Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chughtai A, Anjum S. Congenital nevus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticmelanomacongenital.html. Accessed April 2nd, 2025.
Definition / general
- Nevi that are present at birth or that arise within the first few postnatal weeks (StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022])
- Benign lesion comprised of bland melanocytes in dermis
Essential features
- Nevi that are present at birth or shortly thereafter (StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022])
- Characterized by bland melanocytic proliferation in the dermis; melanocytes prominently cluster around dermal appendages and show maturation in the depth
- Excellent prognosis
Terminology
- Congenital melanocytic nevus (CMN) / giant hairy nevus (StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022])
- Large / giant CMN has been described as bathing trunk / vest / shoulder sleeve / stocking / glove nevi, depending on the site
ICD coding
- ICD-10: D22.30 - melanocytic nevi of unspecified part of face
Epidemiology
- M = F
- Found in 1 - 2% of newborns, 0.6 - 1.6% of the population
- Incidence of malignant change has been reported more in females, large nevi and axial lesions
- Lesion over vertebral column can have associations with leptomeningeal melanocytosis, hydrocephalus, spina bifida or meningomyelocele
- Large lesions are commonly associated with neurocutaneous melanosis (3 - 15%), hypertrophy of affected limb and SCALP syndrome
- References: An Bras Dermatol 2017;92:200, StatPearls: Congenital Nevus [Accessed 15 September 2022], StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022], Elder: Lever's Histopathology of the Skin, 11th Edition, 2014, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
Sites
- Trunk and legs, followed by head and neck, feet and hands
- Can be multiple
- Can have satellite lesions with large / giant lesions
Pathophysiology
- Believed to develop due to unregulated growth of melanoblasts during fifth to twenty fourth week of gestation (An Bras Dermatol 2017;92:200)
