Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nguyen HQ, Phung TL. Kaposiform hemangioendothelioma & tufted angioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuehemangioendotheliomakaposiform.html. Accessed April 1st, 2025.
Definition / general
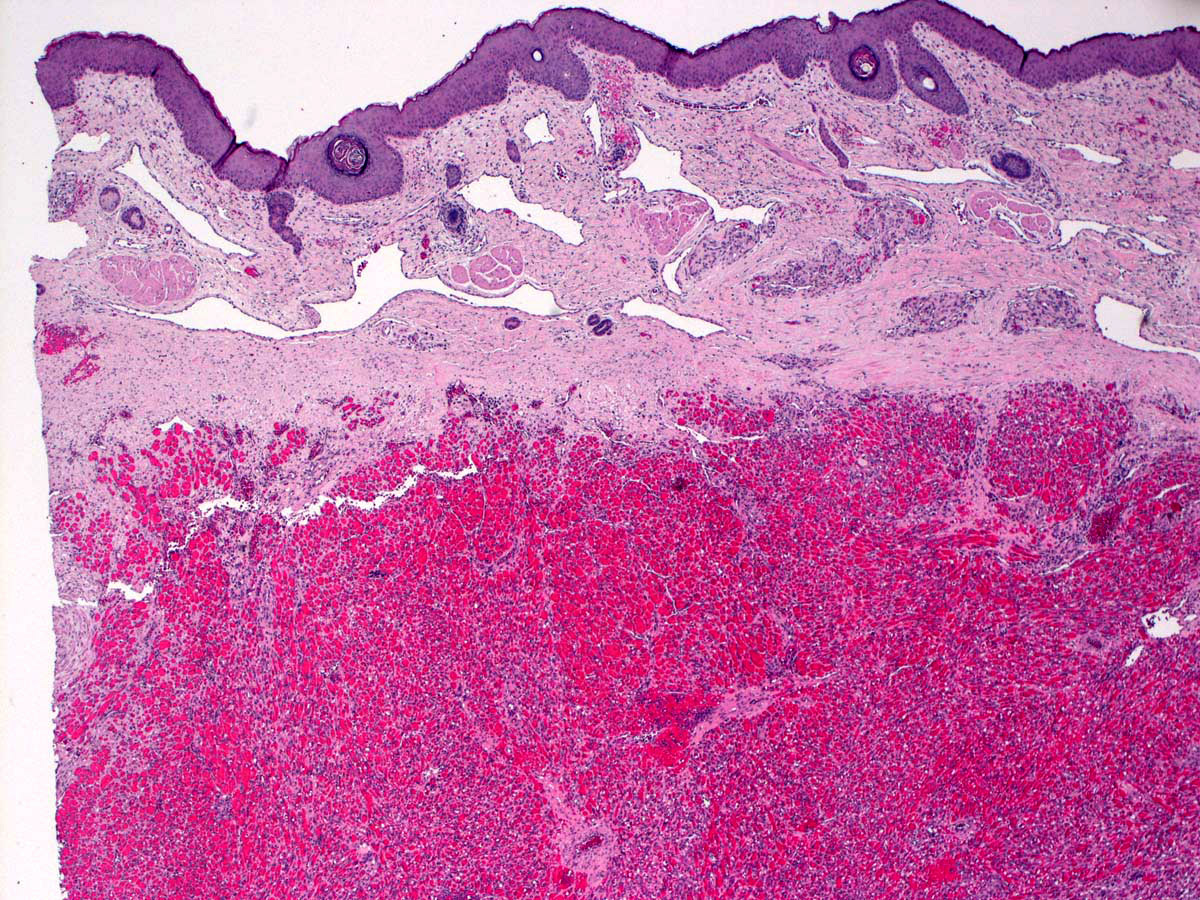
- Kaposiform hemangioendothelioma (KHE) is a rare and locally aggressive endothelial neoplasm that often involves the entire dermis and extends into the subcutaneous tissue
- Characterized by proliferation of spindle shaped endothelial cells and associated capillary hemangioma-like lymphatic vessels
- Predominantly presents in children, often at birth or shortly after birth
- Tufted angioma (TA) is a benign vascular neoplasm that often occurs in children and often presents at birth or shortly after birth
- TA, a more superficial lesion, is otherwise identical to KHE, with KHE representing a more aggressive form with higher morbidity; tufted angioma may spontaneously regress in some cases but KHE does not
- KHE and TA both have strong association with Kasabach-Merritt phenomenon (KMP)
Essential features
- Discrete lobules of capillaries in swirling growth pattern (glomeruloid structures) are typical
- Lymphangioma-like areas, composed of lymphatic vessels at the periphery of nodules of spindle endothelial cells
ICD coding
Epidemiology
- Majority present in infancy to teenage years
- 50% in the first year of life (Br J Dermatol 2018;179:457)
- Adult cases have been reported (Ann Plast Surg 2009;62:456, Cutis 2006;78:341)
Sites
- Most common sites are extremities; may involve the skin and subcutaneous tissue
- Can occur in soft tissue and noncutaneous sites
- Retroperitoneum and peritoneum are frequent extracutaneous sites involved by KHE
