Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Collie CJ, Ho JD. Folliculitis decalvans. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorfolliculitisdecalvans.html. Accessed December 2nd, 2024.
Definition / general
- Folliculitis decalvans is a neutrophilic scarring alopecia characterized by pustules, perifollicular erythema and follicular tufting
Essential features
- Neutrophilic scarring alopecia variant
- More common in men
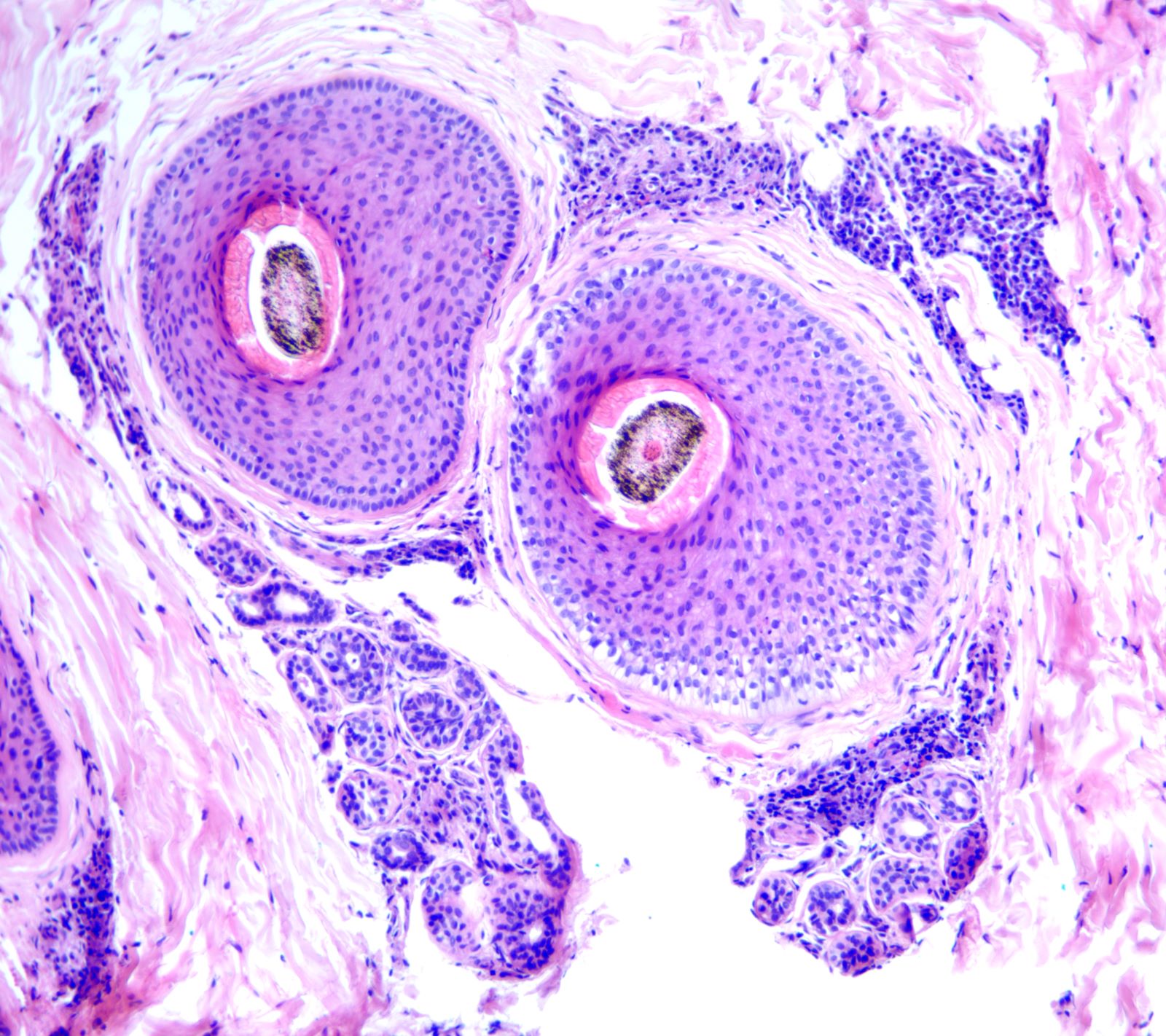
- Presents with scarring alopecia, follicular pustules and resultant compound follicles that give the clinical appearance of tufting
- Typical histologic findings include a dense neutrophilic and mixed inflammatory cell infiltrate involving the upper follicle with accompanying perifollicular and interfollicular fibrosis, loss of sebaceous glands and compound follicle formation
- Staphylococcus aureus may be cultured from pustules but their pathogenic role is unclear
- Untreated disease may result in extensive and irreversible hair loss
- Reference: Dermatol Ther 2008;21:238
