Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alani AM, Desar S, Torres-Cabala CA. Blue nevus / cellular blue nevus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticbluenevus.html. Accessed March 30th, 2025.
Definition / general
- Common blue nevus (BN) was first described in 1906 (Virchows Arch Pathol Anat 1906;186:212)
- Typical clinical presentation is that of a blue to black macule, papule or nodule on the head, distal extremities or buttock
- Blue nevus is characterized by a dermal proliferation of melanocytes
- Common (dendritic) blue nevus:
- Dermal proliferation of melanocytes (dermal melanocytosis) presenting as a blue to black nodule; sometimes multiple; amelanotic lesions may occur (StatPearls: Blue Nevus [Accessed 30 August 2021])
- Mostly acquired but it can rarely be congenital
- LAMB (lentigines, atrial myxomas and blue nevi) (J Am Acad Dermatol 1984;10:72)
- NAME (nevi, atrial myxoma, myxoid neurofibromas and ephelides) (Adv Anat Pathol 2009;16:365, StatPearls: Blue Nevus [Accessed 30 August 2021], Br J Dermatol 1980;103:421)
- Epithelioid blue nevus, a rare variant, may be associated with Carney complex (a multiple neoplasia syndrome) (J Cutan Pathol 2019;46:954, Semin Diagn Pathol 1998;15:216)
- Bluish black color due to the deep location and abundant melanin; it can be amelanotic (Am J Dermatopathol 1999;21:225)
- Cellular blue nevus:
- Pigmented biphasic tumor with a component of classic blue nevus and distinct cellular areas of spindled to oval melanocytes with clear or finely pigmented cytoplasm (Arch Pathol Lab Med 2011;135:327, Adv Anat Pathol 2009;16:365)
- May be clinically and histologically confused with melanoma