- Head and neck, mediastinum and trunk involvement has also been reported (Am J Surg Pathol 2004;28:559, Int J Clin Exp Pathol 2015;8:13711)
Pathophysiology
- Pathogenesis of KHE is poorly understood
- May derive from the lymphatic endothelium (Am J Surg Pathol 2004;28:559)
- Expresses the vascular markers CD31 and CD34
- Expresses vascular endothelial growth factor receptor 3 (VEGFR3), required for lymphangiogenesis
- Expresses the lymphatic markers D2-40 and PROX1
- No reported association with human herpesvirus 8 (HHV8) infection
Etiology
- Etiology is unknown
- Surgical manipulation of KHE or trauma can stimulate Kasabach-Merritt phenomenon (Ann Plast Surg 2009;62:456, J Pediatr Surg 2002;37:E29)
- Likely multifactorial with genetic factors contributing, although mutations are likely sporadic rather than germline
Clinical features
- Usually occurs in infants and children, with 50% occurring in the first year of life
- Cutaneous lesions present with atypical indurated, red to purple plaques with ill defined borders and occasional telangiectasias, without purpura or petechiae
- Typically accompanied by hypertrichosis or hyperhidrosis overlying the lesion
- Most tumors occur in the extremities; less frequently in the trunk, head and neck and mediastinal regions (Am J Surg Pathol 2004;28:559, Int J Clin Exp Pathol 2015;8:13711)
- Deep lesions in the retroperitoneum or intrathoracic region may present as a bluish, purpuric hue on the overlying skin and may be mistaken for a bleeding disorder
- Tumors can cause pain or functional impairment of the involved area (Int J Clin Exp Pathol 2015;8:13711)
- Over 70% of KHE develop Kasabach-Merritt phenomenon, which consists of (J Pediatr 2013;162:142, Pediatr Clin North Am 2010;57:1085):
- Consumptive coagulopathy
- Thrombocytopenia
