Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Holliday D, Prieto-Granada CN. Special site nevus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticspecialsitenevus.html. Accessed March 30th, 2025.
Definition / general
- Melanocytic nevi located on specific anatomical sites, such as the scalp, ear, breast, umbilicus, genital skin, acral skin, axilla and other flexural sites that may demonstrate atypical histologic features (Am J Dermatopathol 2016;38:867, Mod Pathol 2006;19:S4)
Essential features
- Benign melanocytic tumors
- May display atypical features, such as pagetoid spread, lentiginous growth and epidermal effacement
- Lack of deep or atypical mitoses
Terminology
- Melanocytic nevi with site related atypia, melanocytic nevi of special sites
ICD coding
- ICD-10:
- ICD-11:
Epidemiology
- Melanocytic nevi of the breast appear to be the most common special site (56%), followed by axilla (16%) and then scalp (12%) (J Cutan Pathol 2020;47:664)
- Melanocytic nevi of the ear do not appear to have a predilection for age (5 - 86 years, mean: 42.4) and occur in a similar frequency between males and females (F:M = 1.1:1) (J Cutan Pathol 2005;32:40)
- Scalp melanocytic nevi are more commonly found in adolescents with a slightly higher frequency of occurrence in males; adults and children are less commonly affected (Br J Dermatol 2011;165:137)
- Breast melanocytic nevi more commonly present in younger females ages 30 - 40 but may occur in both men and women (J Am Acad Dermatol 2016;75:364, J Cutan Pathol 2004;31:137)
