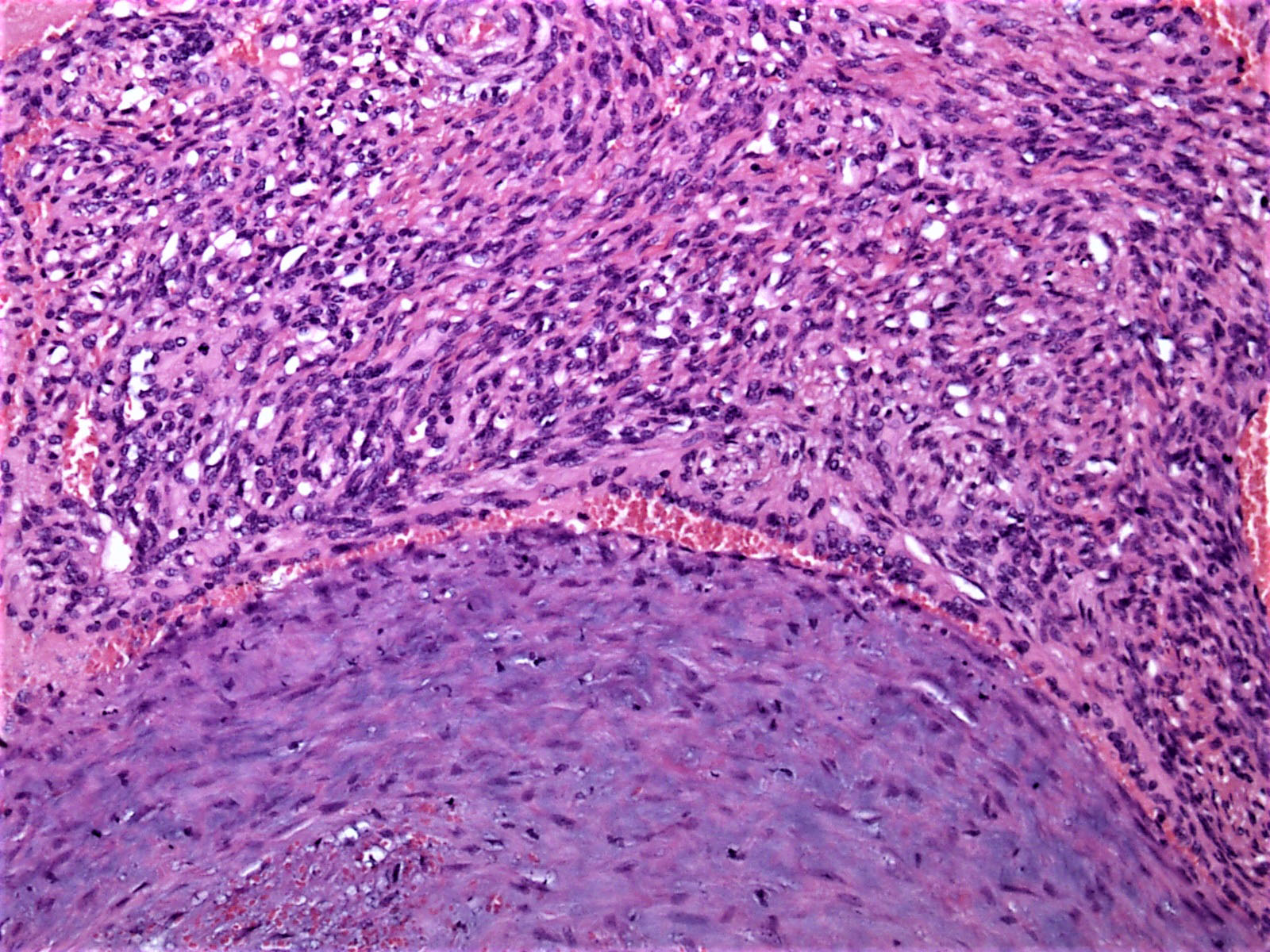
Microscopic (histologic) description
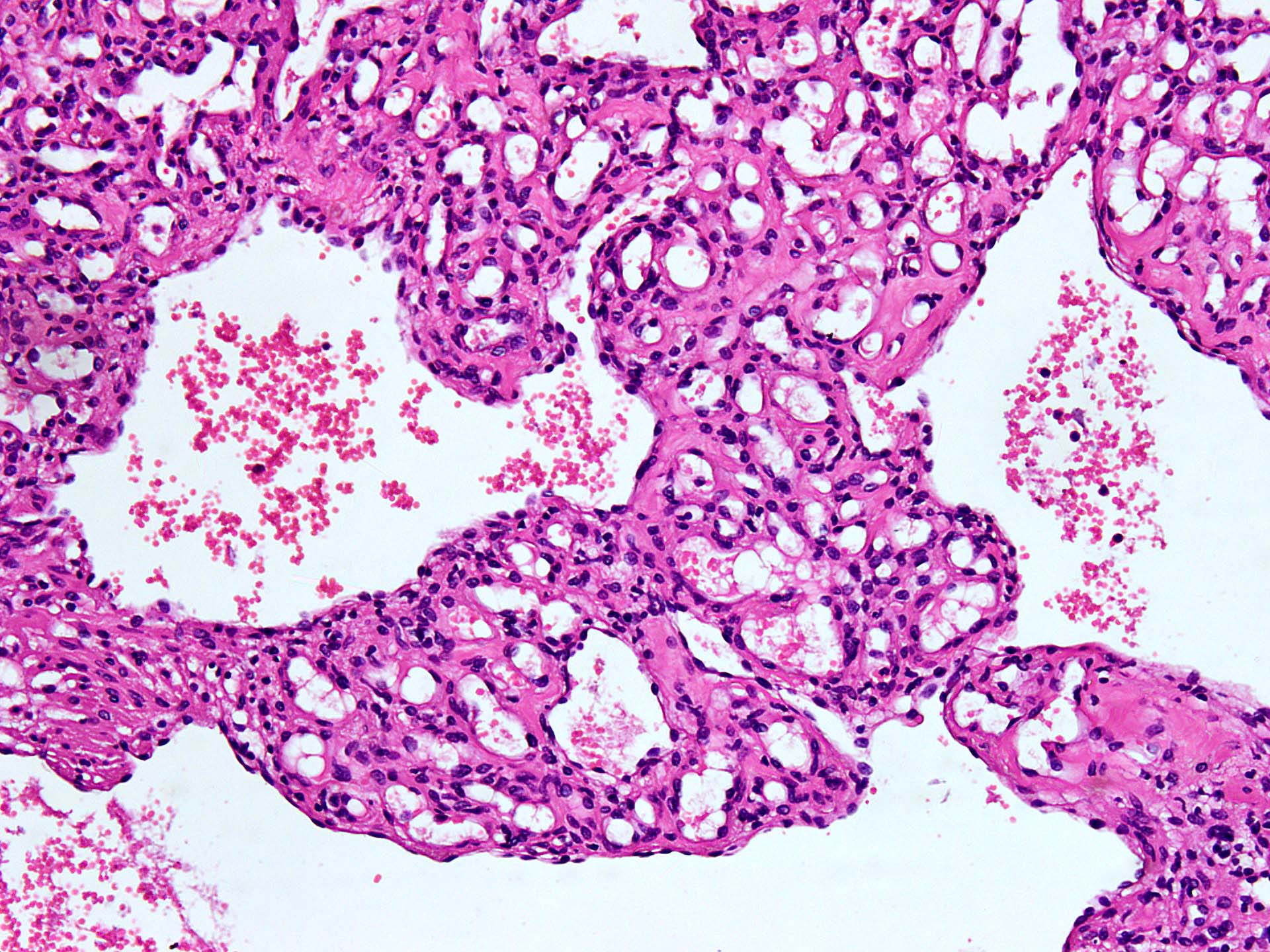
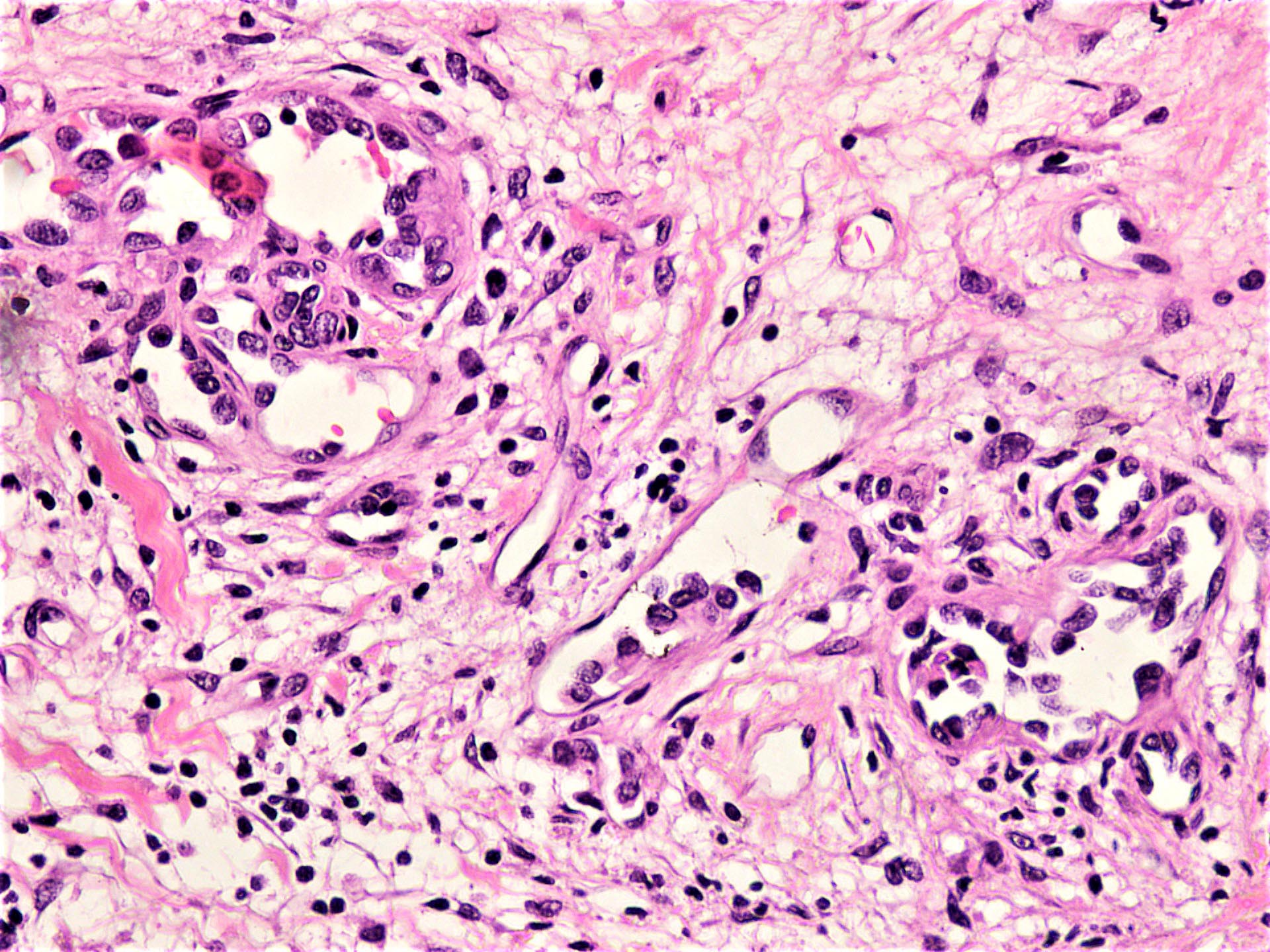
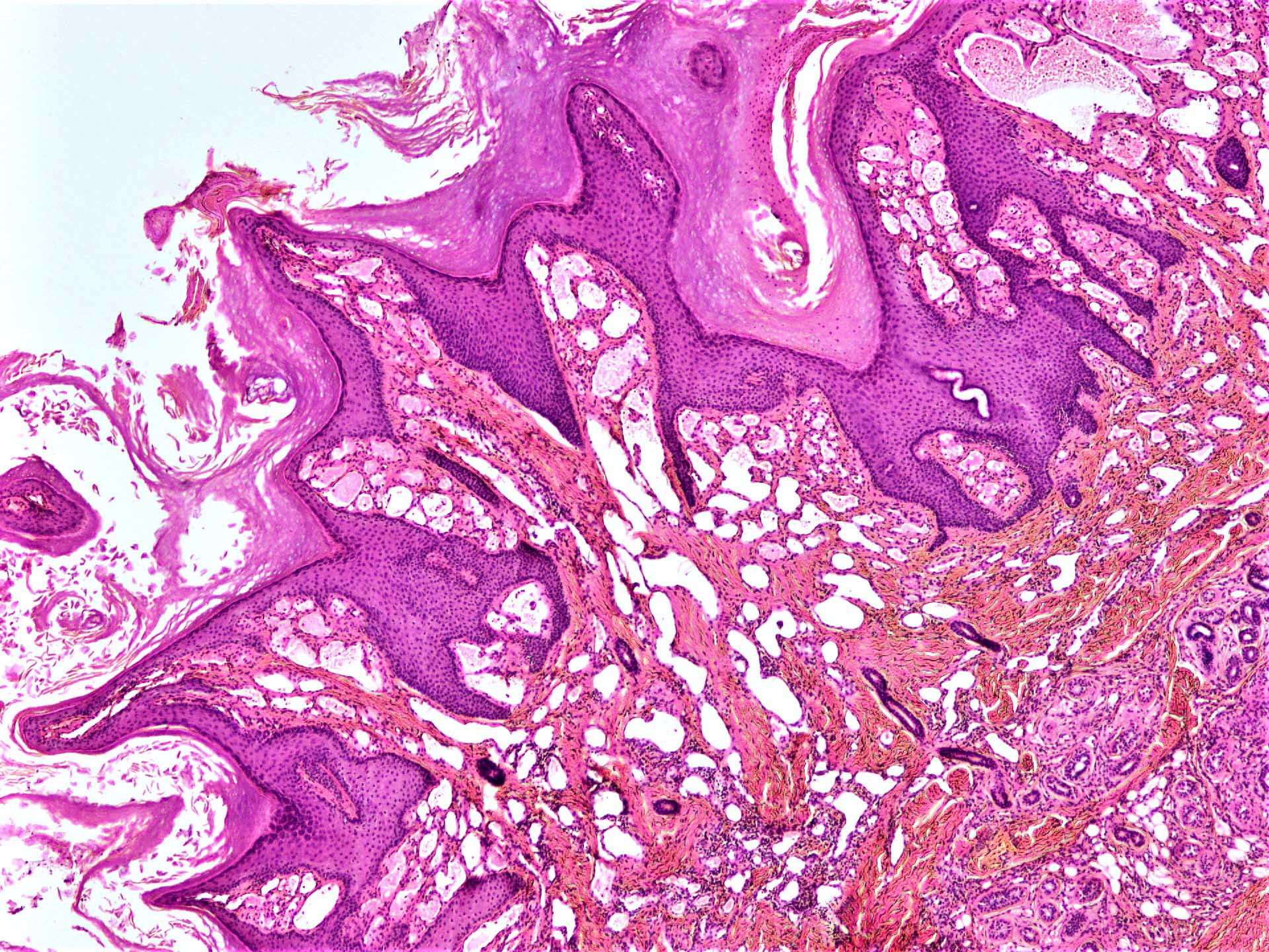
- Lobules of capillary sized vascular channels, lined by single layer of flattened endothelial cells
- Large feeding vessel is usually seen at the deeper aspect
- Associated lymphocyte infiltrate may be seen (Cardiovasc Pathol 2017;28:59)
- Anastomosing hemangioma: anastomosing vascular channels lined by flattened endothelium; deep occurrence
