Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Bui CM, Smoller BR. Pityriasis rubra pilaris. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpityriasisrubra.html. Accessed April 2nd, 2025.
Definition / general
- Pityriasis rubra pilaris (PRP) is a rare, chronic, idiopathic disorder characterized by an acute cutaneous eruption with potential to quickly progress to erythroderma
Essential features
- Includes acquired and hereditable forms
- Clinical presentation is characterized by papulosquamous / erythematosquamous dermatosis
- Affects all ages with variable clinical courses
- Can be associated with HIV
- CARD14 mutation has been detected in patients with familial PRP
- Histopathologic findings are characteristic
ICD coding
- ICD-10: L44.0 - pityriasis rubra pilaris
Epidemiology
- All ages, 2 peaks: first and sixth to seventh decades (JAMA Dermatol 2016;152:670)
- No gender difference (JAMA Dermatol 2016;152:670)
- Large majority of PRP cases are acquired (Am J Clin Dermatol 2018;19:377)
- HIV associated type VI PRP (Br J Dermatol 1996;135:1008)
Sites
- Skin, nails and hair (Pediatr Dermatol 1986;3:446, Arch Dermatol 1964;89:515)
Pathophysiology
- CARD14 mutation and dysfunction of vitamin A metabolism have been suggested to play a role in the pathogenesis (Br J Dermatol 1981;104:253, J Cutan Pathol 2020;47:425)
Etiology
- Etiology not clearly defined (Am J Clin Dermatol 2018;19:377)
- Onset of acquired PRP has been associated with malignancy, infection, medications, vaccines, ultraviolet exposure and skin trauma (Am J Clin Dermatol 2010;11:157)
- Heritable PRP is associated with CARD14 mutation (Am J Hum Genet 2012;91:163)
Clinical features
- Can be localized or diffuse / erythroderma
- Localized lesions are often found in elbows, knees and thighs
- Characteristics are diffuse and confluent, orange-red, well defined plaques with normal appearing skin islands (sparing), scaling follicular papules and scaling on palms and soles
- Variable degree of pruritus is common
- Nail changes are common
- Scalp alopecia or transient eruptive seborrheic keratosis with no evidence of an internal malignancy may occur (J Cutan Pathol 2021;48:133, Actas Dermosifiliogr 2014;105:955, Clin Exp Dermatol 2004;29:554, Acta Derm Venereol 1988;68:443, J Eur Acad Dermatol Venereol 2009;23:217, J Am Acad Dermatol 1989;20:801)