- Genital melanocytic nevi most commonly present in premenopausal, reproductive age woman with a median age of 26 years but may occur in children and commonly involve mucosal sites (Am J Surg Pathol 2008;32:51)
- Acral melanocytic nevi occur with a frequency of 10 - 30% in the population and are more common in patients of color (Arch Dermatol 2010;146:1085)
Pathophysiology
- Melanocytic nevi can be either acquired or congenital
- Acquired melanocytic nevi are thought to result from activation of oncogenes such as BRAF (usually BRAF V600E) or NRAS, resulting in clonal proliferation of melanocytes (J Invest Dermatol 2019;139:1762)
- Congenital melanocytic nevi are thought to result from arrested migration of melanocyte precursor neural crest derived stem cells within the dermis
Etiology
- Etiology of variation in histologic features of site specific melanocytic nevi is not known
- Possible causes that determine these peculiar cytologic and architectural features are unknown; developmental factors or hormonal changes (e.g., those occurring in adolescence and pregnancy) have been suggested as contributing factors
Diagrams / tables
| Nevi site | Atypical nevi features | Differentiating features from melanoma |
| Scalp | Lentiginous growth, pagetoid spread, loss of symmetry | Lack of severe atypia (uniform atypia), dermal maturation, lack of deep or atypical mitoses |
