Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khazaeli M, Motaparthi K. Rheumatoid nodule. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorrheumatoidnodules.html. Accessed March 30th, 2025.
Definition / general
- Rheumatoid nodules are the most common extra-articular manifestation of rheumatoid arthritis (RA) (Semin Cutan Med Surg 2007;26:100)
- Subcutaneous rheumatoid nodules are firm, nontender and movable within the subcutaneous tissue; however, they could also be attached to underlying structures, such as the periosteum, fascia and tendons (Am J Med 1984;76:279)
Essential features
- Rheumatoid nodules are the most common extra-articular manifestation and characteristic lesion in rheumatoid arthritis patients (Clin Rheumatol 2019;38:3041)
- Most common on pressure points (such as the olecranon process); however, they may occur at other sites, including within the lung and other internal organs (Clin Rev Allergy Immunol 2017;53:371)
- Subcutaneous rheumatoid nodules are firm, nontender and movable within the subcutaneous tissue; however, they could also be attached to underlying structures, such as the periosteum, fascia and tendons (Am J Med 1984;76:279)
- Rheumatoid nodules are clinical predictors of more severe arthritis, seropositivity, joint erosions and rheumatoid vasculitis (J Am Acad Dermatol 1983;8:439)
- Presence of rheumatoid nodules often suggests a need for more aggressive treatment of the underlying rheumatoid arthritis to prevent sequelae (Can Fam Physician 2005;51:35)
- Necrobiosis, with fibrin deposition and palisading epithelioid histiocytes, is a typical histologic feature of rheumatoid nodules (Clin Rheumatol 2019;38:3041)
ICD coding
- ICD-10: M06.30 - rheumatoid nodule, unspecified site
Epidemiology
- Rheumatoid arthritis is the most common inflammatory arthritis; affects 0.5 - 1.0% of the population (Rheum Dis Clin North Am 2001;27:269)
- 30 - 40% of all patients with rheumatoid arthritis develop nodules (Ann Rheum Dis 2006;65:601)
- Low concordance rate for rheumatoid arthritis in monozygotic twins highlights the importance of environmental factors (Br J Rheumatol 1993;32:903)
- Smoking is an independent risk factor for rheumatoid arthritis, particularly rheumatoid factor (RF) positive disease (Arthritis Rheum 1997;40:1955)