- Cutaneous malignancies (e.g., basal cell carcinoma, Merkel cell carcinoma, squamous cell carcinoma and cutaneous Kaposi sarcoma) may also be present at the time of PRP diagnosis or ensuing months (Australas J Dermatol 2002;43:48, J Am Acad Dermatol 1996;35:781)
- 6 types of PRP (Br J Dermatol 1996;135:1008)
- Type I (classic adult type)
- 55% of PRP patients
- Presents with classic findings of PRP and spreads caudally
- Majority clear within 3 years
- Type II (atypical adult type)
- 5% of PRP patients
- Eczematous dermatitis with ichthyosiform scale on legs and palmoplantar keratoderma, occasional alopecia
- Chronic clinical course
- Type III (classic juvenile type)
- 10% of PRP patients
- Resembles type I
- Erythroderma is less common
- Majority clear within 3 years
- Type IV (circumscribed juvenile type)
- 25% of PRP patients
- Circumscribed, erythematous follicular papules and scaly plaques on elbows and knees
- Variable clinical course
- Type V (atypical juvenile type)
- 5% of PRP patients
- Eczematous dermatitis with ichthyosiform scaly plaques, palmoplantar keratoderma, follicular hyperkeratosis and scleroderma-like changes of hands and feet
- Onset in first few years of life
- Chronic clinical course
- Type VI
- < 1% of PRP patients
- Associated with HIV infection
- Resembles type I
- Follicular occlusion tetrad of dissecting cellulitis of the scalp, pilonidal sinus / cyst, hidradenitis suppurativa and acne conglobate may be accompanied
- Type I (classic adult type)
Diagnosis
- Definitive diagnosis is based on clinicopathologic findings
- Lesions most often appear on the face, chest and scalp with caudal migration interspersed with areas of unaffected skin
- Small, scaly papules surround hair follicles
- Palms or soles may develop an orange-red waxy keratoderma (Am J Clin Dermatol 2010;11:157)
- Diagnosis is confirmed via biopsy in conjunction with clinical characteristics
- Checkerboard pattern of parakeratosis and orthokeratosis is characteristic for PRP
- Follicular plugging is common
- Acantholysis and increased granular cell layer
- No blood test is available; however, diagnosis of familial forms of PRP can be supported by Sanger sequencing for mutations of the CARD14 gene (Am J Clin Dermatol 2018;19:377)
Case reports