| Ear | Pagetoid spread, irregular nesting pattern, cytologic atypia, may induce host inflammatory response | Dermal maturation, lack of severe atypia (uniform atypia), symmetry, lack of deep or atypical mitoses |
| Breast | Dyshesive nests, cytologic atypia, rete effacement | Dermal maturation, symmetry, effacement of rete limited to center, lack of deep or atypical mitoses |
| Genital | Large dyshesive nests, lentiginous growth, asymmetry is common, pagetoid spread | Dermal maturation, lack of deep or atypical mitoses, limited pagetoid spread |
| Acral | Lentiginous growth, pagetoid spread | Lentiginous growth does not involve crista profunda intermedia, lack of deep or atypical mitoses, dermal maturation |
Clinical features
- Melanocytic nevi of the ear:
- May present as macules or papules
- Uniform coloration (light or dark brown) (Busam: Pathology of Melanocytic Tumors, 1st Edition, 2018)
- Melanocytic nevi of acral skin:
- More common in patients of color (J Am Acad Dermatol 2016;74:724)
- Well circumscribed
- Parallel furrow dermoscopic patterns are common
- Melanocytic nevi of the genitals:
- Predilection for premenopausal and reproductive age women (Am J Surg Pathol 2008;32:51)
- May affect hair bearing and mucosal sites
- Melanocytic nevi of the breast:
- Predilection for premenopausal and reproductive age women (J Am Acad Dermatol 2016;75:364)
- Irregular borders
- Irregular pigment network and nonuniform dots and globules
- Melanocytic nevi of the scalp:
- More common in adolescent males (Br J Dermatol 2011;165:137)
- Flat, papular or plaque-like
- Perifollicular hypopigmentation commonly seen on dermoscopy
- Melanocytic nevi of the umbilicus:
- More common in women
- The umbilicus and periumbilical region are considered to be anatomically located in the milk line, an ectodermal ridge associated with mammary gland and breast development (Histopathology 2015;66:363)
Diagnosis
- Clinical presentation and dermoscopic findings
- Definitive diagnosis is made through histologic examination of excised specimen
Case reports
- 5 year old girl with an asymptomatic, brown, pigmented macule on the left nipple areolar complex (Breast J 2016;22:237)
- 18 year old woman with an asymptomatic raised, pigmented swelling over the scalp since birth, with initial focal hair loss followed by rapid enlargement of the lesion with hair growth (Int J Trichology 2019;11:253)
- 24 year old woman with pain, itching and discharge from left ear nevus, mimicking pyogenic granuloma (Otol Neurotol 2022;43:e137)
- Man in his mid 30s with a pigmented lesion on the glans penis that quickly grew in size over a 10 month period, mimicking melanoma (JAAD Case Rep 2020;6:323)
- 43 year old woman with a large brown-yellow cerebriform plaque on the dorsum of the hand present since birth (Indian J Dermatol Venereol Leprol 2021;87:876)
Treatment
- Complete excision
Microscopic (histologic) description
