Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesCite this page: Carlquist EM, Stuart LN, Gardner JM. Stevens-Johnson syndrome. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorstevensjohnsonsyndrome.html. Accessed March 31st, 2025.
Definition / general
- Historically there has been controversy as to whether Stevens-Johnson syndrome (SJS) is a distinct entity or at the center of the disease spectrum that includes erythema multiforme (EM) and toxic epidermal necrolysis (TEN)
- Currently, there is an increasing trend for SJS and TEN as representing the ends of a spectrum of severe epidermolytic adverse cutaneous drug reactions (Orphanet J Rare Dis 2010;5:39)
Terminology
- SJS: keratinocyte necrosis; epidermal detachment < 10% body surface area; the beginning of the spectrum (Orphanet J Rare Dis 2010;5:39)
- SJS / TEN: considered point of overlap of two diseases in patients with 10 - 30% body surface area epidermal detachment (N Engl J Med 1994;331:1272)
- TEN: severe disease state and the end of a spectrum of epidermolytic adverse cutaneous drug reactions; full thickness epidermal necrosis; epidermal detachment > 30% body surface area (Orphanet J Rare Dis 2010;5:39)
- Atypical SJS: referred to by some as severe mucositis with Mycoplasma pneumoniae infection but without skin lesions (Pediatrics 2007;119:e1002), while others argue that the classification of SJS requires cutaneous involvement (Pediatr Dermatol 2006;23:546)
Epidemiology
- Incidence: 1.2 - 6 per million persons per year (Allergol Int 2006;55:9)
- Increased incidence with HIV (Orphanet J Rare Dis 2010;5:39)
Sites
- Lesions usually begin on trunk and spread centrifugally
Pathophysiology
- Mechanism unknown but appears to be CD8+ T cell mediated immune reaction (J Allergy Clin Immunol 2011;127:S74)
- Granulysin, a mitochondrial protein, is most important factor in epidermal destruction; is found in blister fluid in increasing concentrations with increased severity of disease (Nat Med 2008;14:1343)
Etiology
- Cases in children are usually associated with infection, especially Mycoplasma pneumonia and herpes simplex virus
- In adults, most cases are due to medications, including:
- Allopurinol (most common cause of SJS and TEN in study of 379 patients in Europe / Israel) (J Am Acad Dermatol 2008;58:25)
- Antibiotics: sulfonamides, cephalosporins, quinolones, aminopenicillins (Orphanet J Rare Dis 2010;5:39)
- Nonsteroidal anti inflammatory drugs (NSAIDs)
