Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Rohr BR. Nodular melanoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticnodularmelanoma.html. Accessed March 31st, 2025.
Definition / general
- Nodular melanoma (NM) is an aggressive histologic subtype of invasive malignant melanoma; it accounts for 16 - 25.6% of primary cutaneous melanomas (Br J Dermatol 2021;185:700)
Essential features
- Nodular melanoma is a rapidly growing, aggressive form of malignant melanoma due to early vertical growth phase
- Nodular melanoma mutations overlap with other melanoma subtypes (both low and high cumulative sun damage)
- Tumor (Breslow) depth is the most important prognostic indicator
ICD coding
- ICD-10: C43.9 - malignant melanoma of skin, unspecified
Epidemiology
- Most common in light skinned adults with history of intermittent or chronic sun damage
Sites
- Head, neck and back in men (Ital J Dermatol Venerol 2021;156:300)
- Legs in women (Ital J Dermatol Venerol 2021;156:300)
Pathophysiology
- Mutation patterns overlap with other melanoma subtypes
- Low cumulative sun damage (LCSD) melanoma (Ital J Dermatol Venerol 2021;156:300)
- Chromosomal abnormalities
- Loss of 9, 10, 6q, 20
- Gains 1q, 6p, 7, 8q, 17q, 20q
- BRAF mutations
- V600E most common
- Activate the MAPK pathway