- Angiomatosis: involvement of multiple tissue planes with irregular and poorly circumscribed edges
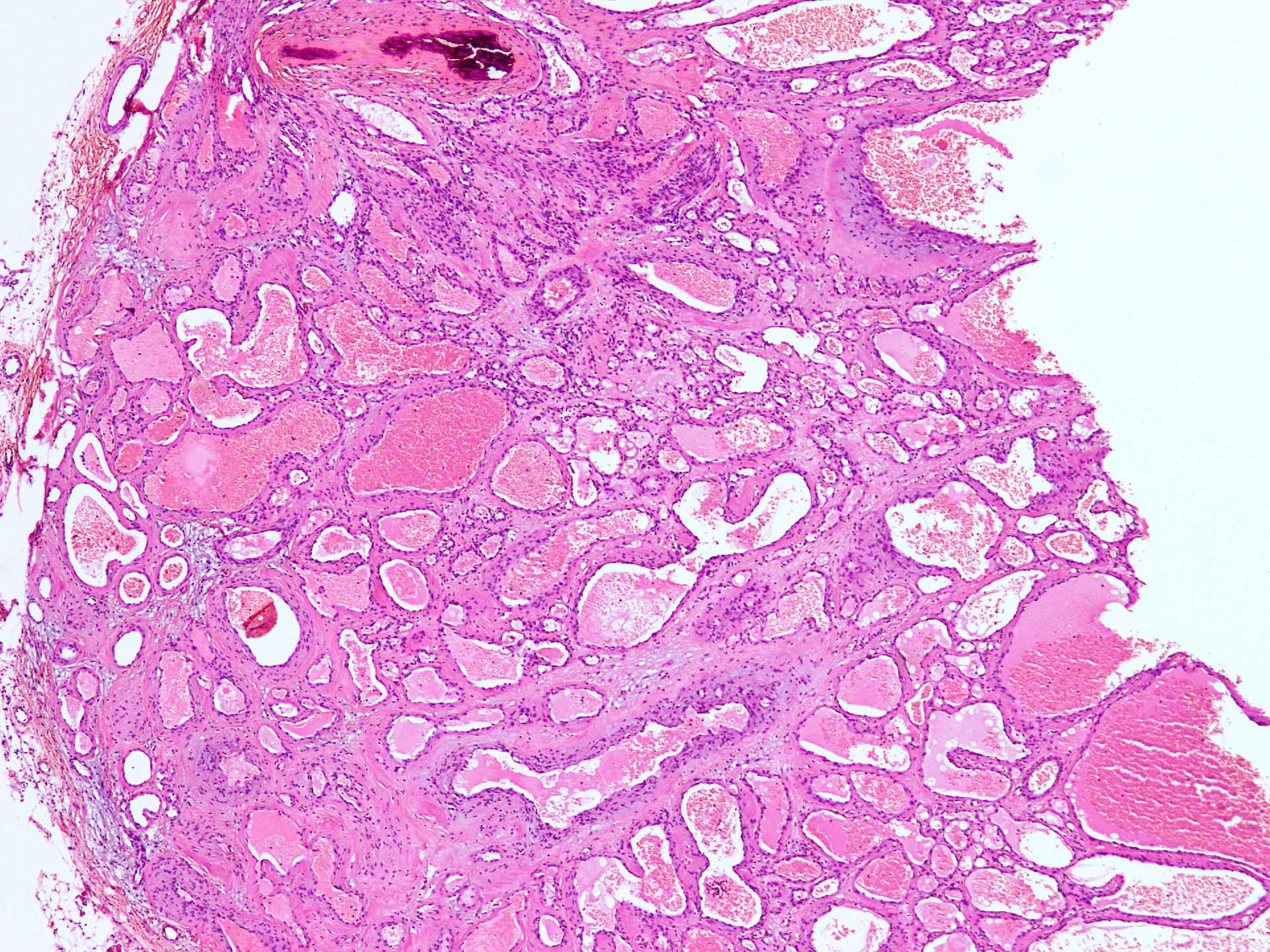
- Cavernous hemangioma: shows predominantly ectatic channels
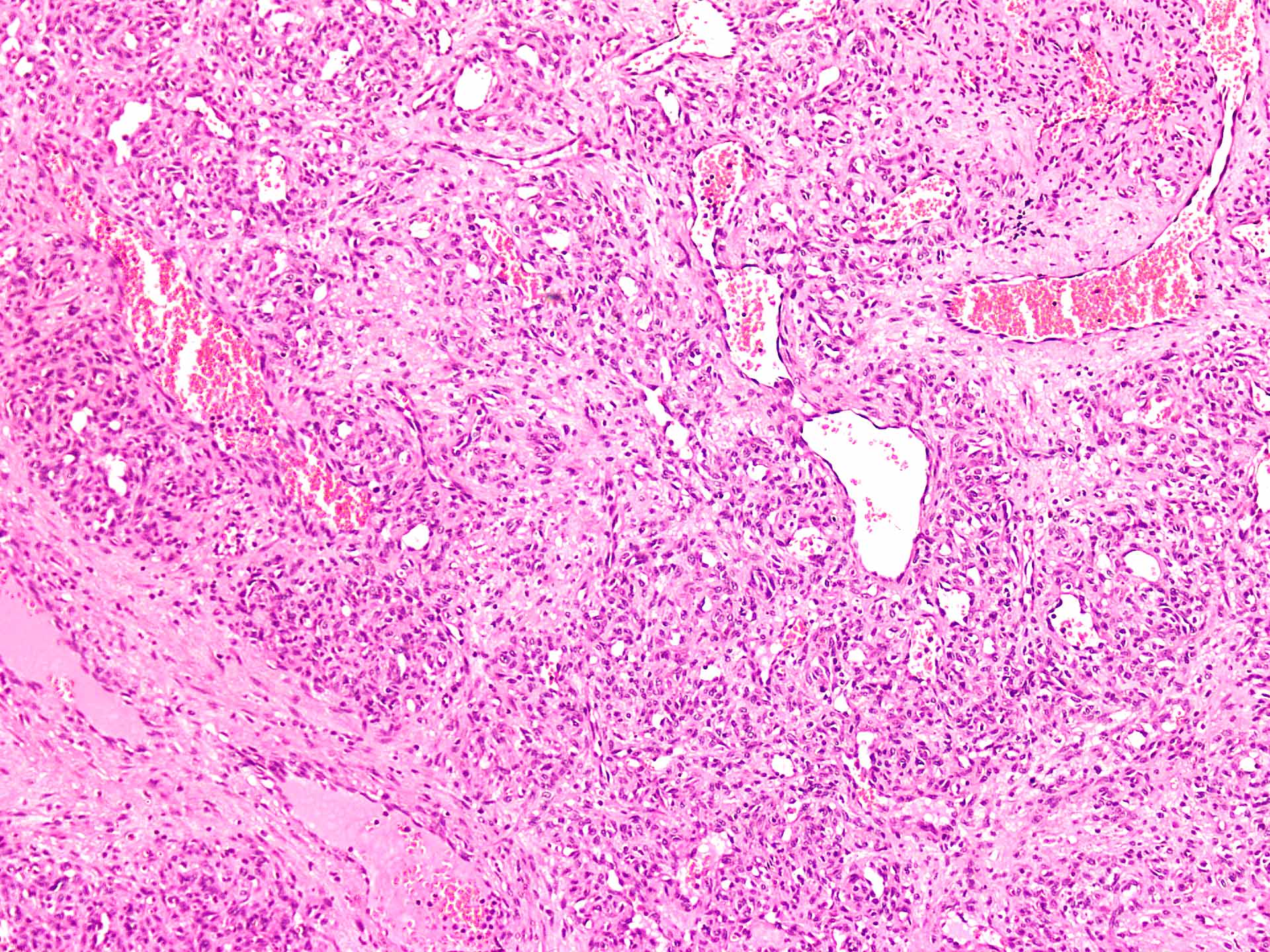
- Congenital hemangioma:
- Solid appearance in rapid growth phase with poorly canalized vessels and mitotically active endothelium
- Surrounding pericyte layer is present
- With maturation, the lumina become prominent and blood flow ensues
- Combination of solid and vascular areas in varying proportions may be seen
