Table of Contents
Definition / general | Terminology | Epidemiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) images | Cytology description | Positive stains | Differential diagnosisCite this page: Do HK. Candida. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorfungicandida.html. Accessed March 30th, 2025.
Definition / general
- Candida albicans is a part of the normal human skin flora
- Cutaneous candidiasis is a superficial infection of skin and mucous membranes and the most common Candidal infection
Terminology
- Cutaneous candidal infections include:
- Oral candidasis
- Candidal intertrigo (affects body folds): acute (wet and red), subacute (red +/- maceration), or chronic (red and dry)
- Candidal diaper dermatitis
- Candidal vulvovaginitis
- Candidal balanitis
- Candidal nail infection: chronic paronychia, onycholysis
Epidemiology
- In U.S., Candida species are a common cause of intertrigo in both elderly and diabetic patients
- Candida species colonize the oropharynx in 30 - 55% of healthy young adults, and are commonly found in normal fecal flora
- 3 out of 4 women will have at least one Candidal vulvoganitis during their lifetime
- For patients with systemic infections, Candida species is now the 4th most common pathogen from blood cultures
- More than 90% of HIV population who are not on highly active antiretroviral therapy will develop oropharyngeal candidiasis and 10% develop esophageal candidasis
- Internationally, Candida species have replaced Cryptococcus species as the most common fungal pathogens affecting immunocompromised hosts
Clinical features