- 2 - 4 fold increase in mortality for patients with extra-articular manifestations, including rheumatoid nodules (J Rheumatol 2002;29:62)
- Early presence of rheumatoid nodules is a predictor of severe extra-articular manifestations (Scand J Rheumatol 2000;29:358)
- Nodules are found predominantly in seropositive patients; however, current or previous smoking is associated with the presence of nodules even after controlling for rheumatoid factor positivity (J Rheumatol 2000;27:630)
- Unlike the production of rheumatoid factor, the development of subcutaneous nodules does not occur in healthy individuals who smoke (Ann Rheum Dis 1990;49:753)
- Patients with rheumatoid arthritis and rheumatoid nodules are also more likely to develop vasculitis (J Rheumatol 2008;35:179)
Sites
- Most commonly arise in the skin; however, they can arise in extracutaneous sites, such as the lung, tendon, vocal cords, occiput and sacrum (Clin Rheumatol 2019;38:3041)
- Subcutaneous nodules:
- Mostly on extensor surfaces at sites of frequent trauma (Ann Rheum Dis 1993;52:625):
- Proximal ulna, olecranon process (where they must be differentiated from olecranon bursitis with enlargement of the synovial layer)
- Extensor tendons of the hand (metacarpophalangeal or the proximal interphalangeal joints)
- Back of the head and ears
- Back of the heels
- Ischial tuberosities
- Bedridden patients can develop nodules on the occiput and ischial areas; nodules occasionally form on tendons and ligamentous tissues, such as the Achilles tendon and vocal cords (Clin Otolaryngol Allied Sci 2003;28:446)
- Mostly on extensor surfaces at sites of frequent trauma (Ann Rheum Dis 1993;52:625):
- Pulmonary nodules:
- Prevalence of pulmonary rheumatoid nodules in patients with rheumatoid arthritis depends in part on the methods used for detection (Medicine (Baltimore) 1968;47:501)
- In rheumatoid arthritis, lung nodules are generally located in subpleural areas or in association with interlobular septa (Med J Aust 1986;144:648)
- Cardiac nodules:
- Rheumatoid nodules may develop in the pericardium, myocardium and valvular structures (Clin Med (Lond) 2001;1:18)
- Central nervous system:
- Rheumatoid nodules have rarely been reported in the CNS (Semin Arthritis Rheum 1989;18:258)
- Other organs (very rare):
- Mucosa and the lip (J Oral Maxillofac Surg 2014;72:1532)
- Thyroid gland (J Med Case Rep 2019;13:159)
- Lymph nodes (BMJ Case Rep 2013;2013:bcr2013009516)
- Liver (Hepatology 2019;69:1345)
- Kidneys (Hepatology 2019;69:1345)
Pathophysiology
- Predominant infiltrating inflammatory cell in the rheumatoid nodule is the macrophage (Arthritis Rheum 1987;30:728)
- Macrophages in the rheumatoid nodules express TNF alpha, IL1 beta and IL1Ra mRNA, particularly in perivascular cells of the stroma and in the palisading layer (Arthritis Rheum 1998;41:1783)
- Cytokines, proteinases and other immune factors:
- A variety of products, particularly cytokines, are produced within rheumatoid nodules; the fibroblasts in the nodules produce large quantities of metalloproteases (J Clin Invest 1972;51:2973)
- Most of the cytokine profile, together with the ability of the tissue to produce metalloproteinases, establishes the rheumatoid nodule as a T helper 1 (Th1) granuloma (Arthritis Rheum 2003;48:334)
- Lymphocytes generate IgG and IgM rheumatoid factor (Arthritis Rheum 2003;48:334)
- There is evidence for (Arthritis Rheum 2008;58:1601):
- Tumor necrosis factor (TNF) alpha
- Interferon gamma
- Interleukin (IL) 1 beta
- IL1 receptor antagonist
- IL10, IL15, IL18 and IL12
- Adhesion molecules, including E-selectin
- Intracellular adhesion molecule (ICAM) 1
- Platelet endothelial cell adhesion molecule (PECAM)
- Vascular cell adhesion molecule (VCAM)
- Deposits of rheumatoid factor and the terminal components of complement are also found on the endothelium of small vessels within nodules (J Rheumatol 2000;27:1839)
- Peptidyl arginine deiminases 2, 3 and 4 and myeloperoxidase have been shown to generate citrullinated and homocitrullinated antigens in necrotic tissue of rheumatoid nodules (Arthritis Res Ther 2016;18:239)
- Neutrophils express these enzymes; through the generation of neutrophil extracellular traps (NETs), they may contribute to autoantigen externalization and may be targeted by anticitrullinated peptide antibodies (ACPA), thus contributing to the inflammatory process within rheumatoid nodules (Sci Transl Med 2013;5:178ra40)
