Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gottesman SP. Syphilis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorsyphilis.html. Accessed April 3rd, 2025.
Definition / general
- Syphilis is primarily a sexually transmitted disease
- Clinically, in the secondary stage, presents with a papulosquamous eruption and has many histologic mimickers, including psoriasis
Essential features
- Lichenoid superficial and deep perivascular and periadnexal lymphohistiocytic inflammation with admixed plasma cells
- Up to 33% of biopsies may lack plasma cells
- Immunohistochemistry is more sensitive than silver stains
Terminology
- Lues venerea, Cupid's disease
ICD coding
- ICD-10: A51.39 - other secondary syphilis of the skin
Epidemiology
- Transmitted via sexual contact
- Can also be transmitted congenitally and rarely via blood products
- More prevalent in men than in women, especially ages 20 - 29
- Higher incidence in gay and bisexual men (MMWR Morb Mortal Wkly Rep 2014;63:402)
Sites
- Skin, mucosal surfaces, eyes, brain / nerves, blood vessels, bones, joints and liver (CDC: Syphilis [Accessed 11 December 2019])
Pathophysiology
- On skin to skin contact, it enters via areas of microtrauma, multiplies locally and disseminates systemically within 24 hours (Infect Dis Clin North Am 2013;27:705)
Etiology
- Treponema pallidum, highly motile coiled spirochete
Clinical features
- Primary syphilis: painless chancre with nontender lymphadenopathy 1 - 3 weeks after exposure
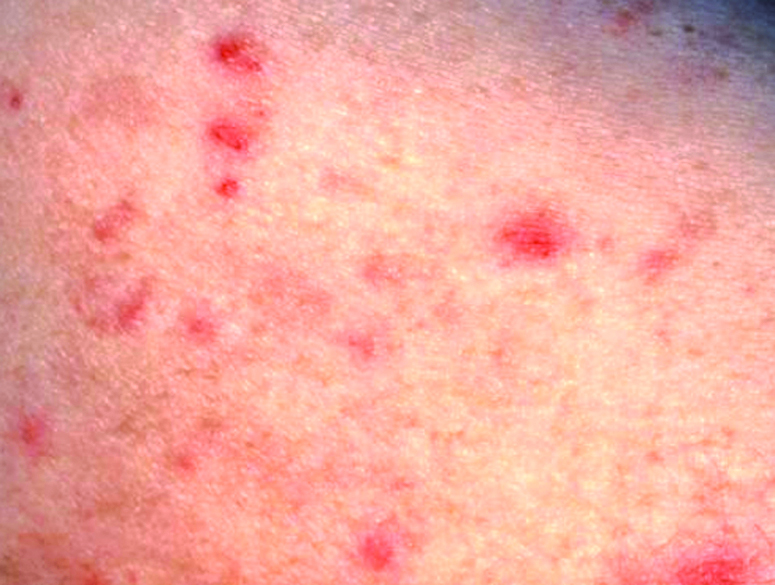
- Secondary syphilis:
- Papulosquamous thin papules on the trunk and extremities, palms and soles, fever and adenopathy
- Rash may resemble a drug eruption, pityriasis rosea and psoriasis
- May present as moth eaten alopecia on the scalp, mucous patches on tongue
- Tertiary syphilis: may present with gummatous lesions, neurologic or cardiovascular symptoms (Infect Dis Clin North Am 2013;27:705)
- Lymph node: solitary inguinal lymphadenopathy associated with syphilitic chancre
Diagnosis
