Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zalaznick H. Lipoid proteinosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorlipoidproteinosis.html. Accessed January 21st, 2025.
Definition / general
- Autosomal recessive condition caused by mutations in the ECM1 gene, which leads to deposits of hyaline material in the skin and mucosal surfaces
Essential features
- Deposits of PAS and PASD positive homogenous, eosinophilic material in the dermis and lamina propria corresponding clinically to waxy yellowish white lesions
- Variable clinical presentation (see clinical features below)
- Autosomal recessive inheritance
Terminology
- Also known as hyalinosis cutis et mucosae or Urbach-Wiethe disease
Epidemiology
- Men and women are equally affected
- Typically occurs in consanguineous families
- Rare, only a few hundred known patients
- Increased incidence in South Africa (likely due to founder mutation, Mol Syndromol 2016;7:26)
Pathophysiology
- Uncertain
- ECM1 (extracellular matrix protein 1) is a component of the extracellular matrix and patients with LP lack functional ECM1 - this leads to hyaline deposits through an unknown mechanism
Etiology
- Autosomal recessive disease
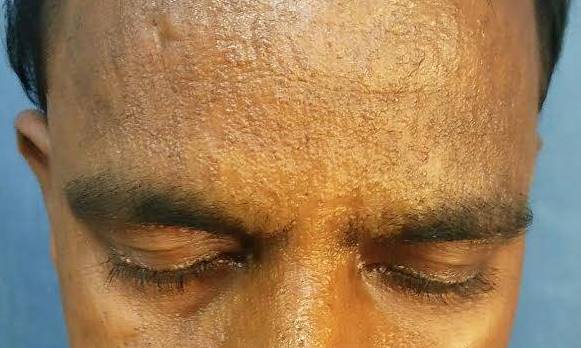
Clinical features
- Clinical features are variable but include (Vahidnezhad: GeneReviews - Lipoid Proteinosis, 2016):