- Risk is highest in retroperitoneal and intrathoracic tumors and large congenital lesions
- KHE typically does not regress
- Regional lymph node metastases are rare; no distant metastases reported to date
- Mortality is approximately 10%, usually secondary to Kasabach-Merritt phenomenon (Am J Surg Pathol 2004;28:559)
Diagnosis
- Clinical presentation (J Pediatr 2013;163:285):
- KHE is suspected in an infant presenting with atypical indurated, red to purple plaques with ill defined borders; most often in the extremities and trunk
- Lanugo hair hypertrichosis and increased sweating are clues for the diagnosis
- Imaging (J Pediatr 2013;163:285):
- Ultrasound is best for superficial and small lesions
- MRI is generally the first choice assessment due to the deep infiltrating nature of tumors; MRI is also helpful in differentiating KHE from other vascular tumors but mainly is used to investigate the extent of disease and response to treatment
- MRI is recommended in patients presenting with severe unexplained coagulopathy and thrombocytopenia, with coexisting cutaneous purpura, to identify deep seated KHE
- Biopsy of the lesion for microscopic examination is possible and safe; biopsy is not recommended in the presence of severe Kasabach-Merritt phenomenon (Br J Dermatol 2018;179:457)
Laboratory
- Laboratory evaluation includes complete blood count, platelet count, coagulation studies (prothrombin time [PT], partial thromboplastin time [PTT], fibrinogen, D dimer)
- Kasabach-Merritt phenomenon is suspected when there is severe thrombocytopenia, hypofibrinogenemia and elevated D dimer
- Liver and kidney function tests performed in acutely ill patients
- Reference: J Pediatr 2013;163:285
Radiology description
- On MRIs, KHE often displays ill defined margins and multiplanar extension with diffuse enhancement (Orphanet J Rare Dis 2020;15:39)