- 49 year old man with paraneoplastic PRP preceding leukemia (Adv Skin Wound Care 2022;35:1)
- 60 year old woman with acantholytic PRP induced by topical use of imiquimod 5% (An Bras Dermatol 2020;95:63)
- 65 year old man with PRP following COVID-19 vaccine (JAAD Case Rep 2022;24:74)
- 68 year old man with PRP with involvement of tongue and palate (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:604)
- 70 year old woman with identification of a pathogenic CARD14 mutation in PRP (BMJ Case Rep 2021;14:e235287)
- 72 year old woman with paraneoplastic PRP (JAAD Case Rep 2023;39:125)
Treatment
- Topical corticosteroids, topical or oral retinoids, cyclosporine, methotrexate, vitamin D analogs, antitumor necrosis factors (anti-IL12 / IL23 or anti-IL17 biologics, either alone or in combination therapy), azathioprine, intravenous immunoglobulin, infliximab, ixekizumab, tildrakizumab, ustekinumab, secukinumab, adalimumab, upadacitinib, narrowband UVB and extracorporeal photochemotherapy (Am J Clin Dermatol 2010;11:157, Am J Clin Dermatol 2018;19:377, Arch Dermatol 2005;141:423, J Am Acad Dermatol 2018;79:353, JAAD Case Rep 2022;27:55, JAAD Case Rep 2023;35:112, Australas J Dermatol 