- More common in patients < 40 years old
- Others V600K, K601E
- V600E most common
- NRAS mutations
- More common in older patients
- Higher frequency compared to superficial spreading melanoma (SSM)
- TERT promoter mutations or amplifications
- Homozygous deletion or mutation in CDKN2A
- PTEN deletions or mutations
- TP53 mutations
- Chromosomal abnormalities
- High cumulative sun damage (HCSD) melanoma (Ital J Dermatol Venerol 2021;156:300)
- Less frequent BRAF mutations versus LCSD
- BRAF V600K most common
- Inactivations in NF1 (30%)
- Copy number increase of CCND1 (20%)
- Activating mutations KIT (~10%)
- TP53 mutations
- ARID2 mutations
- Chromosomal aberrations
- TERT promoter mutations
- Less frequent BRAF mutations versus LCSD
- Lower prevalence of mutated genes compared to SSM
- NOTCH4, RPS6KA6, BCL2L12, ERBB3, TERT, SNX31, SSPO, ZNF560
Etiology
- Variable pathways (Ital J Dermatol Venerol 2021;156:300)
- Low or high cumulative sun damage (CSD)
- Genetic mutations (see Pathophysiology)
Clinical features
- Pigmented or nonpigmented (pink) papule or nodule with rapid growth
- Frequently ulcerated
- May lack classic ABCDE clinical signs to raise suspicion for melanoma
- ABCDE: asymmetry, border irregularity, color variation, diameter > 6 mm, other evolution history