- T1 weighted imaging shows isointensity compared with adjacent muscle
- T2 weighted imaging reveals hyperintensity
- Changes in adjacent bone or joint are common, including destruction of the cortex or epiphysis and joint invasion
Prognostic factors
- Typically does not regress
- Surgical excision of the tumor is curative in the majority of cases
- Outcome is strongly associated with sites, tumor size and the progression of consumptive coagulopathy (J Pediatr 2013;162:142)
- Mortality rate is about 10% in patients with Kasabach-Merritt phenomenon; however, it is decreasing due to better pharmacologic therapy and supportive care (N Engl J Med 2004;350:1764)
- Most common cause of death includes hemorrhage, sepsis and organ failure
Case reports
- Newborn baby girl with a firm, nonblanchable, purple plaque on the right lateral lower leg (Am J Dermatopathol 2018;40:231)
- 21 month old boy with tumor in the basitemporal region presenting as epistaxis (Childs Nerv Syst 2021;37:2057)
- 3 year old boy presented with swelling below the knee and violet skin lesion (Clin Sarcoma Res 2020;10:12)
- 5 year old girl with sudden onset of bilateral lower limb weakness and back pain following a fall (Int J Spine Surg 2020;14:426)
- 9 year old girl presented with a 2 year history of pain and swelling in the left leg (Am J Case Rep 2019;20:1923)
- 38 year old man with tumor growing under the left tongue (Curr Oncol 2016;23:e517)
Treatment
- Various treatment modalities, including surgical resection, pulsed dye laser and multiple pharmacological agents have been reported based on limited case series, case reports and clinical experience without large observational studies or randomized trials
