Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gill P, Aung P. Atypical fibroxanthoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticafx.html. Accessed April 2nd, 2025.
Definition / general
- Rare low grade malignant cutaneous tumor of uncertain differentiation
- First described in the 1960s by EB Helwig (Arch Pathol Lab Med 2016;140:376)
Essential features
- Low grade malignant cutaneous neoplasm
- Usually presents on the sun exposed skin (e.g. head and neck) of elderly patients with a slight male predominance
- Histologically, a dermal based, well circumscribed tumor composed of pleomorphic, irregularly arranged, spindled to epithelioid cells with numerous mitotic figures
- Diagnosis of exclusion that requires the evaluation of multiple immunohistochemical studies to rule out other differential diagnoses
- Size, substantial involvement of the subcutis or beyond, perineural invasion, lymphovascular invasion or necrosis may suggest a diagnosis of pleomorphic dermal sarcoma instead
Terminology
- Dermal variant of superficial undifferentiated pleomorphic sarcoma / malignant fibrous histiocytoma
ICD coding
- ICD-O: 8830/1 - atypical fibroxanthoma
Epidemiology
- Elderly patients with a slight male predominance (Am J Dermatopathol 2010;32:533)
- Rarely, young patients with Li-Fraumeni syndrome or xeroderma pigmentosum
Sites
- Sun exposed skin (usually head and neck)
Pathophysiology
- Unclear but likely associated with ultraviolet induced damage
Etiology
- Associations with ultraviolet radiation exposure and ultraviolet radiation signature mutations in TP53, Li-Fraumeni syndrome, xeroderma pigmentosum, radiotherapy, immunosuppression, organ transplantation
Clinical features
- Rapidly growing, single red to pink nodule or polypoid tumor
- Usually less than 2 cm in diameter (Am J Dermatopathol 2010;32:533)
- May be ulcerated (J Cutan Pathol 2010;37:301)
- Clinical differential may include squamous cell carcinoma or basal cell carcinoma
Diagnosis
- Diagnosis of exclusion