- Similar proinflammatory cytokines and cell adhesion molecules, in the rheumatoid nodule and synovial membrane, suggests that similar pathogenic processes result in the chronic inflammation and tissue destruction within these lesions (Arthritis Rheum 1998;41:1783)
Etiology
- Smoking is an independent risk factor for rheumatoid arthritis, particularly rheumatoid factor (RF) positive disease (Arthritis Rheum 1997;40:1955)
- Some patients treated for rheumatoid arthritis with methotrexate have a noticeable increase in the size and number of rheumatoid nodules (Proc Natl Acad Sci U S A 1991;88:2441)
- Genetic factors:
- IL4 receptor (IL4R) single nucleotide polymorphisms are associated with rheumatoid nodules (Arthritis Res Ther 2010;12:R75)
- HLA: less important for development of nodules than for other extra-articular disease features (Arthritis Rheum 2004;50:753)
Clinical features
- Subcutaneous rheumatoid nodules:
- Firm, nontender and movable within the subcutaneous tissue; however, they can also be attached to underlying structures, such as the periosteum, fascia and tendons (Am J Med 1984;76:279)
- Nodules vary in consistency, from firm immovable masses when they are small to soft mobile masses when they are large (Ann Rheum Dis 1993;52:625)
- Nodules may ulcerate or may become gangrenous (Ann Rheum Dis 1993;52:625)
- Pulmonary nodules (Med J Aust 1986;144:648):
- Generally asymptomatic but can lead to complications, including:
- Pleural effusion
- Pneumothorax
- Pyopneumothorax
- Bronchopleural fistula
- Hemoptysis
- Generally asymptomatic but can lead to complications, including:
- Cardiac nodules:
- Presence of subcutaneous nodules is associated with valvular thickening, nodules and insufficiency (mainly of the mitral and aortic valves on echocardiography) (Rheumatol Int 1999;18:163)
- Symptoms related to the presence of nodules are rare but syncope or death (due to heart block from a lesion situated in the conduction system) can occur (Ann Rheum Dis 1983;42:389)
- Stroke or other manifestations of arterial embolization may result from nodules on a heart valve (J Heart Valve Dis 1997;6:77)
Diagnosis
- Subcutaneous rheumatoid nodules:
- Multiple subcutaneous nodules, in the presence of rheumatoid factors and in the absence of any joint complaints, firmly suggest a diagnosis of rheumatoid nodulosis (Ann Rheum Dis 1949;8:1)
- Biopsy of mature lesions, though often not necessary, shows necrobiosis, with fibrin deposition and palisading epithelioid histiocytes (Clin Rheumatol 2019;38:3041)
Laboratory
- Rheumatoid nodules are found predominantly in rheumatoid factor (RF) positive patients (Am J Med 1984;76:279)
Case reports
- 33 year old woman with a 3 year history of rheumatoid arthritis treated with methotrexate, after total thyroidectomy for hypothyroidism (J Med Case Rep 2019;13:159)
- 56 year old man diagnosed 2 years earlier with seronegative rheumatoid arthritis (RA) presents with acute right sided hemiplegia and dysarthria (J Community Hosp Intern Med Perspect 2017;7:175)
- 57 year old woman, with an overlap syndrome of both rheumatoid arthritis (RA) and autoimmune hepatitis, developed multiple skin nodules (Clin Rheumatol 2011;30:719)
- 57 year old man with rheumatoid arthritis and myasthenia gravis developed an asymptomatic erythematous plaque on his nose and skin colored nodules on the elbows (Int J Dermatol 2007;46:33)
Treatment
- Subcutaneous nodules (G Ital Dermatol Venereol 2018;153:243):
- Treatment of rheumatoid nodules is unnecessary because they are often asymptomatic
- Nodules may ulcerate, become infected, or compress nerves or articular structures; surgical excision may be necessary and may include skin grafting for extremely large nodules
- Intralesional injection of steroids may also be considered
- Nodules managed with disease modifying antirheumatic drugs (DMARDs) may shrink, persist or worsen
Clinical images
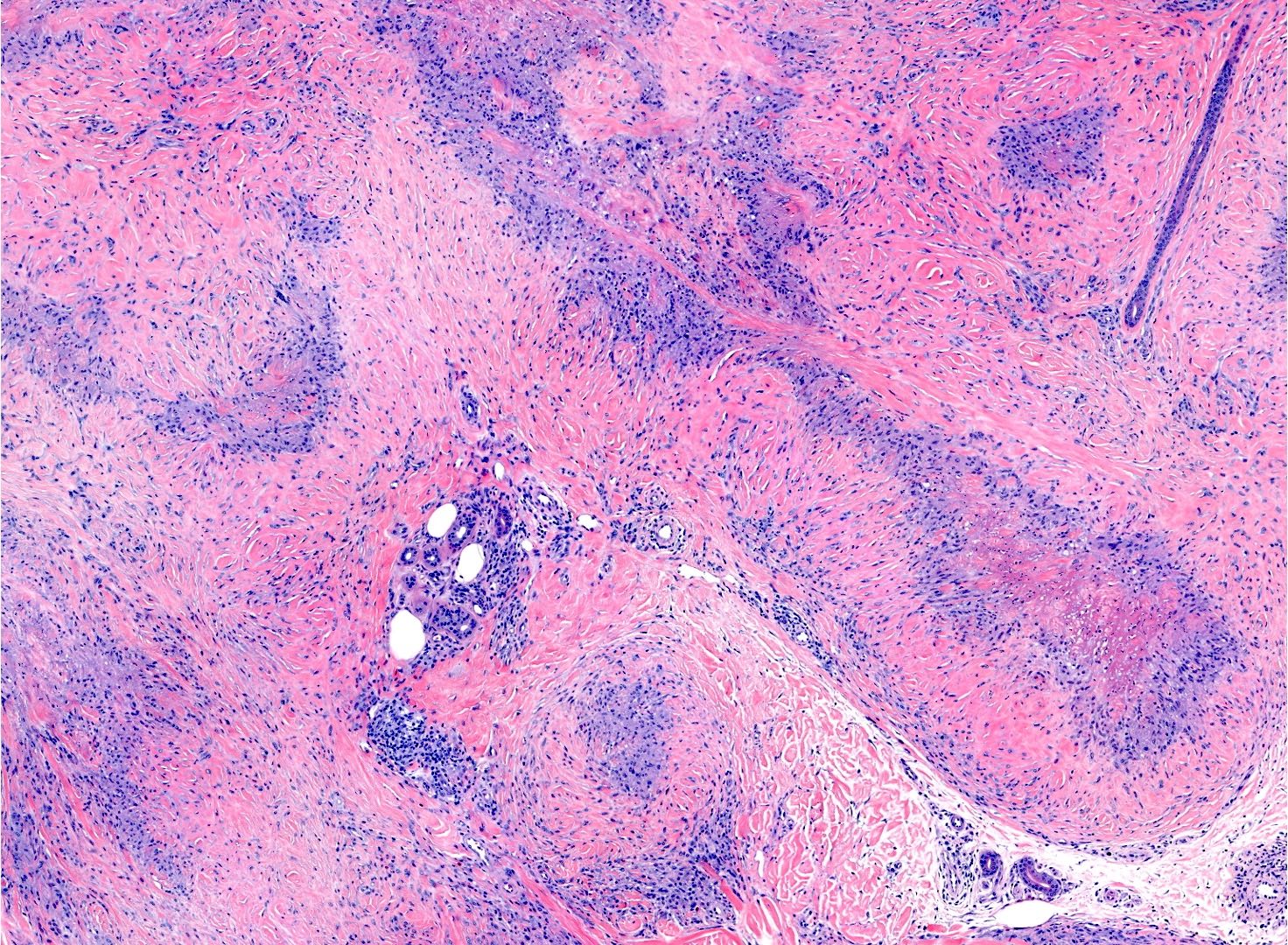
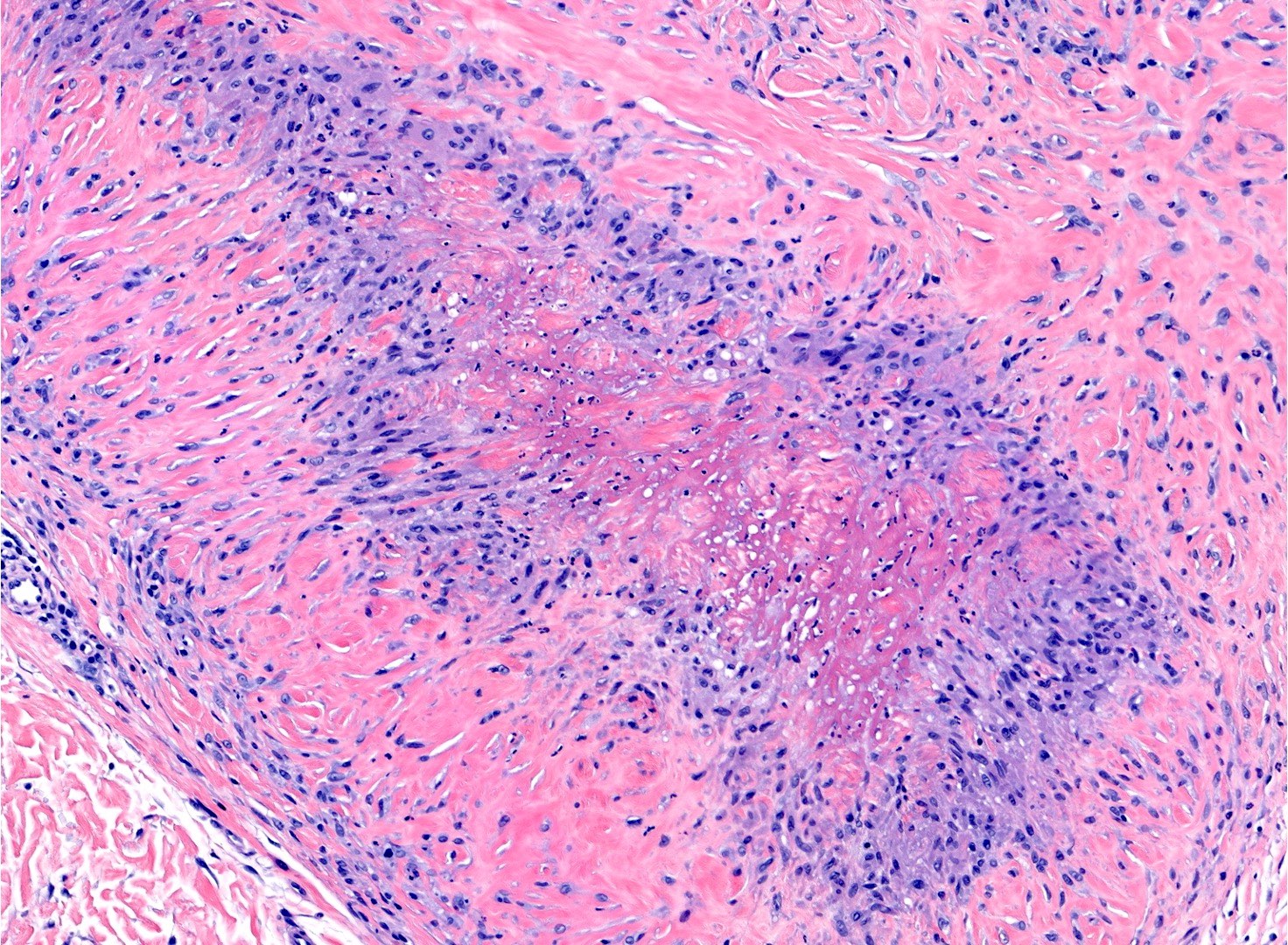
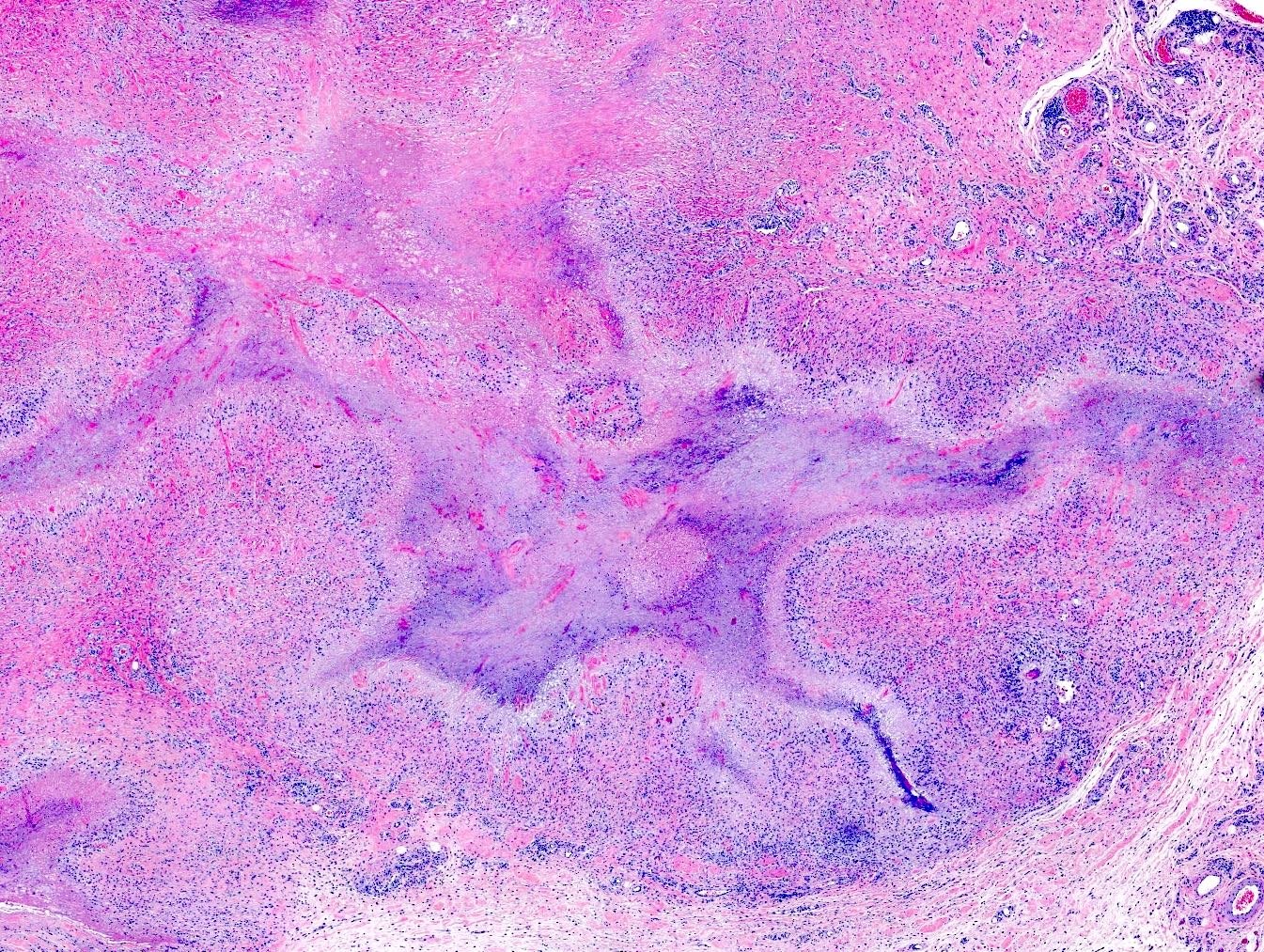
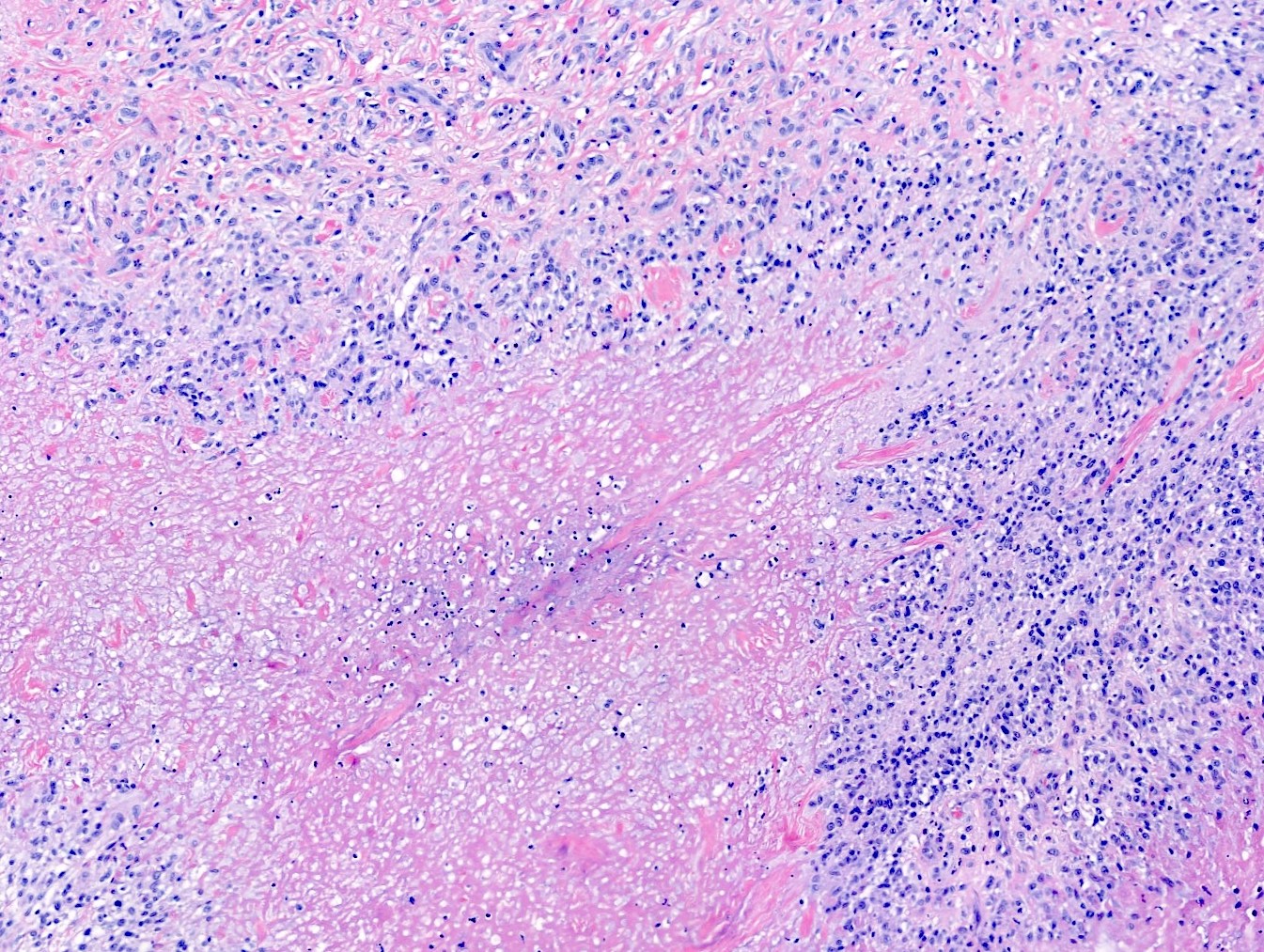
Microscopic (histologic) description
- Central area of fibrinoid necrosis surrounded by palisading macrophages and lymphocytes (Arthritis Rheum 1987;30:728)
- Necrobiosis, with fibrin deposition and palisading epithelioid histiocytes (Clin Rheumatol 2019;38:3041)
- Leukocytoclastic vasculitis (with associated immunoglobulin [Ig], fibrin deposition and complement activation) can be found in 33% of all rheumatoid nodules (Semin Cutan Med Surg 2007;26:100)