- Surgical resection is considered cured; however, complete resection is not always possible due to poorly defined margins, involvement of vital organs or accompanied Kasabach-Merritt phenomenon
- Pharmacologic therapy is recommended in KHE with symptomatic Kasabach-Merritt phenomenon and showed positive results, including reducing tumor mass, improving symptoms and resolving coagulopathies
- Embolization may be useful in decreasing tumor mass before starting pharmacologic therapy
- Radiation therapy is used as last resort treatment for tumors refractory to other therapies (J Pediatr 2013;163:285, Dermatol Pract Concept 2015;5:91, World J Pediatr 2018;14:322)
Clinical images
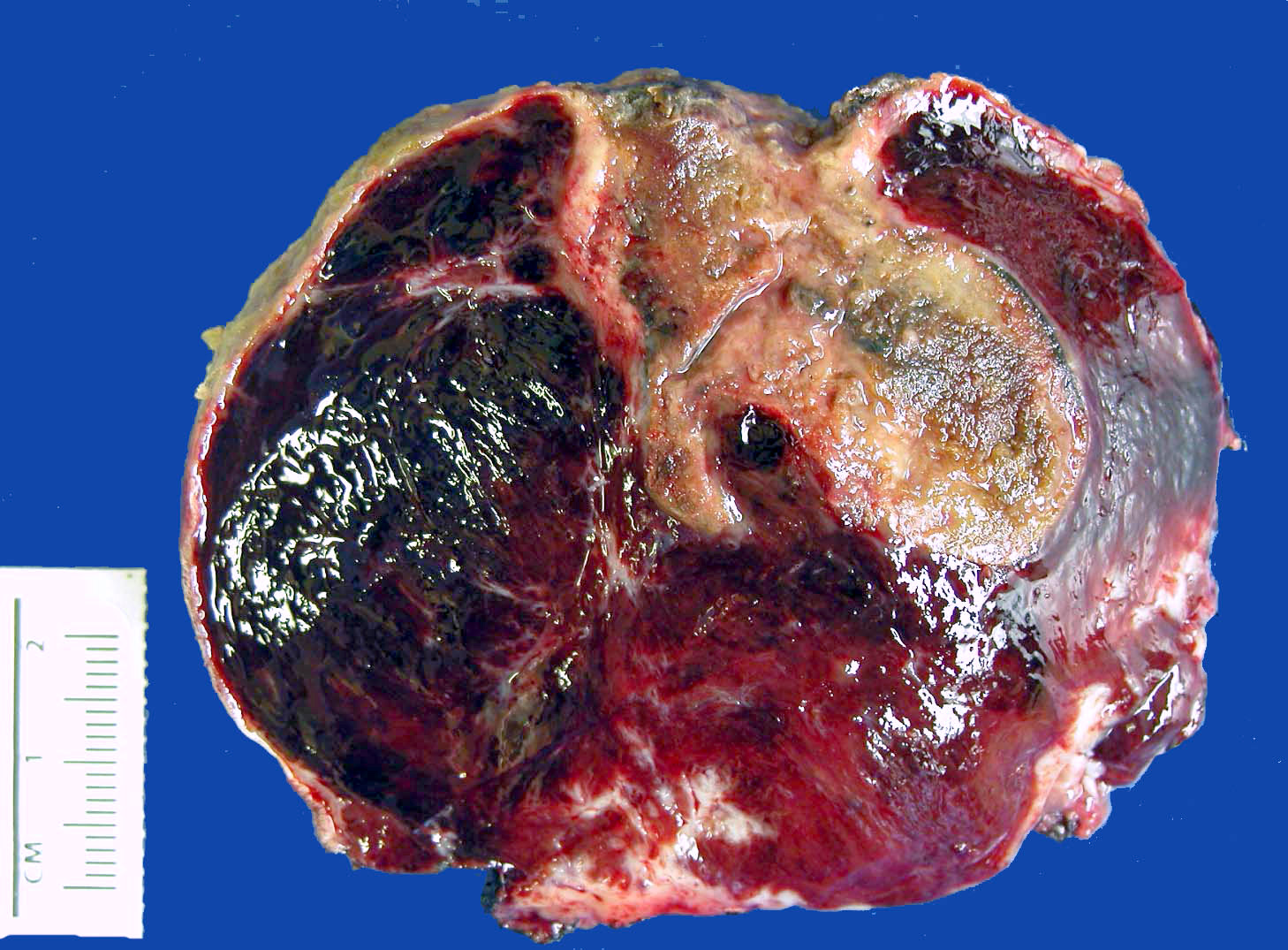
Gross description
- Skin: ill defined violaceous plaques and occasional telangiectasias, without purpura or petechiae
- Deep soft tissue: multiple nodules with associated prominent desmoplasia as tumor infiltrates
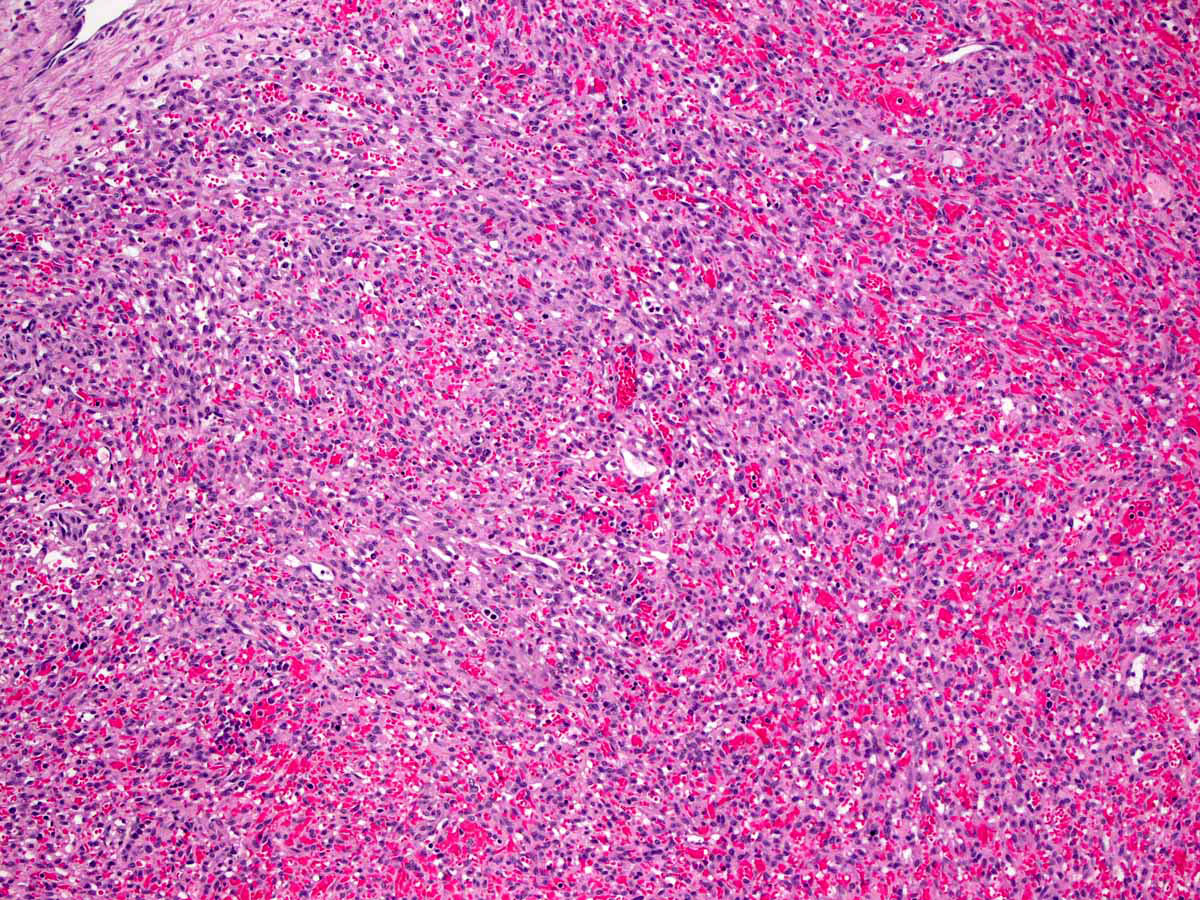
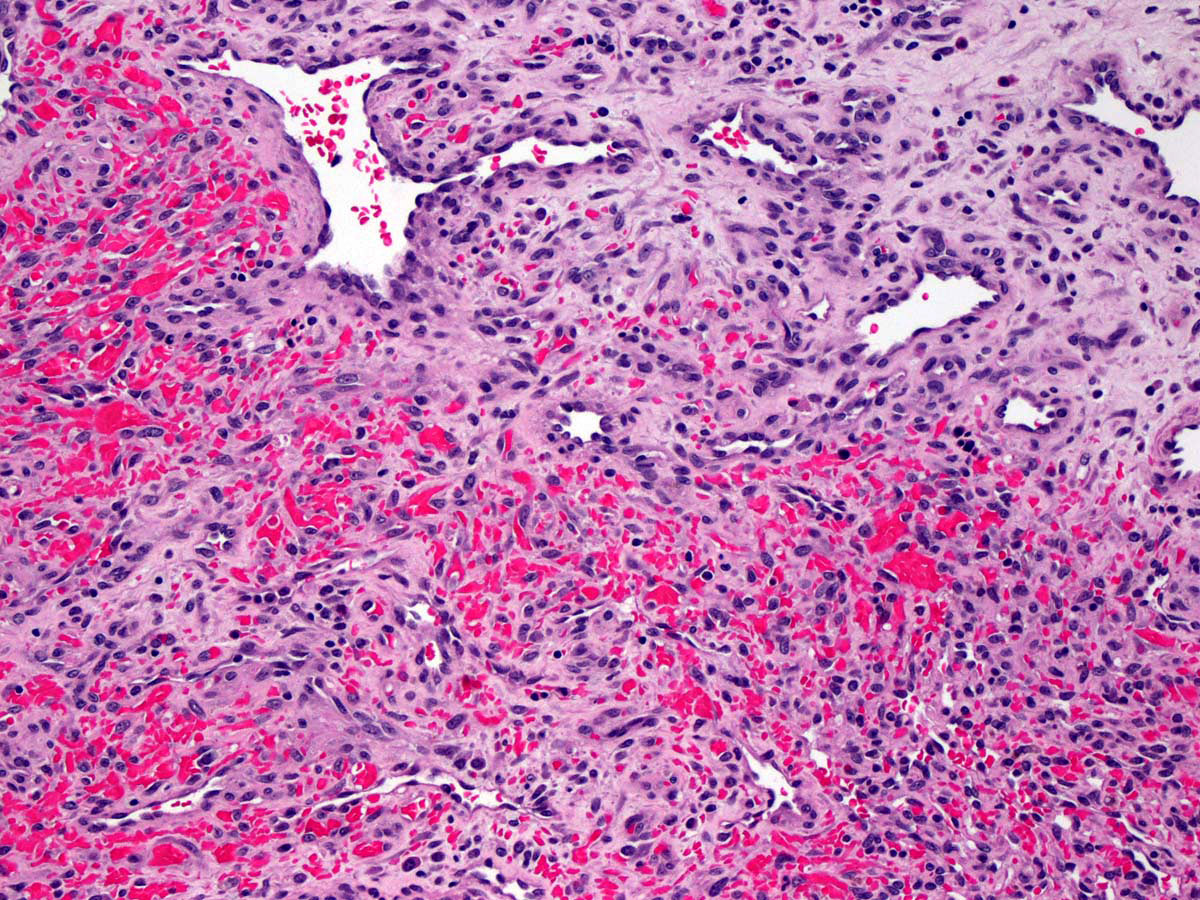
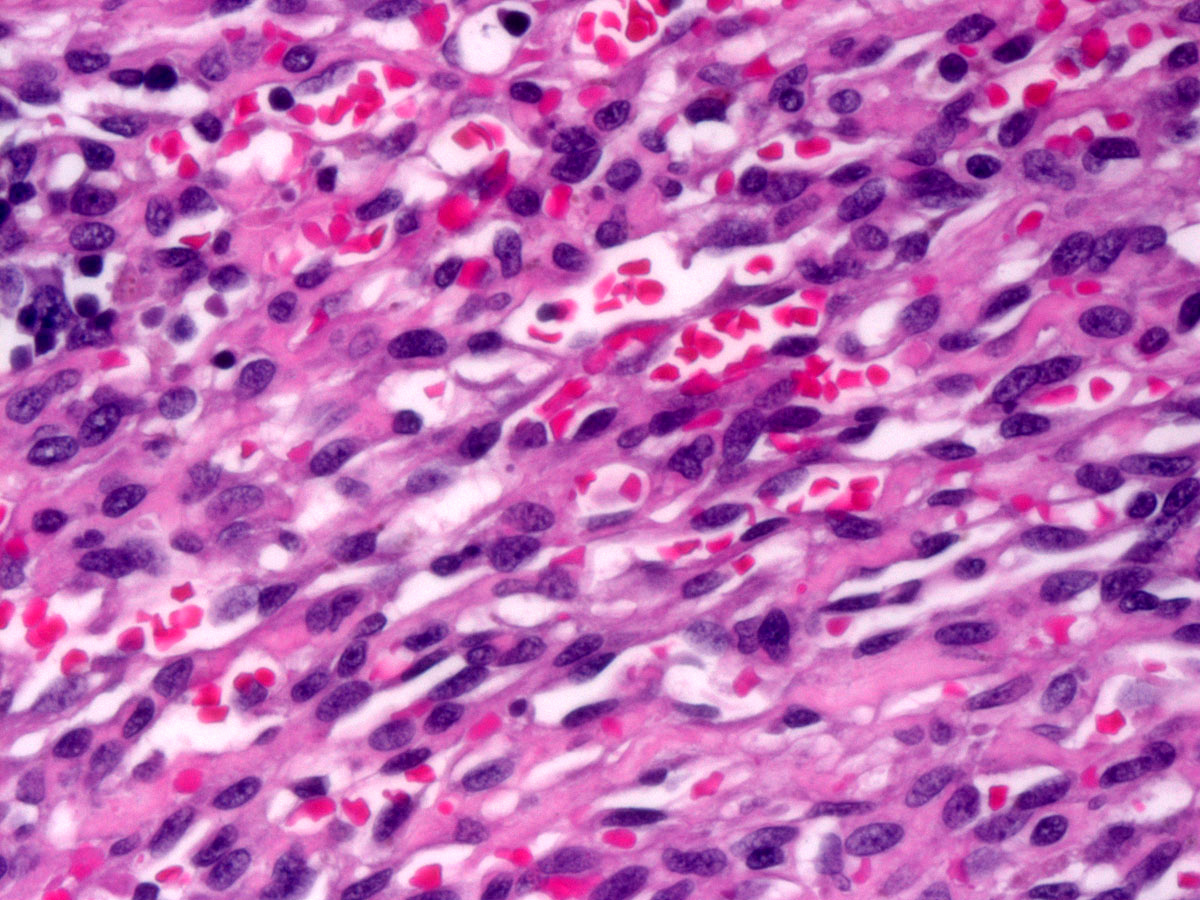
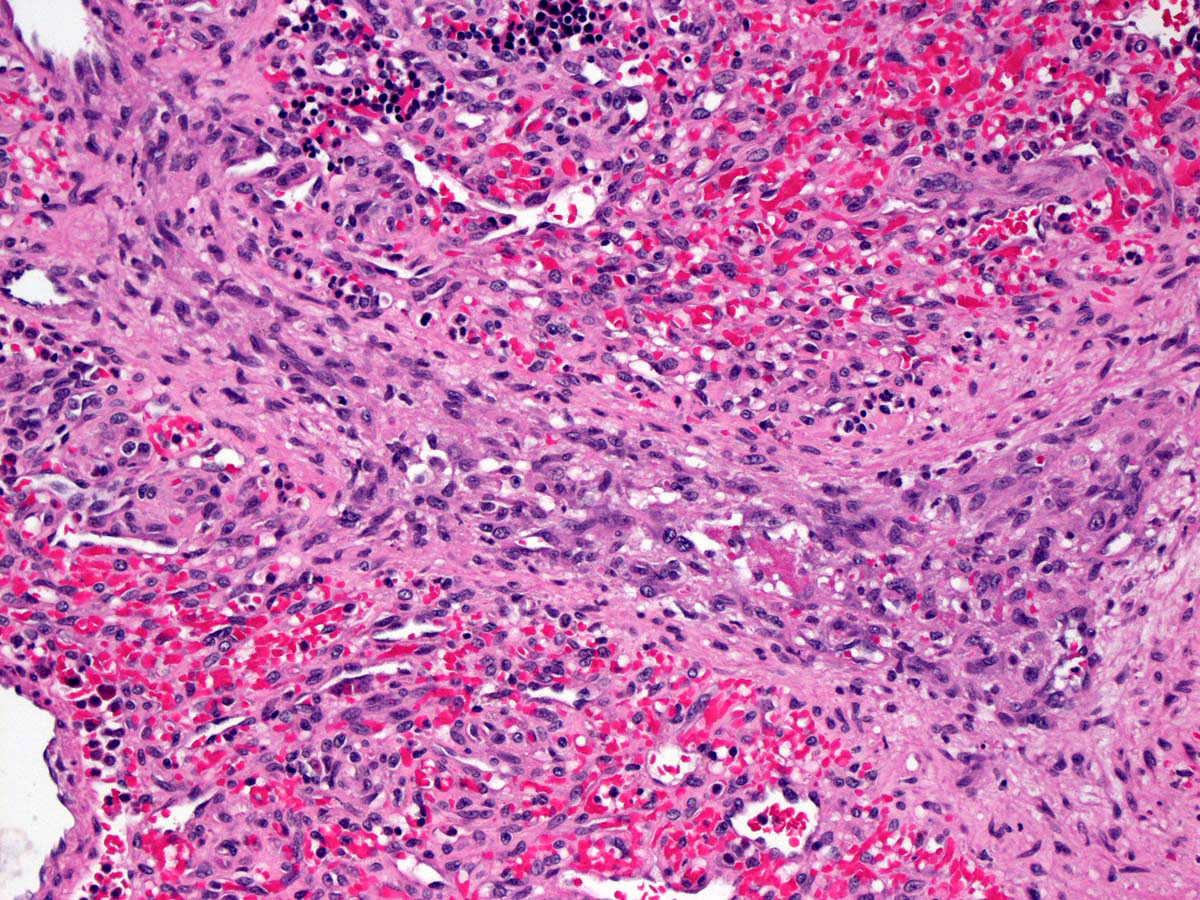
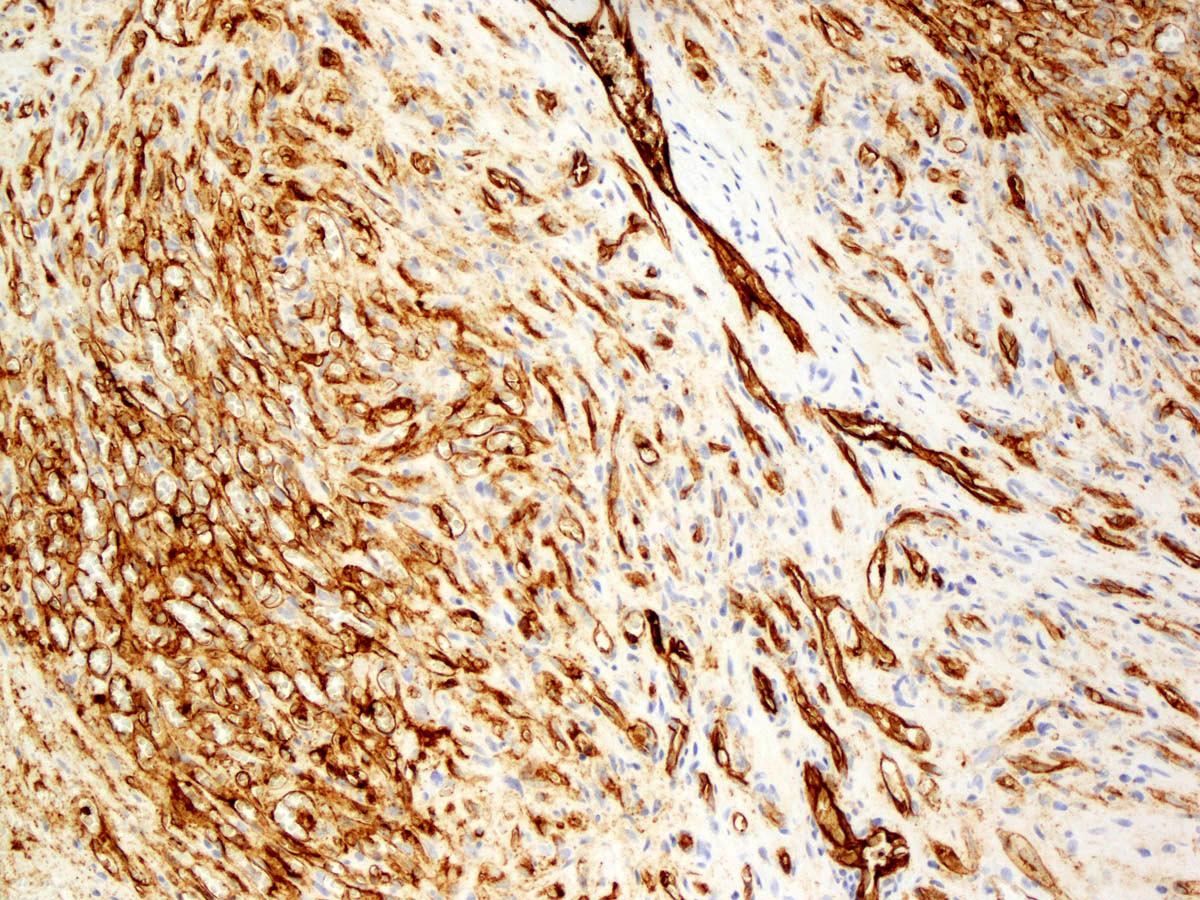
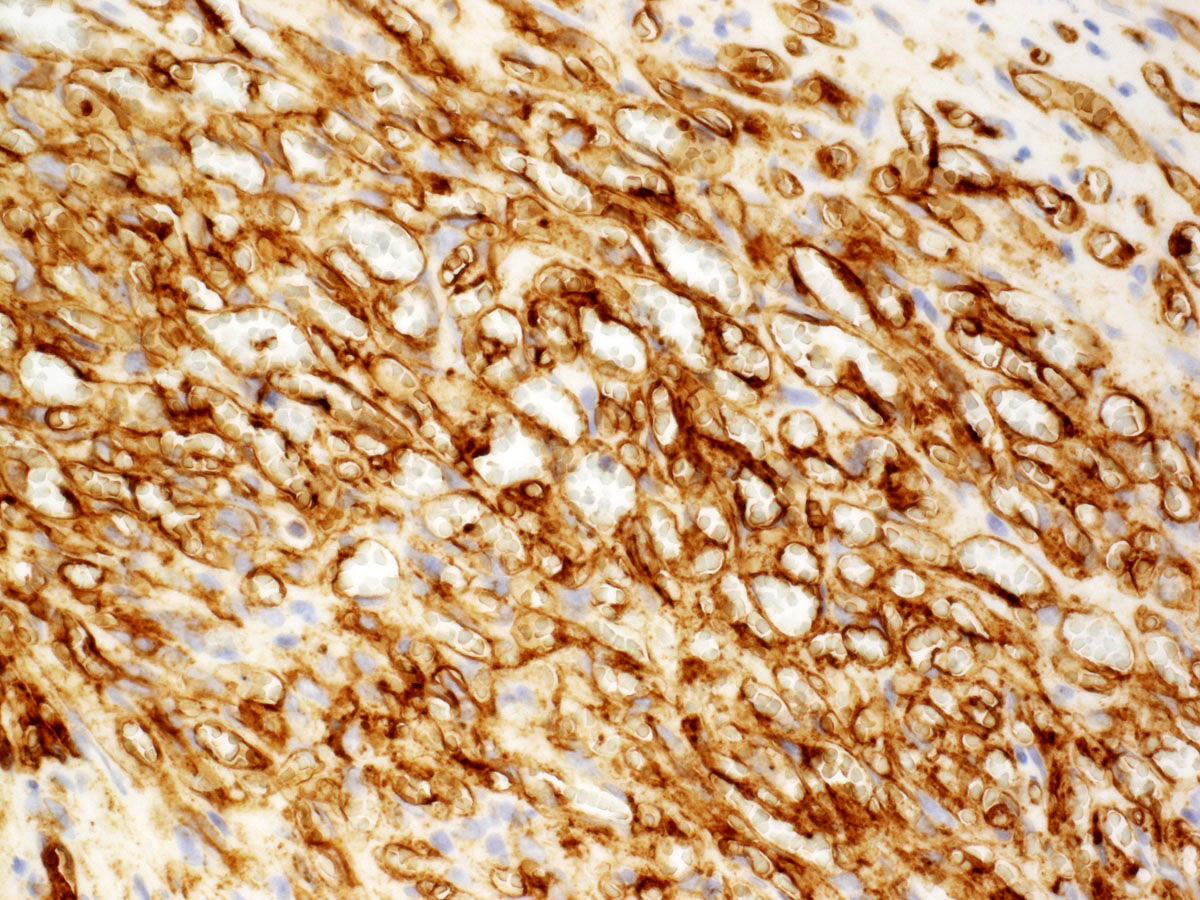
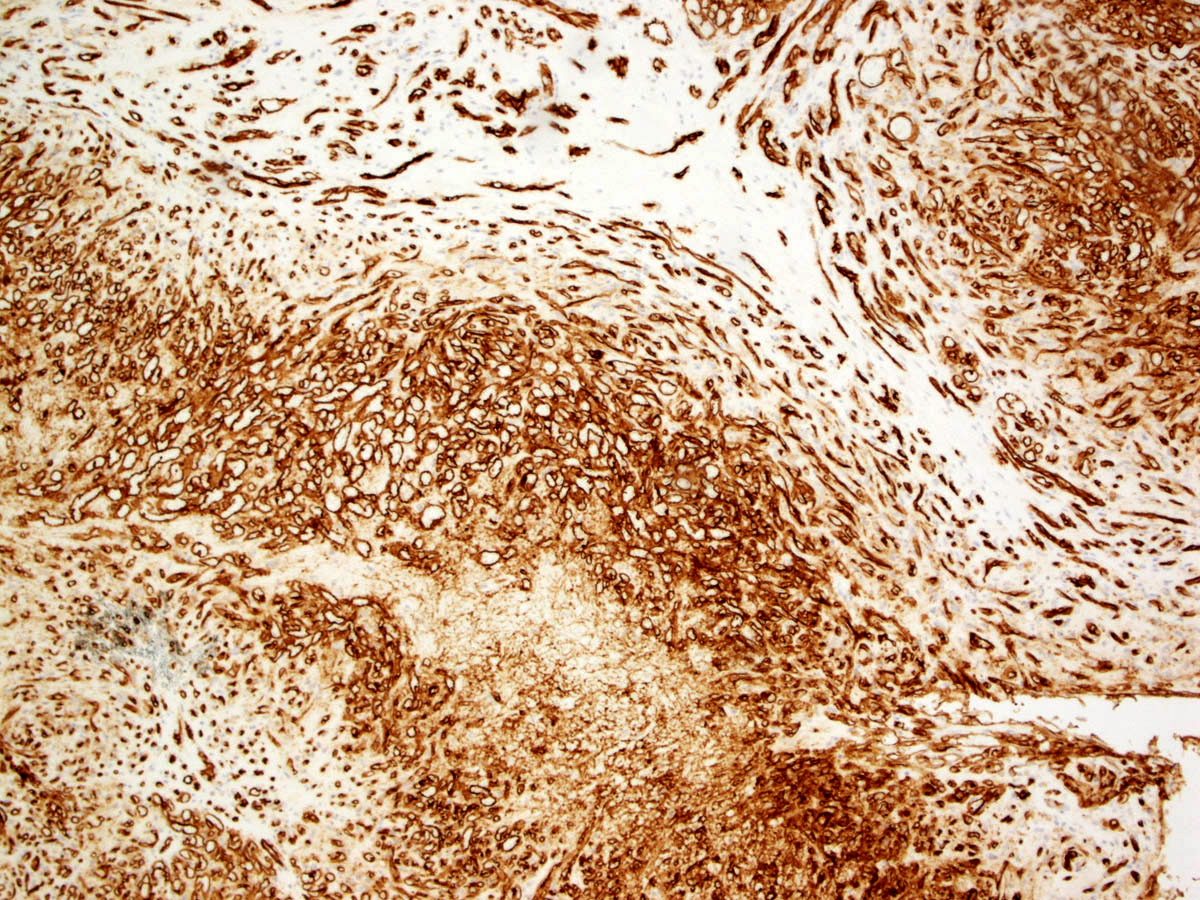
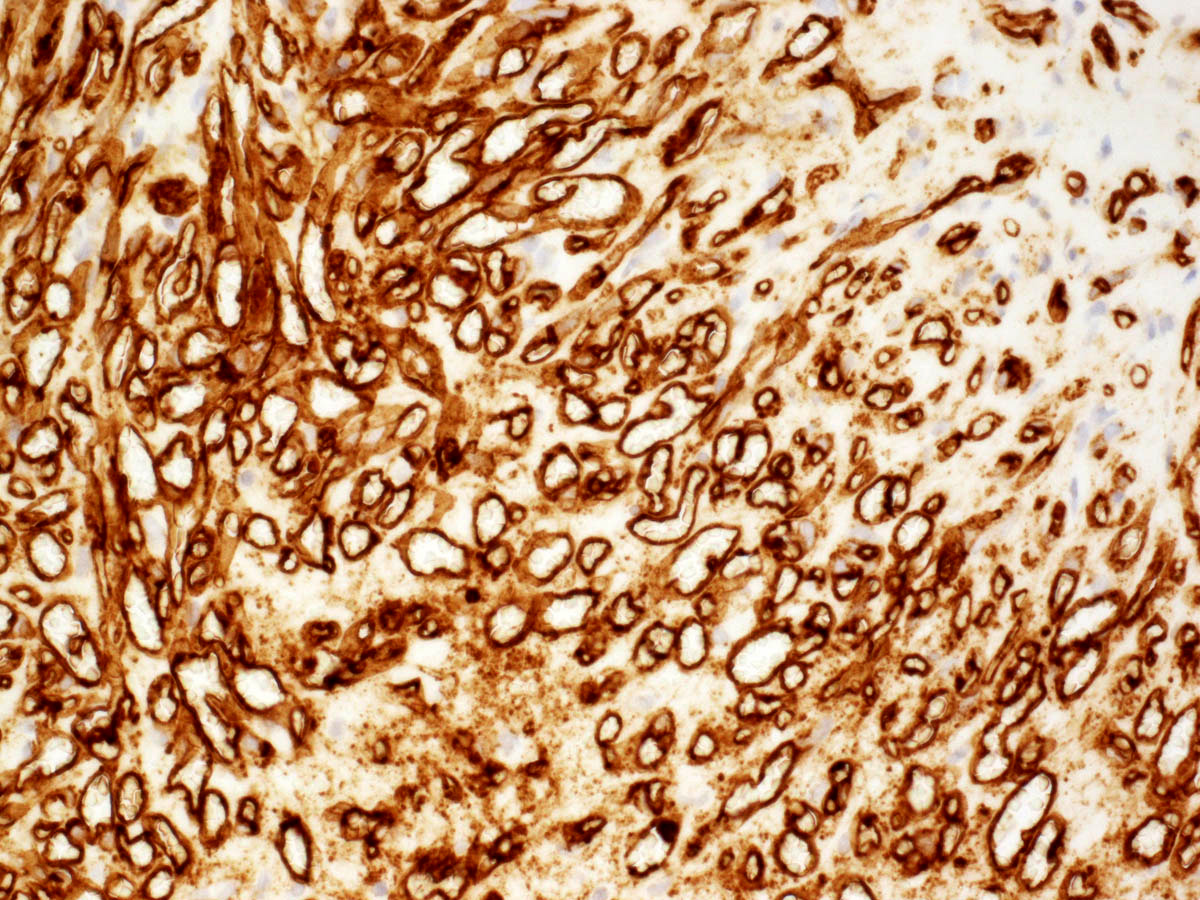
Microscopic (histologic) description
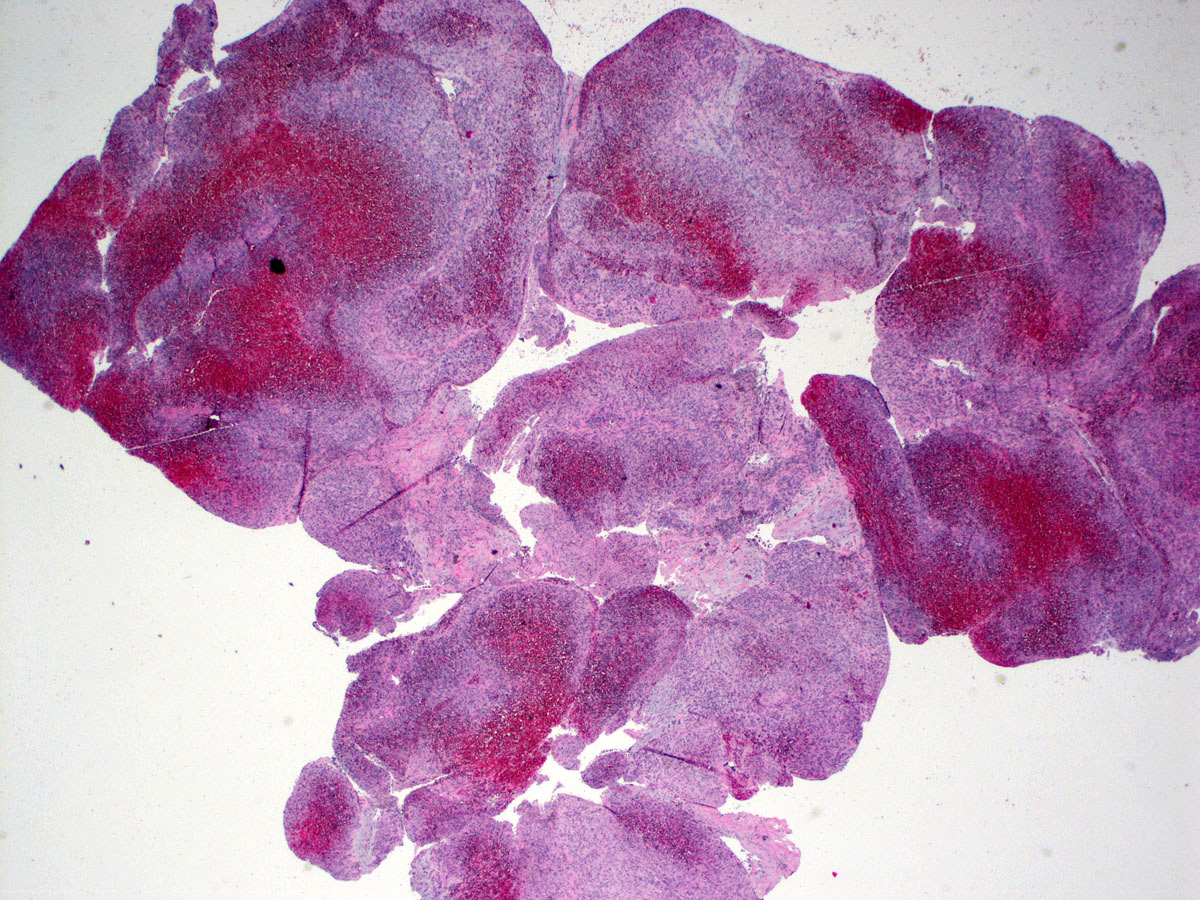
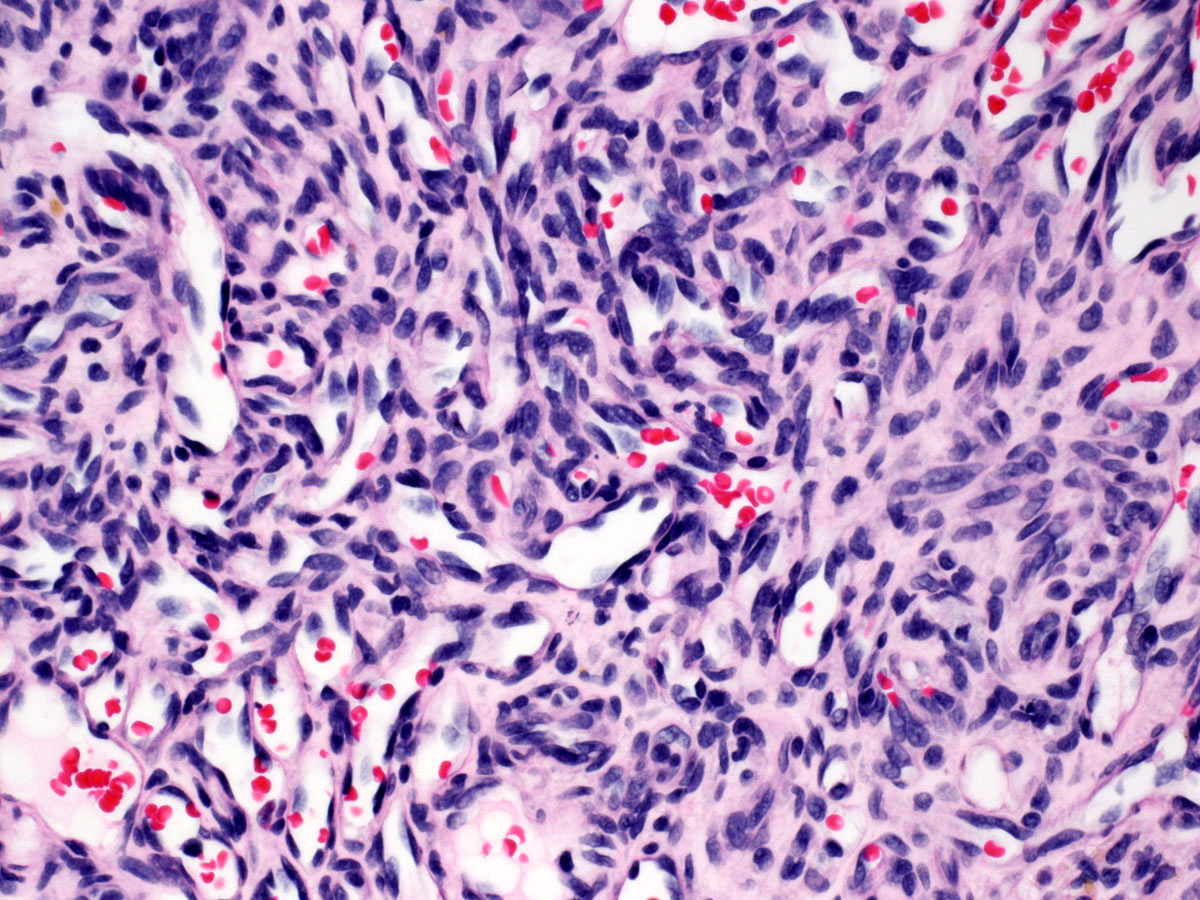
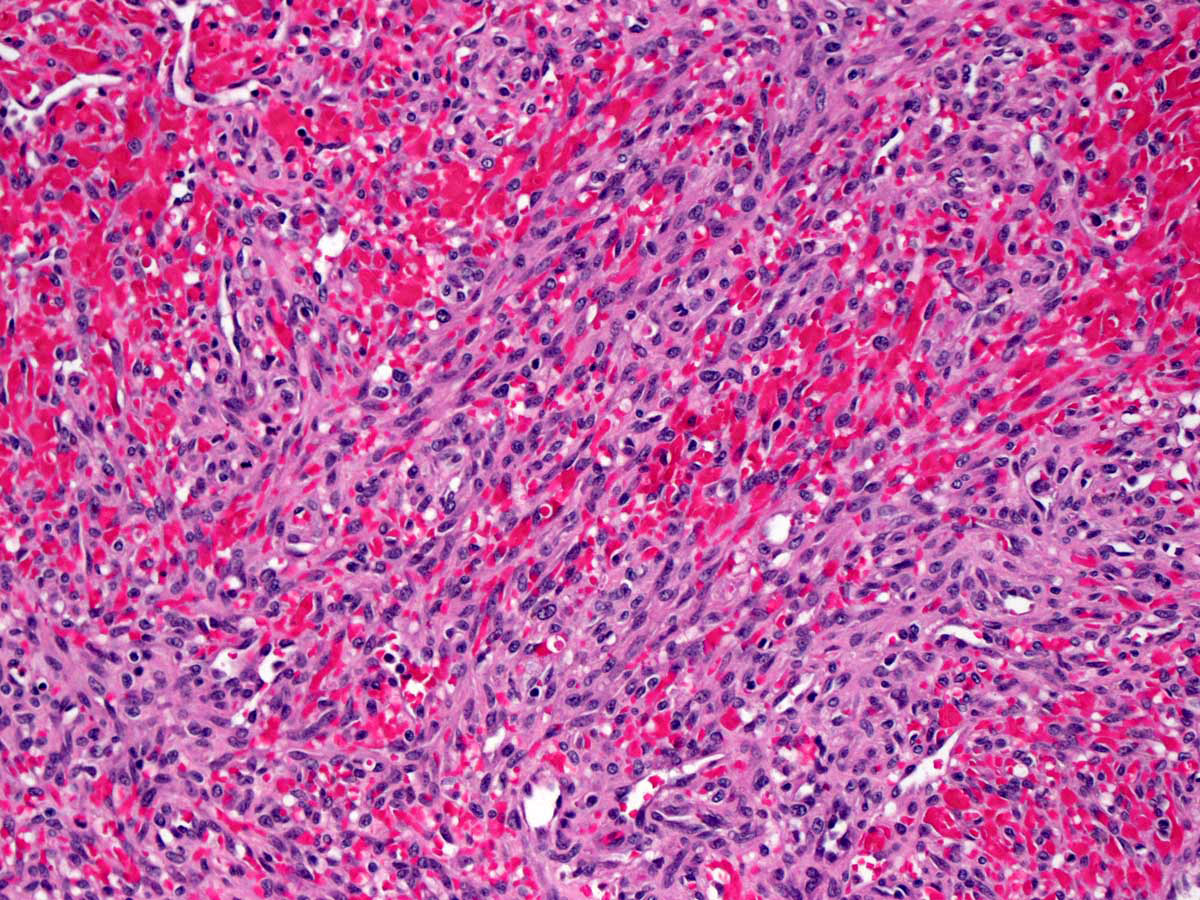
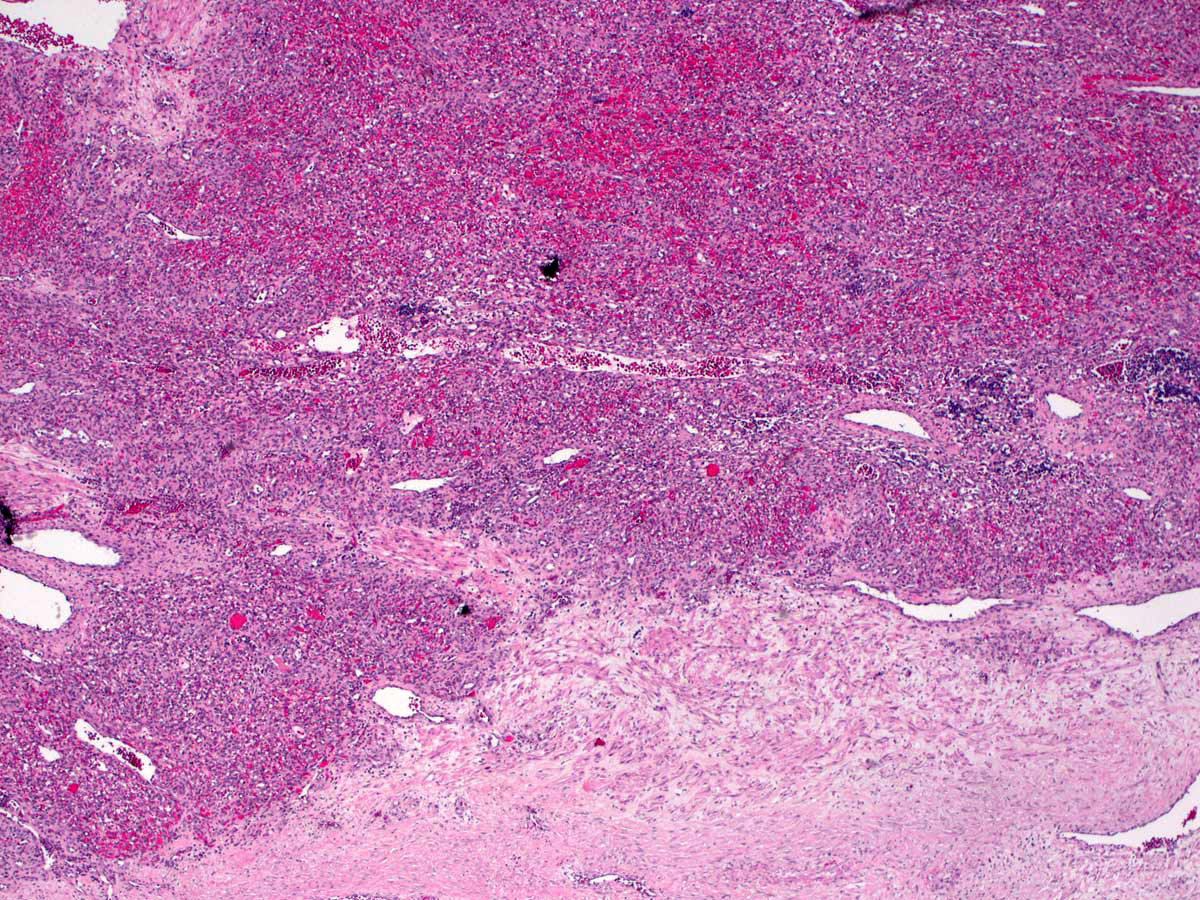
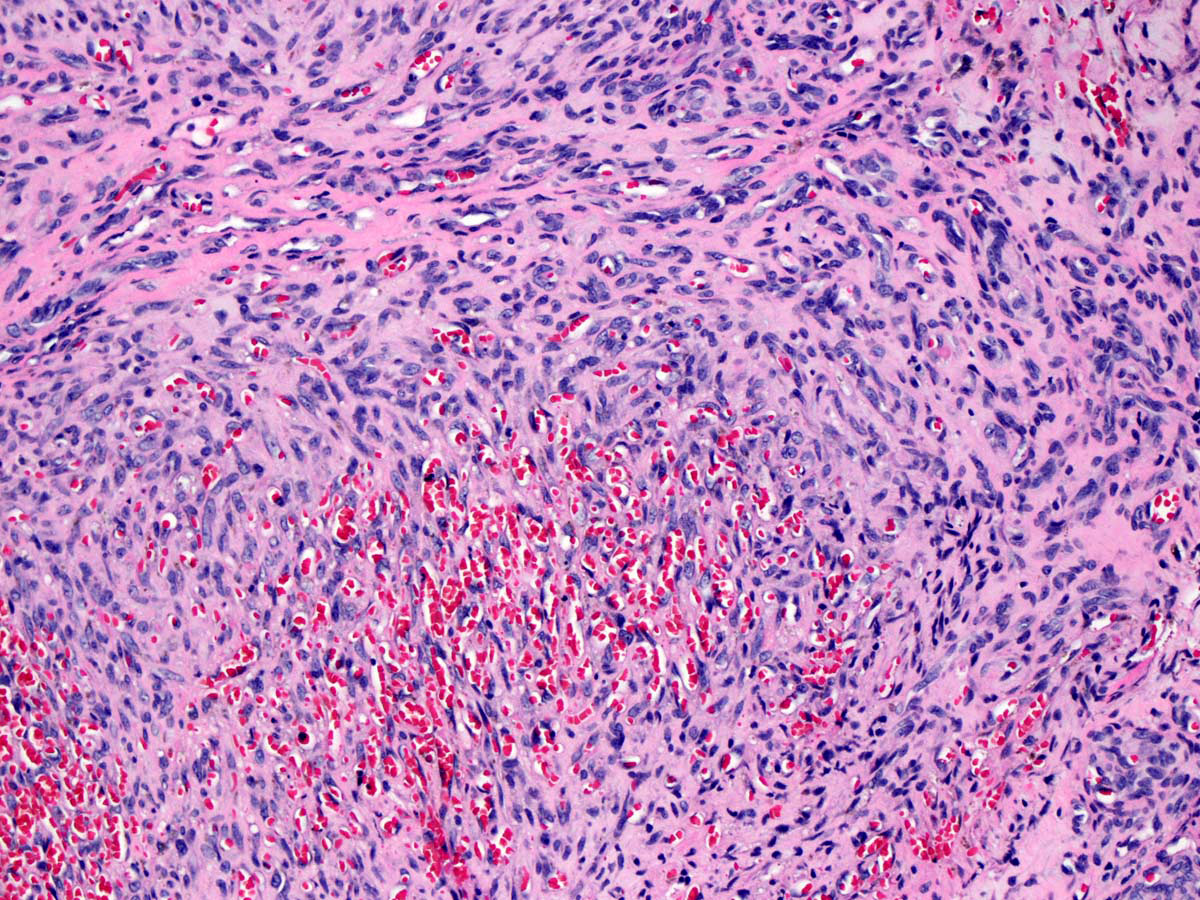
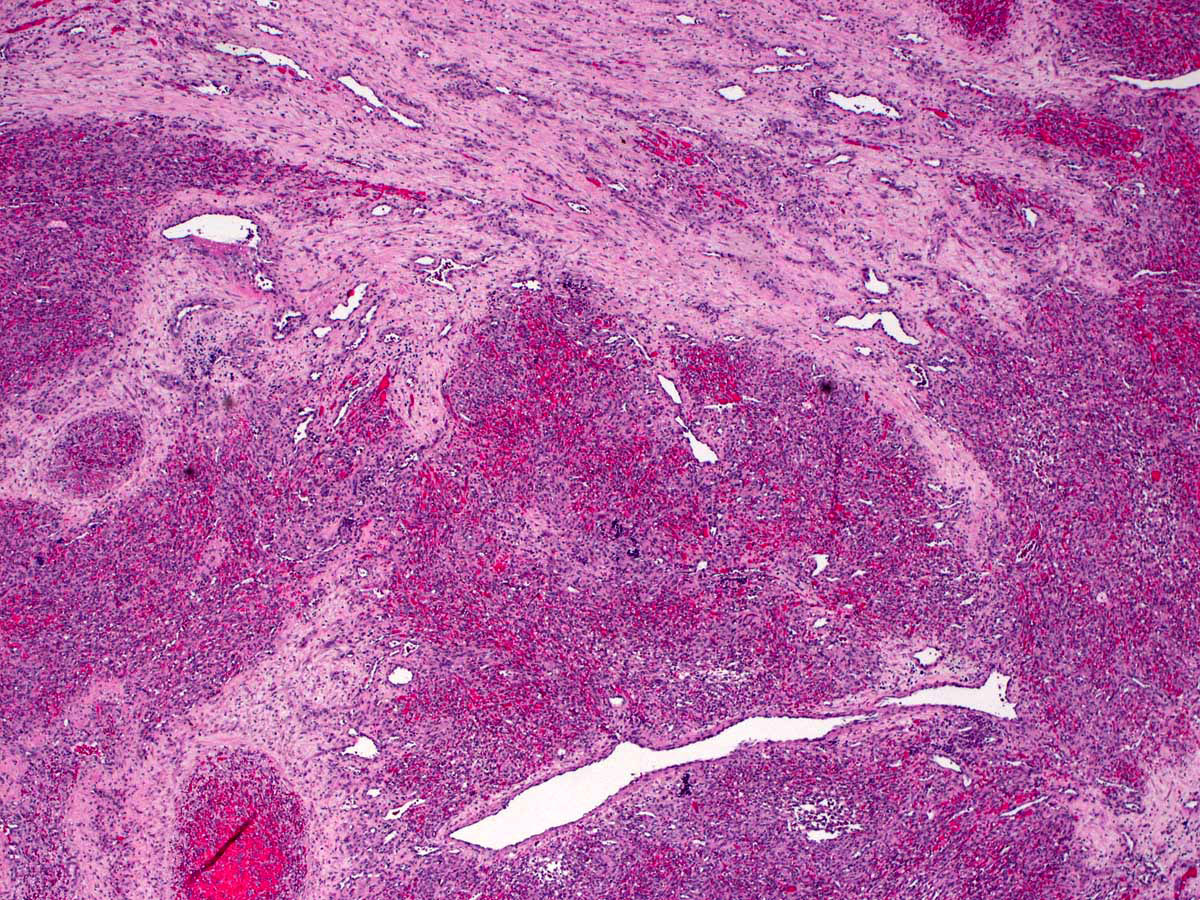
- Glomeruloid structures are a characteristic feature of the tumor
- Infiltrating sheets or nodules of spindled tumor cells arranged in short fascicles with slit-like vascular lumina
- Swirling growth pattern of spindled cells gives a glomeruloid appearance