- Requires use of ancillary techniques (i.e. immunohistochemistry panels) to rule out other differential diagnoses
- Rendering a definitive diagnosis on superficial biopsies alone may be difficult, given the differential diagnosis of pleomorphic dermal sarcoma
Prognostic factors
- Low grade tumor with an almost always benign clinical course
- Recurrence may occur due to incomplete surgical removal
- Metastasis is rare (Am J Dermatopathol 2015;37:455)
Case reports
- 24 year old man with xeroderma pigmentosum and a rapidly growing conjunctival mass (Ocul Oncol Pathol 2015;1:254)
- 72 year old man with an ulcerated nodule on the lower leg (J Cutan Pathol 2017;44:951)
- 74 year old man with a mass on the ear (An Bras Dermatol 2019;94:239)
- 75 year old man with an intermittently bleeding nodule on the left temple and 90 year old man with a violaceous nodule on the vertex of the scalp (JAAD Case Rep 2018;4:292)
Treatment
- Complete surgical removal with wide local excision or Mohs micrographic surgery (Dermatol Clin 2019;37:253)
Gross description
- Single red to pink nodule or polypoid tumor, usually less than 2 cm in diameter and may be ulcerated and covered with serum crust
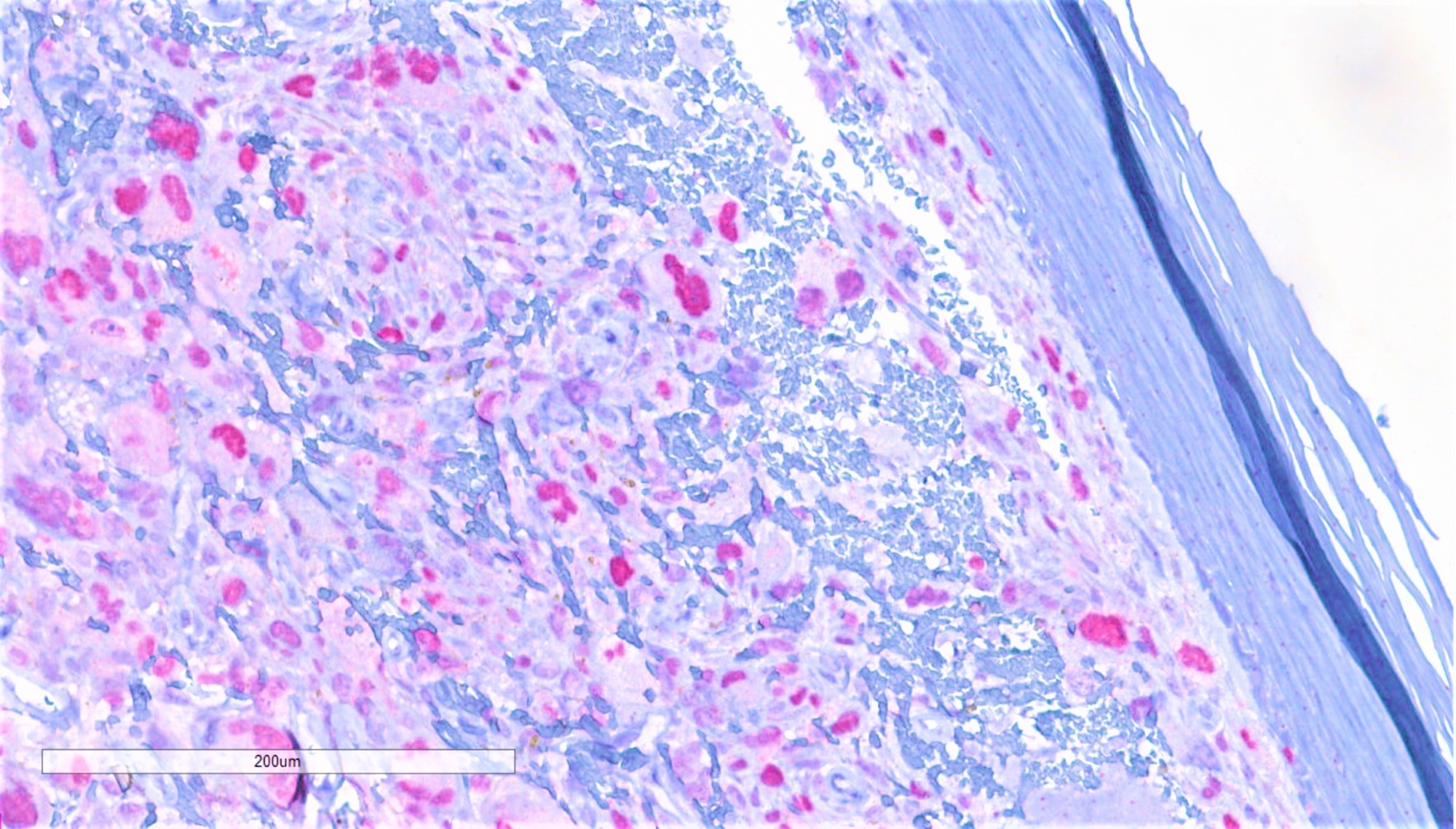
Microscopic (histologic) description
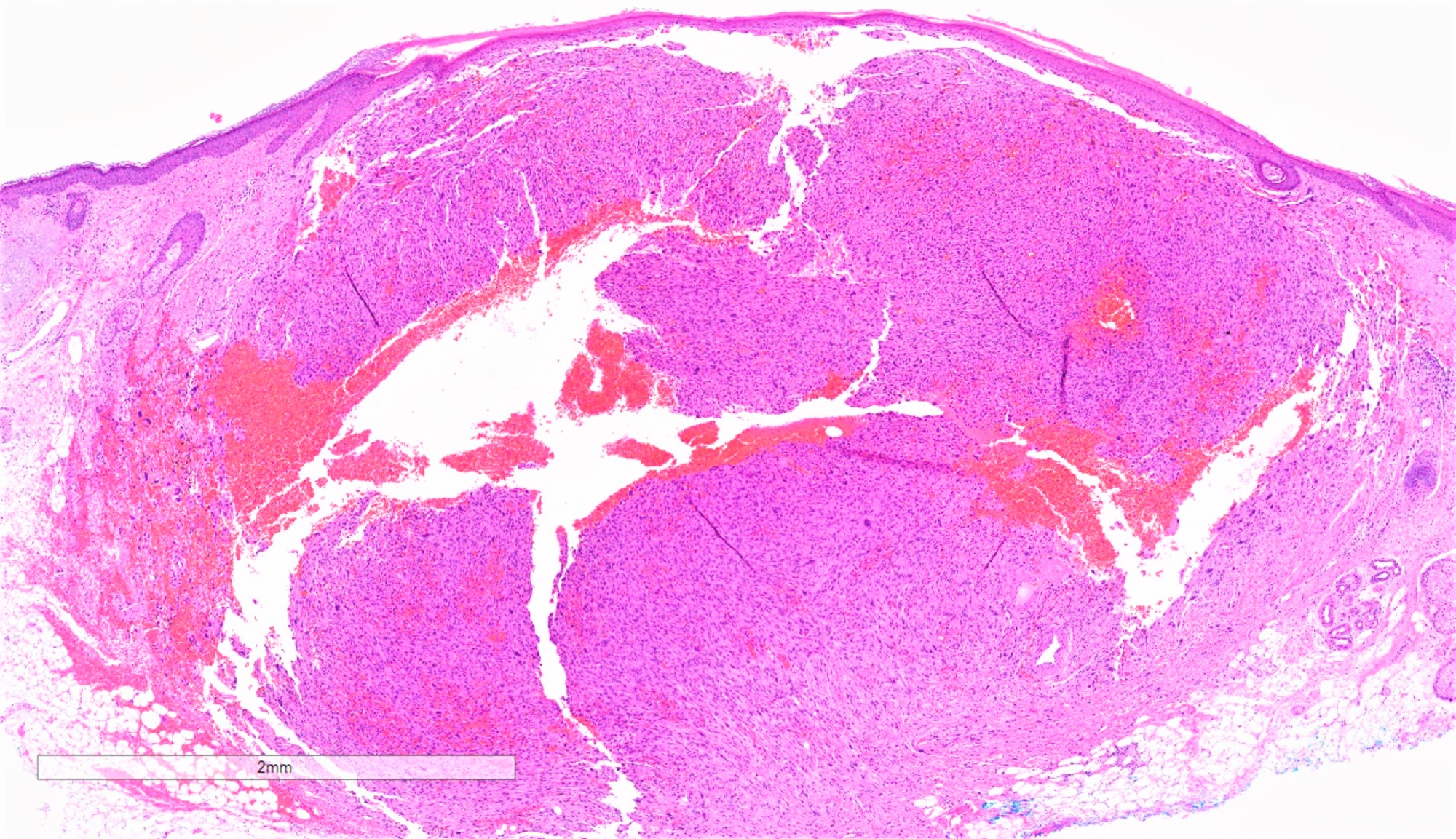
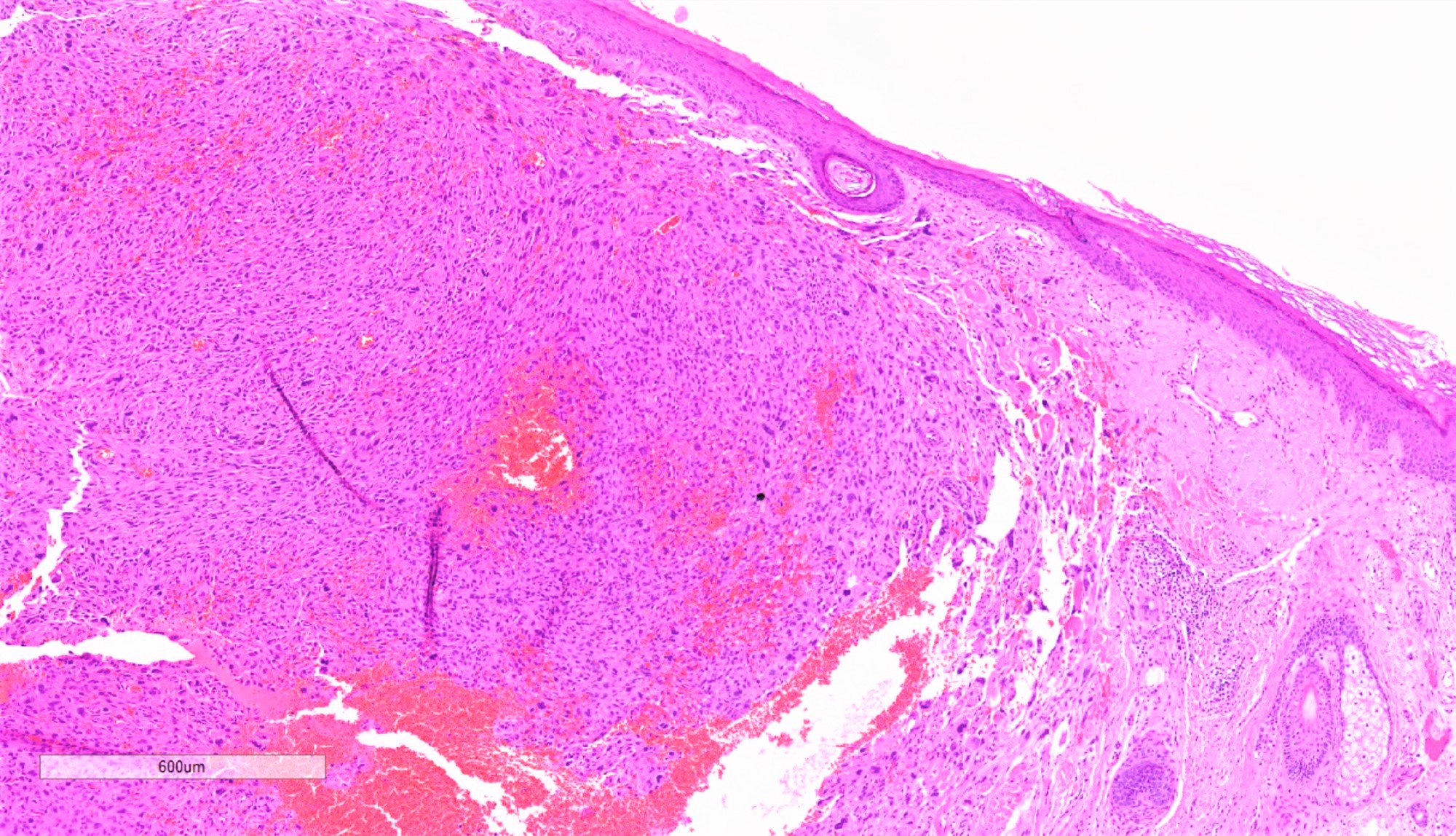
- Dermal based, well circumscribed tumor
- Composed of irregularly arranged spindled to epithelioid cells with no involvement of the subcutis
- Necrosis, lymphovascular invasion and perineural invasion should not be present
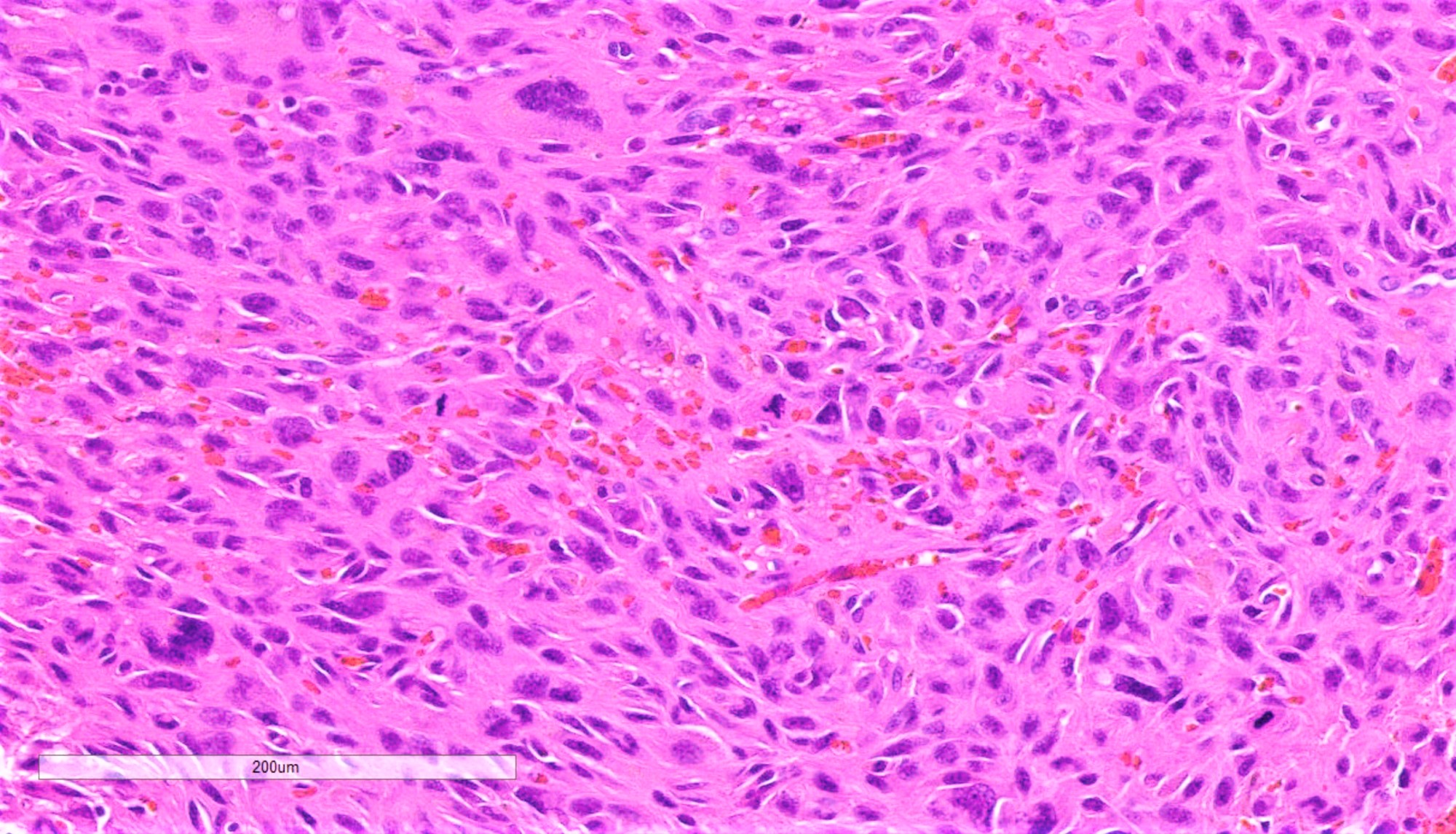
- Cytomorphologically, lesional cells are highly bizarre and atypical, with marked pleomorphism in size and shape, abundant eosinophilic cytoplasm, occasional multinucleation and numerous mitotic figures, including atypical forms
- Epidermal collarette, ulceration and actinic changes, including prominent solar elastosis, may be present
- No connection to the overlying epidermis and no in situ component