- Many nevi from special sites have typical features that, when taken in conjunction with the unusual morphologic features that may be present and the patient’s clinical information, assist in deciding whether the lesion is an atypical melanocytic proliferation or a nevus with special site features
- A junctional melanocytic proliferation in a patient > 50 years without a bland dermal component should be regarded as suspicious, while a relatively atypical lesion in a younger patient is unlikely to be malignant
- Equally as important is the morphology of the melanocytes present, with vertically orientation and coarse melanosomes conveying higher risk of malignancy
- Melanocytic nevi of the ear (Am J Dermatopathol 2005;27:111):
- Frequently display poor lateral circumscription
- Junctional nests may not be centered and can be placed within inter-rete spaces and along sides of rete
- May display pagetoid spread
- Irregular nesting pattern
- Cytologic atypia that is uniformly present may be seen
- May induce a host inflammatory response
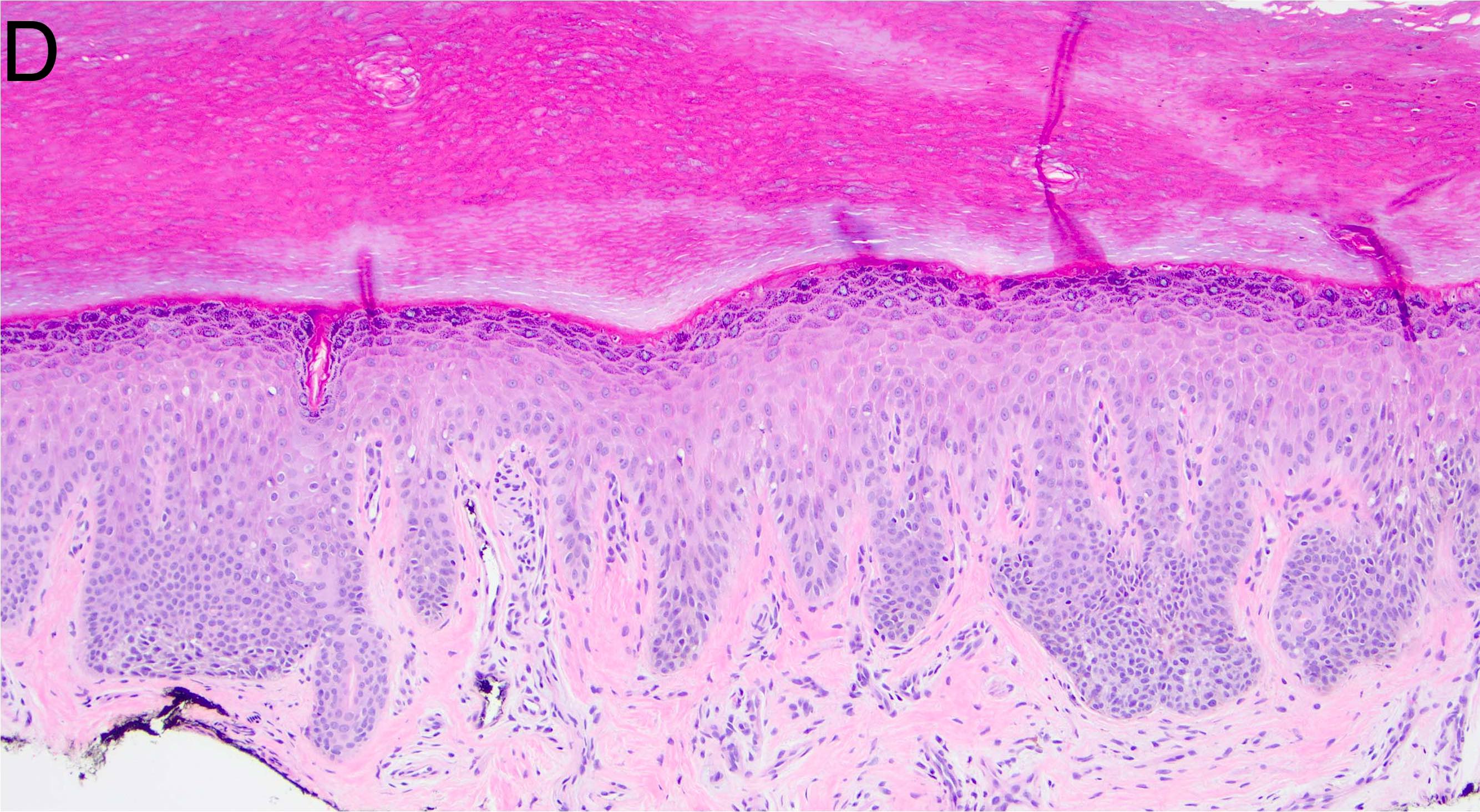
- Melanocytic nevi of the acral skin (Am J Dermatopathol 2016;38:867):
- May have unusually prominent pagetoid or lentiginous growth pattern
- Should not display high grade cytologic atypia
- Dermal component should display well formed nests and maturation with descent
- Cytologic atypia and mitotic activity should not be seen in dermal component
- There is an absence of lentiginous involvement of the crista profunda intermedia