- Noninvoluting congenital hemangioma (NICH) shows well formed capillaries and vascular channels
- Involuting examples show thickening of basement membranes and fibrosis in the background
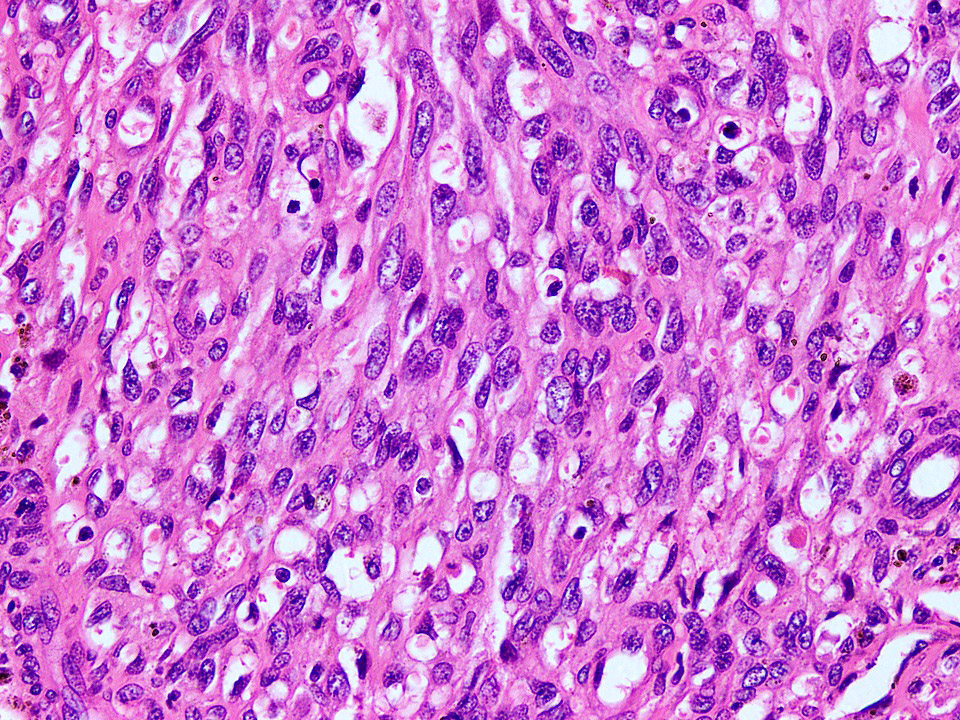
- Epithelioid hemangioma:
- Well formed small vessels are lined by plump endothelial cells with abundant eosinophilic cytoplasm and round enlarged nuclei, accompanied by abundant eosinophils in the background
- Lobulated, well demarcated with maturation of vascular lumina at the periphery
- Glomeruloid hemangioma: resembles glomerular capillaries
- Hobnail hemangioma: hobnail nuclei protruding into vascular lumina; circumscribed
- Infantile hemangioma:
- Proliferation of capillary lobules; has a distinct natural history involving three stages (i.e., proliferation, partial regression and complete regression):
- Early proliferative stage: lobules of immature dendritic type cells with intervening stroma, large feeding vessels and occasional presence of perineural involvement
- Early regression: capillaries dilate and eventually start disappearing; apoptotic debris in basement membrane with increased numbers of pericapillary mast cells.