- Benign metastasizing variant is critical to recognize to avoid aggressive treatment (Eur J Dermatol 2008;18:586, J Craniomaxillofac Surg 2010;38:601)
- Atypical cellular blue nevus:
- Rare variant between cellular blue nevus and malignant blue nevus (melanoma arising in association to blue nevus or blue nevus-like melanoma) (Clin Lab Med 2017;37:401)
- May be associated with sentinel lymph node deposits, which generally does not indicate adverse biological behavior
Essential features
- Blue nevi are not uncommon; more frequent in females (F:M = 2:1) and adults < 40 years
- Common blue nevus is composed of bipolar spindle dendritic melanocytes associated with dense collagenous stroma
- Cellular blue nevus is usually a biphasic lesion composed of fusiform to ovoid cells with clear cytoplasm, arranged in nests and surrounded by collagen, pigmented dendritic and bipolar cells and melanophages
- Cellular and atypical cellular blue nevi lack high mitotic activity, atypical mitotic figures, necrosis and marked pleomorphism
Terminology
- Dendritic blue nevus
- Common blue nevus
- Dermal dendritic melanocytic nevus
- Nevus of Jadassohn
- Tièche nevus
- Jadassohn-Tièche blue nevus
ICD coding
Epidemiology
- Common blue nevus:
- Young adults
- F:M = 2:1 (StatPearls: Blue Nevus [Accessed 30 August 2021])
- Cellular blue nevus:
- Middle aged individuals
- F:M = 2:1 (Am J Dermatopathol 1988;10:289)
- Caucasians more than dark skinned races
- Benign but rarely recurs or involves regional lymph nodes (J Cutan Pathol 2010;37:102)
- Melanomas may arise from cellular blue nevus (J Cutan Pathol 2012;39:1094, Am J Dermatopathol 2020;42:313)
- Atypical cellular blue nevus:
- Wide age of presentation: 4 - 78 years
- F > M
Sites
- Common blue nevus:
- Predilection to extremities (dorsa of hands and feet), buttock, scalp and face (Am J Dermatopathol 1988;10:289)
- Extracutaneous can occur; conjunctiva oral mucosa, lymph nodes, vagina, prostate (Adv Anat Pathol 2009;16:365)
- Cellular blue nevus:
- Buttock and sacrococcygeal more common (Am J Dermatopathol 1988;10:289)
- Also scalp, face, trunk and extremities with predilection to dorsal foot (Am J Dermatopathol 1988;10:289)
- Atypical cellular blue nevus:
- Buttocks, head and neck and extremities
Pathophysiology
- Common blue nevus:
- May be due to arrested melanocytic migration or from specific stem cells within the dermis (Arch Pathol Lab Med 2011;135:327)
- Blue color is a result of reflection, a phenomenon known as the Tyndall effect (StatPearls: Blue Nevus [Accessed 30 August 2021])
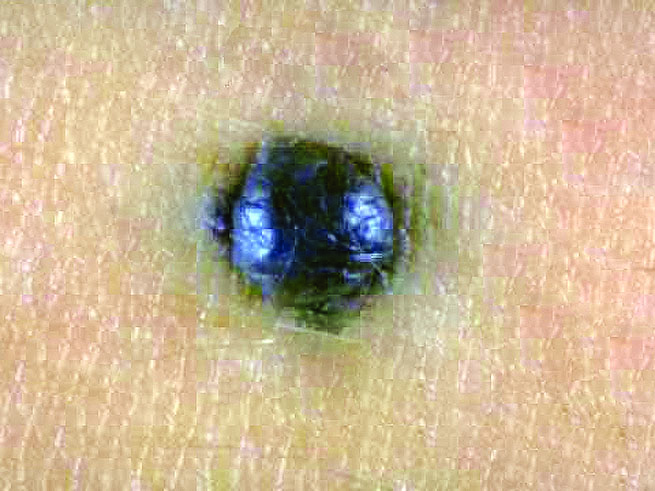
Clinical features
- Common blue nevus:
- Well demarcated, dome shaped, blue-black
- Small (< 1 cm) (Adv Anat Pathol 2009;16:365)
- Cellular blue nevus:
- Slowly growing, grayish blue-black nodules
- Large (> 1 cm); can be up to 10 cm (Clin Lab Med 2017;37:401)
- Atypical cellular blue nevus:
- Bluish deep dermal nodules
Diagnosis
- Clinical presentation
- Dermoscopy shows homogenous, structureless pigment pattern, with variety of colors (blue, white-blue, black, brown and polychromatic) (J Cutan Pathol 2007;34:543, J Am Acad Dermatol 2012;67:199)
- Definite diagnosis is made on excision specimen through histologic examination
Case reports
- Common blue nevus:
- 14 year old girl with persistent blue nevus that presented with prominent extension beyond the scar of the original excision, mimicking melanoma (J Am Acad Dermatol 2004;50:S118)
