Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Hamilton C, Ray J, Asadbeigi SN. Squamous cell carcinoma in situ / Bowen disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticcisgeneral.html. Accessed March 30th, 2025.
Definition / general
- Characterized by full thickness involvement of the epidermis by dysplastic squamous cells
- Bowen disease and squamous cell carcinoma in situ (SCCIS) are used interchangeably to describe epidermal SCCIS of both sun damaged and sun protected skin (J Cutan Aesthet Surg 2021;14:449)
Essential features
- Squamous cell carcinoma in situ is squamous cell carcinoma (SCC) confined to the epidermis and superficial adnexal epithelium
- Full thickness epidermal squamous cell dysplasia
- Disordered maturation with atypical keratinocytes (Front Med (Lausanne) 2023;10:1281540)
- No invasion of the underlying dermis (Indian Dermatol Online J 2022;13:177)
Terminology
- Bowen disease
- Intraepidermal carcinoma
- Erythroplasia (of Queyrat)
- If at glans penis (Ann Dermatol 2009;21:419)
ICD coding
Epidemiology
- More frequent in
- White, fair skinned people
- M = F (World J Clin Cases 2019;7:2910)
- > 60 years of age
- Risk factors
- High sun / ultraviolet (UV) exposure
- Immunosuppression
- Arsenic
- Human papillomavirus (HPV) infections (Breast J 2020;26:1234)
Sites
- Can occur anywhere
- More common in sun exposed skin but also occurs in non-sun exposed areas