- Dermoscopy features (DermNet: Dermoscopy of melanoma [Accessed 16 March 2023])
- Isolated globules
- Blue-gray veil
- White streaks
- Irregular linear or dotted vessels
- Multiple colors (2 - 3)
Diagnosis
- Scoop shave biopsy or excisional biopsy preferred
- Histopathologic diagnosis is gold standard
- Sentinel lymph node biopsy
- For primary tumors with Breslow depth 0.8 mm or deeper
- Breslow depth: measured from the top of the granular layer or base of ulceration to the deepest invasive melanoma cell
Prognostic factors
- Adverse prognosis indicators (Ital J Dermatol Venerol 2021;156:300)
- Thicker (Breslow) depth - most important
- + Ulceration
- Dermal mitoses
- Deeper anatomic (Clark) level of invasion (I - V)
- + Lymphovascular invasion
- + Neurotropism
- Increased risk of local recurrence
- + Sentinel lymph node biopsy
- Positive excision margins
- Report proximity of melanoma in situ (MIS) or invasive malignant melanoma (MM) to excision margins when able
Case reports
- Newborn girl with giant congenital primary nodular melanoma in utero (BMC Pediatr 2021;21:121)
- 33 year old woman with amelanotic nodular melanoma on the vulva (BMC Womens Health 2021;21:289)
- 42 year old woman with amelanotic nodular melanoma appearance within superficial spreading melanoma (J Cosmet Dermatol 2022;21:3949)