- Predisposing factors for opportunistic infection with C. albicans include:
- Infancy or elderly
- Warm climate
- Occlusive clothing, poor personal hygiene, dental plates
- Immune deficiencies (low levels of immunoglobulins, HIV, cancer)
- Broad spectrum antibiotic treatment
- High dose estrogen contraceptive pills or pregnancy
- Chemotherapy or immunosuppressive medications such as systemic steroids
- Locally applied topical steroids
- Diabetes mellitus, obesity, Cushing syndrome and other endocrine conditions
- Iron deficiency
- Malnutrition
- Underlying dermatological disease like psoriasis, lichen planus, irritant contact dermatitis
- Mortality is relative low for cutaneous Candidal infection in healthy patients; however, the mortality rate is up to 30 - 40% in disseminated / systemic candidasis in immunosuppressed patients
- The characteristic skin manifestation is red and white patches on mucosal surfaces (leukoplakia)
- In skin folds, it results in moist fissuring with a superfical erythema patch with satellite papulopustules
Diagnosis
- KOH preparation and skin scraping is the easiest and most cost effective method for diagnosing cutaneous candidiasis
- Culture from intact pustule or skin biopsy tissue can support the diagnosis
Case reports
- Extensive cutaneous candidiasis revealing cutaneous T cell lymphoma: 2 cases (Ann Dermatol Venereol 2006;133:566)
Treatment
- Note: please confirm accuracy of medications below before use
- Oral candidiasis:
- Nystatin oral suspension x 10 - 14 days or until 48 - 72 hours after resolution of symptoms