- 15 year old girl with poliosis overlying a nevus with blue nevus features (Dermatol Online J 2008;14:20)
- 35 year old man with multiple pigmented lesions of the penis (J Cutan Pathol 2004;31:185)
- 38 year old woman with blue-black discoloration of the proximal lunula of her right thumbnail (Australas J Dermatol 2020;61:164)
- 40 year old woman with blue-gray pigmentation on the nail of her left fourth finger (J Am Acad Dermatol 2008;58:1021)
- 41 year old woman with a nodular swelling in left axilla (Am J Clin Pathol 1984;81:367)
- 47 year old man with blue macule under the right first toenail (Dermatol Online J 2017;23:13030)
- 52 year old man with elevated prostate specific antigen and mild obstructive lower urinary tract symptoms (Case Rep Urol 2018;2018:7820717)
- 53 year old woman with large plaque type blue nevus with subcutaneous cellular nodules (Am J Surg Pathol 2000;24:92)
- 68 year old man with discoloration of right thumbnail (J Cutan Pathol 2020;47:1111)
- 69 year old man with blue nevus with satellitosis mimicking malignant melanoma (J Eur Acad Dermatol Venereol 2001;15:570)
- Cellular blue nevus:
- 14 year old boy with a giant, infiltrative facial tumor (J Clin Pathol 2007;60:82)
- 16 year old girl with tender right sided submandibular neck mass (Am J Otolaryngol 2021;42:103139)
- 19 year old man with 0.5 cm epidermal cyst (Case #7)
- 19 year old man with pilonidal sinus (J Cutan Pathol 2007;34:942)
- 28 year old woman with intracranial extension (J Clin Neurosci 2000;7:453)
- 29 year old man with a pigmented lesion of the perilimbal conjunctiva on the right eye since birth (Ann Clin Lab Sci 2017;47:477)
