Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lobos C, Mazzei ME. Subacute cutaneous lupus erythematosus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorsubacutelupus.html. Accessed April 3rd, 2025.
Definition / general
- Lupus erythematosus is an autoimmune disease that involves a pathological spectrum ranging from a skin limited disease to a severe multisystemic illness
- Skin lesions can be classified as specific (eruptions diagnostic of or unique to lupus erythematosus) and nonspecific (commonly seen in but not unique to lupus erythematosus) (J Am Acad Dermatol 1981;4:471)
- Specific skin lesions include acute, subacute and chronic cutaneous lupus erythematosus
Essential features
- Subacute cutaneous lupus erythematosus (SCLE) presents clinically as a photosensitive, nonscarring, nonatrophy producing eruption
- Associated anti-SSA / Ro autoantibodies (40 - 100%); anti-SSB / La antibodies are often present as well
- Drug induced in 30% of cases (Br J Dermatol 2012;167:296)
- 50% of patients can progress to systemic disease (An Bras Dermatol 2014;89:118)
- Microscopic features include vacuolar interface changes, apoptotic keratinocytes and superficial (or superficial and deep) perivascular lymphocytic infiltration; dyskeratotic keratinocytes can extend into upper spinous layers (this last feature is more specific to SCLE but is a rare finding)
- While certain microscopic features may suggest a particular subtype of cutaneous lupus erythematosus, significant overlap in histopathologic findings exist between subtypes and final diagnosis requires clinicopathologic and laboratory correlation
ICD coding
Epidemiology
- F > M (6:1)
- More frequent in young to middle aged women
- Neonatal forms of SCLE may occur in infants whose mothers have anti-SSA / Ro or U1RNP autoantibodies (Indian Dermatol Online J 2014;5:7)
Sites
- Sun exposed skin: face, V area of the neck, extensor surfaces of the arms and upper back