- T. pallidum can be visualized using darkfield microscopy
- Blood and cerebrospinal fluid (CSF) analysis
- Skin biopsy for H&E, special stain and immunohistochemical analysis (Infect Dis Clin North Am 2013;27:705)
Laboratory
- Nontreponemal and treponemal tests are performed on blood serum
- Nontreponemal tests: rapid plasma reagin (RPR) test or venereal disease research laboratory (VDRL) test
- Treponemal tests: Treponema pallidum particle agglutination assay (TPPA) or fluorescent treponemal antibody absorption (FTA-ABS) test
- Cerebrospinal fluid (CSF) analysis
- Lymphocytic pleocytosis and elevated cerebrospinal fluid total protein
- Cerebrospinal fluid venereal disease research laboratory test confirms diagnosis of neurosyphilis
- Of note, cerebrospinal fluid fluorescent treponemal antibody absorption test has a high false positive rate but is more sensitive than cerebrospinal fluid venereal disease research laboratory test
Prognostic factors
- Favorable with early treatment
Case reports
- 27 year old man presents with recurrent oral ulcers (J Indian Acad Oral Med Radiol 2014;26:436)
- Man in his late 20s presented with a rash and multiple lytic lesions of the bones (BMJ Case Rep 2014 Sep 19;2014)
- 36 year old man with progressive vision loss (Case Rep Infect Dis 2014;2014:352047)
- 39 year old man presents with generalized weakness, joint aches (Cleve Clin J Med 2017;84:510)
- 59 year old man presents with ulcer of the hard palate (J Med Case Rep 2019;13:227)
Treatment
- Penicillin is the main drug of choice
- If a pregnant patient with syphilis is allergic to penicillin, an attempt should be made on penicillin desensitization with an allergist
- Other medications for nonpregnant adults are doxycycline, tetracycline and ceftriaxone (Infect Dis Clin North Am 2013;27:705, CDC: Syphilis [Accessed 11 December 2019])
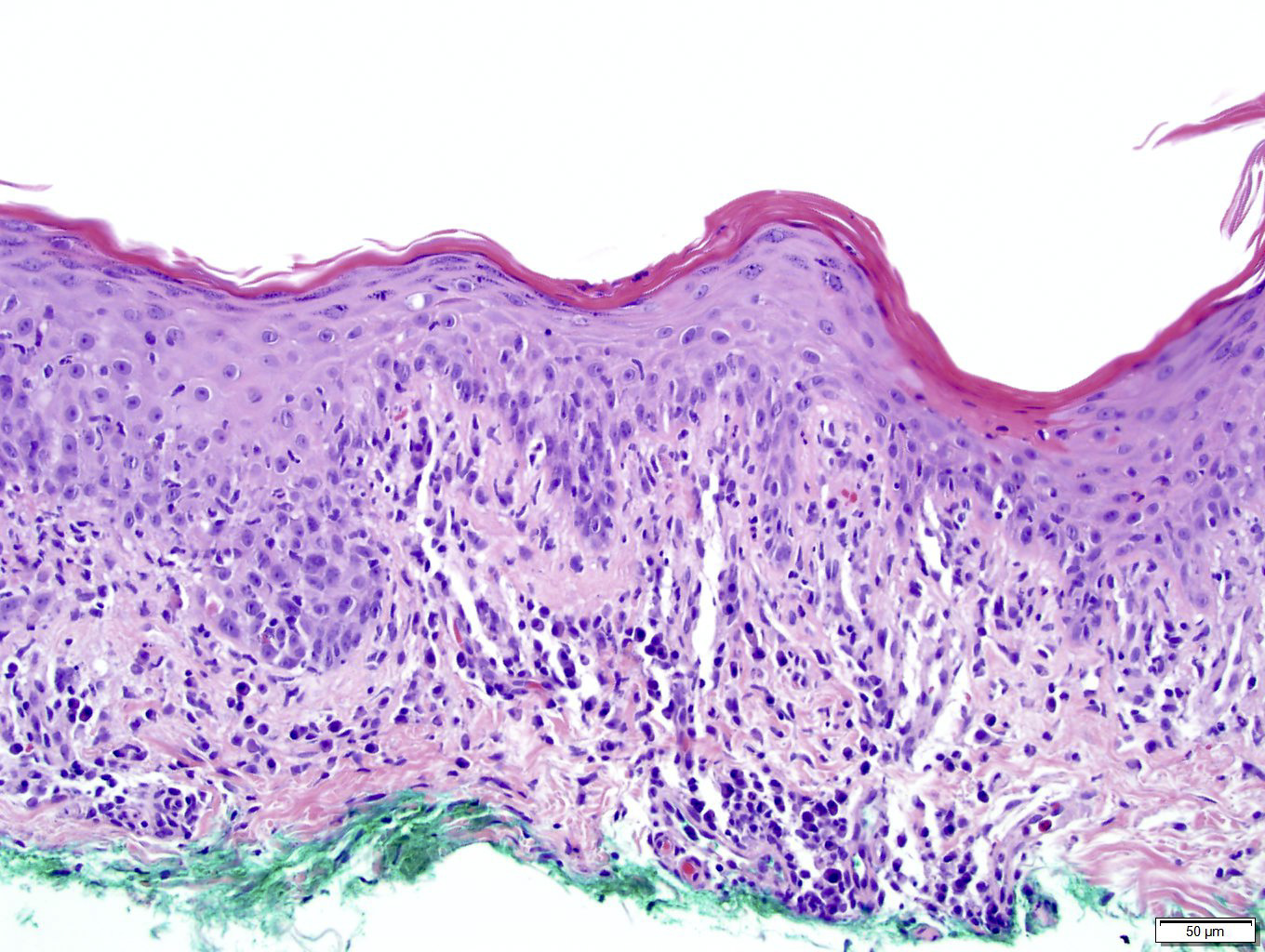
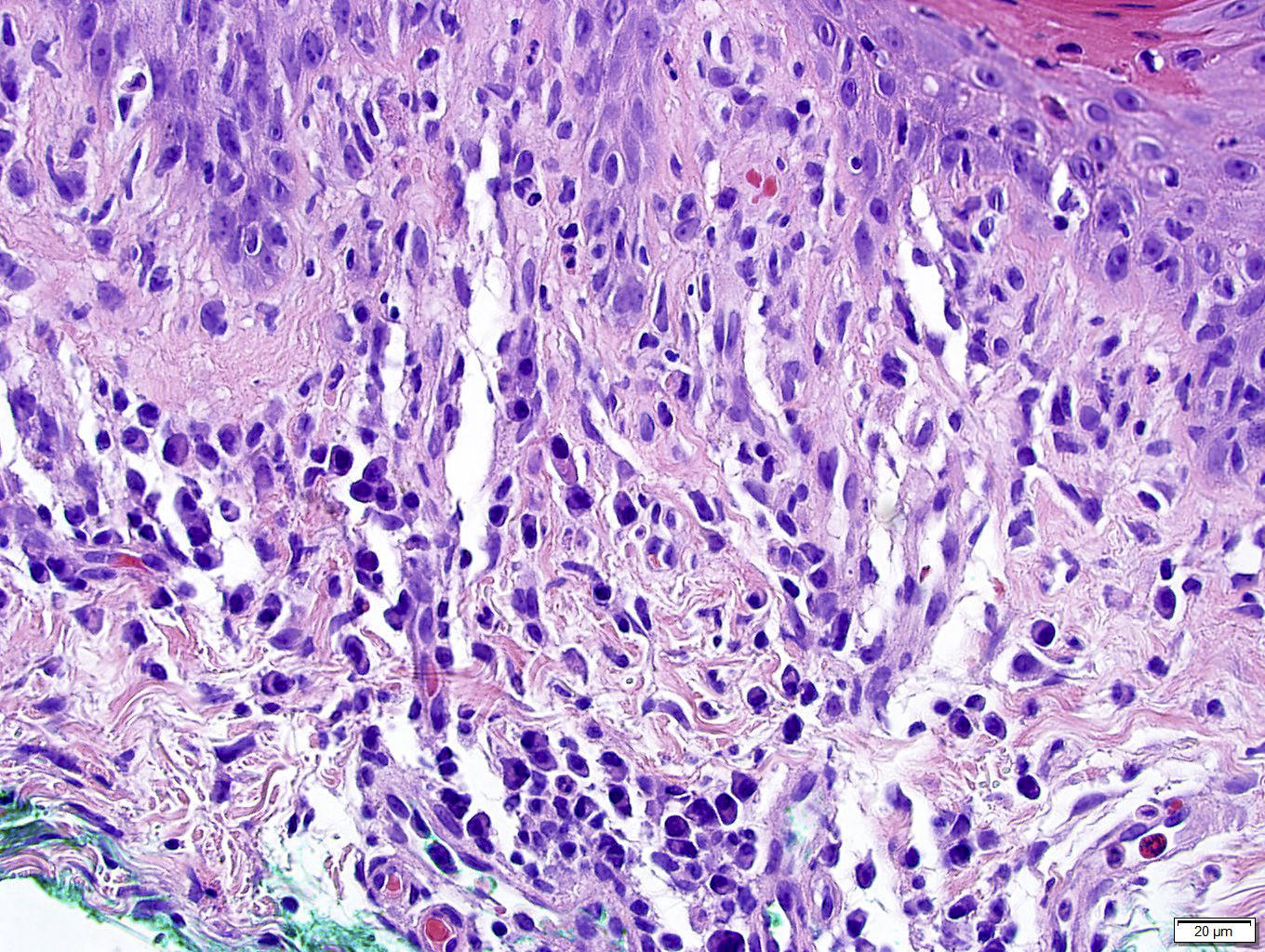
Microscopic (histologic) description
- Primary syphilis: ulcer with lymphoplasmacytic inflammation
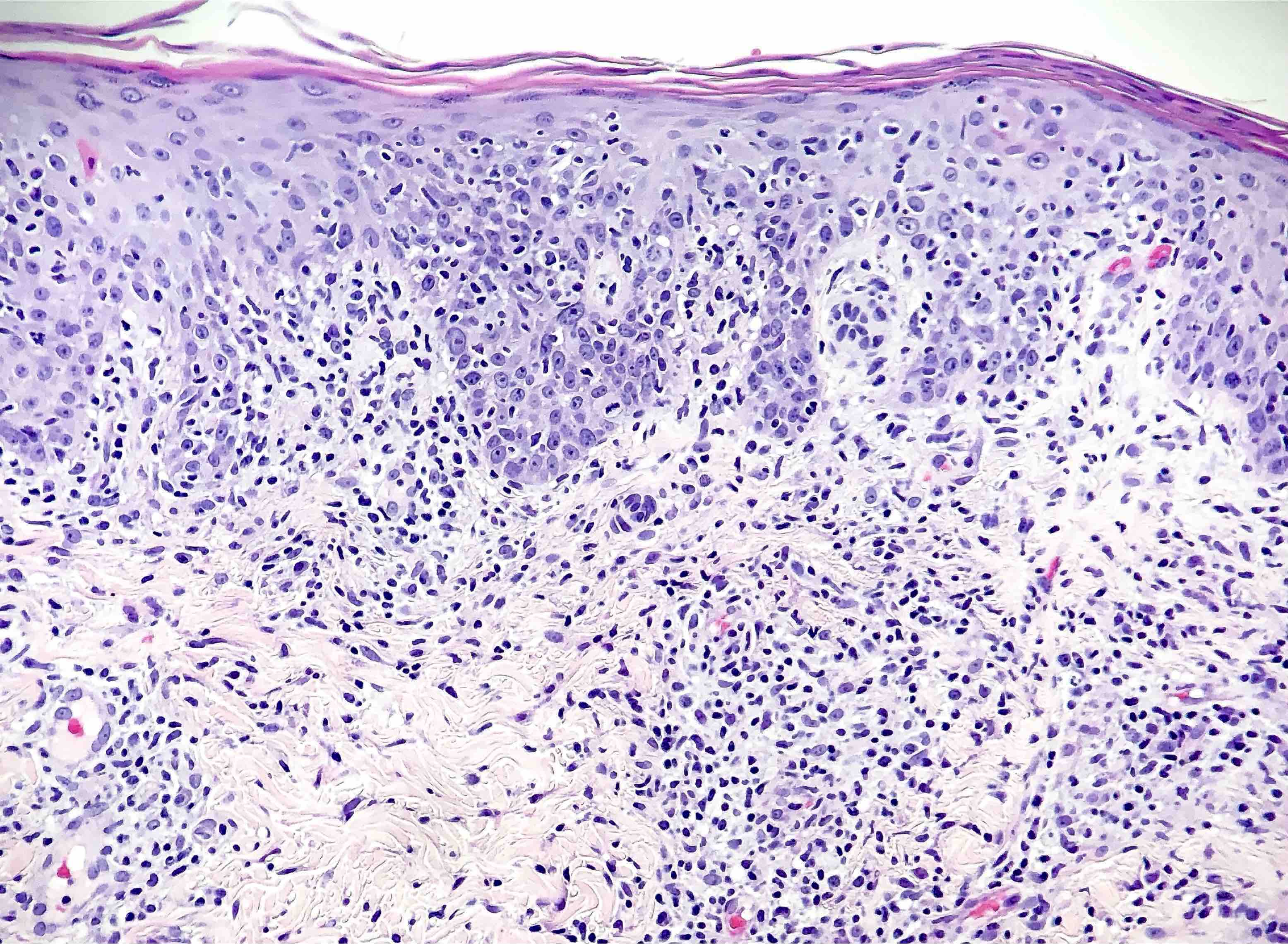