- Commonly involved areas: head and neck, lower limbs, upper limbs (J Am Acad Dermatol 1992;27:406)
- Less commonly involved areas: subungual, periungual, genital and perianal sites
Pathophysiology
- Poorly characterized
- May often relate to TP53 mutations, which are present in 7 - 45% of SCCIS cases (Biomedicines 2021;9:171)
Etiology
- Multifactorial
- Ultraviolet radiation damages the skin cell nucleic acids, leading to the mutation and cloning of the p53 gene (StatPearls: Intraepidermal Carcinoma [Accessed 9 October 2024])
- Diseases or drugs capable of suppressing immune responses to skin damage also can trigger the mutation of squamous cells
- Arsenic exposure causes oxidative stress, antioxidant depletion, immune dysfunction, genotoxicity, impaired DNA repair and disrupted signal transduction (Toxicol Appl Pharmacol 2023;479:116730)
- HPV in predominantly genital and periungual lesions but it is also reported in extragenital cases
- HPV16 as the most prevalent subtype (Int J Cancer 1983;32:563)
Clinical features
- Usual presentation is a solitary, slow growing, scaly, erythematous patch or plaque
- Variable in size (millimeters to centimeters)
- Can remain unchanged for many years
- Can have a crusting, pigmented or verrucous appearance and can resemble psoriasis