- Midface is usually spared (Indian Dermatol Online J 2014;5:7)
Pathophysiology
- Genetic predisposition, drug biotransformation and epigenetic dysregulation in different immune cells, NETosis and participation of the innate immune system (Curr Opin Rheumatol 2018;30:490)
- Adaptive immune system creates autoantibodies that react inaccurately to self antigens that are present in cellular debris after apoptosis; this process results in the activation and recruitment of B and T cells and the production of immune complexes, which cause direct tissue injury (Int J Womens Dermatol 2019;5:320)
- Photosensitivity is correlated with association to anti-SSA / Ro autoantibodies (~70%) (J Eur Acad Dermatol Venereol 2016;30:2097)
Etiology
- Often idiopathic
- Sun exposure (UVA and UVB)
- Drugs: 20 - 30% of cases are drug induced; at least 100 agents have been reported (terbinafine, TNFα inhibitors, antiepileptics and proton pump inhibitors are most frequently associated) (JAAD Case Rep 2019;5:271)
- Transplacental passage of autoantibodies (neonatal lupus erythematosus)
Clinical features
- Erythematous annular variant: raised pink-red borders and central clearing
- Papulosquamous variant: chronic psoriasiform or eczematous appearance (G Ital Dermatol Venereol 2018;153:216)
- Nonscarring, nonatrophic; commonly resolves with hypopigmentation
- Patient can have a mild systemic illness with musculoskeletal complaints and serological abnormalities
- Approximately 50% of patients with SCLE meet criteria for systemic lupus erythematosus; despite this SLE categorization, it is believed that these patients with SCLE / SLE have a lower incidence of severe central nervous system disease, renal disease and severe systemic vasculitis than patients with SLE without SCLE (J Am Acad Dermatol 2016;74:862)