Epidemiology
- Limited data but accounts for ~10% of primary cicatricial alopecia in some series (J Am Acad Dermatol 2004;50:25)
- More common in males (J Dermatol 2018;45:450)
- Considered to be the most common neutrophilic scarring alopecia encountered in clinical practice (Skin Appendage Disord 2019;5:309)
Sites
- Scalp; occipital and vertex areas are favored (Dermatol Ther 2008;21:238)
- Rarely involves beard (Indian J Dermatol Venereol Leprol 2021;87:569)
Pathophysiology
- Poorly understood
- S. aureus may act as a superantigen to induce T cell activation (Dermatol Ther 2008;21:238)
- Genetic predisposition has been suggested in some patients (Br J Dermatol 2000;143:195)
Etiology
- Possible role for S. aureus
Clinical features
- Patients frequently complain of pain, pruritus and a burning scalp sensation (Dermatol Ther 2008;21:238)
- Presents with erythematous papules and pustules, which eventuate in patches of scarring hair loss
- Pustules may be present around the periphery of scarred areas (Indian J Dermatol Venereol Leprol 2021;87:569)
- Aberrant healing of destroyed infundibular epithelium results in numerous terminal hairs protruding from one follicular ostium (compound follicles or tufting)
- Reported dermoscopic findings include a lack of follicular ostia, tufted hairs, perifollicular starburst pattern and yellow crusts (J Am Acad Dermatol 2021;85:1185)
- Extensive scarring may be seen in longstanding disease
Diagnosis
- History (sex, presence of pustules, location of hair loss)
- Examination (findings as discussed above)
- Biopsy
Prognostic factors
- If untreated, may lead to extensive scarring (J Am Acad Dermatol 2021;85:1185)
- Timely treatment in patients with visible remaining terminal or vellus hairs in involved areas may lead to retention of hair
- Squamous cell carcinoma may occur at sites of longstanding, untreated disease (Dermatol Online J 2019;25:13030)
Case reports
- 32 year old man with folliculitis decalvans and concomitant orofacial granulomatosis (Postepy Dermatol Alergol 2018;35:317)