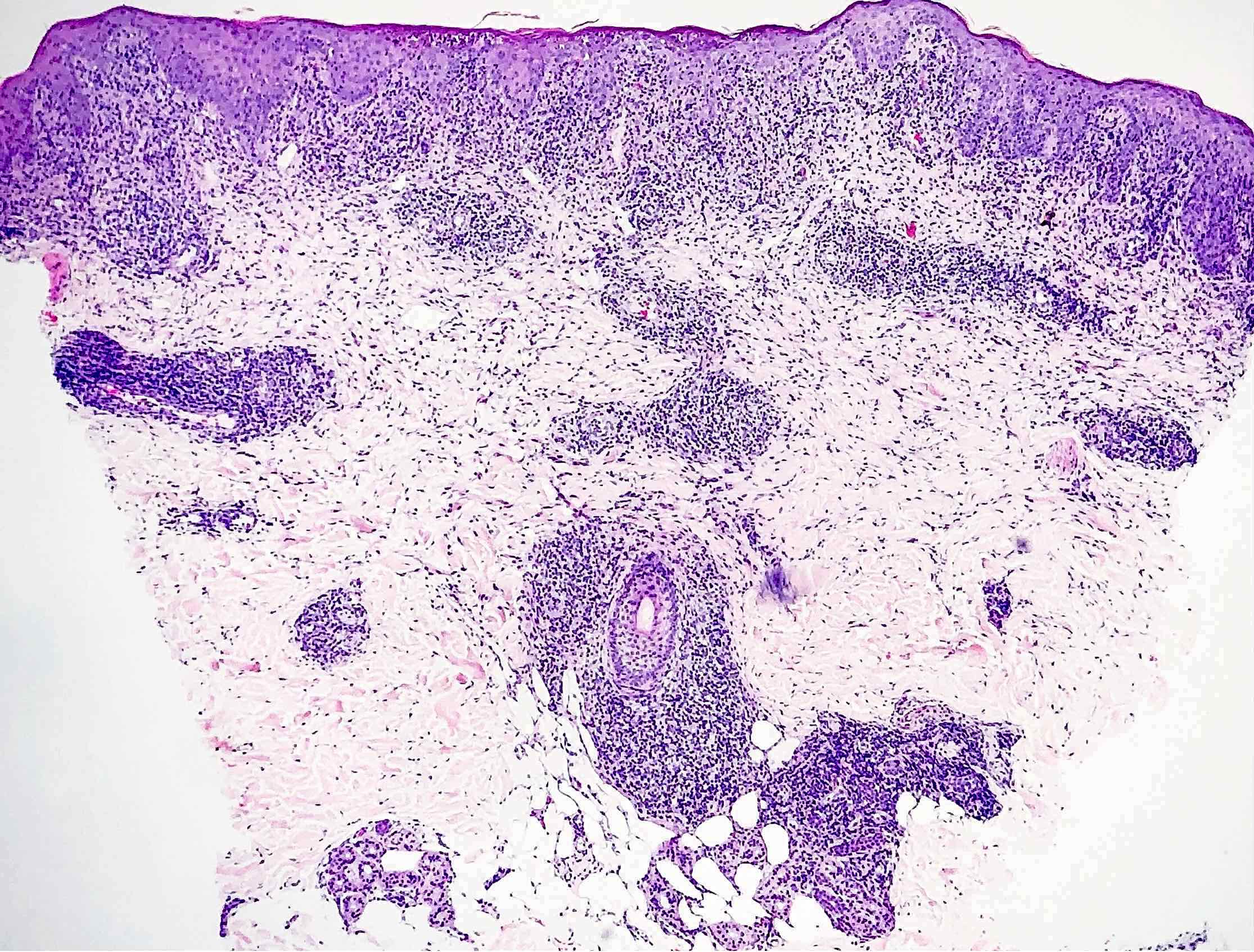
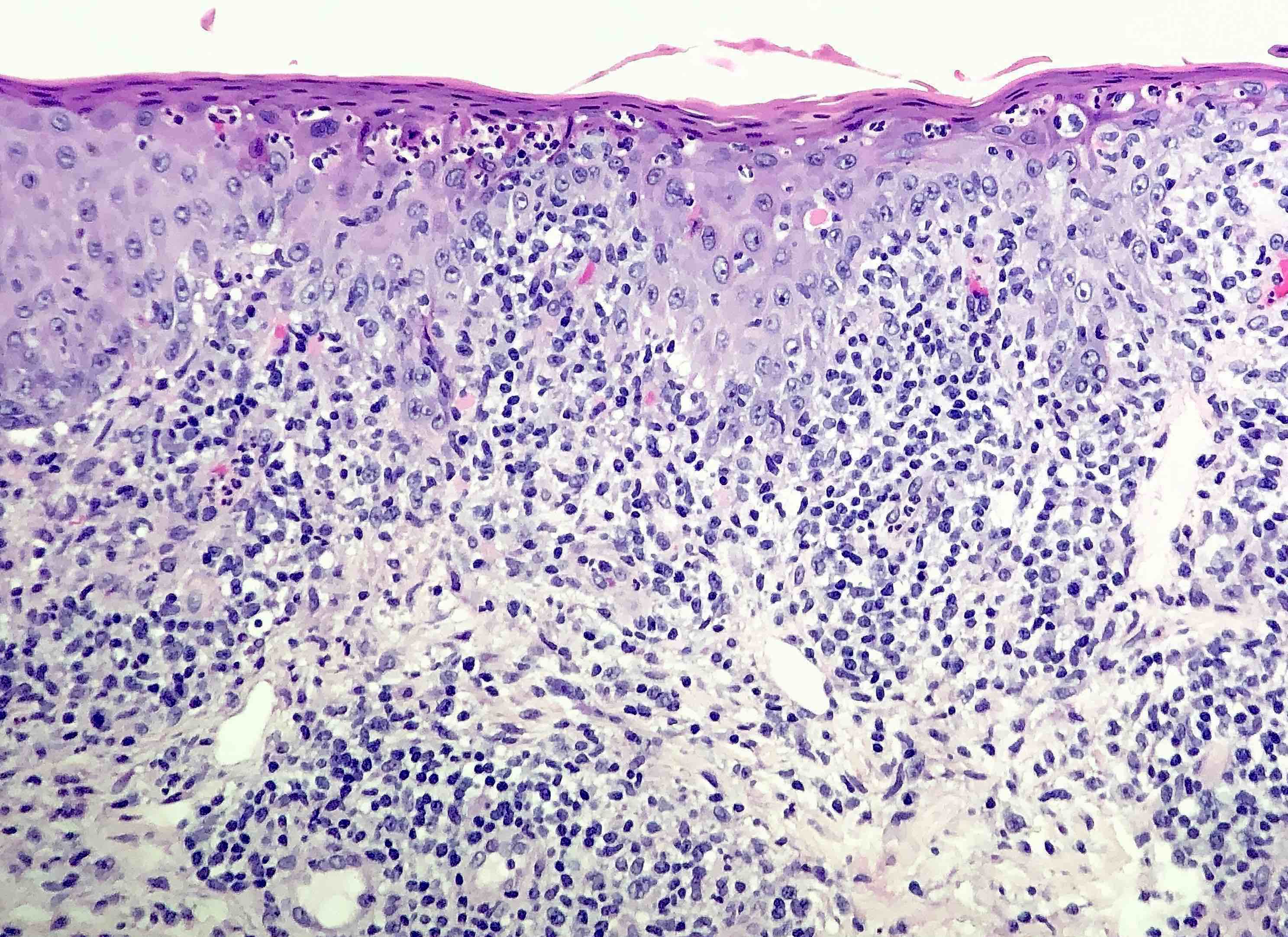
- Secondary syphilis:
- Lichenoid superficial and deep perivascular and periadnexal lymphohistiocytic inflammation with admixed plasma cells
- Plasma cells may be absent in 33% of biopsies
- Eosinophils can be present
- Marked endothelial swelling and proliferation of blood vessels can be seen
- Commonly identified are vacuolar interface change, acanthosis or lymphocyte exocytosis
- In late secondary syphilis, granulomatous inflammation may be present
- Microabscess formation of the hair follicle has also been seen
- Condyloma lata (lesions on genital skin) show marked epidermal hyperplasia and inflammatory infiltrate akin to secondary syphilis
- Tertiary syphilis: large areas of necrosis with peripheral mixed inflammatory infiltrate and Langhans giant cells
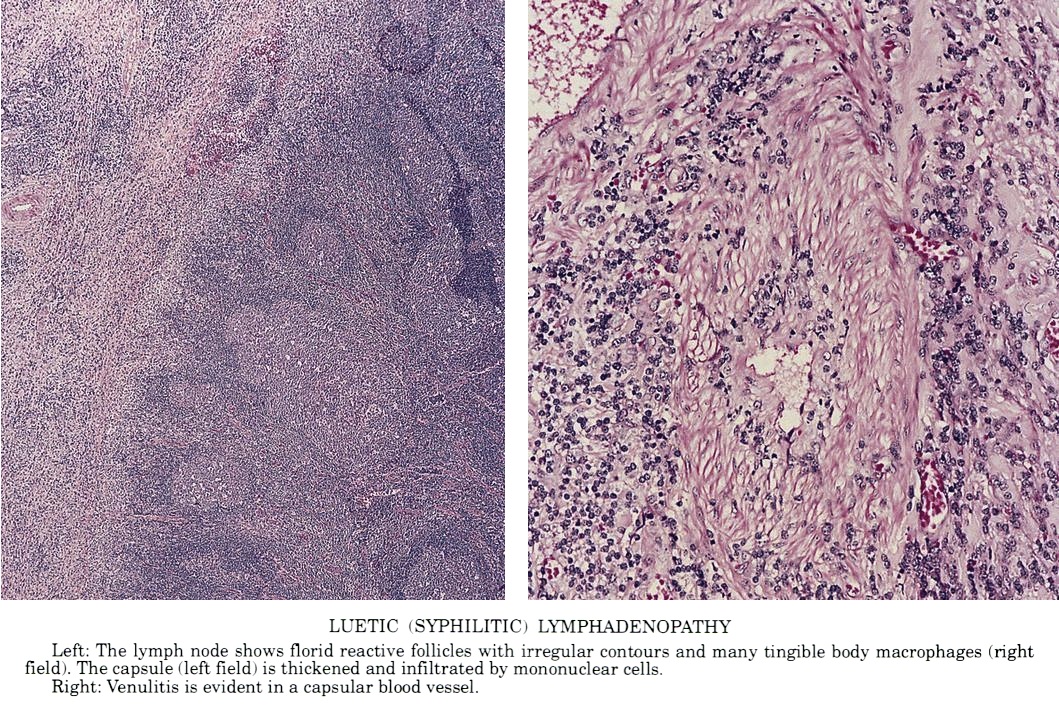
- Lymph node:
- Primary syphilis:
- Capsular and pericapsular fibrosis, follicular hyperplasia, diffuse interfollicular plasma cells, prominent endarteritis outside the capsule