- 30 year old woman, 40 year old woman and 43 year old man with cellular blue nevi of the eyelid (J Am Acad Dermatol 2008;58:257)
- 31 year old man with xanthomatosis and diabetes mellitus (Indian J Dermatol Venereol Leprol 2001;67:200)
- 34 year old man with nevus cells in sentinel lymph node (Eur J Dermatol 2008;18:586)
- 37 year old woman with abnormal uterine bleeding (Int J Gynecol Pathol 2021;40:349)
- 58 year old woman with a blue spot on the lanula of the left thumb (Dermatol Ther 2020;33:e13763)
- 61 year old woman with a pigmented nodule on her right buttock (J Cutan Pathol 2005;32:385)
- 63 year old man with yellowish papular lesion of the upper eyelid (Ophthalmic Plast Reconstr Surg 2017;33:e122)
- Atypical cellular blue nevus:
- 8 year old boy with pigmented lesion in the buttock since birth, with progressive growth in 2 years (An Bras Dermatol 2017;92:110)
- 28 year old woman with a black skin lesion on the dorsum of the right foot (Dermatopathology (Basel) 2019;6:20)
- 37 year old woman with pedunculated thigh mass (J Dermatol 2000;27:730)
- 43 year old man with a tender mass on his left anterior chest (Am J Dermatopathol 2021;43:e61)
- 46 year old white man with a mass on his right buccal mucosa (Head Neck Pathol 2013;7:171)
Treatment
- Common and cellular blue nevus: excision
- Atypical cellular blue nevus:
- Excision with at least 1 cm margins
- Close follow up
- Reference: Ann Otol Rhinol Laryngol 2021;130:1407
Clinical images
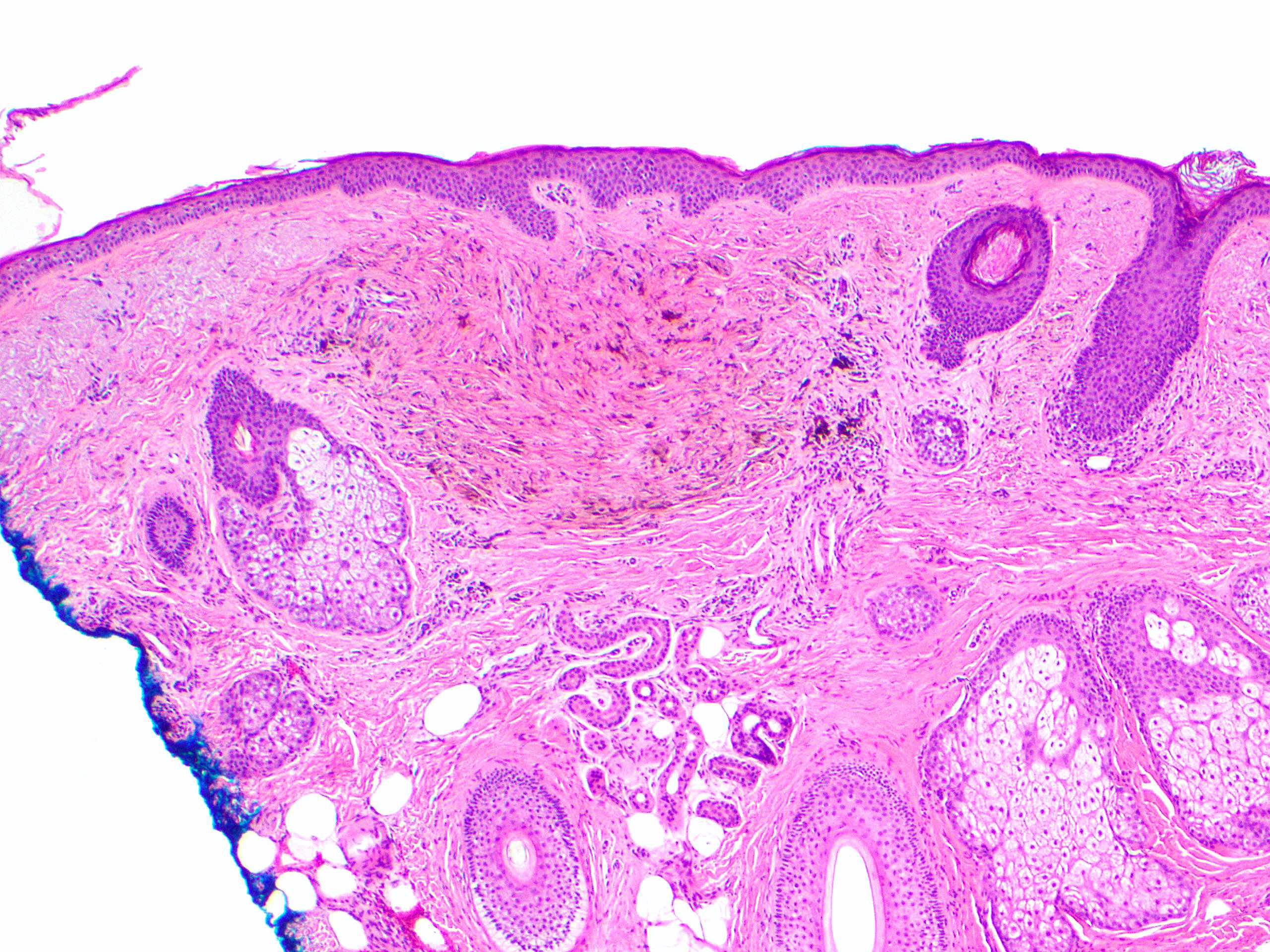
Microscopic (histologic) description
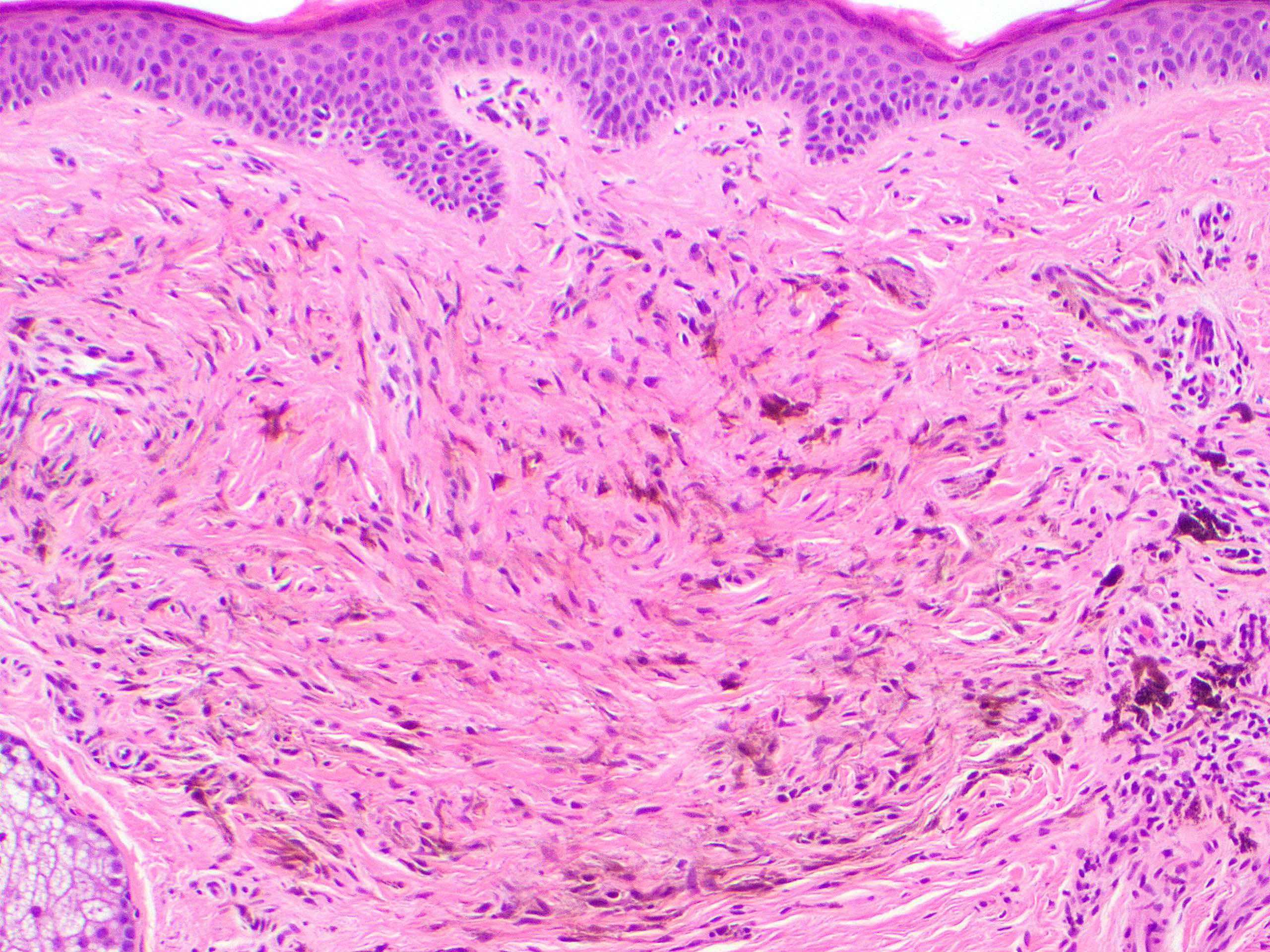
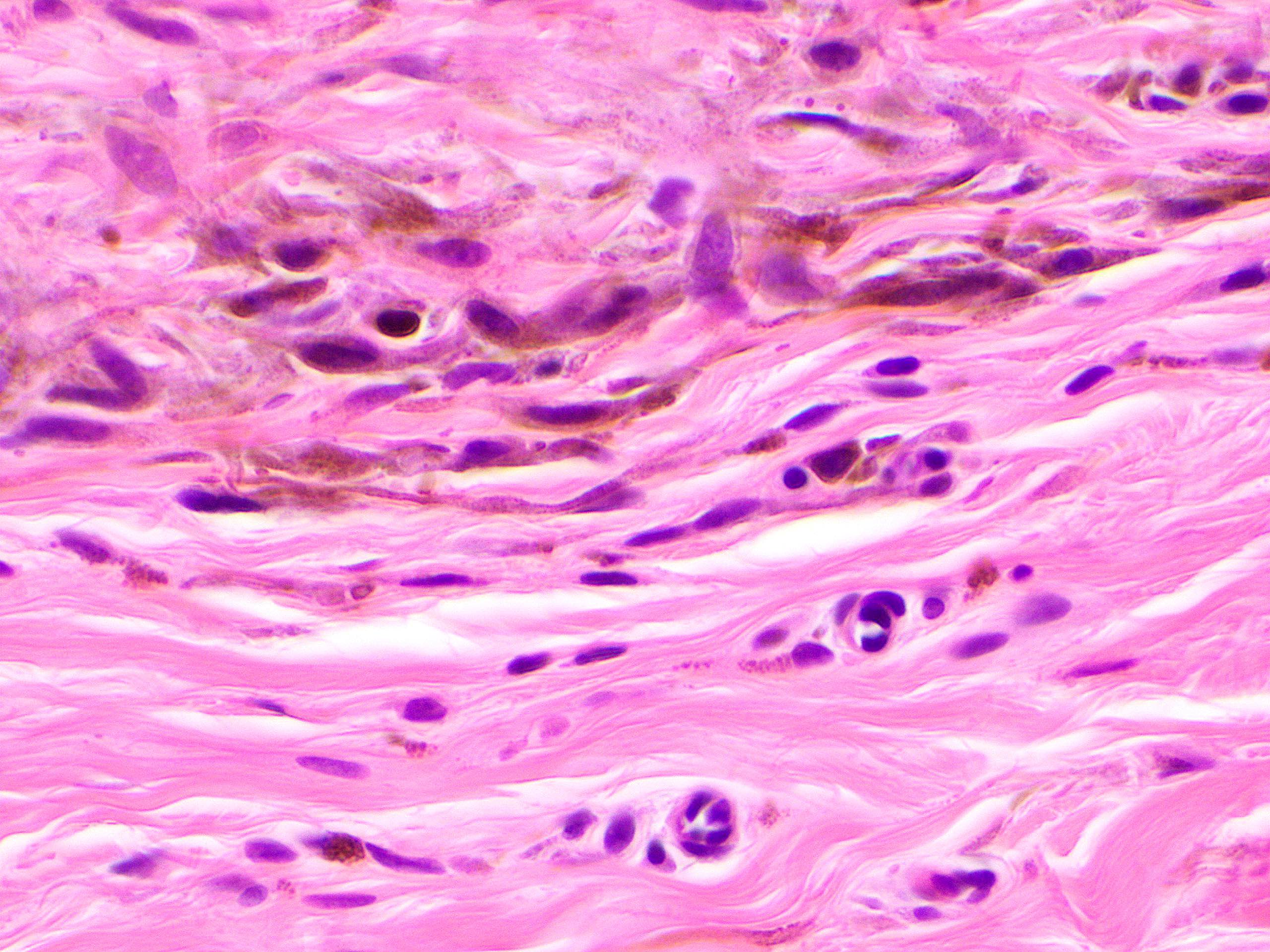
- Common blue nevus:
- Dermal proliferation of pigmented dendritic bipolar spindle melanocytes associated with fibroblastic and collagenous stroma (Adv Anat Pathol 2009;16:365)
- Admixed scattered heavily pigmented melanophages
- Melanocytes aggregate around blood vessels, nerves or cutaneous appendages (Clin Lab Med 2017;37:401)
- May present in the superficial dermis or extend into subcutis (Clin Lab Med 2017;37:401)
- No maturation
- No cytologic atypia, no mitotic figures (Clin Lab Med 2017;37:401)
- Nodal blue nevi, in perinodal fat, capsule and septa but not in parenchyma (Am J Surg Pathol 1984;8:907)
- Junctional activity present only in combined nevus (Clin Lab Med 2017;37:401)
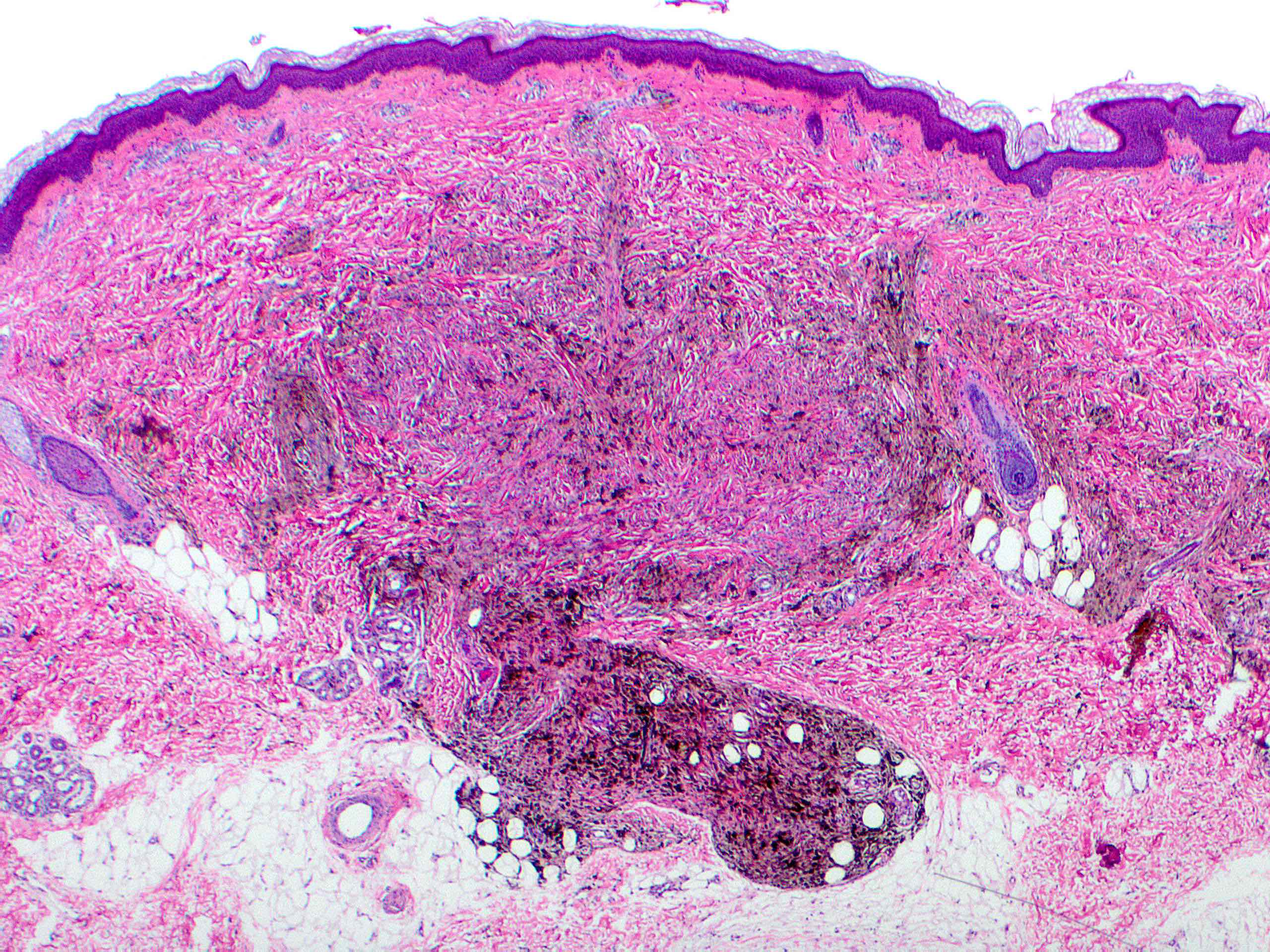
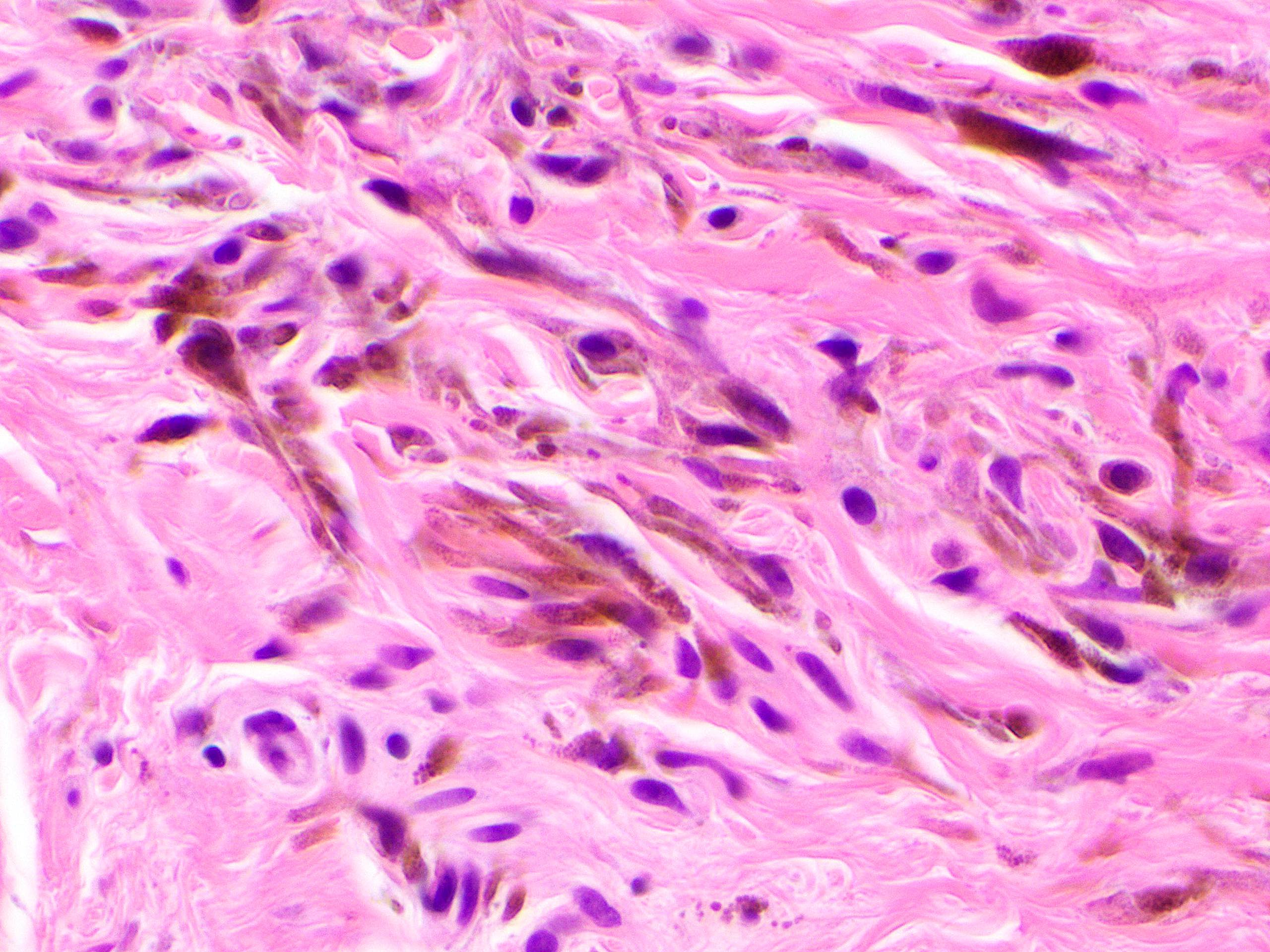
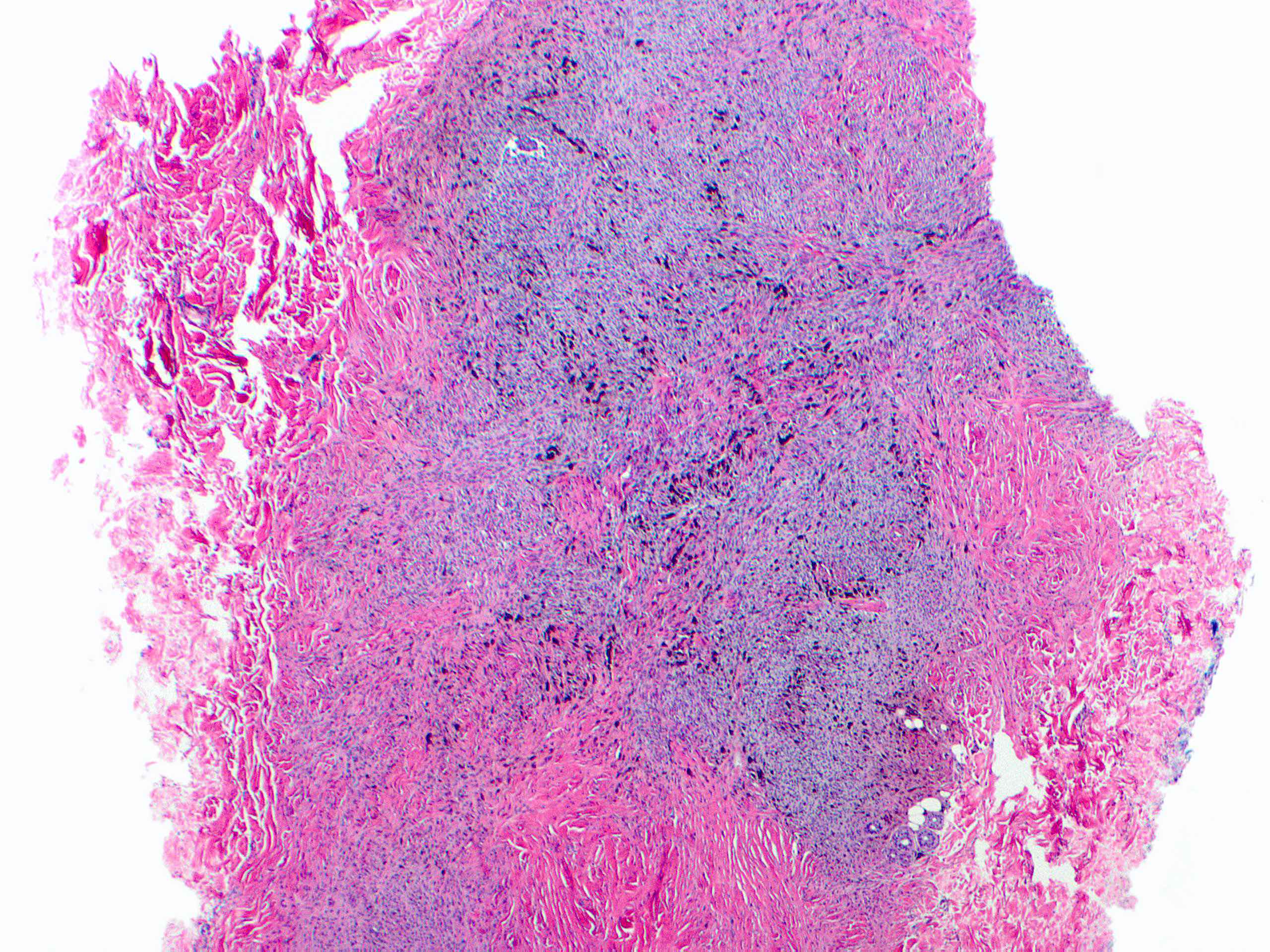
- Cellular blue nevus:
- Well circumscribed lesion, occupying superficial and mid dermis, sometimes extending to deep dermis and subcutis (Adv Anat Pathol 2009;16:365)
- Oval to plump spindle cells intermingled with dendritic melanocytic cells; usually not heavily pigmented (Adv Anat Pathol 2009;16:365)
- Variable numbers of melanophages
- Margin may be pushing and infiltrates adjacent nerve trunks (Clin Lab Med 2011;31:345)
- Alveolar pattern:
- Nests of amelanotic cells with clear cytoplasm
- Surrounded by collagen, dendritic melanocytes and melanophages in variable amounts
- Neuronevoid or fascicular pattern (Clin Lab Med 2017;37:401)
- Mitotic activity is usually absent and should be low (< 1/mm²)
- No atypical findings (including cell crowding, nuclear atypia, hyperchromasia, necrosis or expansile growth)
- Junctional activity present in combined nevus