- Occur as a result of in utero somatic mutations of genes that play a role in the mitogen activated protein kinase (MAPK) pathway (mainly NRAS); this leads to the overproliferation of melanocyte lineage cells and thus the formation of CMNs (StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022], StatPearls: Congenital Nevus [Accessed 15 September 2022])
Etiology
- No known etiology
Clinical features
- Flat or raised lesion, heavily pigmented, hairy
- Based on size classified as:
- Small (< 1.5 cm)
- Medium (1.5 - 20 cm)
- Large (> 20 - 40 cm)
- Giant (> 40 cm) (StatPearls: Congenital Nevus [Accessed 15 September 2022])
- Clinical relevance relies on their association with increased risk of melanoma and central nervous system involvement (neurocutaneous melanosis) (StatPearls: Congenital Nevus [Accessed 15 September 2022])
Diagnosis
- Clinical presentation and histological examination is diagnostic
Laboratory
- Usually not required
Prognostic factors
- Excellent prognosis
- Increased size of the lesion is linked to the increased risk of melanoma (J Am Acad Dermatol 2013;68:441)
Case reports
- Neonate boy presented with a giant congenital melanocytic nevus (Cureus 2021;13:e15210)
- 19 month old boy and 4 year old girl presented with neurocutaneous melanosis in association with large congenital melanocytic nevi (Front Neurol 2019;10:79)
- 2 year old girl presented with giant congenital melanocytic nevus (Indian Dermatol Online J 2020;11:79)
- 12 year old girl presented with giant congenital melanocytic nevus (J Med Case Rep 2018;12:175)
- 16 year old girl presented with oral congenital melanocytic tumor (Head Neck Pathol 2015;9:481)
Treatment
- Surgical excision (StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022])
- Other treatment modalities include laser, radiotherapy, dermabrasion, cryotherapy, electrotherapy and chemical peels (StatPearls: Congenital Melanocytic Nevi [Accessed 15 September 2022])
Clinical images
Contributed by Mark R. Wick, M.D.
Images hosted on other servers:
Gross description