- 63 year old African American woman with nodular melanoma on the forearm (Eplasty 2019;19:e10)
- 69 year old man with dyspnea associated with a large nodular melanoma (Cureus 2021;13:e16819)
Treatment
- Treatment includes excision with or without sentinel lymph node biopsy; additional treatment based on stage (NIH: Melanoma Treatment (PDQ®) - Health Professional Version [Accessed 16 March 2023])
- Wide local excision 1 - 2 cm
- Sentinel lymph node biopsy for stage pT1b or higher
- Targeted or immunotherapy / checkpoint inhibitors
- Targeted therapies include BRAF and MEK inhibitors
- Talimogene laherparepvec (T VEC) injections
- Interleukin 2
- Chemotherapy
- Radiation therapy
- Regular skin examination with a dermatologist
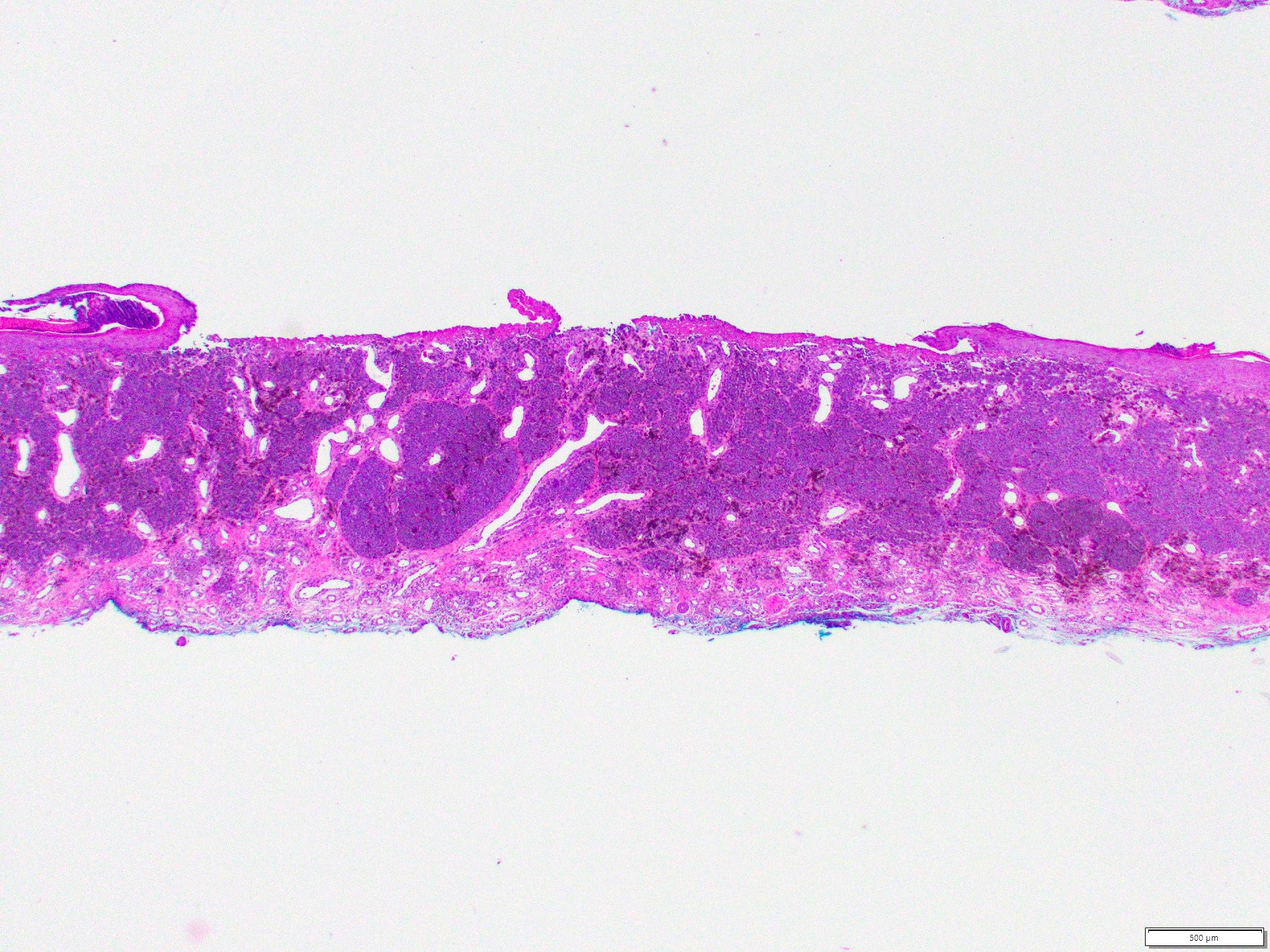
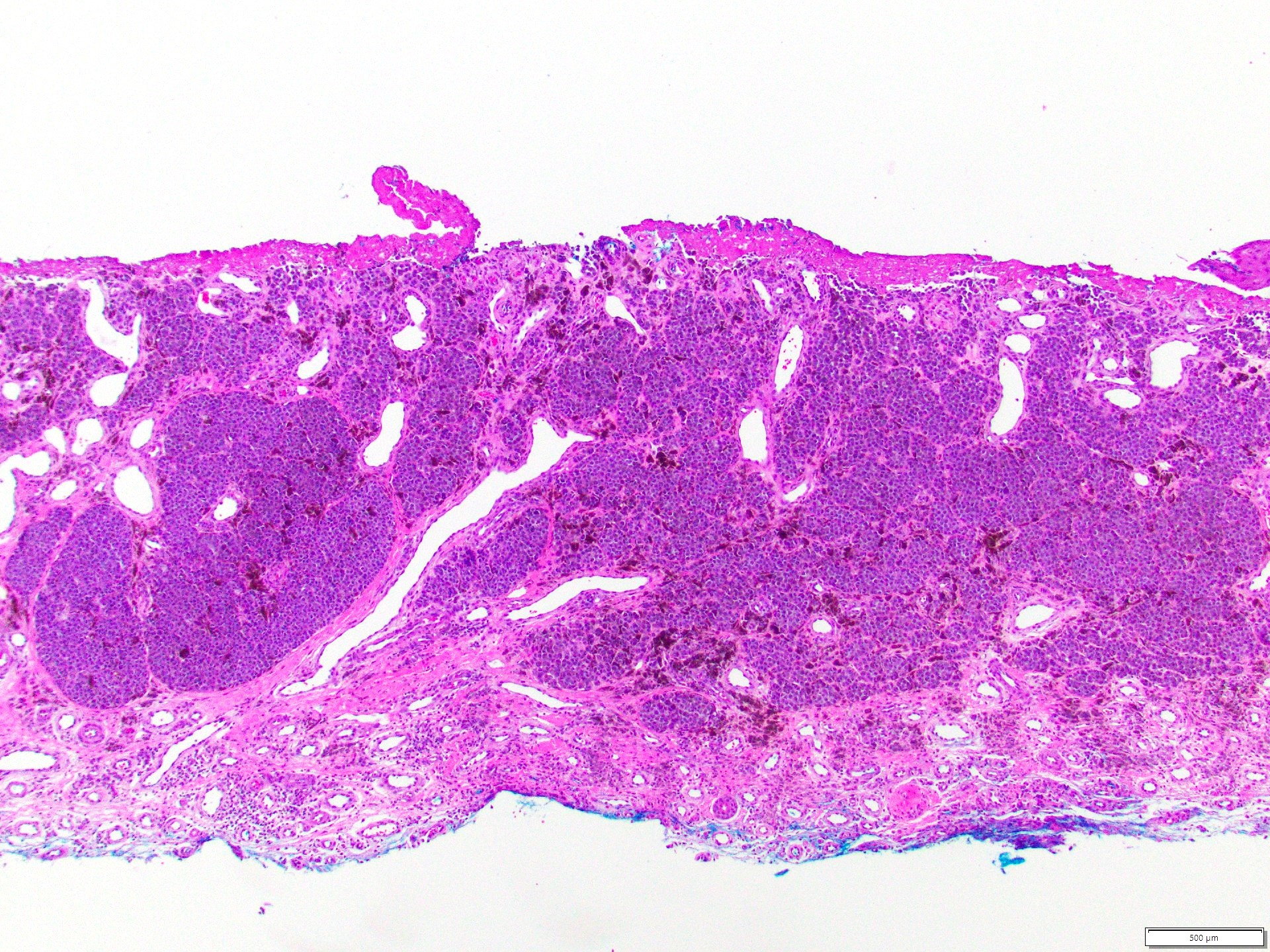
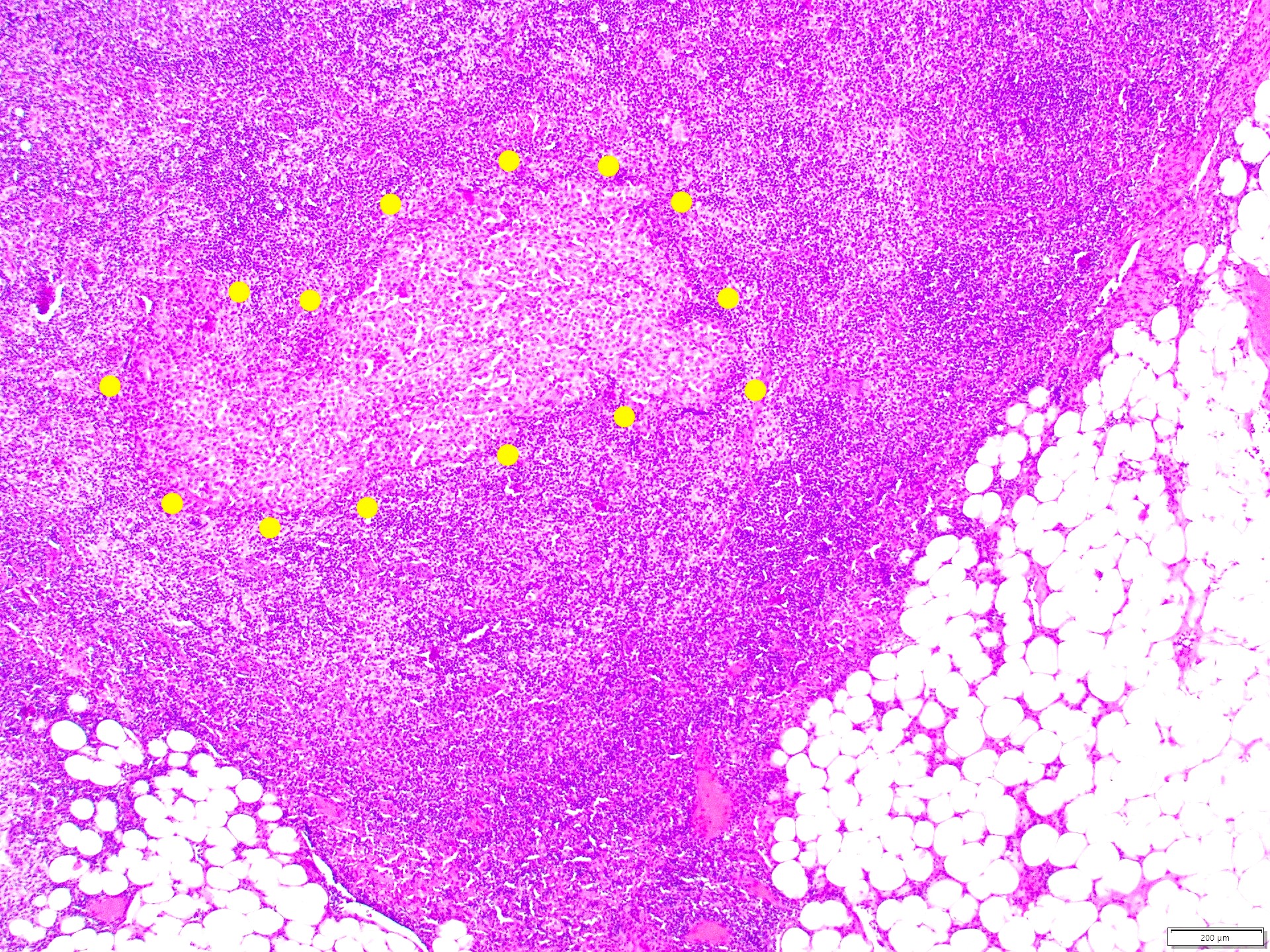
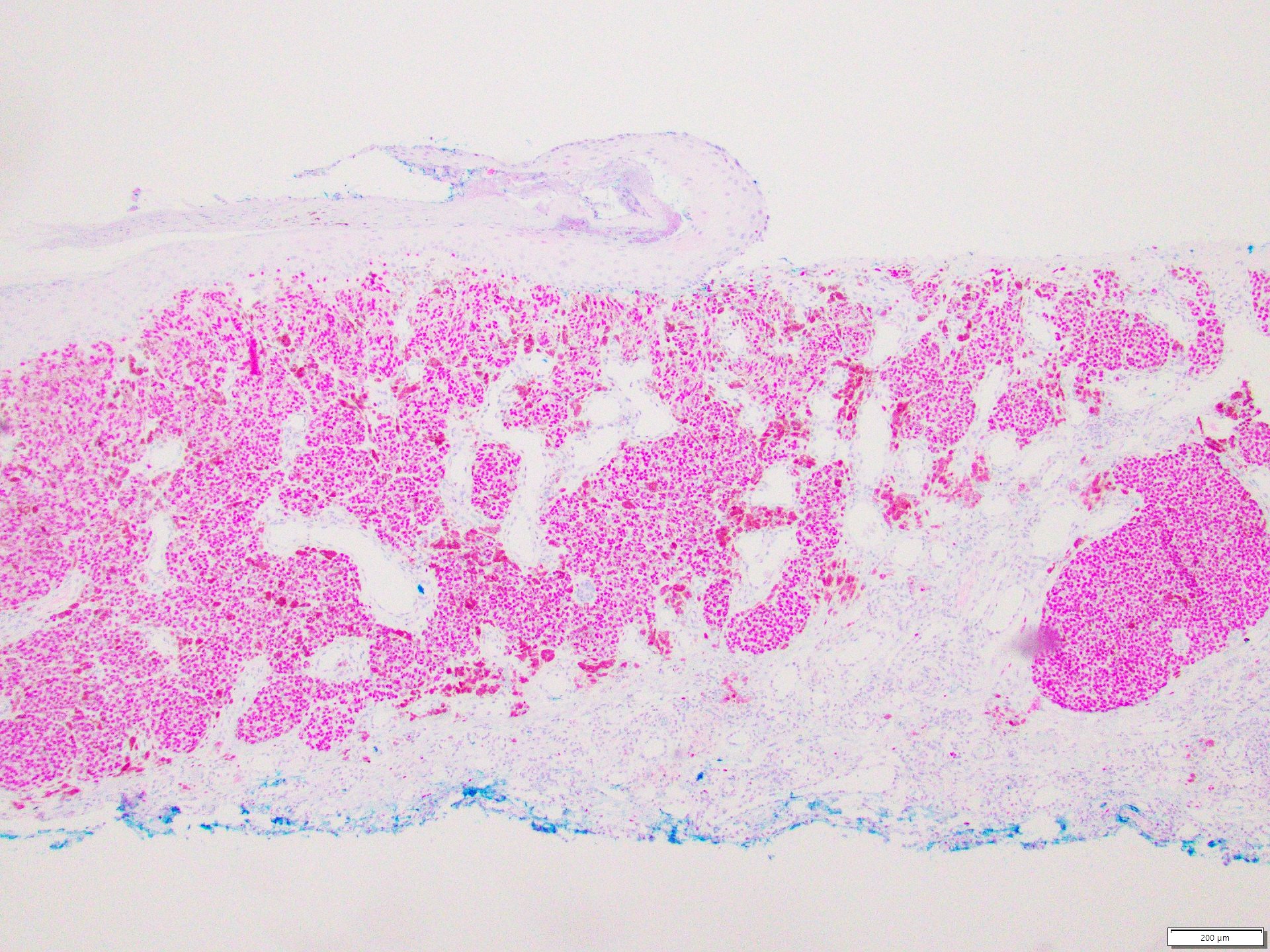
Microscopic (histologic) description
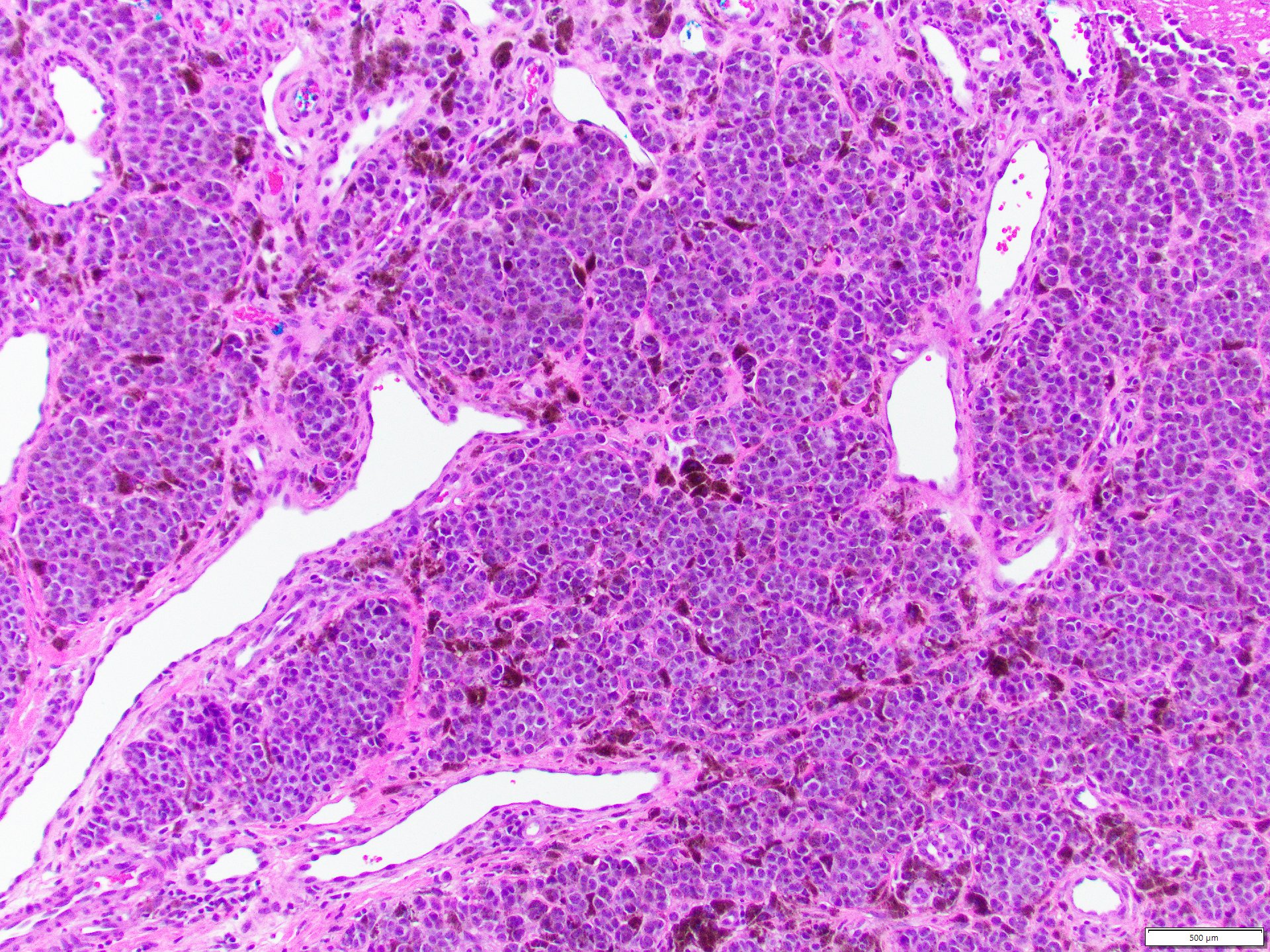
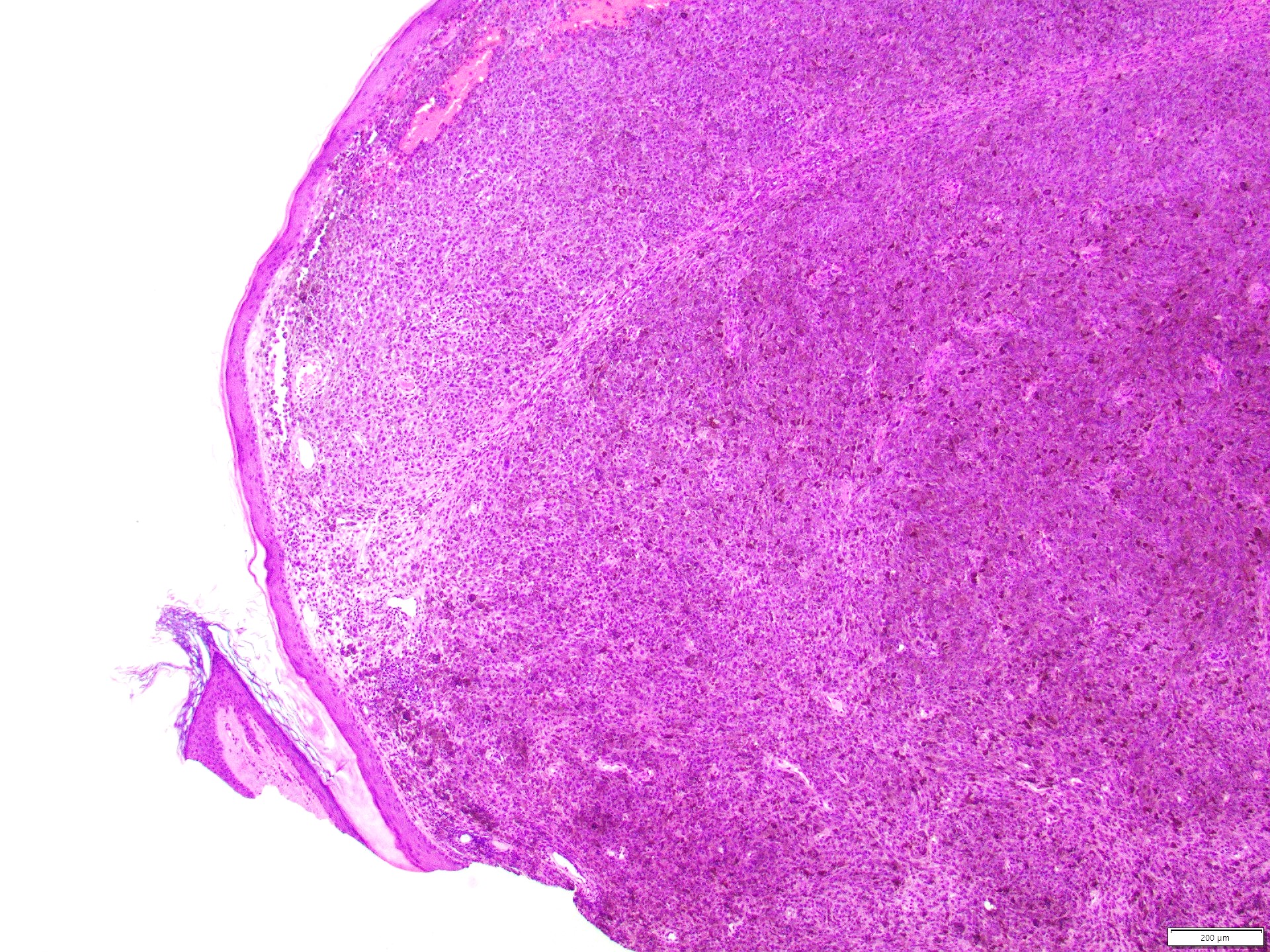
- Atypical nests and sheets of mitotically active dermal melanocytes with limited overlying junctional component
- No radial growth phase
- No intraepidermal melanocytic proliferation beyond 3 epidermal ridges on either side of the tumor mass (Ital J Dermatol Venerol 2021;156:300)