- Concomitant Sjögren syndrome may occur due to shared presence of anti-SSA / Ro antibodies (Mayo Clin Proc 2017;92:406)
Diagnosis
- Clinicopathologic correlation is indispensable
- Blood tests: ANA, anti-Ro / SSA, anti-La / SSB, anti-dsDNA
- Skin biopsy
Laboratory
- ANA positive in 50 - 80% of patients with SCLE (J Am Acad Dermatol 2016;74:862)
- Anti-Ro / SSA (40 - 100%) > anti-La / SSB (15%); others: anti-dsDNA (5 - 24%), anti-Sm (7 - 18%) (Histopathology 2022;80:233)
- 50% fulfill 4 or more classification criteria for systemic lupus erythematosus (Clin Dermatol 2018;36:442)
Prognostic factors
- 3 out of 10 patients can develop systemic disease (Br J Dermatol 2010;162:91)
- Although SCLE patients frequently have cytopenias, they rarely progress to clinically significant renal or central nervous system disease (Clin Dermatol 2018;36:442)
Case reports
- 40 year old woman with Sjögren syndrome with terbinafine induced SCLE (Acta Reumatol Port 2020;45:288)
- 68 year old woman with plaque psoriasis with ustekinumab induced SCLE (JAAD Case Rep 2019;5:271)
- 75 year old woman with metastatic ovarian carcinoma, with checkpoint inhibitor immunotherapy induced SCLE (Dermatol Online J 2019;25:13030)
- 80 year old man with omeprazole induced SCLE (JAMA Dermatol 2020;156:1013)
Treatment
- Sun protection
- Topical corticosteroids
- Antimalarial therapy (Br J Dermatol 2011;164:465)
- Systemic corticosteroids and other immunosuppressants are indicated when there are other organs involved (Int J Dermatol 2006;45:320)
Clinical images
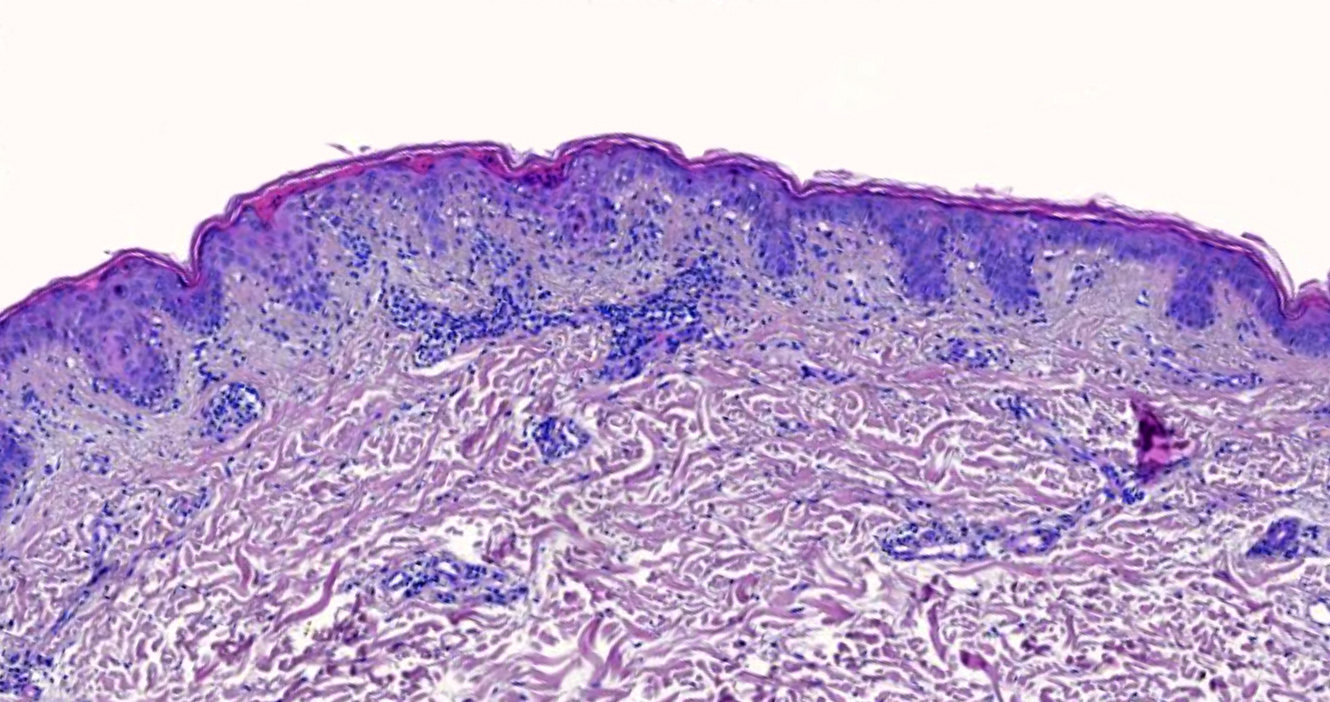
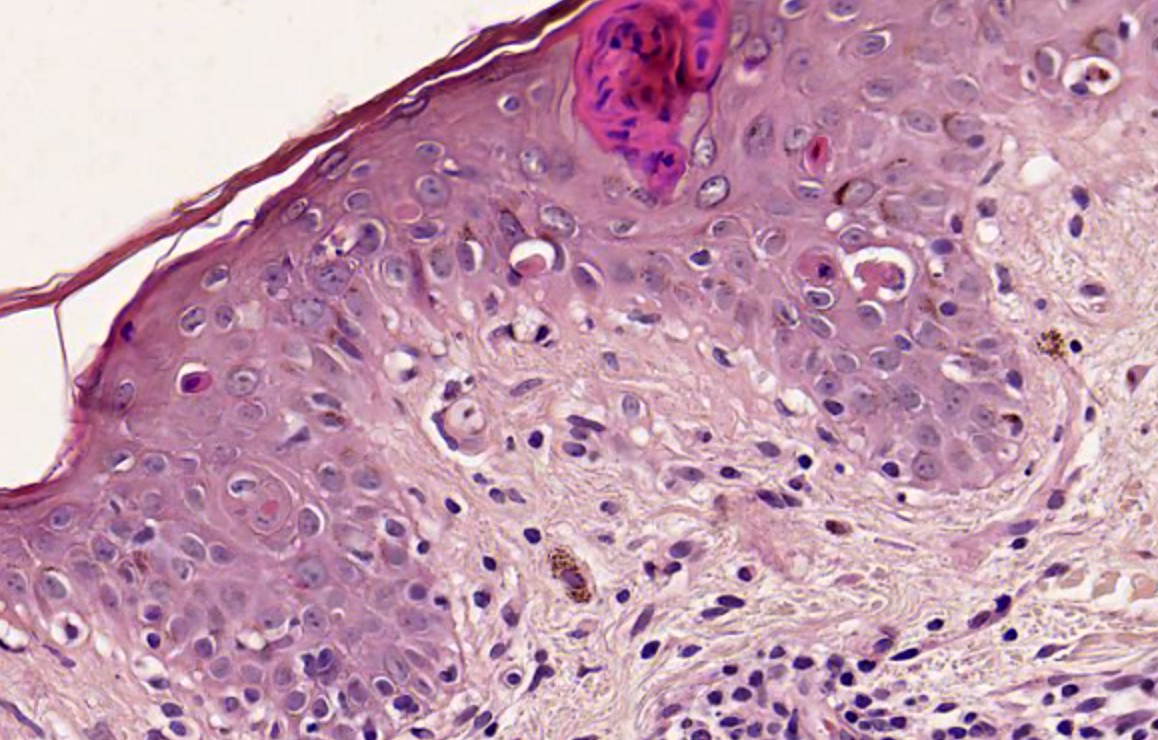
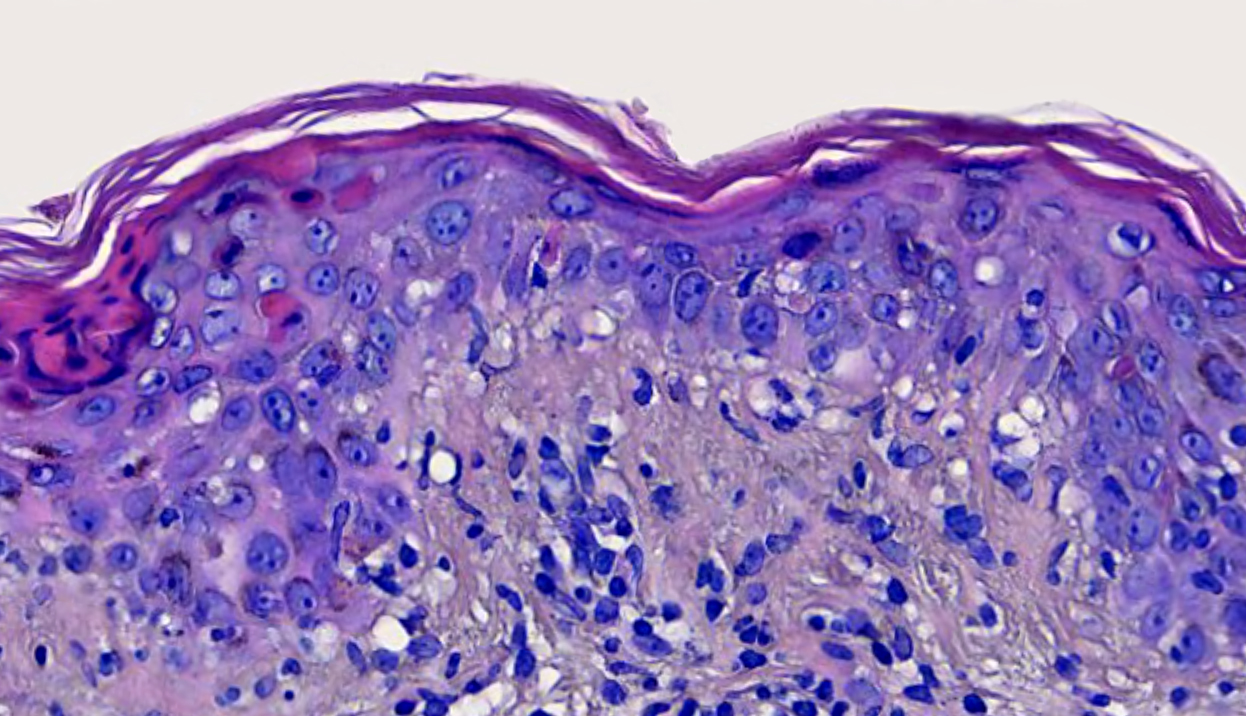
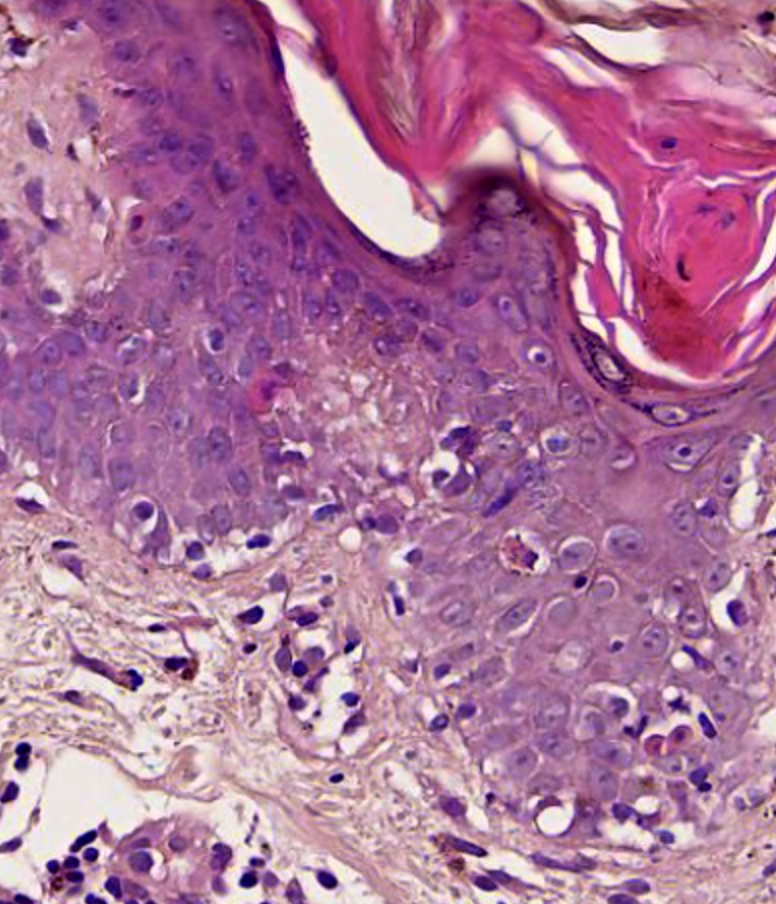
Microscopic (histologic) description
- Interface dermatitis with variable degrees of basal layer vacuolization and scattered cytoid bodies (Lupus 2012;21:577)
- Occasionally, basal layer vacuolation and keratinocyte apoptosis may be so severe that full thickness epidermal necrosis may result, generating a differential diagnosis of erythema multiforme