- Flat or slightly raised pigmented lesion usually exhibiting hair (Dermatol Pract Concept 2020;10:e2020068)
Gross images
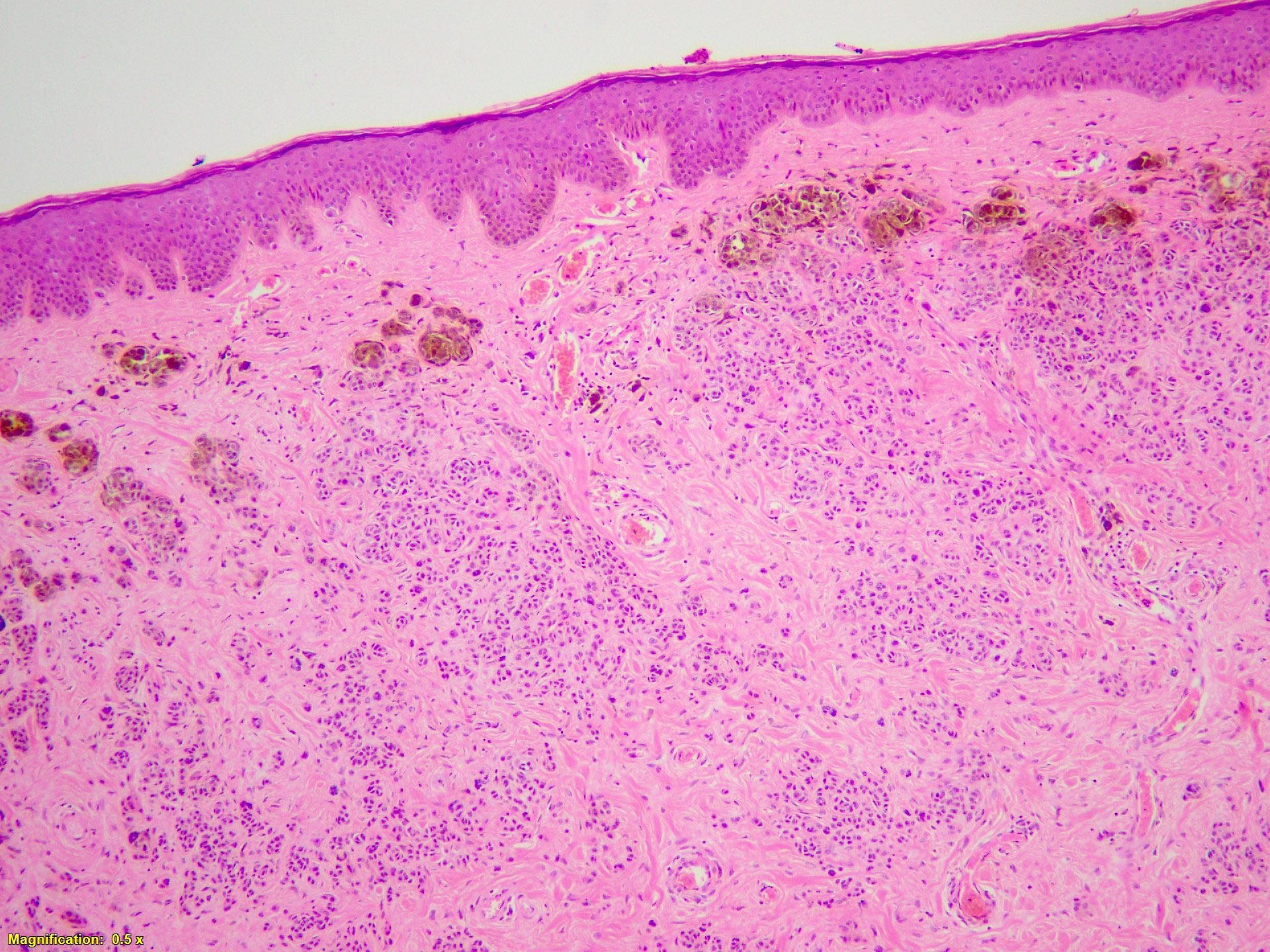
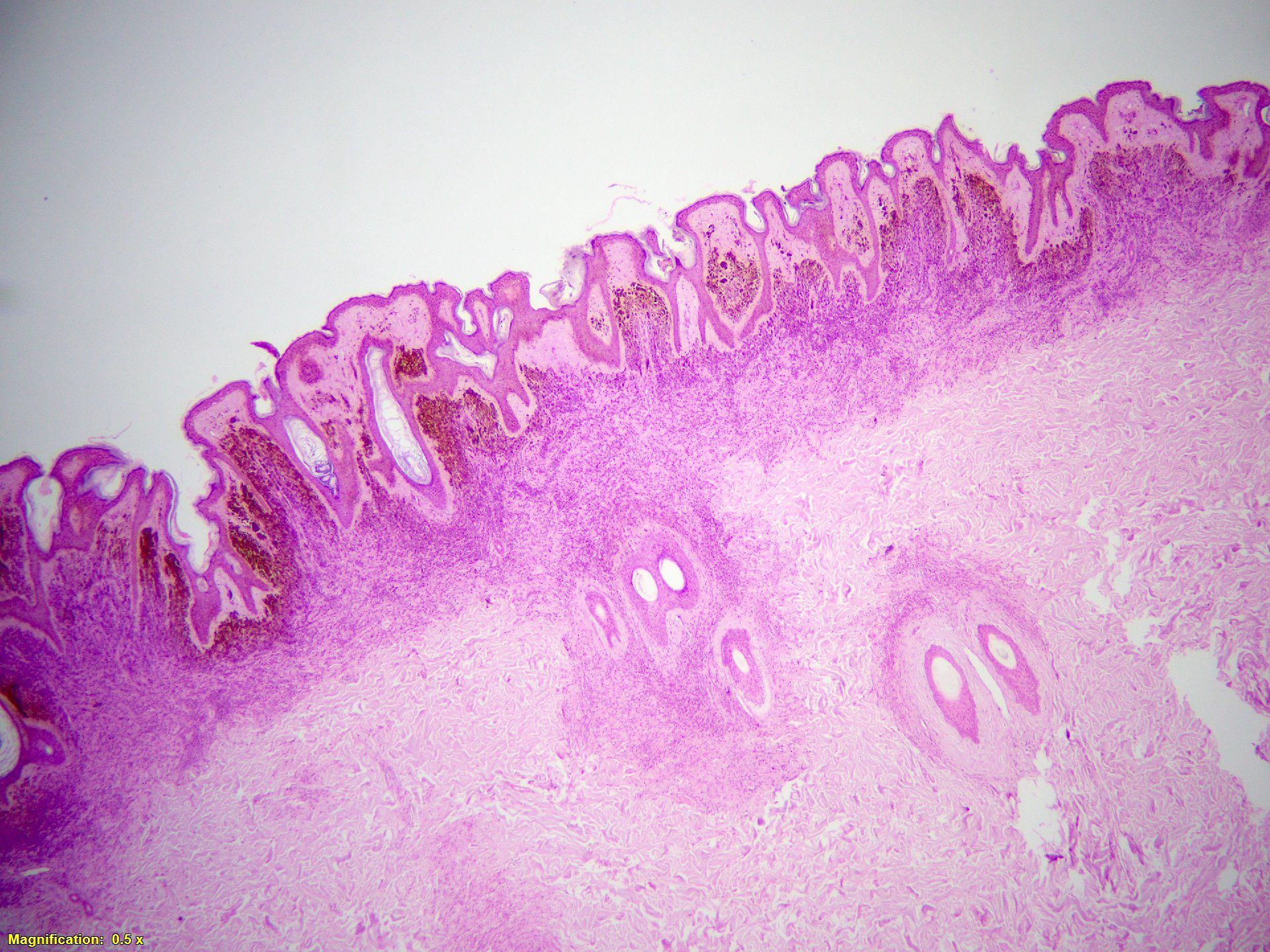
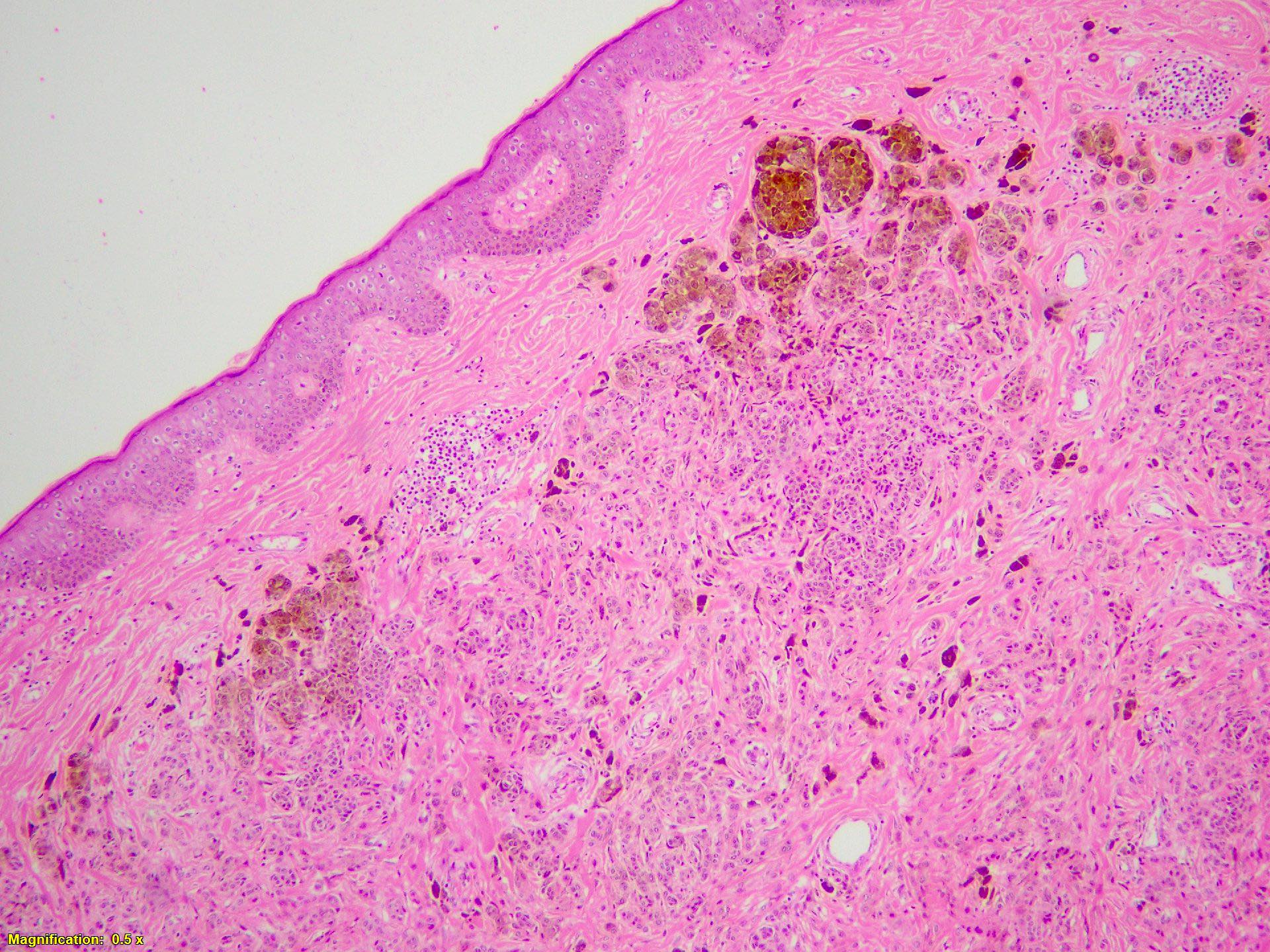
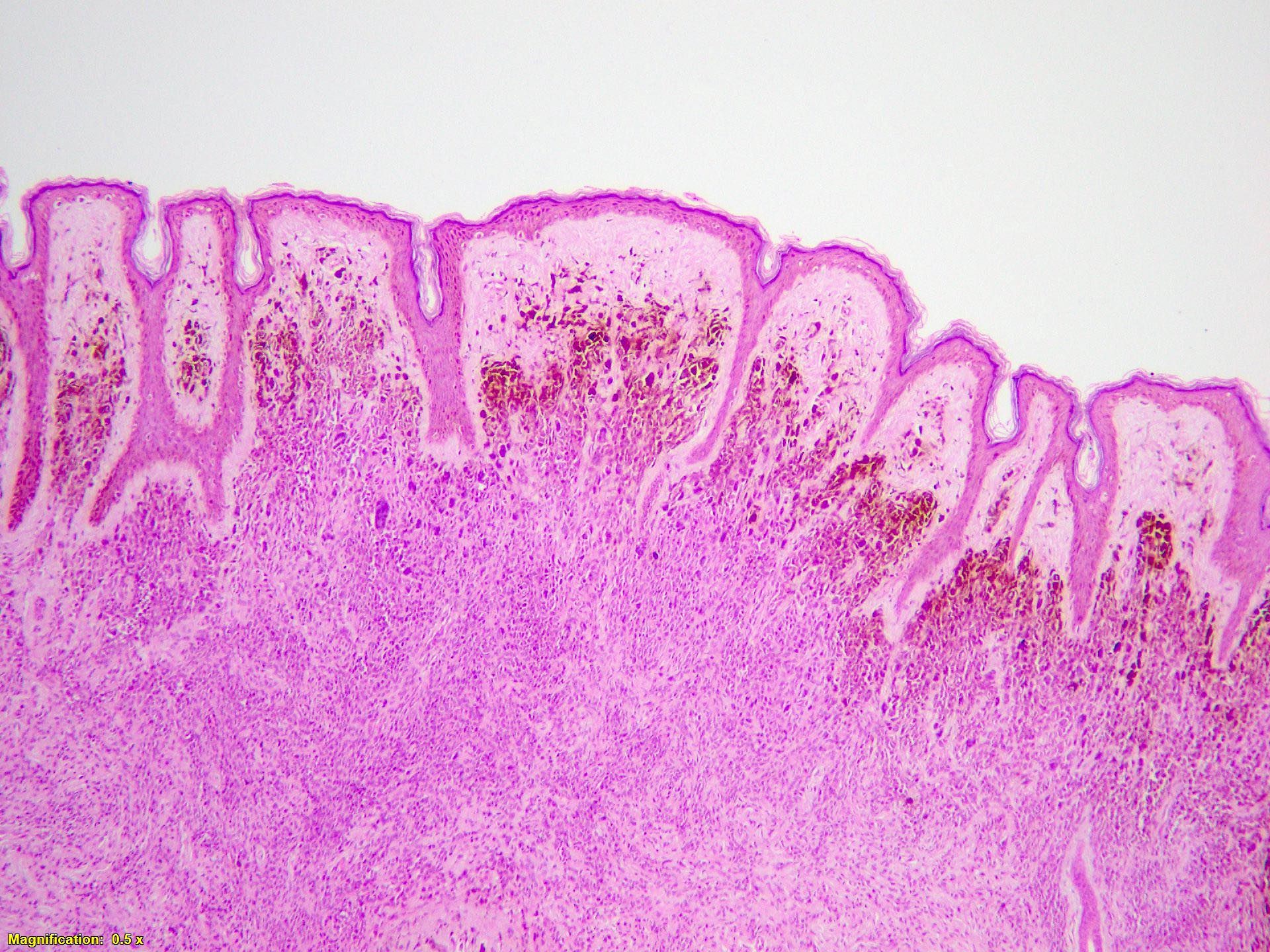
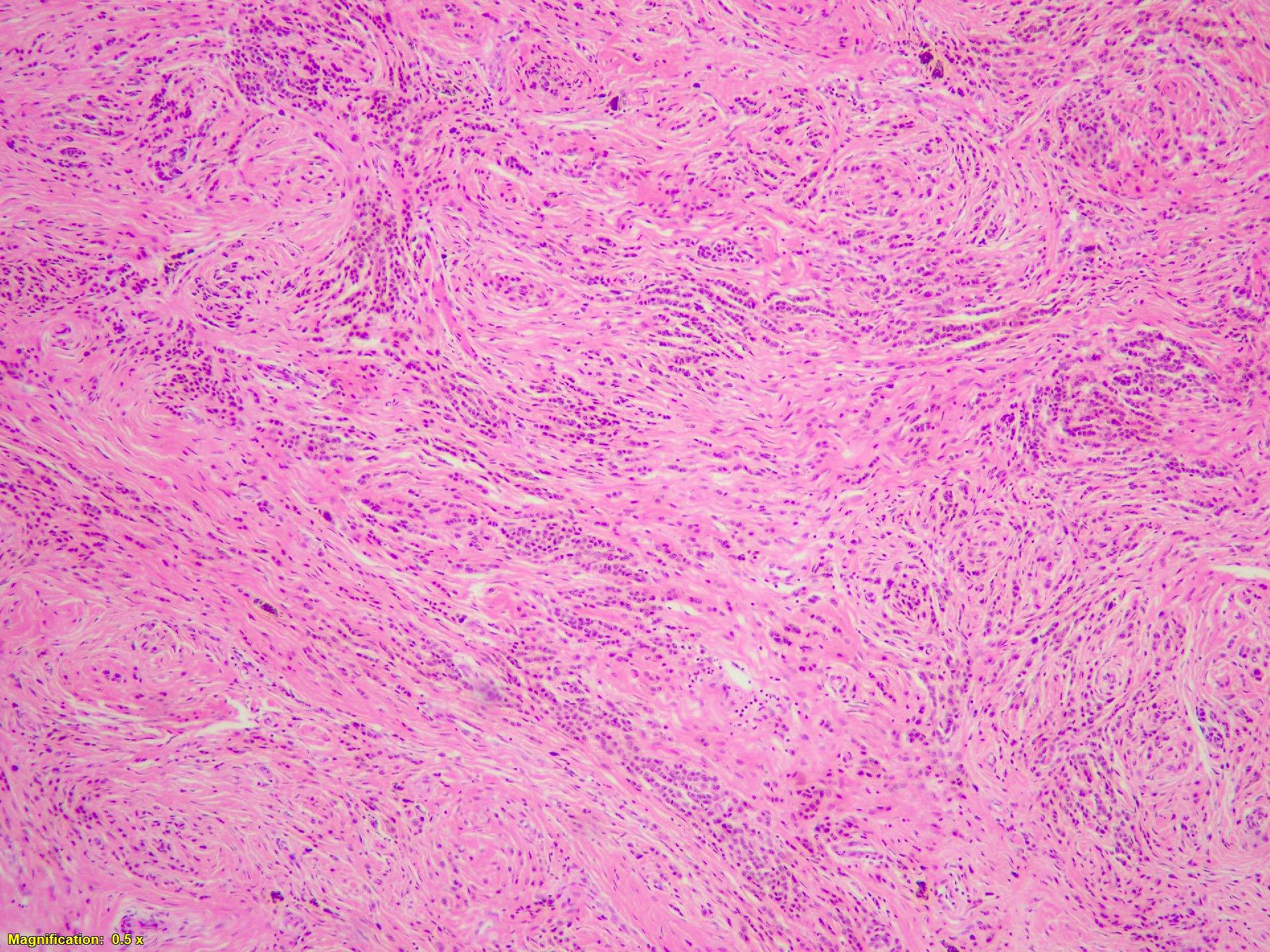
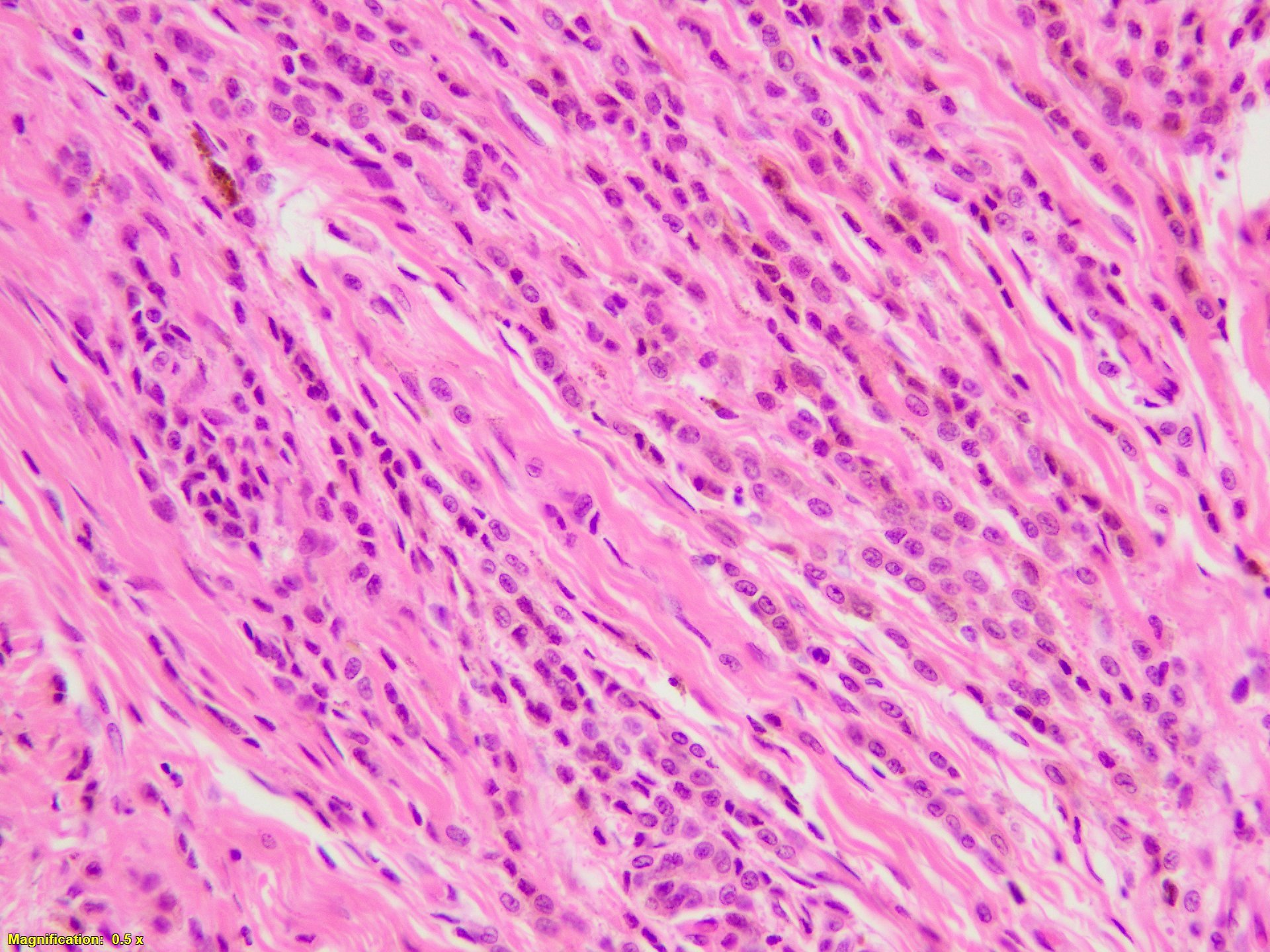
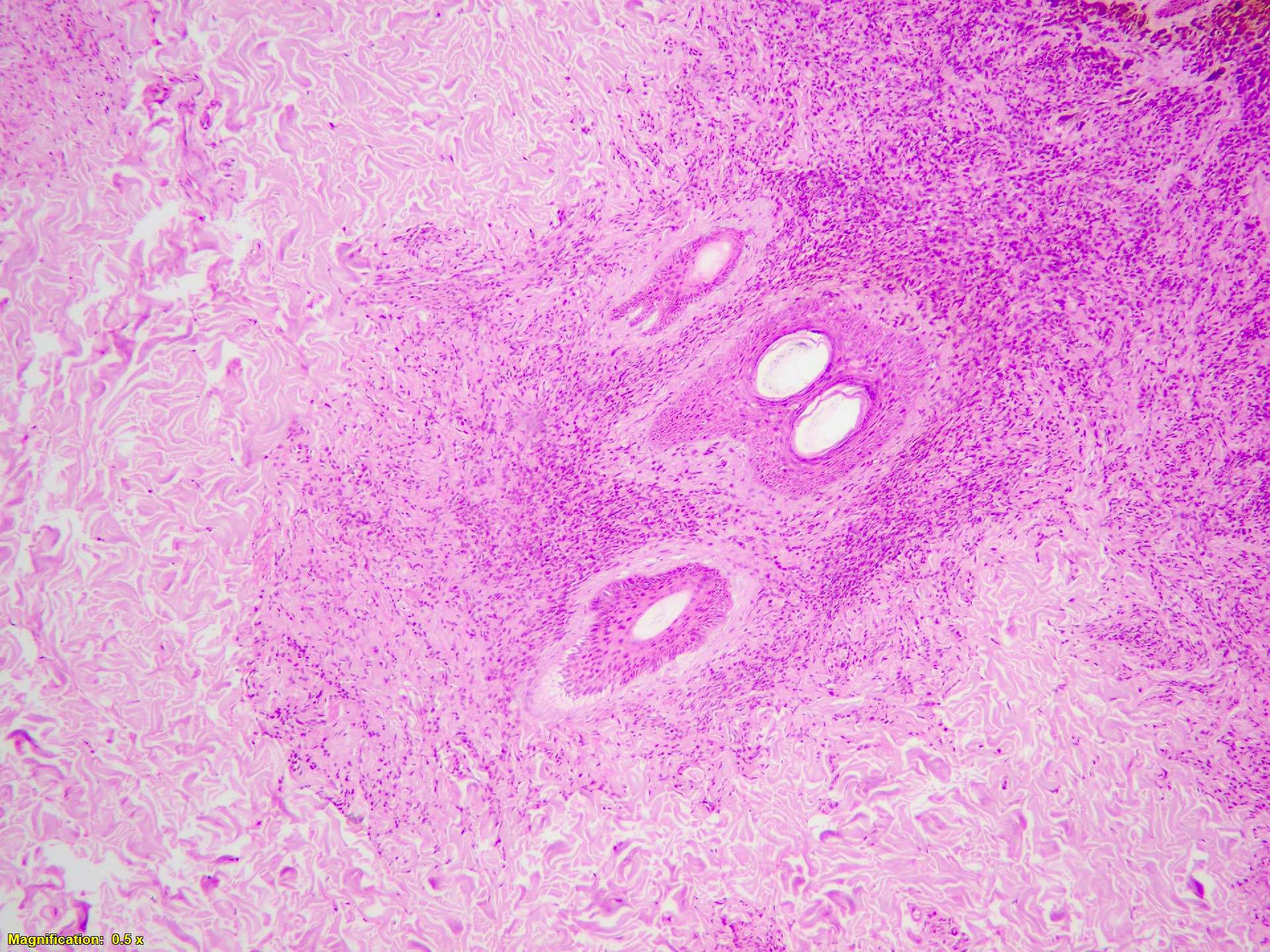
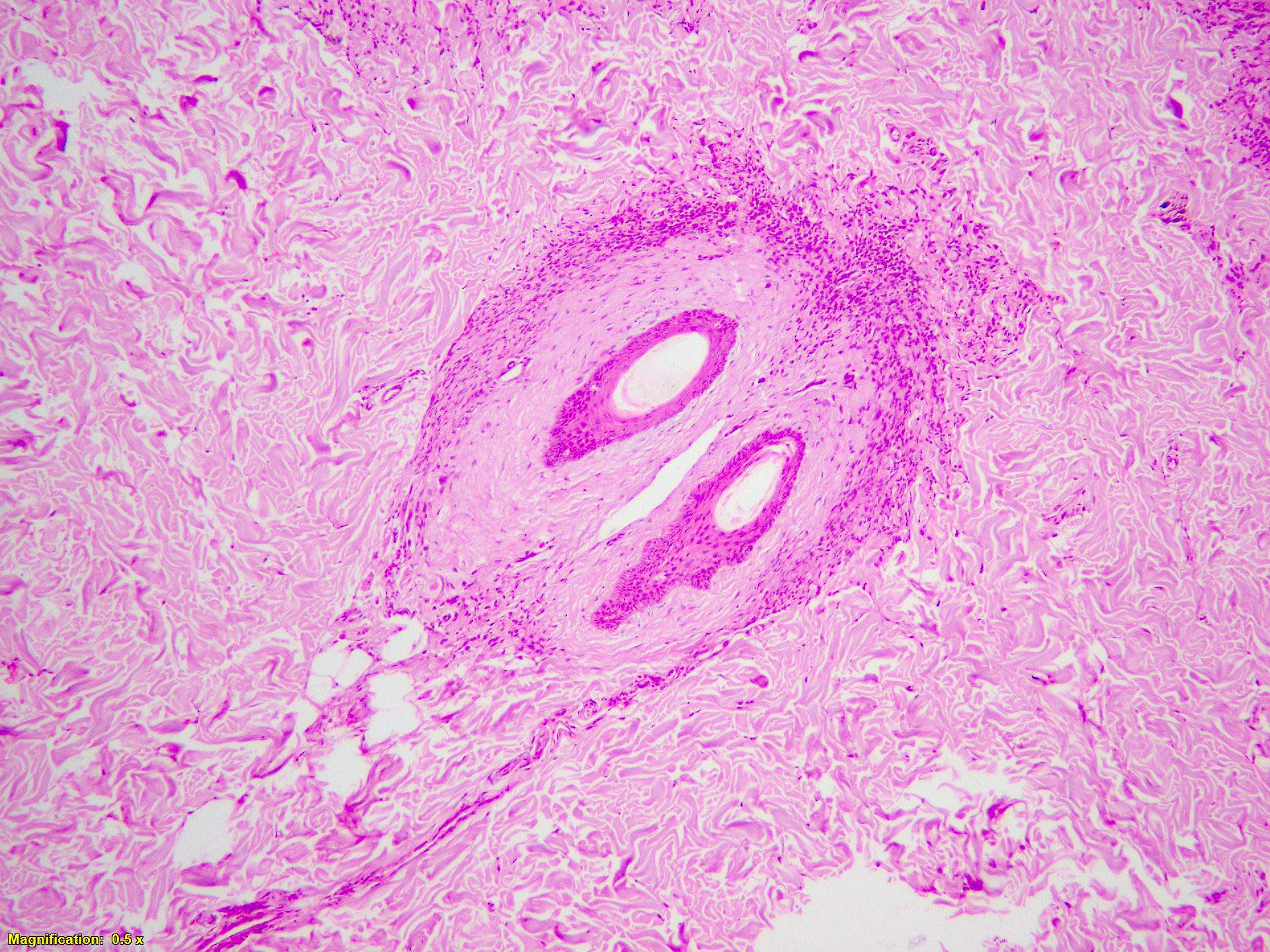
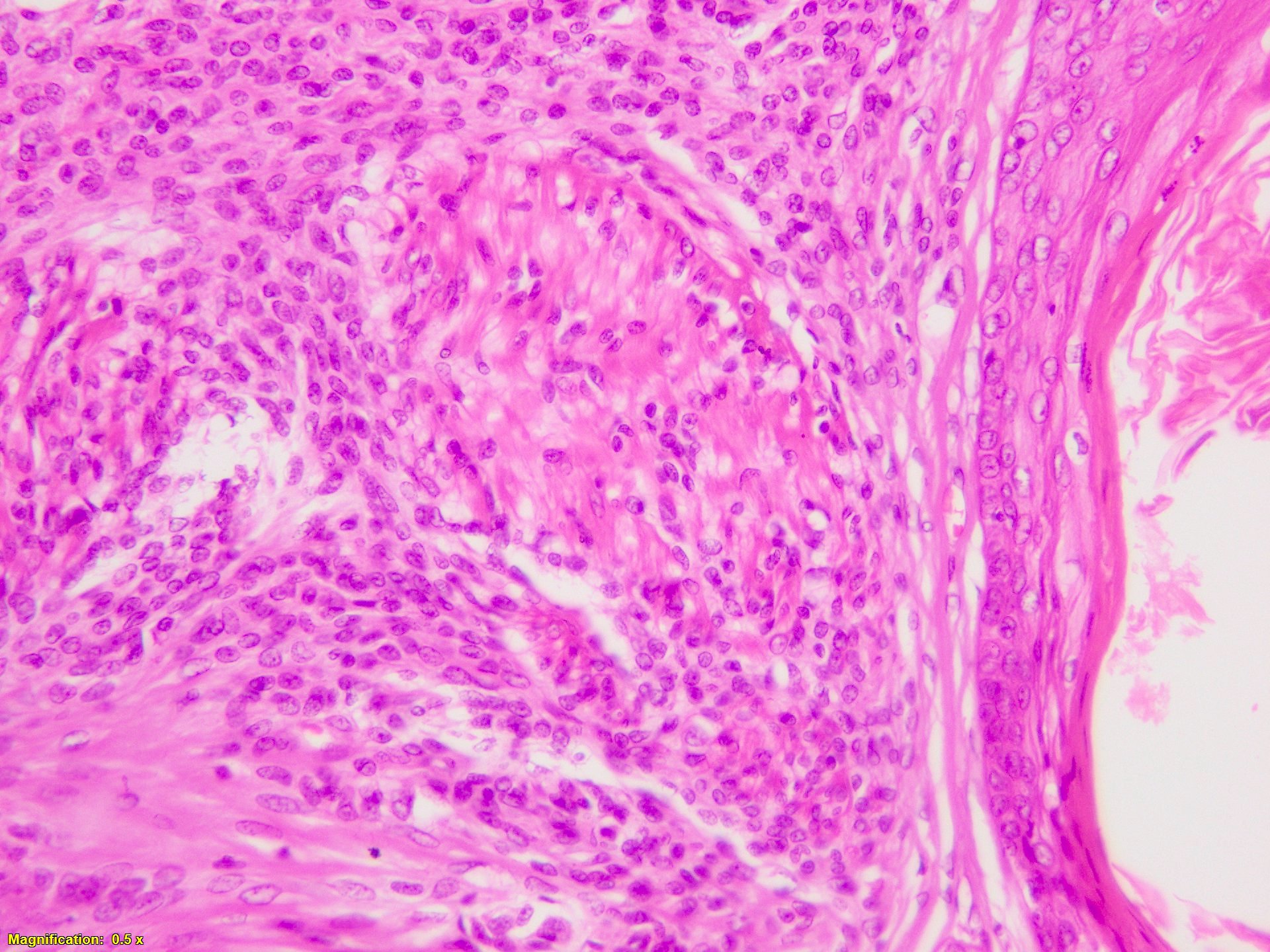
Microscopic (histologic) description
- Diffuse melanocytic proliferation in dermis with extension into subcutaneous fat
- Grenz zone is identified between epidermis and melanocytes
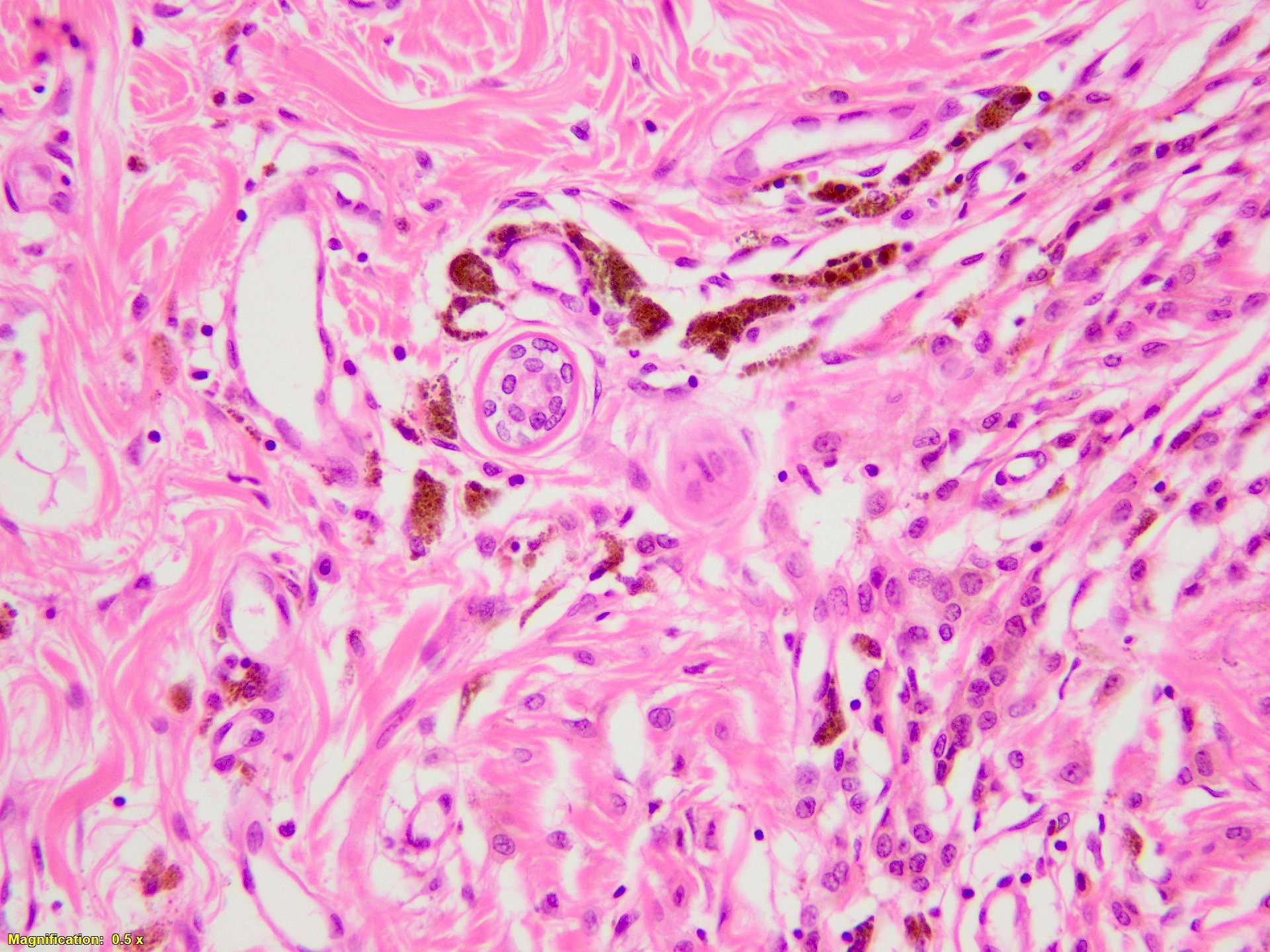
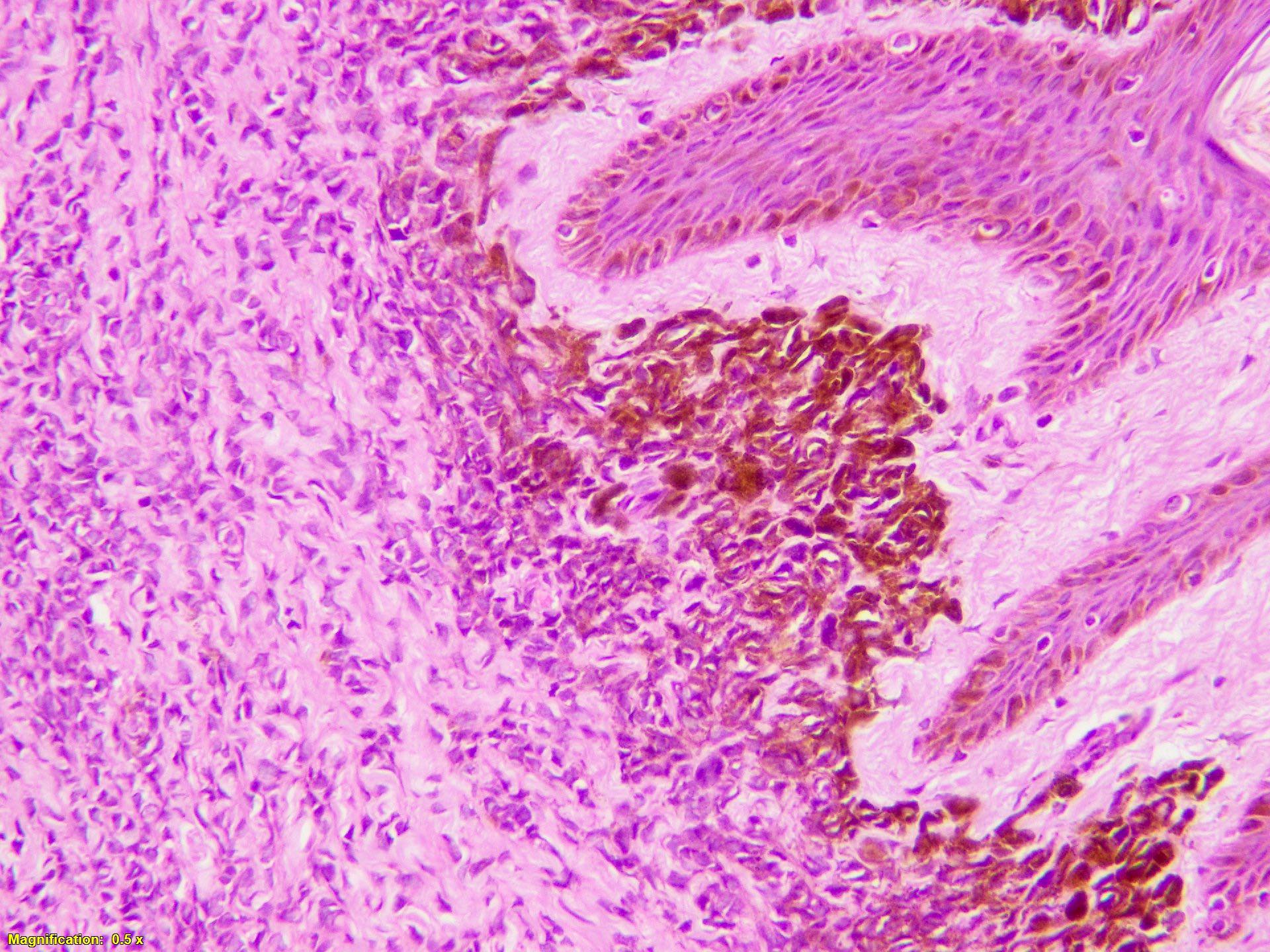
- Nevus cells encircle and extend to walls of dermal appendages, perineural space and blood vessels, and can dissect through collagen bundles
- Variable pigmentation and focal neurotization may be present
- Sparse mitotic activity
- Neonates / young children can have any of these worrisome features: cytological atypia, increased mitotic activity, large junctional nests and pagetoid spread