- 45 year old man with bilateral erythematous pustular lesions on the cheeks in the beard area (Indian J Dermatol Venereol Leprol 2021;87:569)
- 45 year old man with a longstanding history of folliculitis decalvans develops metastatic squamous cell carcinoma (Dermatol Online J 2019;25:13030)
- 52 year old Hispanic man with a longstanding history of folliculitis decalvans develops squamous cell carcinoma (JAAD Case Rep 2021;15:42)
Treatment
- Generally, topical / systemic antibiotics and anti-inflammatory agents are the mainstay of treatment as listed below (Dermatol Ther 2008;21:238, Acta Derm Venereol 1992;72:143, Singapore Med J 2003;44:84)
- Topical antiseptics / antibiotics
- Topical / intralesional steroids
- Systemic antibiotics (tetracyclines, fusidic acid, cotrimoxazole, erythromycin)
- Prednisone
- Zinc sulfate supplements
Clinical images
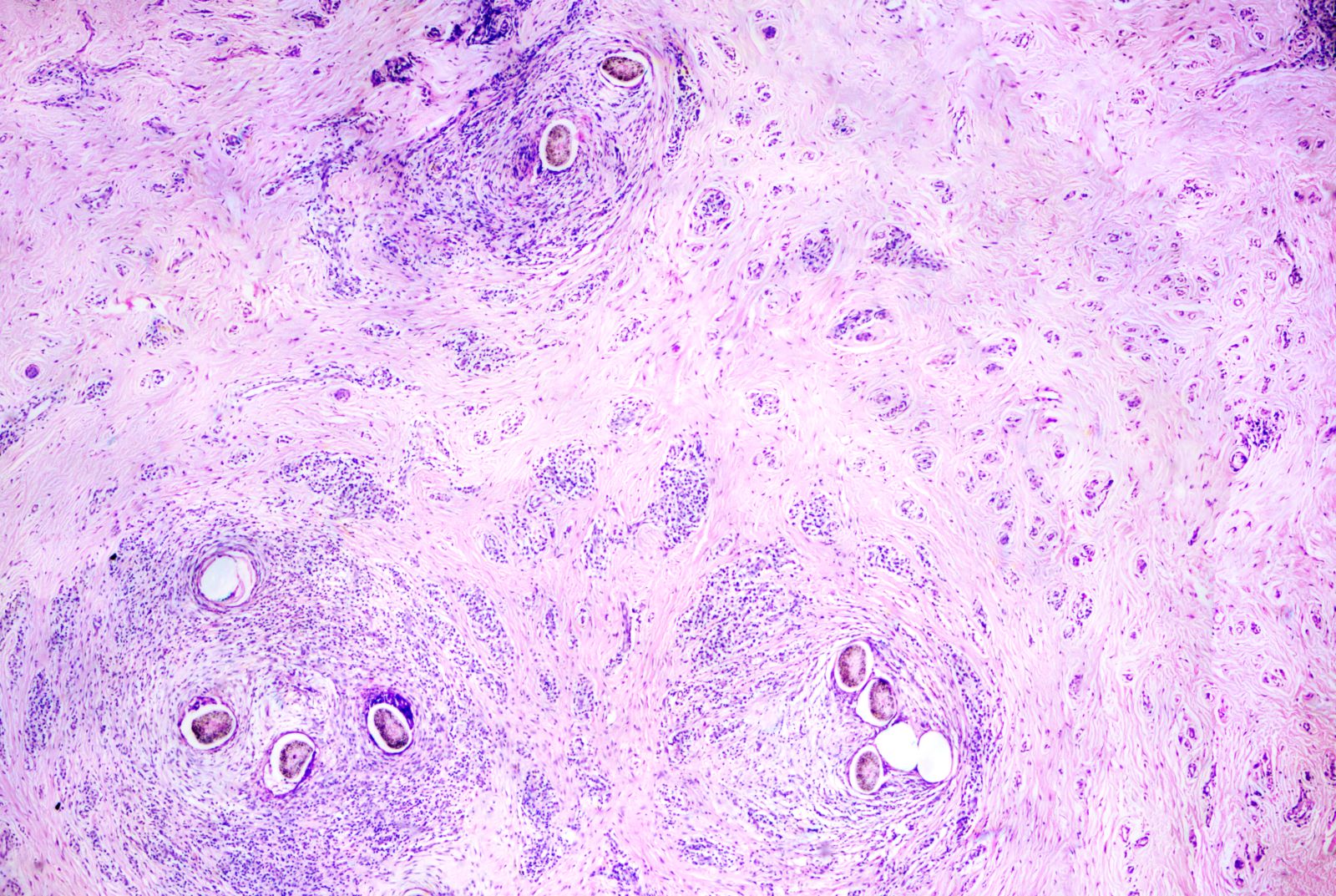
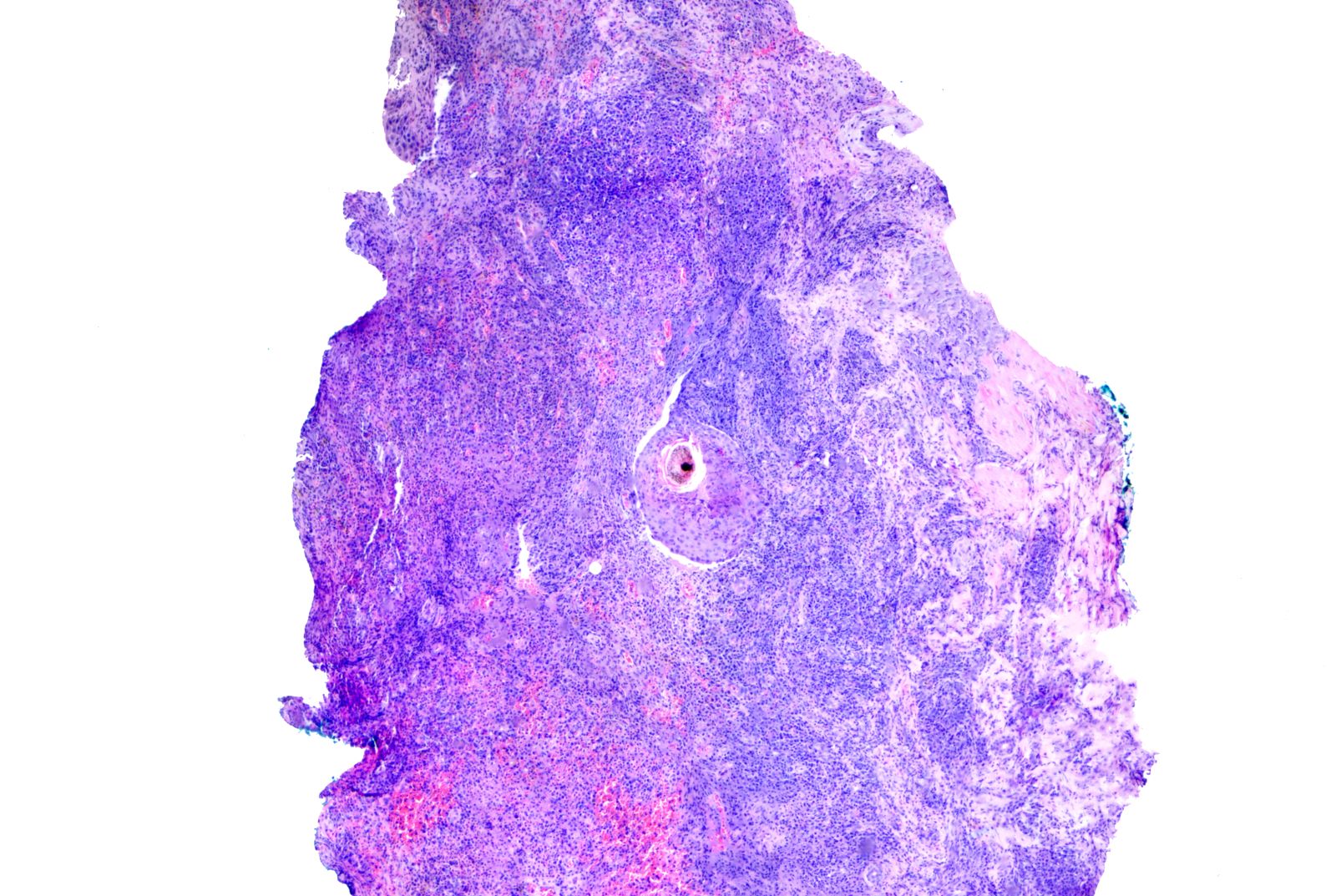
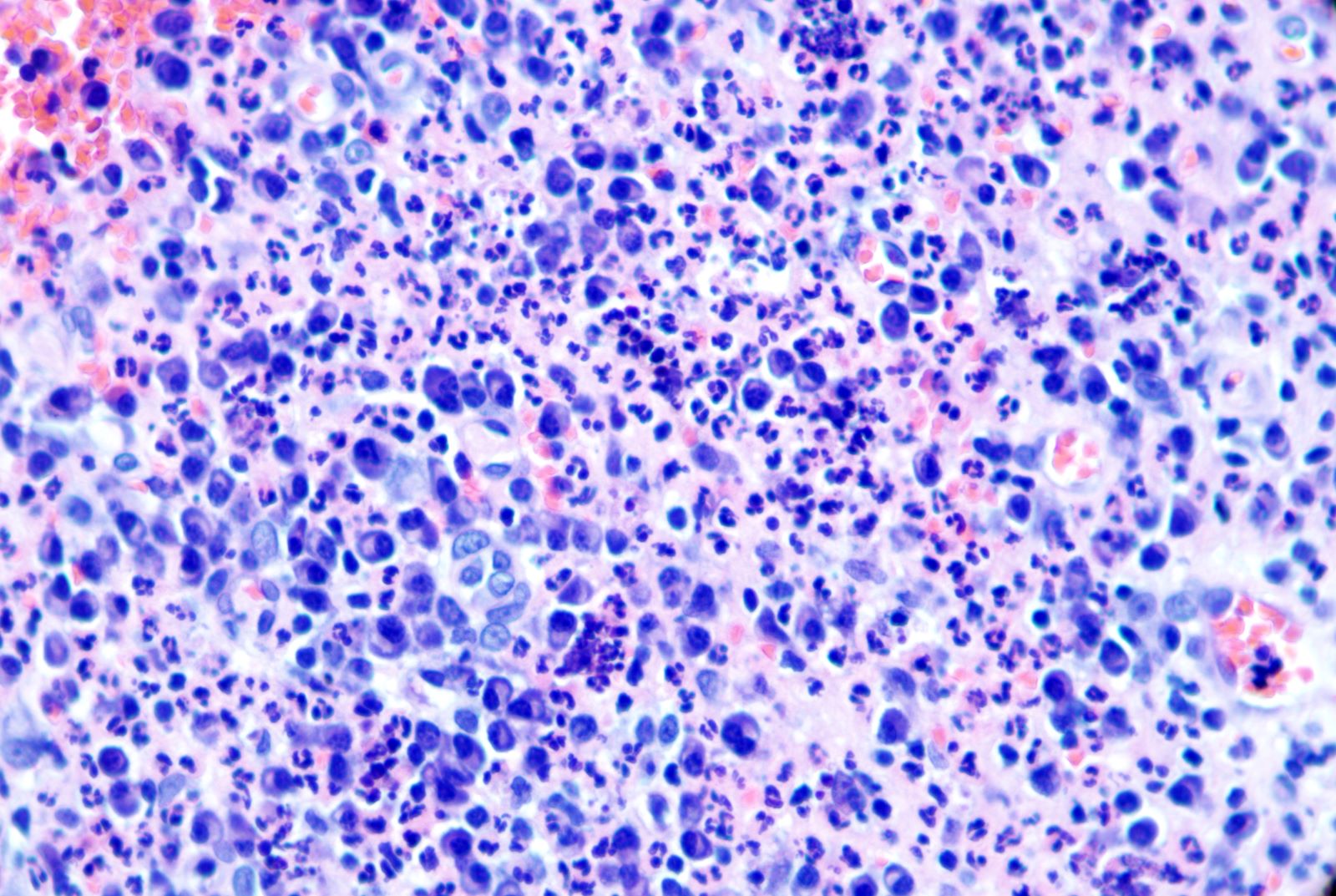
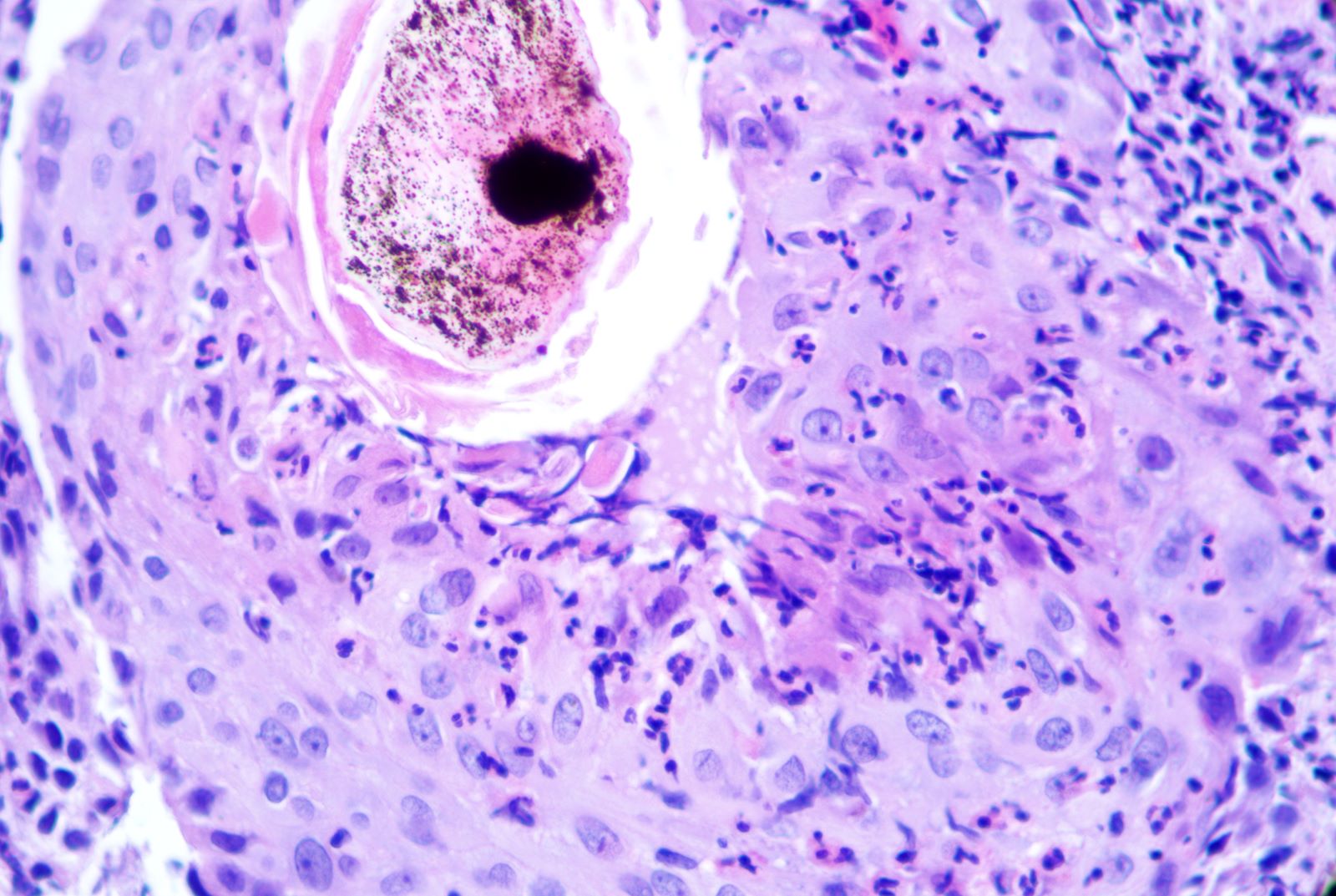
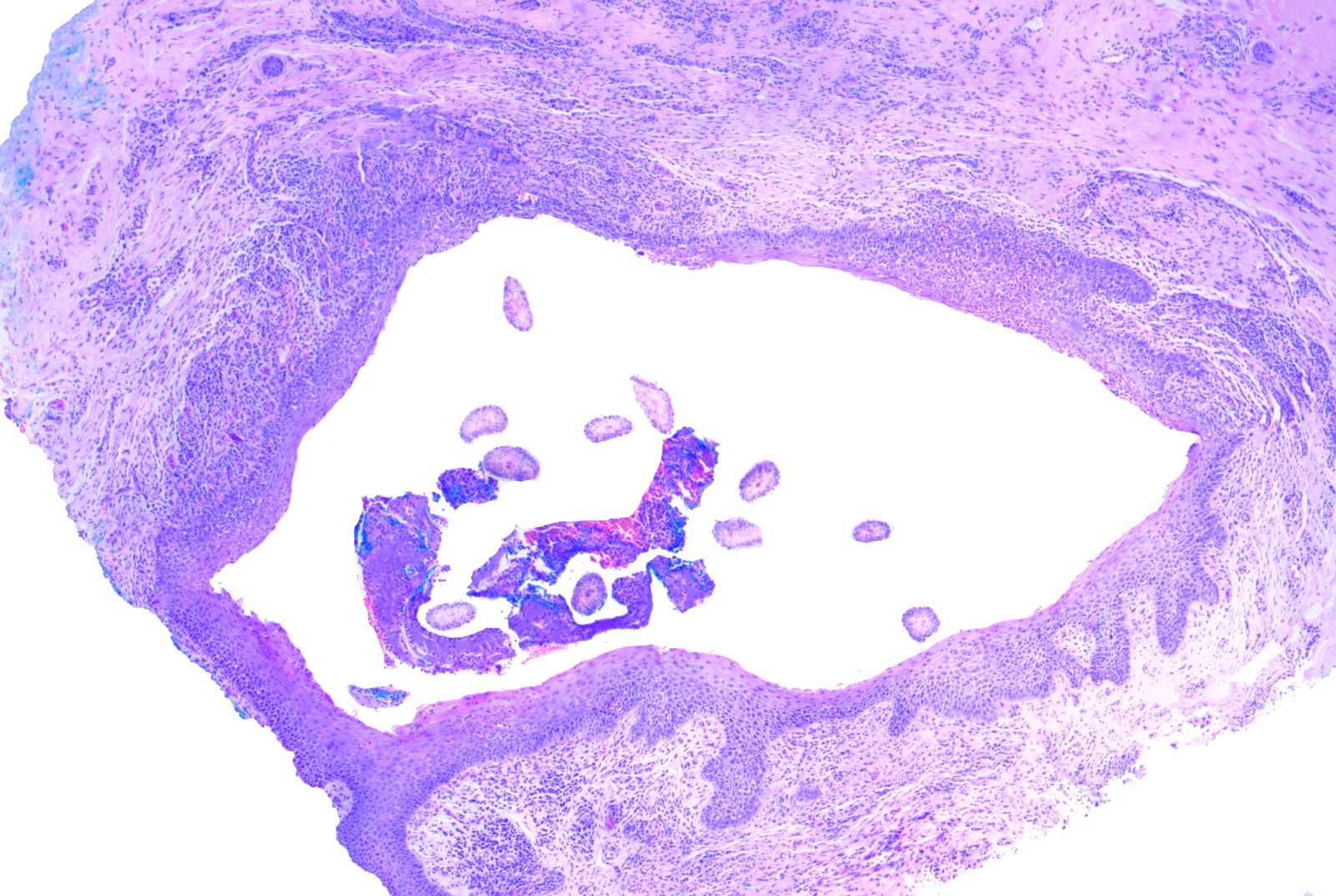
Microscopic (histologic) description