- With or without melanin pigment
- Frequent features (Arch Pathol Lab Med 2020;144:500, Ital J Dermatol Venerol 2021;156:300)
- Polypoid / exophytic profile
- Brisk tumor infiltrating plasma cells (TIPs)
- Tumor size > 10 mm
- Ulceration
- Epidermal collarettes
- High mitotic rate
- Necrosis
- Multiple phenotypes
- Epithelioid with vesicular nuclei
- Abundant cytoplasm
- Possible spindled phenotype
- Pleomorphism and lichenoid inflammation
- Pathologic stage classification AJCC guidelines, 8th edition (2018) (Ital J Dermatol Venerol 2021;156:300)
- Tumor (Breslow) depth is strongest predictor of clinical outcome, used for staging
- Measure vertically from top of granular layer of the epidermis to the deepest invasive melanoma cells
- If ulcerated, measure from base of ulcer
- Round to nearest 0.1 mm using ocular micrometer
- Avoid measuring vascular invasion, microsatellites, involvement of skin appendages
- Tumor (Breslow) depth is strongest predictor of clinical outcome, used for staging
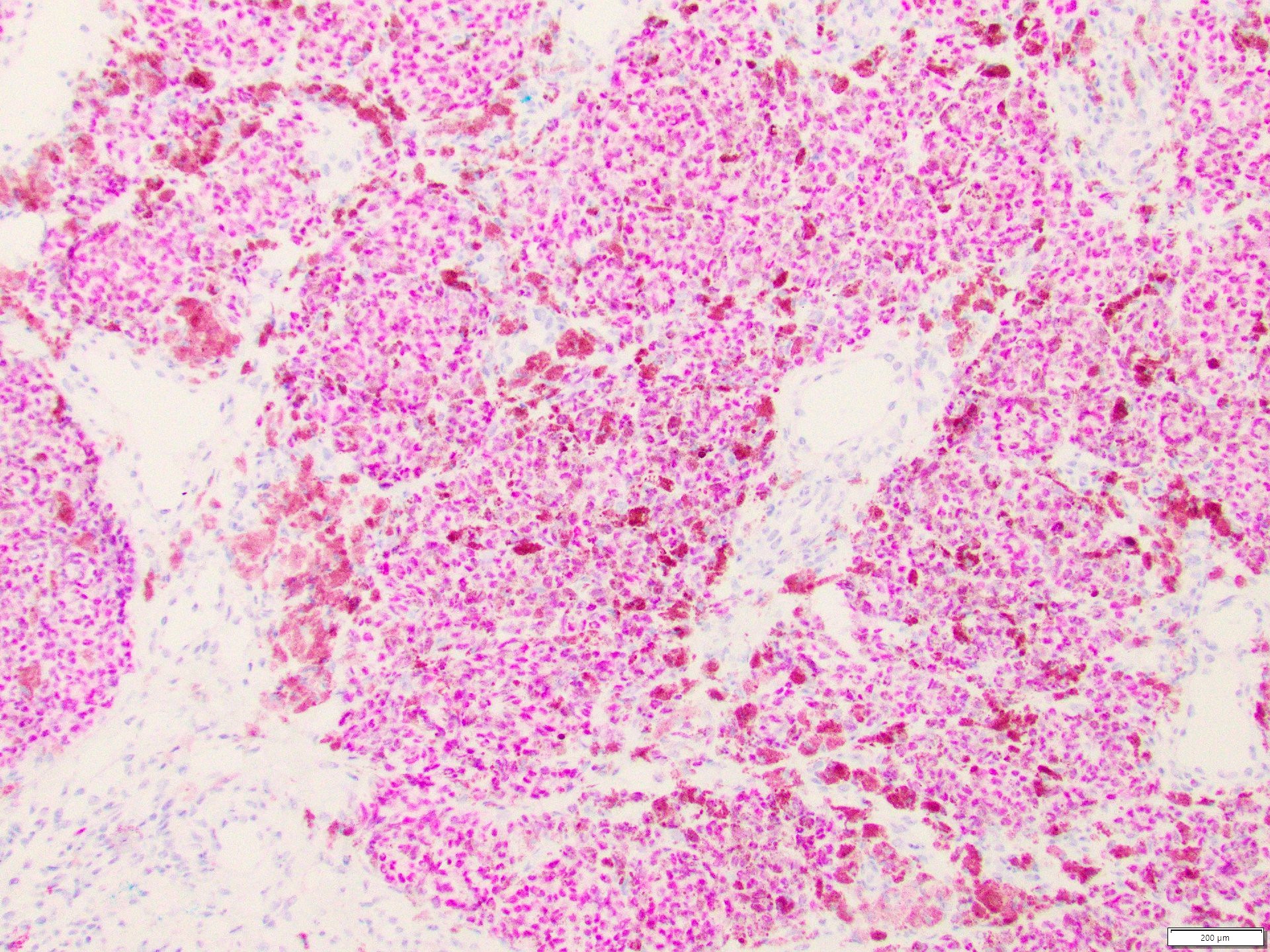
Microscopic (histologic) images
Positive stains
- SOX10 (nuclear)
- MelanA / MART1 (cytoplasmic)
- PRAME
- HMB45
- S100
- MITF
- Tyrosinase
- BRAF variable
- Reference: Semin Diagn Pathol 2022;39:239
Negative stains