- Glomeruloid structures contain red cell fragments, intracellular and extracellular hyaline granules, hemosiderin and microthrombi as evidence of red cells and platelets sequestration and destruction
- Lymphangioma-like areas with thin walled ectatic vessels at the periphery of nodules of spindled cells; in some extremes, it can present as a discrete lymphangioma
- Well formed vessels with pericyte component are present
- Mitoses are present but tumor cells show minimal cytologic atypia
- Tufted angioma usually involves the dermis but may extend to the fascia and muscle
- Multiple lobules of tightly packed spindle endothelial cells with slit-like lumina throughout the dermis, creating a cannonball appearance, intermingled with scattered tufts of capillaries
- Lymphangioma-like areas, composed of lymphatic vessels at the periphery of nodules of spindle endothelial cells
- References: Am J Surg Pathol 1993;17:321, Am J Surg Pathol 2004;28:559, An Pediatr (Barc) 2015;83:201, Pediatr Dev Pathol 2000;3:556
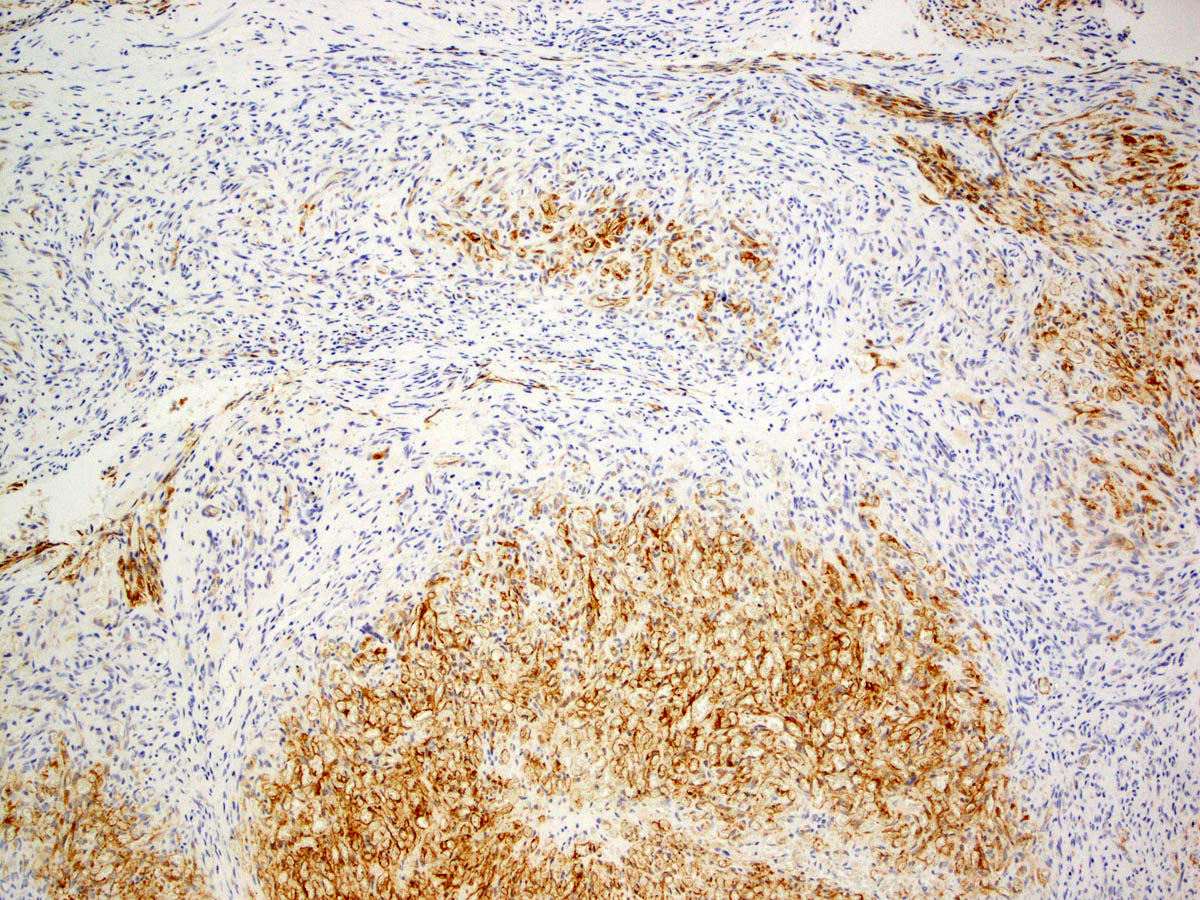
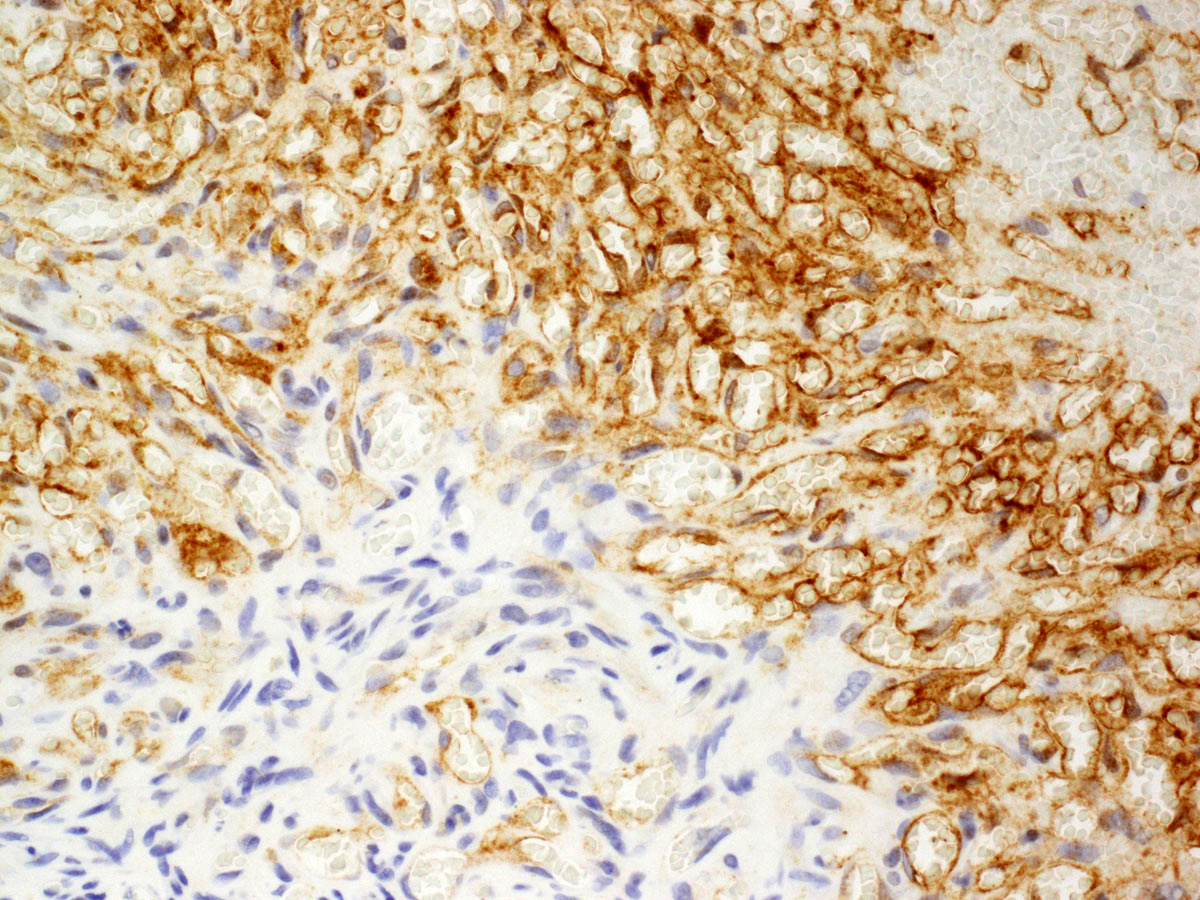
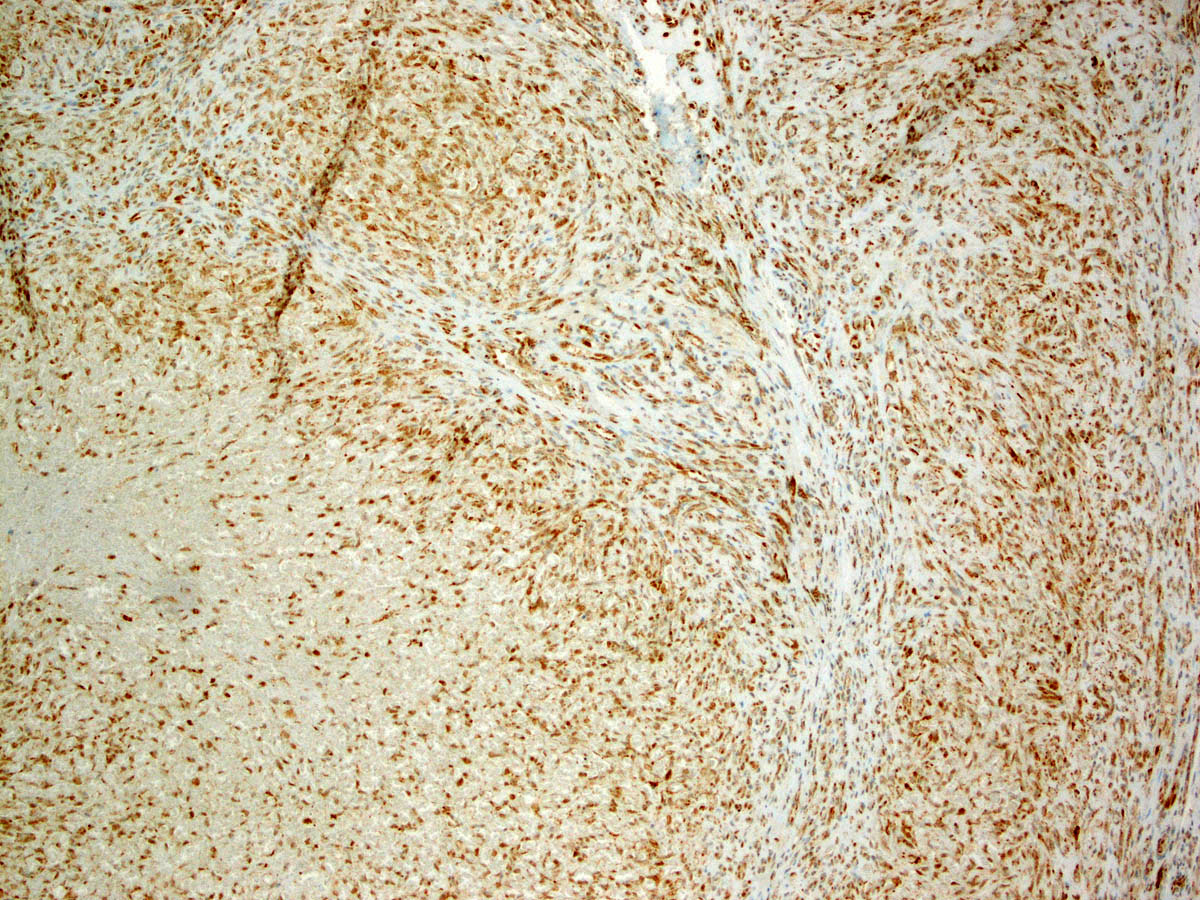
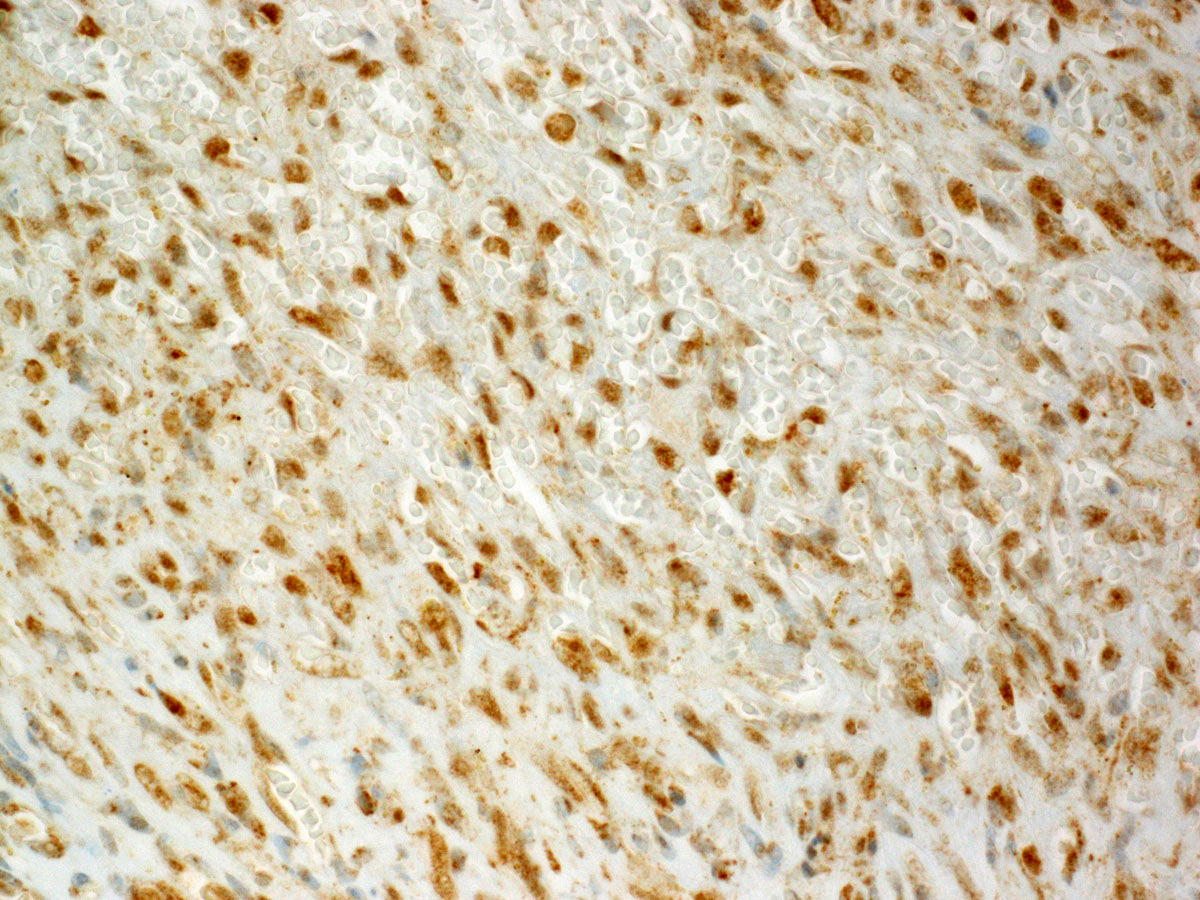
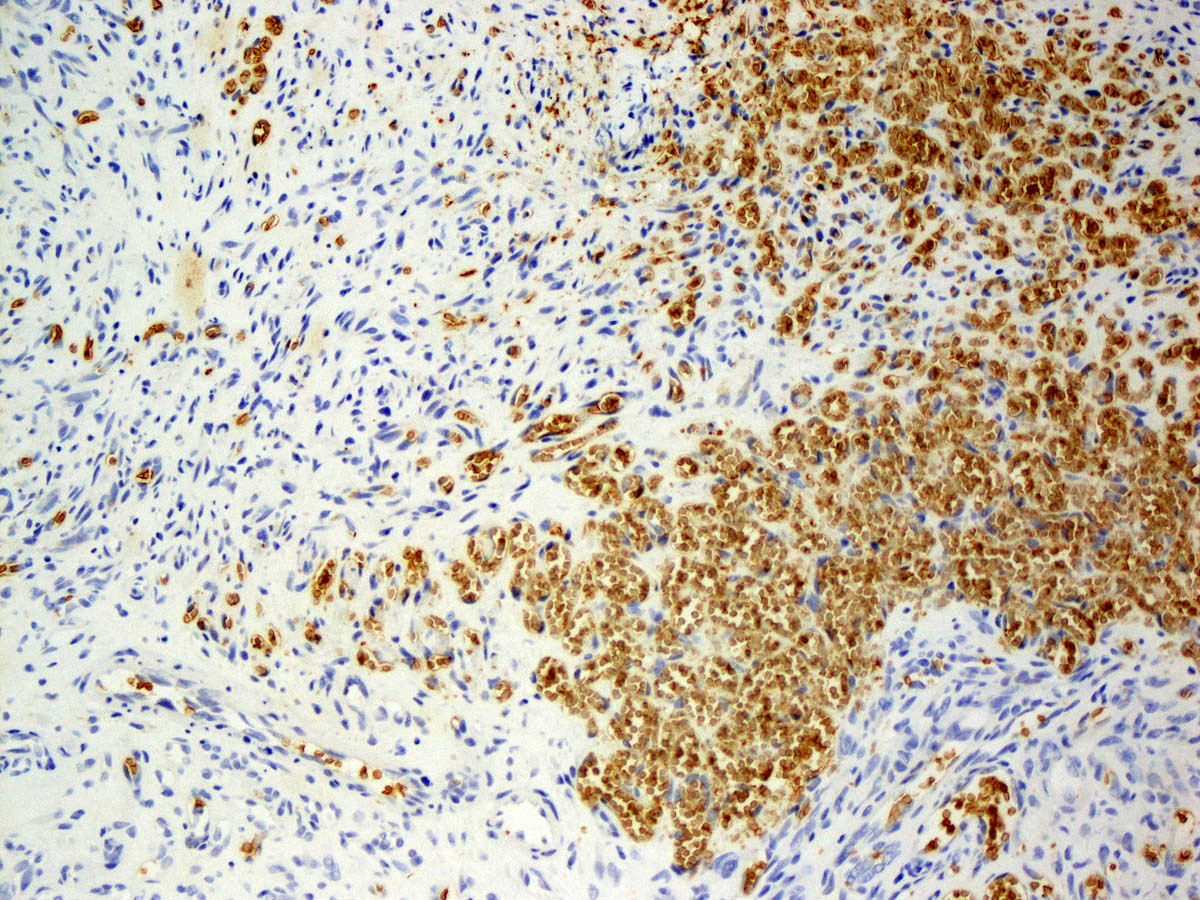
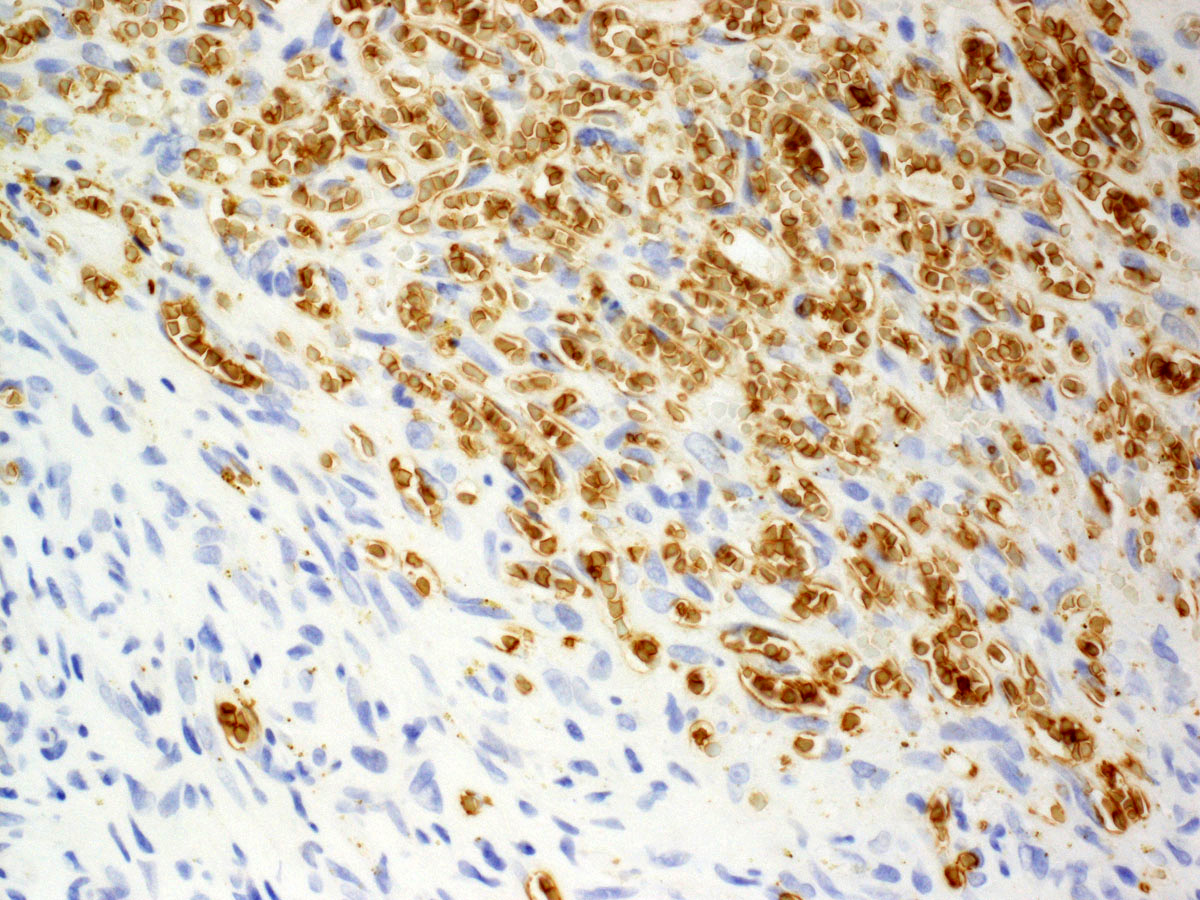
Microscopic (histologic) images
Contributed by Thuy L. Phung, M.D., Ph.D.
Positive stains
- Expresses endothelial cell markers, including CD31, CD34, ERG and FLI1
- Lymphatic markers (PROX1 and podoplanin) are expressed in peripheral lymphatic component (Kaposi-like areas), useful in differentiating it from other vascular lesions of infancy; glomeruloid structures lack these antigens (Am J Surg Pathol 2004;28:559)
Negative stains
- Tumor is negative for GLUT1 (which is positive in infantile hemangioma) and HHV8 (positive in Kaposi sarcoma) (Am J Surg Pathol 2004;28:559)