- Histologic variants (Am J Dermatopathol 2010;32:533):
- Spindle cell (Am J Dermatopathol 2015;37:509)
- Clear cell
- Granular cell (Cesk Patol 2014;50:34)
- Keloidal (Am J Dermatopathol 2010;32:713)
- Myxoid
- Pseudoangiomatous (Ann Diagn Pathol 2013;17:502)
- Pigmented (Histopathology 1998;33:537)
- Plaque-like
- May have forms with osteoclast giant cells, osteoid and chondroid formation (Am J Dermatopathol 2010;32:533)
Microscopic (histologic) images
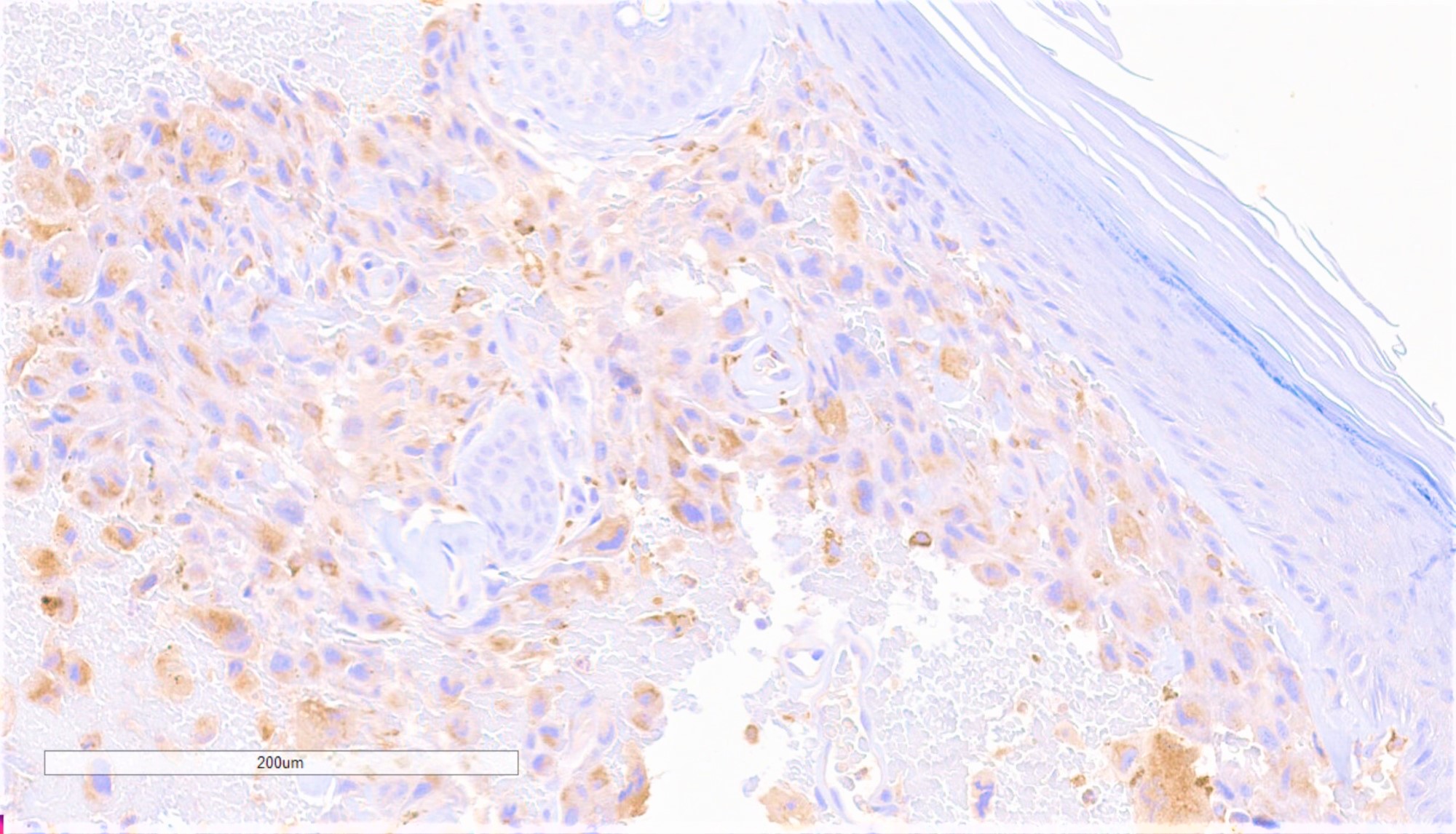
Positive stains
- Nonspecific: CD10, CD99, procollagen 1, vimentin (Australas J Dermatol 2005;46:235, Stomatologiia (Mosk) 2005;84:36, J Cutan Pathol 2007;34:415, Am J Clin Pathol 2002;117:126)
- May be positive for CD68, CD163, CD117, MITF, factor XIIIa, CD31, MelanA and HMB45 in multinucleated giant cells, SMA, EMA, p63 (Am J Dermatopathol 2008;30:34, Am J Dermatopathol 2014;36:888, J Cutan Pathol 2010;37:301, Am J Dermatopathol 2010;32:533)
Negative stains
Molecular / cytogenetics description
- Genetics are currently poorly understood
- FAT1, NOTCH1/2, CDKN2A, TP53, TERT mutations (Mod Pathol 2018;31:418)
- Loss of 9p and 13q, gain of 8q, gain of CDKN2A (Clin Sarcoma Res 2019;9:2)
- TERT promoter mutations (Mod Pathol 2014;27:502)
Videos
Atypical fibroxanthoma and mimics
Atypical fibroxanthoma pearls
Sample pathology report
- Vertex scalp, skin shave:
- Malignant spindle cell neoplasm predominantly in dermis, consistent with atypical fibroxanthoma, present at tissue edges (see comment)
- Comment: Sections show a dermal, poorly differentiated pleomorphic neoplasm, characterized by large and bizarre spindled to epithelioid cells with abundant eosinophilic cytoplasm, occasional multinucleation and numerous mitotic figures. Adjacent dermis contains solar elastosis. The overlying epidermis does not have a connection to the tumor. Immunohistochemical studies show that lesional cells are positive for CD68 and negative for CAM5.2, AE1 / AE3, CD31 and S100. Overall, these features support the above interpretation.