- Dermoscopic features can include scale, glomerular vessels, yellow crust, hemorrhage, hypopigmentation and linear irregular vessels (World J Clin Cases 2019;7:2910)
- Pigmented variants exist and may clinically resemble melanoma (Int J Dermatol 2020;59:e316)
Diagnosis
- Characteristic clinical features
- Definitive diagnosis is made by shave, punch or excisional biopsies (Indian Dermatol Online J 2022;13:177)
Prognostic factors
- ~3 - 5% of all SCCIS lesions progress to invasive SCC (Br J Hosp Med (Lond) 2022;83:1)
- Invasion risk is slightly higher in genital SCCIS (Br J Dermatol 2007;156:11)
- 8 proteins (TNC, FSCN1, SERPINB1, ACTN1, RAB31, COL3A1, COL1A1, CD36) are associated with invasion and metastasis in SCCIS (J Transl Med 2022;20:416)
Case reports
- 32 year old woman with scaly plaque on left hand (J Cutan Aesthet Surg 2021;14:449)
- 48 year old man with erythematous patch on left hand (World J Clin Cases 2019;7:2910)
- 57 year old woman with SCCIS of the left nipple (Breast J 2020;26:1234)
- 85 year old White woman with red scaly plaques (JAAD Case Rep 2022;26:57)
- 90 year old woman with progressively enlarging pink mass (JAAD Case Rep 2024;51:54)
Treatment
- Small, isolated lesions of SCCIS can be treated with surgical excision, curettage and electrodesiccation (C&E), cryosurgery, topical fluorouracil or imiquimod (Cochrane Database Syst Rev 2013;2013:CD007281)