Electron microscopy description
- Spindle endothelial cells lining the slit-like channels have plump nuclei outstretching into the lumen; the basement membrane of these channels is thin and contains pericytes
- Within the slit-like channels are platelets, lymphocytes and macrophages
- Neoplastic cells contain cytoplasmic phagocytic vesicles (Ultrastruct Pathol 2013;37:452)
Molecular / cytogenetics description
- GNA14 mutations have been reported in KHE, as well as tufted angioma and pyogenic granuloma (Semin Pediatr Surg 2020;29:150975)
Sample pathology report
- Soft tissue, left face, biopsy:
- Consistent with kaposiform hemangioendothelioma
- Clinical history: facial mass; differential diagnosis: kaposiform hemangioendothelioma
- Gross description: The specimen is received in a single container labeled with the patient's name and left facial mass. It consists of an aggregate of irregularly shaped, red-tan, hemorrhagic soft tissue measuring 1.5 x 0.7 x 0.2 cm. Portions of tissues are submitted for cytogenetic studies and electron microscopy and are snap frozen for possible future studies. The remaining tissue is wrapped in filter paper and submitted in cassettes 1 and 2 for microscopic examination.
- Microscopic examination: 4 H&E slides. Immunohistochemical stains: CD31, CD34, GLUT1, D2-40 and FLI1. All controls are appropriate.
- Sections of the left facial mass biopsy show interconnecting sheets and nodules of plump, spindled endothelial cells lining a network of proliferative capillaries and smaller rounded vessels with occasional slit-like appearance that contain erythrocytes. In some areas, the capillary network is markedly congested, getting a more cavernous appearance. Occasionally, a vague glomeruloid pattern is seen. Few of these smaller rounded vessels contain intravascular