- Banal appearing nests along eccrine apparatus are an acceptable feature in acral nevi
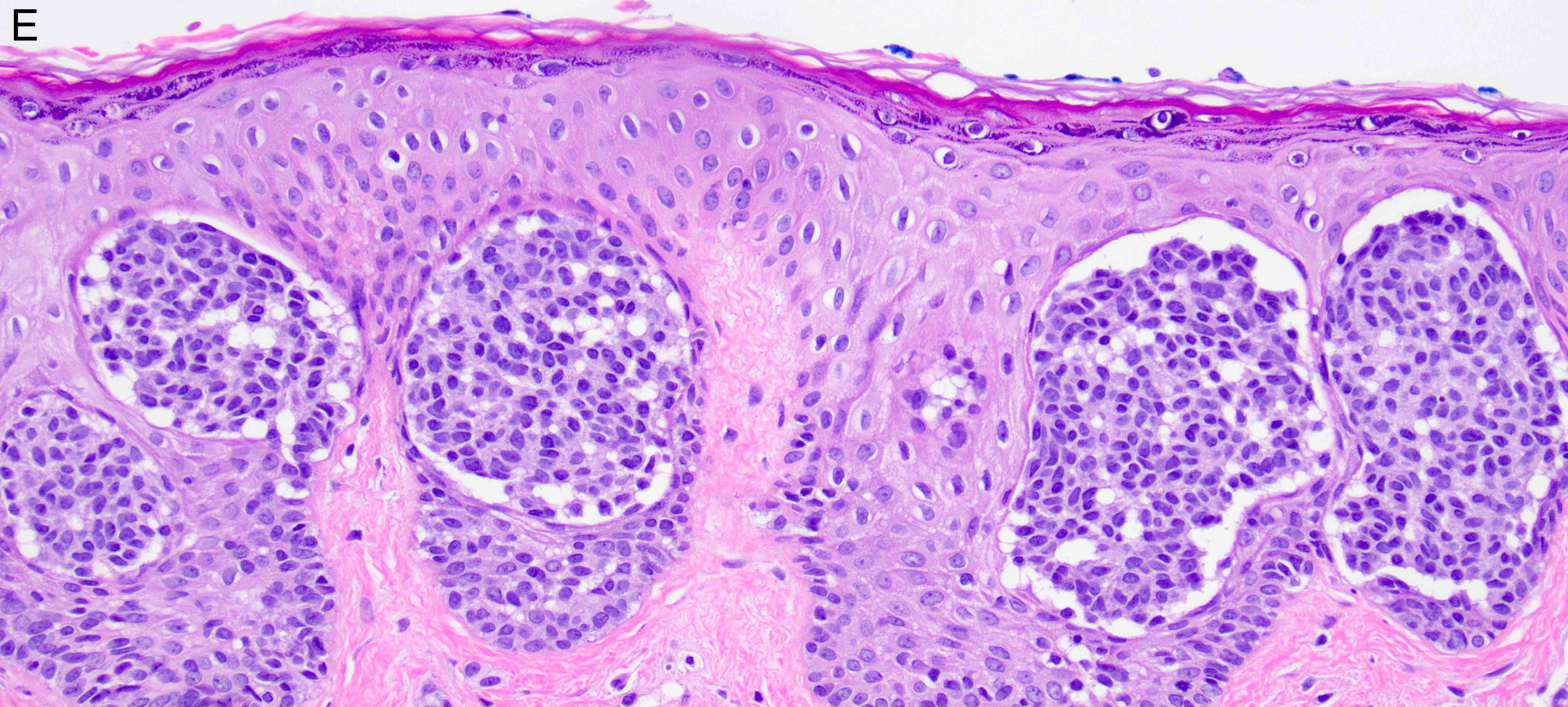
- Melanocytic nevi of the genitals (Am J Surg Pathol 2008;32:51):
- May contain large dyshesive irregular nests in close proximity to one another
- May contain a prominent lentiginous component
- Deeper nests may evoke a stromal fibrotic host response
- Lesion should maintain symmetry, circumscription and maturation
- Pagetoid growth can be seen but typically does not extend into granular layer
- Junctional component may extend into adnexal structures
- Significant cytologic atypia can occur
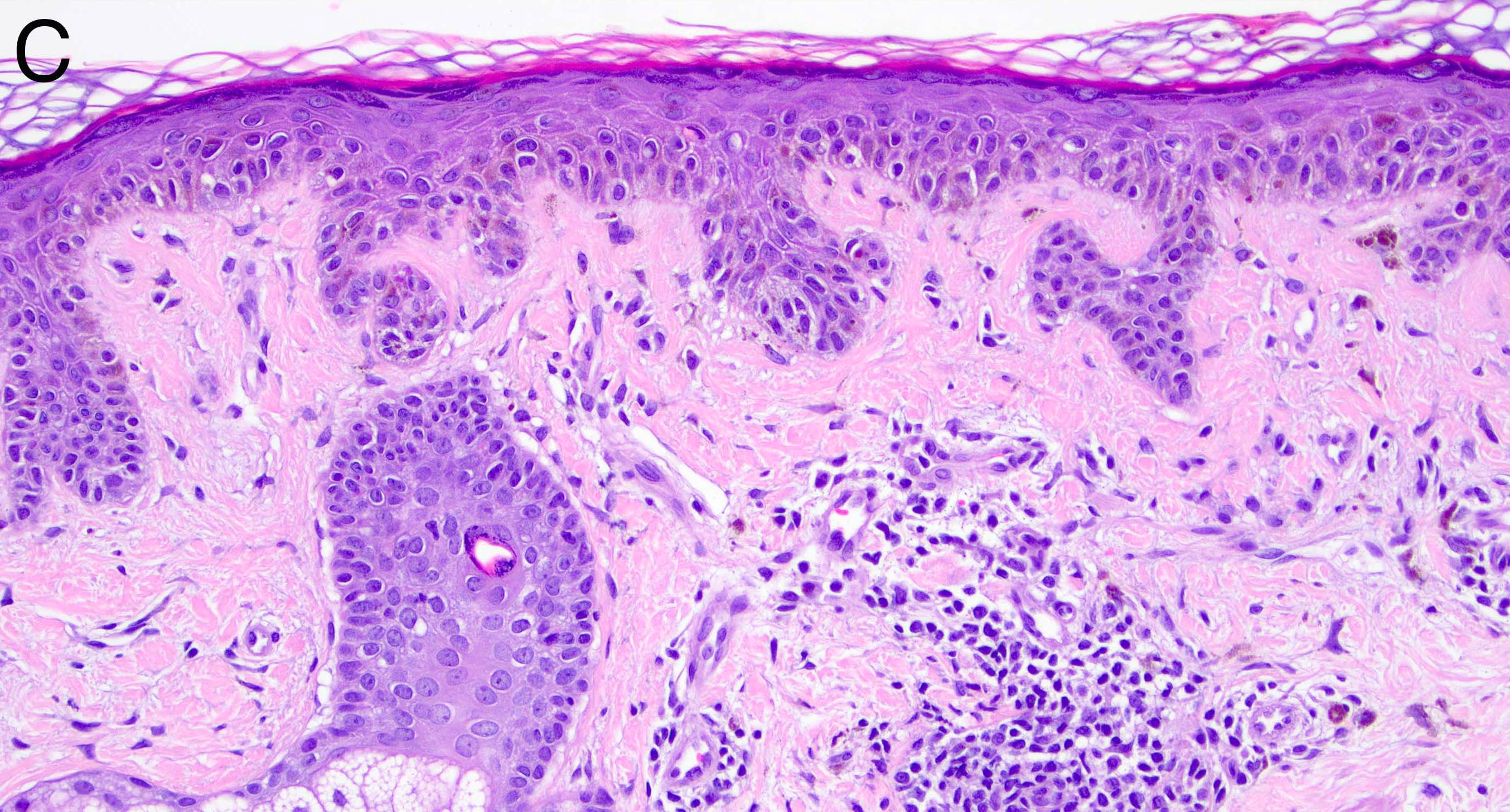
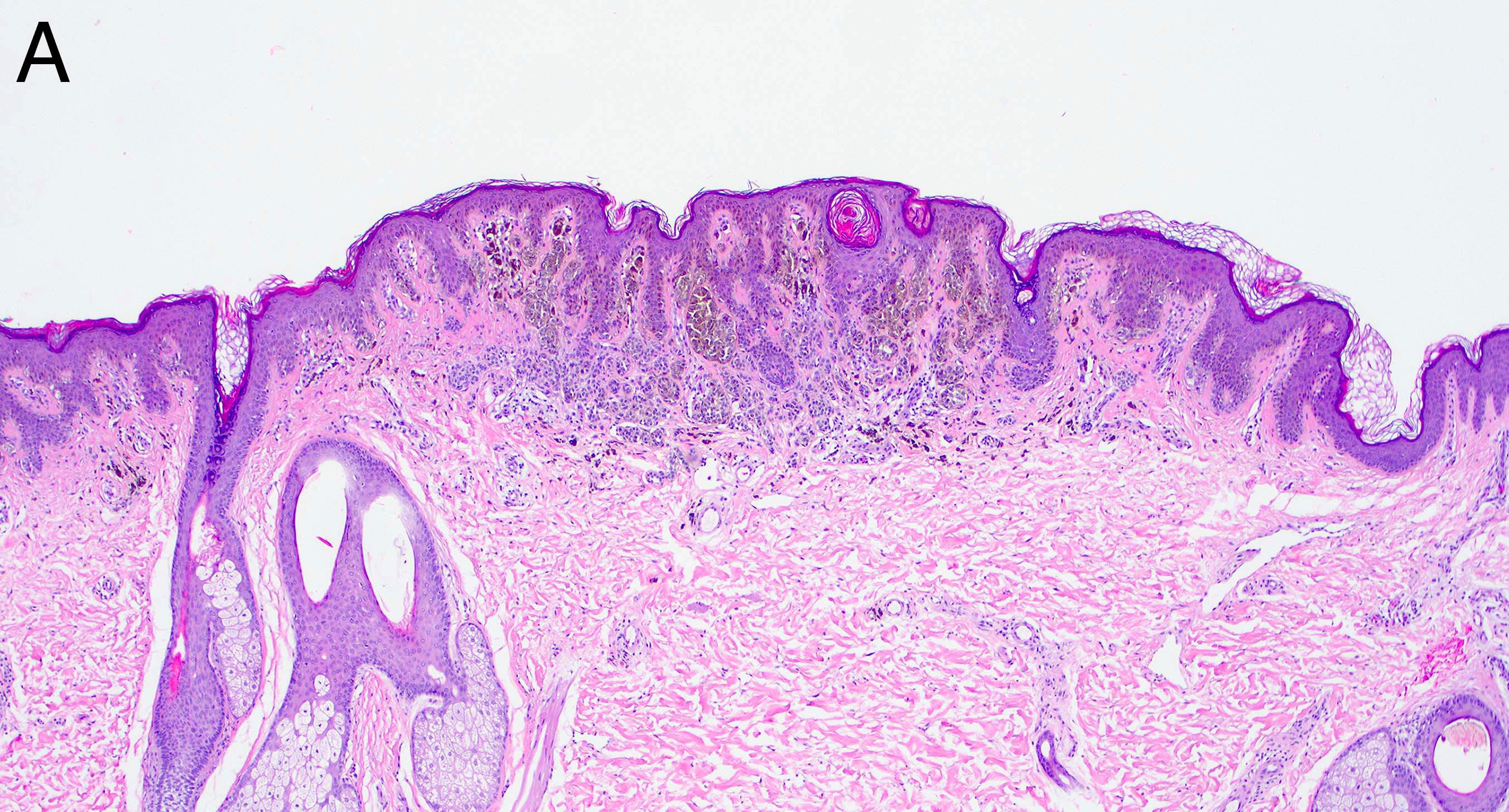
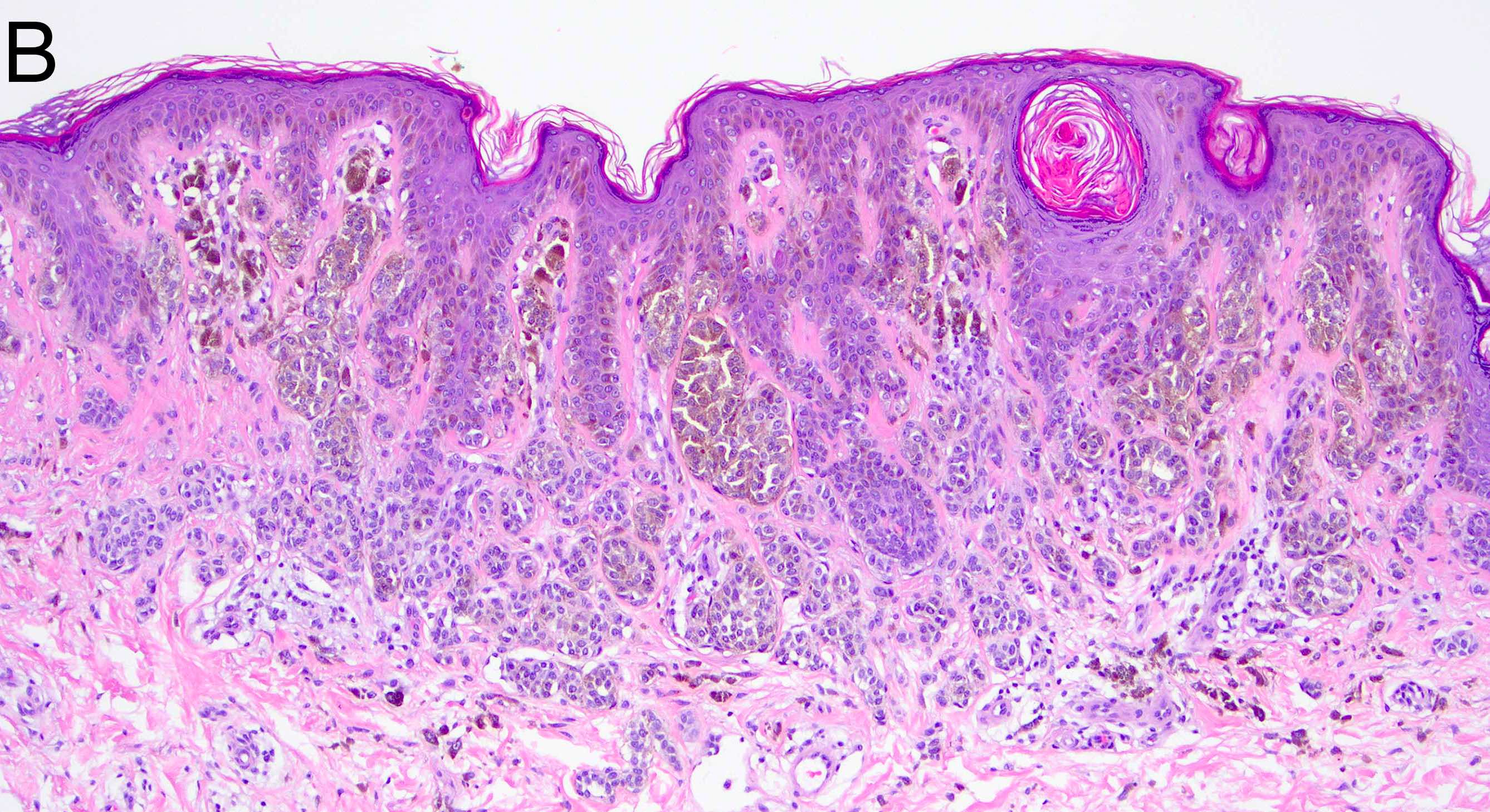
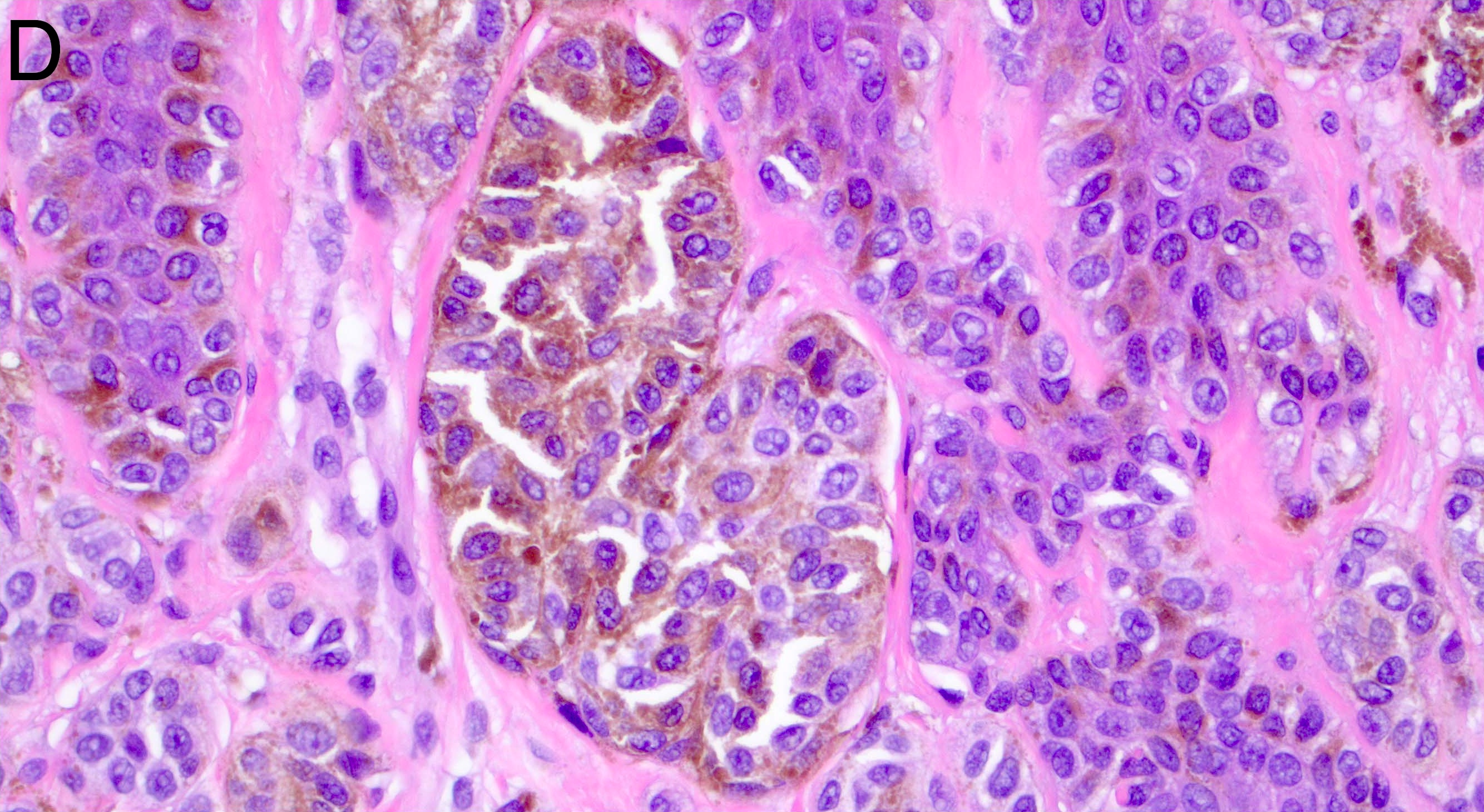
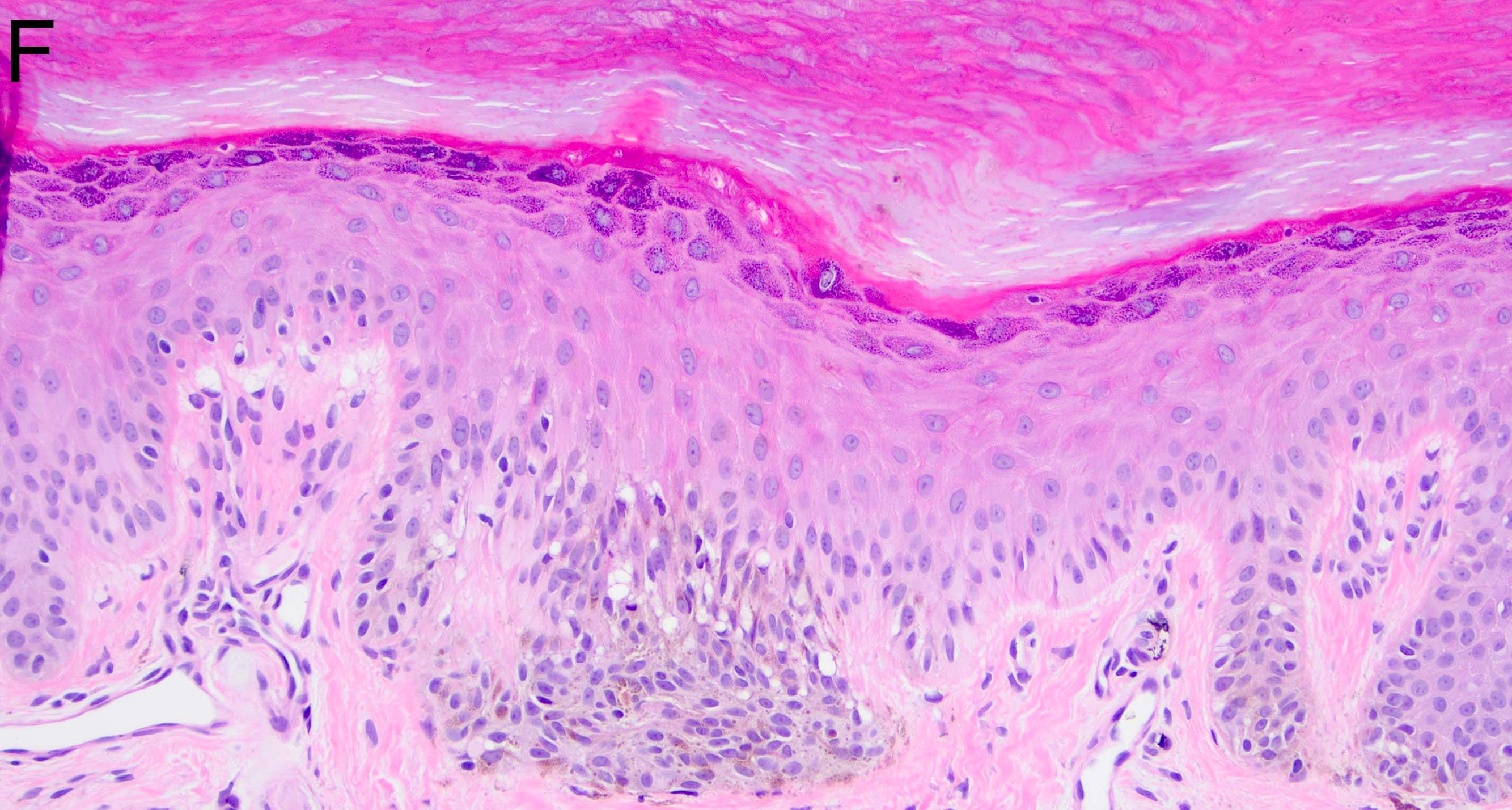
- Melanocytic nevi of the breast (Am J Dermatopathol 2016;38:867):
- May contain large irregular dyshesive nests in close proximity to one another
- Junctional nests may not be centered and can be placed within inter-rete spaces and along sides of rete
- Nests may have variable pigmentation (results in globules seen on dermoscopic exam)
- Nests may have prominent horizontal streaming resulting in rete blunting or epidermal effacement
- Cytologic atypia is common
- Maturation with melanocyte descent should be retained
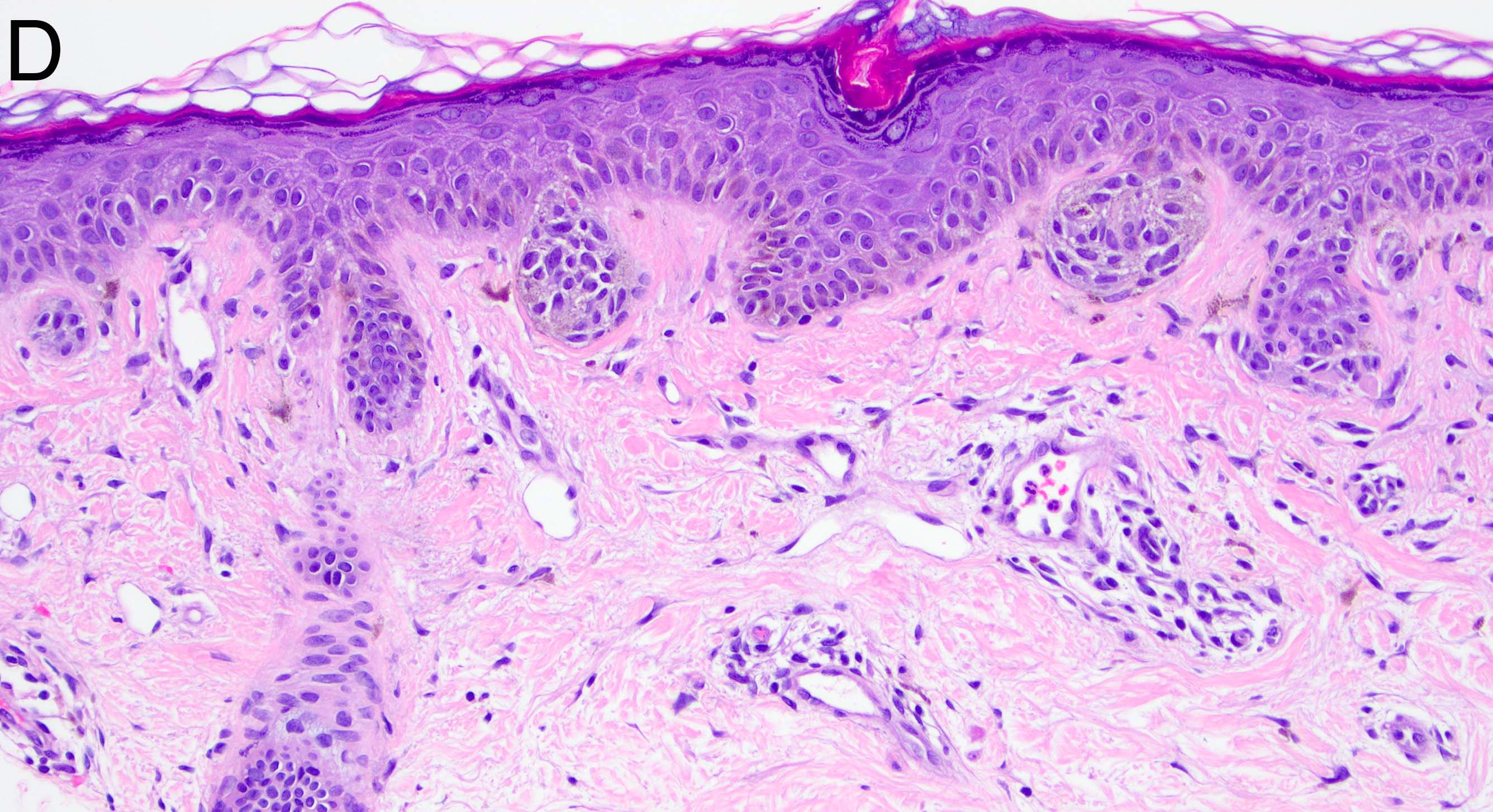
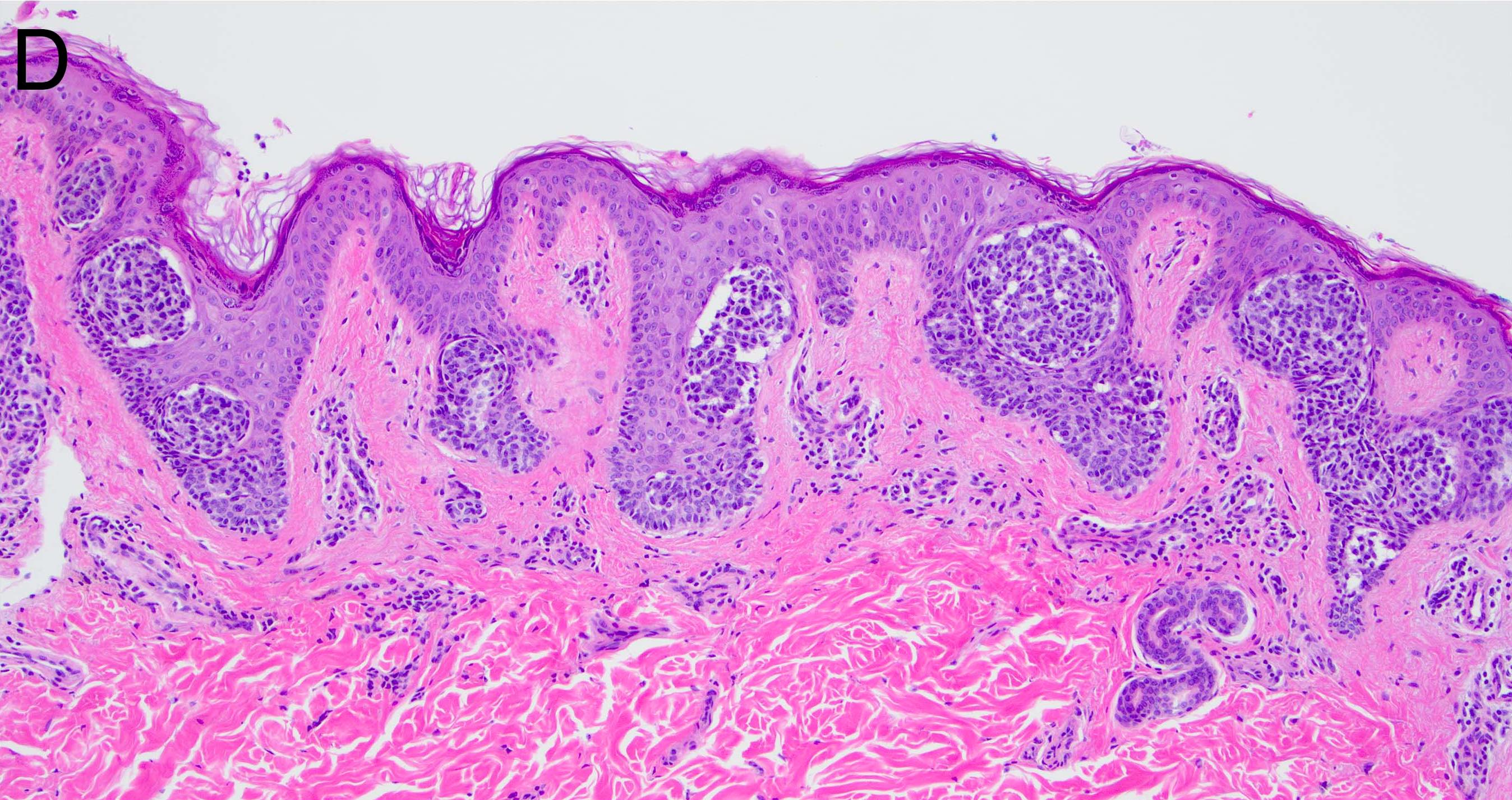