- Large lesions (> 3 cm) may be treated with photodynamic therapy (if available) or topical fluorouracil (J Am Acad Dermatol 2024;90:58)
Clinical images
Gross description
- Slightly raised, large, scaly, erythematous plaque with irregular border
- Usually single patch or verrucous growth (J Cutan Aesthet Surg 2021;14:449)
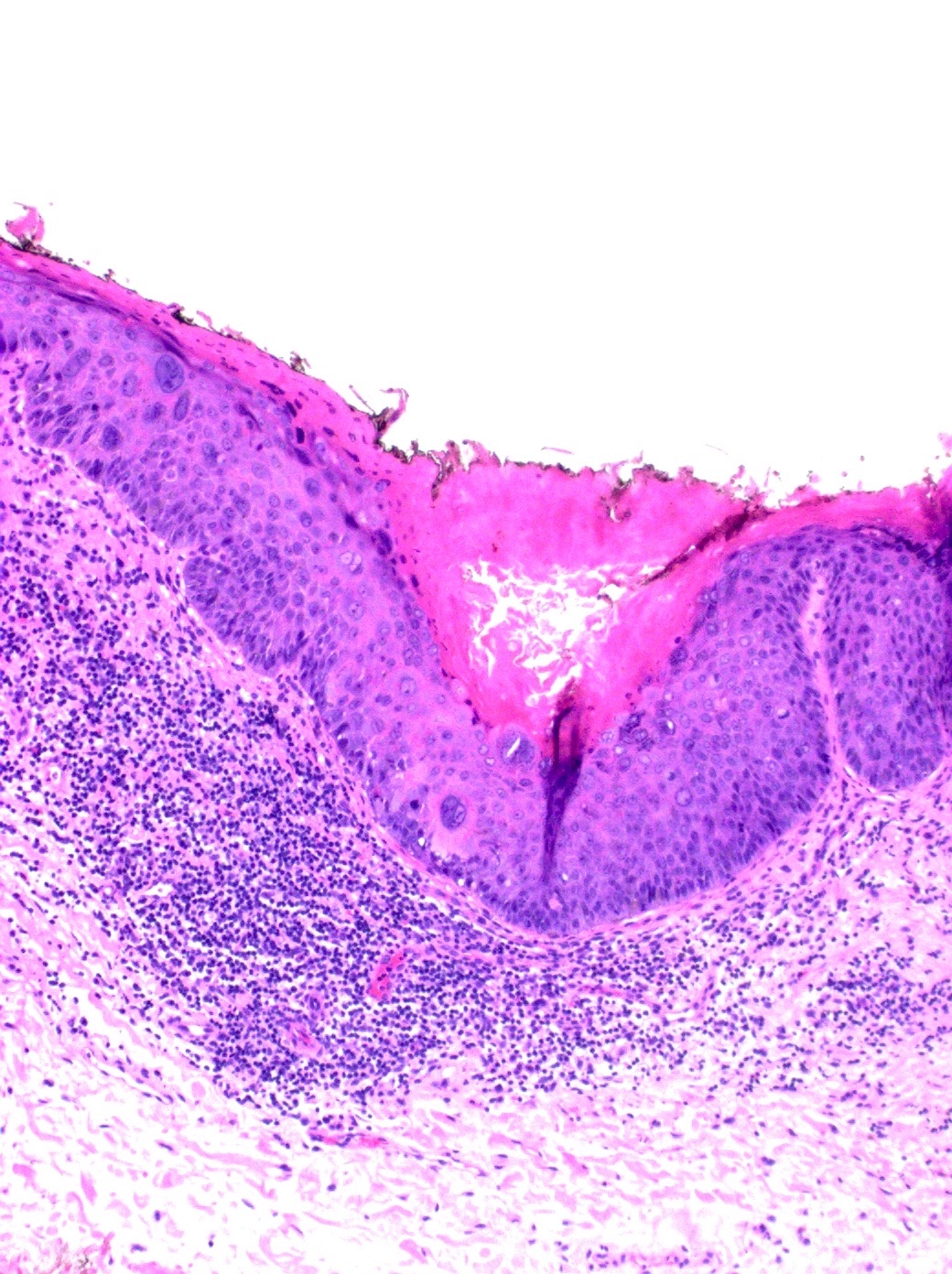
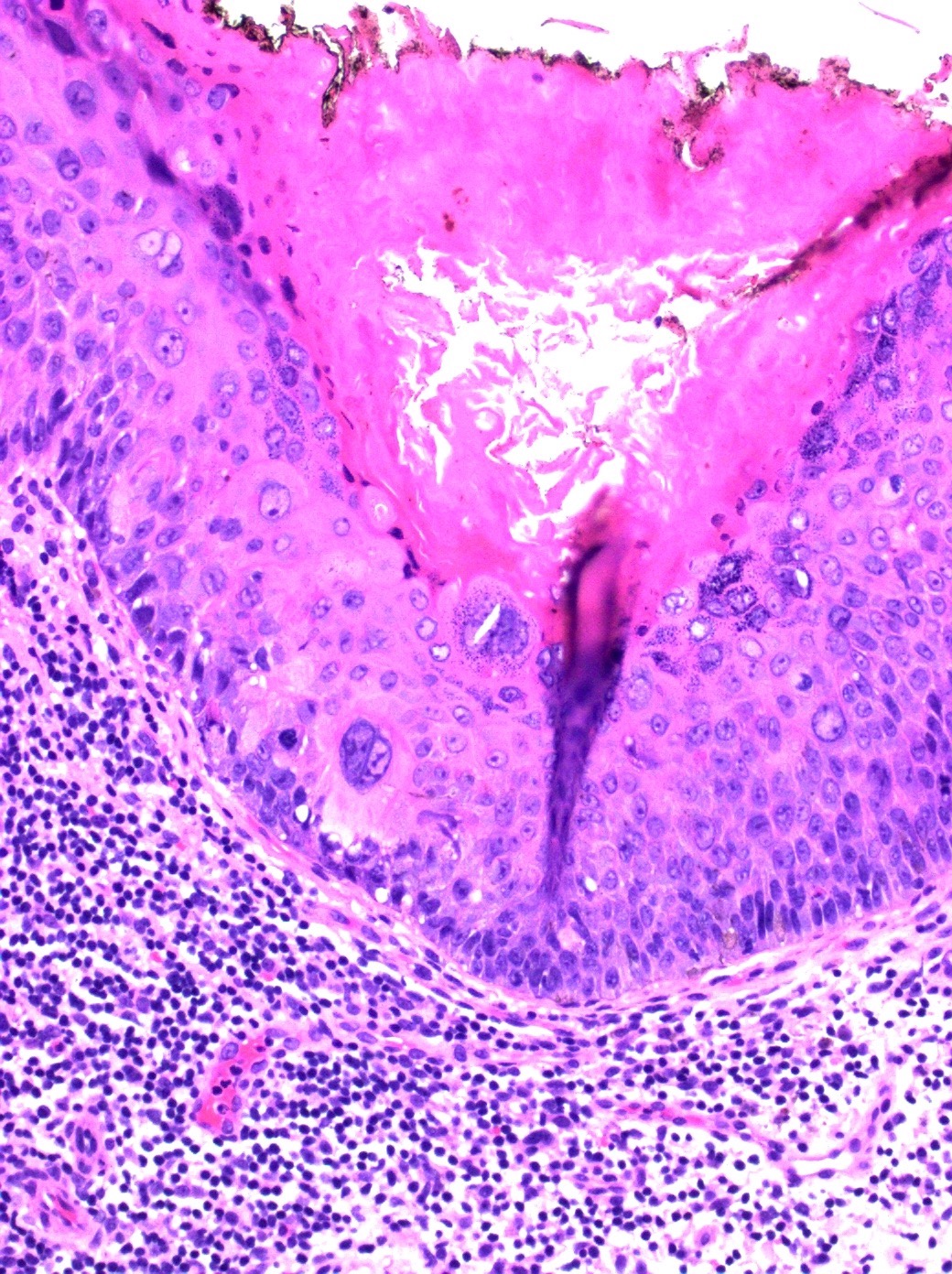
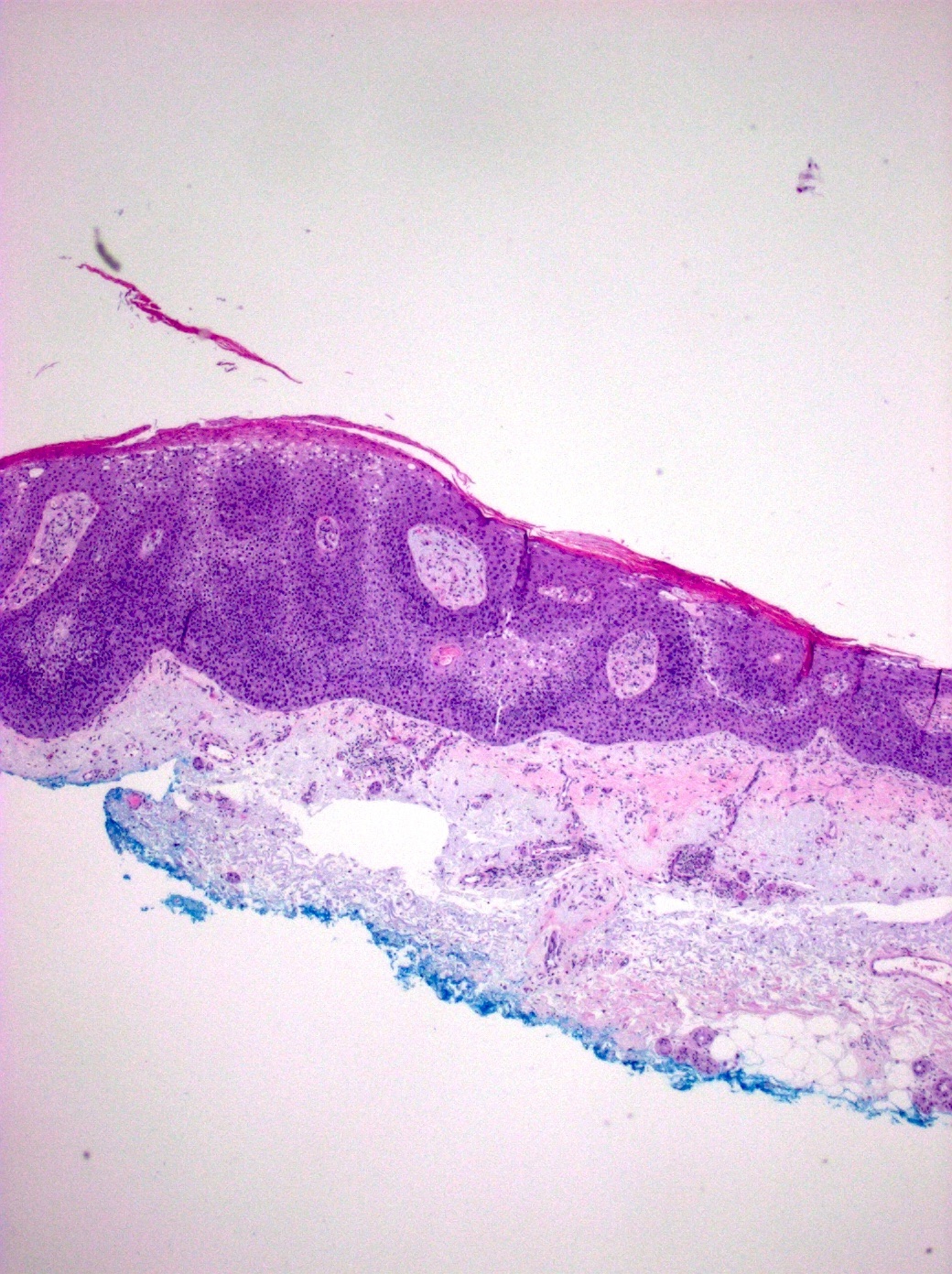
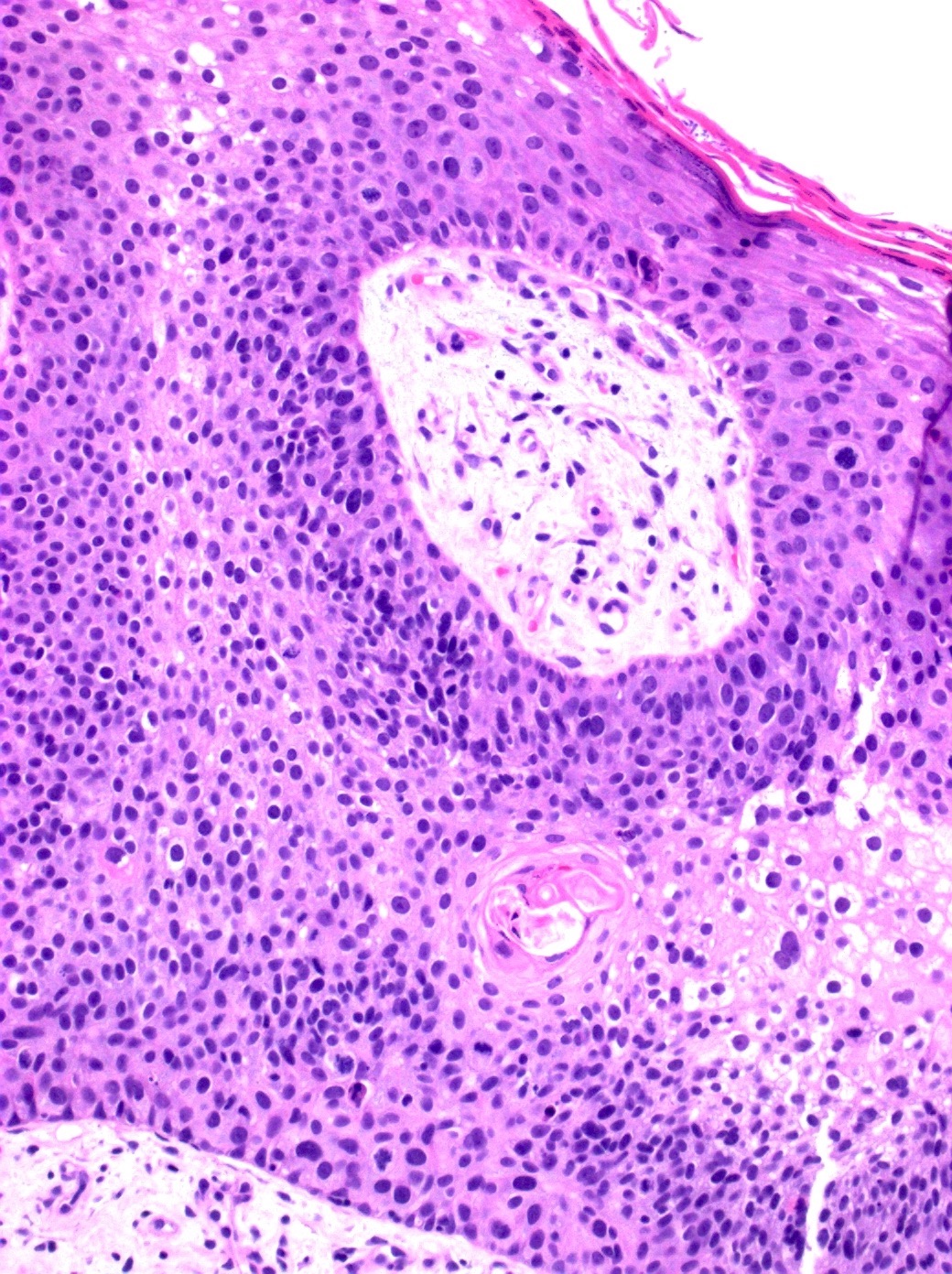
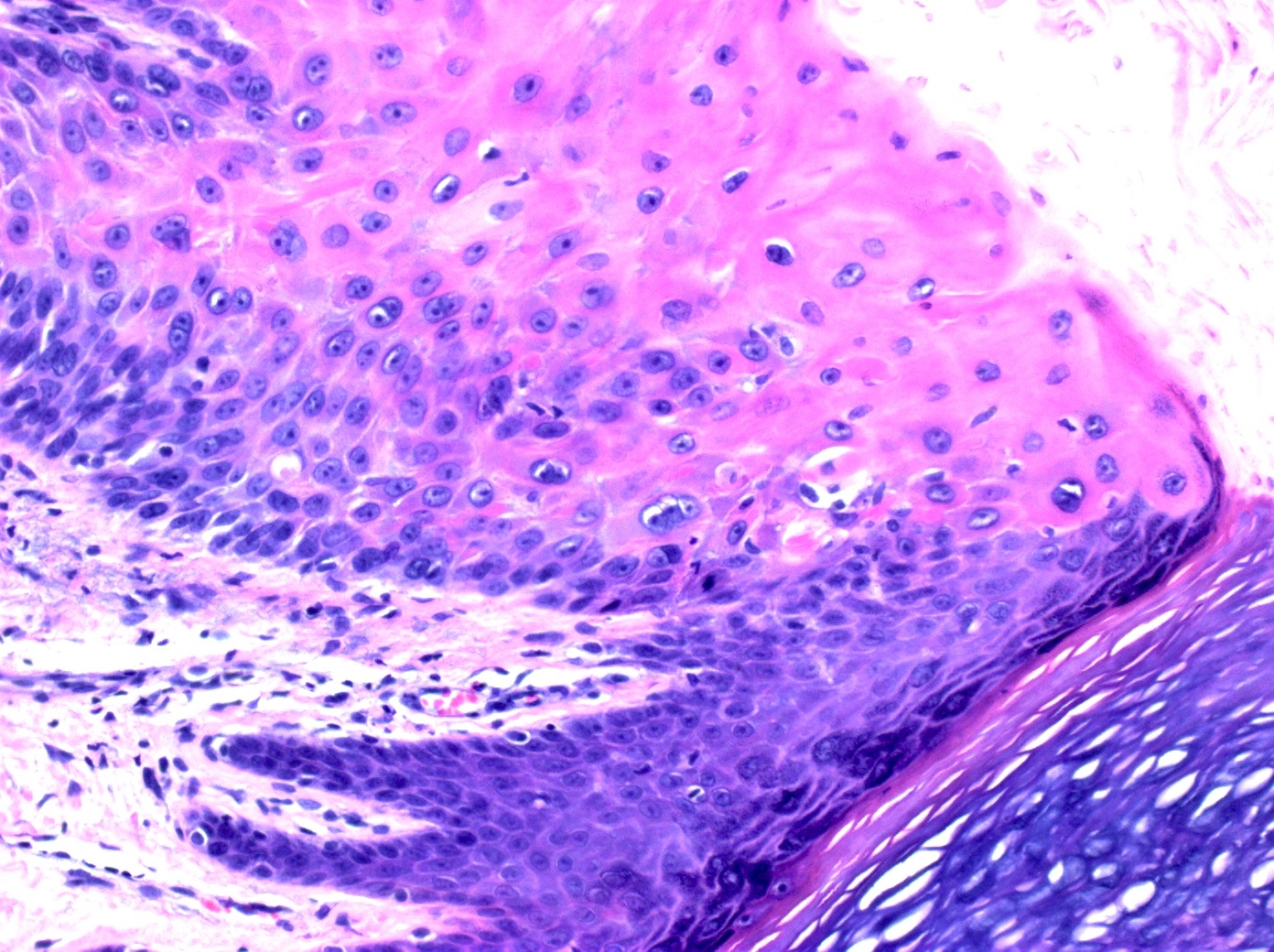
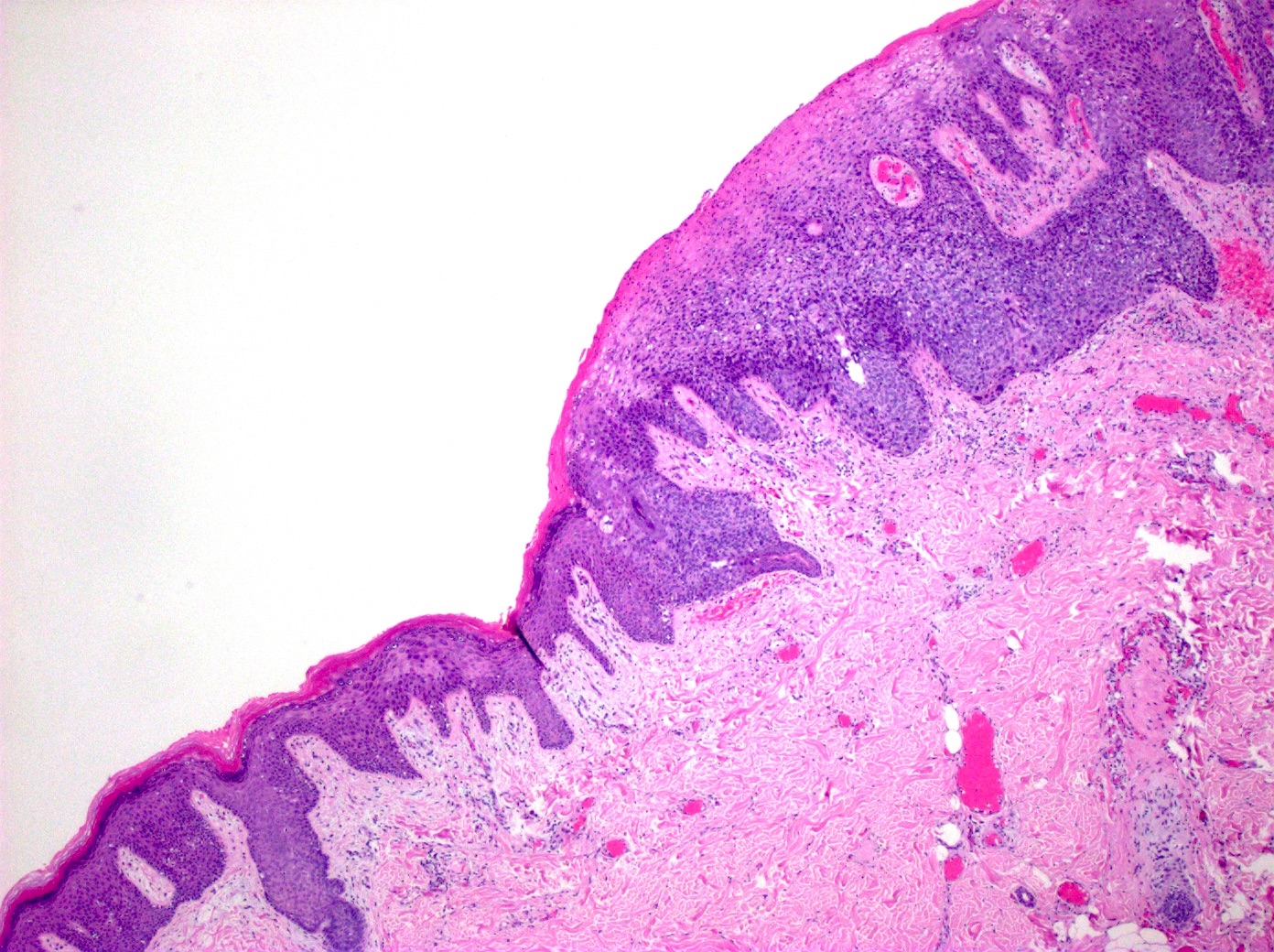
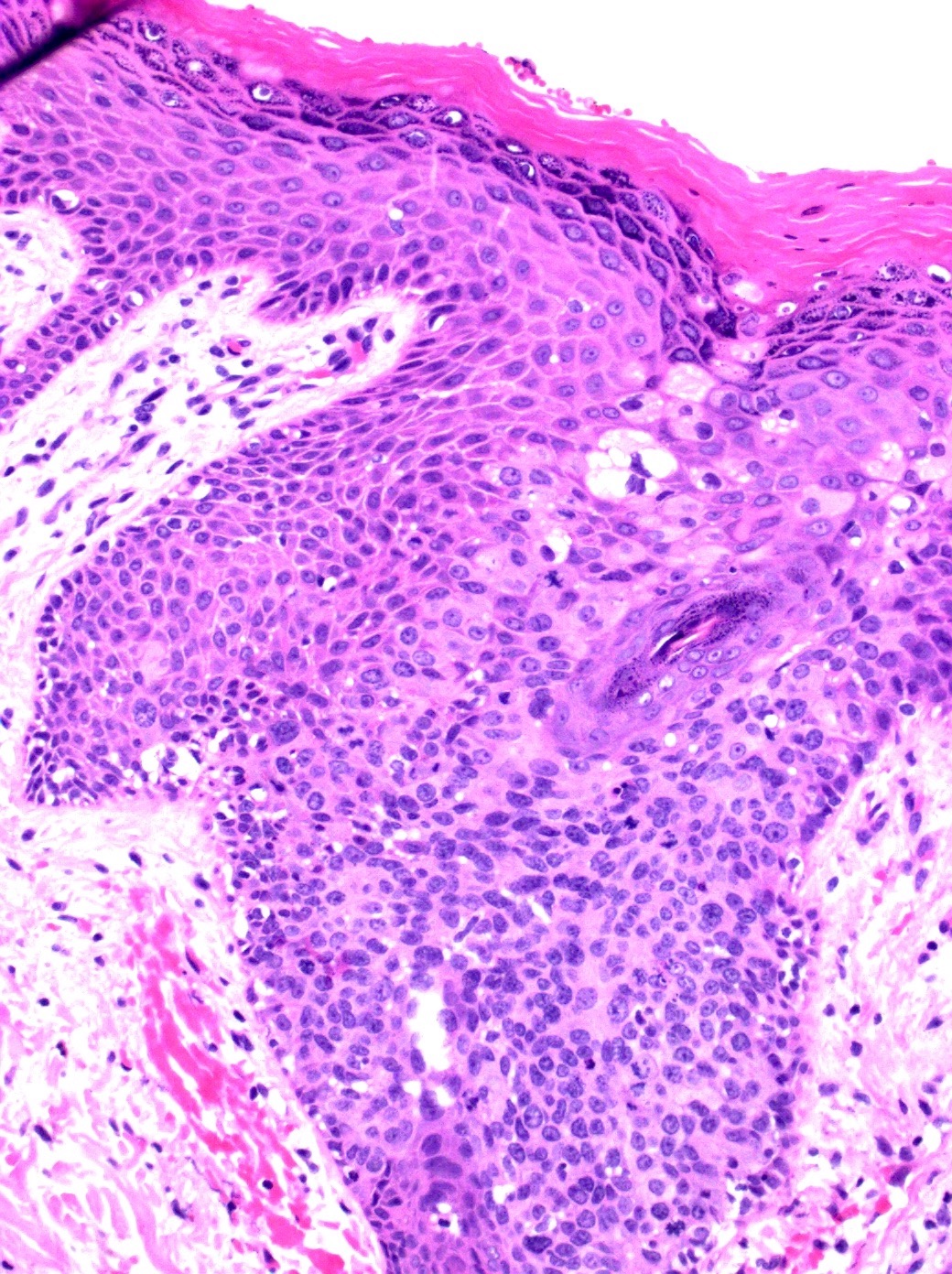
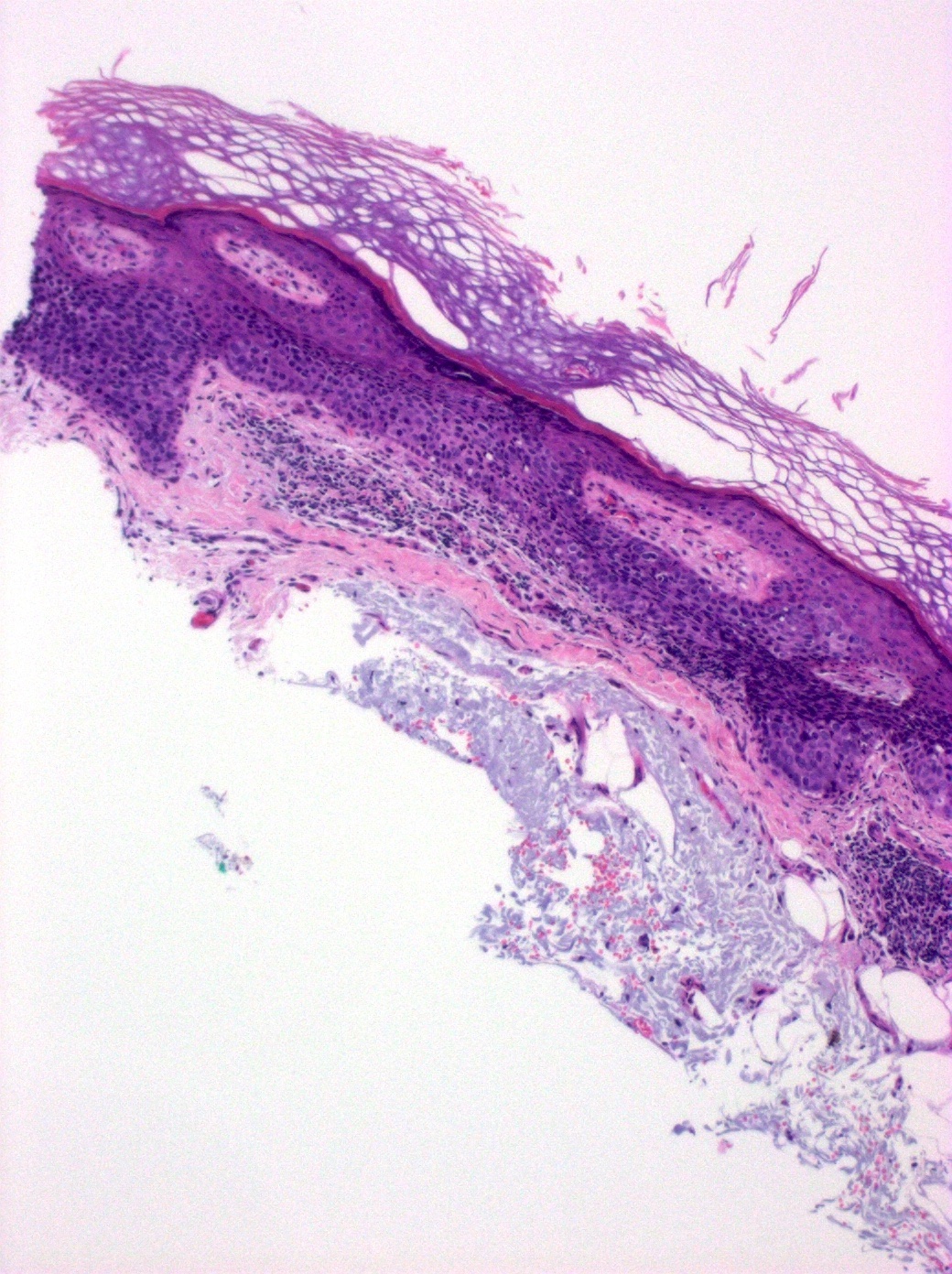
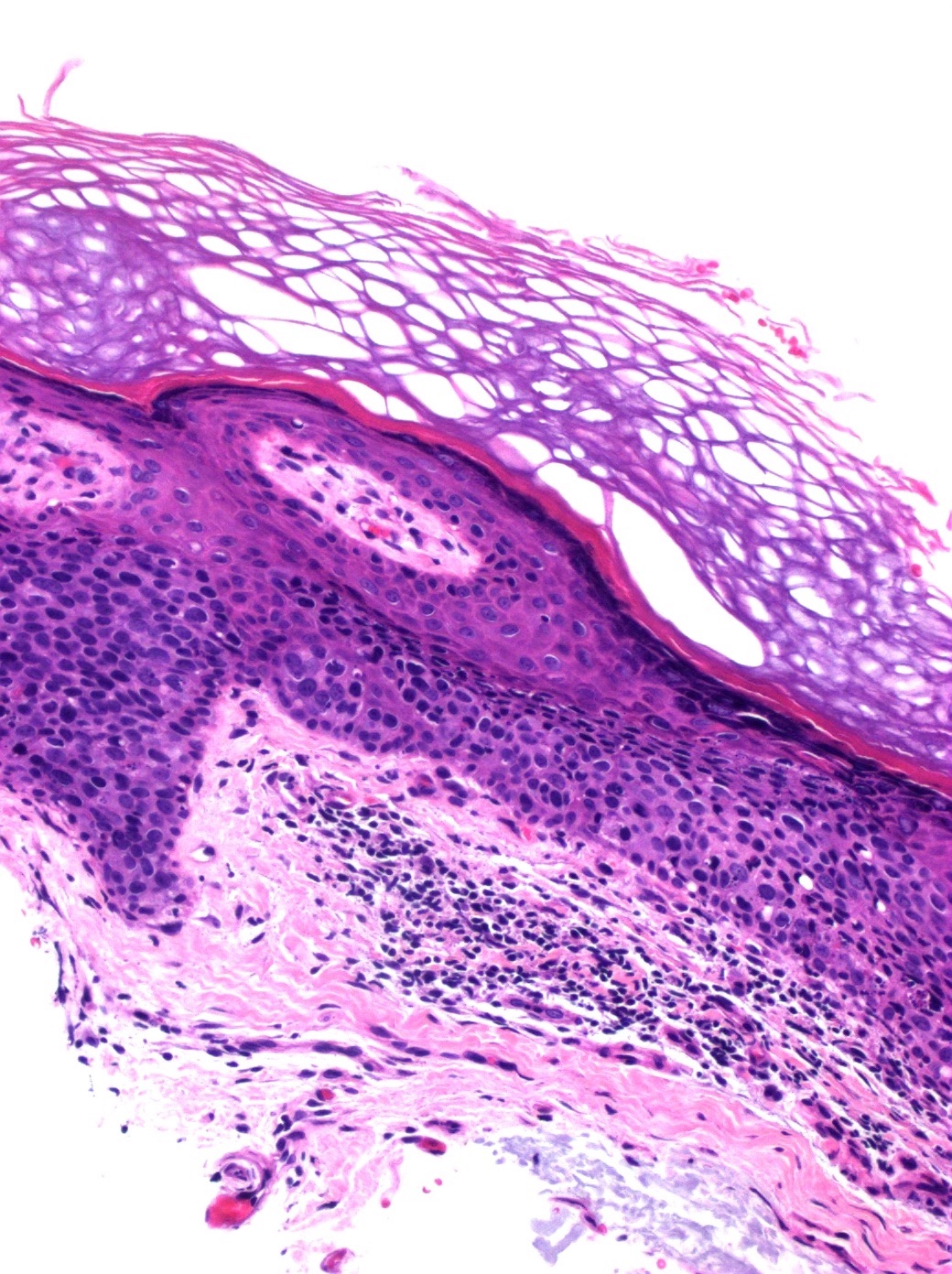
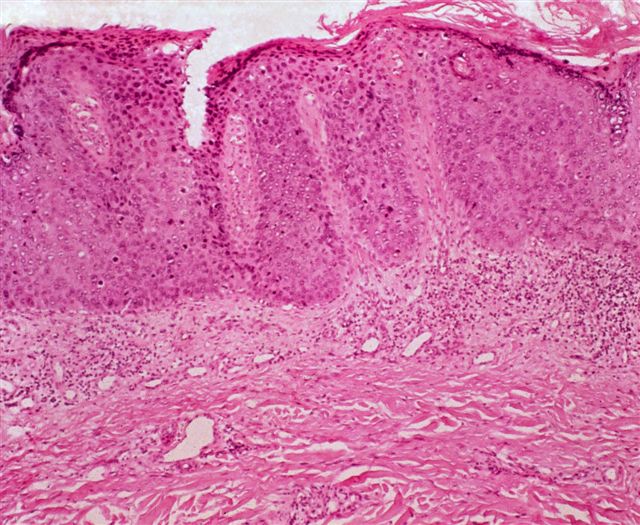
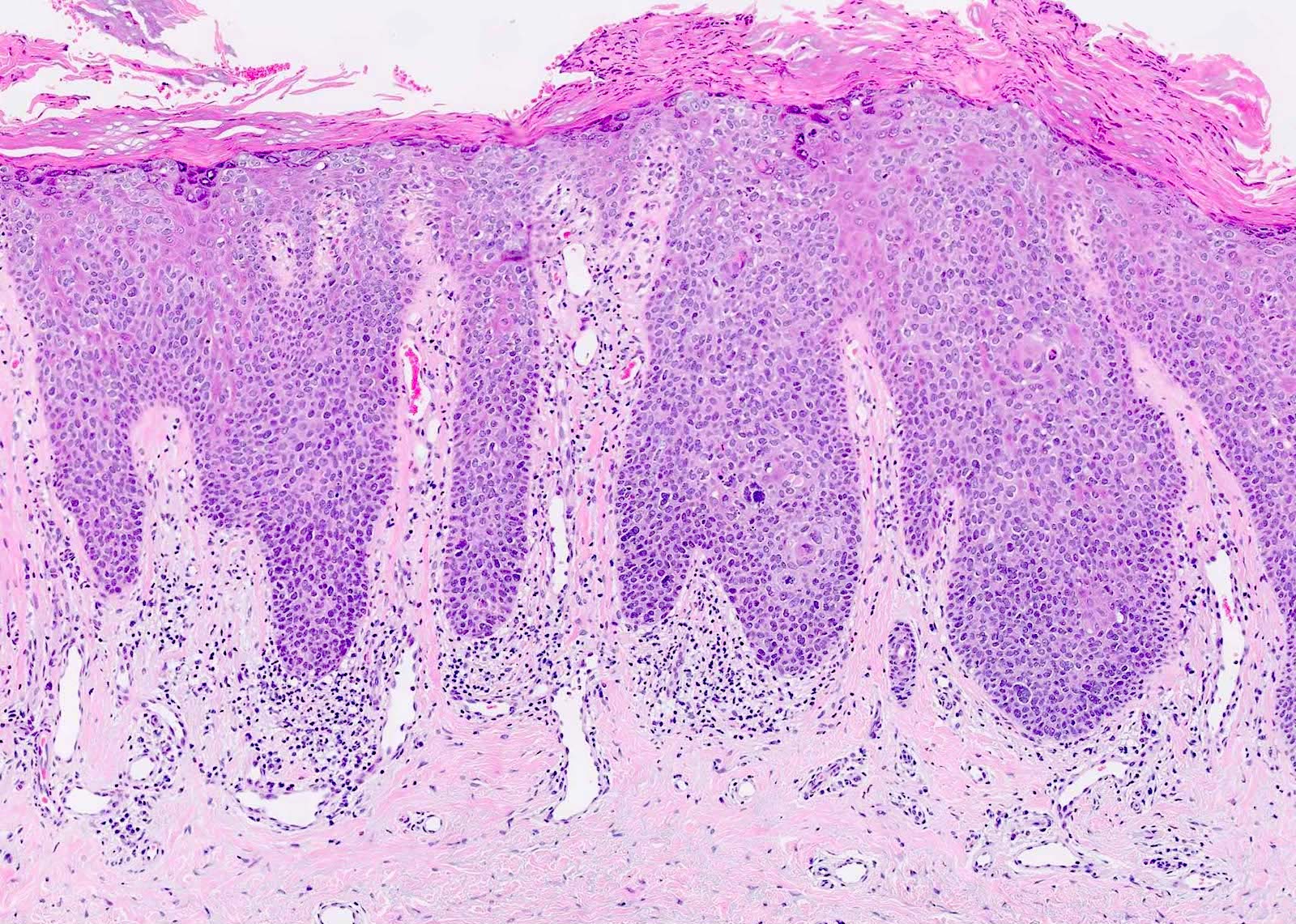
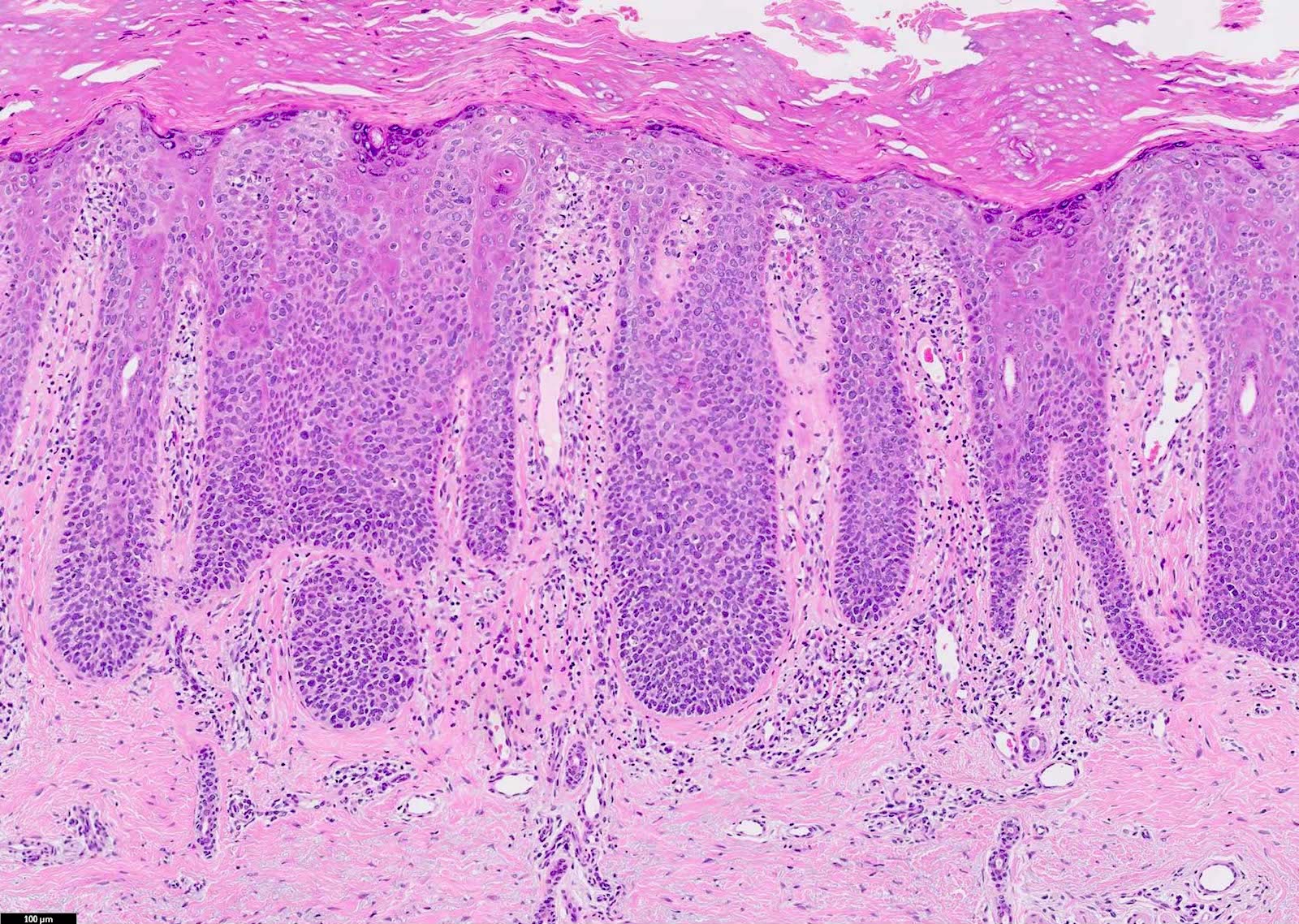
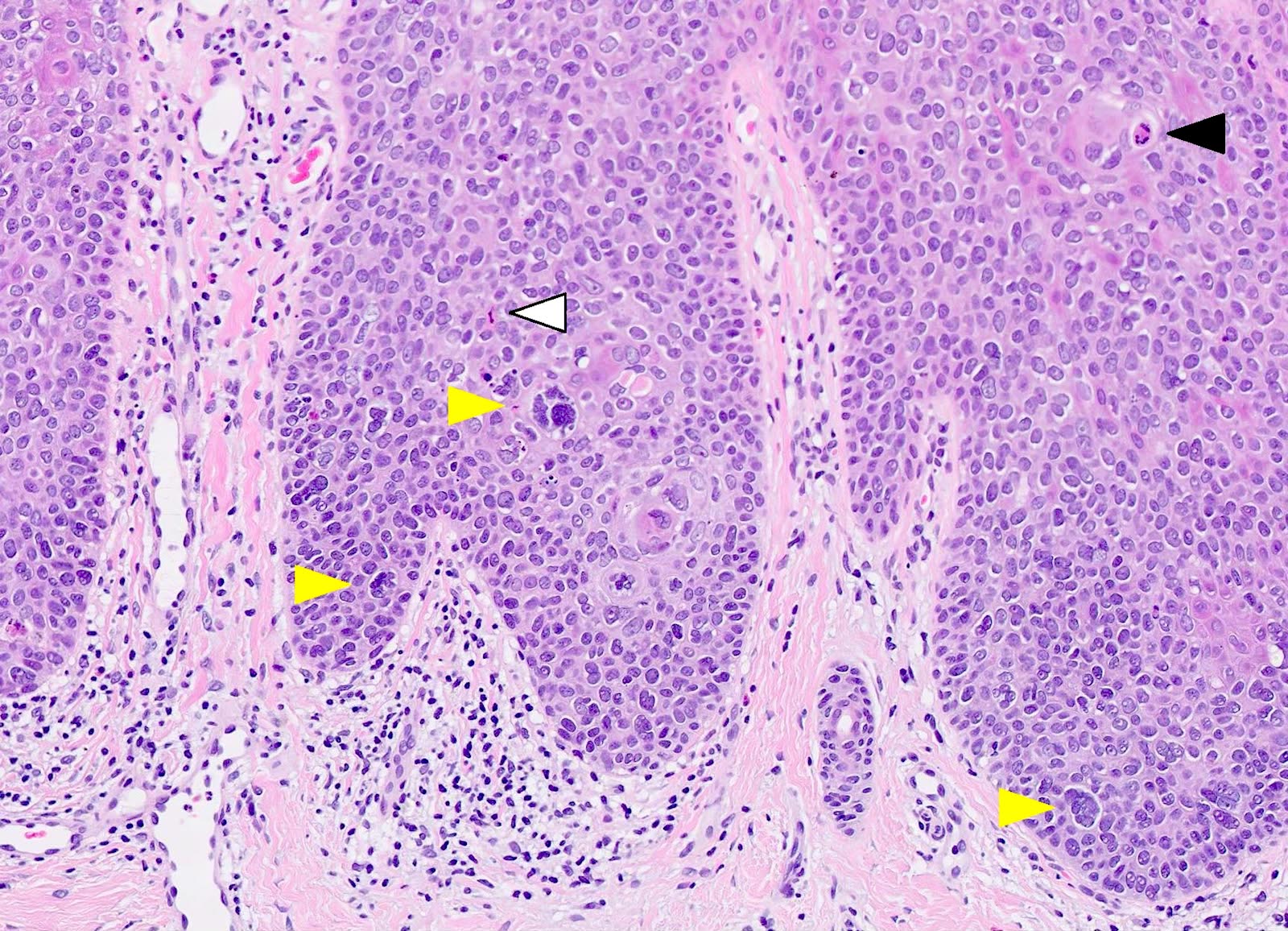
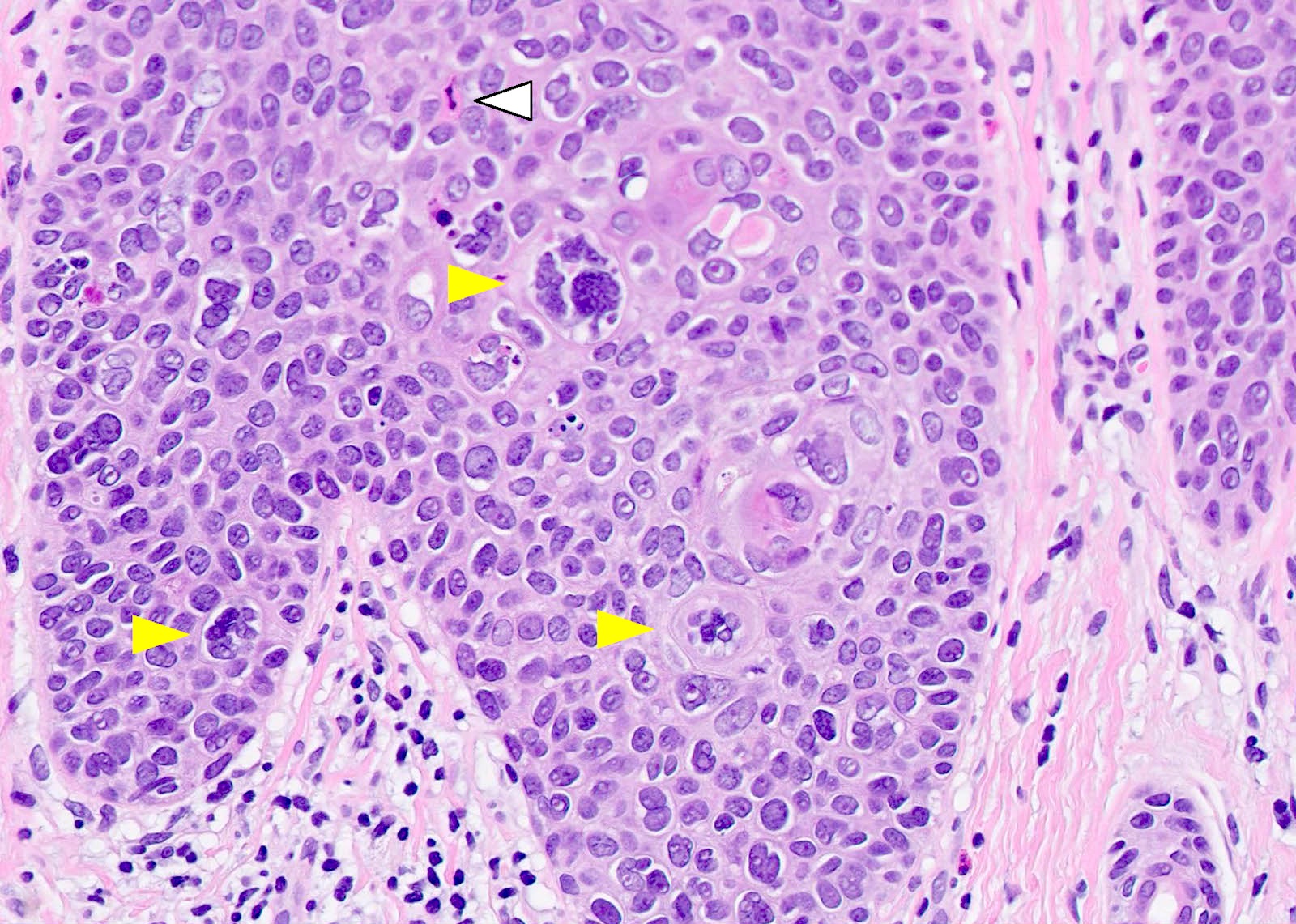
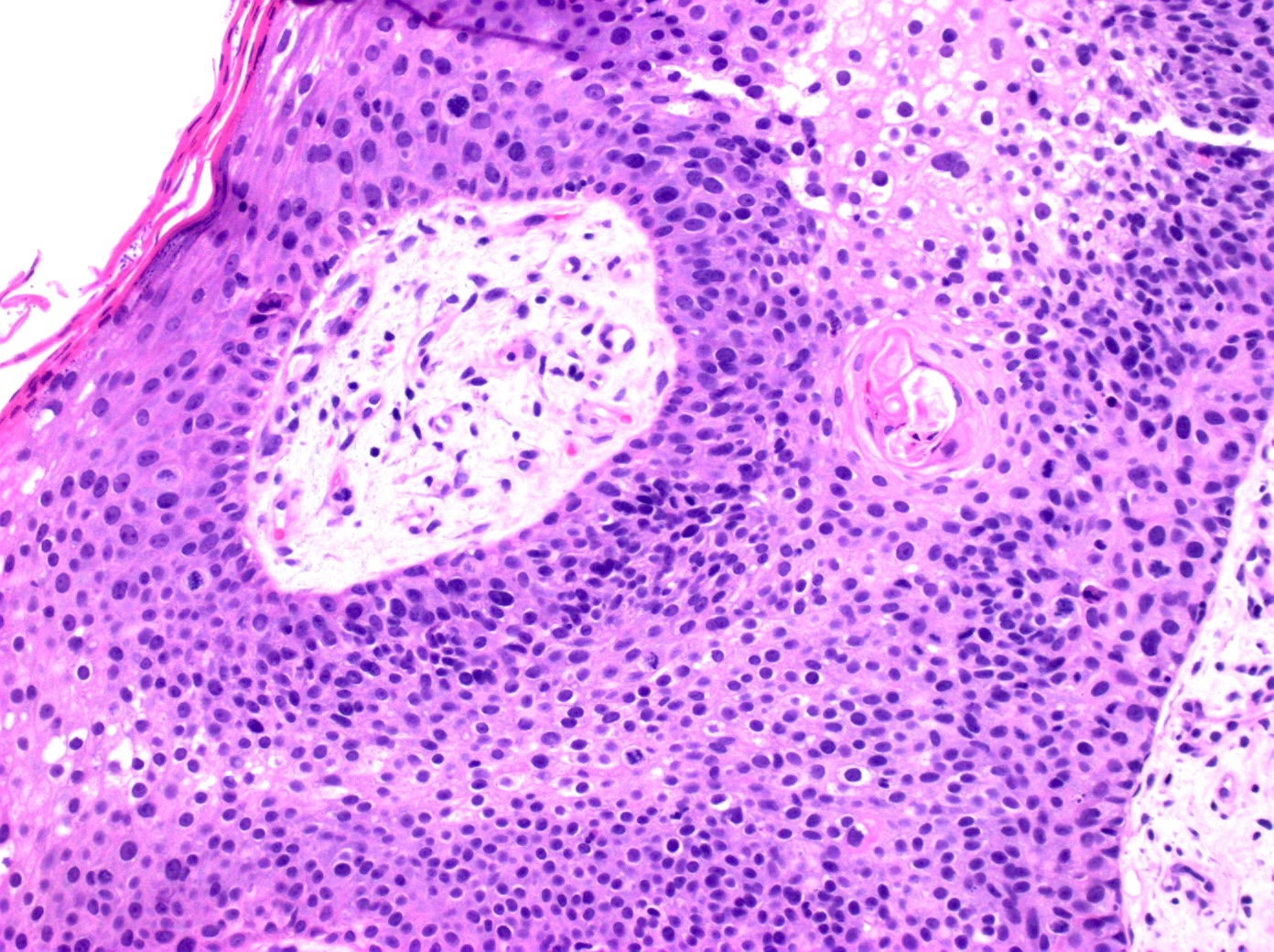
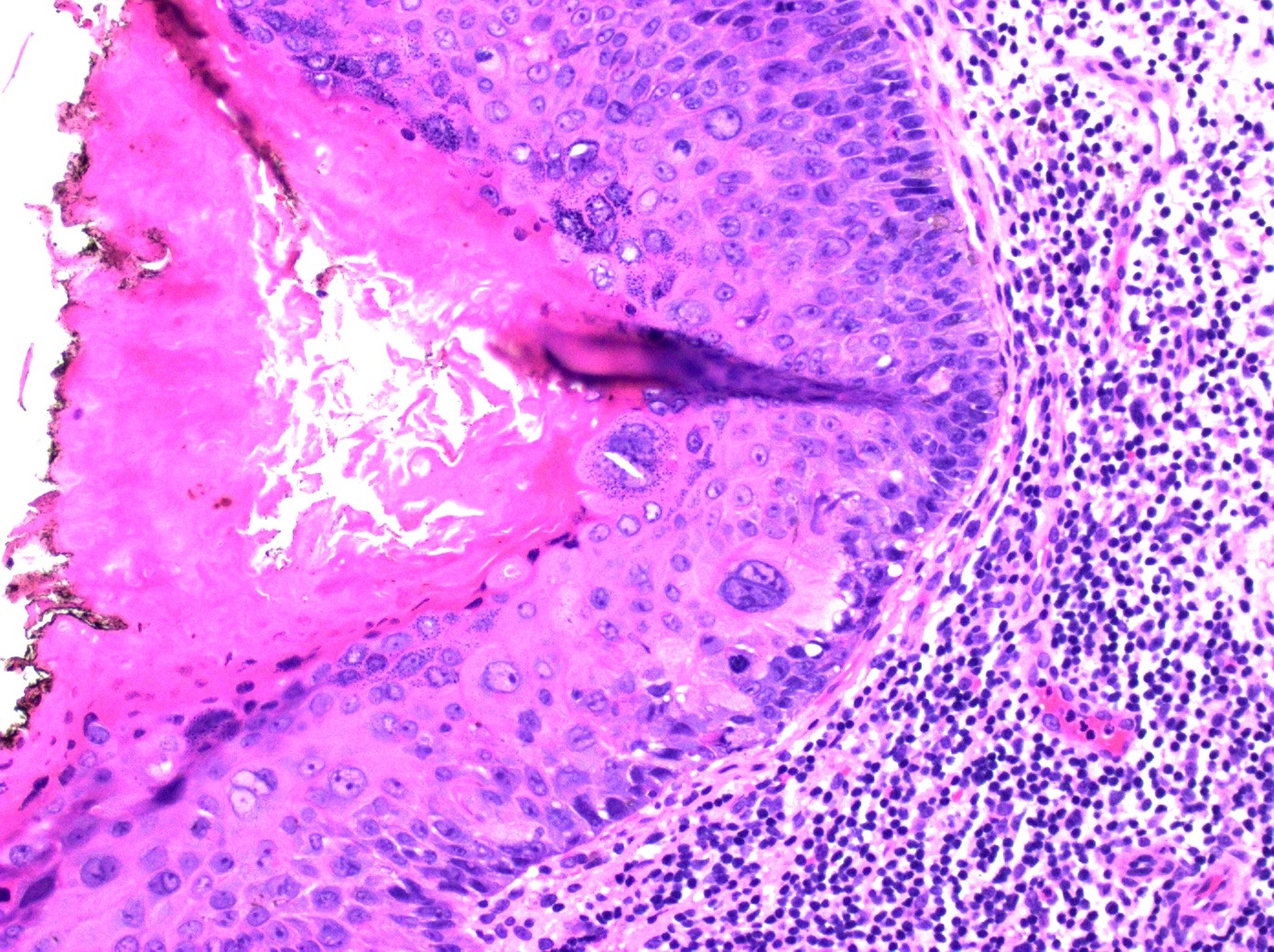
Microscopic (histologic) description
- General histologic features
- By definition, requires full thickness keratinocyte atypia, although may be surrounded by normal keratinocytes
- Also involves the intraepidermal portions of the skin adnexa
- Commonly has parakeratosis and could be associated with hyperkeratosis
- Architectural and cellular atypia, apoptotic cells, individual cell dyskeratosis