- Anticonvulsants: carbamazepine, phenytoin, phenobarbital (Orphanet J Rare Dis 2010;5:39)
- Corticosteroids
- ALDEN (algorithm for assessment of drug causality in SJS and TEN) provides a structured approach to determine the responsible drug (Clin Pharmacol Ther 2010;88:60), although no identifiable cause in some cases (Orphanet J Rare Dis 2010;5:39)
Diagrams / tables
Clinical features
- Drug associated cases typically present one to three weeks following initiation of therapy with the offending drug; occurs more rapidly with re-challenge (N Engl J Med 1994;331:1272)
- Fever, malaise, cutaneous and mucosal eruption
- Cutaneous and mucosal lesions are tender
- Nikolsky sign positive for epidermal detachment with application of tangential mechanical pressure (Orphanet J Rare Dis 2010;5:39)
- Eruption consists of either "flat atypical target" lesions or erythematous to purpuric macules, many with central epidermal necrosis or blister formation
- Epidermal detachment < 10% body surface area
- Variable GI and respiratory tract involvement (Orphanet J Rare Dis 2010;5:39)
- Potentially fatal, a medical emergency
Diagnosis
- Based on clinical picture plus confirmatory skin biopsy showing vacuolar interface alteration, often with epidermal necrolysis (Orphanet J Rare Dis 2010;5:39)