- Folliculitis decalvans is a "top heavy" disease; i.e., the upper follicle (isthmus to infundibulum) is affected more than the inferior follicle (Dermatol Ther 2008;21:238, Br J Dermatol 1998;138:799)
- Like most alopecias, features best appreciated on transversely grossed 4 mm punch biopsy
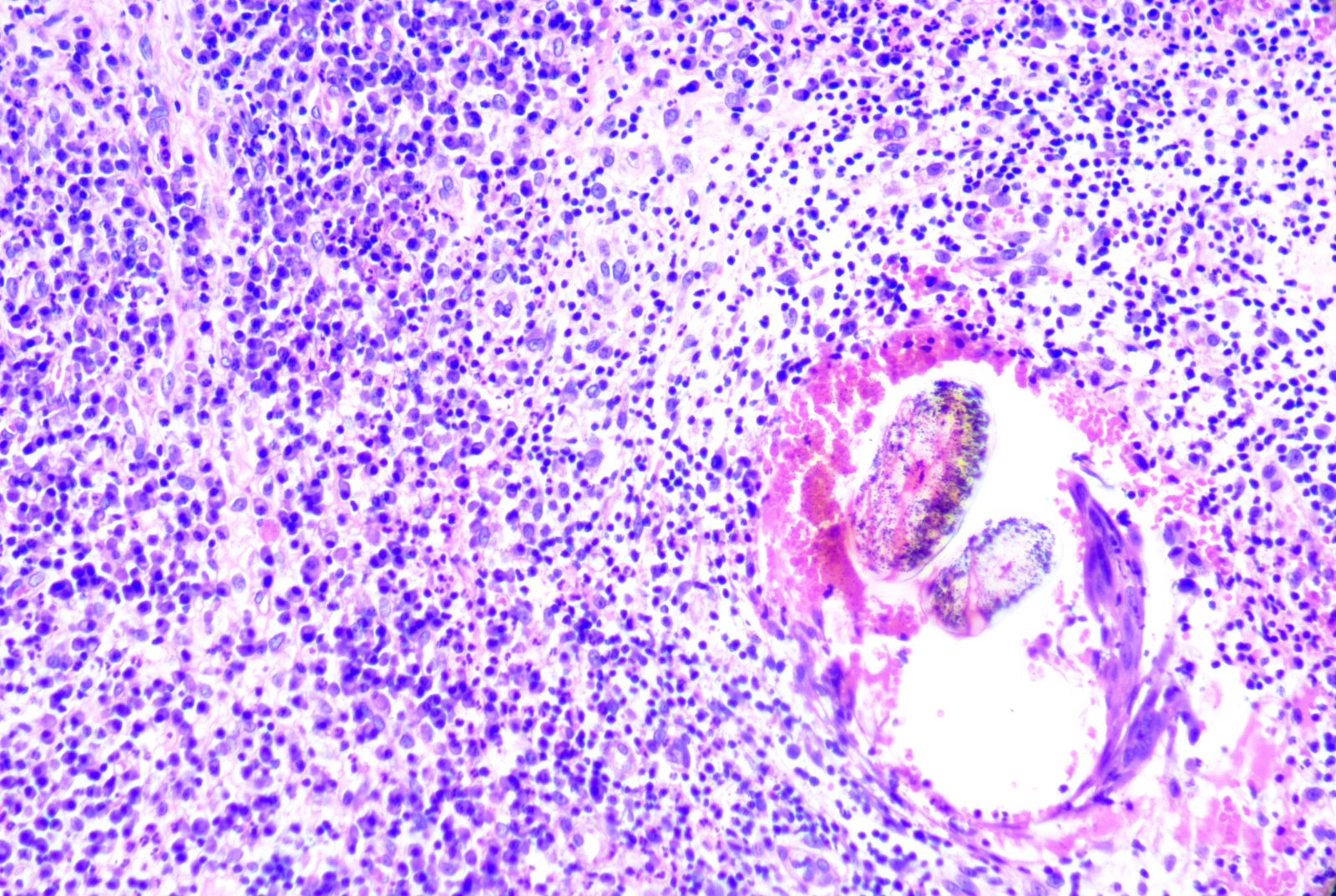
- Inflammation
- Variably dense perifollicular and interfollicular neutrophilic infiltrate heaviest towards the upper follicle (isthmus to infundibulum) (J Am Acad Dermatol 2016;75:1101)
- Intrafollicular pustules may occur in acute / active disease (J Am Acad Dermatol 2021;85:1185)
- Mixed inflammatory cells including plasma cells, eosinophils, lymphocytes and histiocytes are common (J Am Acad Dermatol 2021;85:1185)
- In additional to perifollicular inflammation, the infiltrate is often interfollicular or perivascular
- In the authors' experience, many cases have a predominantly lymphoplasmacytic infiltrate with no discernible neutrophils, particularly in longstanding disease
- Fibrosis pattern