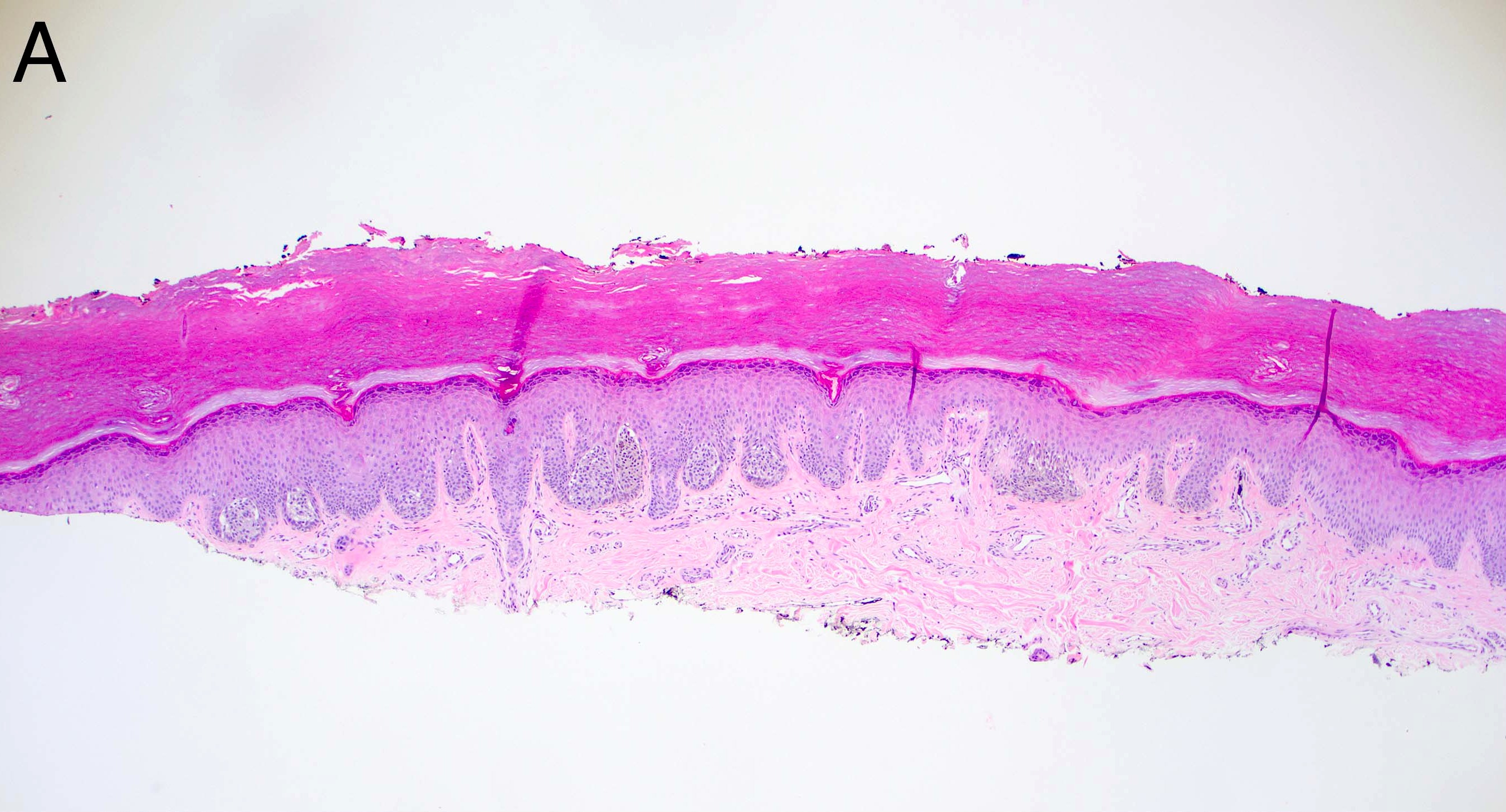
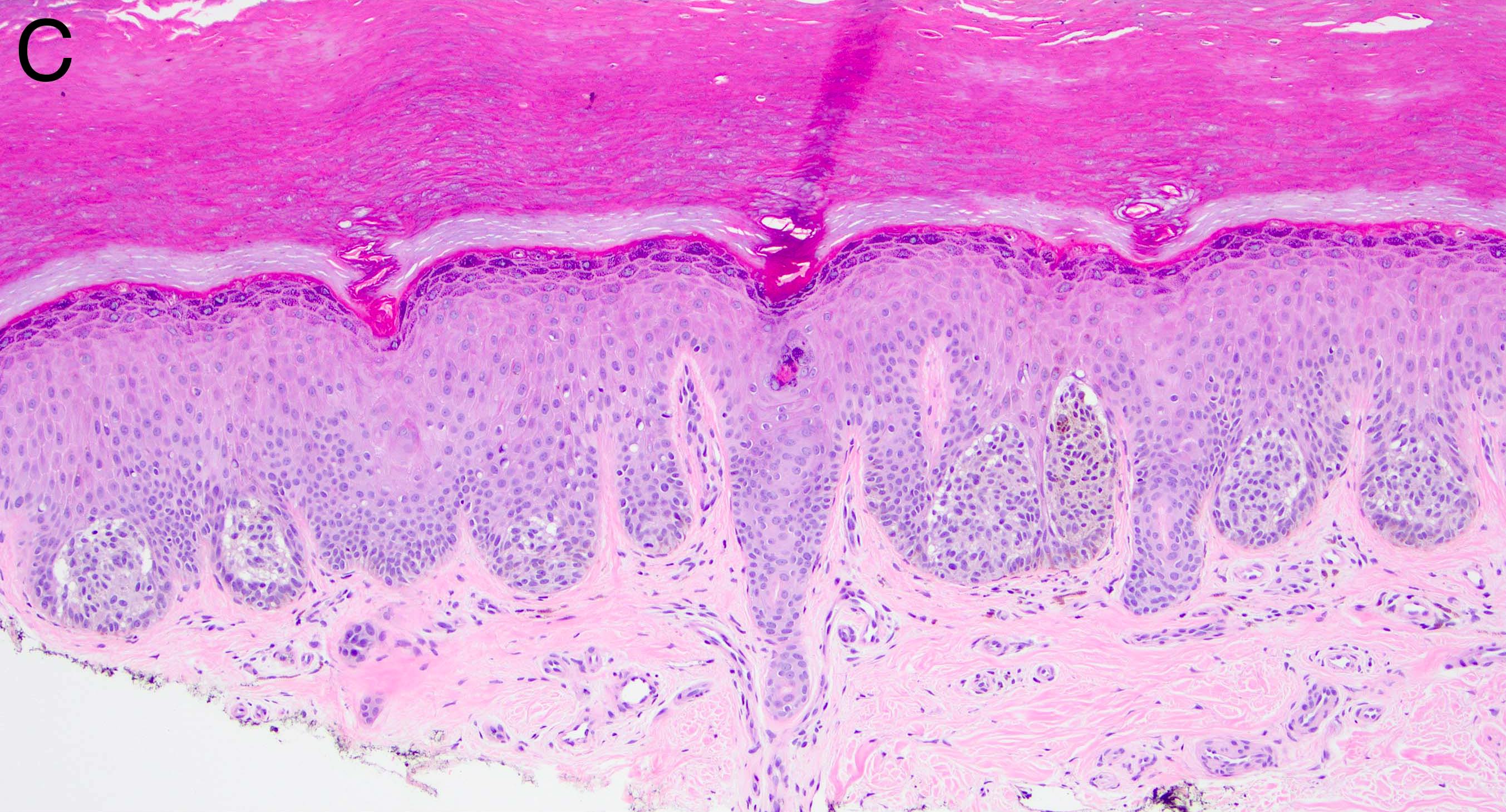
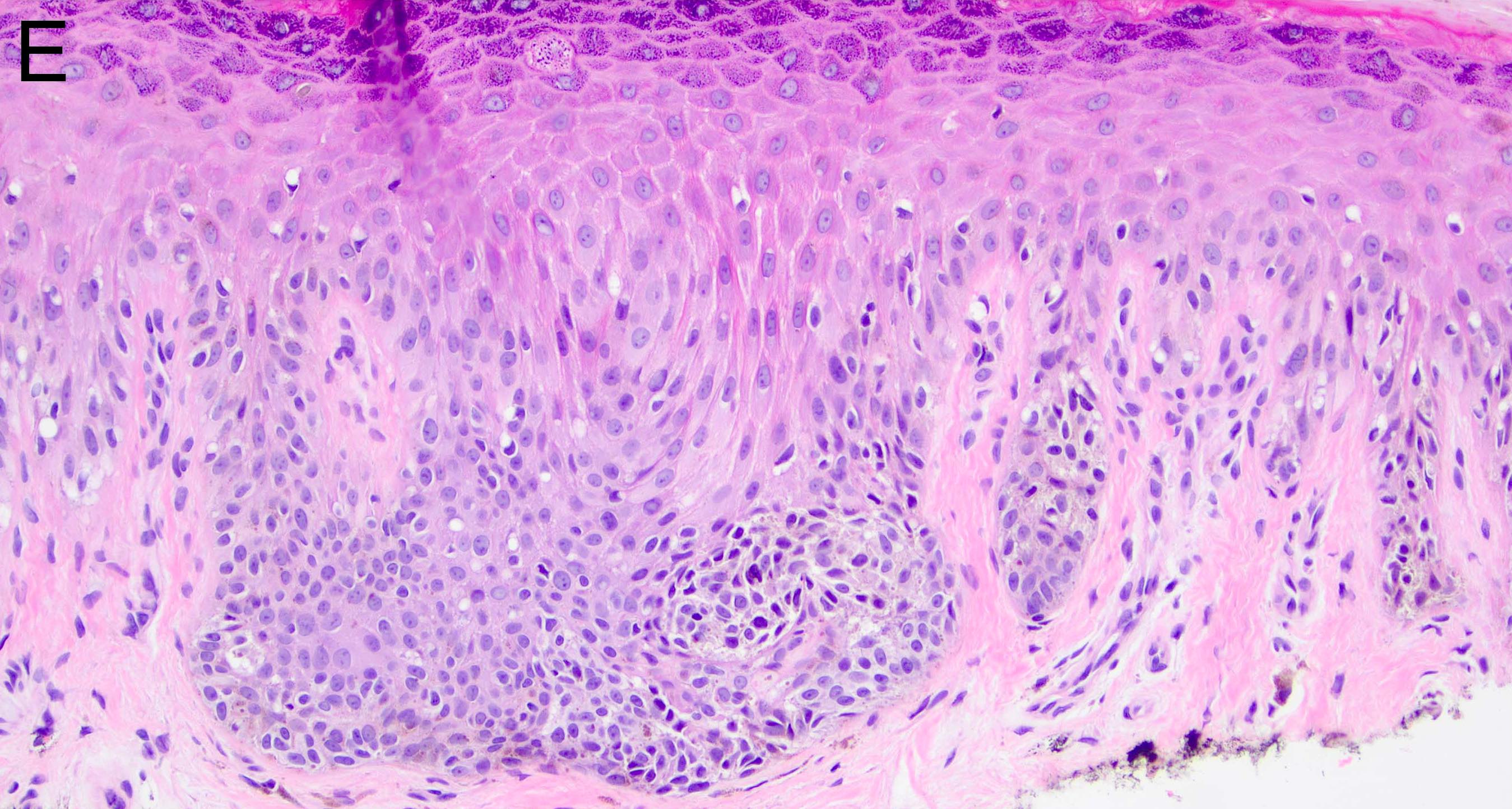
- Melanocytic nevi of the scalp (Am J Dermatopathol 2016;38:867):
- Melanocytes can be enlarged with irregular nuclei but atypia should be uniform throughout the nevus
- May contain large irregular nests in close proximity to one another
- Lentiginous growth may be prominent
- Pagetoid spread is a common feature
- Lesion can have broad junctional involvement and involve adnexa
- Single cell dispersion can be seen at lateral edges
- Lateral circumscription and maturation should be maintained, however symmetry may be lost (Am J Dermatopathol 2016;38:867)
- Prominent stromal fibrotic response can be seen
- Melanocytic nevi of the umbilicus (Histopathology 2015;66:363):
- May have large variability in the size of junctional nests with a dyshesive pattern
- Junctional nests may not be centered and can be placed within inter-rete spaces and along sides of rete
- May have lamellar fibrosis that is confluent and extends into the reticular dermis, entrapping dermal melanocytes
- Maturation of entrapped cells may be impaired, however surrounding unentrapped melanocytes should continue to mature normally
- Shouldering, bridging and lentiginous growth pattern are common
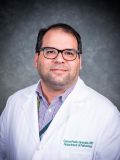
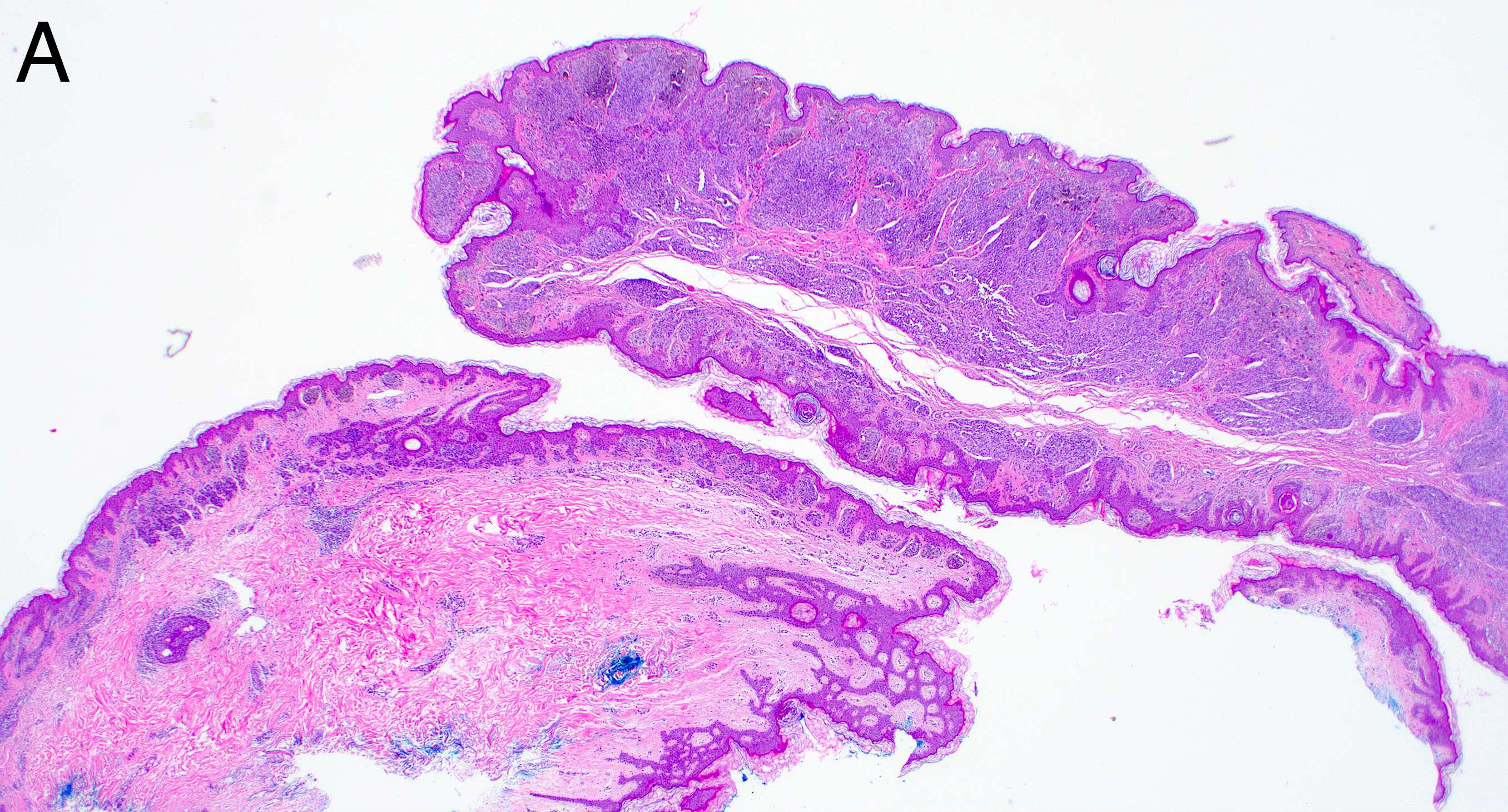
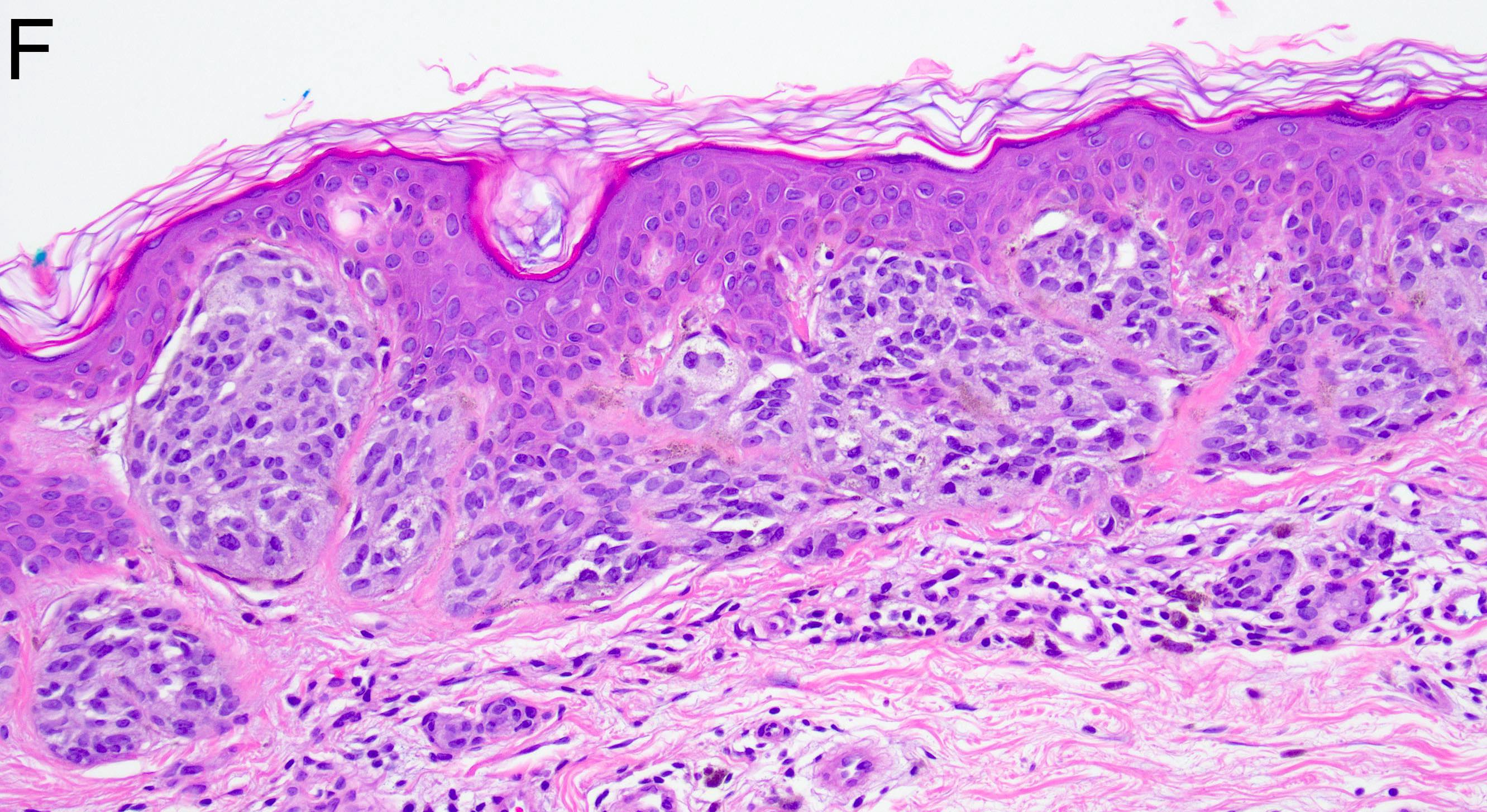
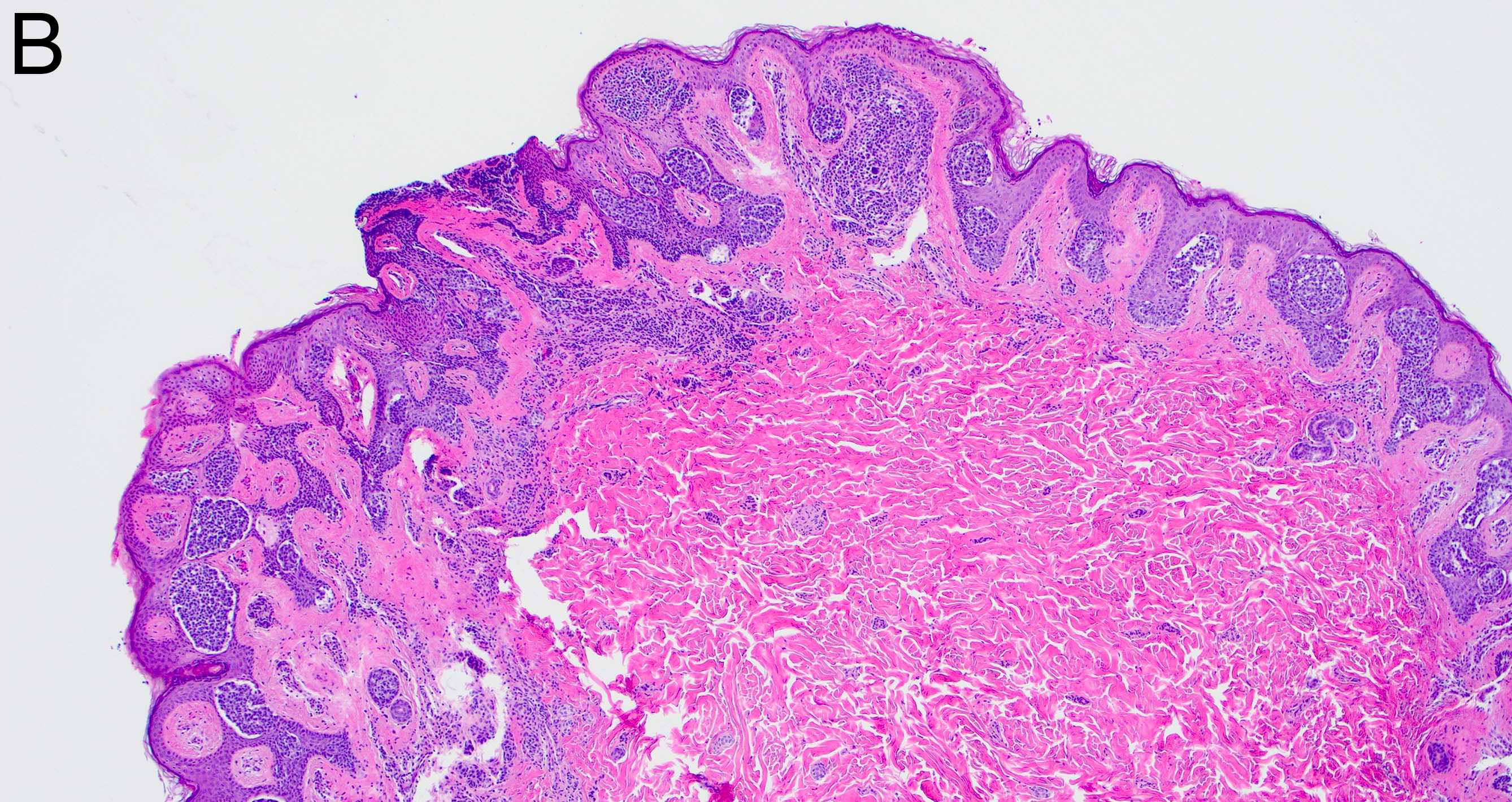