- Noncaseating granulomas and abscesses are rare
- Spirochetes easiest to identify within blood vessel walls
- Secondary / tertiary syphilis: follicular hyperplasia
- Primary syphilis:
- References: J Cutan Pathol 2004;31:595, J Am Acad Dermatol 2015;73:1025, J Am Acad Dermatol 2020;82:156
Microscopic (histologic) images
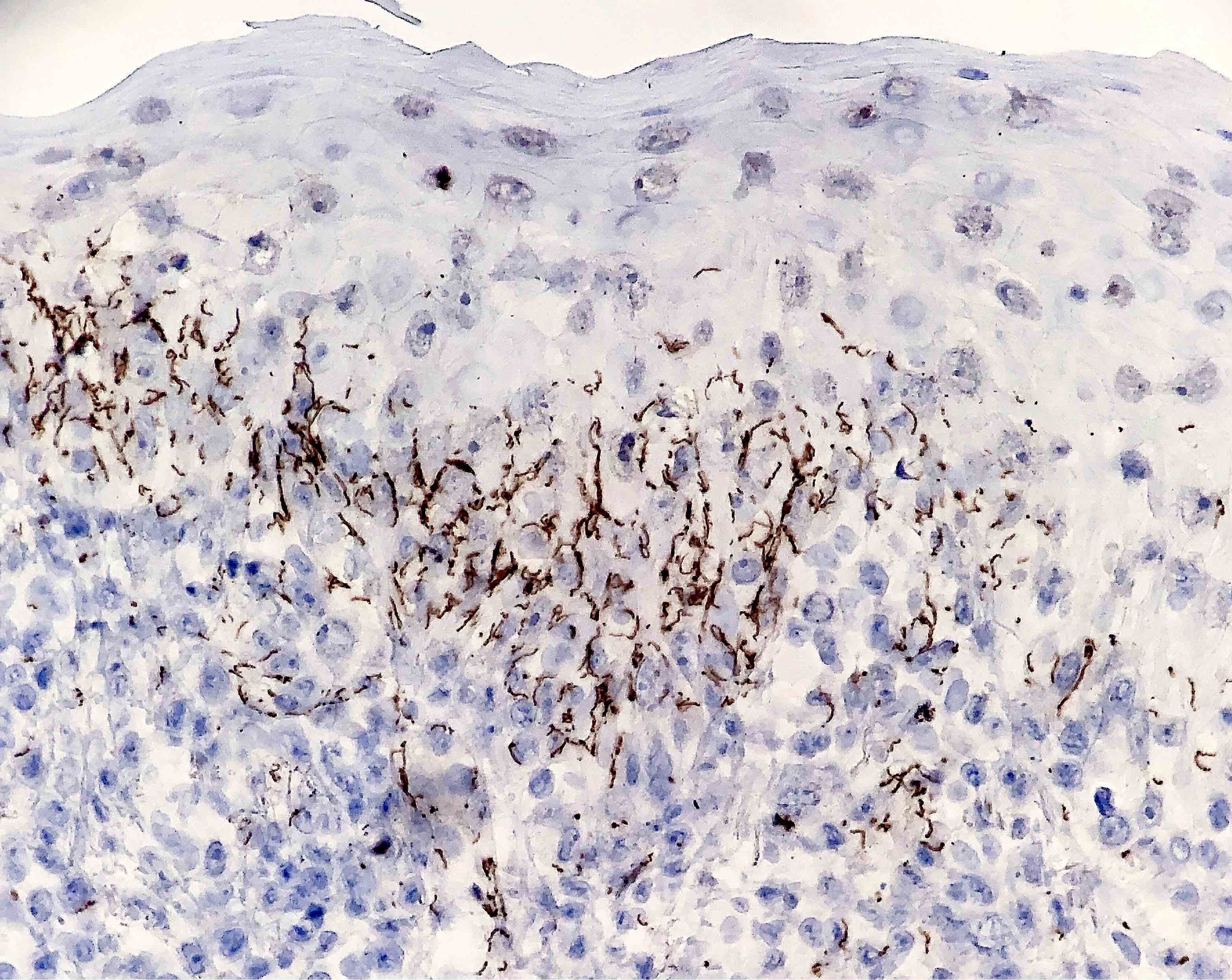
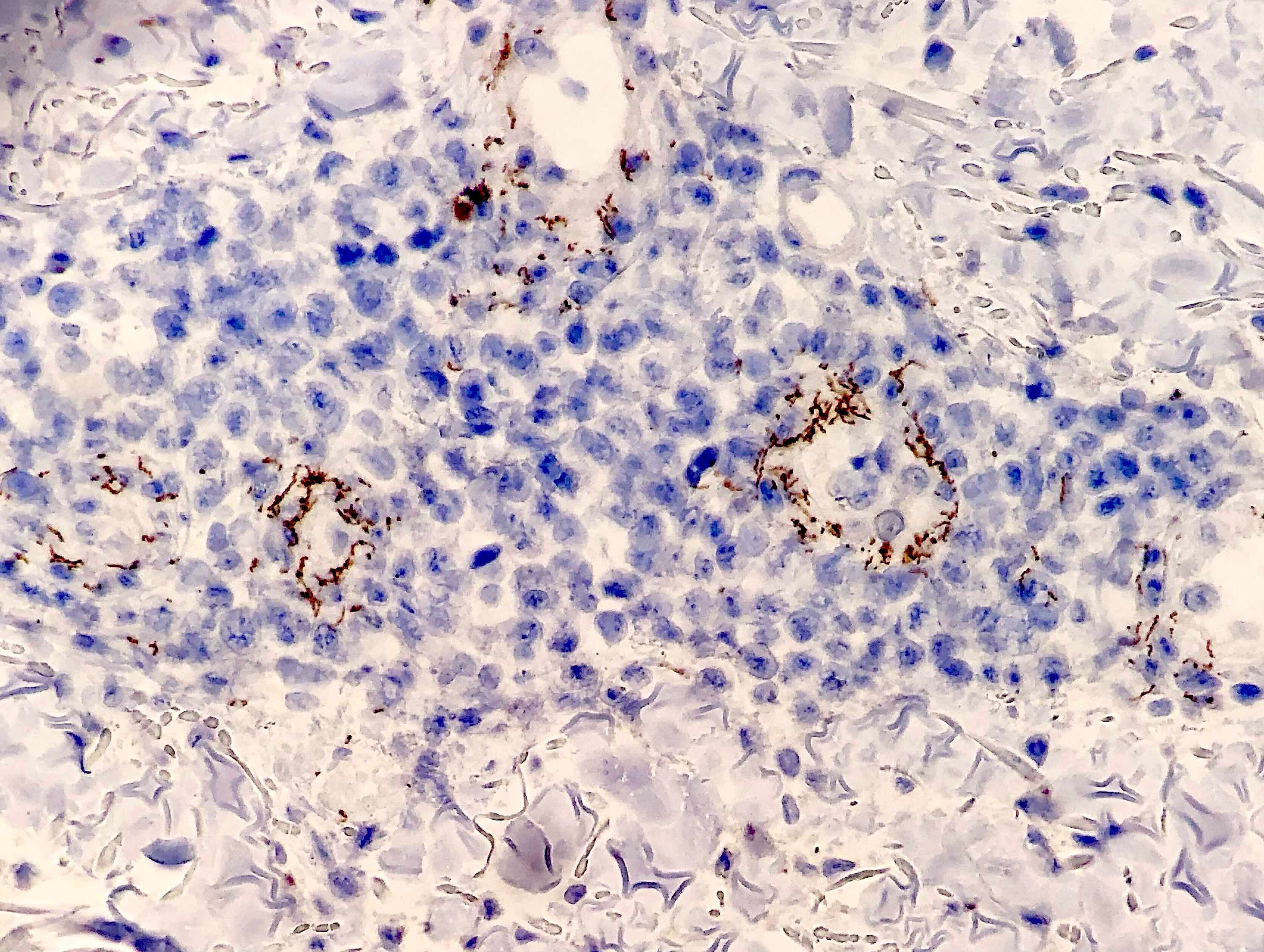
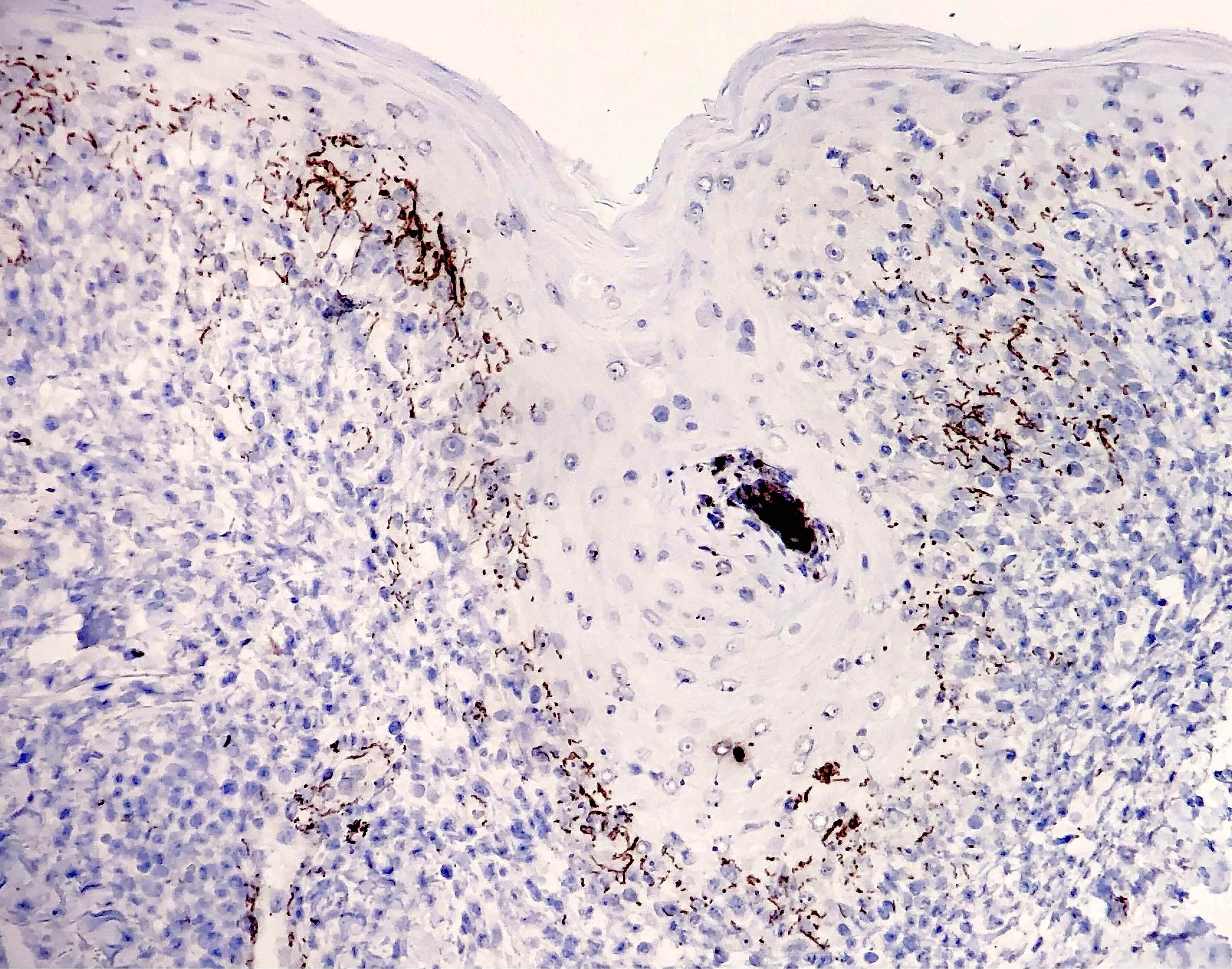
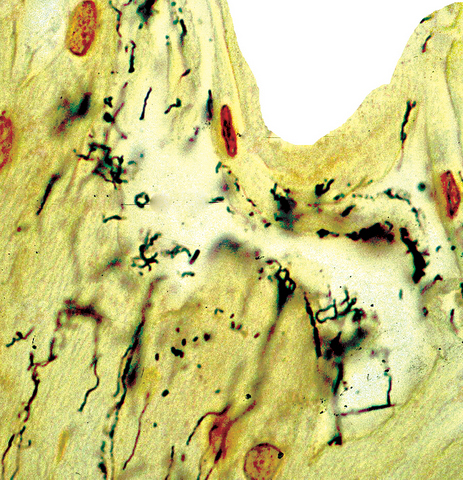
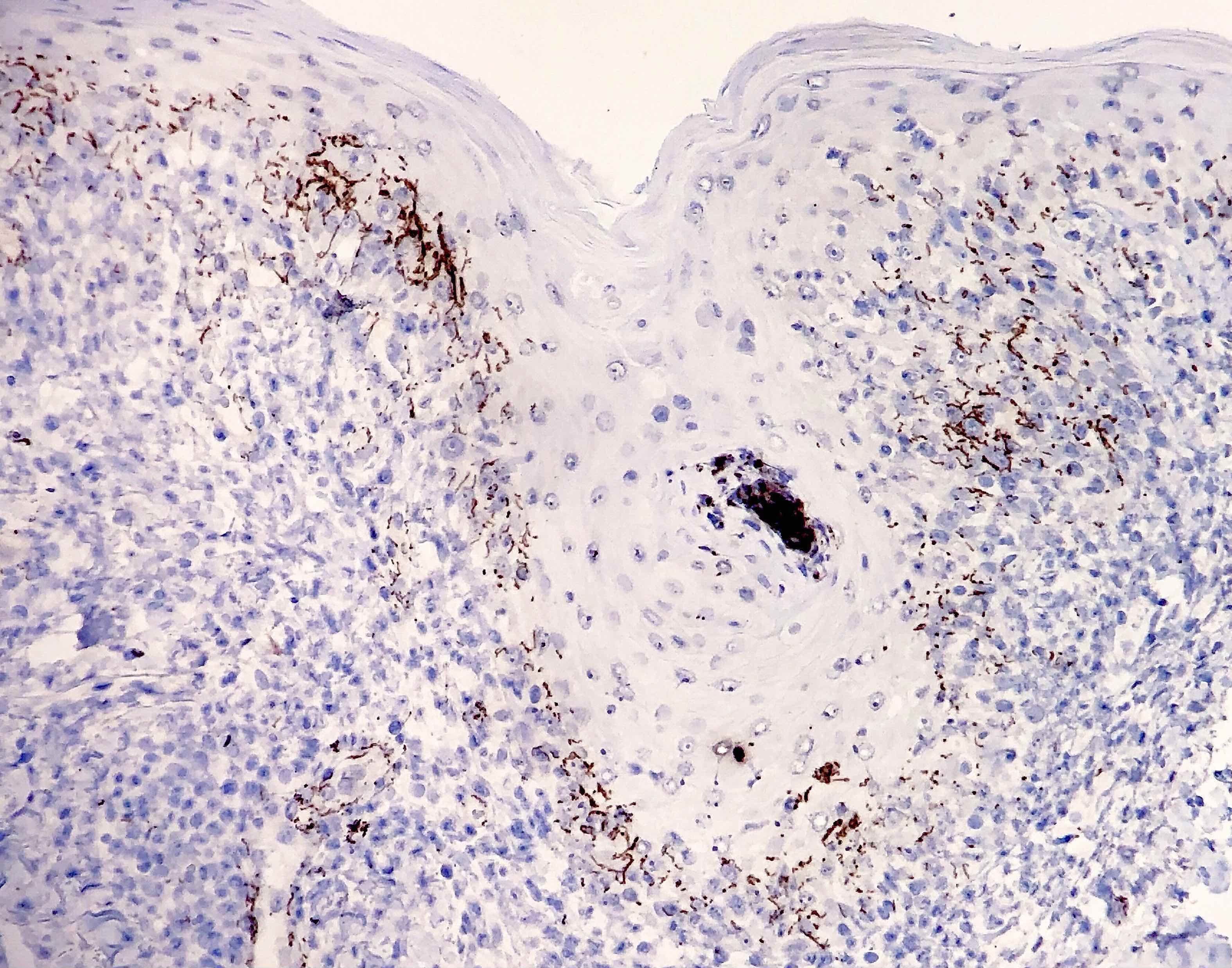
Contributed by Silvija P. Gottesman, M.D., Hillary Rose Elwood, M.D., Mark R. Wick, M.D. and AFIP images
Positive stains
- Silver stains: Warthin-Starry or Steiner stain (41% sensitive) (J Cutan Pathol 2004;31:595)
- Immunohistochemical stain: treponema (71% sensitive) (J Cutan Pathol 2004;31:595)
Negative stains
- Not relevant to the diagnosis
Molecular / cytogenetics description
- PCR based techniques can be used on tissue
Sample pathology report
