Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hamza M, Shalin SC. Tubular apocrine adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticapocrinetubularadenoma.html. Accessed March 27th, 2025.
Definition / general
- Benign dermal adnexal neoplasm of apocrine derivation
- May be associated with organoid nevus, nevus sebaceus of Jadassohn and syringocystadenoma papilliferum (SCAP)
- Most cases show apocrine differentiation but eccrine differentiation may be present as well
- Reference: Int J Mol Sci 2021;22:5077
Essential features
- Rare, benign adnexal neoplasm
- Most common location is the scalp but can occur on other sites (Hum Pathol 2018;73:59)
- Microscopically, it is a well circumscribed intradermal tumor composed of tubules lined by 2 cell layers or more in a fibrous, sometimes hyalinized stroma
Terminology
- Also called apocrine adenoma, tubular adenoma, tubulopapillary hidradenoma, papillary tubular adenoma
- Considerable overlap with papillary eccrine adenoma; may be part of the same spectrum (Am J Dermatopathol 1992;14:149, Am J Dermatopathol 1993;15:482, Int J Mol Sci 2021;22:5077)
ICD coding
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
Epidemiology
- Age distribution of tubular apocrine adenoma is very wide, ranging from 28 to 85 years according to one study (Hum Pathol 2018;73:59)
Sites
- Most common location is scalp
- Rarely occurs in the nose, eyelid, leg, trunk, axilla, chest, external auditory meatus, cheek, vulva
Pathophysiology
- Associated with organoid nevus, nevus sebaceus of Jadassohn and syringocystadenoma papilliferum (SCAP) (J Cutan Pathol 1989;16:230)
- BRAF p.V600E mutations are detected in 50 - 64% of syringocystadenomas papilliferum and 66% of tubular adenomas, respectively (Cancers (Basel) 2022;14:476)