- Late regression / end stage: ghosts of capillaries, rings of basement membrane with rare endothelial cells having immunophenotype of placental capillaries (GLUT1, LeY, CD15, CCR6, IDO and IGF2 positive)
- Proliferation of capillary lobules; has a distinct natural history involving three stages (i.e., proliferation, partial regression and complete regression):
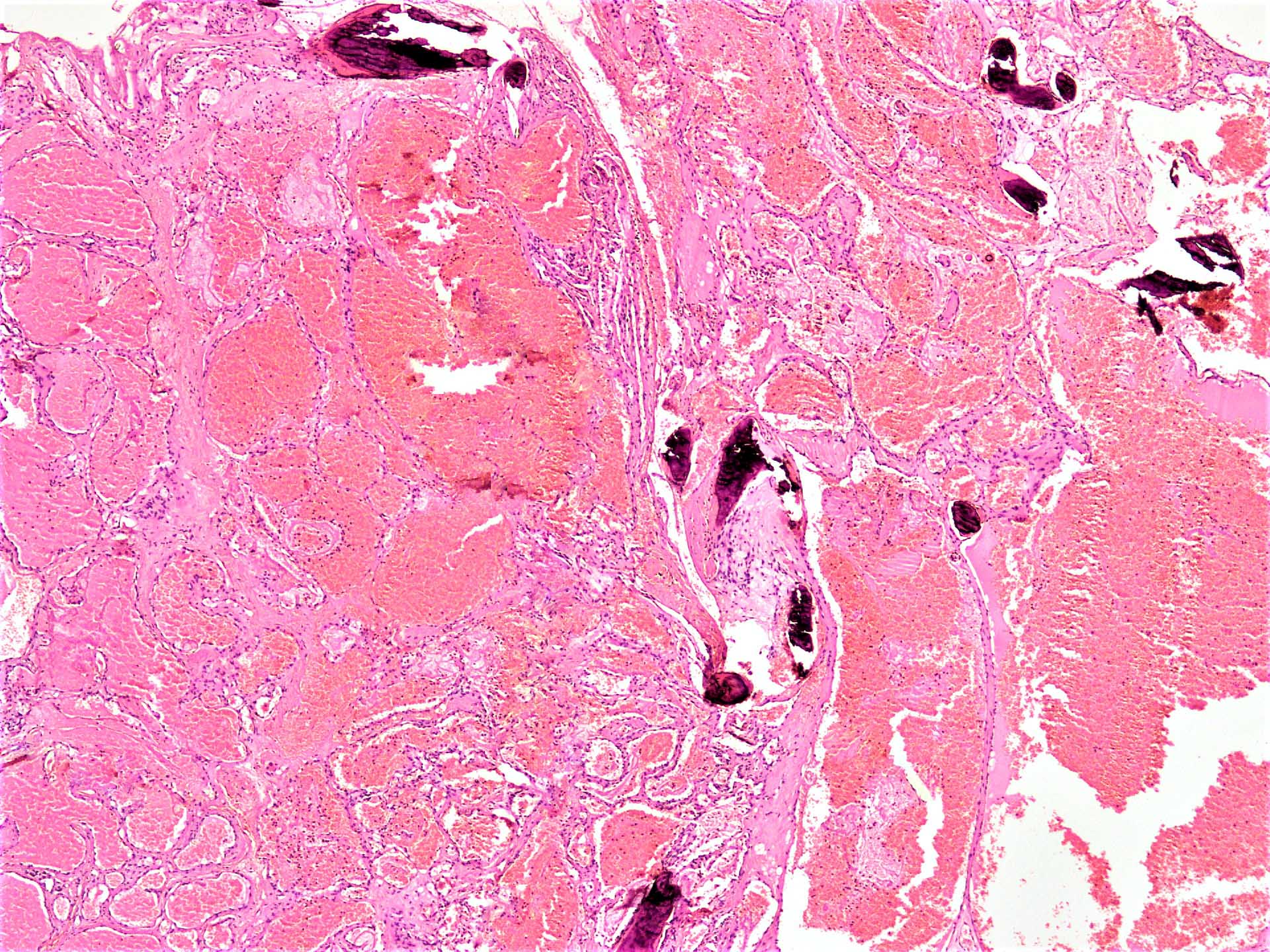
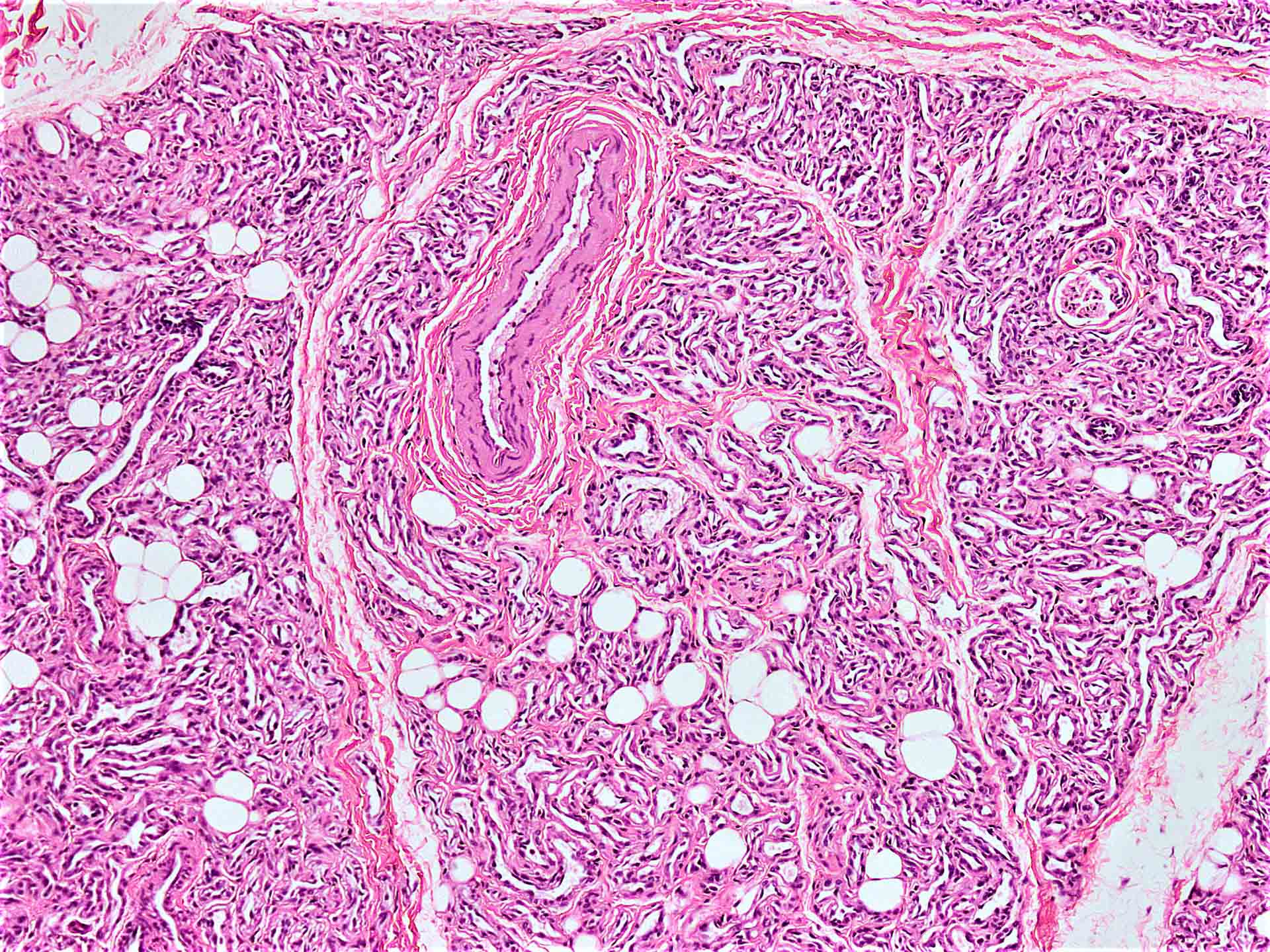
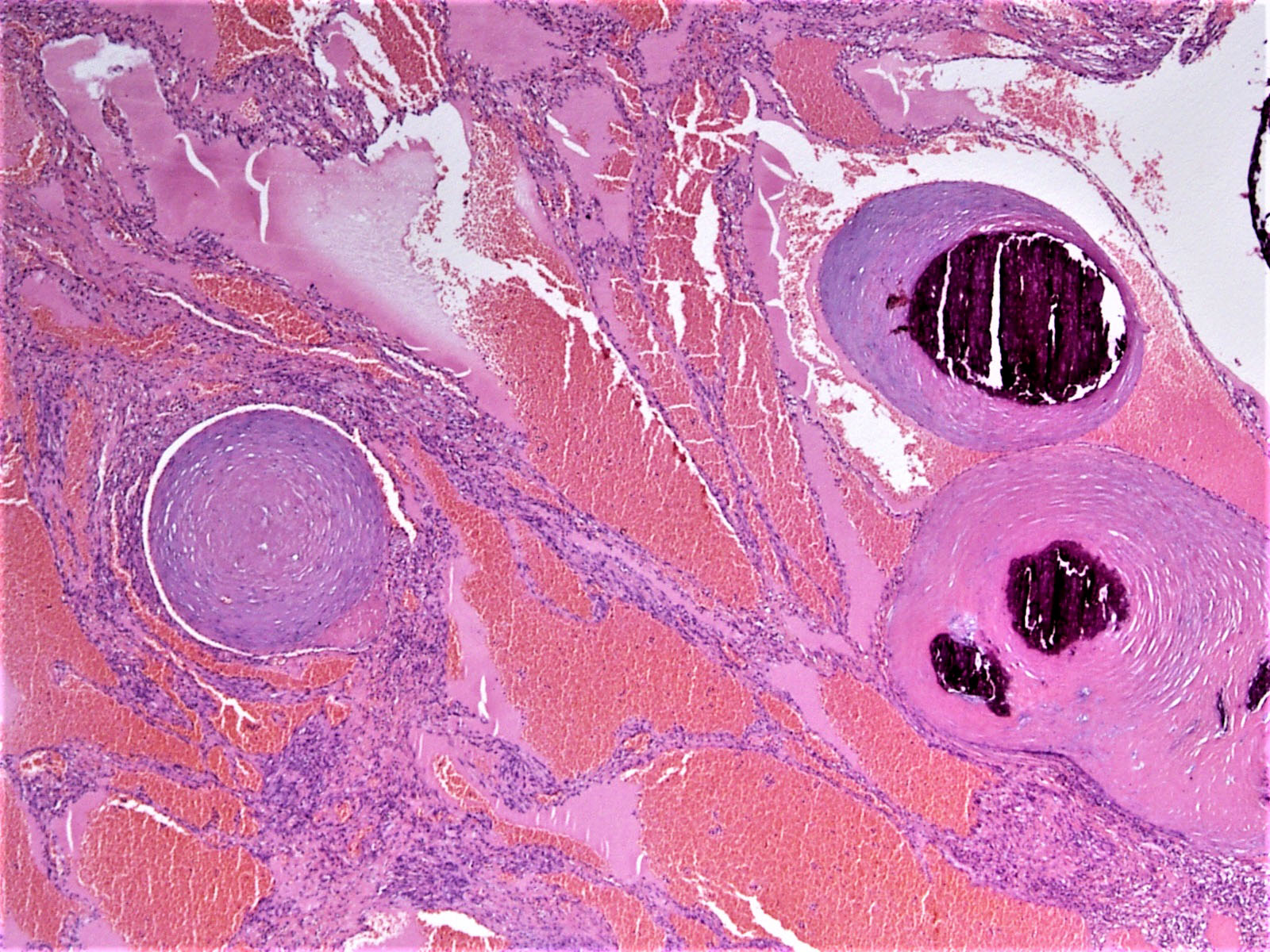
- Intramuscular angioma:
- Arises within skeletal muscle in association with variable amount of mature adipose tissue, phleboliths and metaplastic bone formation
- Shows a combination of lymphatics, variable sized veins and arteriovenous component
- Lobular capillary hemangioma / pyogenic granuloma: ulceration with dense mixed inflammation
- Microvenular hemangioma:
- Poorly defined, in superficial and deep dermis
- Small venule-like channels lined by single layer of endothelial cells which lack mitotic activity, surrounded by single layer of pericytes; these venules appear to dissect hyalinized collagen bundles of the dermis but lack multilayering and HHV8 positivity
- Sinusoidal hemangioma:
- Well demarcated proliferation of dilated, congested and thin vascular channels anastomosing in a sinusoidal manner
- Intervening stroma is scant and scant smooth muscle may be present in the wall
- Mitotic activity is not seen
- Spindle cell hemangioma: proliferating spindle cells with intraluminal phleboliths
- Verrucous hemangioma: hyperkeratosis and involvement of several tissue planes
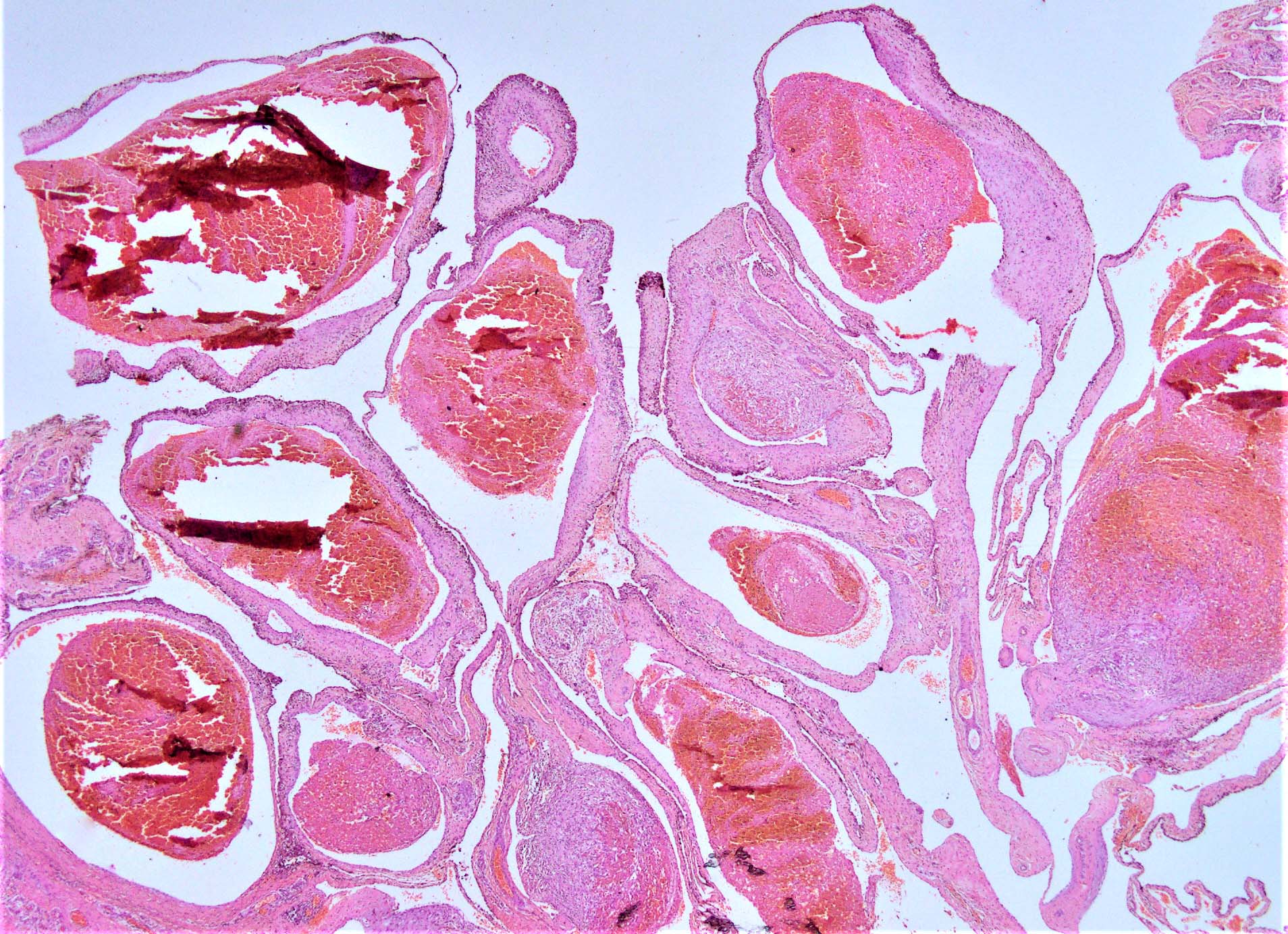
Microscopic (histologic) images
Contributed by Nasir Ud Din, M.B.B.S.