- Proliferation nodules in CMN
- Large epithelioid melanocytes with mild nuclear pleomorphism
- Mitoses are typically rare and do not exceed 1 mitosis/mm2
- No abnormal mitosis or necrosis
- Remain stable for a prolonged period of time and may regress spontaneously
- References: Elder: Lever's Histopathology of the Skin, 11th Edition, 2014, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
Microscopic (histologic) images
Positive stains
- S100
- SOX10
- MelanA / MART1
- HMB45 (positive only in superficial part)
- References: Elder: Lever's Histopathology of the Skin, 11th Edition, 2014, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019
Negative stains
Molecular / cytogenetics description
- NRAS mutation (Front Med (Lausanne) 2021;8:637857, Elder: Lever's Histopathology of the Skin, 11th Edition, 2014)
- BRAF mutations are also reported in CMN; however, they are uncommon (Pigment Cell Melanoma Res 2015;28:661)
Sample pathology report
- Pigmented skin lesion at scalp, excision:
- Congenital melanocytic nevus (see comment)
- Comment: Benign lesion with excellent prognosis.
- Microscopic description: A dermal based proliferation of melanocytes arranged in small nests and cords, dissecting through dermal collagen bundles. A grenz zone is identified between epidermis and melanocytes. The melanocytes are bland with variable amount of melanin granules. The melanocytes ensheath pilosebaceous units and extend into arrector pili muscle. The lesion shows maturation at depth of the lesion. No evidence of cellular atypia, frequent mitoses or necrosis is found. The margins are clear.
Differential diagnosis
- Acquired melanocytic nevi:
- Present in adults
- Location can be variable
- Prominent nesting pattern, presence of epidermal / junctional component and prominent neurotization
- Can ensheath dermal appendages, however, no involvement of walls of dermal appendages or arrector pili muscle is seen
- Immunohistochemical profile is similar to CMN
- Commonly have BRAF mutations (Pigment Cell Melanoma Res 2015;28:661, Elder: Lever's Histopathology of the Skin, 11th Edition, 2014, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
- Melanoma:
- Proliferation nodules in congenital melanocytic nevus can mimic melanoma
- Melanoma usually presents in older adults
- Location can be variable
- Melanoma usually has asymmetry, epidermal involvement, cellular pleomorphism, brisk / abnormal mitosis, pagetoid spread and necrosis
- PRAME stain is positive in melanoma
- HMB45 stains melanocytes in the superficial and deeper parts of the lesion in melanoma
- In addition to NRAS mutation, melanoma also harbors BRAF, KIT, PTEN, TERTp, CDKN2A and TP53 mutations (Cell 2015;161:1681, Elder: Lever's Histopathology of the Skin, 11th Edition, 2014, Calonje: McKee's Pathology of the Skin, 5th Edition, 2019)
Board review style question #1
Congenital melanocytic nevi commonly harbor which of the following molecular alterations?
- ALK
- BRAF
- KRAS
- NRAS
- p16
Board review style answer #1
Board review style question #2
Board review style answer #2