- BRAF and KRAS mutations may be present (Hum Pathol 2018;73:59)
Clinical features
- Clinically asymptomatic, well defined nodule
- Usually < 2 cm but reported up to 7 cm (Int J Mol Sci 2021;22:5077)
Diagnosis
- Skin biopsy
Prognostic factors
- Lesion is considered benign; complete excision is recommended to prevent recurrence (Medicine (Baltimore) 2021;100:e28002)
Case reports
- 34 year old woman with 10 year history of foot nodule consistent with tubular apocrine adenoma (J Dermatol 2019;46:e45)
- 36 year old woman with an asymptomatic tubular apocrine adenoma of the vulva (Indian Dermatol Online J 2018;9:346)
- 63 year old man with recurrence of a tubular apocrine adenoma of the left upper eyelid after incomplete excision (Saudi J Ophthalmol 2019;33:304)
Treatment
- Complete excision is curative (Int J Mol Sci 2021;22:5077)
Gross description
- Firm, slow growing, dermal, skin colored nodule
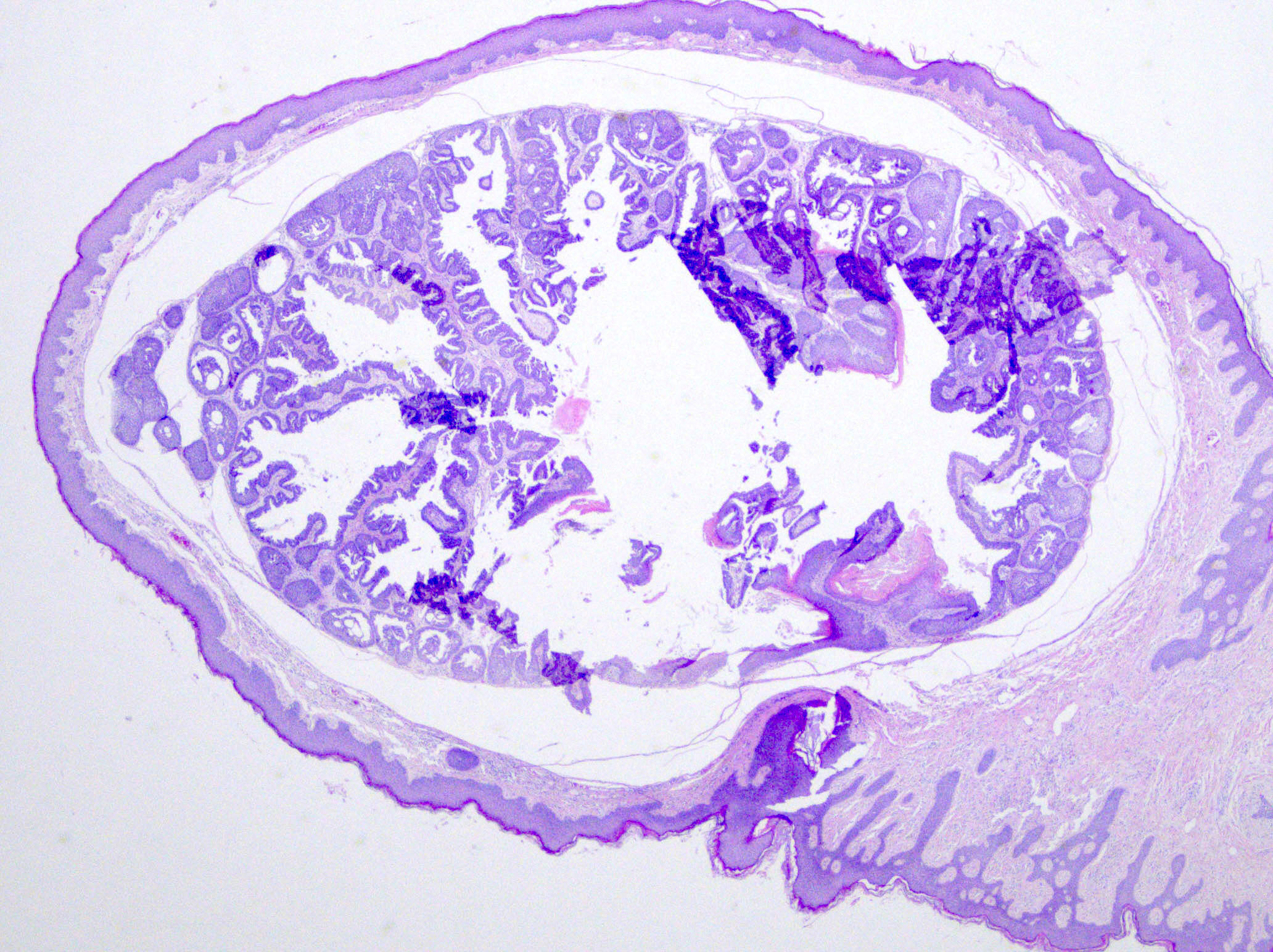
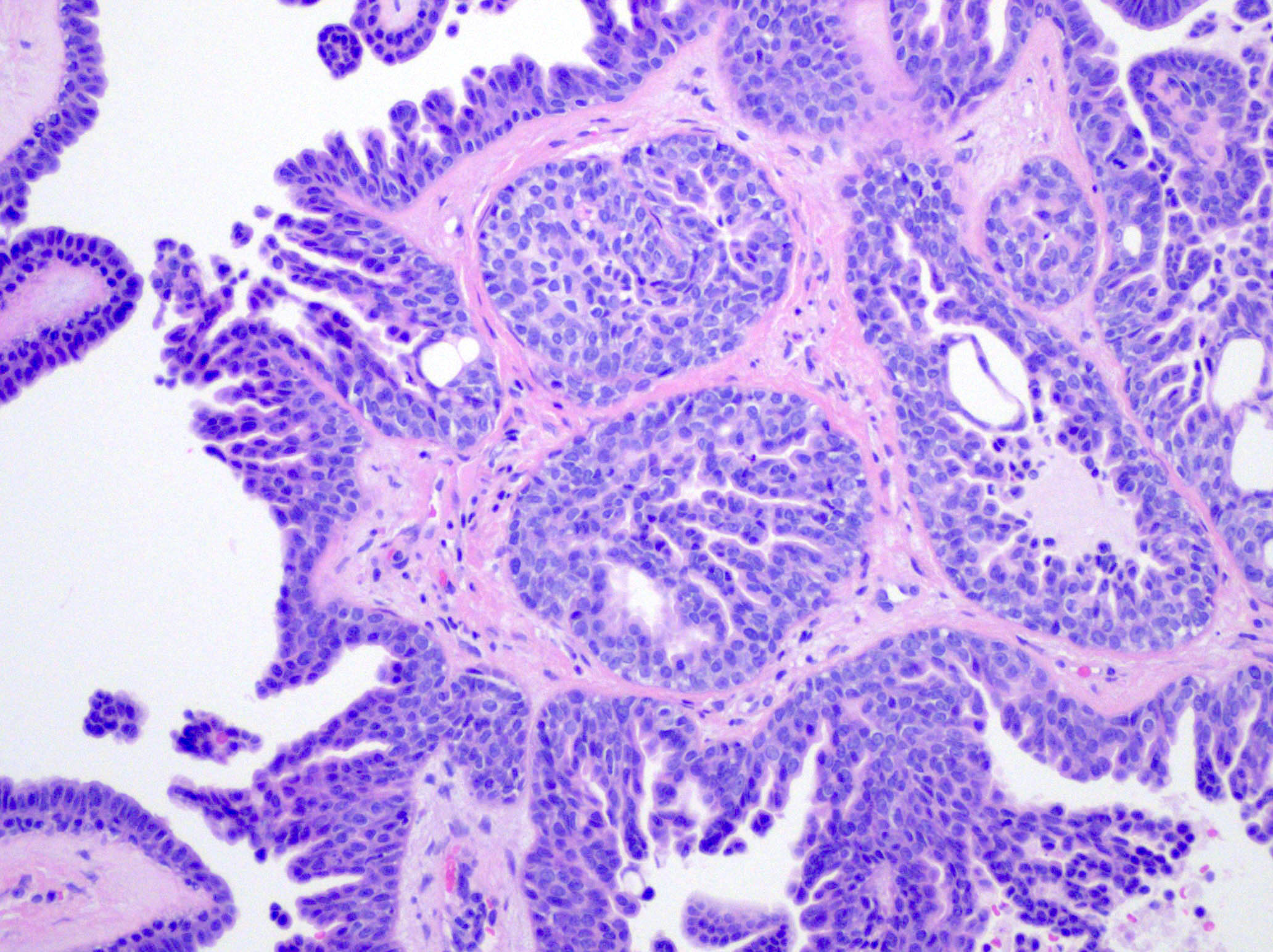
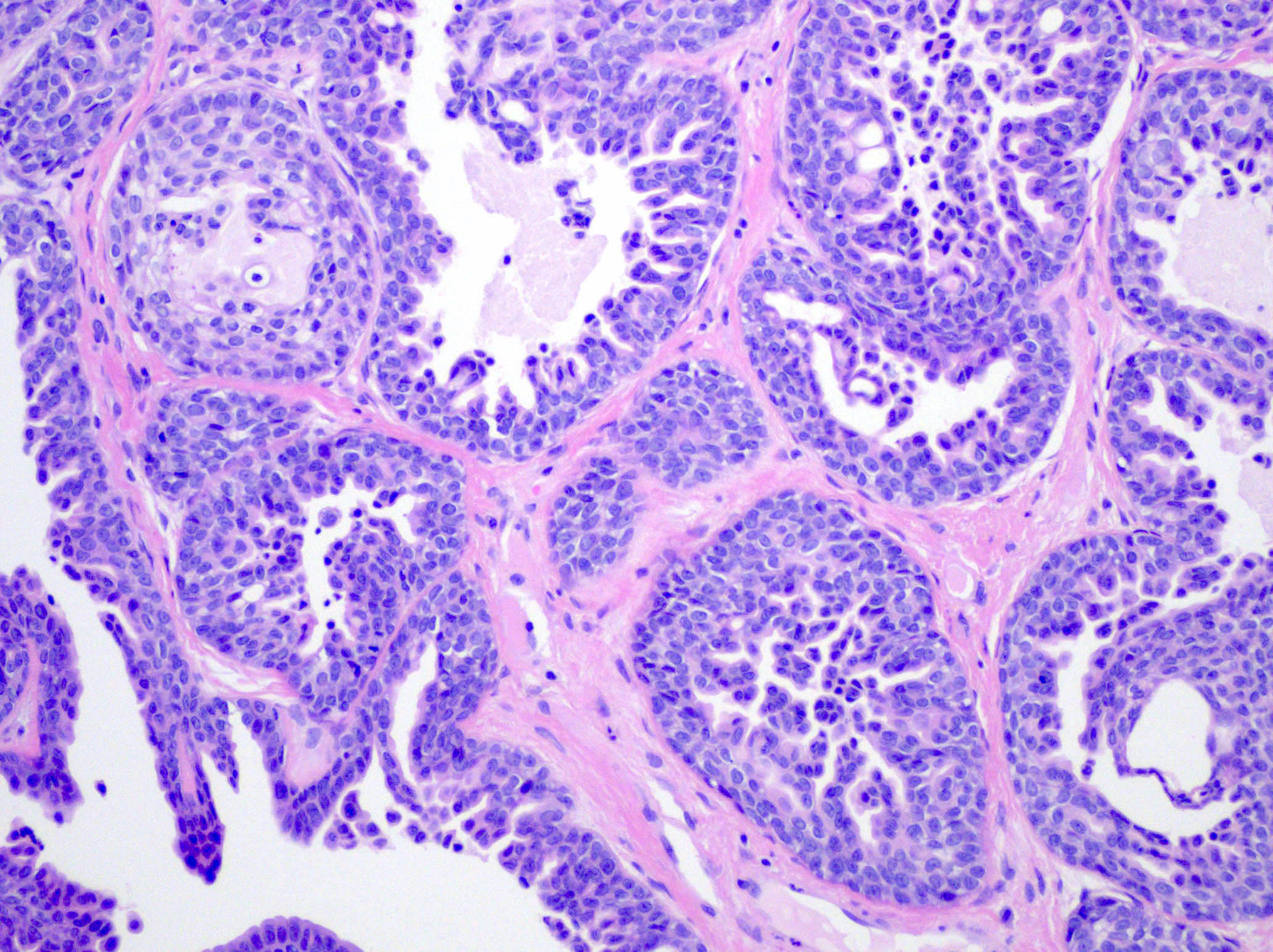
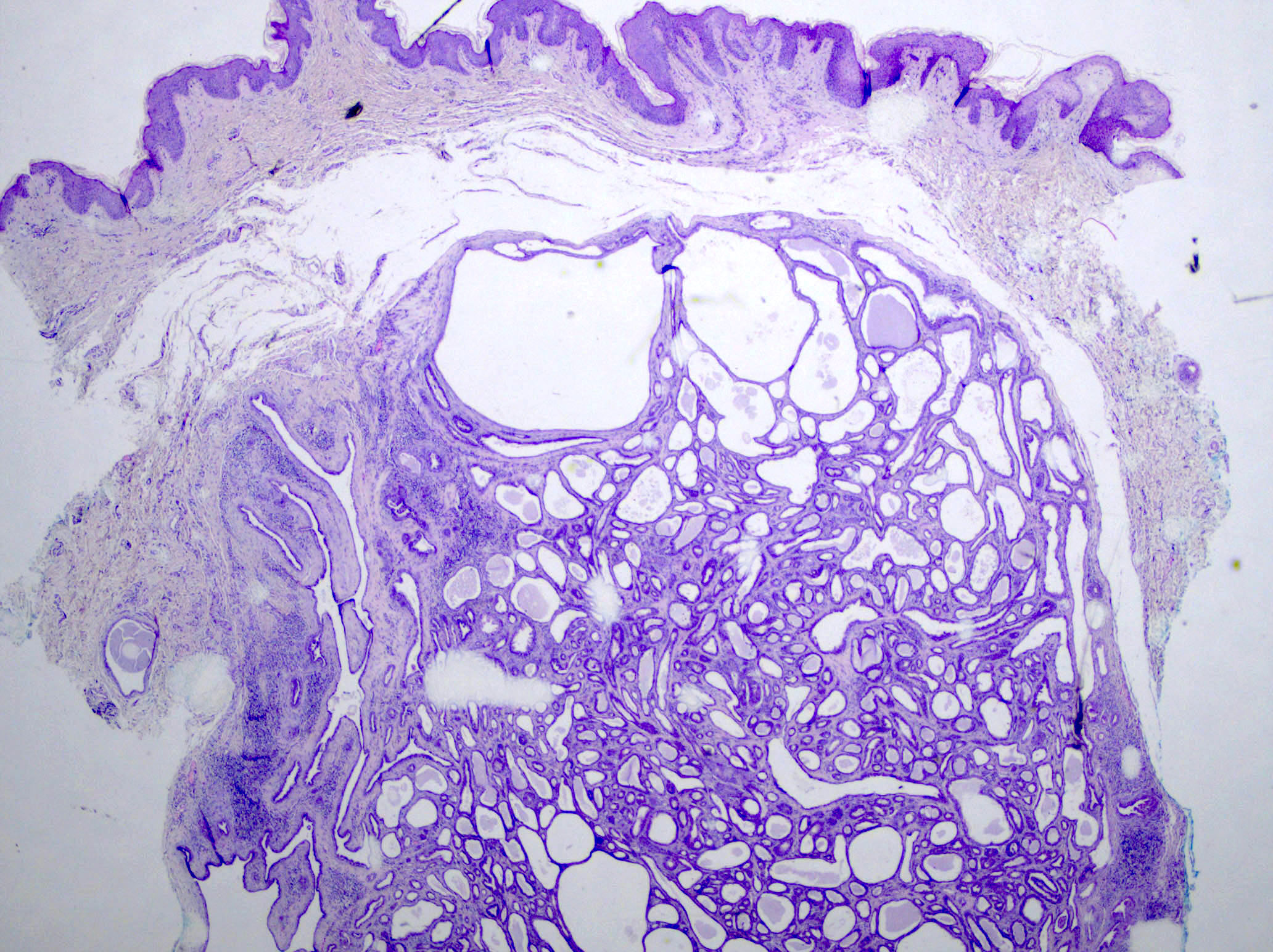
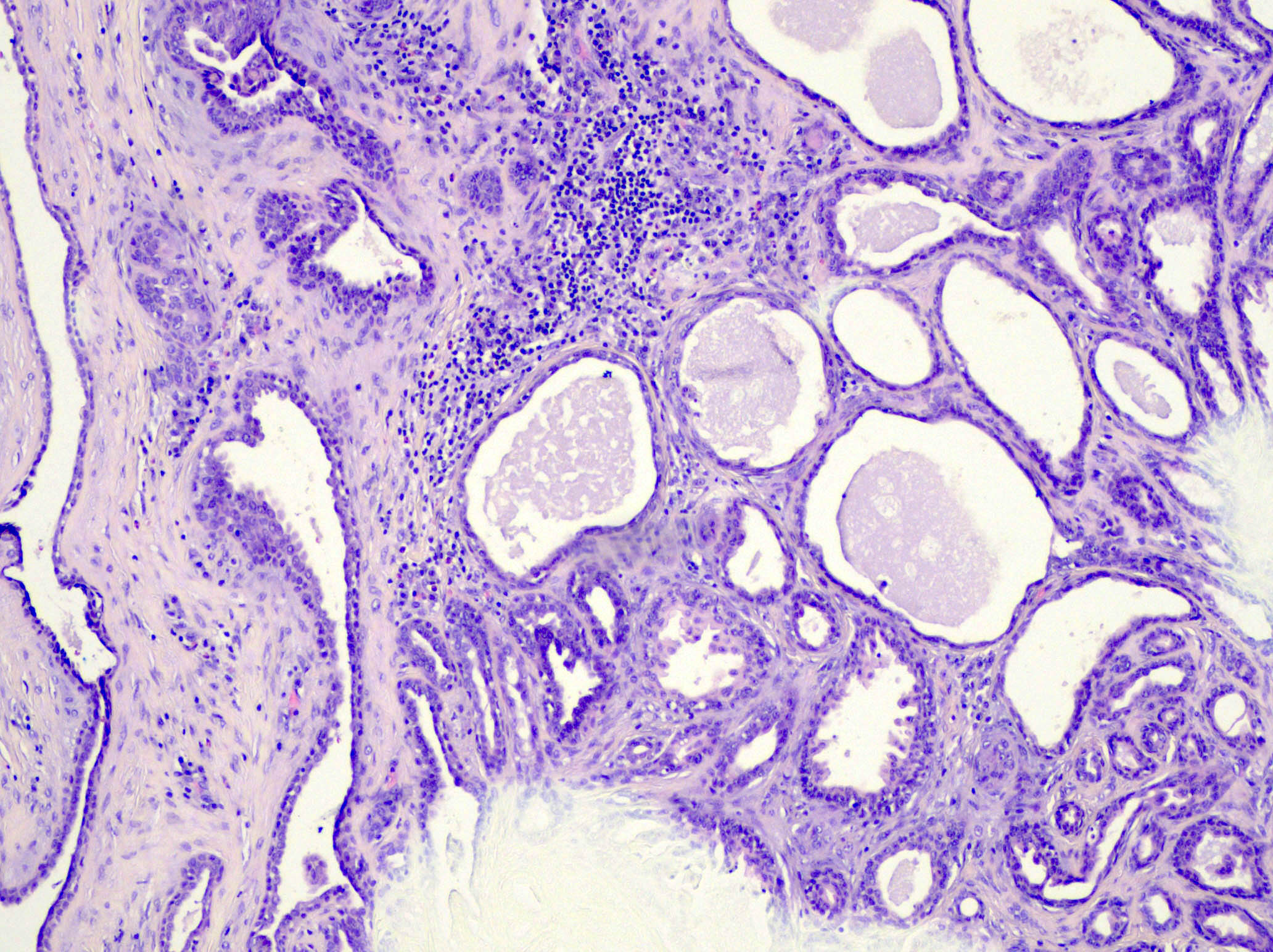
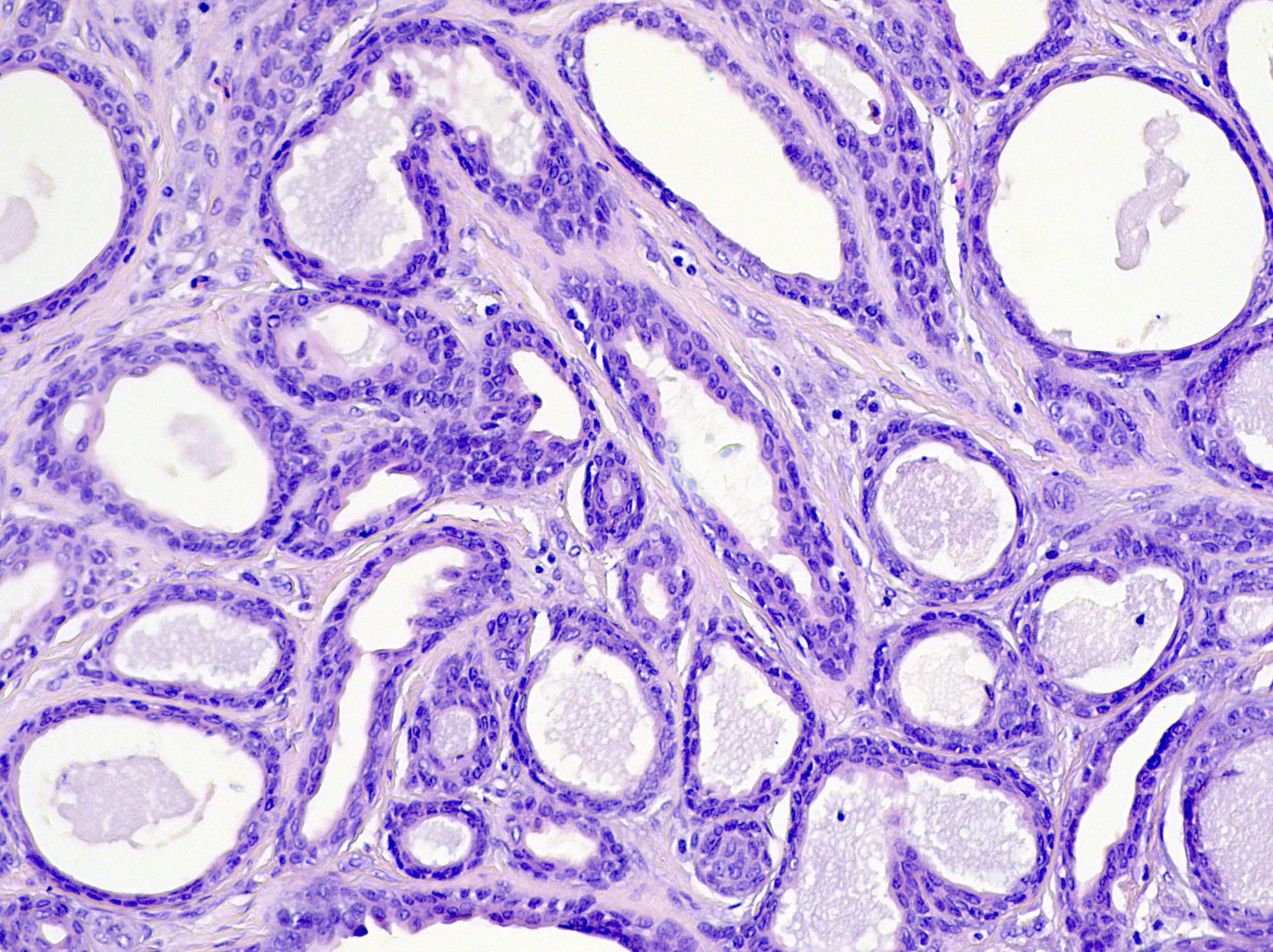
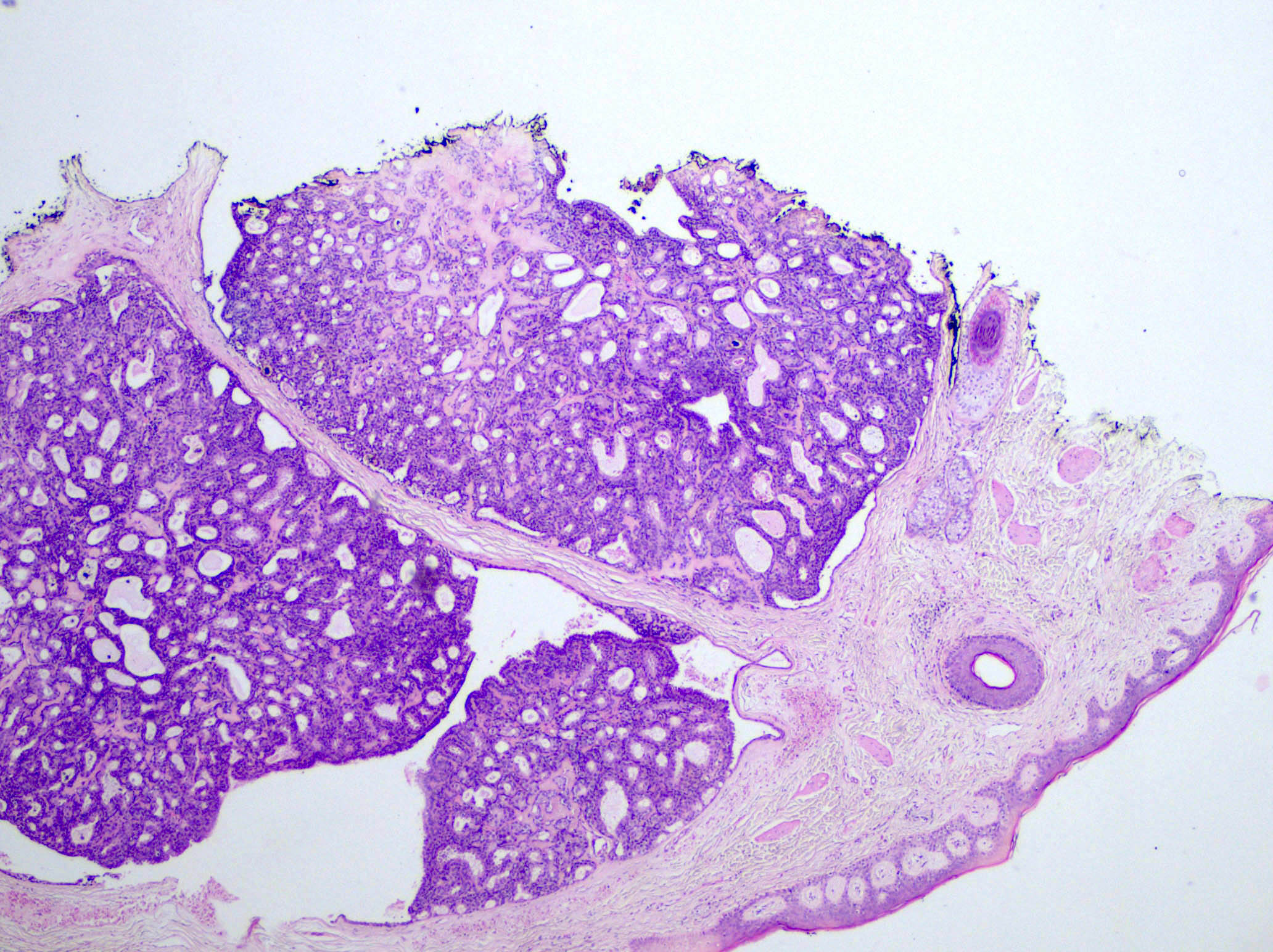
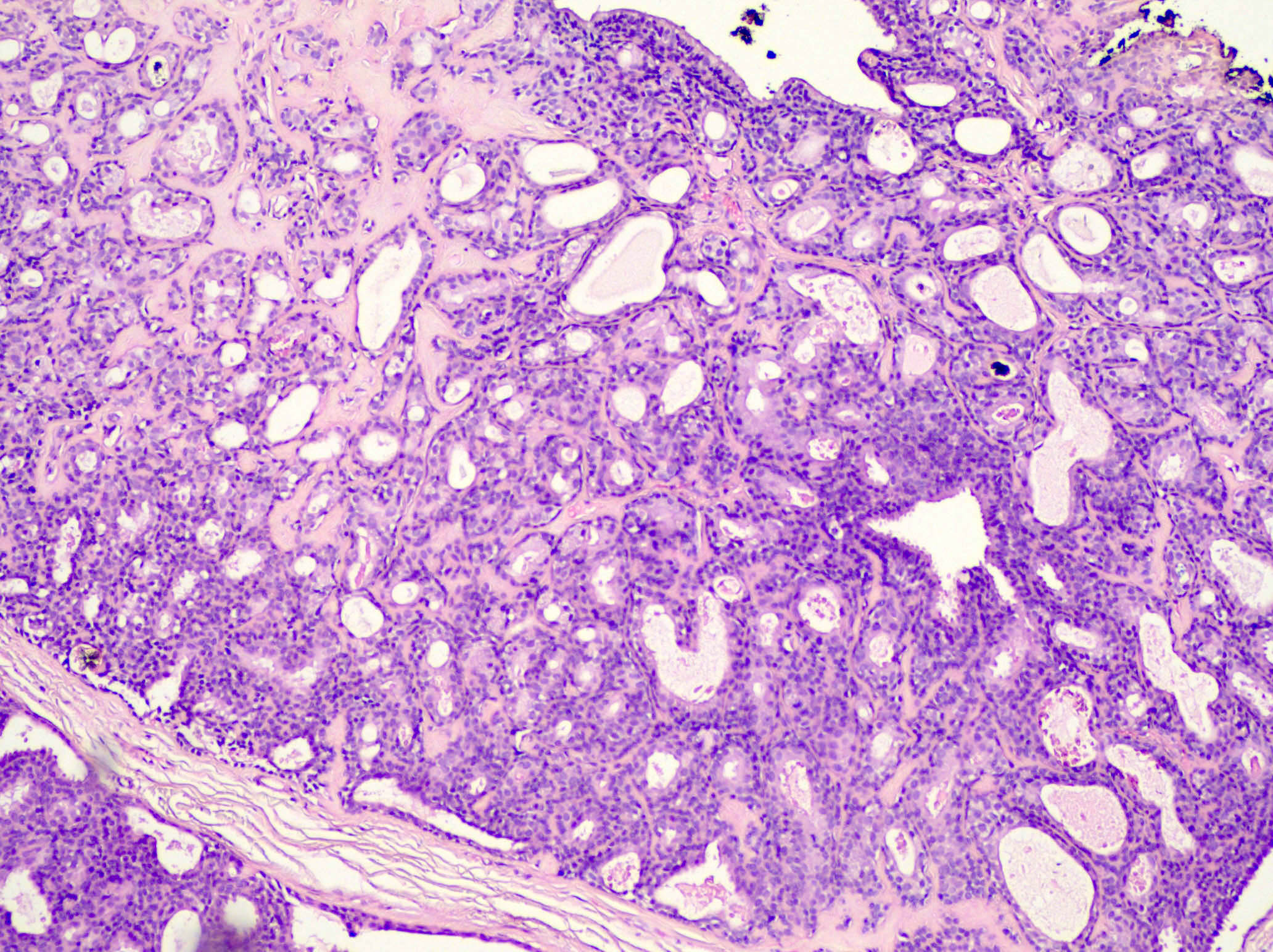
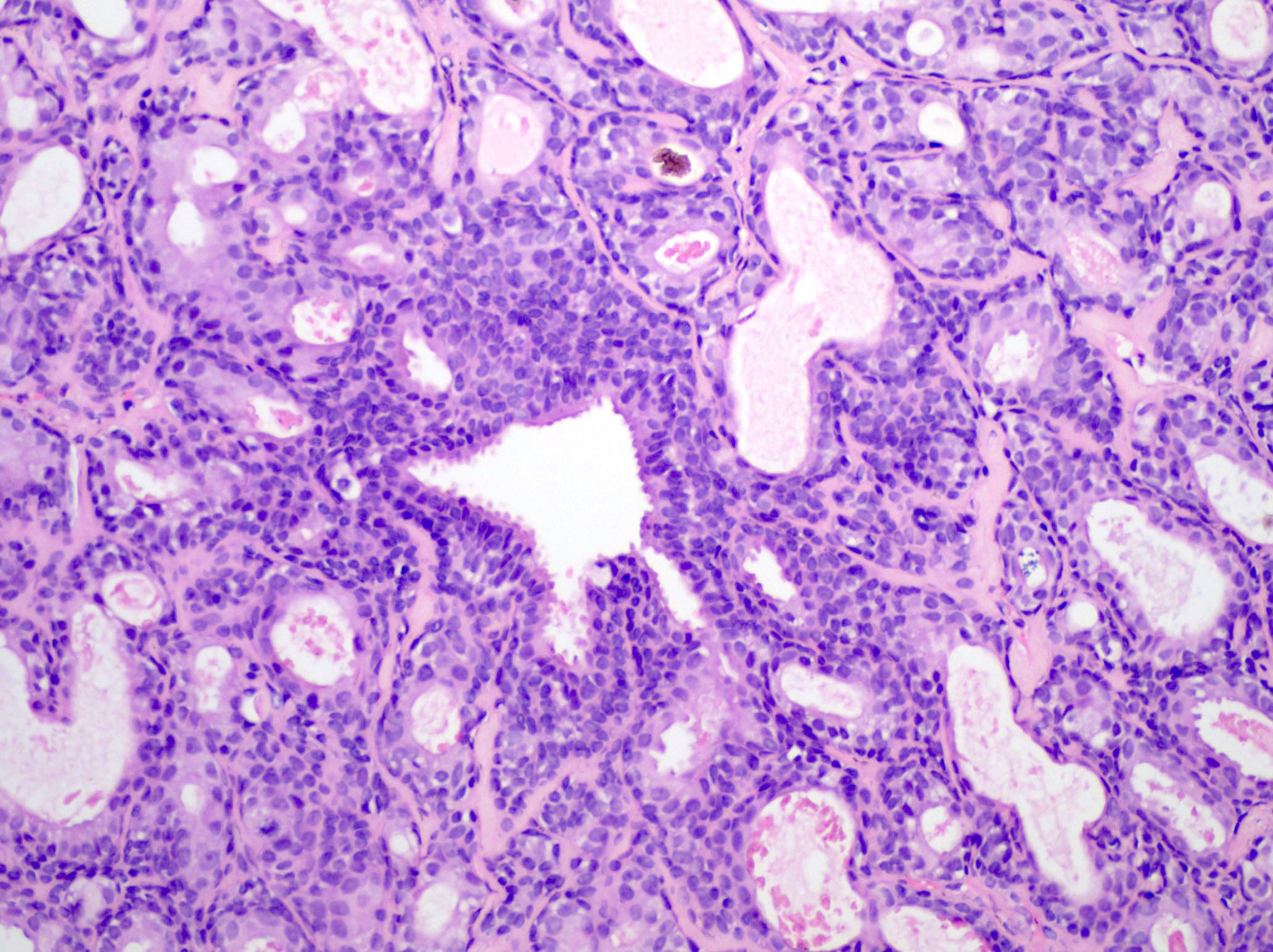
Microscopic (histologic) description
- Well circumscribed dermal neoplasm that may extend into subcutis
- Lobular pattern of dermal and subcutaneous tubular apocrine structures often encased by a fibrous, sometimes hyalinized stroma
- Lobules have dilated, variably sized, well formed tubules lined by 2 layers of epithelial cells
- Pseudopapillae are common but true papillae are more often associated with SCAP
- Decapitation secretion by apical layer and flattened outer myoepithelial layer