- Concentric perifollicular fibrosis (Histopathology 2010;56:24)
- Interfollicular fibrosis (very suggestive of folliculitis decalvans) (Histopathology 2010;56:24, J Am Acad Dermatol 2021;85:1185)
- Deep fibrous tracts replacing follicles with significant drop out in later lesions (Histopathology 2010;56:24)
- General features common to scarring alopecias
- Loss of sebaceous glands (J Am Acad Dermatol 2021;85:1185)
- Decreased follicular counts
- Dilated eccrine glands (Am J Dermatopathol 2019;41:871)
- Follicular destruction with naked hair shafts and a foreign body granulomatous reaction are common in very inflammatory disease (Am J Dermatopathol 2018;40:498)
- Epidermal changes
- Compound follicles defined as multiple hair shafts (often in groups of 4 - 10 hairs) contained within 1 dilated follicular ostium (Histopathology 2010;56:24, J Am Acad Dermatol 2016;75:1101, Br J Dermatol 1998;138:799)
- Epidermal acanthosis (early disease) (J Am Acad Dermatol 2021;85:1185)
Microscopic (histologic) images
Positive stains
- Gram stain may reveal gram positive cocci in clusters consistent with S. aureus
- Not routinely performed
Sample pathology report
- Skin, scalp, punch biopsy:
- Neutrophilic scarring alopecia consistent with folliculitis decalvans (see comment)
- Comment: Transverse sections reveal 10 hairs in anagen and terminal in size. Sebaceous glands are markedly reduced in number. There is a moderately dense perifollicular, interfollicular and perivascular inflammatory cell infiltrate composed of neutrophils, plasma cells, lymphocytes and scattered eosinophils. Intrafollicular neutrophils with superficial pustule formation are seen. The inflammation increases in density towards the infundibulum. There is both concentric perifollicular fibrosis and interfollicular fibrosis. Fibrous tracts and naked hair shafts with a focal foreign body granulomatous reaction are present at deeper levels. Compound follicles in groups of up to 8 hairs are identified. The overlying epidermis is acanthotic and scale crust containing neutrophils are present. PAS stain is negative for fungal elements.