Differential diagnosis
- Pleomorphic dermal sarcoma:
- Histologically similar to atypical fibroxanthoma but larger and shows substantial involvement of the subcutis or beyond, perineural invasion, lymphovascular invasion or necrosis
- Behaves in a more aggressive manner than atypical fibroxanthoma
- Melanoma:
- Usually associated with an in situ component in the overlying epidermis
- Melanin pigment, lymphovascular invasion, perineural invasion, involvement of the subcutis and microsatellites may also be present
- Lesional cells are positive for melanocytic immunohistochemical markers (e.g. SOX10, S100, MelanA, HMB45, tyrosinase and MITF), although reactivity to melanocytic markers other than S100 and SOX10 may be lost in spindle cell / desmoplastic variants
- Squamous cell carcinoma:
- Usually associated with a connection to the overlying epidermis and an in situ component
- Keratin, intercellular bridging, invasion of the subcutis, perineural invasion and lymphovascular invasion may be present
- Lesional cells are positive for p40 (Am J Surg Pathol 2014;38:1102)
- Angiosarcoma:
- Atypical fibrous histiocytoma:
- Usually presents in younger patients, lacks prominent actinic changes and may have areas of classic dermatofibroma in the periphery of the tumor
- Leiomyosarcoma:
- Usually positive for smooth muscle markers, such as smooth muscle myosin and desmin
- Metastatic carcinoma:
- Should be considered in the differential diagnosis for patients with a known history of carcinoma
- Lesional cells are usually positive for pancytokeratin and other immunohistochemical markers similar to the primary tumor
- Superficial CD34+ fibroblastic tumor:
Additional references
Board review style question #1
The finding of which of the following additional histologic features in the lesion shown above would most likely favor a diagnosis of melanoma over atypical fibroxanthoma?
- Presence of an in situ component
- Presence of numerous mitotic figures, including atypical forms
- Presence of pigment
- Reactivity for MITF
Board review style answer #1
A. Presence of an in situ component. Choice B is incorrect because numerous mitotic figures, including atypical forms, are seen in both melanoma and AFX. Choice C is incorrect because pigment can be seen in both AFX (hemosiderin) and melanoma (melanin). Choice D is incorrect because reactivity for anti-MiTF may be seen in both melanoma and AFX.
Comment Here
Reference: Atypical fibroxanthoma
Comment Here
Reference: Atypical fibroxanthoma
Board review style question #2
Assuming all other listed markers are negative, a positive immunohistochemical study with which marker is most consistent with a diagnosis of atypical fibroxanthoma?
- CD10
- p40
- S100
- Smooth muscle myosin
Board review style answer #2
A. CD10. Choice B is incorrect because p40 positivity suggests a diagnosis of squamous cell carcinoma. Choice C is incorrect because S100 positivity suggests a diagnosis of melanoma or neural tumor. Choice D is incorrect because smooth muscle myosin positivity suggests a diagnosis of smooth muscle tumor.
Comment Here
Reference: Atypical fibroxanthoma
Comment Here
Reference: Atypical fibroxanthoma