- Cuboidal to columnar cells with eosinophilic cytoplasm and round bland nuclei
- Often hyaline and clear cell change
- May show cyst formation with papillae or pseudopapillae protruding into the lumen
- Variable overlying epidermal hyperplasia
- Rare connection with overlying epidermis
- References: J Cutan Pathol 1987;14:114, Saudi J Ophthalmol 2019;33:304, Int J Mol Sci 2021;22:5077
Microscopic (histologic) images
Contributed by Mugahed Hamza, M.B.B.S. and Sara C. Shalin, M.D., Ph.D.
Positive stains
Negative stains
Electron microscopy description
- Tall columnar cells on basal lamina forming acini
- Cells lining tubules have luminal microvilli and apical pinching
- Conspicuous mitochondria, prominent Golgi
- Lipid rich cytoplasmic secretory vacuoles
- Decapitation secretion (J Am Acad Dermatol 1984;11:639)
Molecular / cytogenetics description
- BRAF p.V600E mutations are detected in 50 - 64% of syringocystadenomas papilliferum and 66% of tubular adenomas, respectively (Cancers (Basel) 2022;14:476)
- BRAF and KRAS mutations may be present (Hum Pathol 2018;73:59)
Sample pathology report
- Skin, scalp, shave biopsy:
- Tubular apocrine adenoma
Differential diagnosis
- Apocrine cystadenoma:
- More dilated, cystic spaces rather than tubules
- Hidradenoma papilliferum:
- Often has complex arborizing papillae, with more closely arranged tumor cells and glands
- Limited to female genital region
- Papillary apocrine carcinoma:
- More cytologic atypia, irregular nuclear contours and a higher mitotic rate along with infiltrative growth
- Papillary eccrine adenoma:
- Classically has features of eccrine rather than apocrine derivation
- Lacks decapitation secretion
- Different clinical presentation and distribution
- Syringocystadenoma papilliferum:
- Usually connects to epidermis