Prognostic factors
- Mortality rate 1 - 5%; rises with increasing surface area of epidermal detachment; higher in elderly (Orphanet J Rare Dis 2010;5:39)
- SCORTEN scoring system is used to rapidly evaluate risk and prognosis (J Invest Dermatol 2000;115:149)
- One study of 27 patients suggested Mycoplasma related disease has a less severe course than drug related cases (Mayo Clin Proc 2010;85:131)
Case reports
- 3.5 year old girl with severe gynecologic sequelae of Stevens-Johnson syndrome and toxic epidermal necrolysis (J Reprod Med 2013;58:354)
- 12 year old boy with Mycoplasma pneumoniae induced recurrent Stevens-Johnson syndrome (Pediatr Dermatol 2013;30:624)
- 19 year old woman with photo induced Stevens-Johnson syndrome (J Am Acad Dermatol 2014;71:e82)
- 19 and 36 year old women with Stevens-Johnson syndrome associated with sulfasalazine (J Crohns Colitis 2011;5:457)
- 28 year old man with Stevens-Johnson syndrome associated with furosemide (J Pharm Pract 2010;23:367)
- 49 year old man with doxycycline-induced Stevens-Johnson syndrome (Cornea 2011;30:595)
- 53 year old woman with Stevens-Johnson syndrome associated with adalimumab (Rheumatol Int 2013;33:1351)
- Associated with sorafenib for metastatic renal cell carcinoma (Urol Int 2013;91:482)