- Dosage for preterm infants is 0.5 mL (50,000 U) to each side of mouth 4 times / day; for infants is 1 mL (100,000 U) to each side of the mouth 4 times/d; for adults 4 - 6 mL (100,000 U) PO swish and swallow qid
- Candidal intertrigo:
- Keep the skin dry, with the addition of topical nystatin powder, clotrimazole, or miconazole twice daily, often in conjunction with a midpotency corticosteroid
- Extensive infection may require the addition of fluconazole (100 mg PO qd for 1 - 2 wk) or itraconazole (100 mg PO qd for 1 - 2 wk)
- Acute intertrigo:
- Can use Domeboro solution, Castellani paint or vinegar/water (1 tbsp vinegar per quart room-temperature water) to apply twice per day for 5 - 10 minutes for 3 - 5 days as needed
- Dry the area with a hair dryer (low heat)
- Can also apply triamcinolone-nystatin cream twice daily
- Subacute intertrigo:
- Can use benzoyl peroxide wash to cleanse the area instead of application of vinegar or Castellani paint
- A topical anticandidal cream of choice is applied twice per day, with or without a mild hydrocortisone cream
- Chronic intertrigo:
- Can use zinc-talc shake lotion once or twice daily, and the hydrocortisone cream / antifungal mixture may be applied at night
- Local hyperhidrosis may be treated with antiperspirants (ie, Arid Extra Dry Unscented, Dry Idea) on a long-term basis
- Candidal diaper dermatitis:
- Goal is to minimize the time the diaper area is exposed to hot and humid conditions; air drying, frequent diaper changes and generous use of baby powders and zinc oxide paste are adequate preventive measures
- Apply topical nystatin, amphotericin B, miconazole or clotrimazole to affected areas twice daily x 7 days