- Fibrovascular cores within papillary structures
- Plasma cells within stroma
- Tubular apocrine adenoma may be a variant
Board review style question #1
Which of the following is true regarding tubular apocrine adenoma?
- Associated with Cowden syndrome
- Associated with mucinous carcinoma
- Most common on the extremities
- Sometimes associated with syringocystadenoma papilliferum
Board review style answer #1
D. Sometimes associated with syringocystadenoma papilliferum. Tubular apocrine adenoma most commonly presents on the scalp, often arising in a background of nevus sebaceus and is sometimes associated with syringocystadenoma papilliferum. Answer A is incorrect because while Cowden syndrome is associated with other cutaneous adnexal tumors, it is not associated with tubular apocrine adenoma. Answer B is incorrect because it is not associated with mucinous carcinoma. Answer C is incorrect because the most common location is on the scalp, not the extremities.
Comment Here
Reference: Tubular apocrine adenoma
Comment Here
Reference: Tubular apocrine adenoma
Board review style question #2
Board review style answer #2
D. Nevus sebaceus. The tumor is a tubular apocrine adenoma, which often arises in a background of nevus sebaceus and is sometimes associated with syringocystadenoma papilliferum. Answer A is incorrect because while Cowden syndrome is associated with other cutaneous adnexal tumors, it is not associated with tubular apocrine adenoma. Answer B is incorrect because it is also not associated with mucinous carcinoma. Answer C is incorrect because while Muir-Torre syndrome is associated with various sebaceous cutaneous neoplasms, it is not associated with tubular apocrine adenoma.
Comment Here
Reference: Tubular apocrine adenoma
Comment Here
Reference: Tubular apocrine adenoma