- Colonic involvement in Stevens-Johnson syndrome (Dig Endosc 2012;24:382)
- 14 adult cases (Ann Allergy Asthma Immunol 2013;110:207)
Treatment
- Withdrawal of all potential medication triggers, especially medications which have been initiated within the past four weeks (Semin Cutan Med Surg 2014;33:10)
- Primarily supportive and symptom targeted (Semin Cutan Med Surg 2014;33:10)
Gross description
- Cutaneous and mucosal lesions
- Eruption consists of either "flat atypical target" lesions or erythematous to purpuric macules, many with central epidermal necrosis or blister formation
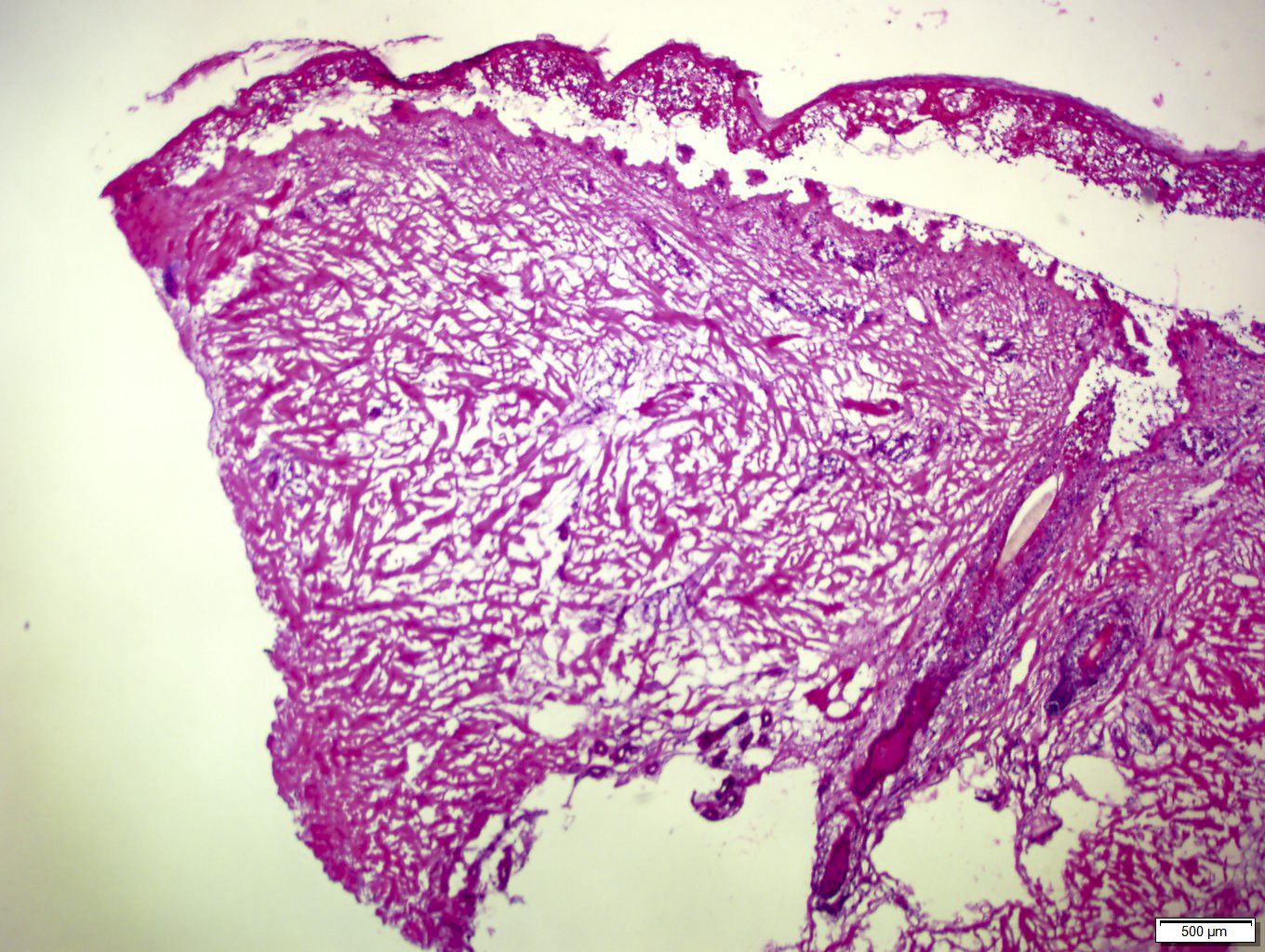
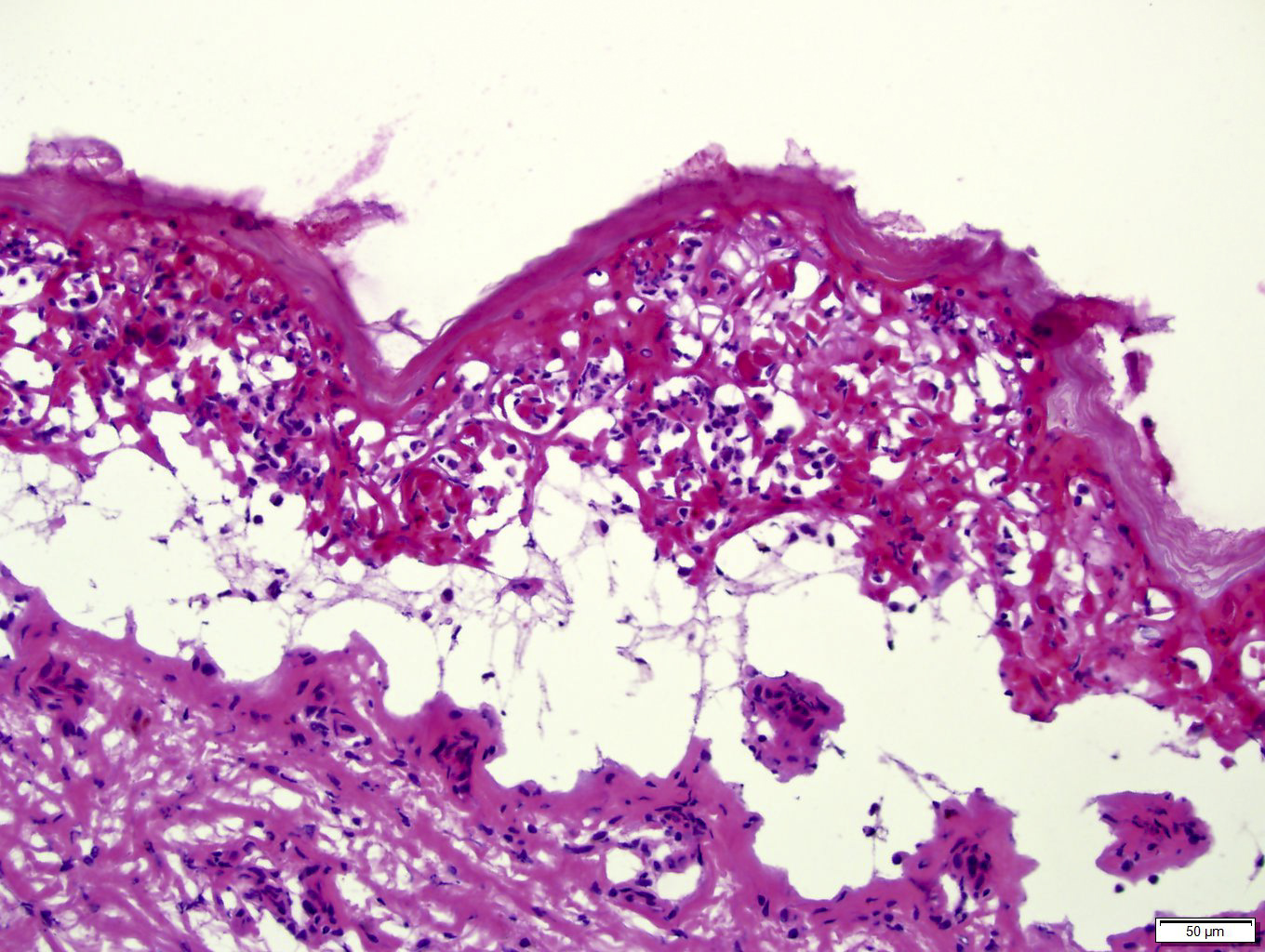
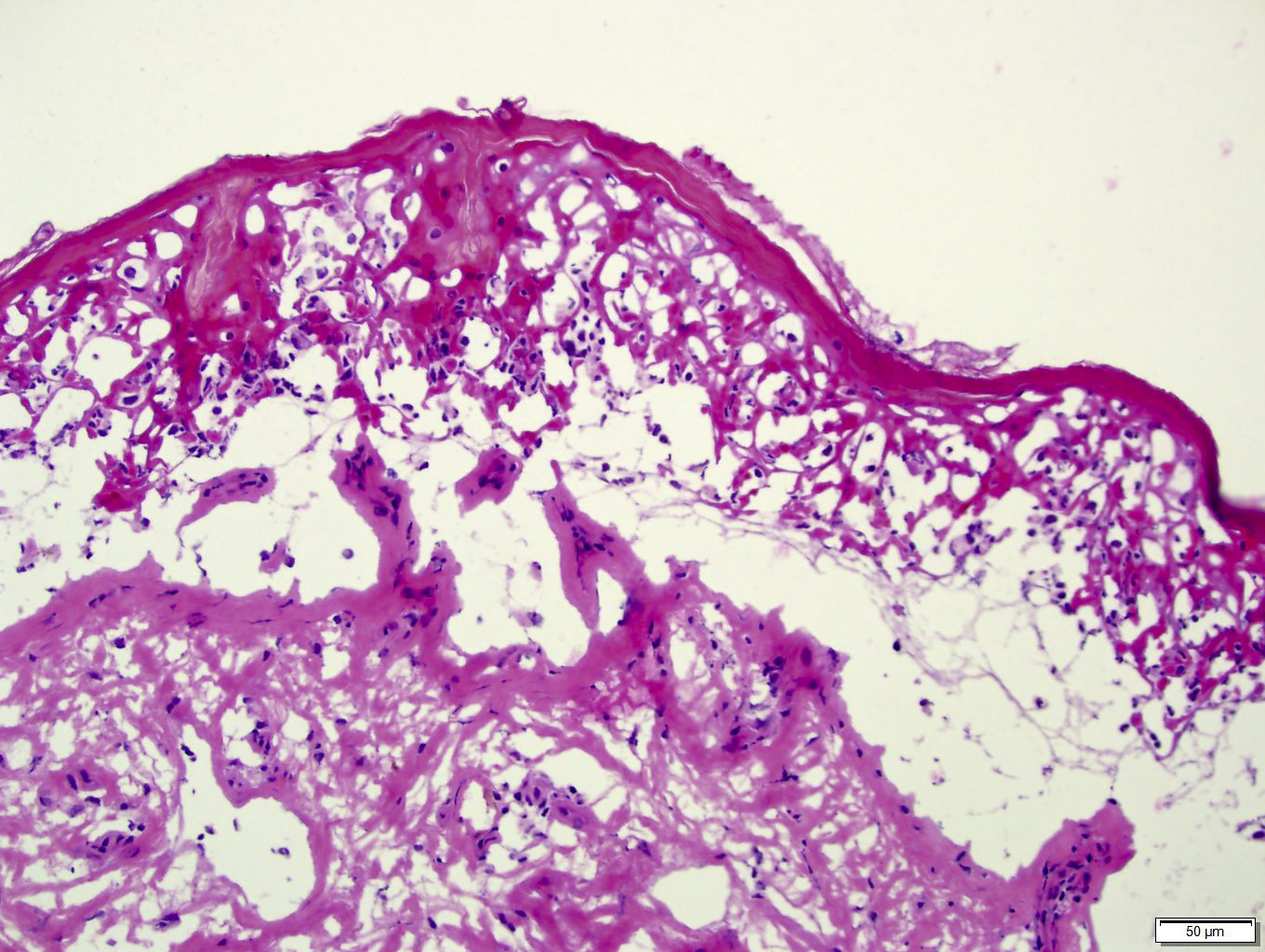
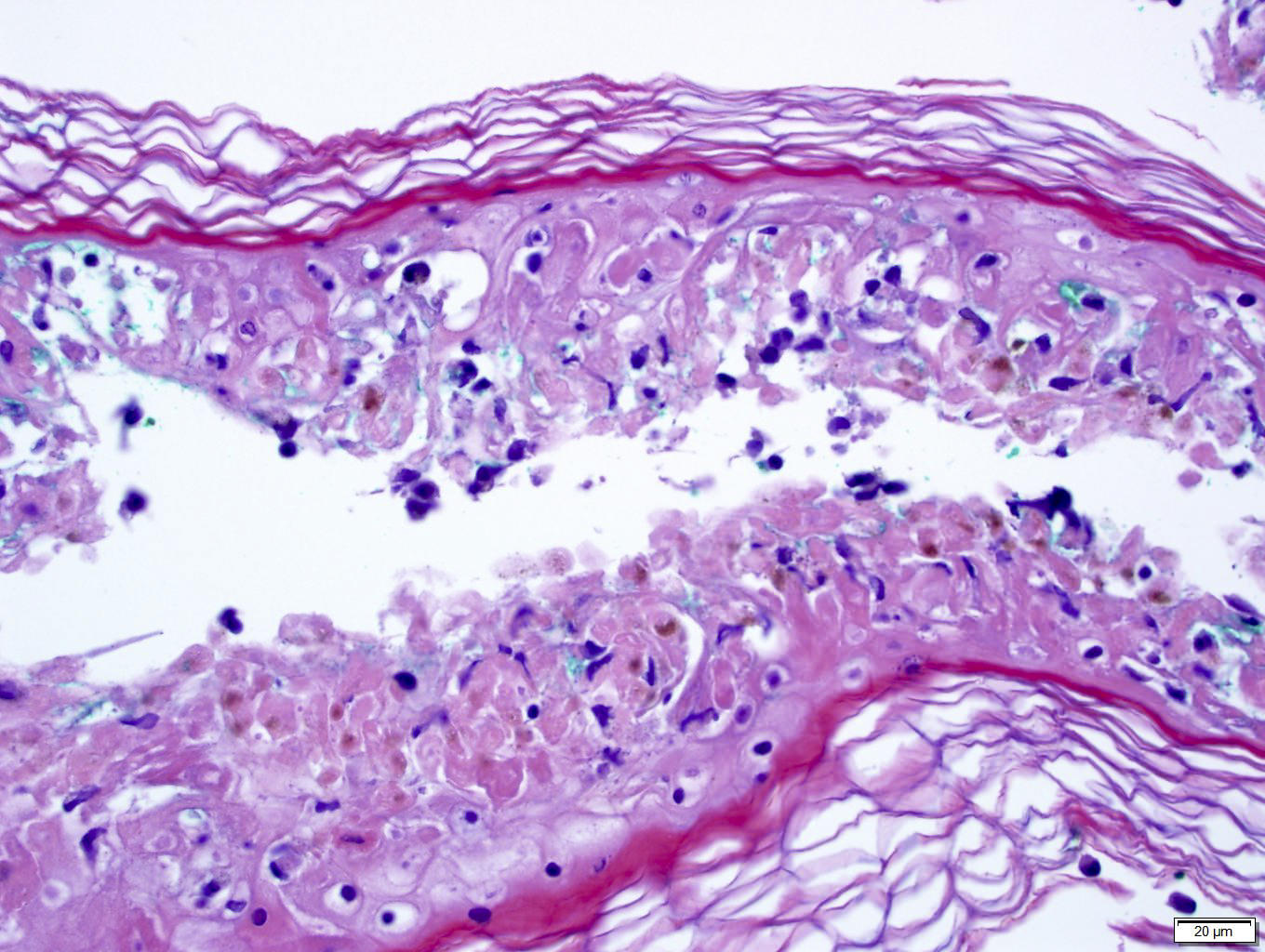
Frozen section description
- Helpful to confirm diagnosis of Stevens-Johnson syndrome
- Patient below had toxic epidermal necrolysis with extensive body surface and mucosal involvement
Microscopic (histologic) description
- Early lesions: apoptotic keratinocytes scattered in basal epidermis
- Later lesions: numerous necrotic keratinocytes, full thickness epidermal necrosis and subepidermal bullae