- Granulomas are typically identified in the subcutis but occasionally may involve the dermis
- Mucin deposition is characteristically absent
Microscopic (histologic) images
Sample pathology report
- Right index finger, excision:
- Palisading granulomas in the subcutis surrounding areas of fibrinoid necrosis, consistent with rheumatoid nodule
Differential diagnosis
- Rheumatic fever nodules (Ann Rheum Dis 1993;52:625):
- Localization: extensor sites, also over the spinous process of vertebrae
- Depth: subcutaneous
- Microscopy (Cureus 2021;13:e12577):
- Histologic appearance varies depending on whether the biopsy is of an early or an established nodule
- Features in early descriptions include increased numbers of dilated blood vessels with peripherally thickened walls, fibrinoid necrosis and fibrosis with attachment to tendons
- Histologically similar to nodules seen in rheumatoid arthritis with central fibrinoid necrosis, surrounded by histiocytes and perivascular lymphocytes and neutrophils
- Age of onset: children
- Persistence: limited
- Rheumatoid factor: absent
- Concomitant joint disease: yes
- Bone erosions: absent
- Granuloma annulare:
- Localization: extensor site or any other site
- Depth: intradermal (subcutaneous)
- Microscopy (Arch Dermatol 1977;113:1681):
- Palisaded or interstitial granulomatous inflammation with mucin unites all forms
- Minimal epidermal changes
- Age of onset: children, young adults
- Persistence: unpredictable
- Rheumatoid factor: absent
- Concomitant joint disease: none
- Bone erosions: absent
- Gouty tophi (Ann Rheum Dis 2013;72:1545):
- Patient with a history of acute mono or oligoarticular arthritis
- Most commonly involving the great toe metatarsophalangeal (MTP) joints
- Hyperuricemia
- White to yellow monosodium urate deposits
- Diagnosis can be confirmed, when necessary, by aspiration and polarized microscopy
- Microscopy (J Int Adv Otol 2016;12:216):
- Tophi are composed of needle shaped aggregates of urate crystals with surrounding foreign body giant cell reaction
- Urate crystals dissolve with routine processing, so fix a smear of crystals in absolute alcohol or nonaqueous fixation