- Markedly altered maturation but usually still some surface keratinization and intercellular bridges present
- Marked nuclear atypia, including nuclear hyperchromasia and multinucleation (Breast J 2020;26:1234)
- Numerous mitotic figures, atypical mitotic figures
- May extend into eccrine sweat glands (not considered invasive disease)
- Variable melanin, variable lymphocytic infiltrate
- May have hemangiomatous vascular proliferation, amyloid globules, adnexal differentiation
- Genital lesions: koilocytosis can be present
- Histologic subtypes
- Clear cell variant: cytoplasmic vacuoles; can show pagetoid cells or ground glass cytoplasm (Biomedicines 2021;9:171)
- Pagetoid: single nests of melanocytes with large and clear cytoplasm
- Verrucous (S Afr Med J 1987;71:527)
- Pigmented: has an increase in melanin pigment deposition
- Helpful key phrases
- Eyeliner sign: a layer of cytologically bland keratinocytes with small ovoid nuclei is often present below the atypical keratinocytes, often focal (Am J Dermatopathol 2024;46:193)
- Windswept appearance: disordered cells with loss of polarity (Indian Dermatol Online J 2014;5:526)
Microscopic (histologic) images
Contributed by Jayden Ray, D.O., Chad Hamilton, D.O., Amy Lynn, M.D., Andrey Bychkov, M.D., Ph.D. and Jijgee Munkhdelger, M.D., Ph.D.
Positive stains
- Pancytokeratin
- p40
- p63
- CK5/6
- EMA: variable
- Increased Ki67 expression