- Erythema multiforme-like lesions may occur, showing exuberant interface tissue reaction (Rowell syndrome)
- Dyskeratotic keratinocytes extending into upper spinous layers is a very characteristic but rare finding of SCLE (J Cutan Pathol 2001;28:1)
- Hyperkeratosis / parakeratosis may be present
- Sometimes focal hypergranulosis
- Superficial and sometimes superficial and deep perivascular lymphocytic infiltrate (Dermatol Ther (Heidelb) 2021;11:131)
- Periadnexal mononuclear cell infiltrate may be present (Dermatol Ther 2021;11:131)
- Dermal mucin, which may be highlighted with Alcian blue or colloidal iron
- Compared with idiopathic SCLE, drug induced variants are more commonly associated with leukocytoclastic vasculitis and have less mucin deposition (J Am Acad Dermatol 2019;81:403)
- Epidermal atrophy, follicular plugging, basement membrane thickening, dermal mucin and pigment incontinence may be present but less prominent than in chronic lupus erythematosus
Microscopic (histologic) images
Immunofluorescence description
- Immunofluorescence is not regularly used to confirm the diagnosis; however, it might help when a clinicopathological correlation is lacking
- Direct immunofluorescence: continuous granular deposition of IgG, IgM and C3 along the dermal epidermal junction (J Invest Dermatol 1992;99:251)
- Lupus band: 65 - 80% of lesional skin and 20% nonlesional skin (Histopathology 2022;80:233)
Sample pathology report
- Skin, arm, biopsy:
- Cutaneous lupus erythematosus (see comment)
- Comment: Epidermal thinning with hyperkeratosis. Vacuolar interface dermatitis with dyskeratotic keratinocytes that extend into upper spinous layers. Superficial perivascular lymphocytic infiltrate. Correlate with clinical and laboratory testing. These findings are more consistent with SCLE subtype.