Differential diagnosis
- Dissecting cellulitis / folliculitis of the scalp (perifolliculitis capitis abscedens et suffodiens) (Histopathology 2010;56:24):
- Another form of neutrophilic scarring alopecia
- Primarily in young black men with large pus filled nodules on the scalp and scarring alopecia
- Bottom heavy mixed inflammatory cell infiltrate resembling granulation tissue in the deep dermis and subcutis
- May have sinus tract formation
- Tinea capitis:
- PAS positive fungi within hair shafts
- Central centrifugal cicatricial alopecia (Clin Cosmet Investig Dermatol 2016;9:175):
- Black women
- Progressive and symmetric peripheral expansion of the lesions
- Lymphocyte predominant inflammatory cell infiltrate in the upper portion of the hair follicle
- Perifollicular but no interfollicular fibrosis
- With follicular rupture, occasional neutrophils may be seen but compound follicles of > 4 hairs are unusual in this entity
- Lichen planopilaris / frontal fibrosing alopecia (Int J Dermatol 2006;45:375):
- Patients with patches of scarring alopecia or loss of frontal hairline; more common in White women but may occur in persons of either sex and any race / ethnicity
- Lymphocytic scarring alopecia
- Perifollicular but no interfollicular fibrosis
- Basal layer vacuolation of the follicular epithelium
Additional references
Board review style question #1
A 25 year old man presents with hair loss involving the vertex of the scalp. Examination reveals numerous pustules, scarring and multiple hairs exiting through a single follicular ostium. A punch biopsy demonstrates the features shown in the associated photomicrographs. PAS stain is negative for fungal elements. What is the most likely diagnosis?
- Folliculitis decalvans
- Frontal fibrosing alopecia
- Lichen planopilaris
- Male pattern hair loss
- Tinea capitis
Board review style answer #1
A. Folliculitis decalvans. This is folliculitis decalvans, which is a neutrophilic scarring alopecia characterized by scarring alopecia, a neutrophilic / mixed inflammatory cell infiltrate and compound follicles (numerous hair shafts in one follicular ostium). Answers B and C are incorrect because frontal fibrosing alopecia and lichen planopilaris are lymphocytic scarring alopecias and do not typically present with pustules. Answer D is incorrect because pattern hair loss is a noncicatricial alopecia characterized by a decreased terminal to vellus ratio and retention of sebaceous glands. Answer E is incorrect because although tinea capitis may have a significant neutrophilic infiltrate and follicular destruction similar to folliculitis decalvans, the PAS stain should demonstrate fungi within hair shafts. Additionally, compound follicles are not a feature of tinea capitis.
Comment Here
Reference: Folliculitis decalvans
Comment Here
Reference: Folliculitis decalvans
Board review style question #2
Which of the following features favors folliculitis decalvans over dissecting cellulitis of the scalp?
- Concentric perifollicular fibrosis
- Decreased follicular density
- Loss of sebaceous glands
- Neutrophilic infiltrate involving the isthmus and infundibulum
- Premature desquamation of the inner root sheath
Board review style answer #2
D. Neutrophilic infiltrate involving the isthmus and infundibulum. While both folliculitis decalvans and dissecting cellulitis of the scalp are neutrophilic scarring alopecias, folliculitis decalvans involves the superior follicle while the latter involves the inferior follicle. Answers A, B, C and E are incorrect because the features listed are nonspecific may be seen in a variety of scarring alopecias.
Comment Here
Reference: Folliculitis decalvans
Comment Here
Reference: Folliculitis decalvans