- Loss of melanocytic markers possible (Dermatopathology (Basel) 2021;8:359)
- Keratin immuostains
- Cytokeratin, AE1 / AE3, OSCAR, CAM5.2
- Rare aberrant expression in melanoma (Dermatopathology (Basel) 2021;8:359)
- Neuroendocrine markers
- Neurofilament, GFAP, synaptophysin, chromogranin, CD56
- Rare aberrant expression in melanoma (Dermatopathology (Basel) 2021;8:359)
- Muscle specific markers
- Macrophage markers
- CD68, CD163
- Rare aberrant expression in melanoma (Dermatopathology (Basel) 2021;8:359)
- Vascular markers
- CD31, CD34
- Rare aberrant expression in melanoma (Dermatopathology (Basel) 2021;8:359)
- Hematopoietic markers
- CD4, CD20
- Rare aberrant expression in melanoma (Dermatopathology (Basel) 2021;8:359)
- Miscellaneous
- FLI1, GATA3, CEA, calretinin, PAX8, PAX2
- Rare aberrant expression in melanoma (Dermatopathology (Basel) 2021;8:359)
Videos
Melanocytic dermpath basics: melanoma, by Dr. Jared Gardner
Sample pathology report
- Skin, biopsy:
- Invasive malignant melanoma, nodular subtype, extending to a Breslow depth of ## (see comment)
- Comment: The sections reveal a predominantly dermal proliferation of sheets and large nests of atypical melanocytes that fail to mature with descent. See melanoma synoptic summary for additional features.
Differential diagnosis