- p16: in lesions associated with HPV
- PAS: positive in cases with vacuolated keratinocytes
- Reference: Am J Surg Pathol 2014;38:257
Negative stains
Videos
SCCIS by Dr. Jerad Gardner
Sample pathology report
- Skin, left forearm, shave biopsy:
- Squamous cell carcinoma in situ (Bowen disease)
- Margins are free of involvement
- Microscopic description: The epidermis is acanthotic and exhibits parakeratosis. The keratinocytes display significant atypia and are enlarged with hyperchromatic nuclei. There is a lack of polarity and the atypia involves the full thickness of the epidermis. A mild inflammatory infiltrate is present.
Differential diagnosis
- Actinic keratosis:
- No full thickness atypia of keratinocytes
- Basal epidermal layer in SCCIS shows little to no visible atypia
- SCCIS typically involves the hair follicle, adjacent follicular epithelium and skin adnexa, whereas actinic keratosis does not tend to involve the adnexa
- Superficially invasive squamous cell carcinoma:
- Invasion of tumor cells through the basement membrane into the dermis
- Superficially invasive SCC shows more resemblance to the precursor actinic keratosis lesions rather than SCCIS
- Clonal seborrheic keratosis:
- Borst-Jadassohn phenomenon (sharply defined nests of keratinocytes within the epidermis), which is known as clonal seborrheic keratosis, can be confused with SCCIS