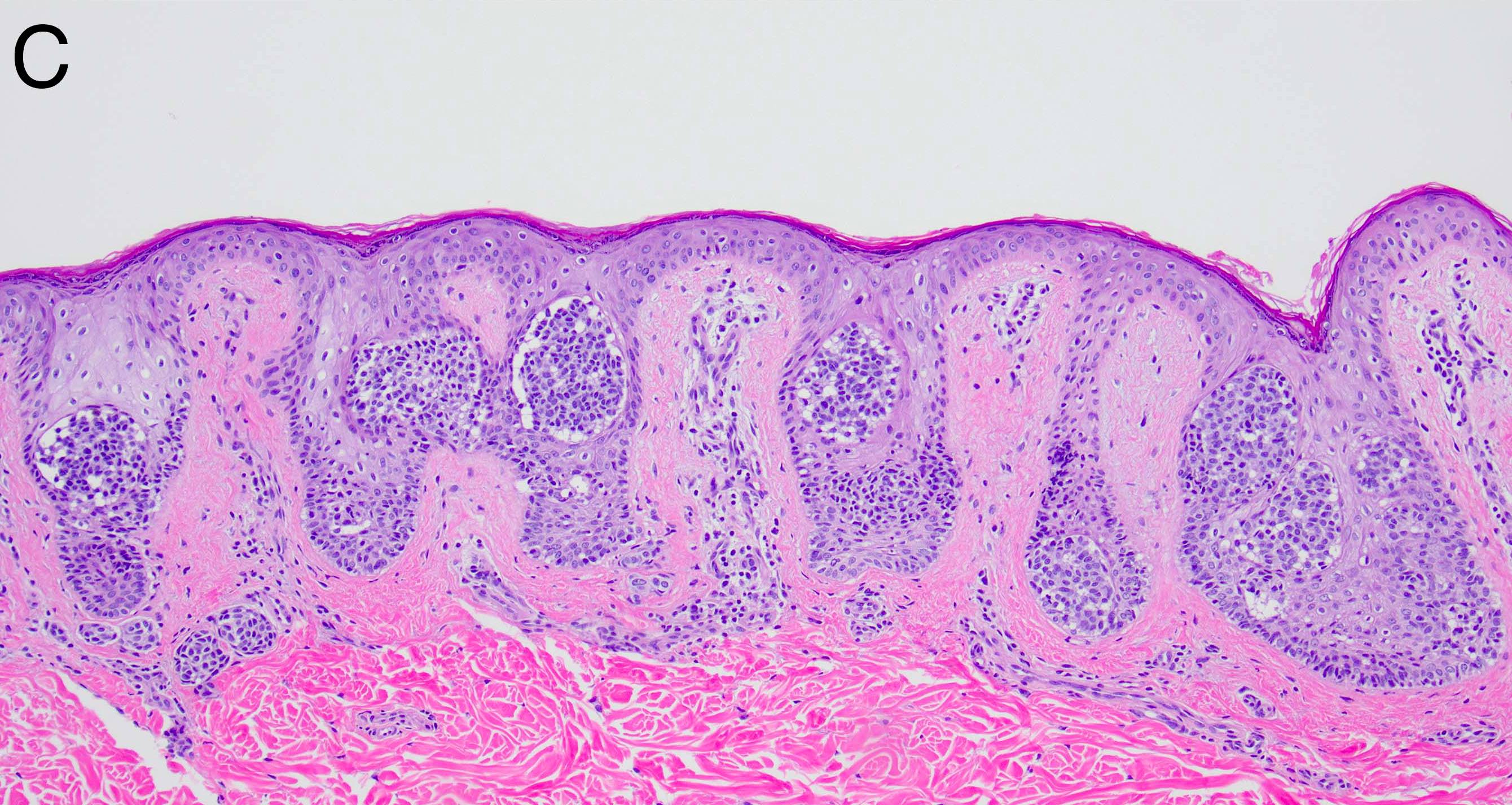
Microscopic (histologic) images
Molecular / cytogenetics description
- Driver mutations in MAPK signaling pathway involving either BRAF V600E or NRAS Q61R / Q61L (J Invest Dermatol 2019;139:1762)
Sample pathology report
- Skin, left breast, biopsy:
- Compound melanocytic nevus with architectural disorder consistent with nevus of special site (see comment)
- Vulva, biopsy:
- Compound melanocytic nevus with features of nevi of special sites, present at peripheral tissue edge (see comment)
- Comment: Histologic sections show a junctional / compound melanocytic proliferation with a junctional component exhibiting architectural disorder in the form of irregularly placed nests containing dyshesive pigmented melanocytes. These features have been associated with melanocytic nevi arising from so called special sites, which include the ear, milk line and genital areas, among others.
Differential diagnosis
- Melanoma:
- May have atypical mitotic figures
- May have marked atypia
- Poor symmetry
- See Diagrams / tables
- Dysplastic nevus:
- Large overlap in histopathologic features with special site nevi
- Poor maturation and occurrence at nonspecial site location
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of these features may be seen in melanoma but should not be observed in nevi from special sites?
- Deep and atypical mitoses
- Effacement of rete ridges
- Lentiginous growth
- Pagetoid spread
Board review style answer #2