- Candidal vulvovaginitis:
- Topical antifungal agents (Micatin, Monistat-Derm), or clotrimazole (Lotrimin, Mycelex) creams twice daily x 7 days or intravaginal appliator QHS x 7 days are curative
- One-time oral therapy with fluconazole (150 mg) or itraconazole (600 mg) is effective and may be a more attractive alternative to some patients, but it is more costly
- Candidal balanitis:
- Topical therapy is effective in most patients
- Evaluate asymptomatic sexual partners and treat them if they are infected to prevent recurrence
- For persistent lesions beyond the genitalia, consider the possibility of underlying diabetes or other diseases
- Candidal paronychia:
- Topical treatment is usually not effective but should be tried for chronic candidal paronychia
- Drying solutions or antifungal solutions are used
- Oral therapy with either itraconazole (pulse dosing with 200 mg bid for 1 wk of each of 3 consecutive months) or terbinafine (250 mg qd for 3 months) is recommended
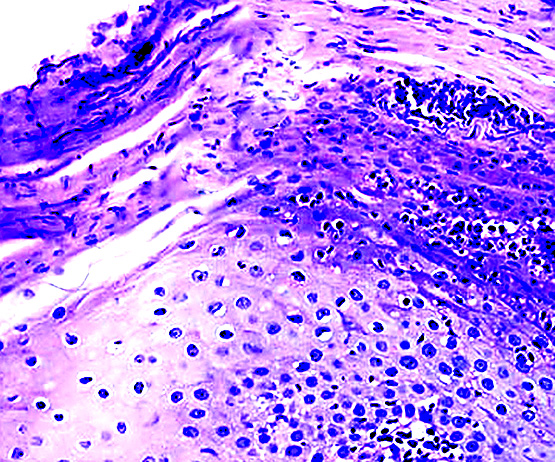
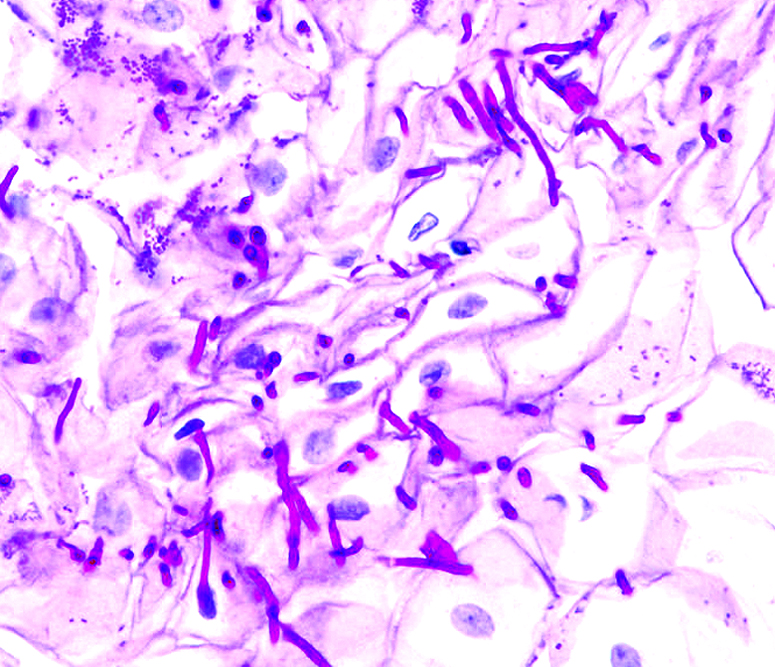
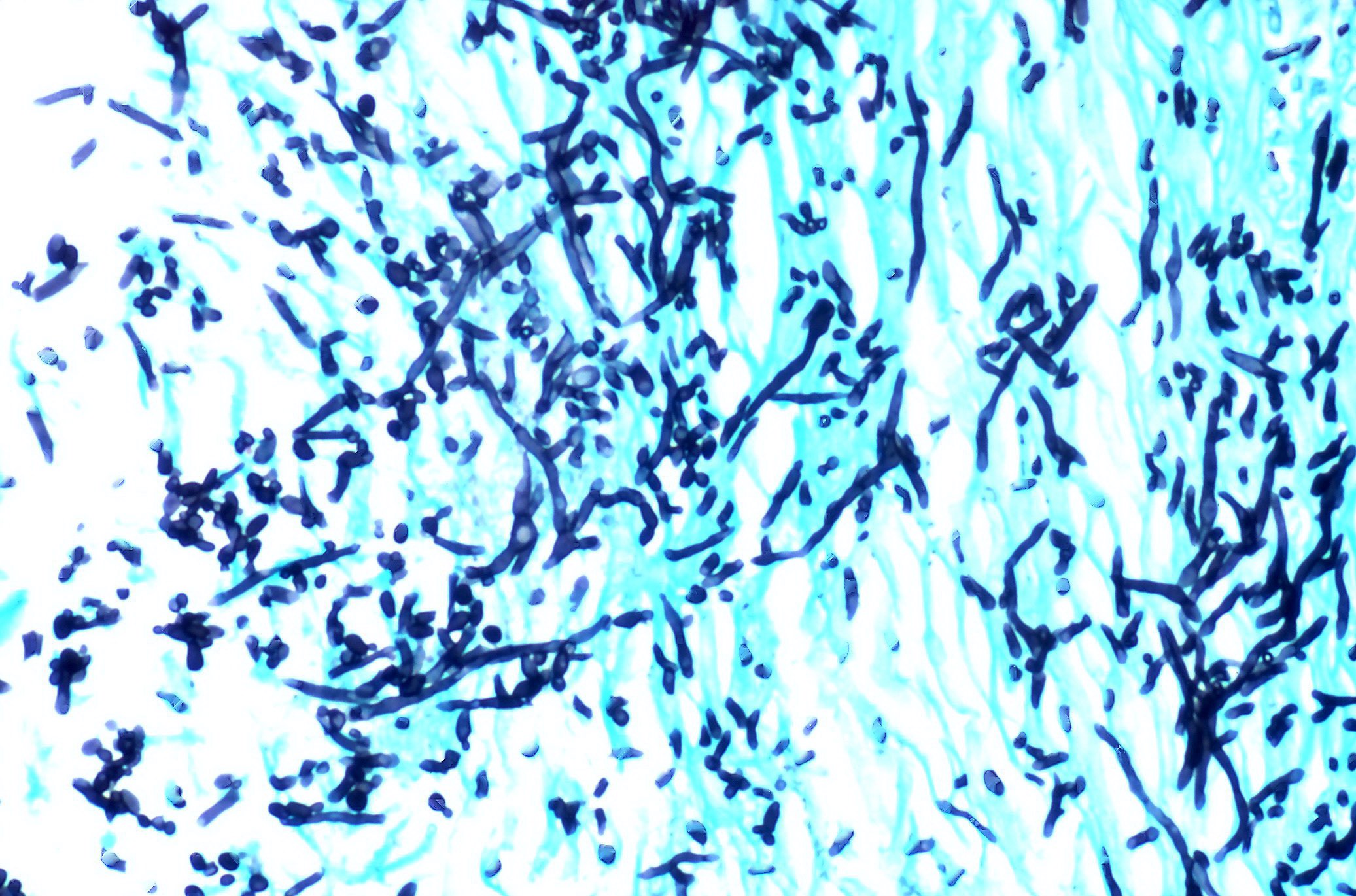
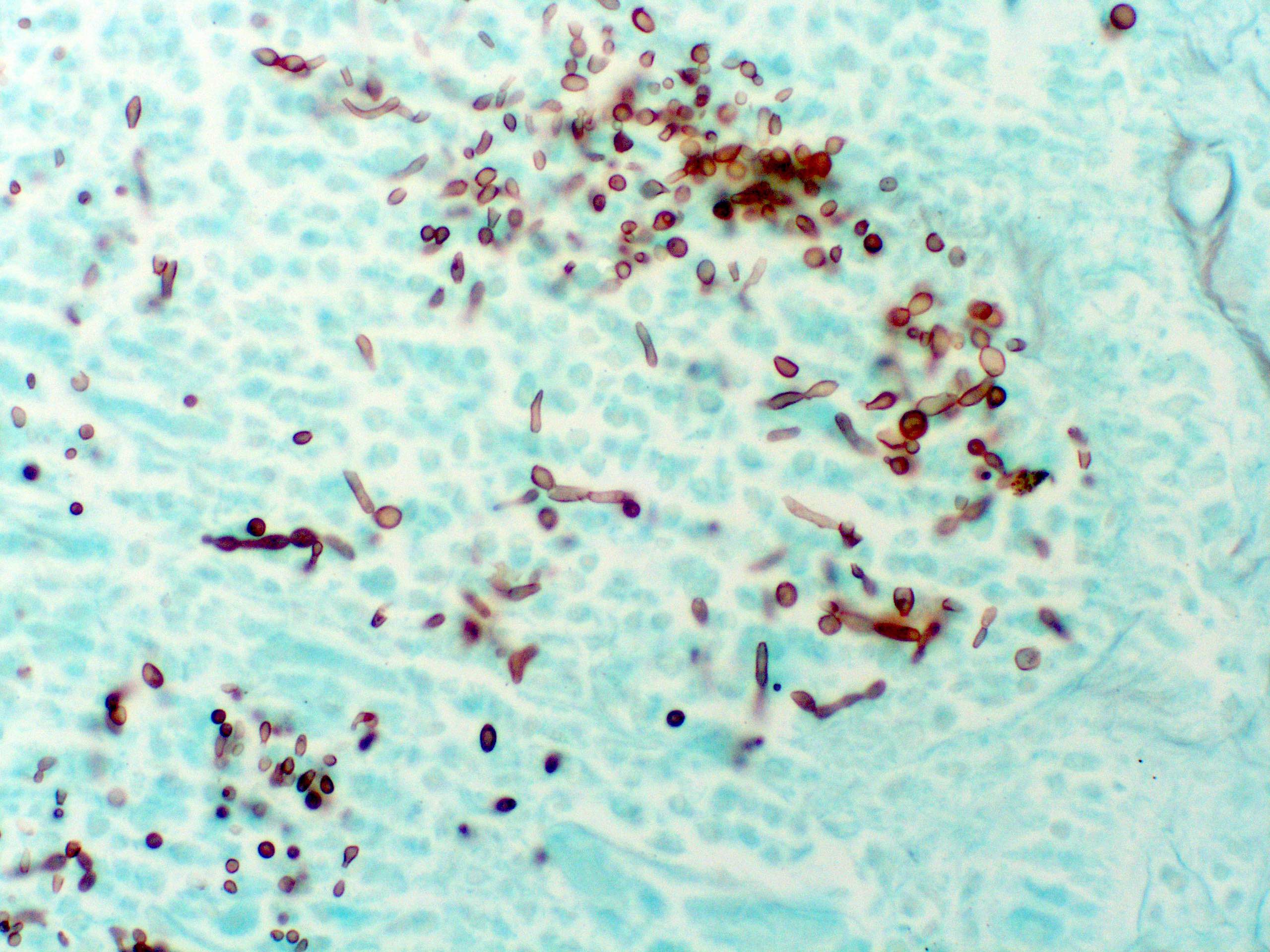
Microscopic (histologic) images
Cytology description
- Periodic Acid-Schiff (PAS) stain reveals nonseptated hyphae, which distinguishes Candida from tinea
Positive stains
- GMS, PAS
Differential diagnosis
- Bacterial vaginosis
- Contact dermatitis with or without colonization
- Intertrigo
- Inverse psoriasis
- Onychomycosis
- Pseudomonas nail bed infection
- Radiation dermatitis
- Seborrheic dermatitis
- Trichomonas infection