- Superficial spreading melanoma:
- Low cumulative sun damage
- Radial growth phase
- Lentigo maligna melanoma:
- High cumulative sun damage
- Radial growth phase
- More common on chronically sun exposed sites of elderly, light skinned adults
- Acral lentiginous melanoma:
- Acral sites
- Not related to cumulative sun damage
- Nevoid melanoma (Ital J Dermatol Venerol 2021;156:300):
- Resembles intradermal nevus, 2 types
- Papillomatous type:
- NRAS mutation most common
- Head, neck, limbs
- Puffy shirt appearance
- Scanning magnification shows dense cellular aggregates surrounded by bent elongated rete ridges lined up side by side
- Maturing nevoid type: limbs, trunk
- Heterogeneous mutations: BRAF, NRAS
- Cutaneous involvement of metastatic malignant melanoma:
- History of prior locoregional invasive melanoma
- Features to favor metastases (Arch Pathol Lab Med 2020;144:500)
- Tumor size < 2 mm
- Absence of tumor infiltrating lymphocytes and plasma cells
- Monomorphism
- Involvement of adnexal epithelium
- Primary dermal melanoma:
- Generally exclude primary dermal in presence of ulceration, precursor melanocytic nevus and any junctional component
- May be impossible to distinguish from nodular melanoma
Additional references
Board review style question #1
Board review style answer #1