2022;63:120, Clin Exp Dermatol 2022;47:2300, Int J Rheum Dis 2023;26:1157, Dermatol Ther 2020;33:e14097, Clin Exp Dermatol 2021;46:1594, SAGE Open Med Case Rep 2023;11:2050313X231160927)
Clinical images
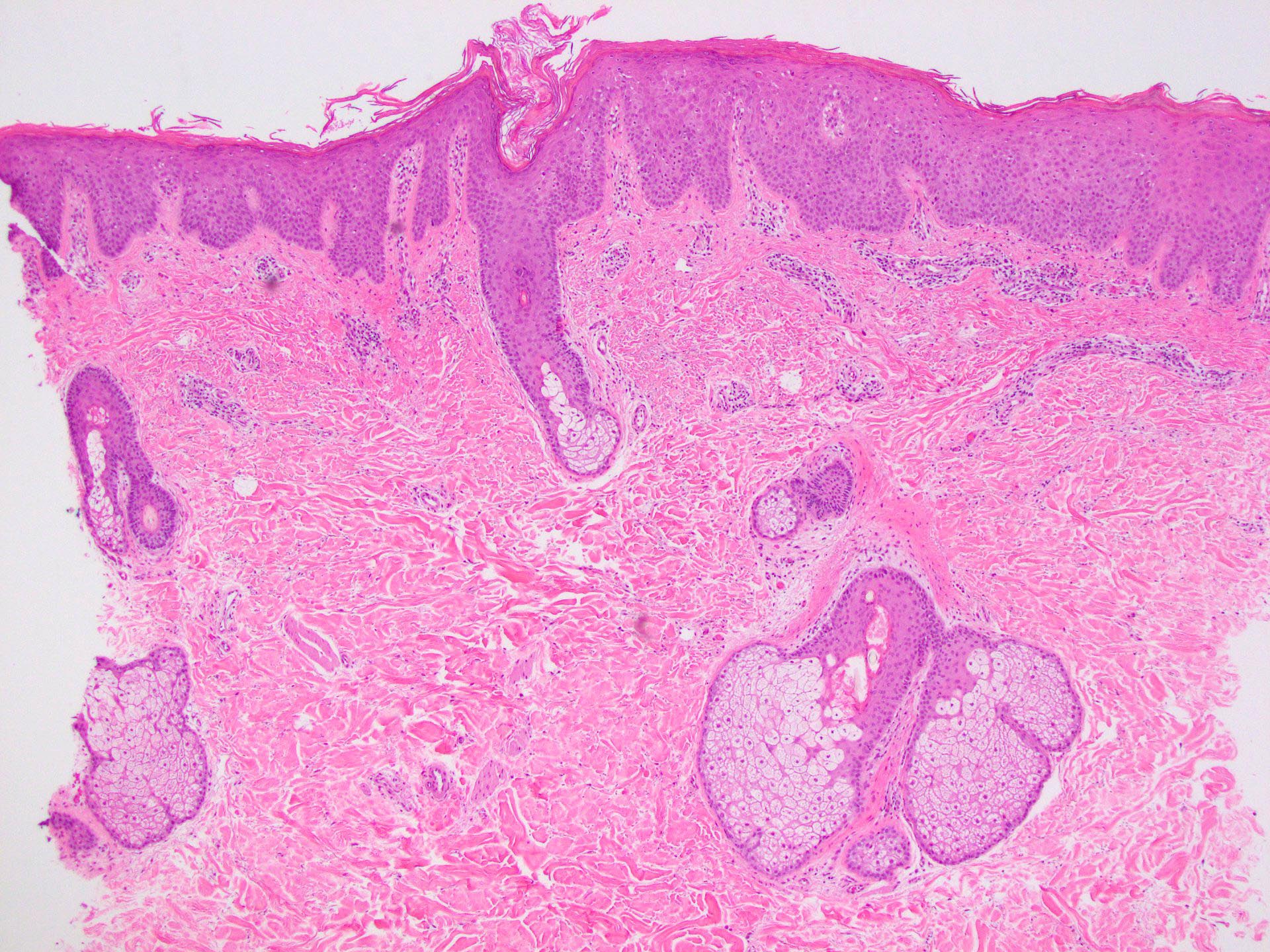
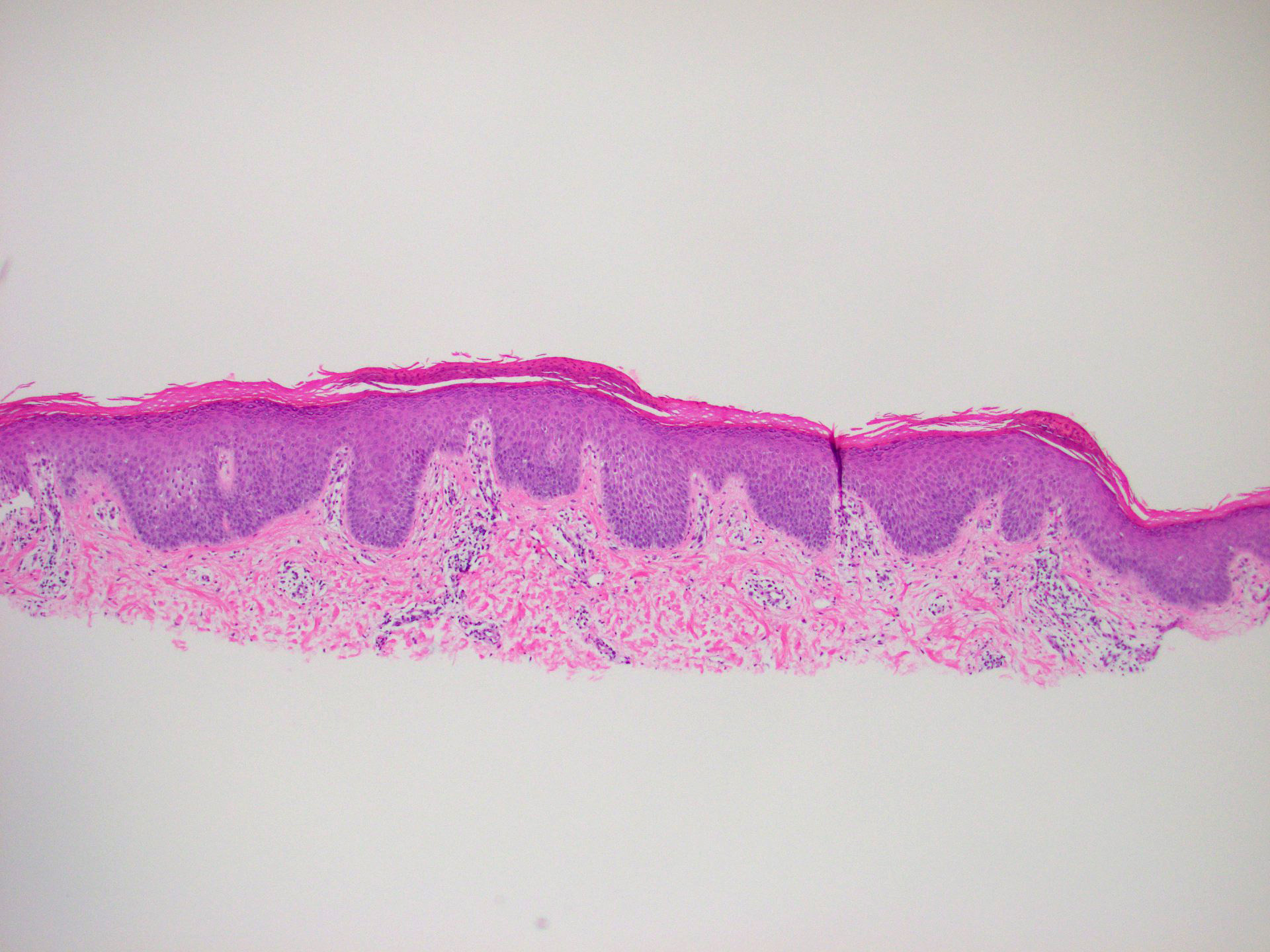
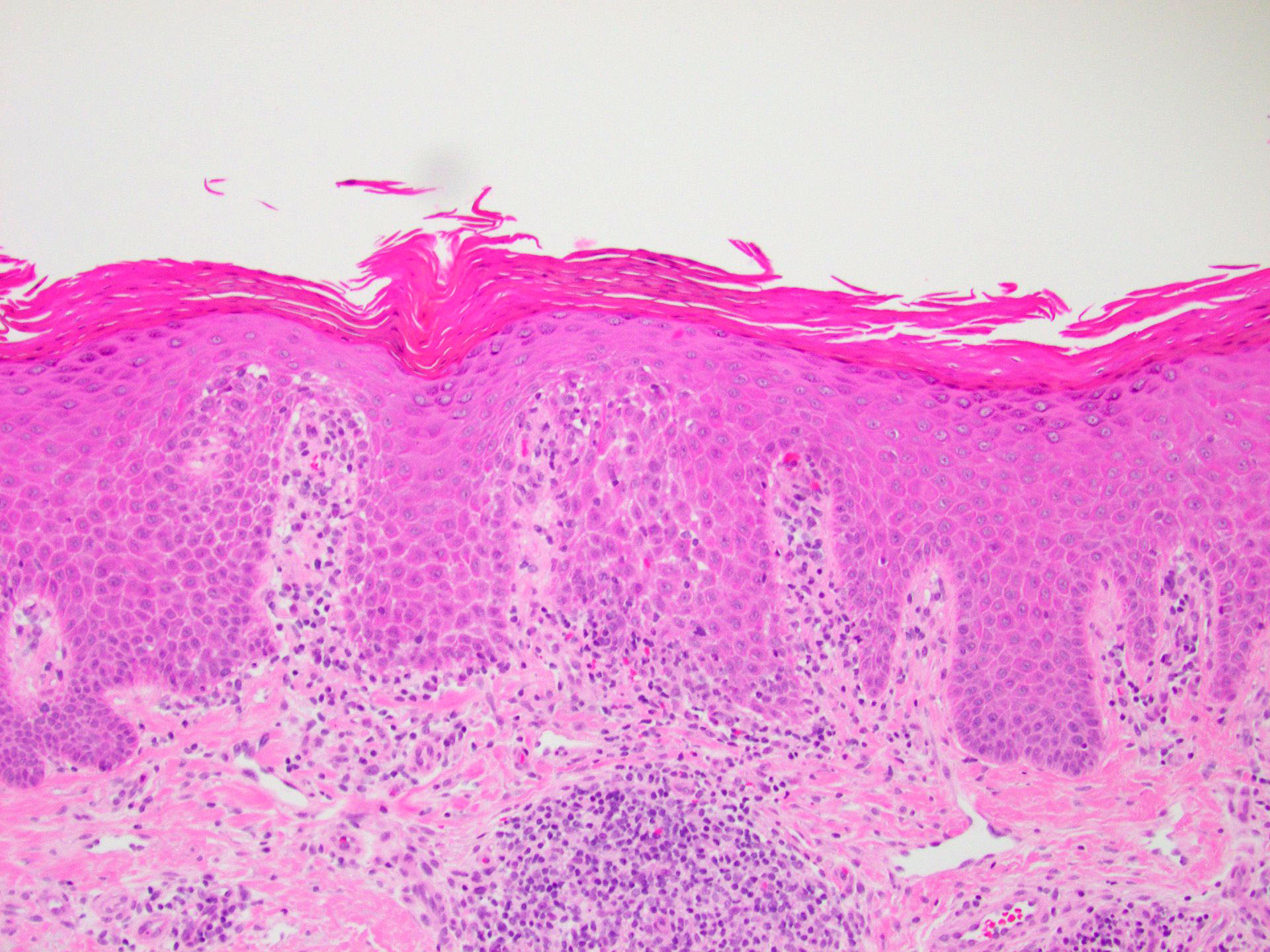
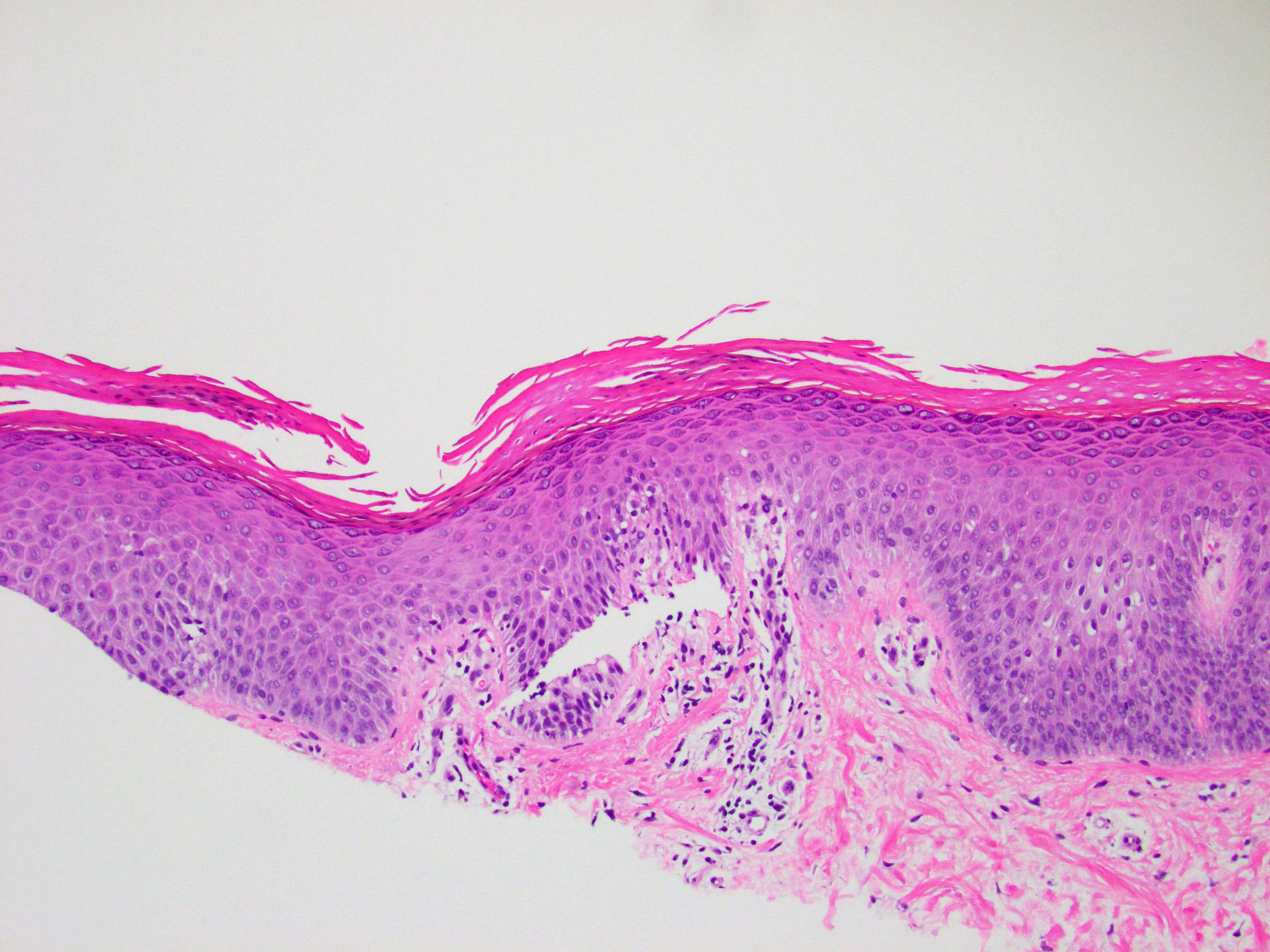
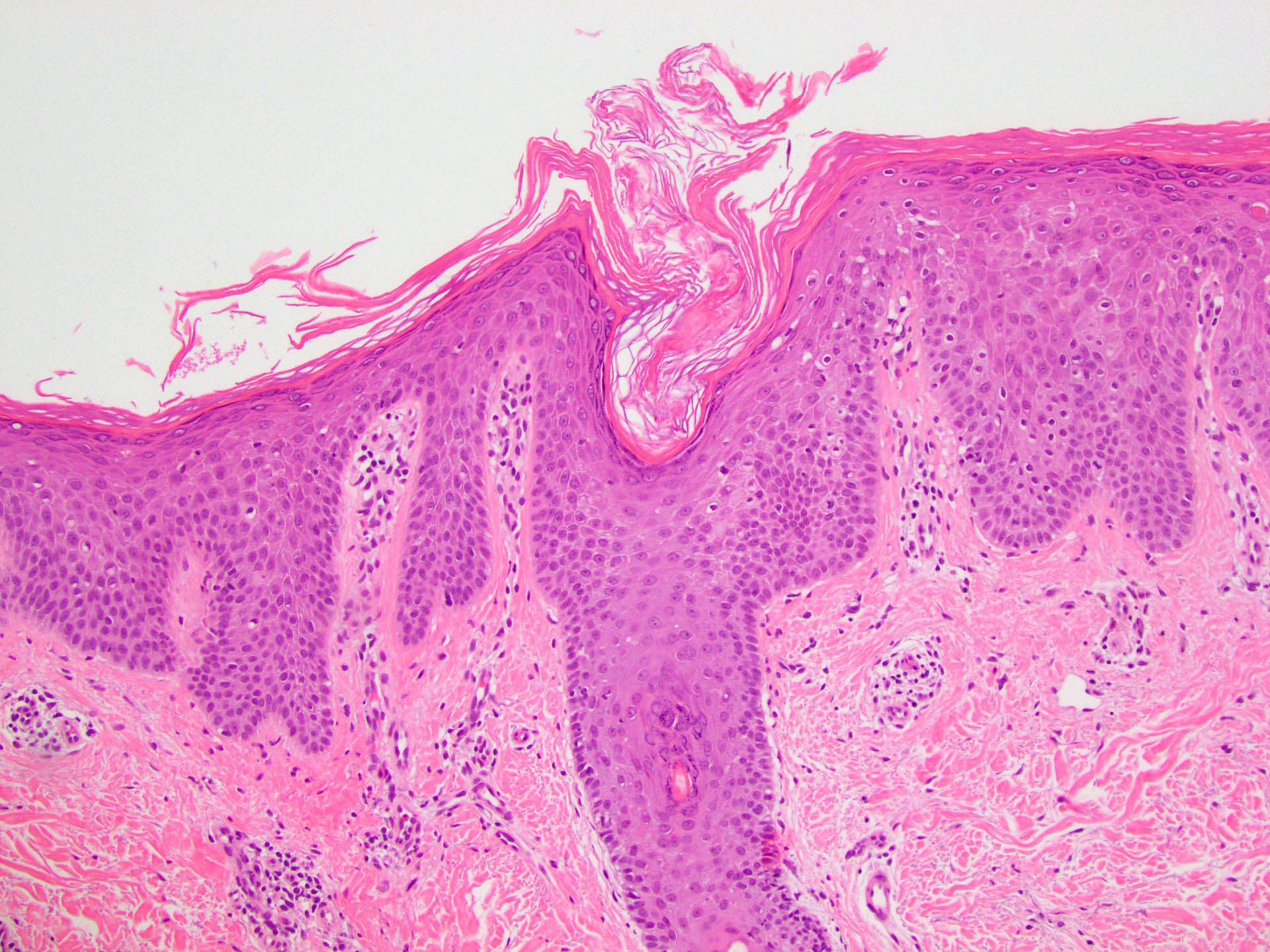
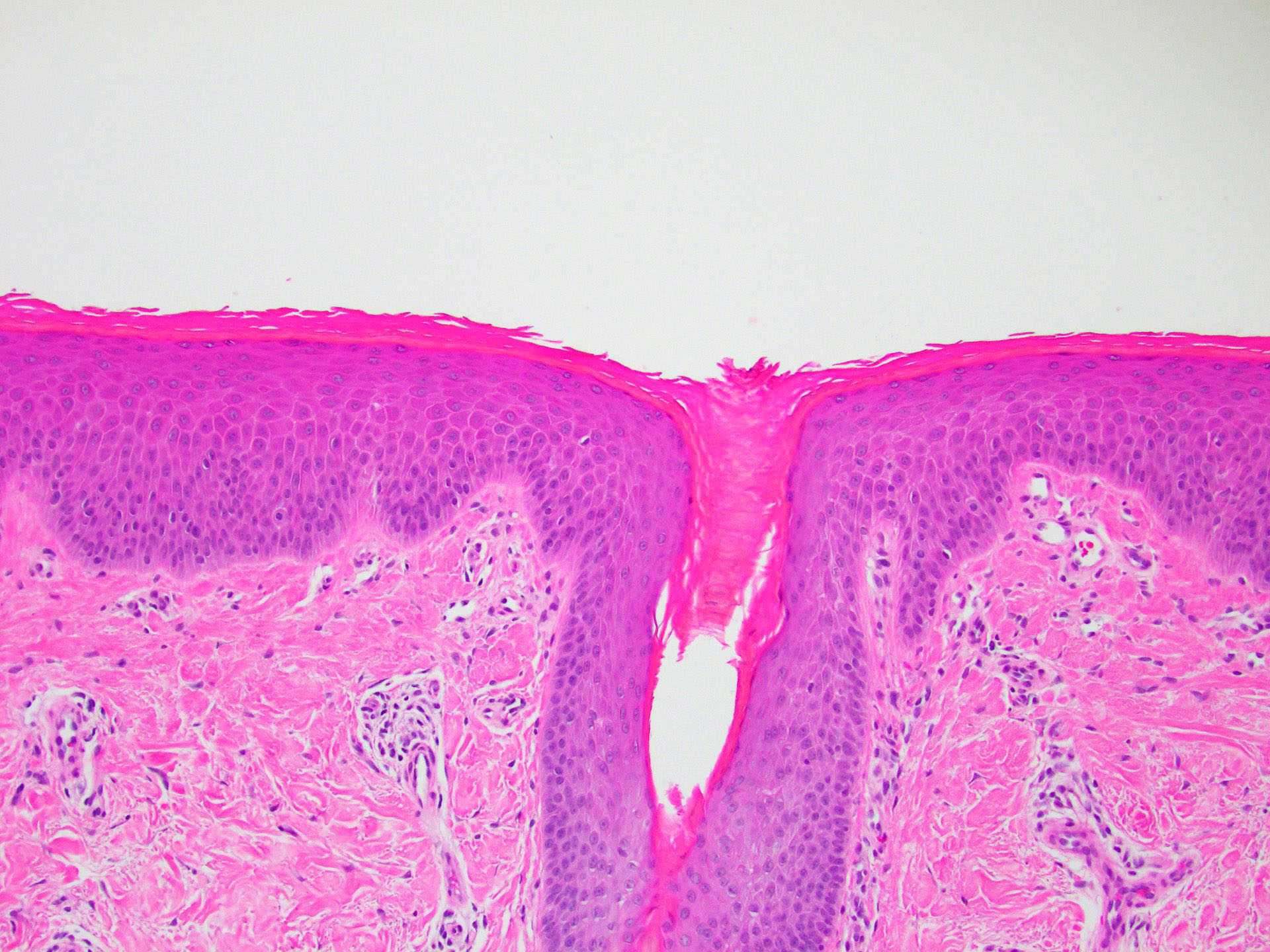
Microscopic (histologic) description
- Orthohyperkeratosis alternating with parakeratosis in both horizontal and vertical directions (checkerboard pattern)
- Follicular plugging
- Mild, irregular, vaguely psoriasiform epidermal acanthosis with broad rete ridges, thick suprapapillary plates and preserved granular layer
- Focal acantholysis, dyskeratosis may be seen (Am J Dermatopathol 1999;21:491)
- Mild superficial perivascular and perifollicular lymphocytic infiltrate; rare eosinophils may be intermixed
- Dilated vessels within papillary dermis
Microscopic (histologic) images
Sample pathology report
- Skin biopsy, face:
- Pityriasis rubra pilaris, classical adult type I (see comment)