- Under polarized light microscopy, they have a needle-like morphology and strong negative birefringence
- Calcinosis cutis (Semin Arthritis Rheum 2005;34:805):
- Dystrophic calcification at sites of microtrauma or inflammation
- Typically occurs in patients with systemic sclerosis, dermatomyositis or overlap connective tissue diseases
- Lesions are composed of calcium hydroxyapatite
- Multiple subcutaneous papules or nodules that are yellow-white in the hands, elbows or feet
- May also occur in soft tissues of the trunk or legs
- Calcinosis lesions may ulcerate and exude chalky white material
- These nodules may be evident on plain radiography
- Microscopy (Actas Dermosifiliogr 2015;106:785):
- Irregular deposits of intensely basophilic acellular material in the dermis and subcutaneous tissue
- Basophilia is so strong that the appearance is of a deep purple
- Deposits are typically well circumscribed with a thin rim of eosinophilic hyalinization and frequently with a host giant cell reaction
- Palisaded neutrophilic granulomatous dermatitis (JAAD Case Rep 2017;3:425):
- Typically associated with underlying disease states, including autoimmune connective tissue disease, lymphoproliferative disorders and infections
- Most common in patients with rheumatoid arthritis
- Can be seen in patients with systemic lupus erythematosus and systemic vasculitis
- Microscopy:
- Early lesions present with neutrophilic infiltrates and leukocytoclastic vasculitis
- Fully developed lesions feature palisaded granulomas with collagen trapping and neutrophil remnants
- Epithelioid sarcoma (Adv Anat Pathol 2006;13:114):
- Malignant mesenchymal neoplasm that exhibits epithelioid cytomorphology and a predominantly epithelial phenotype
- Microscopy:
- Classic or conventional, distal type:
- Dermal / subcutaneous nodule(s)
- Can simulate granulomatous process, with or without necrosis (pseudogranulomatous morphology)
- Fairly uniform plump small to medium sized cells with eosinophilic cytoplasm (Adv Anat Pathol 2016;23:41)
- Spindle cells can also be identified and often appear more conspicuous at the periphery of a nodule
- Mildly atypical nuclei with vesicular chromatin and small nucleoli
- Variable mitotic activity
- Mixed chronic inflammatory infiltrate common