B. Granular layer. Breslow depth is measured from the top of the granular layer to the deepest invasive melanoma cell. If there is an ulceration, then Breslow depth is measured from the base of the ulceration.
Comment Here
Reference: Nodular melanoma
Comment Here
Reference: Nodular melanoma
Board review style question #2
What is the key prognostic indicator for primary cutaneous melanoma?
- Clark level
- Dermal mitoses
- Tumor (Breslow) depth
- Ulceration
Board review style answer #2
C. Tumor (Breslow) depth. Breslow depth is the most important prognostic indicator when looking at primary tumor information.
Comment Here
Reference: Nodular melanoma
Comment Here
Reference: Nodular melanoma
Board review style question #3
In a cutaneous nodular melanoma presenting on sites with low cumulative sun damage, which BRAF mutation is most common?
- BRAF K601E
- BRAF V600D
- BRAF V600E
- BRAF V600K
- BRAF V600R
Board review style answer #3
C. BRAF V600E. The other BRAF mutations may also be seen in melanoma; however, BRAF V600E is the most common of these in nodular melanomas on low cumulative sun damage sites. On high cumulative sun damage sites, BRAF V600K is most common of the BRAF mutations.
Comment Here
Reference: Nodular melanoma
Comment Here
Reference: Nodular melanoma