- Hoarse cry as an infant, hoarse voice
- Moniliform blepharosis (papules on the eyelid margins)
- Vesicles with hemorrhagic crust on skin and oral mucosa in early lesions
- Lesions evolve into waxy yellowish white papules, nodules or plaques
- Poor wound healing
- Calcifications in the brain, particularly a "bean shaped" calcification above the pituitary fossa
- Seizures
- Behavioral issues such as memory impairment, paranoia, aggressive behavior, hallucinations and lack of fear (involvement of the amygdala)
- Parotitis and poor dental hygiene
- Upper respiratory infections
- Shortened tongue, difficulty in protruding tongue
- Patchy alopecia
Diagnosis
- Clinical suspicion followed by sequencing of the ECM1 gene
- Biopsy may be helpful but is not required for the diagnosis
Laboratory
- There are no specific laboratory findings
Radiology description
- Brain CT can identify calcifications but is not needed for diagnosis
Prognostic factors
- Patients with lipoid proteinosis have a normal life expectancy
- However, deposits in the larynx can lead to airway obstruction and may need to be ablated
Case reports
- 26 year old man presented with a three year history of itchy lesions (Case #433)
- 37 year old woman presenting with progressive mouth dryness (Pathol Res Pract 1998;194:855)
- Woman with exclusive and complete bilateral amygdala destruction (Wikipedia: S.M. (Patient) [Accessed 4 August 2020])
Treatment
- Lesions can be excised or ablated but there is no curative treatment
Gross description
- Skin or mucosa with waxy yellowish white nodules
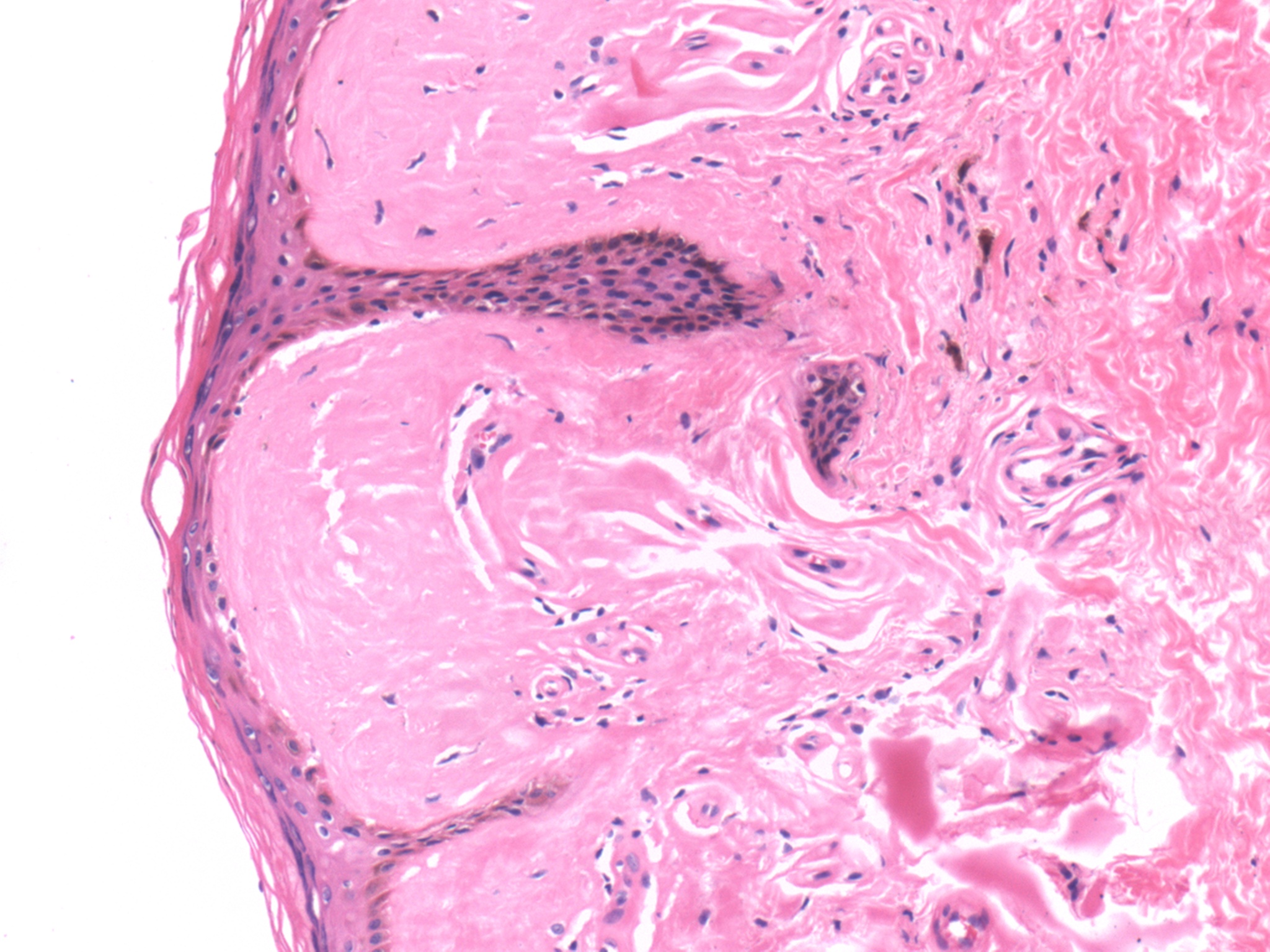
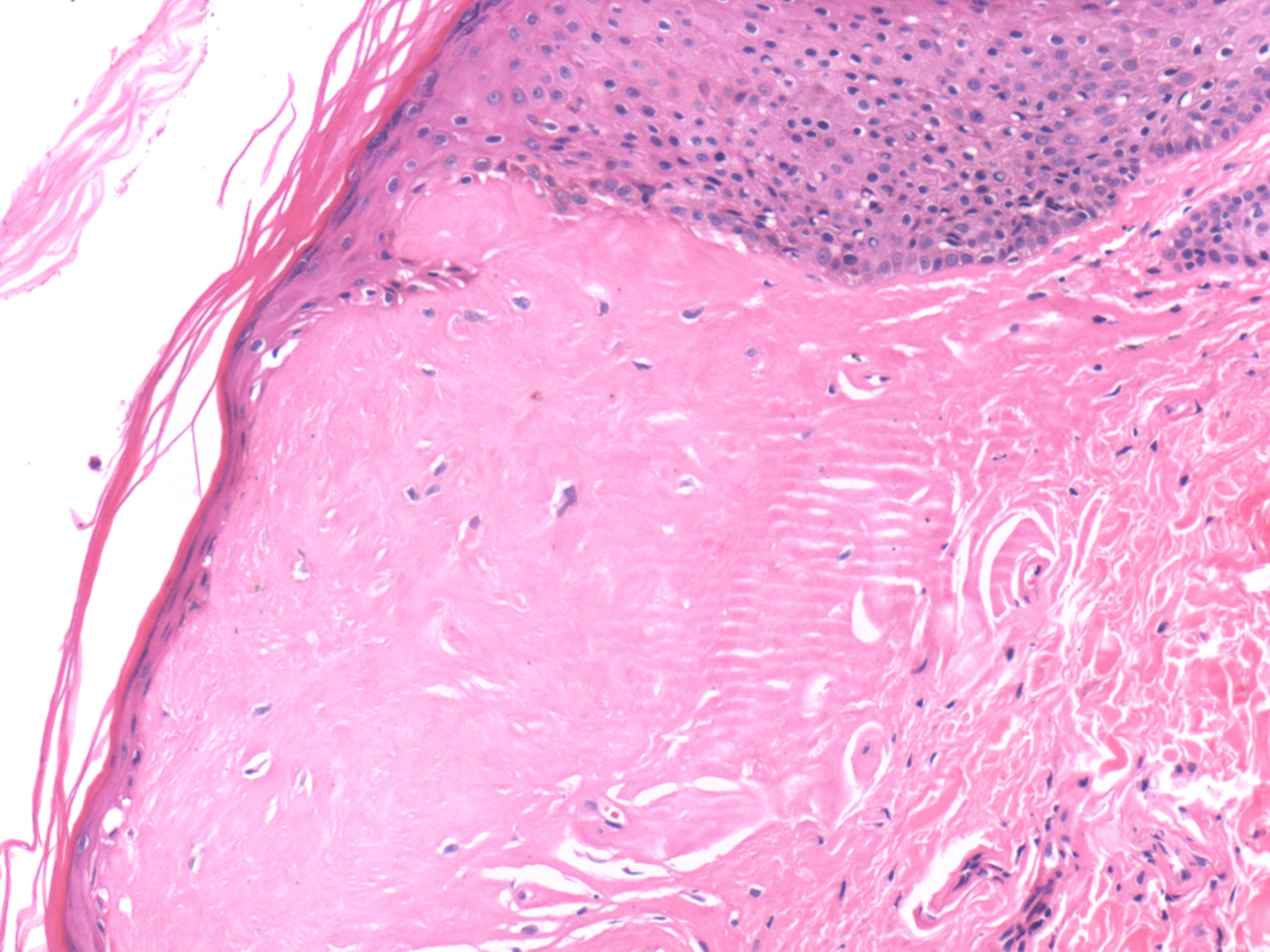
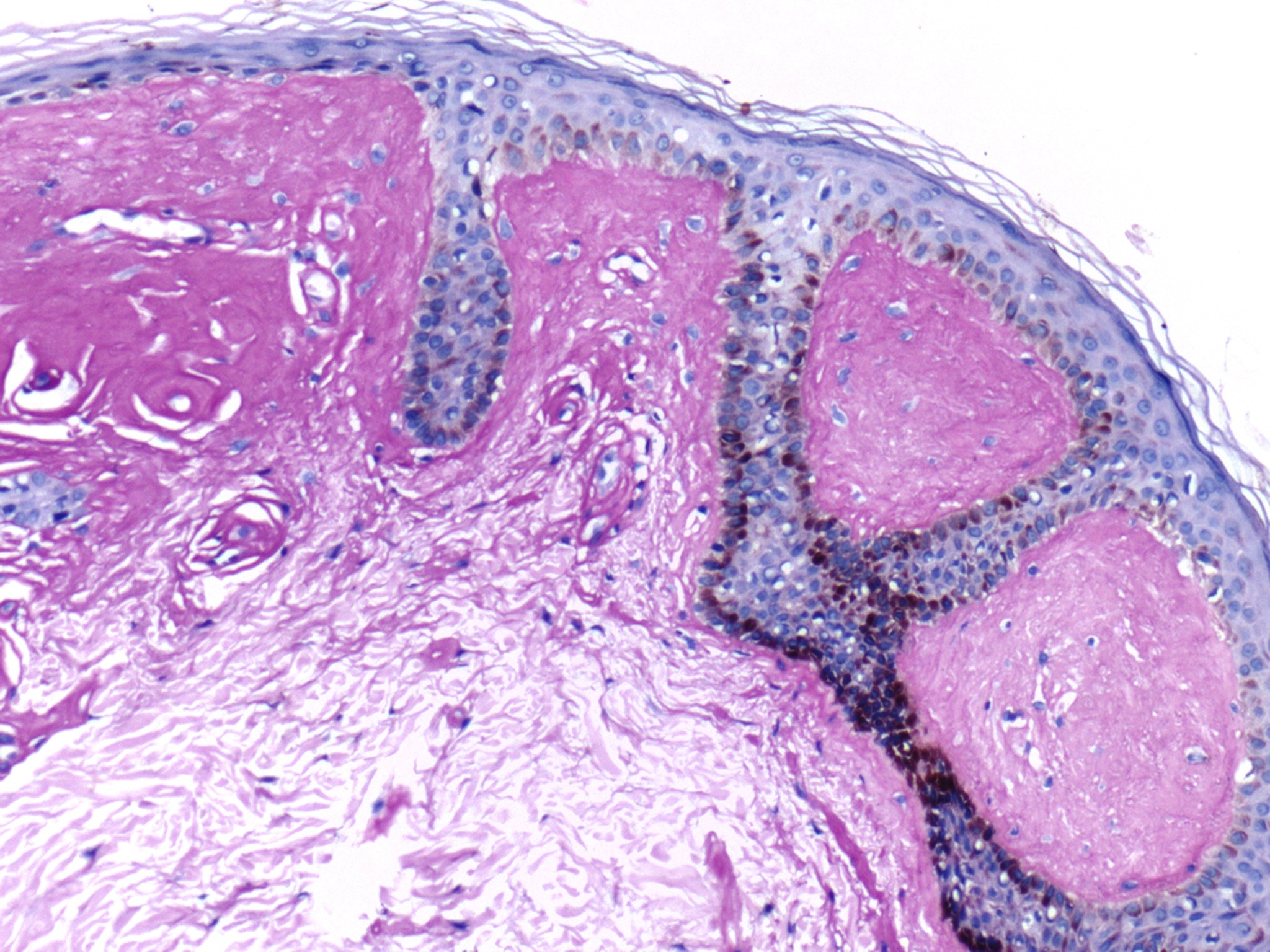
Microscopic (histologic) description
- Amorphous, eosinophilic mostly acellular hyaline material in the papillary dermis and extending around sweat glands and blood vessels
- In mucosal biopsies can be seen surrounding salivary gland acini
Microscopic (histologic) images
Positive stains
Negative stains
- Congo red, immunofluorescence for ECM1 (J Dermatol Sci 2004;35:151)
Differential diagnosis
- Amyloidosis
- Deposits are similar on H&E but special stains for amyloid will be positive
- Porphyria
- Histologic appearance of early lesions in lipoid proteinosis can be similar to those of porphyria
- Both show hyaline deposits involving blood vessels
- Lesions in porphyria are limited to sun exposed areas, which is not true of lipoid proteinosis
- Smokeless tobacco keratosis (Arch Pathol Lab Med 2004;128:e17)
- Similar deposits of amorphous, eosinophilic PAS and PASD+ material in the lamina propria around vessels and salivary glands
- More focal than lipoid proteinosis and limited to oral cavity
- Lesions of smokeless tobacco keratosis are reversible when use of smokeless tobacco products is discontinued
Additional references
Board review style question #1
The deposits seen in lipoid proteinosis are:
- Known to be made of amyloid AA
- Negative for PASD
- Positive for Congo red
- Positive for PAS
Board review style answer #1
D. The deposits in lipoid proteinosis are positive for PAS, positive for PASD, negative for Congo red and are of unknown composition (but are not amyloid)
Comment Here
Reference: Lipoid proteinosis
Comment Here
Reference: Lipoid proteinosis
Board review style question #2
The histologic appearance of lipoid proteinosis is best described as:
- An infiltrate of histiocytes and foreign body giant cells engulfing elastotic fibers
- Dense, band-like lymphocytic infiltrate in dermis that obscures the dermoepidermal junction
- Hyaline deposits in the dermis, particularly around blood vessels and sweat glands
- Marked fatty infiltration of the dermis
- Orthokeratotic hyperkeratosis and papillomatosis of stratum spinosum
Board review style answer #2
C. Hyaline deposits in the dermis, particularly around blood vessels and sweat glands
Comment Here
Reference: Lipoid proteinosis
Comment Here
Reference: Lipoid proteinosis