- Minimal atypia / mitotic activity and absence of nuclear crowding help with differentiation
- Paget disease:
- Bowenoid actinic keratosis:
- Can be histologically indistinguishable from SCCIS
- SCCIS and Bowenoid actinic keratosis are different based on the presence or absence of dysplasia in the follicular epithelium; Bowenoid actinic keratosis shows partial thickness atypia with less severity of atypia (J Eur Acad Dermatol Venereol 2010;24:228)
- Melanoma in situ:
- SCCIS can resemble melanoma in situ, especially in cases with pagetoid Bowen disease or Bowen disease with focal clear cell changes
- Immunohistochemistry with melanocytic markers can help with differentiation
Board review style question #1
Board review style answer #1
A. CK7 and CK5/6. CK7 will be positive in Paget disease but negative in SCCIS. CK5/6 will be negative in Paget disease but positive in SCCIS. Answer C is incorrect because these are markers for melanoma. Answer D is incorrect because these are neuroendocrine markers. Answer B is incorrect because Ki67 will tell you the proliferation index but will not differentiate SCCIS from Paget disease.
Comment Here
Reference: Squamous cell carcinoma in situ / Bowen disease
Comment Here
Reference: Squamous cell carcinoma in situ / Bowen disease
Board review style question #2
Board review style answer #2