- Angiomatoid variant containing numerous dilated blood vessels has been described (J Cutan Pathol 2005;32:385)
- Nodal involvement:
- Is rare and often takes the form of subcapsular sinus and occasionally parenchymal deposits (Eur J Dermatol 2008;18:586, Int J Surg Pathol 2014;22:570, J Cutan Pathol 2010;37:102)
- Cells are histologically identical to the parent lesion, with no pleomorphism or mitotic activity
- Not true metastasis and does not alter prognosis
- Atypical cellular blue nevus:
- Like cellular blue nevus and a background of common blue nevus is invariably present
- Nests and fascicles of spindle and epithelioid cells
- Lower portion may show an infiltrative border (Arch Pathol Lab Med 2011;135:327, Histopathology 2004;45:433)
- Mild cytologic atypia, nuclear hyperchromasia and pleomorphism centered in the lower aspect of the nevus (Adv Anat Pathol 2009;16:365)
- Low mitotic activity of < 2/mm² (Adv Anat Pathol 2009;16:365)
- Abnormal mitosis or necrosis never present (J Cutan Pathol 1998;25:252, Arch Pathol Lab Med 2011;135:327)
- Perineural and periadnexal infiltration typically present (J Cutan Pathol 1998;25:252)
- Perivascular lymphocytic infiltrate is often seen at the edge of the lesion (J Cutan Pathol 1998;25:252)
- Presence of more cytologic atypia, cell crowding, greater mitotic activity, abnormal mitoses and necrosis are consistent with malignant blue nevus (melanoma mimicking blue nevus; melanoma arising in association with blue nevus) (Arch Pathol Lab Med 2011;135:327)
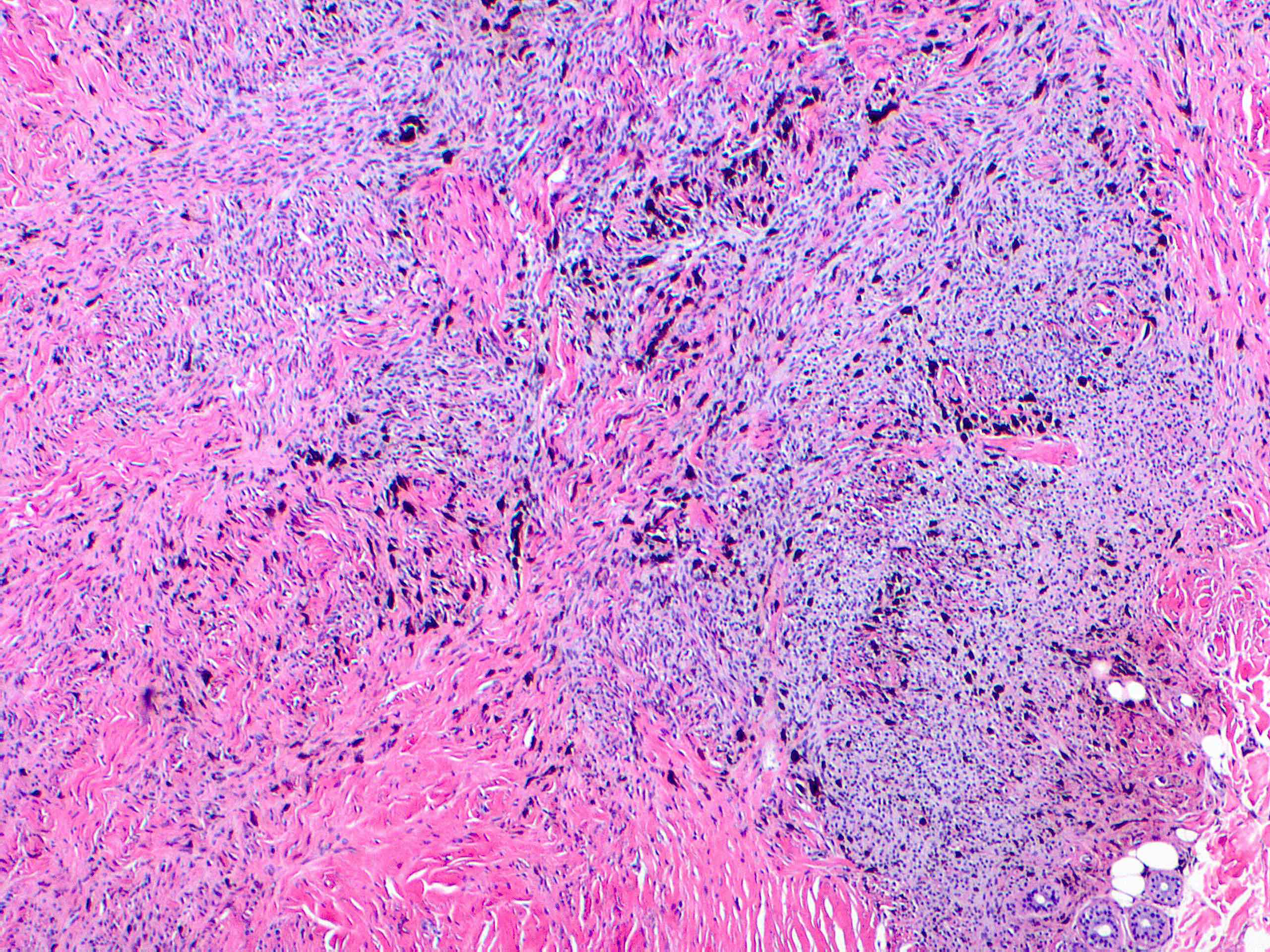
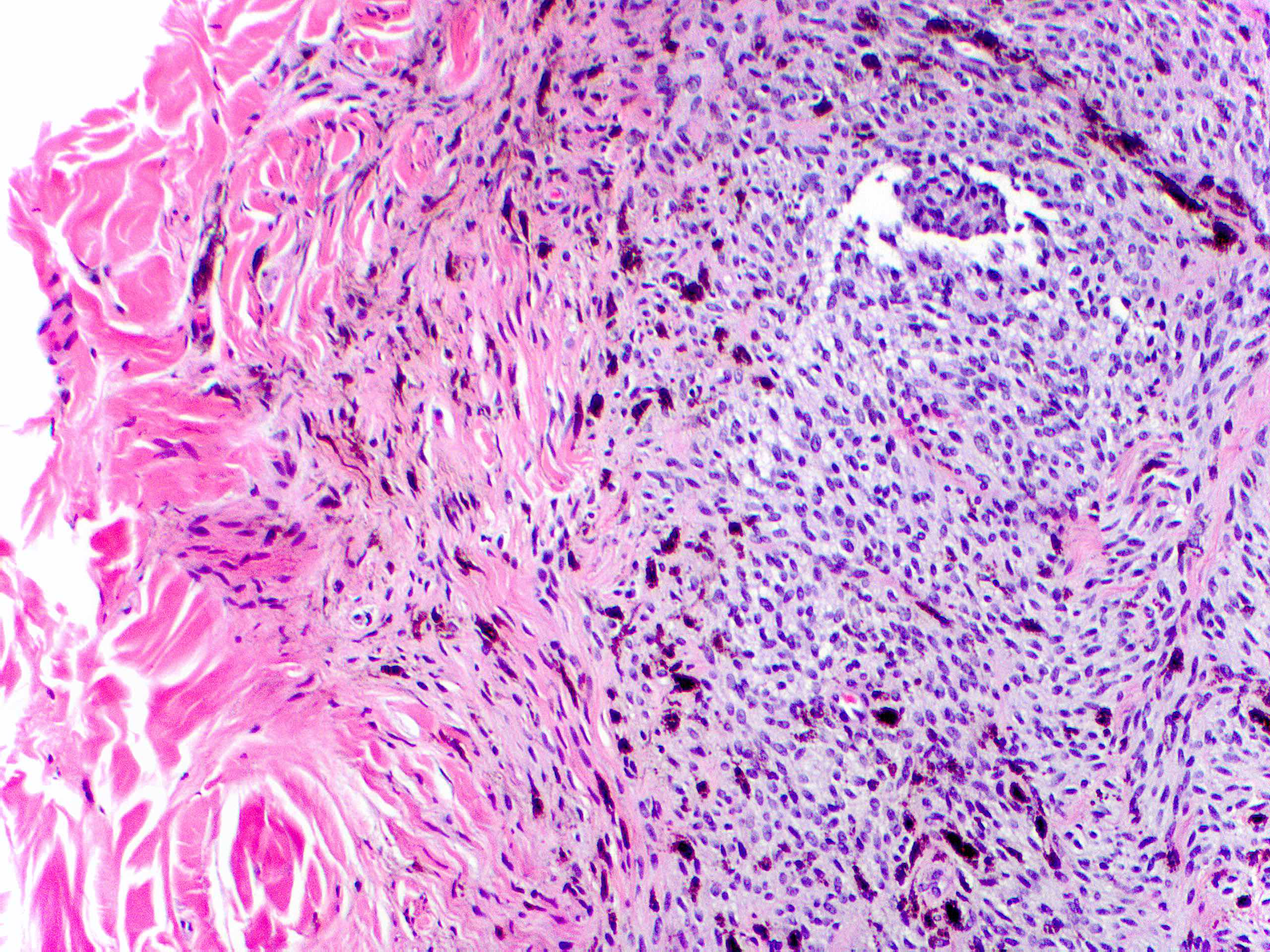
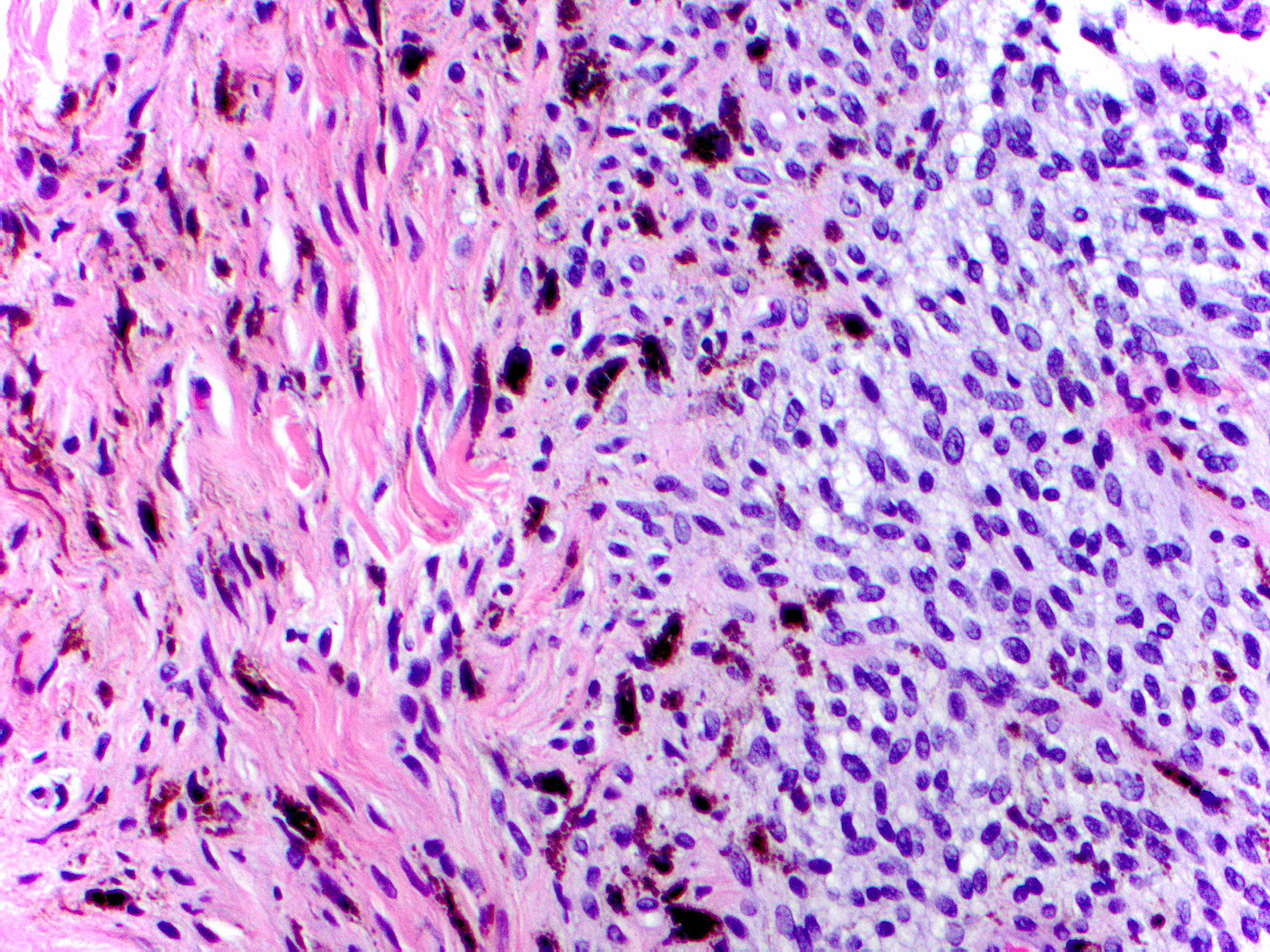
Microscopic (histologic) images
Contributed by Carlos A. Torres-Cabala, M.D.