- Dystrophic calcification and metaplastic bone formation
- Proximal, large cell type (Am J Surg Pathol 1997;21:130):
- Infiltrative growth pattern with less defined peripheral borders
- Multiple large nodules
- Large polygonal cells with abundant eosinophilic cytoplasm
- Rhabdoid morphology common
- Vesicular nuclei with prominent macronucleoli
- Mitoses, necrosis and hemorrhage common
- Classic or conventional, distal type:
- Necrobiosis lipoidica:
- Atrophic, yellow depressed plaques, usually on legs of diabetic patients
- Microscopy (Indian J Endocrinol Metab 2012;16:614):
- Layered inflammatory process and alternating zones of necrobiosis involving the full thickness of the dermis
- Changes tend to become more pronounced deeper in the dermis and may extend into the septal panniculus
- Areas of necrobiosis are poorly defined and run into each other with broad foci of inflammatory infiltrate intervening
- Variable histiocytic infiltrate with multinucleated giant cells surrounds these areas
- Accompanying inflammatory infiltrate is predominantly lymphocytic with plasma cells and occasional eosinophils
Board review style question #1
Board review style answer #1
C. IL4 receptor (IL4R) single nucleotide polymorphisms are associated with rheumatoid nodules (Arthritis Res Ther 2010;12:R75)
Comment Here
Reference: Rheumatoid / rheumatic nodules
Comment Here
Reference: Rheumatoid / rheumatic nodules
Board review style question #2
A 57 year old man with rheumatoid arthritis and myasthenia gravis developed an asymptomatic erythematous plaque on his nose and skin colored nodules on his elbows. If the elbow nodules get biopsied, what is the most probable microscopic pattern?
- Central area of fibrinoid necrosis surrounded by palisading macrophages and lymphocytes
- Layered inflammatory process and alternating zones of necrobiosis involving the full thickness of the dermis
- Mildly atypical nuclei with vesicular chromatin and small nucleoli
- Neutrophilic infiltrates and leukocytoclastic vasculitis
Board review style answer #2
A. Central area of fibrinoid necrosis surrounded by palisading macrophages and lymphocytes
Comment Here
Reference: Rheumatoid / rheumatic nodules
Comment Here
Reference: Rheumatoid / rheumatic nodules