fibrin thrombi. In some areas, the interstitium shows hyalinizing changes. Extravasated red blood cells are seen, as well as hemosiderin laden macrophages. Mitotic activity is low. No significant cytologic atypia is seen. The spindle cells are positive for the vascular markers CD31, CD34, D2-40 and FLI1 and are negative for GLUT1.
Differential diagnosis
- Kaposi sarcoma:
- Older or immunocompromised patients
- Very rare in children, except in Africa
- Nodular stage presents predominantly as a solid eosinophilic spindle cell area that often lacks endothelial lining and associated with red blood cell extravasation
- Lacking of hemangioma-like areas
- Positive for HHV8
- Infantile hemangioma:
- Distinct lobules of capillary vessels
- Lacks spindle cells and glomeruloid areas
- Positive for GLUT1 and Lewis Y antigen
- Regresses spontaneously
- Not associated with Kasabach-Merritt phenomenon
- Spindle cell hemangioma:
- Occurs in distal extremities of adults
- Biphasic tumor
- Admixture of thin walled, congested cavernous vascular spaces and solid areas of spindled to epithelioid endothelial cells
- Vacuolated (blister) endothelial cells
- Large, calcified thrombi and thrombosis may be present
- IDH1 mutations
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true about kaposiform hemangioendothelioma?
- A small proportion of tumors occur in infant and young children
- May be associated with fatal consumptive coagulopathy
- Tumor is indistinguishable from Kaposi sarcoma and is positive for HHV8
- Tumor may regress completely without treatment
- Tumor does not metastasize
Board review style answer #2
B. May be associated with fatal consumptive coagulopathy
Comment Here
Reference: Kaposiform hemangioendothelioma
Comment Here
Reference: Kaposiform hemangioendothelioma