Virtual slides
Cytology description
- Aspiration is not advised, as there is high risk of uncontrolled bleeding
Positive stains
- CD31 (PECAM1): cytoplasmic and membranous positivity; highly sensitive and very specific for vascular differentiation
- CD34: cytoplasmic and membranous positivity; less specific
- ERG: nuclear positivity, stains all vascular tumors, more specific than FLI1
- GLUT1: positive in infantile hemangioma and negative in congenital hemangioma
- FLI1: nuclear positivity; stains all vascular tumors
- von Willebrand factor (vWF): granular cytoplasmic positivity
- Thrombomodulin (CD141): cytoplasmic positivity
- Ulex europaeus agglutinin I (UEAI): membranous staining, sensitive but nonspecific, also stains epithelial cells (Arch Histol Cytol 2004;67:187)
- Claudin5: component of endothelial tight junctions; highly sensitive but less specific
- Podoplanin (D2-40): more specific for lymphatic differentiation (Blood 2019;134:1912)
- Vascular endothelial growth factor receptor 3 (VEGFR3): membrane staining
- PROX1: suggested marker of neoplastic endothelial cells (Am J Surg Pathol 2012;36:351)
- CIZ1: nuclear protein; upregulated in mucosal hemangiomas (Pathol Oncol Res 2019;25:1653)
- WT1: variable cytoplasmic positivity in vascular neoplasms (Am J Dermatopathol 2011;33:569)
Negative stains
- HHV8: kaposi sarcoma (Arq Bras Oftalmol 2021 Sep 10 [Epub ahead of print])
- TFE3: high grade epithelioid hemangioendothelioma (Mod Pathol 2020;33:591)
- SMA: pericytes and vascular smooth muscle stain positive
- Desmin: vascular smooth muscle stains positive
- Cytokeratin: variable positivity may be seen in some examples of angiosarcoma; however, mostly negative (Case Rep Med 2016;2016:8919012)
Electron microscopy description
- Not required for diagnosis in routine cases
- Endothelial cells show cytoplasmic folds on luminal surface, junctional complexes and cytoplasmic pinocytic vesicles (Cancer Res 1990;50:4787)
Electron microscopy images
Molecular / cytogenetics description
- Not required for routine diagnosis of hemangioma
- May be helpful in difficult cases
- RASA1 mutations: arteriovenous malformations, Klippel-Trenaunay syndrome, Sturge-Weber syndrome, Parker-Weber syndrome (Am J Hum Genet 2003;73:1240, Br J Dermatol 2008;158:1035, Hereditas 2018;155:24)
- GNAQ mutation: Sturge-Weber syndrome (N Engl J Med 2013;368:1971)
- PDGFRβ and its downstream signaling pathways (PI3K / Akt / mTOR) are activated in infantile hemangioma (J Invest Dermatol 2019;139:1574)
- More relevant in intermediate and malignant vascular lesions
Videos
Spindle cell hemangioma
Cutaneous vascular tumors
Sample pathology report
- Liver, lobectomy:
- Benign vascular lesion, consistent with hemangioma (see comment)
- Comment: The tumor is completely excised with free margins. Evidence of embolization is seen, with presence of acellular material within the lumina of large caliber vessels, accompanied by areas of infarction within the lesion.
Differential diagnosis
- Granulation tissue:
- Sites of trauma, commonly cutaneous or mucosal
- Shows associated inflammatory infiltrate and edema
- Feeding vessels are not seen commonly
- Lobular capillary hemangioma is common mimicker
- Correlation with clinical history is important
- Hemangioendothelioma:
- Mimics proliferating phase of congenital hemangioma
- Retiform type mimics hobnailing seen in proliferating phase of congenital hemangioma
- Not well circumscribed
- Clinical presentation with consumptive coagulopathy is common in both
- May be associated with other anomalies
- Requires more aggressive treatment
- Kaposi sarcoma:
- Mimics proliferating phase of congenital hemangioma due to compact cellularity and slit-like spaces
- Eosinophilic hyaline globules are not seen in hemangioma
- HHV8 association is not seen in hemangioma
- Requires aggressive treatment
- Angiosarcoma:
- Malignant vascular tumor with infiltrative growth
- Marked nuclear pleomorphism and brisk mitotic activity
- Visceral location is more common compared to hemangioma
Additional references
Board review style question #1
A newborn shows a nodular growth on his scalp. Over the next couple of weeks, the lesion starts shrinking. Despite reassurances from the pediatrician, the parents insist on excision. Upon pathological examination, it shows a network of capillary sized vessels with large feeding vessels near the base, shown in the above photomicrograph. The diagnosis in this case is
- Infantile hemangioma
- Noninvoluting hemangioma
- Partially involuting hemangioma
- Rapidly involuting hemangioma
Board review style answer #1
A. Infantile hemangioma. This case is an example of infantile hemangioma, which typically shows regression after birth, unlike congenital hemangioma, which grows with the patient, at least to some extent. Within the umbrella of congenital hemangioma, there is partial involution over time with shrinkage and secondary changes. Noninvoluting examples grow with the baby and rapidly involuting ones regress at a much faster rate, ultimately disappearing completely.
Comment Here
Reference: Hemangioma
Comment Here
Reference: Hemangioma
Board review style question #2
A 9 year old boy presents with a purple nodular / bosselated lesion on the left leg, with involvement of the plantar and dorsal aspects of foot (as shown in the clinical photograph). He has had this lesion since birth and it has grown with him since then. The microscopic examination shows well formed vascular channels of variable size lined by a single layer of endothelial cells. The most likely diagnosis in this case is
- Birth mark
- Infantile hemangioma
- Kaposiform hemangioendothelioma
- Lobular capillary hemangioma
- Noninvoluting congenital hemangioma
Board review style answer #2
E. Noninvoluting congenital hemangioma. Noninvoluting congenital hemangioma is present at birth and grows with the child. As the name implies, there is no microscopic evidence of involution if a biopsy is performed. Birth marks commonly present with a flat, pigmented / reddish appearance of the skin rather than the appearance given in the clinical photograph, which shows prominent vascular marking, like the appearance of the lesion with some areas showing bosselation. Infantile hemangioma rapidly regresses after birth. Lobular capillary hemangioma presents as a nodular growth, commonly associated with ulceration of the skin or mucosa. Kaposiform hemangioendothelioma clinically presents commonly on the head and neck and trunk region, with a strong association with Kasabach-Merritt syndrome (consumptive coagulopathy). Microscopically, it shows glomeruloid proliferation and spindle cell morphology with slit-like spaces on microscopic examination.
Comment Here
Reference: Hemangioma
Comment Here
Reference: Hemangioma