Differential diagnosis
- Acute lupus erythematosus:
- Specific lesions include central face malar violaceous erythema that resolves without scarring (butterfly rash), photosensitive maculopapular rash, blistering rash (acute toxic epidermal necrolysis-like ACLE due to extensive interface dermatitis) mainly in photo exposed areas, mucosal erosions and ulcerations
- Histopathology shows vacuolar interface dermatitis with relatively mild lymphocytic inflammation; there may be dermal edema and microhemorrhage
- Chronic cutaneous lupus:
- Erythematous and scaly plaques located mainly in the face and scalp, that may lead to scarring / alopecia if not treated
- Microscopic findings include epidermal atrophy, hyperparakeratosis, follicular keratotic plugging and basement membrane thickening with vacuolar interface changes
- Additionally, the density of the infiltrate tends to be heaviest in chronic cutaneous lupus
- Dermatomyositis:
- Heliotrope rash, swelling of the eyelids, shawl sign, Gottron papules, photosensitive rash, Gottron sign, holster sign, mechanic hands and Raynaud phenomenon
- Microscopic findings include interface dermatitis that can resemble lupus erythematosus, increased dermal mucin, sparse perivascular lymphocytic infiltrate
- Erythema multiforme:
- Triggered by infections (mainly herpes simplex virus), medications, vaccines
- Round, erythematous papules, which later develop into target lesions: central area with epidermal necrosis surrounded by a lighter edematous area with a peripheral erythematous margin
- Microscopic changes include interface changes with mild to moderate infiltrate of lymphocytes; there may also be subepidermal bullae and epidermal necrosis
Board review style question #1
A 35 year old woman presents with multiple nonscarring erythematous annular plaques that arise in photo exposed areas 8 weeks after introducing terbinafine for treatment of onychomycosis. A biopsy of one of the lesions was performed (shown above). What is the most likely diagnosis?
- Chronic lupus erythematosus
- Dermatomyositis
- Erythema multiforme
- Stevens-Johnson syndrome
- Subacute cutaneous lupus erythematosus
Board review style answer #1
E. Subacute cutaneous lupus erythematosus
Comment Here
Reference: Subacute cutaneous lupus erythematosus
Comment Here
Reference: Subacute cutaneous lupus erythematosus
Board review style question #2
A 50 year old man with a history of recent onset hypertension treated with enalapril presented with a 1 month history of annular and erythematous polycyclic plaques with peripheral scale that were located in sun exposed areas. No other systemic manifestations were found. Serologic test results were positive for ANA, anti-Ro / SSA and anti-La / SSB, while negative for ds-DNA, anti-histone and anti-Smith. Which histopathological finding that can be seen in this image is more characteristic of the patient's clinical type?
- Dyskeratotic keratinocytes extending to upper layers
- Epidermal atrophy
- Pigment incontinence
- Superficial perivascular lymphocytic infiltrate
- Vacuolar interface dermatitis
Board review style answer #2
A. Dyskeratotic keratinocytes extending to upper layers
Comment Here
Reference: Subacute cutaneous lupus erythematosus
Comment Here
Reference: Subacute cutaneous lupus erythematosus