B. Arsenic exposure causes oxidative stress and can cause SCCIS. Answer C is incorrect because HSV does not cause SCCIS; however, human papillomavirus (HPV) is a known cause of SCCIS. Answer D is incorrect because a lack of time outdoors is not a known risk factor of SCCIS; however, ultraviolet (UV) radiation is a known risk factor for SCCIS. Answer A is incorrect because antihistamine use is not a known risk factor for SCCIS. Drugs or diseases that cause immunosuppression are, however, a known risk factor for SCCIS.
Comment Here
Reference: Squamous cell carcinoma in situ / Bowen disease
Comment Here
Reference: Squamous cell carcinoma in situ / Bowen disease
Board review style question #3
Board review style answer #3
C. Full thickness atypia. The image displays squamous cell carcinoma in situ (SCCIS). Full thickness atypia is a key characteristic of SCCIS and is needed to differentiate SSCIS from actinic keratosis. Answer A is incorrect because actinic keratosis and SCCIS can display atypical mitosis. Answer D is incorrect because actinic keratosis and SCCIS can both have multinucleated cells. Answer B is incorrect because SCCIS and actinic keratosis can both have dermal lymphocytic infiltrate, which is not a necessary finding for either of these diagnoses.
Comment Here
Reference: Squamous cell carcinoma in situ / Bowen disease
Comment Here
Reference: Squamous cell carcinoma in situ / Bowen disease