- Comment: The clinical history and images showing widespread erythema with areas of noninvolved skin present on the face, neck and trunk were reviewed. Histopathologic examination reveals hyperparakeratosis and orthokeratosis in a checkerboard pattern with hyperkeratotic plugging of a hair follicle. The clinical - pathologic findings are consistent with pityriasis rubra pilaris.
Differential diagnosis
- Psoriasis (especially guttate):
- Increased papillary dermal vascular ectasia
- More parakeratosis
- More likely to have hypogranulosis and intracorneal neutrophils
- Digitate dermatosis (small plaque parapsoriasis):
- More lymphocyte exocytosis
- Less prominent orthoparakeratotic hyperkeratosis
- Sézary syndrome:
- Atypical lymphocytes (large, hyperchromatic or convoluted nuclei) in a sparse dermal infiltrate (Semin Cutan Med Surg 2018;37:18)
- Phrynoderma (vitamin A deficiency):
- Less psoriasiform epidermal hyperplasia
- CARD14 associated papulosquamous eruption:
- Regular psoriasiform acanthosis with elongated rete ridges
- Lacks acantholysis (J Cutan Pathol 2020;47:425)
Board review style question #1
Board review style answer #1
A. Checkerboard hyperkeratosis pattern. Alternating vertical and horizontal orthoparakeratosis and parakeratosis (checkerboard pattern) is characteristic for PRP. Answer B is incorrect because perivascular lymphocytic infiltrate with hyperkeratosis is more commonly seen in cases of psoriasis. Answer D is incorrect because sparse superficial inflammation is more characteristic of eczema. Answer C is incorrect because psoriasiform patterns can be found in a wide variety of skin disorders and is not specific for PRP.
Comment Here
Reference: Pityriasis rubra pilaris
Comment Here
Reference: Pityriasis rubra pilaris
Board review style question #2
What is the mutation associated with pityriasis rubra pilaris (PRP)?
- BRAF
- CARD14
- KRAS
- TERT
Board review style answer #2
B. CARD14. Mutations in CARD14 have been identified in the familial form of PRP. Answers A and D are incorrect because these mutations are found more commonly in melanomas but not identified in PRP. Answer C is incorrect because KRAS mutations are found in a wide variety of cancers but have not been identified in PRP to date.
Comment Here
Reference: Pityriasis rubra pilaris
Comment Here
Reference: Pityriasis rubra pilaris