- Epidermal changes are often accompanied by a moderate or dense lymphocyte predominant dermal infiltrate
- Less commonly, neutrophils and eosinophils are present (Mayo Clin Proc 2010;85:131)
- Less common findings are red blood cell extravasation, pigment incontinence, regenerating epidermis, parakeratosis and necrosis of hair follicle (Mayo Clin Proc 2010;85:131)
- Clinical correlation is essential to distinguish erythema multiforme, SJS and TEN, as they may look nearly identical histologically
- Cannot reliably distinguish based on full thickness epidermal necrosis / necrolysis, because EM may have it and SJS / TEN may not, depending on the site of the biopsy
Microscopic (histologic) images
Differential diagnosis
- Other entities with vacuolar interface dermatitis (with individual keratinocyte necrosis):
- Acute graft-versus-host disease (GVHD)
- Connective tissue disease (including lupus and dermatomyositis)
- Fixed drug eruption
- Pityriasis lichenoides (PLEVA or PLC)
- Subacute radiation dermatitis
- Viral exanthems
- Other entities with desquamation and epidermal detachment:
- Bullous pemphigoid
- Congenital bullous diseases, such as epidermolysis bullosa
- Other autoimmune blistering diseases
- Pemphigus
- Staphylococcal scalded skin syndrome
- TEN
Additional references