- Skin, punch biopsy:
- Psoriasiform lymphohistiocytic inflammation with plasma cells (see comment)
- Comment: There is psoriasiform epidermal hyperplasia with superficial and deep perivascular lymphohistiocytic infiltrate. Admixed plasma cells are also noted. The infiltrate forms a band beneath the hyperplastic epidermis and envelopes some of the adnexal structures. Endothelial swelling of the superficial vascular plexus is present. A treponemal immunohistochemical stain shows numerous coiled spirochetes in the lower half of the epidermis. These findings are diagnostic of syphilis.
Differential diagnosis
- Pityriasis lichenoides et varioliformis acuta:
- Differentiation on histologic grounds is difficult as some cases may also have plasma cells
- Treponema-, silver-
- Pityriasis rosea:
- Similar clinically
- Basilar spongiosis and extravasated red blood cells are more likely
- Neutrophils in the stratum corneum are less common
- Mycosis fungoides:
- Papillary dermal fibrosis and complete vacuolar changes are more often seen
- While late lesions may have plasma cells, they are rarely seen in early lesions
- Alopecia areata:
- Also can show peribulbar lymphocytic inflammation
- Peribulbar plasma cells will not be present
Board review style question #1
A 28 year old man presents with fever, sore throat, lymphadenopathy and a skin rash. Which of the following is the most important cutaneous finding that should prompt suspicion of syphilis?
- Erythematous scaly papules on the palms and soles
- Genital mucocutaneous ulceration
- Maculopapular eruption on the trunk and extremities
- Mucosal patches on the bilateral oral commissures
Board review style answer #1
Board review style question #2
A punch biopsy specimen from a 26 year old woman with a rash shows superficial and deep perivascular and periadnexal lymphocytic inflammation. The presence of which of the following should prompt the pathologist to order treponemal immunohistochemical stain?
- Histiocytes
- Mucin
- Neutrophils
- Plasma cells
Board review style answer #2