Common blue nevus
Cellular blue nevus
Positive stains
- Common blue nevus:
- SOX10 (Clin Lab Med 2017;37:401, Arch Pathol Lab Med 2011;135:327)
- HMB45 (diffuse and strong) (J Cutan Pathol 1991;18:261, Clin Lab Med 2017;37:401)
- MelanA / MART1
- S100 (may be negative)
- Preserved BAP1 (Clin Lab Med 2017;37:401)
- Preserved p16
- Cellular blue nevus:
- SOX10
- HMB45 (diffuse) (Am J Surg Pathol 1990;14:748, Clin Lab Med 2017;37:401)
- MelanA / MART1
- S100
- Ki67 < 2 - 3%
- Preserved BAP1 (Clin Lab Med 2017;37:401, Am J Dermatopathol 2020;42:313)
- Preserved p16
- Atypical cellular blue nevus:
- HMB45 (Clin Lab Med 2017;37:401)
- Increased Ki67 (Clin Lab Med 2017;37:401)
Molecular / cytogenetics description
- Common blue nevus:
- GNAQ and GNA11 mutations (Clin Lab Med 2017;37:401, Nature 2009;457:599)
- No BRAF, NRAS or NF1 mutations (N Engl J Med 2010;363:2191)
- Cellular blue nevus:
- GNAQ and GNA11 mutations (Nature 2009;457:599)
- No chromosomal aberrations (Am J Surg Pathol 2005;29:1214)
- Atypical cellular blue nevus:
- Complex copy number aberrations involving 4 or more chromosomal regions are indicative of malignancy (Mod Pathol 2016;29:227)
Sample pathology report
- Common blue nevus:
- Skin, hand, dorsum, right, punch biopsy:
- Blue nevus, present at peripheral and deep tissue edges (see comment)
- Comment: Histological sections reveal a proliferation of spindle shaped melanocytes admixed with abundant pigment laden macrophages in dense collagenous background. The spindle cells have bland cytologic features. These findings support the above diagnosis.
- Skin, hand, dorsum, right, punch biopsy:
- Cellular blue nevus:
- Skin, buttock, right, ellipse:
- Skin and subcutis with scar and cellular blue nevus, margins of resection are free of cellular blue nevus (see comment)
- Comment: Sections show a dermal scar and an adjacent proliferation of spindle and epithelioid melanocytes occupying the dermis. Dendritic melanocytes showing classic blue nevus appearance are present at the periphery of the lesion. No nuclear atypia, necrosis or mitosis are identified. Immunohistochemical studies reveal the lesion cells to be diffusely positive for SOX10 and HMB45 and to show preserved expression of BAP1 (nuclear) and p16 (nuclear and cytoplasmic). The MIB1 proliferative rate is < 1%. These findings support the above diagnosis.
- Skin, buttock, right, ellipse:
- Atypical blue nevus:
- Skin, forearm, right, ellipse:
- Skin and subcutis with atypical blue nevus, present at peripheral margins of resection (see comment)
- Comment: Sections show a proliferation of spindle and epithelioid melanocytes involving dermis and focally extending into subcutis. The melanocytes are arranged in nests and fascicles. The lower portion of the nevus shows infiltrative growth with mild cytologic atypia and minimal pleomorphism. Perineural invasion is present. Rare mitotic figures (1/mm²) are identified; however, abnormal mitosis or necrosis are not identified. Immunohistochemical studies were performed. The lesion cells are diffusely positive for HMB45. A double MART1 / Ki67 study reveals low proliferation rate. Preserved expression of BAP1 is noted, along with focal expression of p16. The lesion appears to be incompletely excised. Re-excision is recommended, if clinically indicated.
- Skin, forearm, right, ellipse:
Differential diagnosis
- Common blue nevus:
- Melanoma mimicking blue nevus, melanoma arising in association with blue nevus, atypical blue nevus
- Congenital dermal melanocytosis:
- Formerly known as Mongolian spot
- Benign fibrous histiocytoma:
- Hemosiderin pigment, no melanin
- Dermatofibrosarcoma protuberans:
- More cellular, tight storiform pattern, infiltrative, has pigmented variant
- Nevus of Ito / nevus of Ota
- Desmoplastic nevus (Arch Pathol Lab Med 2011;135:327)
- Desmoplastic Spitz nevus
- Metastatic melanoma:
- Blue nevus-like cutaneous melanoma metastasis
- Cellular blue nevus:
- Atypical cellular blue nevus
- Cellular neurothekeoma (Histopathology 2004;45:433)
- Dermatofibroma (Histopathology 2004;45:433)
- Blue nevus-like melanoma (melanoma mimicking blue nevus, melanoma arising in association with blue nevus):
- Scalp or heel lesion with marked nuclear atypia, numerous mitotic figures, some atypical and necrosis
- Variable epithelioid tumor cells (Clin Lab Med 2011;31:345)
- Clear cell sarcoma:
- EWSR1 rearrangement (Histopathology 2004;45:433)
- Atypical cellular blue nevus (Arch Pathol Lab Med 2011;135:327):
- Cellular blue nevus
- Blue nevus-like melanoma (Histopathology 2004;45:433, Am J Surg Pathol 2008;32:36)
- Desmoplastic melanoma (Clin Lab Med 2011;31:345)
- Cellular neurothekeoma
- Clear cell sarcoma
- Dermatofibroma
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Epithelioid blue nevus is associated with
- Carney complex
- Birt-Hogg-Dubé syndrome
- Muir-Torre syndrome
- Neurofibromatosis
- Tuberous sclerosis
Board review style answer #2